1. Introduction
Terminal ileitis (TI) is chronic inflammation of the terminal portion of the ileum. This condition is typically diagnosed endoscopically and histologically. The presence of superficial or deep ulcers in the terminal ileum upon either direct visualization or histologic inspection following biopsy is consistent with this diagnosis.1 TI most commonly presents with right lower quadrant abdominal pain. Other common associated symptoms include nausea, vomiting and diarrhea. In patients with these symptoms, a workup will be initiated that will eventually lead to an endoscopic diagnosis with TI. The most common macroscopic findings in patients with TI include ulcers, nodular or erythematous mucosa, and polypoid lesions.2 Many times significant histopathologic features of the ileum can be discovered following endoscopy and biopsy but these patients with TI can be asymptomatic. The incidental finding of TI in asymptomatic patients can be attributed to the increased frequency of colonoscopy with ileoscopy in patients for screening. A recent study found that in a subset of individuals diagnosed with TI based on the macroscopic histological findings on biopsy described above, 91.2% were deemed to have non-specific findings.3 The lack of diagnostic specificity in patients with asymptomatic TI presents problems in subsequent workup and potential therapy. This is exacerbated by the fact that TI is commonly associated with the diagnosis of Crohn’s disease (CD) by many clinicians which can lead to misdiagnosis and treatment of a condition that is not truly present.
2. Mimickers of CD
Classically, TI is associated with a diagnosis of CD, as this is the most common portion of the gastrointestinal (GI) tract affected in patients with this disease. However, there are many other causes of terminal ileitis that need to be evaluated before initiating treatment for Crohn’s disease. These causes of TI, if not considered well, have potential consequences without proper treatment. The treatments for some of these other etiologies of TI also are often much less debilitating with fewer side effects, compared to lifelong CD therapy. Some of these alternative etiologies of TI include ulcerative colitis (UC), small bowel tuberculosis, and malignancy. Another etiology that is paramount to keep in the differential when performing a workup for TI is non-steroidal anti-inflammatory (NSAID) use.4 This is a particularly important example of an etiology of TI with a much simpler and safer treatment as opposed to CD, as suggested above.
NSAID use has become so widespread and significant, especially recently with increased efforts to limit the opioid prescription epidemic, that patients and clinicians alike run the risk of overlooking excessive use as a potential health concern. Similarly, while the association of NSAIDs and irritation and ulceration of the stomach and duodenum are well understood by both the medical community and general public, the potential danger that this medication class poses to the lower portions of the GI tract simply are not well known. Patients will likely not report NSAID use when discussing their symptoms as they are likely not aware of their potential harmful effect. Clinicians may also forget to ask about NSAID use and may also be less likely to consider NSAIDs as a cause of inflammation of the ileum in particular.4 Manifestations of TI associated with NSAID enteropathy have the potential to be equally as severe. Macroscopic findings include ulcerations and erythema. The ileocecal valve is more commonly affected in NSAID associated TI and diaphragmatic strictures of the ileum are considered pathognomonic for NSAID induced damage.2 TI due to NSAIDs is more commonly asymptomatic compared to a systemic process like CD. This is important to be aware of this presentation and repeat colonoscopy with ileoscopy after NSAID cessation.
