Understanding institutional living
There is little dignity in institutional life. Residents with dementia live behind locked doors and wander sanitized corridors to the distant sound of televisions furnishing minimalist common spaces, void of personal touches and designed for easy maintenance. Yet, although nearly all Canadians over 65 polled in 2021 (97%) reported not wanting to reside in long-term care (LTC) facilities (NIA, 2021), little has been done to challenge the institutional model of dementia/elder care, even if reforms and cultural trends have had some success in improving elements of the nursing home experience (e.g., Maison des aînés in Quebec, Sherbrooke Community Centre in Saskatchewan). Still today, LTC facilities offer little to endow residents’ lives with meaning (Gleeson et al., 2019; Weiner & Ronch, 2003). As residents are merely considered objects of costly medical and domestic care tainted by the stigma of sickness and death (Hummel & Tettamanti, 2009). Even following media coverage of high death rates in LTCs during COVID-19’s first and second waves (Carette, 2021; Fisman et al., 2020), politicians still support the institutional model as Canada’s default option for dementia care. Consequential to this preference, physical safety trumps all other concerns, leading substitute decisionmakers (whether family members or medical professionals) to prematurely committing people with dementia to locked LTC units (Ferreira et al., 2015). Family caregivers and substitute decisionmakers often resign themselves to the seeming absence of other viable options. For people with dementia, the disadvantages and dangers of institutions are many. They may:
receive only physical care (with quality depending on staffing levels) when neither emotional nor social care are government funded (Bannerjee & Armstrong, 2015);
contract easily transmitted infections, such as COVID-19 and influenza;
lack privacy (Tufford, et al., 2017);
lose liberty, autonomy and dignity (Heggestad et al., 2013; Lai, 2022; Šaňákova & Ĉáp, 2019);
wear incontinence products instead of being helped to the toilet, resulting in frequent urinary-tract infections (Salsbury Lyons, 2010);
very likely be depressed (Crick, 2019);
be inappropriately controlled with physical and chemical restraints (e.g., antipsychotic drugs) (Koncul, et al., 2023; Lai, 2022; Steele & Swaffer, 2022);
endure physical and psychological abuse (Lai, 2022; Steele & Swaffer, 2022);
deteriorate mentally and physically (Steele & Swaffer, 2022);
likely develop dental problems, leading to malnutrition, weight loss, and frailty (Slaughter, et al., 2017; Yoon et al., 2018); and
suffer from lockdowns during disease outbreaks (e.g., COVID-19, influenza) when family and friends are banned, preventing them from receiving support and improved care under their loved ones’ monitoring (Koncul, et al., 2023).
Yet, if Canadians condemn the state of LTC (Lloyd et al., 2014), why do our governments keep funding and building institutions? Compared with other OECD countries, Canada drastically underfunds home care for seniors (Drummond et al., 2020). Canada’s spending on geriatric institutions, as a percentage of GDP, is over five times higher than its spending on home care (Drummond et al., 2020). In 2020-2021, compared with 11% of total provincial healthcare spending going to LTC, only half that (5%) went to home and community care (HCC). Across provinces, HCC spending, as a percentage of 2020-2021 continuing-care budgets varied widely. For example, Newfoundland-Labrador spent the most (42%), in comparison to Ontario (40%), British Columbia (39%), and Quebec with the least (22%). This yields a provincial average of $300/person on HCC in 2020-2021 (Busby, 2022). Underfunding is compounded by government spending generally flowing to institutional beds or programs, not individual elders, aggravating the mismatch between elder service demand and supply.
