Submitted:
21 January 2024
Posted:
22 January 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
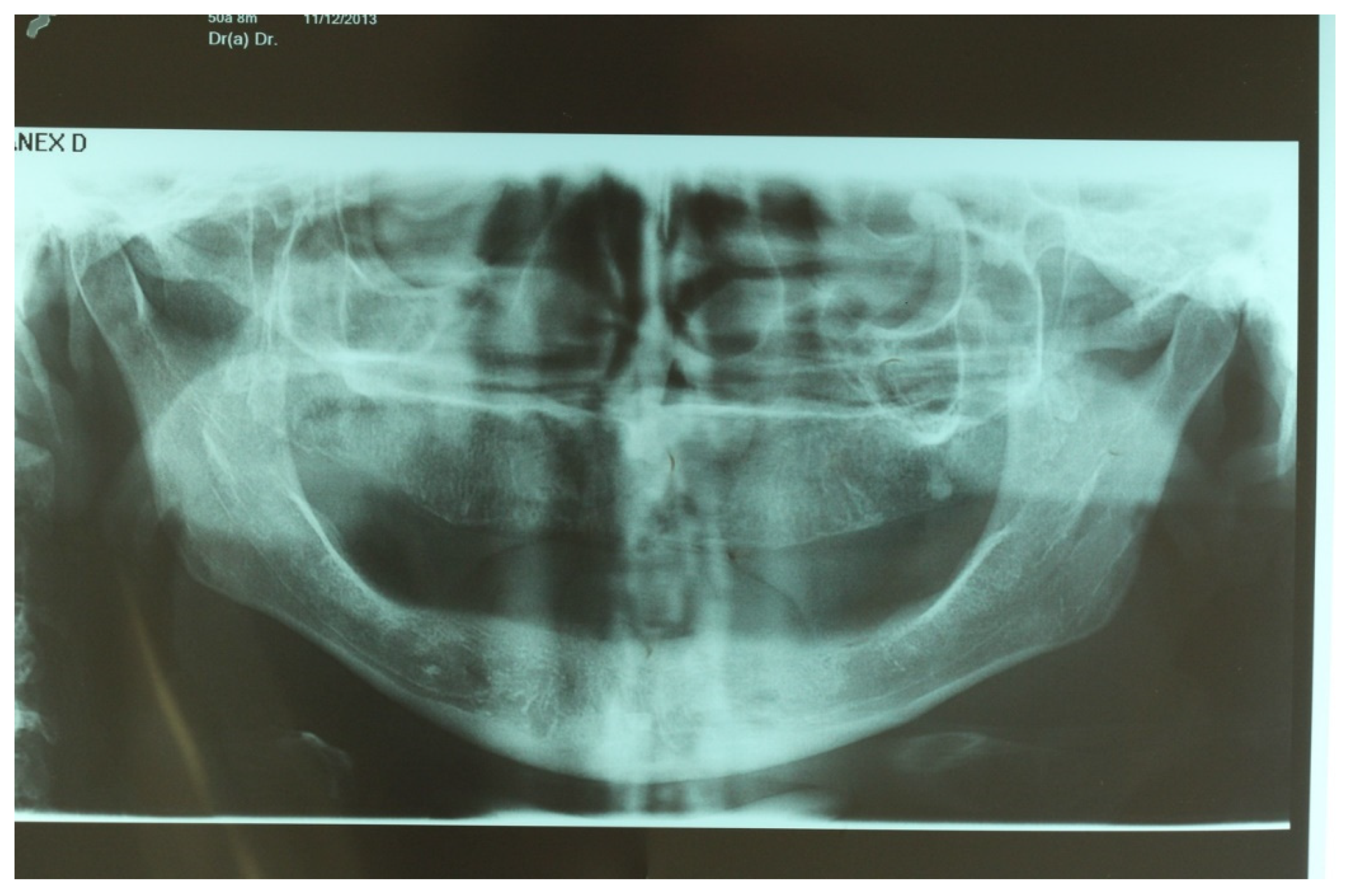
Pre-Surgical Evaluation
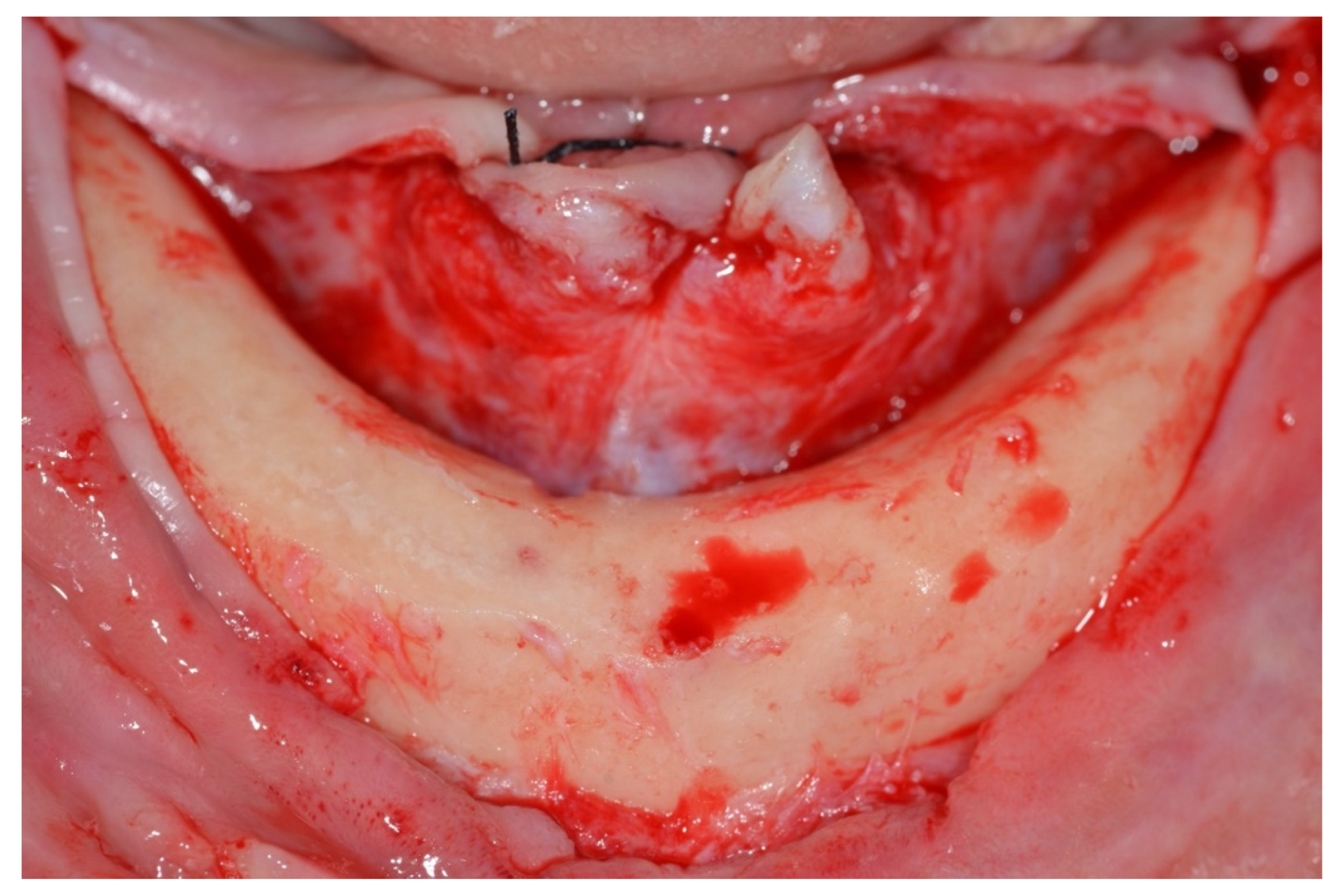
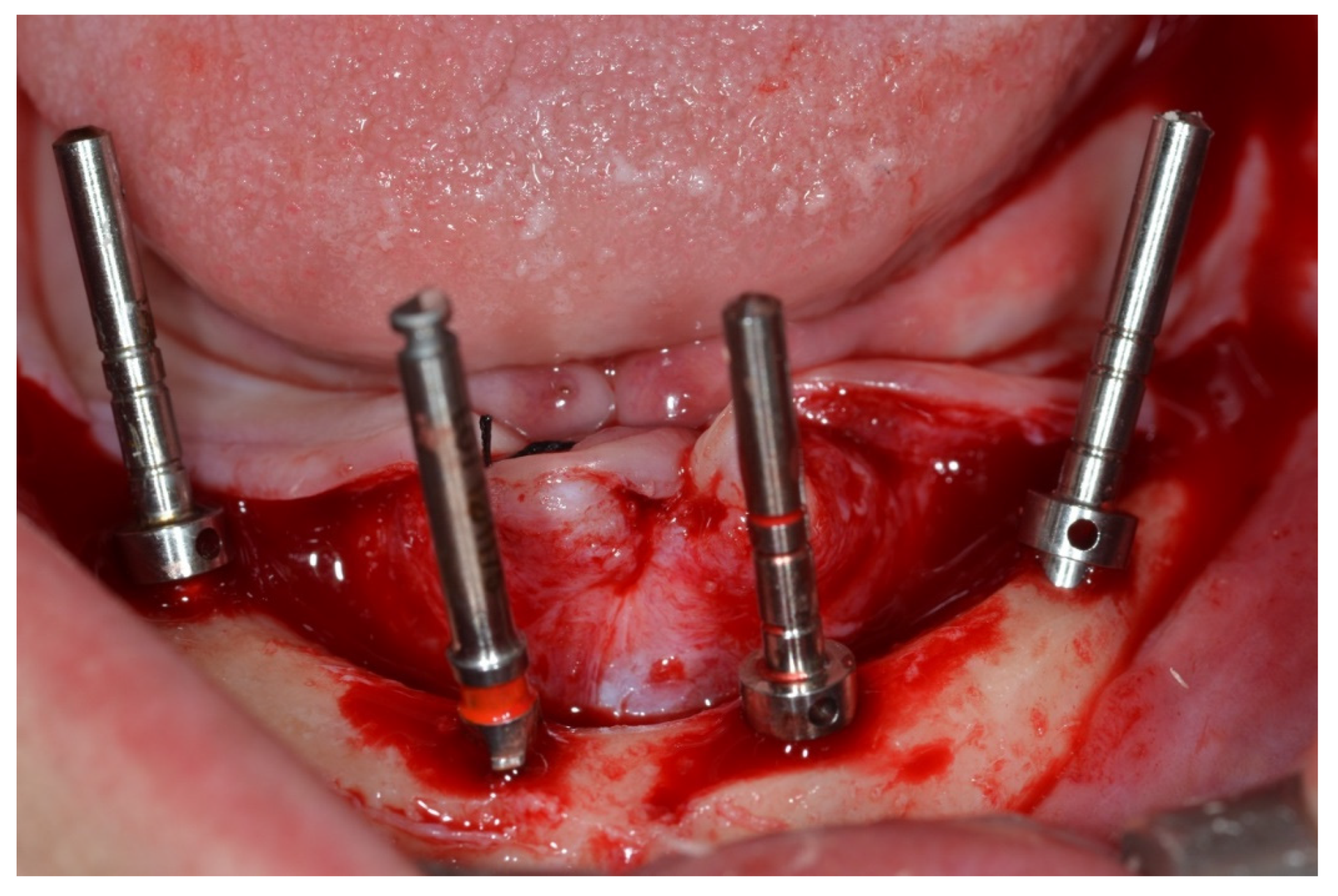
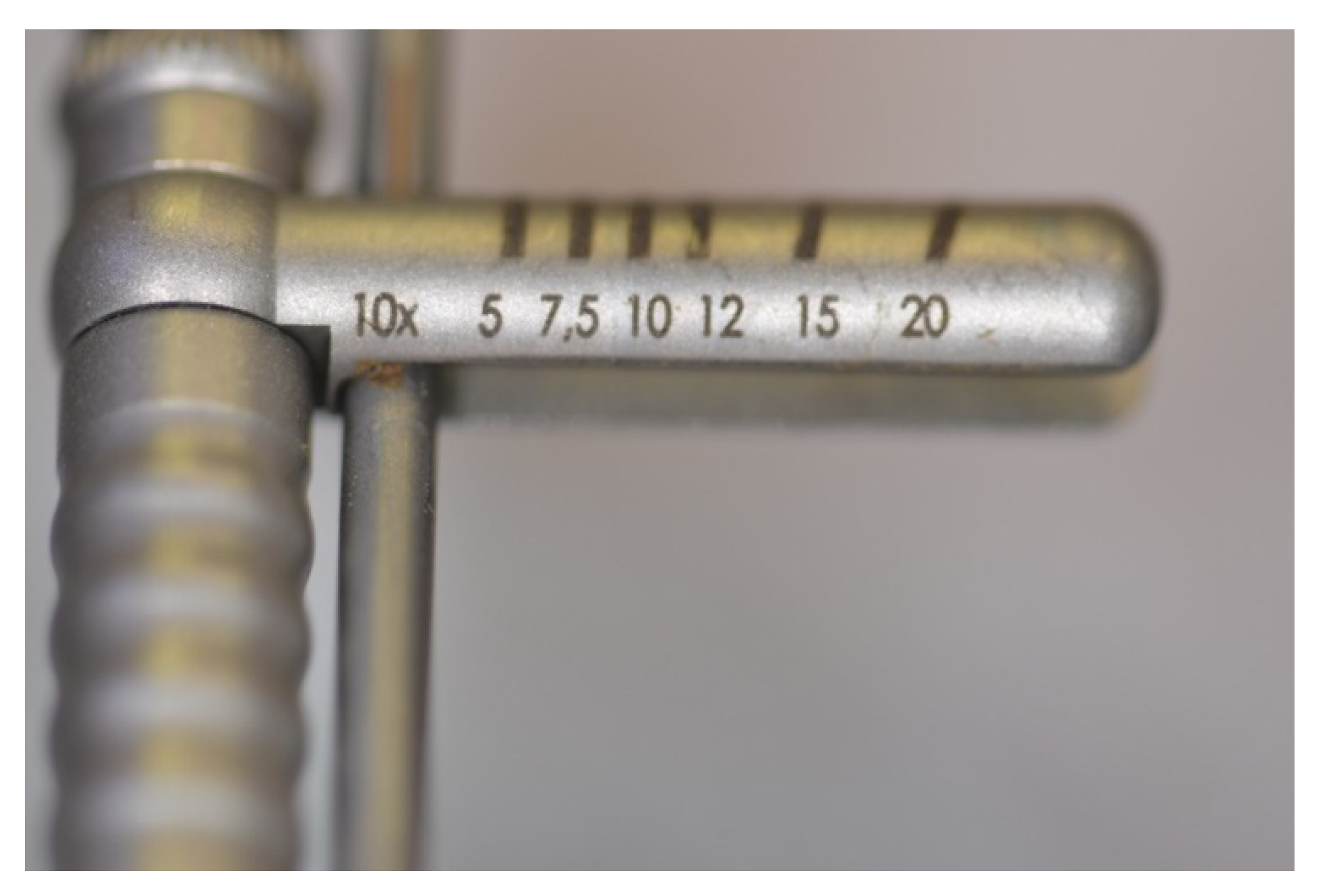
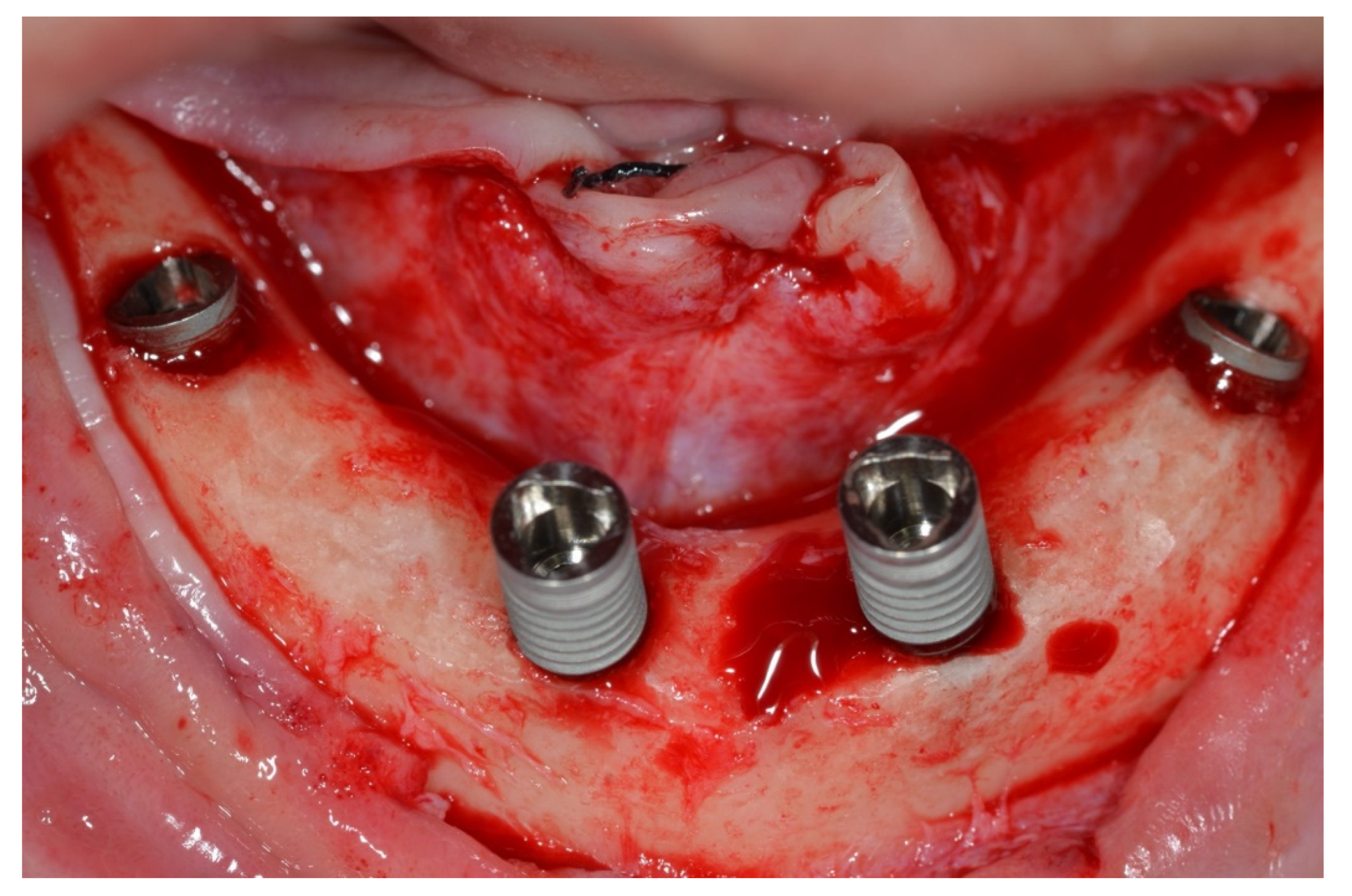
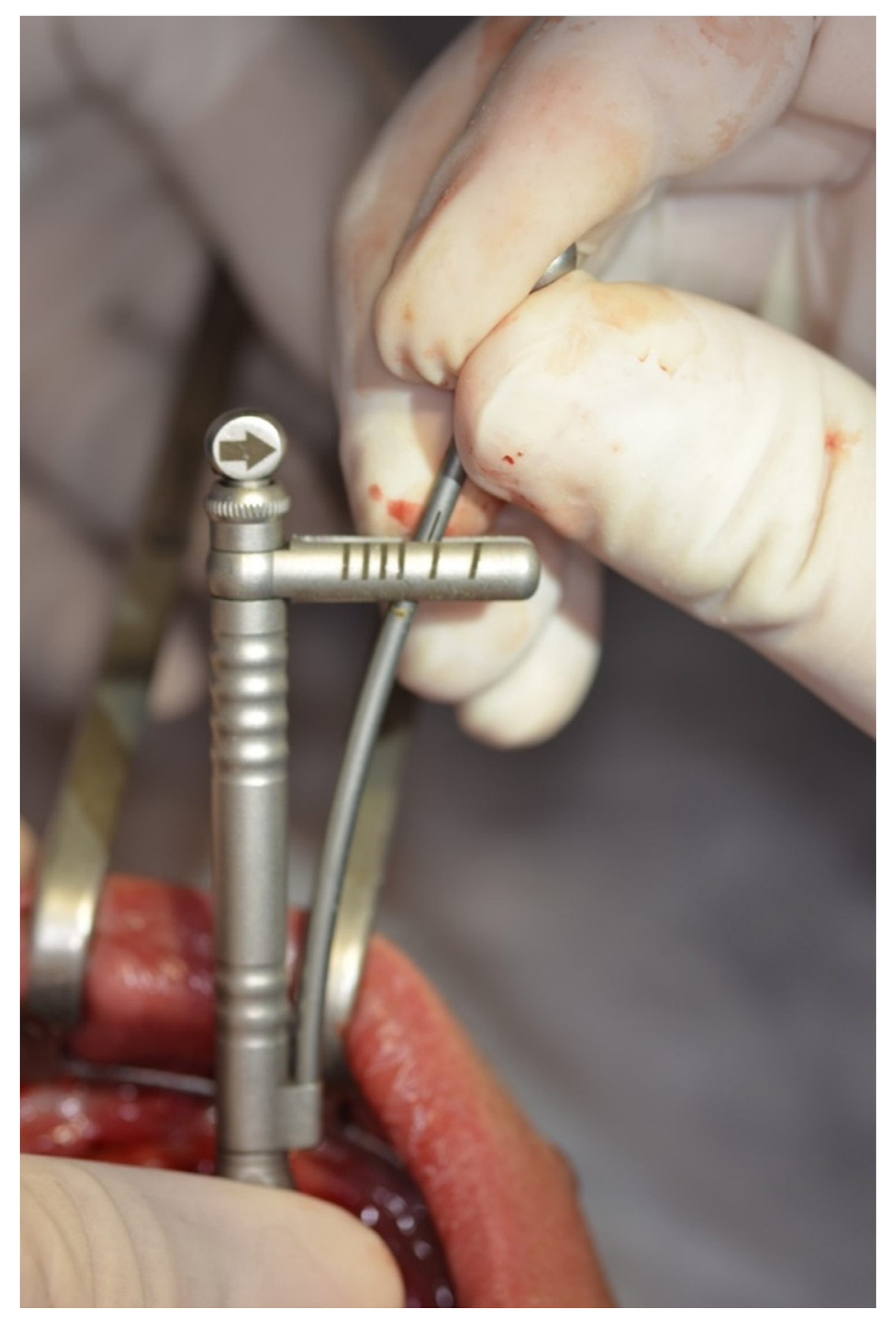
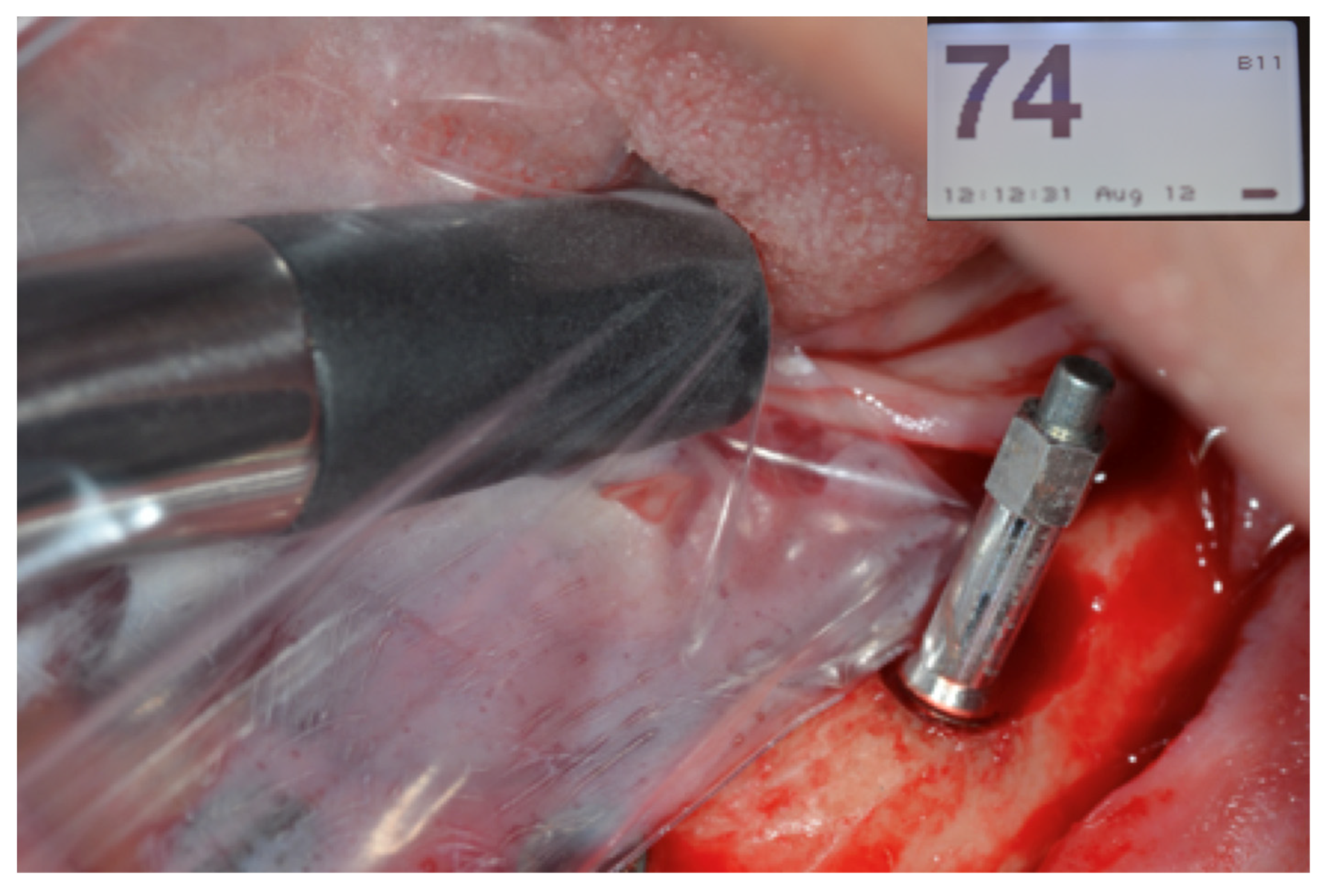
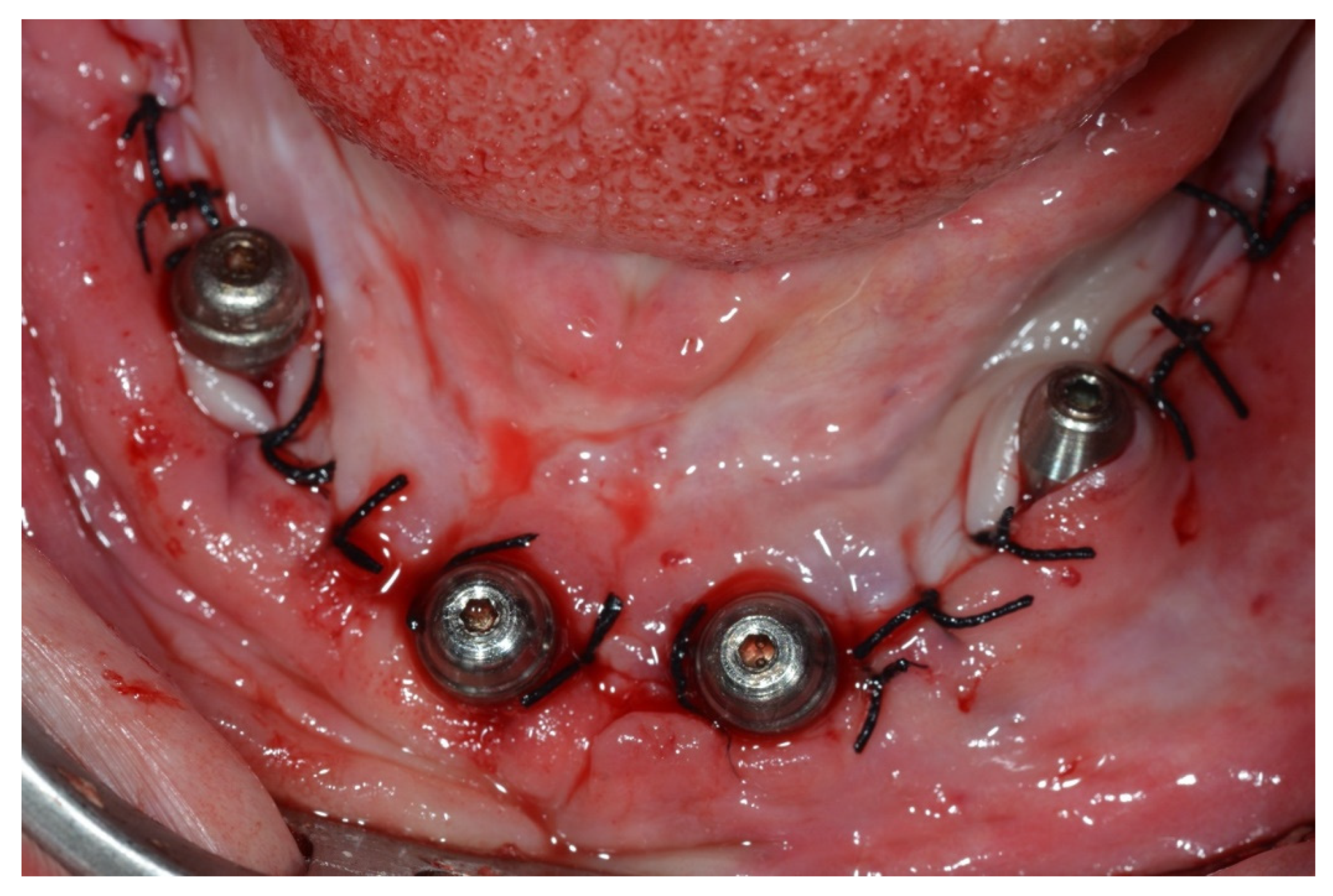
Surgical Protocol
Prosthetic Protocol
Follow-Up
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Meridith, N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont 1998, 11, 491–501. [Google Scholar]
- Szmukler-Monkler, S.; Salama, H.; Reingewirtz, Y.; Dubruille, J.H. Timing of loading and effect of micromotion on bone-dental implant interface: review of experimental literature. J Biomed Mater Res 1998, 43, 192–203. [Google Scholar] [CrossRef]
- Del Fabbro, M.; Testori, T.; Kekovic, V.; Goker, F.; Tumedei, M.; Wang, H.L. A Systematic Review of Survival Rates of Osseointegrated Implants in Fully and Partially Edentulous Patients Following Immediate Loading. Journal of Clinical Medicine 2019, 8, 2142. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, G.S.Y.; de Magalhães, K.M.F.; Rocha, E.P.; Dos Santos, P.H.; Assunção, W.G. Oral health-related quality of life and satisfaction in edentulous patients rehabilitated with implant-supported full dentures all-on-four concept: a systematic review. Clinical Oral Investigation 2022, 26, 83–94. [Google Scholar] [CrossRef]
- Agliardi, E.L.; Pozzi, A.; Romeo, D.; Del Fabbro, M. Clinical outcomes of full-arch immediate fixed prostheses supported by two axial and two tilted implants: A retrospective cohort study with 12-15 years of follow-up. Clin Oral Implants Res 2023, 34, 351–366. [Google Scholar] [CrossRef] [PubMed]
- Wazen, R.; Currey, J.; Guo, H.; Brunski, J.; Helms, J.; Nanci, A. Micromotion-induced strain fields influence early stages of repair at bone–implant interfaces. Acta Biomater 2013, 9, 6663–6674. [Google Scholar] [CrossRef]
- Lee, J.; Pyo, S.W.; Cho, H.J.; An, J.S.; Lee, J.H.; Koo, K.T.; Lee, Y.M. Comparison of implant stability measurements between a resonance frequency analysis device and a modified damping capacity analysis device: An in vitro study. J Periodontal Implant Sci 2020, 50, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Tumedei, M.; Piattelli, A.; Degidi, M.; Mangano, C.; Iezzi, G. A Narrative Review of the Histological and Histomorphometrical Evaluation of the Peri-Implant Bone in Loaded and Unloaded Dental Implants. A 30-Year Experience (1988–2018). Int J Environ Res Public Health 2020, 17, 2088. [Google Scholar] [CrossRef] [PubMed]