As alluded to earlier, there are many causes of terminal ileitis beyond CD and NSAID use. They can range from self-limiting infections to infiltrative disorders or other systemic processes as well as even malignancy. The etiologies range from relatively benign to more concerning conditions and using other clues in the history and physical examination can help to arrive at the correct diagnosis. Eosinophilic gastroenteritis is one such differential diagnosis and it can present with symptoms similar to CD such as abdominal pain and diarrhea.5,6 Endoscopically there may be erythema, erosions and eventually strictures leading to obstruction.7 However biopsies obtained would have significant infiltration by eosinophils unlike in CD.8–10 Hence the presence of significant number of eosinophils on the pathology specimen can help to differentiate from CD. Intestinal tuberculosis commonly manifests as terminal ileitis and has similarly detrimental and potentially devastating long-term effects as CD. The ileocecal region is frequently affected in intestinal tuberculosis.11 Both conditions can present with ulcerations, stenosis, fistulas.7 Like CD, the treatment regimen of someone diagnosed with intestinal tuberculosis following a diagnosis of terminal ileitis is far from benign and could pose significant health risks and side effects to the patient by itself. Apart from having involvement of the intestine, the patient may have pulmonary involvement as well in cases of tuberculosis as well as risk factors such as being from an endemic part of the world, having history of incarceration or being immunocompromised among others. This is another reason why ruling out a more manageable terminal ileitis etiology like NSAID use is vital to avoid unnecessary and potentially harmful treatment regimens. In the history of such patients, there may be some clues that may also help to arrive at the correct diagnosis as well as potential risk factors that may be present. There are also more manageable infections that can result in terminal ileitis including Cytomegalovirus (CMV) ileitis, Salmonella and Yersinia infections.1 These acute infections do not have the same chronic risks that tuberculosis or CD present. Biopsy and culture during colonoscopy are the best ways to diagnose these acute infections.4 The history itself may also provide some information such as being immunocompromised or exposure to sick contacts.
Another key etiology to bear in mind when faced with a histopathological diagnosis of terminal ileitis is malignant disease. In the small bowel, lymphoma is the most common malignancy, representing nearly half of all cases, followed by adenocarcinoma and leiomyosarcoma.4 In terms of clinical presentation, it is essentially impossible to distinguish malignancy from any of the other etiologies previously discussed. When presenting as a solitary mass, lymphoma in the small bowel can narrow the lumen in a very similar fashion to CD, such that the two might be confused even during endoscopy.4 Circumferential thickening of the terminal ileum along with ulceration and fistula formation can occur similar to CD.12,13 It can also lead to ulcerations in addition to obstruction in the terminal ileum and can be detected on ileoscopy.13,14 This unfortunate tendency for a similar presentation requires the clinician to be vigilant in the terminal ileitis workup.
Other mimickers that need to be kept in mind include vasculitides and infiltrative disorders.7 Behcet’s disease is an example of inflammatory condition that involves multiple systems including the gastrointestinal tract and present with ulcerations involving the terminal ileum as well as similar clinical symptoms.15,16 It can also have skipped lesions but they tend to be less diffuse as compared to CD.17 Infiltrative disease such as amyloidosis and sarcoidosis can also involve the small bowel and present with TI.7 These are more systemic processes and will likely have involvement of multiple organs at the same time as compared to CD though CD may also exhibit certain extra-intestinal manifestations. The extra-intestinal manifestations may such as oral aphthous ulcers, erythema nodosum may also be present in cases of some of the vasculitides.
Additionally, in attempting to workup newly discovered terminal ileitis, it is important to keep in mind the results of one study that found that asymptomatic terminal ileitis (without clinical features including diarrhea, fever, GI bleeds, or weight loss) improved with only symptomatic therapy. Aggressive therapy for CD, for example, is unnecessary in patients who do not present with the significant clinical features. In some cases, this premature treatment of CD can cause negative health consequences on its own. Hence considering a repeat endoscopic assessment with a colonoscopy after a time interval may be a good option to evaluate for any progression of disease along with monitoring the clinical course as opposed to aggressive initiation of medical therapy.
In one case report of a patient presenting with bloody diarrhea and an area of stenosis in the transverse colon, the histological interpretation was “consistent with Crohn’s disease”.18 The patient was started first on glucocorticoids and then on azathioprine when the steroids yielded no improvement. All of the medications attempted caused significant side effects to the patient without relieving his initial symptoms.18 Stricturoplasty was performed and medications without any clinical benefit. It was only after another pathologist examined the initial specimen that a tentative diagnosis of NSAID induced colopathy was suggested and further corroboration of the medical history revealed an extensive history of diclofenac usage.18 This patient did not have terminal ileitis, but protean presentations and inadequate history taking can lead to misdiagnosis.
