1. Introduction
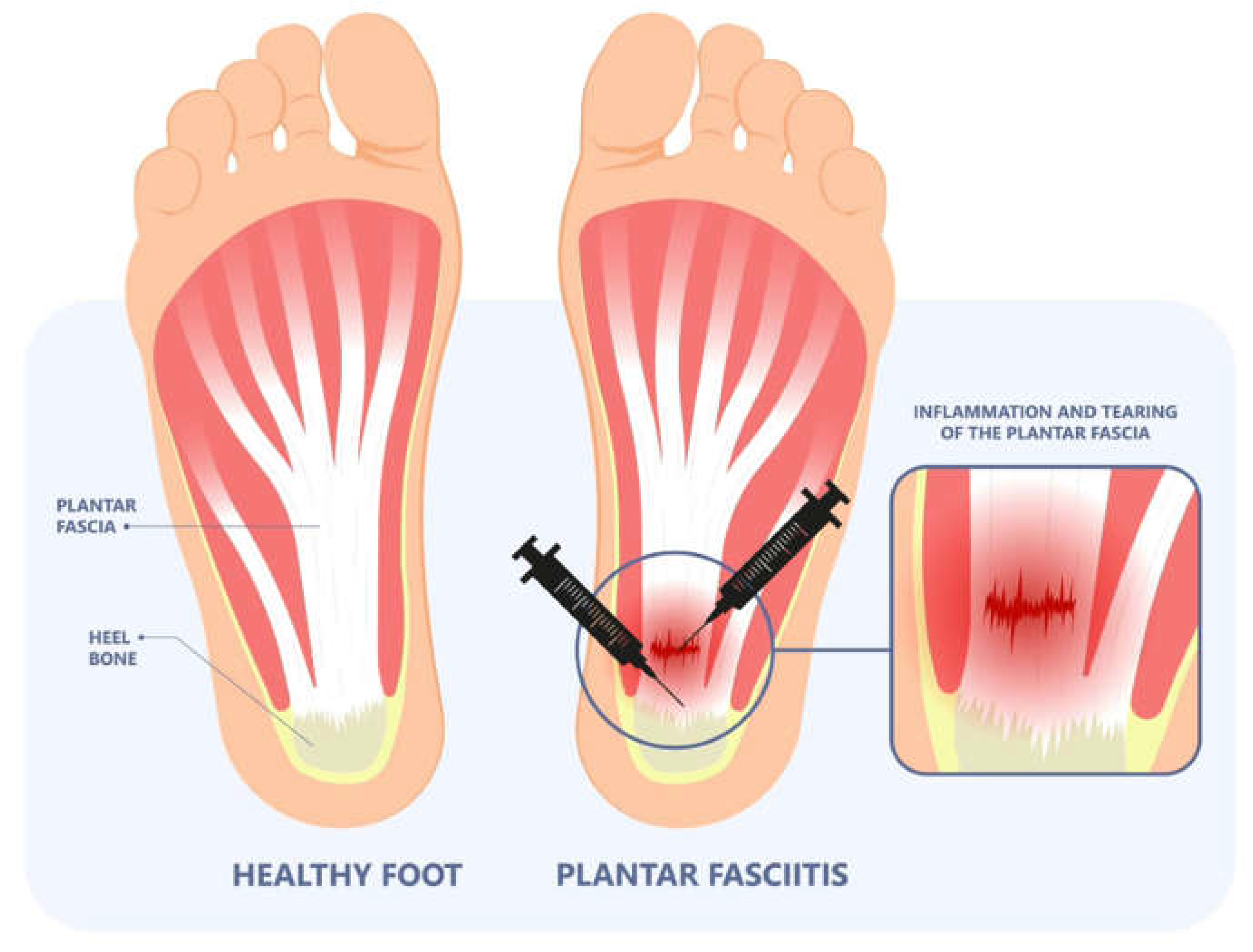
Nearly one in ten people will experience plantar fasciopathy in their lifetime [
1]. Several diverse pathologies, including neurologic, arthritic, traumatic, neoplastic, infectious, or vascular, may lead to plantar enthesopathy [
2]. Enthesopathy experienced in the plantar aspect of the foot may be Plantar Fasciosis (PF), a self-limiting condition often associated with chronic pain and tightness upon standing in the morning and is exacerbated by long periods of standing or walking. A diagnosis is made based on patient history, risk factors, and physical examination. Risk factors often include excessive running, high arch, obesity, and a sedentary lifestyle [
3]. A study by Rano (2001) found that BMI (body mass index) plays a more significant role in plantar enthesopathy than foot structure [
4]. Commonly associated with a high BMI are metabolic syndrome and diabetes, which complicates the diagnosis by adding compression of Baxter’s nerve, the first branch off of the lateral plantar nerve, and tarsal tunnel syndrome, mimicking fascial pain. Another leading factor in Plantar Fasciosis is defects in the collagen matrix within the plantar fascia. The body’s most common protein is collagen, the main structural protein in connective tissues, including plantar fascia [
5]. Micro and larger tears can occur in the plantar fascia band after prolonged strain or repetitive shocks, which, if the stress persists, can ultimately result in the inability of the body to repair itself naturally, resulting in irritation and inflammation.