- Sotto-Maior, B.S.; Rocha, E.P.; Almeida, E.O.; Freitas-Júnior, A.C.; Anchieta, R.B.; Del Bel Cury, A.A. Influence of high insertion torque on implant placement – an anisotropic bone stress analysis. Braz Dent J 2010, 21, 508–514. [Google Scholar] [CrossRef]
- Dos Santos, M.V.; Elias, C.N.; Lima, J.H.C. The effects of superficial roughness and design on the primary stability of dental implants. Clin Implant Dent Relat Res 2011, 13, 215–223. [Google Scholar] [CrossRef]
- Gonzáles-Martín, O.; Lee, E.A.; Veltri, M. CBCT fractal dimension changes at the Apex of immediate implants placed using undersized drilling. Clin Oral Impl Res 2012, 23, 954–957. [Google Scholar] [CrossRef] [PubMed]
- Isoda, K.; Ayukawa, Y.; Tsukiyama, Y.; Sogo, M.; Matsushita, Y.; Koyano, K. Relationship between the Bone Density Estimated by Cone-Beam Computed Tomography and the Primary Stability of Dental Implants: Relationship between Bone Density and Implant Stability. Clin Oral Implant Res 2012, 23, 832–836. [Google Scholar] [CrossRef] [PubMed]
- Jimbo, R.; Tovar, N.; Anchieta, R.B.; Machado, L.S.; Marin, C.; Teixeira, H.S.; Coelho, P.G. The combined effects of undersized drilling and implant macrogeometry on bone healing around dental implants: an experimental study. Int J Oral Maxillofac Surg 2014, 43, 1269–75. [Google Scholar] [CrossRef] [PubMed]
