1. Introduction
Geriatric hip fractures are considered to be a serious orthopedic problem globally[
1]. The incidence of hip fractures in advanced age is increasing due to the aging society [
2]. Hip fractures are a serious problem in terms of morbidity and mortality, and early detection and early ambulation are important for these patients [
3]. Prolonged immobilization in the postoperative period can lead to pneumonia, heart failure, delirium, muscle weakness and even death in patients [
4]. When early surgery for trauma patients is planned, it is important that the surgeon carefully considers the duration of surgery, soft tissue trauma, the anticipated amount of blood loss, and post-operative resuscitation if necessary [
5].
As a result of biomechanical studies on the surgery of intertrochanteric femur fractures, the dynamic hip screw (DHS), proximal femoral nail (PFN), and proximal femoral nail antirotation (PFNA) methods have been described. While DHS is an appropriate treatment method for stable intertrochanteric fractures, this method is not preferred for unstable fractures [
6]. PFNA, which has a spiral blade, was developed with the aim of providing rotational and angular stability in intertrochanteric fractures [
7]. There are several types of proximal femoral nail (PFN). InterTAN and proximal femoral intramedullary nails, which have an interlocking lag screw and compression screw, provide intraoperative compression and rotational stability [
8].
It is important that the position given to the patient during surgery does not complicate imaging and surgical exposure while enabling fracture reduction. In trochanteric region fractures of the femur, patient positioning can be performed as supine on the radiolucent table, lateral decubitus on the radiolucent table, and supine on the fracture table [
9]. These three types of positioning each have their own advantages and disadvantages.
The fracture table or traction table is commonly used to achieve and maintain reduction in lesions around the hip (hip arthroscopy, minimally invasive hip arthroplasty, fracture fixation). While the traction table provides axial traction on the legs, it prevents traction of the trunk thanks to a perineal post. It also allows for manipulation because the limb parts are articulated. While its important advantages are that an assistant is not required for traction, a single surgeon is usually sufficient, and imaging is easy, among its important disadvantages are perineal nerve damage, inconvenience for obese patients, and the fact that it is expensive [
4,
10].
The important advantages of the lateral decubitus position are its suitability for exposure in obese patients and the fact that it can be performed on all universal tables and allows for movement of the fracture after opening, while its important disadvantages are the need for more than one assistant and the fact that imaging is a problem and that rotation cannot be compared with the other leg [
4].
The important advantages of the supine hemilithotomy position are that it is performed on a radiolucent table based on manual traction, there are no complications caused by continuous traction, and radiological imaging is easy. Its important disadvantages are that a longitudinally adjustable table is required and that two or more assistants are required [
11].