It is important to consider other etiologies of TI before prescribing therapy for CD. A lack of improvement on a CD treatment regimen might be an indication to investigate other potential etiologies and could subsequently save the patient significant negative effects from unneeded medications.
3. Methods
After obtaining Institutional review board (IRB) approval we obtained medical records utilizing ICD-10 (International Classification of Diseases, Tenth Revision) codes K50.0-K52.0 (Crohn’s disease [regional enteritis], Ulcerative colitis, Other and unspecified noninfective gastroenteritis and colitis). All the charts were reviewed and 229 patients met the inclusion criteria. The inclusion criteria was presence of isolated terminal ileitis that was biopsy proven. This was a retrospective study performed by reviewing the charts of patients at our academic medical center diagnosed with biopsy proven isolated terminal ileitis from May 2011 through May 2016. Demographics and diagnostic information was then collected from the existing medical records of these patients (
Supplementary Tables 1,2). The gathered demographic data for each patient included age, gender, and body mass index (BMI). It was then noted whether patients had associated CD, ulcerative colitis, or evidence of another etiology either based on biopsy results or clinical workup. The degree of each patient’s workup and the subsequent results were tabulated; these parameters included stool culture, presence of bacteria in the culture,
Clostridium difficile (C. difficile) testing results, CT scan indicative of ileitis, colonoscopy with ileoscopy, and inpatient evaluation (with length of hospital stay if applicable) versus outpatient evaluation. The details of the biopsy report of the terminal ileitis were noted as well. Finally, each patient’s treatment for the ileitis was detailed including medications and any gastrointestinal surgeries that had been performed. Following the data collection, the data was analyzed using SPSS software with chi square analysis used to analyze the categorical variables. P<0.05 was considered statistically significant.
4. Results
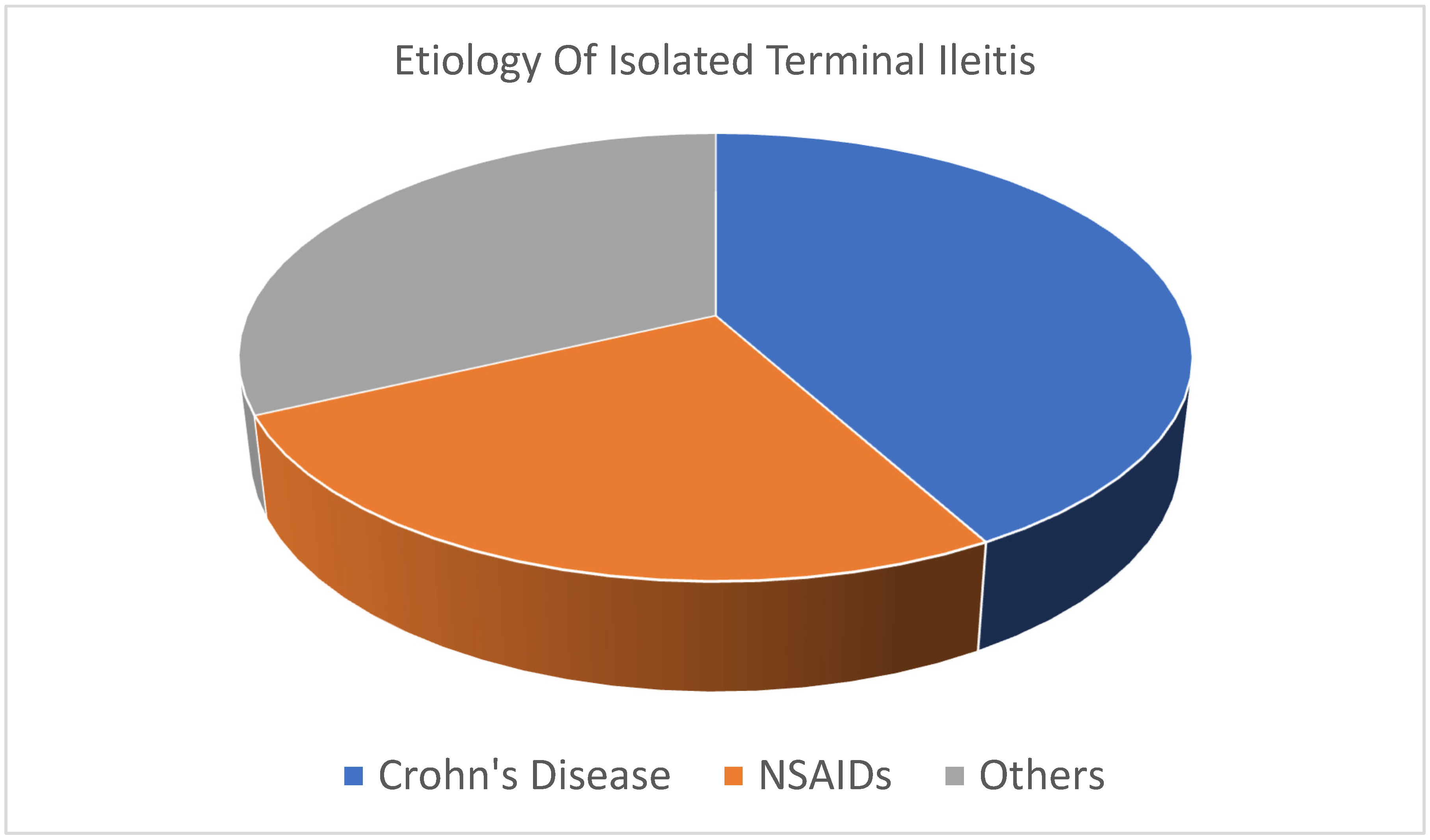
A total of 229 patients with isolated terminal ileitis on biopsy were reviewed. The mean age of our patients was 43.7 years old. Of the patient group, 49% (n=113/229) were males and the rest were females. Only 42% of patients with ITI were eventually diagnosed with Crohn’s disease. Stool cultures were performed in 37% (n=86/229) of patients with positive results in 0.04% (n=4/86) of the patients. Most patients were treated with antibiotics after diagnosis of ileitis without determination of the exact etiology of the condition. Amongst those evaluated, one had tuberculosis, one had ischemic ileitis and one had Meckel’s diverticulum. Non-steroidal anti-inflammatory drug use accounted for 26% (n=59/229) of ITI cases.