- Trisi, P.; Todisco, M.; Consolo, U.; Travaglini, D. High versus low implant insertion torque: a histologic, histomorphometric, and biomechanical study in the sheep mandible. Int J Oral Maxillofac Implants 2011, 26, 837–849. [Google Scholar]
- Khayat, P.G.; Arnal, H.M.; Tourbah, B.I.; Sennerby, L. Clinical outcome of dental implants placed with high insertion torques (up to 176Ncm). Clin Implant Dent Relat Res 2013, 15, 227–233. [Google Scholar] [CrossRef]
- Greenstein, G.; Cavallaro, J. Implant insertion torque: its role in achieving primary stability of restorable dental implants. Compend Contin Educ Dent 2017, 38, 88–95. [Google Scholar] [PubMed]
- Aldahlawi, S.; Demeter, A.; Irinakis, T. The effect of implant placement torque on crestal bone remodeling after 1 year of loading. Clinical, Cosmetic and Investigational Dentistry 2018, 10, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Dahdal, S.; Alkhori, I.; Shihabi, S. Evaluation of the effectiveness of high insertion torques on implant stability quotient(ISQ) and marginal bone loss of implants in posterior mandible. Int J Dentistry Oral Sci 2021, 8, 4887–4891. [Google Scholar]
- Elbeialy, R.R.; El-Beialy, W.R. Outcome of dental implants placed with high insertion torque. Egyptian Dental Journal 2017, 63, 299–306. [Google Scholar] [CrossRef]