The aim of this study is to clinically and radiologically compare the use of the supine hemilithotomy position, the lateral decubitus position, and the traction table when performing PFN surgery for femoral intertrochanteric fractures in the geriatric age group.
2. Materials and Methods
We created our study retrospectively. Ethics committee approval for the study was obtained from Gaziantep University Ethics Committee. Data were obtained from the hospital electronic data system. Patients who were over 65 years old, had acute femoral intertrochanteric fractures, and underwent osteosynthesis with short PFN between 2020 and 2022 were included in the study.
Patients were followed up for at least one year. Patients who died within one year and patients with less than one year of follow-up were removed from the study. Exclusion criteria were pathologic fracture, open fracture, use of open methods during surgery, use of additional implants, infection in the incision area, blood disease, polytrauma, and severe acute or chronic inflammatory diseases. Our study was conducted with 170 patients selected according to the inclusion and exclusion criteria.
The AO/OTA (AO Foundation/Orthopedic Trauma Association) classification was used for fracture classification. In previous studies, 31A1.2 and 31A1.3 were classified as stable, while 31A2.1, 31A2.2, 31A2.3, 31A3.1, 31A.2, 31A3.3 were classified as unstable[
12].
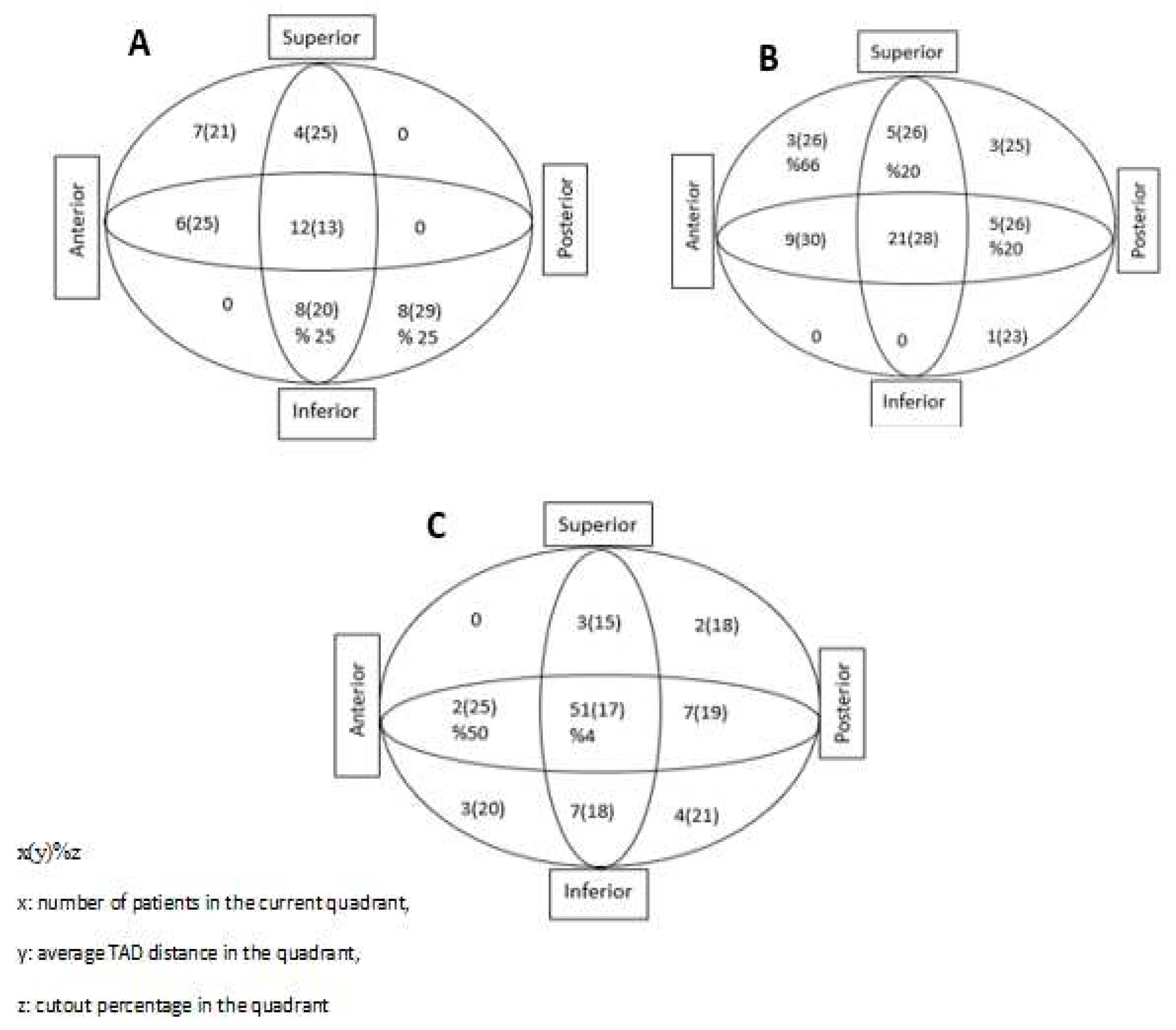
While collecting data, for the preoperative period, the patient’s age, gender, preoperative comorbidities (diabetes, hypertension, coronary artery disease, heart failure, renal failure, asthma, COPD, dementia, and cerebrovascular disease), ASA score (American Society of Anesthesiologists score), and the number of days between occurrence of fracture and surgery were examined. Perioperative data were evaluated as the duration of surgery from the beginning of anesthesia until the patient left the operating room. For the postoperative period, postoperative complications, length of stay in the intensive care unit, and length of stay in hospital were examined, while in postoperative radiographs, tip-apex distance (TAD), collodiaphyseal angle (CDA), and Cleveland-Bosworth quadrants were examined to evaluate the placement of the lag screw in the femoral head (
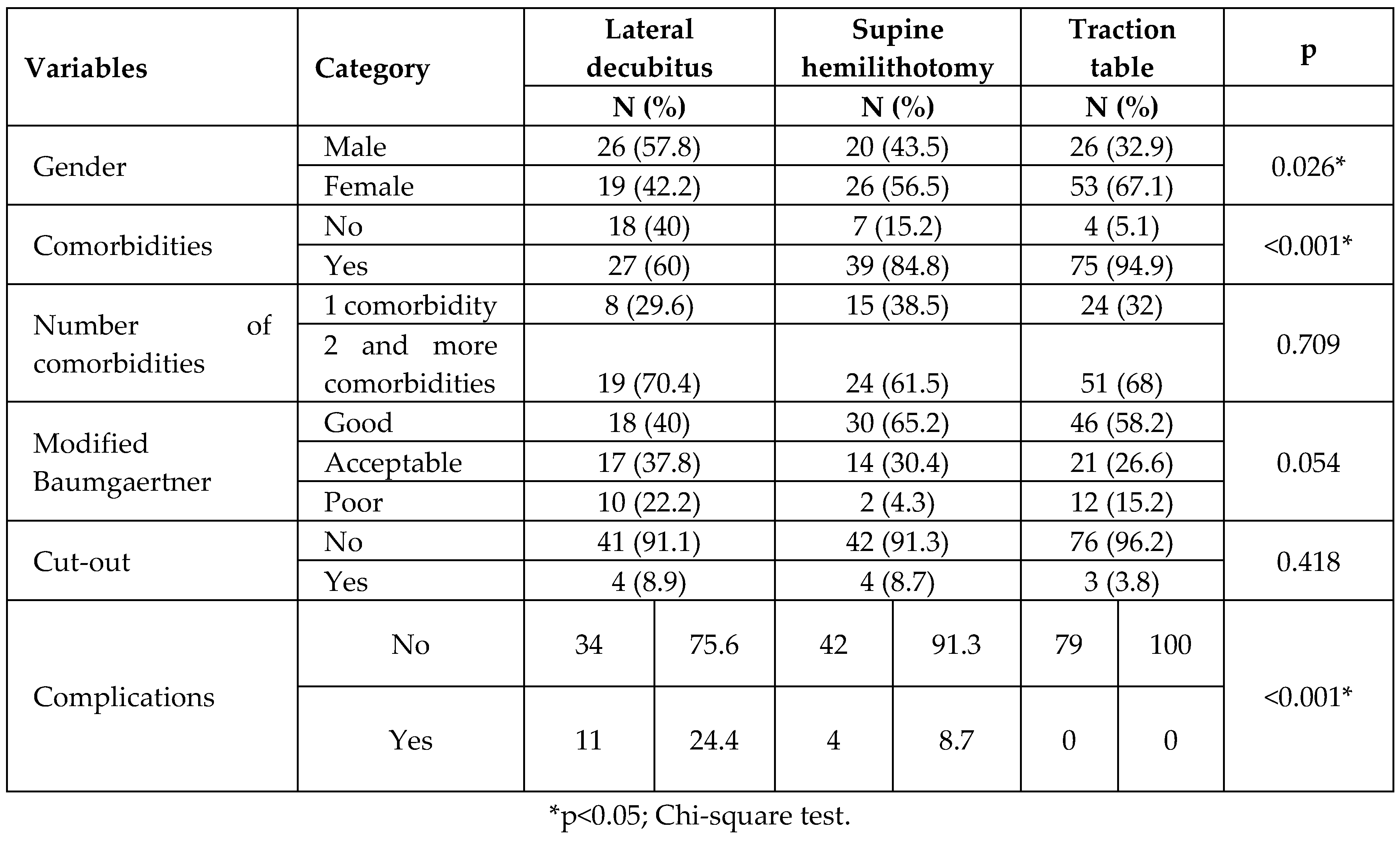
Figure 1). In addition, implant failure and cut-out evaluations were made during the follow-ups. Quality of fracture reduction was evaluated according to the modified Baumgaertner criteria (
Table 1).
Surgical procedures were performed under spinal anesthesia. All surgical procedures were performed by orthopedic surgeons in the same team with at least five years of specialized experience. All patients were given 1 g of cefuroxime sodium parenterally one hour before surgery and low-molecular-weight heparin 12 hours before surgery for VTE prophylaxis. VTE prophylaxis was recommenced at the twelfth hour postoperatively. After the patients were positioned on the operating table, the surgical site was routinely cleaned with povidone-iodine and sterile draping was performed in all groups.
The PFN(ASES® Medikal,Gaziantep,Turkey) has a trapezoidal cross-section, 125° and 130° collodiaphyseal angle options, and a system that provides head/neck compression with an 11 mm lag screw and 7 mm compression screw. The distal end of the nail has a double screw hole that can be locked statically or dynamically. By means of proximal screws, interfragmentary compression of up to 15 mm can be achieved.