Primarily due to the unclear etiology of plantar fasciosis, several standard-of-care treatments are available. Still, the most beneficial treatment can only be determined by accurate diagnosis with differentials such as nerve entrapments, micro tears, fibro-lipomas (frequently misdiagnosed as bursae), microfractures of the calcaneus, exostosis, enthesopathy, and systemic inflammatory disorders. Three categories exist in which standard, nonsurgical treatments are classified. Treatments are typically divided into reducing pain and inflammation, reducing tissue stress, and restoring muscle strength and flexibility of involved tissues [
6]. Standard-of-care treatment options for plantar fasciosis often include corticosteroid injections, non-steroidal anti-inflammatory drugs (NSAIDs), night splints, taping, stretching, exercise, foot orthosis, and extracorporeal shock wave therapy [
7]. Regarding pain treatment, a study by Nahin (2018) found that most patients use over-the-counter medications, such as NSAIDs, whereas approximately 40% of patients use prescription medications [
8]. The number of PF cases has more than doubled from 2010 to 2018 and is likely to continue to increase, ultimately raising the annual economic burden of PF. Each year, nearly
$600 is spent per person on NSAIDs alone. Including additional costs of standard treatment, the annual cost associated with PF is
$284 million [
9]. However, most PF studies follow patients up to less than one year. Given the chronic and relapsing nature of PF, more research needs to be conducted to understand the best treatment mode and better estimate the overall economic burden of PF [
10]. If a patient has attempted standard care of treatment with no relief after 6 to 12 months, they may qualify for partial or complete plantar fasciotomy. Of the patients who have failed standard-of-care treatments and qualify for plantar fasciotomy, patients with no previous foot trauma and only unilateral symptoms attain the best results from an endoscopic plantar fascia release [
11]. While surgical interventions have shown some success, the removal of greater than 40% of the plantar fascia may have detrimental effects on other ligamentous and bony structures in the foot [
12]. Another study showed that during an open partial release of the plantar fascia, an incision of the fascia greater than 50% was associated with increased pain [
13]. With the increased risk of detrimental effects after surgery and a potential increase in pain, especially in the lateral column, there is a clear need for additional treatment options.
Given the limited treatment options for defects of the plantar fascia, we propose using Wharton’s Jelly (WJ) to supplement the damaged tissue to minimize the negative symptoms of plantar fasciosis when used alongside non-surgical standard-of-care practices. Specifically, Wharton’s jelly contains collagen types I, III, and V and fibrous structures comparable to the extracellular matrices (ECM) of human articular cartilage, tendons, and dermal tissues [
14]. WJ protects vessels in the umbilical cord from external forces. A recent study shows that when WJ is used, significant defects in the articular cartilage scaffold can be mitigated [
15]. As there is a clear need for an alternative intervention for plantar enthesopathy, we present a retrospective analysis of Wharton’s jelly used with shockwave therapy and class IV lasers for defects in the plantar fascia.