The federal government recently announced voluntary standards for improving LTC. Given that, in Canada’s largest province, Ontario, LTC regulations are rarely enforced (Flood et al., 2021), how will more standards improve care? With current seniors’ demographic growth, LTC-expansion plans will do little more than replace decommissioned beds (Drummond et al., 2020). Canadian governments should look far beyond regulating and expanding LTC, instead, replacing the institutional-elder-care model with community-based alternatives. To initiate this trend, we must first understand what drives elders’ institutionalization. For a start, systemic ageism (discrimination based on age) clouds much of Canada’s social policies and practices regarding end-of-life services and caregiver supports. Healthcare-quality decline with age is well reported (Nemiroff, 2022). Elders encounter paternalistic physician attitudes (Dahlke et al., 2021); higher rates of under- and overtreatment (Mistry, 2021); barriers to timely, effective care (Nemiroff, 2022); and, in the face of functional decline, a deficit in alternatives to barren, segregated institutions (Herron, Kelly & Aubrecht, 2021). As a driver of institutionalization, systemic ageism is bolstered by systemic ableism (discrimination based on ability). People with dementia are discredited as active participants in society and, more crucially, as agents in their own lives (Milne, 2010). Through confinement to LTC, people with dementia suffer epistemic and humanitarian injustices. Indeed, within institutions, management of residents with dementia contradicts the United Nations Convention on Rights of Persons with Disabilities (UNCRDP), a treaty that Canada signed. As Steele and colleagues (2020) point out, “care homes commonly employ a wide range