Patients were placed supine on the operating table. Then, a folded sheet in the form of a roll was placed under the fracture side and elevated. The unaffected leg was then placed in the lithotomy apparatus. The leg was flexed and abducted. Next, the leg apparatus of the unaffected part of the operating table was removed and the upper torso was lateralized to ensure lateralization of the pelvis. The scope was then adjusted so as to enter through the middle. The surgical assistant achieved fracture reduction by performing longitudinal traction and rotation. Fracture reduction and implant placement were assessed by imaging with C-arm fluoroscopy.
The patients were anesthetized on the stretcher and then transferred to the traction table. One leg was placed in the lithotomy apparatus, and the foot on the fracture side was put in a boot and tightly bound. A perineal post was used to prevent the patient from sliding downward. The sheet was rolled up under the affected hip and elevated, and the upper torso was lateralized. The scope was then passed through the middle and positioned. Fracture reduction was achieved with traction apparatus and hinges on the sole of the boot that allowed rotation, and when appropriate reduction was achieved, the apparatus was locked.
After the patients were anesthetized on the operating table, the patient was turned on his/her side with the fractured extremity positioned superiorly. Then, supports were placed behind the sacrum and in front of the abdomen. The fluoroscope was positioned on the opposite side to the surgeon. Fracture reduction was achieved by the assistant using longitudinal traction and rotation.
After all preparations were made on the operating table, incision was made from the proximal lateral aspect of the greater trochanter by taking anterior-posterior and lateral radiographs under C-arm fluoroscopy control. Firstly, proximal reaming was performed. Diaphyseal reaming was not performed in any patient. Then, a short proximal femur nail (10-13 mm wide, 170-240 mm long) was fixed first with a longitudinal lag screw (11 mm) and then with a compression screw (7 mm). Next, a distal locking screw was fixed statically. Finally, after checking the position of the implant under fluoroscopy control, suturing and dressing were performed.
Prophylactic 4x1 g cefazolin sodium was given parenterally to all patients in the first 24 hours after surgery. All patients were given low-molecular-weight heparin for the first three weeks. All patients were mobilized on the first postoperative day with partial weight bearing with a walker and quadriceps exercises were begun.
The SPSS 25.0 software package was used for statistical analysis of the data. Categorical measurements were summarized as number and percentage, while continuous measurements were summarized as mean and standard deviation (median and minimum-maximum where necessary). Chi-square test or Fisher test statistics were used to compare categorical variables. In comparing continuous measurements between groups, distributions were checked, and one-way analysis of variance (ANOVA) was used for variables with parametric distribution, while Kruskal-Wallis test was used for variables without parametric distribution. In pairwise comparisons between groups, post hoc analyses were used for normally distributed parameters, while Mann-Whitney U test was used for non-normally distributed parameters. In all tests, the statistical significance level was set at 0.05.
3. Results
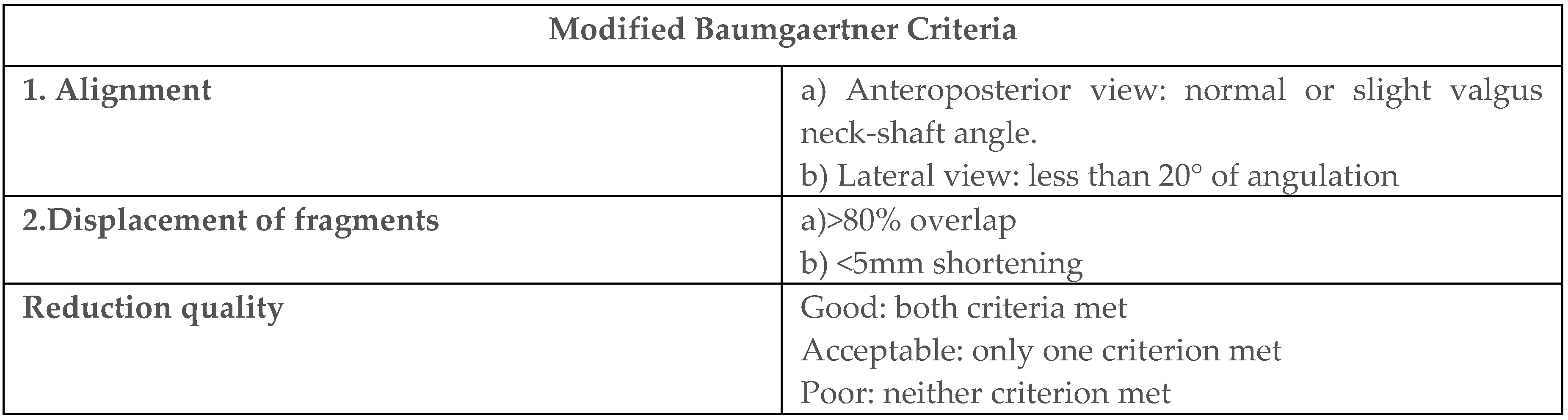
The mean age of the patients was 77.77±8.8; 42.4% of patients were male and 57.6% were female. In terms of positioning, 26.5% of the patients were placed in the lateral decubitus position, 27.1% were placed in the supine position, and 46.5% were included in the traction table group (
Table 2).