- Misch, C. Classifications and treatment options of the completely edentulous arch in implant dentistry. Dent Today 1990, 9, 26, 28–30. [Google Scholar]
- Misch, C.E.; Judy, K.W. Classification of partially edentulous arches for implant dentistry. Int J Oral Implantol 1987, 4, 7–13. [Google Scholar]
- Malo, P.; Rangert, B.; Nobre, M. “All-on-Four” immediate-function concept with Branemark system implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res 2003, 5, 2–9. [Google Scholar] [CrossRef]
- Malo, P.; Rangert, B.; Nobre, M. All-on-4 immediate-function concept with Brånemark system implants for completely edentulous maxillae: a 1-year retrospective clinical study. Clin Implant Dent Relat Res 2005, 5, S88–S94. [Google Scholar] [CrossRef]
- Misch, C.E.; Perel, M.L.; Wang, H.L.; Sammartino, G.; Galindo-Moreno, P.; Trisi, P.; Steigmann, M.; Rebaudi, A.; Palti, A.; Pikos, M.A.; Schwartz-Arad, D.; Choukroun, J.; Gutierrez-Perez, J.L.; Marenzi, G.; Valavanis, D.K. Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent 2008, 17, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Daprile, G.; Piatelli, A. Determination of primary stability: a comparison of the surgeon’s perception and objective measurements. Int J Oral Maxillofac Implants 2010, 25, 558–561. [Google Scholar] [PubMed]