Figure 1 depicts the common etiologies of isolated terminal ileitis.
Treatment generally involved antibiotics, initiation of biologics or use of mesalamine products. The mean length of hospitalization was 1.25 days. Mean BMI of our patients was 25 kg/m2 and there was no statistically significant association noted between ITI and BMI. Presence of Crohn’s disease with ITI had a statistically significant association with positive C. difficile infection and subsequent need for treatment with biologics for isolated disease (p<0.001).
5. Discussion
Terminal ileitis is an entity that is encountered more readily given the increasing number of colonoscopies being performed along with intubation of the terminal ileum. This gives rise to the thought as to whether the terminal ileum should be intubated in all patients or not especially if they are asymptomatic.3 This may often be incidentally detected in asymptomatic patients and also on other diagnostic modalities such as imaging studies and capsule endoscopy may also reveal inflammation in the terminal ileum.7 As mentioned earlier, at times even CD can be asymptomatic and be mild enough that may not warrant treatment in every case especially aggressive treatment. However, as colonoscopies are performed for screening and surveillance, often the terminal ileum is intubated as part of routine practice. When terminal ileitis is discovered in completely asymptomatic patients then it poses a great dilemma for the provider and the patient. It can lead to extensive additional work up and even possibly a repeat endoscopic procedure in the future for follow up to assess whether the changes persist or resolve or evolve. At times they may resolve especially if due to self -limiting conditions or due to recent exposure to medications such as NSAIDs. Hence the finding of terminal ileitis on routine colonoscopies performed in asymptomatic patients is a challenge to address. There are numerous etiologies of terminal ileitis apart from CD and it is important to consider these differentials when evaluating a patient for TI. Not only CD, but also Ulcerative Colitis can lead to TI.5 Other inflammatory disease states such as vasculitides as well as infectious etiologies, medications, malignancies or infiltrative processes (amyloidosis, sarcoidosis) can all potentially lead to TI.7 Given the wide range of potential underlying etiologies and considerably different treatment approaches, it is imperative to be aware of them.