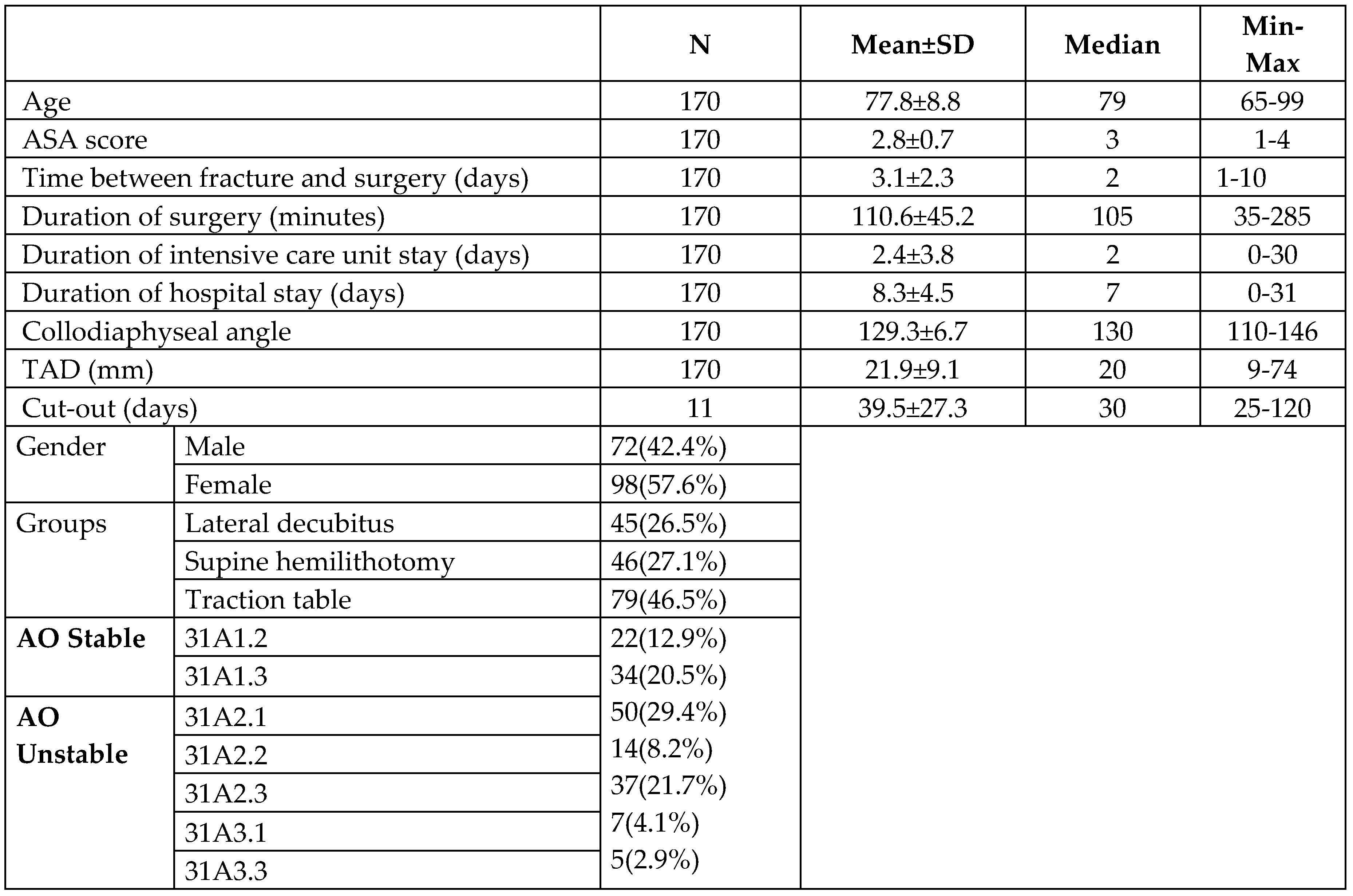
Complications were mostly detected in patients who underwent surgery in the lateral decubitus position, and these were found to occur at a statistically significantly higher rate than in other groups (
Table 3).
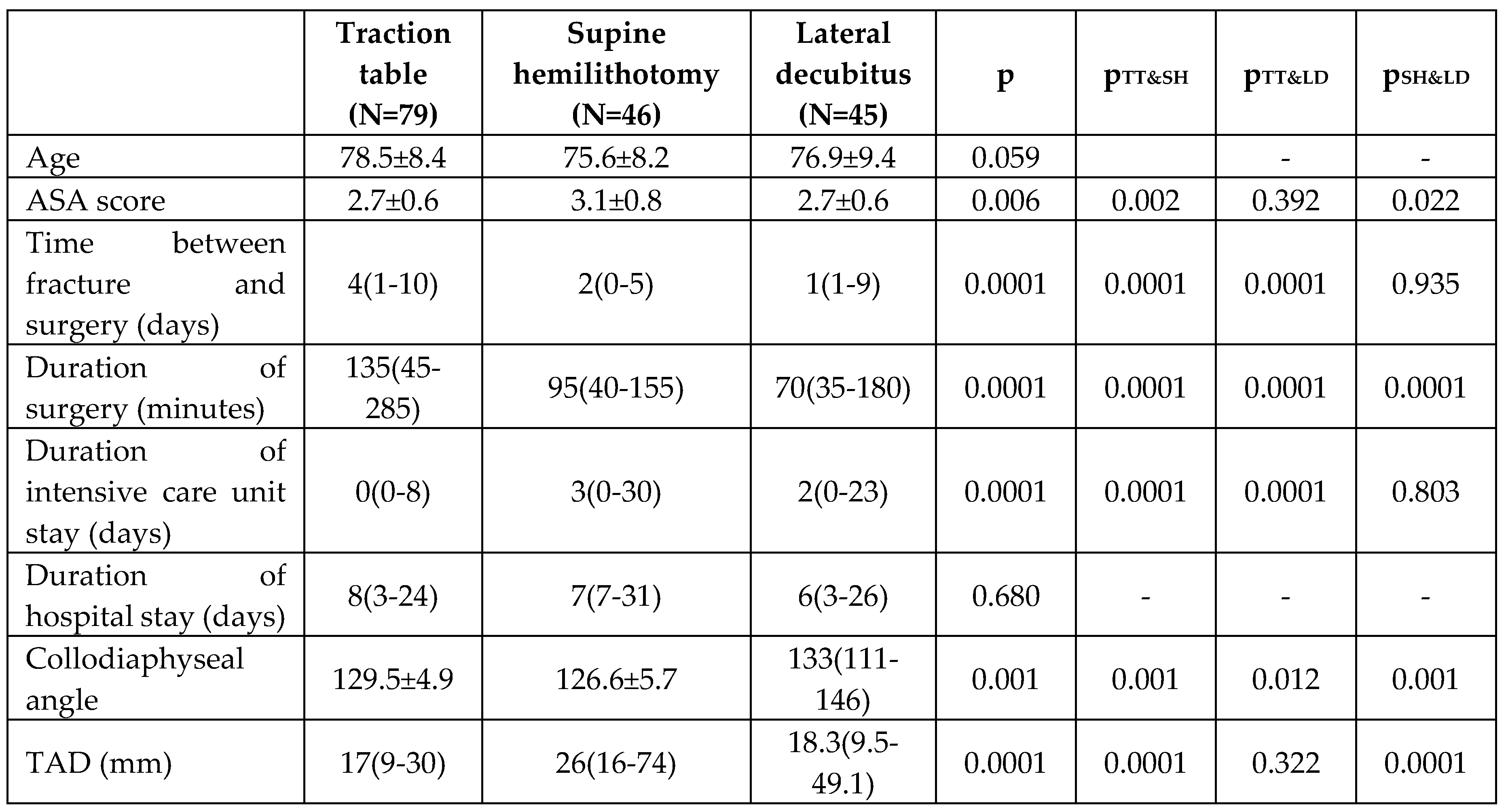
Patients’ ages, ASA scores, time from fracture to surgery, duration of surgery, number of days in intensive care after surgery, Cleveland-Bosworth measurements, collodiaphyseal angle measurements and tip-apex distances show statistically significant differences according to groups (p <0.05). When the median values were examined, the time from fracture to surgery for individuals in the traction table group was found to be higher than in the other groups. The duration of surgery of individuals in the traction table group was found to be higher than in the other groups, the collodiaphyseal angle values of individuals in the supine position group were found to be lower than in the other groups, and the tip-apex distance of individuals in the supine position group was found to be higher than in the other groups (
Table 4).