2. Materials and Methods
2.1. Materials and Methods
All methods complied with the FDA and American Association of Tissue Banks (AATB) standards. This study was conducted under an Institute of Regenerative and Cellular Medicine IRB-approved protocol (RL-UCT-001), and informed consent was obtained from the study participants. The Wharton’s jelly tissue allografts were processed and distributed by Regenative Labs. CryoText Plus is a minimally manipulated WJ allograft tissue product for homologous use only. The Wharton’s jelly is aseptically dissociated from the rinsed umbilical cord. After dissociation, 100 mg of Wharton’s Jelly is suspended in approximately 2mL of sterile Sodium Chloride 0.9% solution (normal saline)(Regenative Labs, Pensacola, FL, USA). FDA guidelines specify minimal manipulation as a human tissue product is not combined with any article except saline and FDA-approved cryopreservatives. The regulations of the human cell and tissue product (HCT/P) require extensive testing to ensure that there are no clinical safety concerns for tissue products. The allografts were purchased by the clinic from Regenative Labs. Patient recruitment, allograft application, and patient tracking were performed at Parker Foot and Ankle.
2.2. Case Presentation
This study included seven consenting individuals who presented with either left or right plantar fasciosis. All individuals had previously exhausted standard-of-care treatment options. The study sample was 57% male and 43% female. The age of the sample ranged from 47 to 66- years- old. Of the sample, five individuals received WJ to the defect site on their left foot, leaving the two remaining individuals to receive WJ to the defect on their right foot. Each individual received a single application of 1cc CryoTextPlus, class IV laser therapy, extracorporeal pulse-activated therapy (EPAT), and a pneumatic boot by Dr. Parker at his clinic, Parker Foot and Ankle, in Houston, Texas. All patients were prescribed optional medication to help combat discomfort. After the initial application, all individuals were assessed at a follow-up visit approximately 11 weeks later to evaluate pain improvement and to ensure no adverse side effects. This series aims to present improvements in patient-reported pain scales after the application of WJ to the site of tissue defect, including laser therapy, EPAT, and a pneumatic boot.
| Patient Number |
Gender |
Age |
Affected Foot |
| 1 |
Female |
47 |
left |
| 4 |
Male |
50 |
left |
| 5 |
Male |
50 |
right |
| 6 |
Female |
57 |
right |
| 7 |
Female |
64 |
left |
| 8 |
Male |
63 |
left |
| 9 |
Male |
66 |
left |
2.3. Patient Care Procedures
The multi-step procedure includes EPAT, applying an umbilical cord tissue matrix known as Wharton’s Jelly, class IV laser therapy, and a walking boot. The lower extremity was prepped and draped in the standard sterile technique. Before applying the tissue allograft, most patients received EPAT at 11 Hrtz, 3.0 bars, and 3231 to 3432 pulses to the affected tissue. One patient received EPAT at 11 Hrtz, 1.4 bars, and 3532 pulses according to the patient’s tolerance. The WJ product used in this study was 1cc of CryoTextPlus, a minimally manipulated tissue allograft. While the patient received EPAT, CryoTextPlus was thawed slowly in a 35-degree bath per laboratory guidelines. The allograft was transplanted along the plantar medial origin of plantar fascia throughout the inflamed tissues utilizing MyLab 15.0 MHz real-time diagnostic ultrasound guidance with a 4 cm transducer head (
Figure 1). Further “needling” in a pin-cushion technique with a 22 gauge needle was performed to encourage neovascularization. At the end of the procedure, the patients received a prefabricated pneumatic boot that was examined for proper fitting. The patient was shown and instructed in detail on how to properly wear and care for the device and demonstrate the ability to apply the device correctly and ambulate without distress. Six patients were prescribed acetaminophen, and one was prescribed hydrocodone for pain management. The patients received class IV laser treatments twice a week for two weeks. The patient’s pain was determined using a visual analog scale (VAS), scoring numerically zero through ten at the initial visit and then again at an average of thirteen weeks after the start of care.