In reviewing the medical charts of these patients diagnosed with TI, multiple variables revolving around their workup and treatment were documented and subsequently analyzed. The primary goal of this project was to gain a better understanding of exactly what processes are causing terminal ileitis in patients with that diagnosis. As the title of this paper suggests, CD is the most likely etiology behind TI in patients with the histological diagnosis and this study supports this notion. Of the 229 patients with TI that were reviewed, CD was the most common etiology. However, this was not by a majority; 42% of the patients with TI were found to have a diagnosis of CD. This gives further credence to the notion discussed in other studies noted in the introduction that while CD is highly associated with TI, there are many other etiologies that must be considered. Our review of these charts confirms that this remainder, those with TI that is not associated with CD, is not at all insignificant. In fact, based on our findings, it is more likely for a patient with TI to have an associated etiology that is not CD.
Of the multiple potential etiologies for TI, the most common one in this study, besides CD, was found to be NSAID-associated TI. NSAID use accounted for 26% of the TI cases reviewed. Previous studies have noted the often overlooked danger of NSAID use in the GI tract. While the potential for ulceration and inflammation in the stomach as a result of NSAID use is well studied and noted by clinicians, the similar effects on the small intestine and colon have not been widely reported. NSAIDs can disrupt the gut mucosal barrier and this is speculated to possibly predispose to development of IBD as it allows the microbiome of the gut to be exposed to the immune system.7 NSAIDs along with aspirin may also contribute by impacting the release of inflammatory markers and altering the aggregation of platelets.19,20 One previous study has shown that stenosis and ulceration of the colon can be directly linked to NSAID use18 and review articles readily report the association of NSAID use and ileitis, along with other portions of the intestine.4 In this study, the goal was to specifically tie NSAID use with inflammation of the ileum in particular. The data collected show a definite correlation between the two, with a significant portion of cases examined here being directly linked to NSAID use. This study aimed to explore various etiologies of TI beyond CD and it was successful in achieving that goal, with multiple other etiologies including UC and malignancy being noted, however the NSAID use finding is particularly notable and important.
As noted earlier, much of the importance in recognizing NSAID use as a common cause of TI is the significantly different therapy that would be used for that diagnosis as opposed to TI resulting from CD, for example. A therapy as simple as stopping all NSAID intake is naturally going to be much safer for the patient than a potentially immune modulating CD treatment regimen. As described in the case study earlier, doctors run the risk of subjecting patients to unnecessary and even dangerous side effects if TI is attributed to CD without first completing a detailed history and workup that might reveal excessive NSAID intake.18 In reviewing the data collected in this study, most of the patients diagnosed with TI via biopsy were treated with antibiotics even if the etiology of the TI was undetermined based on the pathology report. Antibiotics are often an appropriate treatment for TI, but this is not always going to be the correct therapy and having an automatic response like this again poses risks for patients.2 Compared to immune modulating therapy, antibiotics for TI are very safe, but treating patients unnecessarily with antibiotics again places them at risk for harmful side effects. This practice also increases the risk for development of antibiotic resistance. Detailed inquiry regarding a patient’s NSAID intake can potentially elucidate a cause for TI and eliminate the need for antibiotics and the subsequent side effects.