of physical and environmental barriers to movement, including locked doors, lap sashes and belts, bed rails, and segregated wards” (p. 9). These physical constraints compound the widespread use of drugs to control residents with dementia, clearly violating their rights to non-discrimination and equality as disabled people (Minkowitz, 2006).
Ableism also drives exclusionary practices even among institutional residents. Those without dementia avoid interacting with residents with dementia, fearing them as examples of ageing’s “physiological failure” (First author, 2022). Institutions’ segregation of residents with dementia reinforces societal discrimination against people living with the condition. At every turn, they are denied participation possibilities, let alone feeling they belong. Because LTC facilities are concurrently work, medical, and living environments, residents have limited opportunities for meaningful involvement. With hierarchies akin to hospitals, LTCs deprive residents of citizenship and demote them to low care-planning priority (First author, 2022). They are seen as objects, not subjects, of their care.
In view of the above, the need for LTC alternatives is not only undeniable, but an urgent human-rights remedy (Steele et al., 2020) and taxpayer-cost saver. Individuals contemplating old age unanimously wish to avoid institutions (First author, 2022). Yet, professionals and families lack tools and knowledge to find other care avenues. Professionals tasked with coordinating care through the lenses of social justice and social change (e.g. social workers) resent this lack (Thériault & Dupuis-Blanchard, 2017). To address this need, our aims in this article are to:
give readers a roadmap for considering all relevant care options;