- Degidi, M.; Daprile, G.; Piatelli, A.; Iezzi, G. Development of a new implant primary stability parameter: insertion torque revisited. Clin Implant Dent Relat Res 2013, 15, 637–644. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, D.; Sennerby, L.; Meredith, N. Measurements comparing the initial stability of five designs of dental implants: a human cadaver study. Clin Impl Dent Relat Res 2000, 2, 85–92. [Google Scholar] [CrossRef]
- Bartold, P.M.; Kuliwaba, J.S.; Lee, V.; Shah, S.; Marino, V.; Fazzalari, N.L. Influence of surface roughness and shape on microdamage of the osseous surface adjacent to titanium dental implants. Clin Oral Impl Res 2011, 22, 613–618. [Google Scholar] [CrossRef]
- Javed, F.; Almas, K.; Crespi, R.; Romanos, G.E. Implant surface morphology and primary stability: is there a connection? Implant Dent 2011, 20, 40–46. [Google Scholar] [CrossRef]
- Campos, F.E.; Gomes, J.B.; Marin, C.; Teixeira, H.S.; Suzuki, M.; Witek, L.; Zanetta-Barbosa, D.; Coelho, P.G. Effect of drilling dimension on implant placement torque and early osseointegration stages: an experimental study in dogs. J Oral Maxillofac Surg 2012, 70, e43–50. [Google Scholar] [CrossRef]