In analyzing the data from the TI patients who were subsequently diagnosed with CD, there were two statistically significant associations noted. Patients with CD were found to have an increased incidence of a positive C. difficile infection and were also found to be statistically more likely to be started on biologic therapy than other etiologies (p<0.001). The fact that CD patients were statistically more likely to be on biologic therapy makes logical sense and is encouraging. This suggests that physicians are less likely to start a patient on a treatment regimen with more serious potential side effects without a definitive diagnosis of CD. Starting a patient with an unknown etiology of TI on biologic therapy is not an advisable clinical decision given the high association of NSAID overuse and TI as demonstrated in this study.
The significant association between CD diagnosis and C. difficile is an interesting association that was not anticipated prior to this study. This suggests that clinicians should be vigilant in testing newly diagnosed CD patients for this infection in order to promptly initiate appropriate therapy. A CD patient with co-occurring C. difficile infection presents problems to a physician because there are now two sources of potential diarrhea and treating one will not resolve the other. By testing CD patients for the infection immediately, the workup and treatment of these patients will become more manageable.
This study does pose a few limitations. The first is the small sample size in this study. Only 226 patients met the requirement of being diagnosed with TI in the past 5 years at this university hospital. It would be preferable to be able to examine more charts and patient records in order to better understand the incidence of the various TI etiologies. This is especially true since several of the etiologies, like Meckel’s Diverticulum, are very rare and therefore more skewed by the smaller sample size. This is also a single center-based study and this is yet another limitation. Being able to review charts from patients at different institutions would similarly be preferable to see if there are institutional differences, not only in TI etiologies, but also how the initial TI diagnosis is worked up and treated. While the data regarding the specific nature of the terminal ileitis, in terms of histopathological description, was collected, this information was not used in the analysis. This is mainly because the pathology descriptions that were noted were not specific enough to analyze or attempt to determine links between certain etiologies. In the future, attempting to correlate specific histopathologic descriptions of TI with certain etiologies could be very helpful. In this study, many of the TI patients were not found to have a clear etiology for their diagnosis and by studying pathological findings in more detail in the future, it may be possible to eventually improve the diagnosis of the etiology of TI in a given patient. Being a retrospective chart based study, the limitations arising from not having adequate documentation in some aspects prevent from further analysis as well.
Overall, the most pertinent findings from this study relate to the incidence of CD and NSAID related injury in the TI patients examined. The concern is that CD is either being overdiagnosed or seen as a presumed diagnosis in patients with TI. This can result in unneeded and potentially harmful therapy. Of the 226 charts examined, fewer than 50% of the TI patients had CD and a substantial portion were found to have TI due to excess NSAID intake. Taking care to perform a detailed history including over the counter medication usage following a TI diagnosis is vital in order to initiate an adequate workup and prescribe an appropriate therapy.
6. Conclusions
Terminal ileitis is commonly associated with CD and is often one of the presenting endoscopic patterns when diagnosed. As it is known to present in such a manner it can sway one towards the diagnosis of CD when other possible etiologies may be the actual cause of inflammation of the terminal ileum. Hence careful consideration on the part of the endoscopist to keep other differentials in mind as TI can occur with a multitude of conditions including self-limiting conditions such as certain infections or from offenders such as medications. Being aware of other contributing conditions and proceeding with further diagnosis and management is imperative to not over diagnosing CD incorrectly and not mistreating it inadvertently with potentially harmful medications.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on
Preprints.org.
References
- Kedia S, Kurrey L, Pratap Mouli V, et al. Frequency, natural course and clinical significance of symptomatic terminal ileitis. J Dig Dis. 2016;17(1):36-43. [CrossRef]
- Bojic D, Markovic S. Terminal ileitis is not always Crohn’s disease. Annals of Gastroenterology : Quarterly Publication of the Hellenic Society of Gastroenterology. 2011;24(4):271. Accessed February 6, 2023. /pmc/articles/PMC3959324/.