3. Results
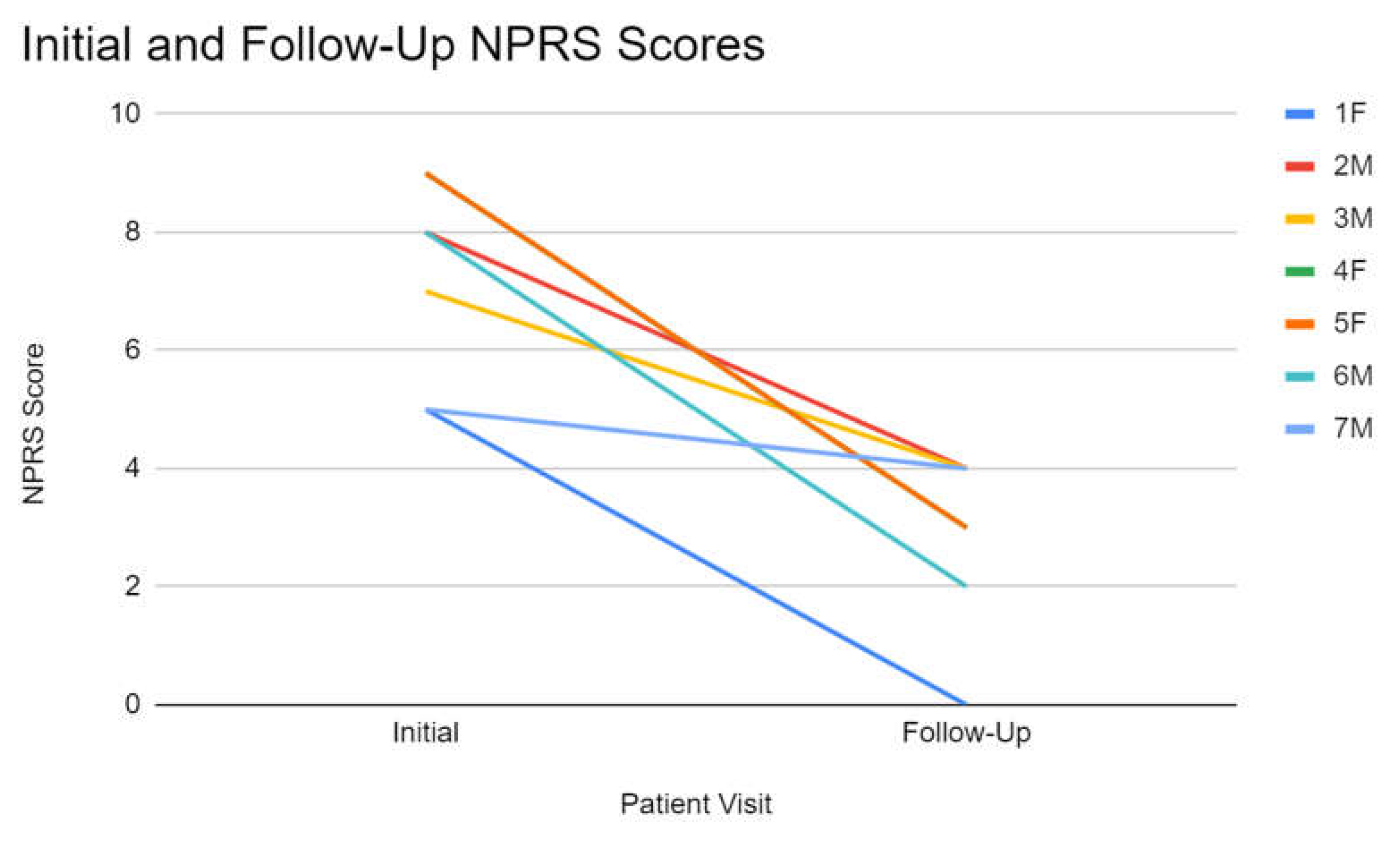
The sample’s initial average VAS score was 6.88. With a 50% improvement, the final average VAS score was 3.44. When comparing gender improvement, females had an initial VAS of 7.66 and a final VAS of 2, which improved 74%. In comparison, males had an initial VAS of 7 and a final VAS of 3.5, improving 50%.
4. Discussion
The results show significant improvement in patient-reported pain relief after utilizing umbilical cord tissue allografts in combination with laser therapy, EPAT, and a pneumatic boot (
Figure 2). The umbilical cord tissue allografts applied in a homologous fashion function as a scaffolding matrix to supply structural support to the damaged tissue. In the umbilical cord, Wharton’s jelly provides structural support and cushioning against compressive forces to ensure the vessels it encases do not tear, stretch, or be subject to excess pressure. Components such as growth factors, cytokines, hyaluronic acid, and extracellular vesicles are found in WJ, contributing to WJ’s regenerative effects [
16]. The tissue allograft is minimally manipulated and immune privileged, so when it is transplanted into the defect of tissue with the same basic function, it supplements the missing or damaged tissue without eliciting an immune response from the recipient.