broaden the options professionals can recommend to elders and their families beyond institutions;
provide tools that empower people with dementia through supported decision-making, rather than the substitute decision-making that currently dominates the institutional landscape; and
discuss both current and potential alternatives to institutional living.
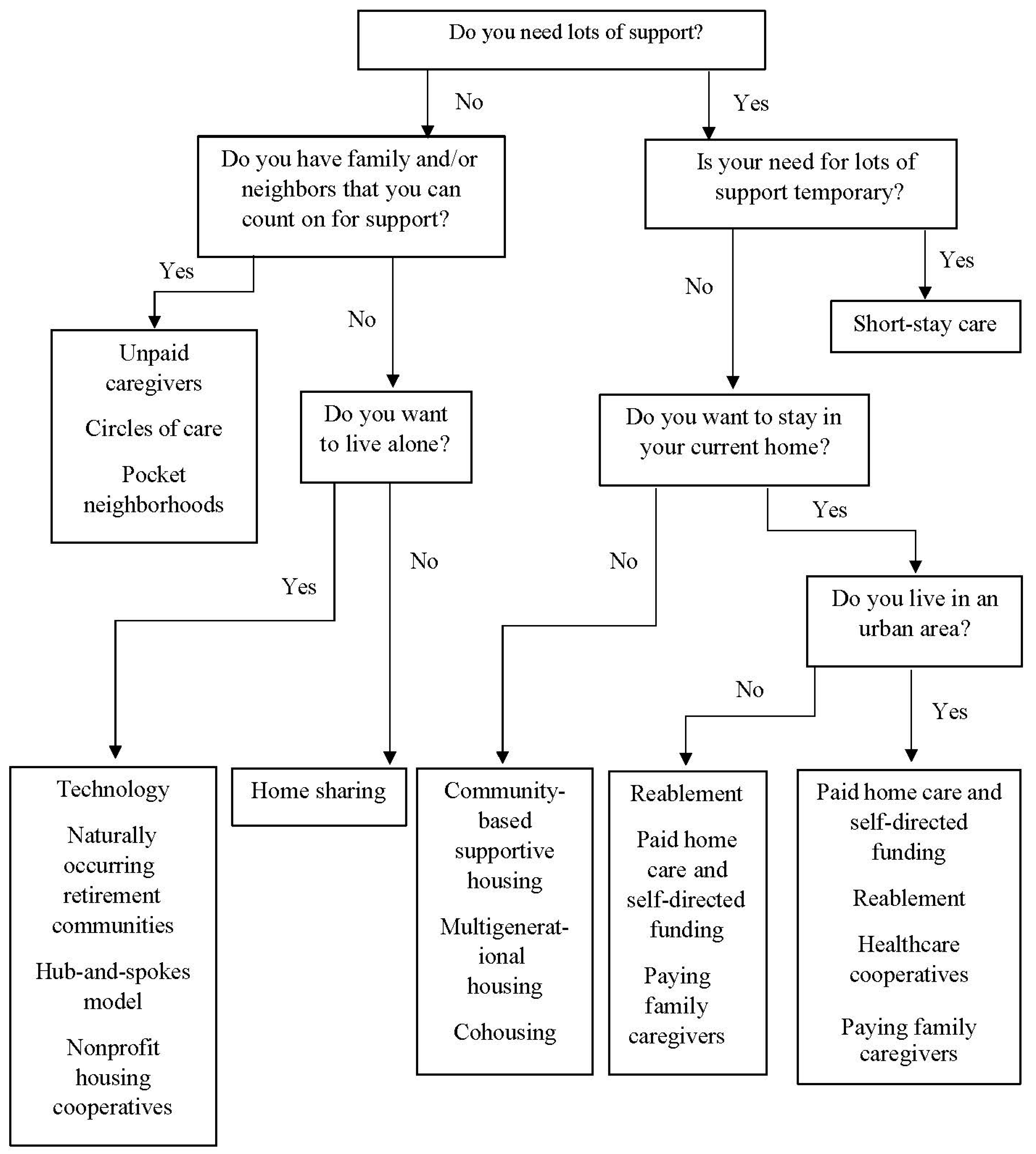
First, we provide a nonexhaustive roadmap (see
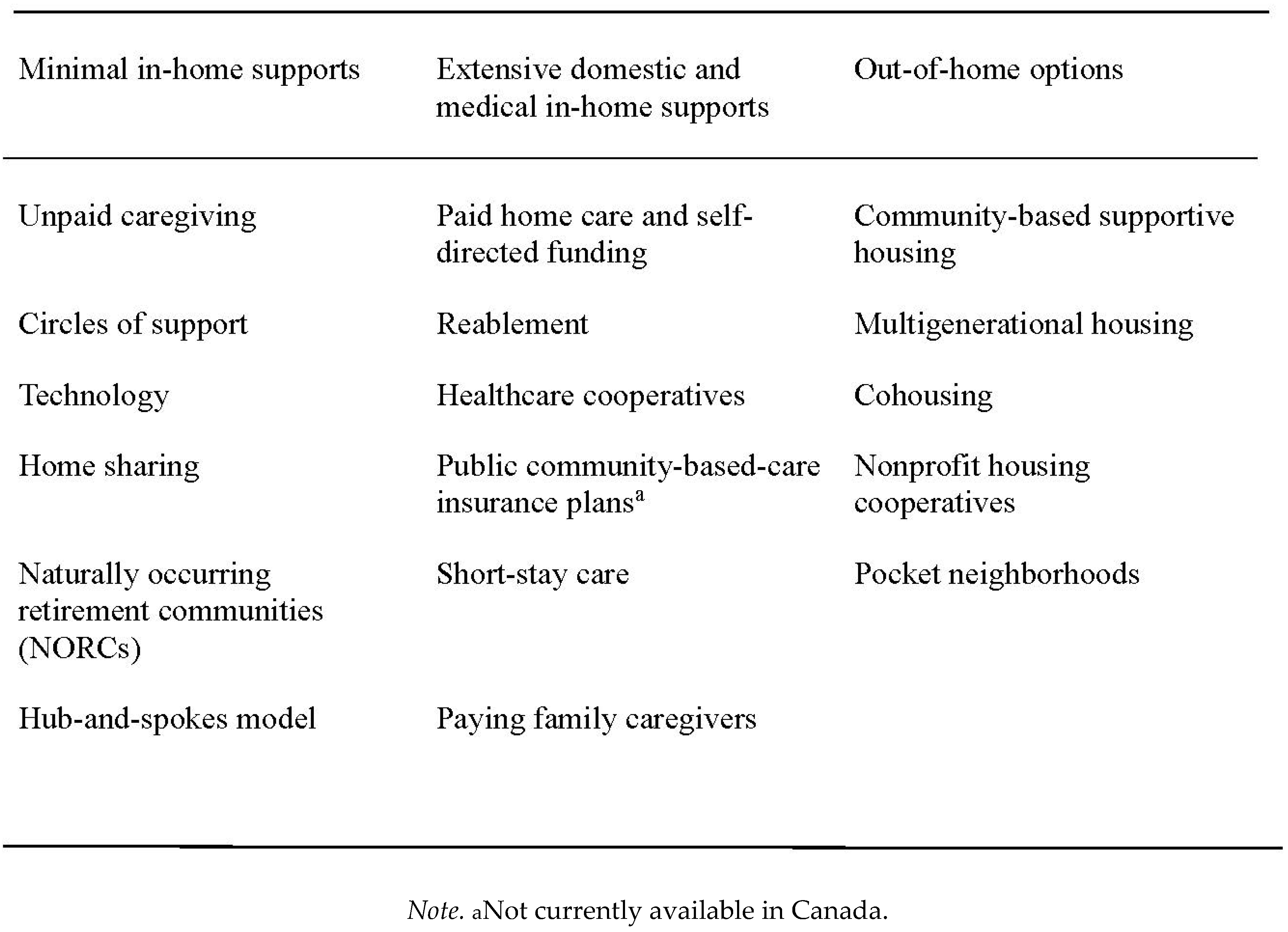
Figure 1) professionals can use to guide decision-making by clients with dementia and their families. We then describe options for supporting people with dementia within their own communities (see
Table 1). All these options should be discussed jointly and based on the person with dementia’s preferences, care needs, social and financial resources.
Our roadmap’s foundation is supported decision-making (SuDM). This approach recognizes the human right of disabled people to participate in decisions about their lives, with support if needed, under the UN Convention on the Rights of Persons with Disabilities (Alzheimer Europe, 2017; UN, 2006). Under SuDM, changed capacity need not disqualify someone from participating in their care planning. Instead, creative accommodations can adapt decision-making to individuals’ current abilities (e.g., supporters listening to nonverbal cues like facial and other bodily expressions). Thus, even as dementia progresses, people with dementia can still be heard. SuDM contrasts with substitute decision-making (SDM), whereby elders appoint people “to make decisions on behalf of another” (LCO, 2023, p. 1), concerning, for instance, their health and property. Although integral to conventional advanced-care planning, substitute decision-makers poorly predict elders’ preferences (Peterson et al., 2020).