- Piatelli, A.; Scarano, A.; Balleri, P.; Favero, G.A. Clinical and histological evaluation of an active “implant periapical lesion”. A case report. Int J Oral Maxillofac Implants 1998, 13, 713–716. [Google Scholar]
- Bashutski, J.D.; D'Silva, N.J.; Wang, H.L. Implant compression necrosis: current understanding and case report. J Periodontol 2009, 80, 700–704. [Google Scholar] [CrossRef]
- Duyck, J.; Corpas, L.; Vermeiren, S.; Ogawa, T.; Quirynen, M.; Vandamme, K.; Jacobs, R.; Naert, I. Histological, histomorphometrical, and radiological evaluation of an experimental implant design with a high insertion torque. Clin Oral Impl Res 2010, 21, 877–884. [Google Scholar] [CrossRef]
- Stavropoulos, A.; Cochran, D.; Obrecht, M.; Pippenger, B.E.; Dard, M. Effect of Osteotomy preparation on osseointegration of immediately loaded, tapered dental implants. Adv Dent Res 2016, 28, 34–41. [Google Scholar] [CrossRef]
- Barone, A.; Alfonsi, F.; Derchi, G.; Tonelli, P.; Toti, P.; Marchionni, S.; Covani, U. The effect of insertion torque on the clinical outcome of single implants: a randomized clinical trial. Clin Implant Dent Relat Res 2016, 18, 588–600. [Google Scholar] [CrossRef]
- Marconcini, S.; Giammarinaro, E.; Toti, P.; Alfonsi, F.; Covani, U.; Barone, A. Longitudinal analysis on the effect of insertion torque on delayed single implants: A 3-year randomized clinical study. Clin Implant Dent Relat Res 201, ;20, 322-332.