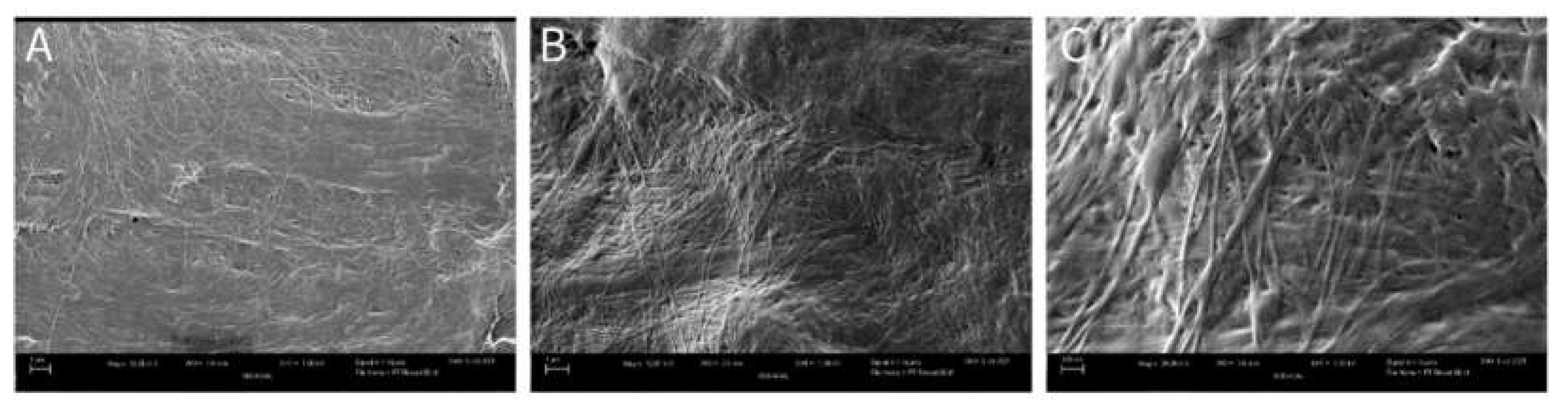
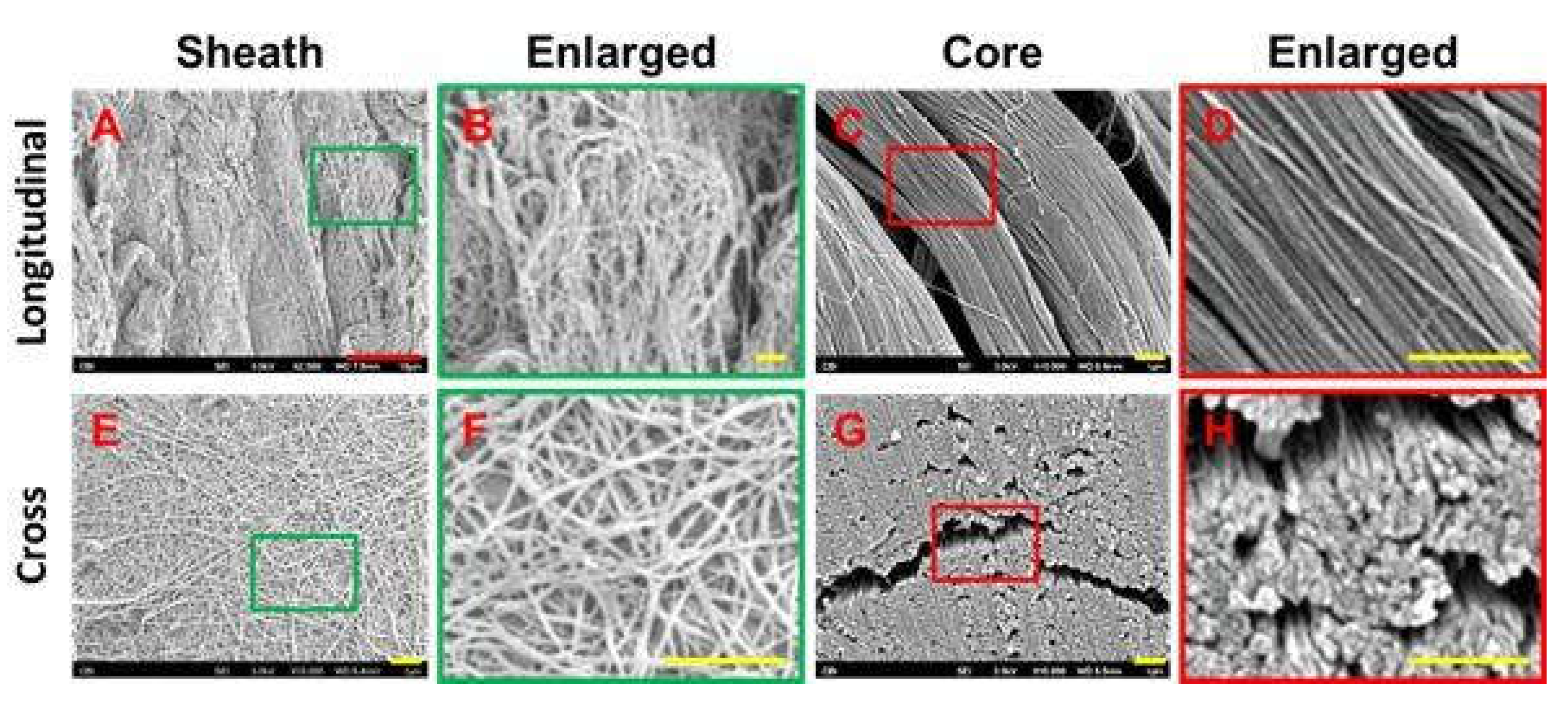
On a molecular level, the similarities in the structure of WJ and the plantar fascia allow for proper and effective supplementation of tissue. Scanning electron microscope (SEM) images of WJ tissue product’s preserved collagen structure compared to an SEM image analysis of healthy plantar fascia reveals homologous crosslinked collagen structures (
Figure 3 and
Figure 4) [
17]. Plantar fascia and WJ are both primarily composed of type 1 collagen [
16]. With structural similarity and makeup at a molecular level, the homologous implementation of WJ into damaged plantar fascia provides equivalent tissue for successful transplantation. SEM imaging of WJ tissue allografts showcases its ability to function as an architectural scaffold for ECM supplementation not only in the fascia but in many other connective tissues around the body.
With the tissue allograft being applied in a fanning technique, it is evenly distributed, allowing optimal coverage of the defective tissue and surrounding area. A pin-cushion technique was utilized to create micro-tears in the tendon, which sends messages to the body to excrete its own growth factors and cause neovascularization. New neovascularization accelerates the nitric oxide pathway, begins transcription, and helps with anti-inflammatory activity, which catalyzes the body’s natural repair process.
EPAT application before WJ injection functions as a modern physiotherapeutic method in treating musculoskeletal conditions [