- Jeong SH, Lee KJ, Kim YB, Kwon HC, Sin SJ, Chung JY. Diagnostic value of terminal ileum intubation during colonoscopy. J Gastroenterol Hepatol. 2008;23(1):51-55. [CrossRef]
- Püspök A, Kiener HP, Oberhuber G. Clinical, endoscopic, and histologic spectrum of nonsteroidal anti-inflammatory drug-induced lesions in the colon. Dis Colon Rectum. 2000;43(5):685-691. [CrossRef]
- Dilauro S, Crum-Cianflone NF. Ileitis: when it is not Crohn’s disease. Curr Gastroenterol Rep. 2010;12(4):249-258. [CrossRef]
- Kinoshita Y, Ishimura N, Oshima N, et al. Recent Progress in the Research of Eosinophilic Esophagitis and Gastroenteritis. Digestion. 2016;93(1):7-12. [CrossRef]
- Goulart R de A, Barbalho SM, Gasparini RG, Carvalho A de CA de. Facing Terminal Ileitis: Going Beyond Crohn’s Disease. Gastroenterology Res. 2016;9(1):1. [CrossRef]
- Matsushita T, Maruyama R, Ishikawa N, et al. The number and distribution of eosinophils in the adult human gastrointestinal tract: a study and comparison of racial and environmental factors. Am J Surg Pathol. 2015;39(4):521-527. [CrossRef]
- Caldwell JM, Collins MH, Stucke EM, et al. Histologic eosinophilic gastritis is a systemic disorder associated with blood and extragastric eosinophilia, TH2 immunity, and a unique gastric transcriptome. J Allergy Clin Immunol. 2014;134(5):1114-1124. [CrossRef]
- Kinoshita Y, Furuta K, Ishimaura N, et al. Clinical characteristics of Japanese patients with eosinophilic esophagitis and eosinophilic gastroenteritis. J Gastroenterol. 2013;48(3):333-339. J Gastroenterol. [CrossRef]
- Kedia S, Das P, Madhusudhan KS, et al. Differentiating Crohn’s disease from intestinal tuberculosis. World J Gastroenterol. 2019;25(4):418-432. [CrossRef]
- Bandi M, Scagliarini L, Anania G, Pedriali M, Resta G. Focus on the diagnostic problems of primary adenocarcinoma of the third and fourth portion of the duodenum. Case report. G Chir. 2015;36(4):183-186. [CrossRef]
- Tangkittikasem N, Boonyaarunnate T, Aswakul P, Kachintorn U, Prachayakul V. Clinical, Radiologic, and Endoscopic Manifestations of Small Bowel Malignancies: a First Report from Thailand. Asian Pac J Cancer Prev. 2015;16(18):8613-8618. [CrossRef]
- Islam RS, Leighton JA, Pasha SF. Evaluation and management of small-bowel tumors in the era of deep enteroscopy. Gastrointest Endosc. 2014;79(5):732-740. [CrossRef]
- Kim DH, Cheon JH. Intestinal Behçet’s Disease: A True Inflammatory Bowel Disease or Merely an Intestinal Complication of Systemic Vasculitis? Yonsei Med J. 2016;57(1):22-32. [CrossRef]
- James DG. Behcet’s syndrome. N Engl J Med. 1979;301(8):431-432. [CrossRef]
- Kim DH, Chan HC hey, Lung PFC, Ng SC, Cheon JH. Ileocolonoscopy in Crohn’s Disease. Atlas of Inflammatory Bowel Diseases. Published online 2015:31-51. [CrossRef]
- Vieth M. [NSAID-colonopathy]. Pathologe. 2006;27(1):65-72. [CrossRef]
- Musumba C, Pritchard DM, Pirmohamed M. Review article: cellular and molecular mechanisms of NSAID-induced peptic ulcers. Aliment Pharmacol Ther. 2009;30(6):517-531. [CrossRef]
- Huang ES, Strate LL, Ho WW, Lee SS, Chan AT. Long-term use of aspirin and the risk of gastrointestinal bleeding. Am J Med. 2011;124(5):426-433. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).