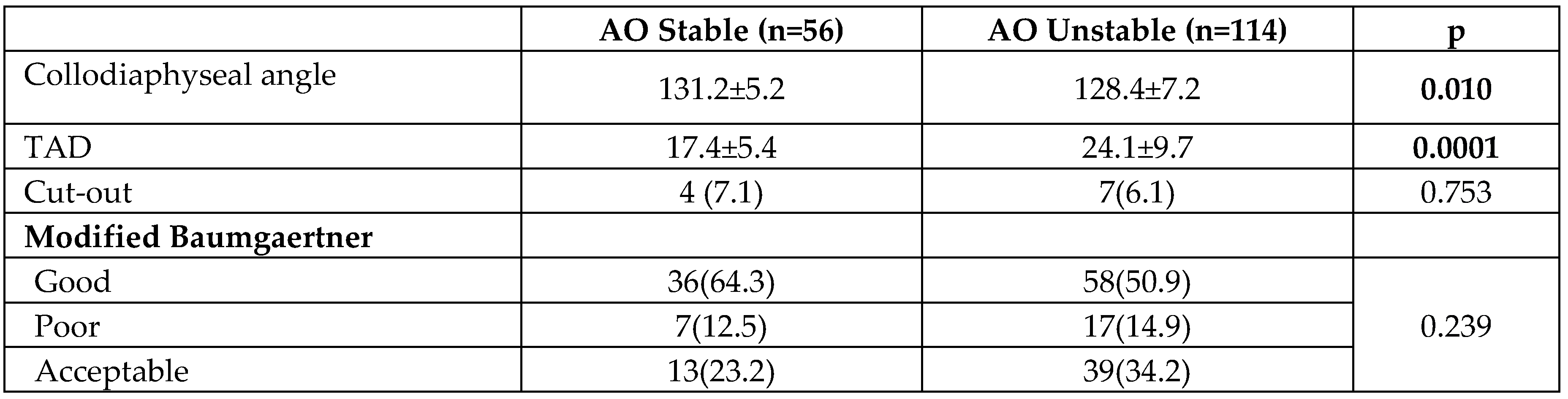
When we evaluated the patients according to fracture stability regardless of the groups, we observed that the TAD measurements were longer in unstable fractures, and that although the CDA values were close to each other, there was a tendency towards varus in unstable fractures (
Table 5).
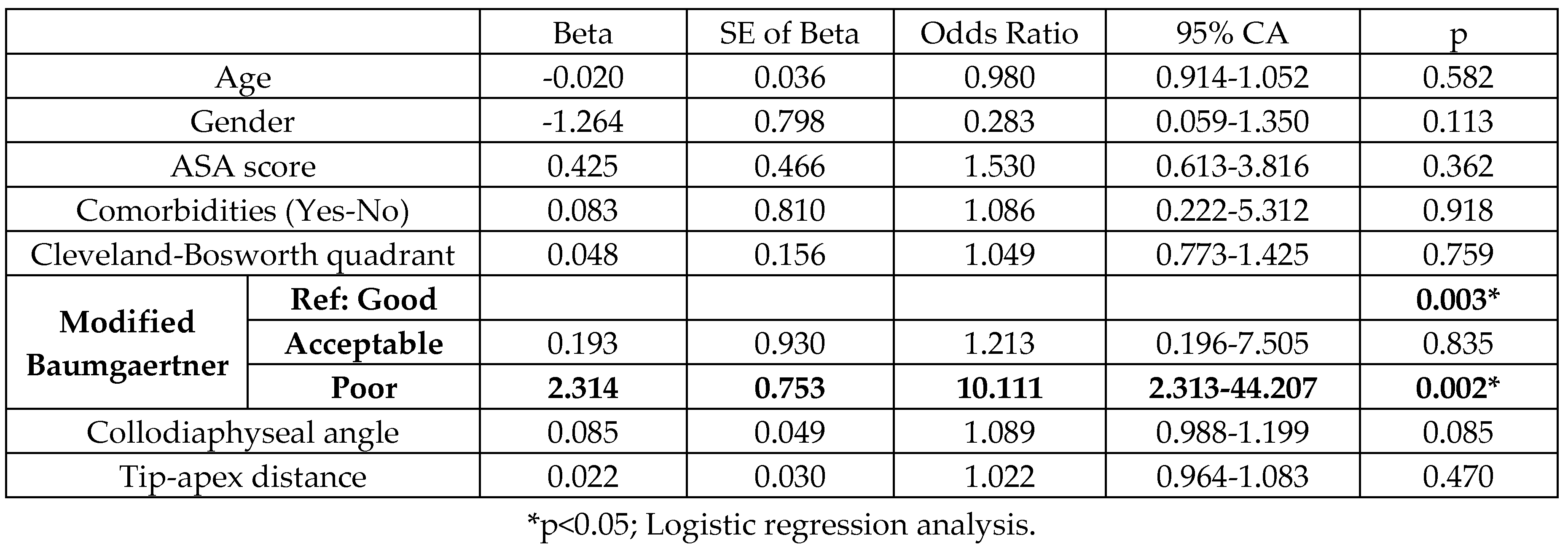
It was concluded that all independent variables included in the model, except the “Modified Baumgaertner” variable, were not significant (p>0.05). According to the modified Baumgaertner criteria, it was determined that patients with ‘poor’ reduction quality had an approximately 10 times higher risk of cut-out than those with ‘good’ reduction quality (OR = 10.111, p = 0.002, 95% confidence interval; 2.313-44.207) (
Table 6). When examining the patients with cut-out complications, among those who underwent surgery in the lateral decubitus position, two patients in the posterior-inferior quadrant and two patients in the inferior-central quadrant were identified; among patients operated on in the supine hemilithotomy position, two patients in the anterior-superior quadrant, one patient in the central-superior quadrant, and one patient in the central-posterior quadrant were identified; among patients undergoing surgery on the traction table, one patient in the central-anterior quadrant and two patients in the central-central, that is, the fifth quadrant, were identified (
Figure 2).