In Canada, younger people with cognitive impairments (developmental disabilities) advocated SuDM as an alternative to guardianship as far back as the 1980s. The 1992 Report of the National Task Force on Alternatives to Guardianship (Panitch, 2008) advocated SuDM as well. It is law in at least six American states and in Peru, Columbia, and Mexico (personal communication, Russell Chloe, Canadian Sociology Association Conference, May 30, 2023). The United Kingdom’s Choice and Control policy also incorporates SuDM (Williams & Porter, 2015). SuDM involves listening to the preferences and self-identified needs of people with dementia, including those expressed nonverbally, using for example strategies for obtaining informed consent from research participants with dementia, such as using pictures to explain abstract concepts, involving trusted people (e.g., family and staff) who have listened to their wishes; building relationships well before discussing decisions; allowing time for decision-making and multiple discussions; and looking for verbal and nonverbal signs of anxiety and other signs of disagreement (Oldfield, 2021). To these strategies Lai (2023) adds providing information in accessible formats and using assistive devices to facilitate communication. She advocates that help for carers in supporting elders’ decision-making by, for example, providing information on challenging legal-incapacity decisions by physicians or courts. We suggest that carers also receive peer or other support in challenging medical power.
Non-Institutional Options for Supporting People with Dementia
We now describe noninstitutional options currently available in Canada, along with those in other countries. We group the options into (a) minimal in-home supports, (b) extensive domestic and medical in-home supports, and (c) out-of-home supports.
Minimal In-Home Supports
In planning service trajectories for people with dementia, professionals should attempt to minimize drastic transformations to peoples’ day-to-day lives. Dementia’s evolution varies widely (Melis et al., 2019), leaving many people able to live at home with supports. Although dementia eventually causes ability losses, diagnosis does not mean immediate need for substantial support or institutionalization. Initially, much support to not need to disrupt people’s lives.
Unpaid caregiving. Unpaid caregivers prevent, or significantly delay, institutionalization. They provide physical and emotional support to parents, friends, or neighbors. They may also organize and monitor paid caregiving. Unpaid caregivers, therefore, save governments substantially in health-care costs. Being essential, they are usually included in care plans to fill paid-service gaps (Carette, 2021; First author, 2022). However, unpaid caregiving can require a lot from the women who mostly do it. Middle-aged family caregivers juggle caring for parents and children living at home (Parry et al., 2023). To accommodate caregiving, they may switch to part-time employment or leave their jobs, leading to increased dependence on their partners, reduced family income, more stress, and worsening mental and physical health (Mar, 2020). These negative impacts are largely tied to insufficient government compensation and workplace accommodation, and to the structural ageism and ableism that shape insufficient elder supports (First author, 2022). However, care can be reciprocal and thereby mitigate negative impacts. Elders may emotionally care for their children/friends/neighbors who provide or organize physical care. In turn, caring for elders provides meaning, life satisfaction, and closeness (Quinn & Toms, 2019).
Nonetheless, the benefits of unpaid caregiving do not diminish the harms of deficient eldercare systems. Professionals should advise unpaid caregivers to monitor their physical and mental health and suggest services that can prevent caregiver burnout (e.g., home care, adult day programs, respite care, tax credits or employment insurance benefits1). Some of these options are covered below. In sum, when unpaid caregiving is coupled with appropriate supports and guidance, not only is caregiver burnout reduced but risk of institutionalization drops.
Circles of support. Circles of support bring together groups of friends or community members who weave a personal safety net around a disabled person, who is empowered through supported decision-making (microboardsontario.com). The concept was pioneered by Judith Snow, a disabled Canadian at the forefront of the independent-living movement in the 1970s (Davis, 2005).
Overall, circles of support can enable people with intellectual disabilities to live well (Araten-Bergman & Bigby, 2022). In Ontario, circles of support can incorporate as nonprofit organizations called microboards to gain legal recognition, access and manage services. Unlike a healthcare proxy or power of attorney, “a Microboard is not guardianship or a vehicle for substitute decision-making. A Microboard has no control or legal authority over a person's life” (Microboards Ontario, 2022).
In contrast, Quebec has formalized the importance of groups of allies for people under a protection mandate. As of November 1, 2022, they must be consulted in homologating (legally implementing) a protection mandate (Curateur public du Québec, 2022). While groups of allies do not necessarily function as Microboard in Ontario or British Columbia do, protection mandates represent growing societal awareness of the importance of community in supporting people who need financial and/or healthcare proxies.