- Warreth, A.; Polyois, J.; Lee, C.T.; Claffey, N. Generation of microdamage around endosseous implants. Clin Oral Impl Res 2009, 20, 1300–1306. [Google Scholar] [CrossRef]
- Consolo, U.; Travaglini, D.; Todisco, M.; Trisi, P.; Galli, S. Histologic and biomechanical evaluation of the effects of implant insertion torque on peri-implant bone healing. J Craniofac Surg 2013, 24, 860–865. [Google Scholar] [CrossRef] [PubMed]
- Rea, M.; Botticelli, D.; Ricci, S.; Soldini, C.; Gonzáles, G.G.; Lang, N.P. Influence of immediate loading on healing of implants installed with different insertion torques – an experimental study in dogs. Clin Oral Impl Res 2015, 26, 90–95. [Google Scholar] [CrossRef]
- Duyck, J.; Roesems, R.; Cardoso, M.V.; Ogawa, T.; De Villa Camargos, G.; Vandamme, K. Effect of insertion torque on titanium implant osseointegration: an animal experimental study. Clin Oral Implants Res 2015, 26, 191–196. [Google Scholar] [CrossRef]
- Eom, T.G.; Kim, H.W.; Jeon, G.R.; Yun, M.J.; Huh, J.B.; Jeong, CM. Effects of different Implant dsteotomy dreparation sizes on implant stability and bone response in the minipig mandible. Int J Oral Maxillofac Implants 2016, 31, 997–1006. [Google Scholar] [CrossRef]
- Muktadar, A.K.; Gangaiah, M.; Chrcanovic, B.R.; Chowdhary, R. Evaluation of the effect of self-cutting and nonself-cutting thread designed implant with different thread depth on variable insertion torques: An histomorphometric analysis in rabbits. Clin Implant Dent Relat Res 2018, 20, 507–514. [Google Scholar] [CrossRef]
- Simunek, A.; Strnad, J.; Kopecka, D.; Brazda, T.; Pilathadka, S.; Chauhan, R.; Slezak, R.; Capek, L. Changes ins stability after healing of immediately loaded dental implants. Int J Oral Maxillofac Implants 2010, 25, 1085–1092. [Google Scholar]
- Gonzáles-Martin, O.; Lee, E.A.; Veltri, M. CBTC fractal dimension changes at the apex of immediate implants placed using undersized drilling. Clin Oral Impl Res 2012, 23, 954–957. [Google Scholar] [CrossRef]
- Makary, C.; Rebaudi, A.; Mokbel, N.; Naaman, N. Peak insertion torque correlated to histologically and clinically evaluated bone density. Implant Dent 2011, 20, 182–191. [Google Scholar] [CrossRef]
- Canizzaro, G.; Leone, M.; Ferri, V.; Viola, P.; Federico, G.; Esposito, M. Immediate loading of single implants inserted flapless with medium or high insertion torque: a 6-month follow-up of a split-mouth randomized controlled trial. Eur J Oral Implantol 2012, 5, 333–342. [Google Scholar]
- Grandi, T.; Garuti, G.; Samarani, R.; Guazzi, P.; Forabosco, A. Immediate loading of single post-extractive implants in the anterior maxilla: 12-month results from a multicenter clinical study. J Oral Implantol 2012, 38, 477–484. [Google Scholar] [CrossRef]
- Grandi, T.; Guazzi, P.; Samarani, R.; Grandi, G. Clinical outcome and bone healing of implants placed with high insertion torque: 12-month results from a multicenter controlled cohort study. Int J Oral Maxillofac Surg 2013, 42, 516–520. [Google Scholar] [CrossRef]
- Bidgoli, M.; Soheilifar, S.; Faradmal, J.; Soheilifar, S. High insertion torque and peri-implant bone loss: Is there a relationship? J Long Term Eff Med Implants 2015, 25, 209–213. [Google Scholar] [CrossRef]
- De Santis, D.; Cucchi, A.; Rigoni, G.; Longhi, C.; Nocini, P.F. Relationship between primary stability and crestal bone loss of implants placed with high insertion torque: A 3-Year prospective study. Int J Oral Maxillofac Implants 2016, 31, 1126–1134. [Google Scholar] [CrossRef]
- Makary, C.; Menhall, A.; Zammarie, C.; Lombardi, T.; Lee, S.Y.; Stacchi, C.; Park, K.B. Primary stability optimization by using fixtures with different thread depth according to bone density: a clinical prospective study on early loaded implants. Materials (Basel) 2019, 12, 2398. [Google Scholar] [CrossRef]
- Berardini, M.; Trisi, P.; Sinajari, B.; Rutjes, A.W.S.; Caputi, S. The effects of high insertion torque versus low insertion torque on marginal bone resorption and implant failure rates: a systematic review with meta-analyses. Implant Dent 2016, 25, 532–540. [Google Scholar] [CrossRef]
- Li, H.; Liang, Y.; Zheng, Q. Meta-analysis of correlations between marginal bone resorption and high insertion torque of dental implants. Int J Oral Maxillofac Implants 2015, 30, 767–72. [Google Scholar] [CrossRef]
- Lemos, C.A.A.; Verri, F.R.; de Oliveira Neto, O.B.; Cruz, R.S.; Luna Gomes, J.M.; da Silva Casado, B.G.; Pellizzer, E.P. Clinical effect of the high insertion torque on dental implants: A systematic review and meta-analysis. J Prosthet Dent 2021, 126, 490–496. [Google Scholar] [CrossRef]
- Atieh, MA.; Baqain, Z.H.; Tawse-Smith, A.; Ma, S.; Almoselli, M.; Lin, L.; Alsabeeha, N.H.M. The influence of insertion torque values on the failure and complication rates of dental implants: A systematic review and meta-analysis. Clin Implant Dent Relat Res. 2021, 23, 341–360. [Google Scholar] [CrossRef]
- Roca-Millan, E.; González-Navarro, B.; Domínguez-Mínger, J.; Marí-Roig, A.; Jané-Salas, E.; López-López, J. Implant insertion torque and marginal bone loss: A systematic review and meta-analysis. Int J Oral Implantol (Berl). 2020, 13, 345–353. [Google Scholar] [PubMed]
- Patzelt, S.B.M.; Bahat, O.; Reynolds, M.A.; Strub, J.R.S. The all-on-four treatment concept: a systematic review. Clin Implant Dent Relat Res 2014, 16, 836–855. [Google Scholar] [CrossRef]
- Cassetta, M.; Brandetti, G.; Altieri, F. Are the Insertion Torque Value and Implant Stability Quotient Correlated, and If So, Can Insertion Torque Values Predict Secondary Implant Stability? A Prospective Parallel Cohort Study. Int J Oral Maxillofac Implants 2022, 37, 135–142. [Google Scholar] [CrossRef] [PubMed]




| Initial | 7 days | P value | 7 days | 60 days | P value | Initial | 24 months | P value | |
| ITV (Ncm) |
Mean ISQ(SD) | Mean ISQ(SD) | Mean ISQ(SD) | Mean ISQ(SD) | Mean ISQ(SD) | Mean ISQ(SD) | |||
| >70 | 63.5 (10.3) |
62.4 (9.7) |
0.3230 | 62.4 (9.7) |
62.6 (4.2) |
0.4633 | 63.5 (10.3) |
64.7 (6.1) |
0.3245 |
| Initial | 7 days | P value | 7 days | 60 days | P value | Initial | 24 months | P value | |
| ITV (Ncm) |
Mean ISQ(SD) | Mean ISQ(SD) | Mean ISQ(SD) | Mean ISQ(SD) | Mean ISQ(SD) | Mean ISQ(SD) | |||
| ≥ 75 | 76.1 (9.3) |
59.7 (9.3) |
<0.001 | 59.7 (9.3) |
62.0 (8.4) |
0.0102 | 76.1 (9.3) |
65.3 (5.1) |
<0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