4. Discussion
The incidence of intertrochanteric fractures has been increasing in recent years as a result of longer life expectancy due to better quality of life and better healthcare services. Numerous methods have been proposed for the treatment of intertrochanteric fractures [
13]. Although the reduction and fixation of unstable fractures is difficult, new strategies and new implants are being developed to achieve successful fixation and to prevent complications such as inadequate fixation due to secondary surgery[
6,
14,
15] . Especially in unstable intertrochanteric fractures, although there is no evidence that the type of intramedullary implant and surgical position reduce the failure rate, the importance of surgical skills, such as reduction with intramedullary nailing, appropriate placement of the intramedullary nail, and appropriate positioning of the lag screw, has been emphasized [
16]. Moreover, reduction quality is one of the most important parameters for obtaining good clinical and radiological results in surgery today [
17,
18]. In our study, the quality of reduction was assessed using a classification categorized into three grades based on a modification of the method developed by Baumgaertner et al. [
19]. Although there was no significant difference in reduction quality between the groups, in the logistic regression analysis comparing patients with and without cut-out regardless of the groups, it was seen that poor reduction quality increased the probability of cut-out tenfold.
Unstable fractures of the trochanteric region (31A2) are more common, the average frequency being around 60%, and in our study, this rate is 59.3%, which is similar to the literature [
20].
In our study, it was observed that the duration of surgery in the group undergoing surgery on the traction table was significantly longer than in the other groups. Furthermore, it was observed that the TAD measurements were lower and the collodiaphyseal angles were better in patients who underwent surgery on the traction table. In a study by Şahin et al. comparing manual traction and the traction table, it was determined that surgery time and total anesthesia time were lower in the manual traction group, whereas the number of assistants required was lower in the traction table group[
21].
In our study, it was found that patients in the group that underwent surgery on the traction table were older and had more comorbidities than individuals in the other groups. The time from fracture to surgery for individuals in the traction table group was longer compared to the other groups due to the consultations required to solve cardiac and internal problems for anesthesia in the preoperative period. Many clinics still require a great many preoperative consultations for geriatric hip fractures, which increases the time from fracture to surgery. In their study, Smeets et al. argue that excessive preoperative examinations and consultations requested for geriatric hip fractures may cause delays in surgery and lead to an increase in complications and mortality [
22]. A recent study emphasizes that cardiology consultation and echocardiogram in the preoperative period for hip fractures in the geriatric age group are both expensive and unnecessary [
23].
In our study, it was observed that the duration of surgery for patients operated on in the lateral decubitus position was significantly shorter compared to the other groups. In a study comparing the traction table and lateral decubitus position, Sadeq et al. emphasized that the surgical time was shorter in the lateral decubitus position, but that the quality of reduction was better on the traction table, results which are similar to those of our study [
24]. In their study, Kakumanu et al. emphasized that the lateral decubitus position makes it easier to find the nail entry point and is a preferable method especially for obese patients [
25]. In our study, complications were most common in patients undergoing surgery in the lateral decubitus position. As a complication, prolonged wound discharge was observed in five patients, and in one of these, washing and debridement were first performed under operating room conditions, and no infection was observed in the long term. DVT was observed in two patients, while pneumonia was observed in one patient, atelectasis in one patient, and delirium in two patients.
It was observed that in patients who underwent surgery in the supine hemilithotomy position, TAD was higher and collodiaphyseal angles were lower than in the other groups. However, not only was reduction quality similar to that of the other groups, but also, when the cut-out rates were examined, it was seen that there was no significant difference from the other groups. In a study comparing the supine hemilithotomy position with the traction table, it was observed that there was no significant clinical or radiological difference between these two positions, except for duration of surgery[
26] . When we look at the literature, well-leg compartment syndrome can be seen in patients in the supine hemilithotomy position, and it is thought that this complication may be due to a surgery duration of over four hours, body mass index, coagulopathy, and perioperative hypotension [
27,
28]. No compartment syndrome complication was observed in any patient in our study. Pulmonary embolism was observed in two patients, while DVT was seen in one patient. Cellulitis was observed around the wound site in one patient and was treated with antibiotic therapy.
It is reported that the most serious complication seen after PFN for unstable femoral intertrochanteric fractures is cut-out and that its incidence ranges between 2% and 3.5% (17). Cut-out results from the collapse of the femur neck shaft angle into a varus position, resulting in the extrusion of the screw from the femoral head[
29]. Although cut-out was observed in 6.4% of all patients in our study, no significant difference was found between the groups.
Intertrochanteric fractures are more common in older patients, and the prolongation of surgical setup and longer duration of surgical procedures due to prolongation of anesthesia in these patients increase complications and mortality[
30]. When all three positions in our study are compared, it can be seen that the duration of surgery was longer on the traction table, but that the length of this period made no significant difference in terms of developing complications.
Following surgery for intertrochanteric fractures, CDA <125° is considered as varus, 125-135° as neutral, and >135° as valgus. Along with studies stating that varus alignment is inappropriate and that neutral or valgus alignment are appropriate, studies conducted on cadavers have shown that the risk of implant failure increases with the increase in the load on the implant due to an increase in varus alignment [
31,
32]. The mean CDA of patients participating in our study was measured as 129.3° in all groups, and when CDAs were compared between groups, it was seen that they were better in the traction table group than in the other groups. No significant relationship was found between cut-out and CDA, regardless of the groups.
TAD is the total distance in millimeters from the tip of the lag screw to the apex of the femoral head, measured on anteroposterior and lateral radiographs after correction for magnification on the radiograph. There are important studies showing that a TAD of <25 mm reduces the risk of cut-out[
29,
33] . In this study, the mean TAD of all patients was 21.9 mm, and the results were significantly better in those who underwent surgery on the traction table compared to other groups, while TAD was measured higher in the supine hemilithotomy position. In addition, following surgery for unstable fractures, TAD measurements were significantly higher than those for stable fractures. Regardless of the groups, no significant relationship was found between TAD and cut-out. In their studies conducted for unstable intertrochanteric fractures, John et al. and Çepni et al. did not find a significant relationship between TAD and cut-out and predicted that TAD alone would not be sufficient to determine the risk of cut-out [
34,
35]. In their study, however, Fuji et al. predicted that TAD>20 mm alone was a prognostic factor for cut-out [
36]. Some clinical studies emphasize that even if TAD is >25 mm, inferior-central placement of the lag screw may be more stable than central-central placement, and also that the cut-off value of 25 mm should be adjusted by considering the difference in femoral head geometry from patient to patient [
20].