Technology. Protective technology can allow people with dementia to remain at home without compromising safety or limiting community engagement. Wearable alerts that trigger a service operator to summon help are a growing industry. Although the alerts’ functions vary according to brand and price, they generally use global-positioning-system and/or fall-detection technology that does not require input from the wearer. Devices can be waterproof, link to other smart devices and encapsulated in pendants or bracelets, depending on the person’s preferences. Even the cheapest device provides medication reminders, two-way voice communication, and monitoring through cellphones and landlines.
Simpler technology, such as people with dementia carrying cards with their names, addresses, and emergency-contact information in wallets, purses or pockets, or wearing pendants or bracelets with identifying information, can facilitate a return home if lost. Carrying this information can reassure people who want to be out in the community, and their family members. Similarly, medic-alert bracelets tell emergency personnel about a person’s medical conditions, allergies, etc. without the person needing to be articulate or conscious.
Home sharing. Home-sharing programs match elders who have unused bedrooms in their homes (e.g., after children leave) with housemates looking for low-cost accommodations. Elders may trade free or low rent for housework or home maintenance. Other benefits for both parties include companionship, security, and mutual caring. As an example, some programs based at universities and colleges match students with elder homeowners (Benzie et al., 2020), who become proxy grandparents for homesick students.
Although home sharing can postpone institutionalization while fostering intergenerational bonds (Bodkin & Saxena, 2017), there are some drawbacks. First, home sharing may not meet elders’ complex or intensive needs, as housemates are more tenants than carers (Poulin, 2022). However, by mutual agreement, the housemate may organize and monitor paid caregivers. Second, people matched by home-sharing programs may turn out to be incompatible. This can create more distress than benefits, particularly in small homes that lack privacy (Bodkin & Saxena, 2017). Nonetheless, some programs safeguard against this outcome through a thorough acquaintance process. Third, municipal zoning may prohibit sharing one’s home with unrelated people. Hence, potential home sharers should seek advice about relevant bylaws before proceeding. Nonetheless, when done well, home sharing cultivates mutually beneficial relationships and fosters stronger community.
Naturally occurring retirement communities (NORCs). Beyond individual homes, naturally occurring retirement communities (NORCs) are apartment buildings where at least half the residents are elders. NORCs may be buildings that, while not intended as such when built, now house an elder majority or communities exclusively for older adults that are neither retirement homes nor LTC facilities (National Institute on Ageing, 2022). Using government or other funding, residents may partner with senior-serving agencies to provide in-home supports at reduced or no cost (Benzie et al., 2020), thereby enabling elders to continue living, and die, at home.
The potential of NORCs is clear in two examples from New York City. Tenants are provided with personal care, nursing assistance, social and educational activities, housecleaning, and transportation (Cohen-Mansfield et al., 2010; Paying for Senior Care, 2023). Services are coordinated by social workers during home visits, along with non-profit organizations allied to each NORC. Although NORCs are not considered suitable where constant surveillance is needed, people with early-to-mid-stage /dementia can participate for years (Freedman et al., 2022).
In Canada, the Ontario Ministry of Health and Long-Term Care funds NORCs in several City-of-Toronto-owned seniors’ buildings.2 Services are provided by personal support workers (PSWs), coordinated by registered practical nurses (RPNs). Eligible tenants receive the following services: personal care, navigating the healthcare system, light housekeeping and laundry, medication reminders, safety checks, light meal preparation, health promotion activities and education, and referral to community resources. In addition, the NORC Innovation Centre (norcinnovationcentre.ca) helps Toronto seniors set up NORCs in their buildings. Outside of Toronto, OASIS (oasis-aging-in-place.com) is working with privately-owned-apartment-building residents and owners in 11 Ontario cities and Vancouver to create NORCs. Despite these efforts, NORCs are an under mobilized resource:
Although more older adults in Ontario live in NORCs than long-term care and retirement homes combined, their potential remains unrealized because little is known about how to successfully create, implement and sustain supportive service programs in NORCs. (Women’s College Hospital, 2023, p. 1)
Not only have NORCs gained legal recognition and standardized funding (Cohen-Mansfield et al., 2010), they answer elders’ preference to age at home. By integrating care and redistributing funds from institutions to community services, municipal and provincial governments save money while significantly improving elders’ quality of life (Béland et al., 2006).