18]. A study by Saxena (2011) demonstrated safe, viable, and successful outcomes in treating Achilles tendinopathy utilizing EPAT as an independent treatment option [
19]. The study found that 78.38% of tendons showed clinically significant improvement by at least one year post-treatment [
19]. No adverse reactions were reported within the study, making EPAT a safe, viable option in the treatment of musculoskeletal conditions.
Laser therapy provides photobiomodulation as a pain-reducing, anti-inflammatory, and tissue-improving modality. Class IV high-intensity laser therapy (HILT) decreases erythrocyte deformability and platelet coagulation, resulting in membrane revitalization, viscosity reduction, and erythrocyte stress adaptation [
20]. With more efficient blood flow, the body’s natural healing factors can be administered to the defective site quicker. High-power class IV laser therapy was used as a pain relief option for patients with oral mucositis [
21]. The study reported an immediate decrease in pain after 94% of sessions, over 50% pain reduction in 61%, and complete elimination of initial pain in 35% of sessions. There were zero reports of increased pain following laser therapy. High-power laser therapy provides non-pharmacologic, patient-friendly, long-lasting, rapid pain relief [
21]. Given the success of independent laser therapy, strong reasoning stands to utilize laser therapy in conjunction with other modalities to increase the success rate of treating plantar fasciosis.