When examining the Cleveland-Bosworth quadrants, the femoral neck is divided into three regions: superior, center and inferior in the coronal plane, and anterior, center and posterior in the sagittal plane, and nine quadrants are defined after the intersection of these regions. In the study by Hwang et al., the center-center or inferior-center quadrants were recommended [
37]. In the study by Karapınar et al., the center-center, inferior-center and inferior-posterior quadrants were found to be safe [
38]. In their study, De Bruijn et al. found the inferior-anterior and inferior-posterior quadrants to be safe [
39]. In our study, when examination was made both within the groups and independently of the groups, no relationship was found between the quadrants alone and the cut-out rate.
5. Conclusions
In conclusion, although PFN surgery performed using a traction table was longer in terms of surgical time compared to the lateral decubitus position and supine hemilithotomy position, the fact that TAD and CDA values were better and that the complication rate was lower is important. Although there was no significant difference in terms of supine hemilithotomy and lateral decubitus position, which can be performed in clinics without a traction table, it was observed that the duration of surgery was shorter but that the complication rate was higher in the lateral decubitus position. When the results are evaluated independently of the groups, we consider that successful fracture reduction is the most important way to prevent cut-out. We believe that it is necessary to be familiar with all methods, since it is very difficult to choose the most appropriate method according to the surgeon’s experience, the hospital’s facilities and conditions, and the patient’s clinical and additional injury. We think that our study will serve as a guide for future prospective studies with larger numbers of participants.
This section is mandatory and should contain the main conclusions regarding the research.
6. Limitations
There are some limited aspects of the study. First of all, the study was planned retrospectively. In addition, bone quality and body mass index were not included. Moreover, the fact that the male-female ratio was not equal, all fractures were unstable, and all surgical interventions were not performed by the same surgeon are among the limitations of our study.
Author Contributions
Onur KAYA; analyzed and interpretation of data, drafted the article and revised it critically for important intellectual content and and wrote the manuscript. Buğra KUNDAKÇI; analyzed and interpretation of data, drafted the article and revised it critically for important intellectual content and wrote the manuscript. Cem ÖNDER; interpretation of data, drafted the article and revised it critically for important intellectual content and and wrote the manuscript. Vahap KURT; interpretation of data, drafted the article and revised it critically for important intellectual content and and wrote the manuscript. Emre ATMACA; drafted the article and revised it critically for important intellectual content and and wrote the manuscript. Fatih TUNÇ; drafted the article and revised it critically for important intellectual content and and wrote the manuscript.
Funding
There are no funding sources to declare.
Institutional Review Board Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Ethics committee approval was obtained from Gaziantep University Ethics Committee.
Conflicts of Interest
There are no conflicts of interest to declare.
References
- T.A. Russell, R. T.A. Russell, R. Sanders, Pertrochanteric hip fractures: time for change, J Orthop Trauma, 25 (2011) 189-190. [CrossRef]
- H.P. Dimai, B. H.P. Dimai, B. Reichardt, E. Zitt, H. Concin, O. Malle, A. Fahrleitner-Pammer, A. Svedbom, W. Brozek, Thirty years of hip fracture incidence in Austria: is the worst over?, Osteoporos Int, 33 (2022) 97-104. [CrossRef]
- Johnell, J. Kanis, Epidemiology of osteoporotic fractures, Osteoporos Int, 16 Suppl 2 (2005) S3-7. [CrossRef]
- K.S. Vig, C. K.S. Vig, C. Adams, J.R. Young, E. Perloff, C.M. O’Connor, C.M. Czajka, Patient Positioning for Proximal Femur Fracture Fixation: a Review of Best Practices, Curr Rev Musculoskelet Med, 14 (2021) 272-281. [CrossRef]
- J.A. Stevens, R.A. J.A. Stevens, R.A. Rudd, The impact of decreasing U.S. hip fracture rates on future hip fracture estimates, Osteoporos Int, 24 (2013) 2725-2728. [CrossRef]
- S.S. 2006.
- Y. Yu, K. Y. Yu, K. Pan, G. Wang, Femoral trochanteric fracture: PFNA spiral blade placement with the aid of an angler, J Int Med Res, 48 (2020) 300060519890782. [CrossRef]
- Y. Huang, C. Y. Huang, C. Zhang, Y. Luo, A comparative biomechanical study of proximal femoral nail (InterTAN) and proximal femoral nail antirotation for intertrochanteric fractures, Int Orthop, 37 (2013) 2465-2473. [CrossRef]
- Z. Zhao, F. Z. Zhao, F. Song, J. Zhu, D. He, J. Deng, X. Ji, P. Tang, Y. Pan, Prone positioning for intramedullary nailing of subtrochanteric fractrures, the techniques of intraoperative fluoroscopy and reduction: A technique note, Injury, 48 (2017) 2354-2359. [CrossRef]
- D.Y. Li, C.G. D.Y. Li, C.G. Liu, K. Zhang, Whether Assisted Intramedullary Nail Implantation Without Traction Table is as Safe and Effective as Using Traction Table of Older Intertrochanteric Fracture Patients?, Clin Interv Aging, 18 (2023) 387-395. [CrossRef]
- M.Ş. Boz, AA. M.Ş. Boz, AA. 2020. [Google Scholar]
- N. Asif, S. N. Asif, S. Ahmad, O.A. Qureshi, L.Z. Jilani, T. Hamesh, T. Jameel, Unstable Intertrochanteric Fracture Fixation - Is Proximal Femoral Locked Compression Plate Better Than Dynamic Hip Screw, J Clin Diagn Res, 10 (2016) RC09-13. [CrossRef]
- L. Hutchings, R. L. Hutchings, R. Fox, T. Chesser, Proximal femoral fractures in the elderly: how are we measuring outcome?, Injury, 42 (2011) 1205-1213. [CrossRef]
- D.G. Lorich, D.S. D.G. Lorich, D.S. Geller, J.H. m: Nielson, Osteoporotic pertrochanteric hip fractures, 2004. [Google Scholar]
- P. Tang, F. P. Tang, F. Hu, J. Shen, L. Zhang, L. Zhang, Proximal femoral nail antirotation versus hemiarthroplasty: a study for the treatment of intertrochanteric fractures, Injury, 43 (2012) 876-881. [CrossRef]
- S.R. Lee, S.T. S.R. Lee, S.T. Kim, M.G. Yoon, M.S. Moon, J.H. Heo, The stability score of the intramedullary nailed intertrochanteric fractures: stability of nailed fracture and postoperative patient mobilization, Clin Orthop Surg, 5 (2013) 10-18. [CrossRef]
- X. Jia, K. X. Jia, K. Zhang, M. Qiang, Y. Chen, The accuracy of intra-operative fluoroscopy in evaluating the reduction quality of intertrochanteric hip fractures, Int Orthop, 44 (2020) 1201-1208. [CrossRef]
- Y.C. Yoon, C.W. Y.C. Yoon, C.W. Oh, J.A. Sim, J.K. Oh, Intraoperative assessment of reduction quality during nail fixation of intertrochanteric fractures, Injury, 51 (2020) 400-406. [CrossRef]
- Kashigar, A. Vincent, M.J. Gunton, D. Backstein, O. Safir, P.R. Kuzyk, Predictors of failure for cephalomedullary nailing of proximal femoral fractures, Bone Joint J, 96-B (2014) 1029-1034. [CrossRef]
- S.M. Chang, Z.Y. S.M. Chang, Z.Y. Hou, S.J. Hu, S.C. Du, Intertrochanteric Femur Fracture Treatment in Asia: What We Know and What the World Can Learn, Orthop Clin North Am, 51 (2020) 189-205. [CrossRef]
- E. Sahin, M. E. Sahin, M. Songur, M. Kalem, S. Zehir, M.A. Aksekili, S. Keser, A. Bayar, Traction table versus manual traction in the intramedullary nailing of unstable intertrochanteric fractures: A prospective randomized trial, Injury, 47 (2016) 1547-1554. [CrossRef]
- S.J.M. Smeets, B.P.W. S.J.M. Smeets, B.P.W. van Wunnik, M. Poeze, G.D. Slooter, J. Verbruggen, Cardiac overscreening hip fracture patients, Arch Orthop Trauma Surg, 140 (2020) 33-41. [CrossRef]
- C.L. Hoehmann, J. C.L. Hoehmann, J. Thompson, M. Long, M. DiVella, S. Munnangi, C. Ruotolo, D.K. Galos, Unnecessary Preoperative Cardiology Evaluation and Transthoracic Echocardiogram Delays Time to Surgery for Geriatric Hip Fractures, J Orthop Trauma, 35 (2021) 205-210. [CrossRef]
- M.H.U. Sadeq, Majeed, G. H., Ali, H. O. H., Al Bayati, M. A., Aledanni, M. S. S: Fixation of unstable intertrochanteric fractures with proximal femoral nailing, 2023.
- R.K. Kakumanu, Kunadharaju, R. T., Beesetty, M. A: & Golla, D, Ease of doing proximal femoral nailing in lateral position in the management of peri-trochanteric femoral fractures in adults, 2019.
- A.P. ÖZGÜR, Ö. 2023.
- I.F. Brouze, S. I.F. Brouze, S. Steinmetz, J. McManus, O. Borens, Well leg compartment syndrome in trauma surgery - femoral shaft fracture treated by femoral intramedullary nailing in the hemilithotomy position: case series and review of the literature, Ther Clin Risk Manag, 15 (2019) 241-250. [CrossRef]
- Z. Ntontis, N. Z. Ntontis, N. Trygonis, P. Bitados, C. Tsatsoulas, E. Pappa, K. Samartzidis, I. Stavrakakis, Well leg compartment syndrome due to the lithotomy position in orthopedic surgery: a report of two cases and a review of the literature, J Surg Case Rep, 2022 (2022) rjac522. [CrossRef]
- M.R. Baumgaertner, S.L. M.R. Baumgaertner, S.L. Curtin, D.M. Lindskog, J.M. Keggi, The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip, J Bone Joint Surg Am, 77 (1995) 1058-1064. [CrossRef]
- A.K. Jaffer, W.K. A.K. Jaffer, W.K. Barsoum, V. Krebs, J.G. Hurbanek, N. Morra, D.J. Brotman, Duration of anesthesia and venous thromboembolism after hip and knee arthroplasty, Mayo Clin Proc, 80 (2005) 732-738. [CrossRef]
- C. Jiamton, K. C. Jiamton, K. Boernert, R. Babst, F.J.P. Beeres, B.C. Link, The nail-shaft-axis of the of proximal femoral nail antirotation (PFNA) is an important prognostic factor in the operative treatment of intertrochanteric fractures, Arch Orthop Trauma Surg, 138 (2018) 339-349. [CrossRef]
- M. Marmor, K. M. Marmor, K. Liddle, J. Buckley, A. Matityahu, Effect of varus and valgus alignment on implant loading after proximal femur fracture fixation, Eur J Orthop Surg Traumatol, 26 (2016) 379-383. [CrossRef]
- Turgut, O. Kalenderer, L. Karapinar, M. Kumbaraci, H.A. Akkan, H. Agus, Which factor is most important for occurrence of cutout complications in patients treated with proximal femoral nail antirotation? Retrospective analysis of 298 patients, Arch Orthop Trauma Surg, 136 (2016) 623-630. [CrossRef]
- S. Cepni, I.O. S. Cepni, I.O. Subasi, A. Sahin, I. Bozkurt, A. Firat, K. Kilicarslan, Tip-neck distance ratio as a novel predictor for failure in cephalomedullary nailing of unstable trochanteric fractures (UTF), Arch Orthop Trauma Surg, 142 (2022) 2619-2626. [CrossRef]
- B. John, A. B. John, A. Sharma, A. Mahajan, R. Pandey, Tip-apex distance and other predictors of outcome in cephalomedullary nailing of unstable trochanteric fractures, J Clin Orthop Trauma, 10 (2019) S88-S94. [CrossRef]
- T. Fujii, S. T. Fujii, S. Nakayama, M. Hara, W. Koizumi, T. Itabashi, M. Saito, Tip-Apex Distance Is Most Important of Six Predictors of Screw Cutout After Internal Fixation of Intertrochanteric Fractures in Women, JB JS Open Access, 2 (2017) e0022. [CrossRef]
- J.H. Hwang, A.K. J.H. Hwang, A.K. Garg, J.K. Oh, C.W. Oh, S.J. Lee, C. Myung-Rae, M.K. Kim, H. Kim, A biomechanical evaluation of proximal femoral nail antirotation with respect to helical blade position in femoral head: A cadaveric study, Indian J Orthop, 46 (2012) 627-632. [CrossRef]
- L. Karapinar, A. L. Karapinar, A. Turgut, M. Kumbaraci, A. Koca, Evaluation of the quadrants of femoral neck-head in the cephalomedullary fixation of intertrochanteric fractures with a helical blade: Is inferior posterior quadrant also safe? A clinical study, Jt Dis Relat Surg, 32 (2021) 93-100. [CrossRef]
- K. De Bruijn, D. K. De Bruijn, D. den Hartog, W. Tuinebreijer, G. Roukema, Reliability of predictors for screw cutout in intertrochanteric hip fractures, J Bone Joint Surg Am, 94 (2012) 1266-1272. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).