The treatment plan’s final component is applying a pneumatic walking boot. The function of the boot is to restrict and limit motion, provide stabilization, immobilize, and add compression to the affected area. Combining the application of WJ tissue allograft, EPAT, laser therapy, and boot application lays the foundation for a new, promising patient care protocol for plantar fasciosis. The results of this study provide data that suggest combining the four modalities improves the symptoms of plantar fasciosis. The 50% improvement in VAS scores reported in this study warrants further research with a larger cohort. The continuation of this research will include grading the thickness of the plantar fascia before and after the applications and additional follow-up visits at 30 days and 120 days post-care procedures with more specified lower extremity pain questionnaires. would further evaluate the efficacy and safety of this protocol in addition to assisting in defining dosage protocols.
5. Conclusions
In conclusion, the observational data obtained from the seven patients presenting with defects of the Plantar Fascia leading to Plantar Fasciosis reports WJ in combination with EPAT, laser therapy, and a pneumatic boot demonstrates statistically significant improvement in pain. Provided that this study has shown success, the reason exists to complete further research to compare this alternative protocol with the current non-surgical standard of care options. Future implications for the use of WJ in conjunction with standard care practices could significantly improve patient outcomes and potentially prevent or postpone invasive surgical procedures in many musculoskeletal defects.
Author Contributions
Conceptualization, R.P., J.S. and T.B.; methodology, R.P.; software, T.Y.; validation, N.L., C.W. and T.Y.; formal analysis, N.L., C.W.; investigation, R.P.; resources, N.L., C.W.; data curation, R.P.; writing—original draft preparation, R.P., N.L., C.W.; writing—review and editing, R.P., N.L., C.W.; visualization, R.P., T.B.; supervision, J.S., T.B.; project administration, T.B.; funding acquisition, R.P., T.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of the Institute of Regenerative and Cellular Medicine (protocol code IRCM-2022-311 and approved on 12 January 2022).
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper
Data Availability Statement
All relevant data in this study is reported within the manuscript.
Acknowledgments
The authors would like to thank Desiree Hornung, administrator, and the staff Stacy, Laura and Greta, at Parker Foot and Ankle for their contribution to data collection and filing.
Conflicts of Interest
Regenerative Labs did not fund Dr.Parker or compensate him for doing this study. The research department of Regenative Labs worked on this publication along with Dr.Parker because he is a clinical site in the ongoing retrospective study backed by an IRB at the IRCM but does not receive any funding or payment from this research.
References
- Trojian, T.; Tucker, A.K. Plantar Fasciitis. Am Fam Physician. 2019, 99, 744–750. [Google Scholar] [PubMed]
- Thomas, J.L.; Christensen, J.C.; Kravitz, S.R.; Mendicino, R.W.; Schuberth, J.M.; Vanore, J.V.; Weil, L.S.; Sr Zlotoff, H.J.; Bouché, R.; Baker, J. ; American College of Foot and Ankle Surgeons heel pain committee (2010). The diagnosis and treatment of heel pain: a clinical practice guideline-revision 2010. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons, 49 (3 Suppl), S1–S19. [CrossRef]
- Goff, J.D.; Crawford, R. Diagnosis and treatment of plantar fasciitis. American family physician 2011, 84, 676–682. [Google Scholar] [PubMed]
- Rano, J.A.; Fallat, L.M.; Savoy-Moore, R.T. (2001). Correlation of heel pain with body mass index and other characteristics of heel pain. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons, 40(6), 351–356. [CrossRef]
- Alabau-Dasi, R.; Nieto-Gil, P.; Ortega-Avila, A.B.; Gijon-Nogueron, G. (2022). Variations in the Thickness of the Plantar Fascia After Training Based in Training Race. A Pilot Study. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons, S1067-2516(22)00054-0. Advance online publication. [CrossRef]
- Cornwall, M.W.; McPoil, T.G. (1999). Plantar fasciitis: etiology and treatment. The Journal of orthopaedic and sports physical therapy, 29(12), 756–760. [CrossRef]
- Heide, M.; Mørk, M.; Røe, C.; Brox, J.I.; Fenne Hoksrud, A. (2020). The effectiveness of radial extracorporeal shock wave therapy (rESWT), sham-rESWT, standardised exercise programme or usual care for patients with plantar fasciopathy: study protocol for a double-blind, randomised, sham-controlled trial. Trials, 21(1), 589. [CrossRef]
- Nahin, R.L. (2018). Prevalence and Pharmaceutical Treatment of Plantar Fasciitis in United States Adults. The journal of pain, 19(8), 885–896. [CrossRef]
- Ahn, J.; Yeo, J.; Lee, S.H.; Lee, Y.J.; Park, Y.; Goo, B.; Ha, I.H. (2023). Healthcare usage and cost for plantar fasciitis: a retrospective observational analysis of the 2010-2018 health insurance review and assessment service national patient sample data. BMC health services research, 23(1), 546. [CrossRef]
- Rhim, H.C.; Kwon, J.; Park, J.; Borg-Stein, J.; Tenforde, A.S. (2021). A Systematic Review of Systematic Reviews on the Epidemiology, Evaluation, and Treatment of Plantar Fasciitis. Life (Basel, Switzerland), 11(12), 1287. [CrossRef]
- Hogan, K.A.; Webb, D.; Shereff, M. (2004). Endoscopic plantar fascia release. Foot & ankle international, 25(12), 875–881. [CrossRef]
- Thompson, J.; Saini, S.; Reb, C.; Daniel, J. (2014). Diagnosis and Management of Plantar Fasciitis. Journal of Osteopathic Medicine, 114(12), 900-901. [CrossRef]
- Brugh, A.M.; Fallat, L.M.; Savoy-Moore, R.T. Lateral column symptomatology following plantar fascial release: a prospective study. J Foot Ankle Surg. 2002 Nov-Dec;41(6):365-71. [CrossRef] [PubMed]
- Sobolewski, K.; Bańkowski, E.; Chyczewski, L.; Jaworski, S. (1997). Collagen and glycosaminoglycans of Wharton’s jelly. Biology of the neonate, 71(1), 11–21. [CrossRef]
- Davis, J.M.; Sheinkop, M.B.; Barrett, T.C. (2022). Evaluation of the Efficacy of Cryopreserved Human Umbilical Cord Tissue Allografts to Augment Functional and Pain Outcome Measures in Patients with Knee Osteoarthritis: An Observational Data Collection Study. Physiologia, 2(3), 109–120. [CrossRef]
- Gupta, A.; Maffulli, N.; Rodriguez, H.C.; Carson, E.W.; Bascharon, R.A.; Delfino, K.; Levy, H.J.; El-Amin, S.F. , 3rd. (2021). Safety and efficacy of umbilical cord-derived Wharton’s jelly compared to hyaluronic acid and saline for knee osteoarthritis: study protocol for a randomized, controlled, single-blind, multi-center trial. Journal of orthopaedic surgery and research, 16(1), 352. [CrossRef]
- Zhang, J.; Yang, Q. (2020). Research on plantar fasciitis. Journal of Stem Cells Research, Development & Therapy, 6(4), 1–8. [CrossRef]
- Rajfur, K.; Rajfur, J.; Matusz, T.; Walewicz, K.; Dymarek, R.; Ptaszkowski, K.; Taradaj, J. (2022). Efficacy of Focused Extracorporeal Shock Wave Therapy in Chronic Low Back Pain: A Prospective Randomized 3-Month Follow-Up Study. Medical science monitor : international medical journal of experimental and clinical research, 28, e936614. [CrossRef]
- Saxena, A.; Ramdath, S., Jr.; O’Halloran, P.; Gerdesmeyer, L.; Gollwitzer, H. (2011). Extra-corporeal pulsed-activated therapy (“EPAT” sound wave) for Achilles tendinopathy: a prospective study. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons, 50(3), 315–319. [CrossRef]
- Brandl, A.; Egner, C.; Reisser, U.; Lingenfelder, C.; Schleip, R. (2023). Influence of high-energy laser therapy to the patellar tendon on its ligamentous microcirculation: An experimental intervention study. PloS one, 18(3), e0275883. [CrossRef]
- Finfter, O.; Cohen, R.; Hanut, A.; Gavish, L.; Zadik, Y. (2023). High-power laser photobiomodulation therapy for immediate pain relief of refractory oral mucositis. Oral diseases, 10.1111/odi.14618. Advance online publication. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).