Hub-and-spokes model. A variant on NORCs is the hub-and-spokes service-delivery model. Unlike NORCs, this model extends from but is not restricted to individual apartment buildings. Health and social services are based in hubs—buildings housing mostly elders (SSAO, October 2022). From hubs, supports are provided to elders in the surrounding community, the spokes (SSAO, November. 28, 2022).
This service-delivery model has multiple benefits: it (a) serves elders in various housing arrangements (e.g., houses, multigenerational homes, apartment buildings with few seniors), (b) reduces costs by not requiring new infrastructure to expand clientele, (c) delivers services to communities of elders, not individuals. The latter service-delivery model is significantly more resource intensive and complex than the hub-and-spokes approach.
In Ontario, the Peel [municipal] Housing Corporation (PHC) partnered with Peel Senior Link, a community agency, to create a hub-and-spokes network in its buildings. The hub provided 399 elders with complex care needs and multiple chronic conditions, including dementia, with personal support, food, transportation, and homemaking. Eligible tenants were supported 24/7 and received up to 8 hours of care a day. This initiative diverted 116 emergency-room visits and prevented placement of 121 elders in LTC facilities (SSAO, June 8, 2021). The hub staff also served seniors within three to five kilometres of the PHC-owned buildings. Employee turnover was lower than within LTC facilities, with a greater proportion of full-time staff (SSAO, June 8, 2021).
Although alluring, the Ontario Government funded the Peel example only once (SSAO, June 8, 2021), a surprising choice since providing supporting elders in community-based housing reduces emergency-room visits, need for Alternative Level of Care (ALC) hospital beds, and institutional placements (SSAO, Oct. 2022; Valluru et al., 2019). For example, compared to the cost of Ontario ALC beds ($842-$949/day/patient), paid home care costs only $45/day/person, far less than LTC beds ($142/day) (Drummond, 2020). It is hence crucial not only to raise professionals’ awareness of such options but to encourage professionals to lobby governments to fund their expansion.
Extensive Domestic and Medical In-Home Supports
Eventually, people with dementia will likely need more extensive daily support. However, this situation need not condemn them to abandoning their homes and communities. There are still in-home options that address most needs of people with dementia.
Community-based geriatric assessment. Planning for more extensive in-home supports should start with a community-based rather than a hospital-based geriatric assessment. Canadians with dementia are in fact 6 times likelier to be institutionalized if the initial assessment is done in hospital (CIHI, 2022) and disproportionately less likely to be referred to community services (Livingston et al., 2020). Hospital administrators, under pressure to control costs, in turn pressure case managers to quickly discharge patients no longer needing acute care. Many with dementia are automatically referred to LTC without consideration of in-home services (Aaltonen et al., 2021), even though these patients could return home if the necessary community services were available (Forbes et al., 2008). Instead, to answer administrative pressures, discharge planners who know little about these patients or their communities apply the same intervention framework ad nauseum. Aware that community-services waiting lists are long, they ask families to choose LTC homes from a list, often unaware of all options available and lacking time to research them (SSAO, April 21, 2021).
To facilitate elder patients’ return home from hospital, patients and their families need integrated continuing-care plans that address worries about daily needs. Hence, planning could start with community-based geriatric assessment, in coordination with the patients’ family physicians, who know their situation well.
In Ontario, Brock Community Health Centre offers a geriatric assessment program to which seniors can refer themselves or be referred by family or healthcare providers. The Centre’s program comprises comprehensive in-clinic and in-home needs evaluation. Relevant community services are then coordinated by an interdisciplinary team along with elders’ primary-care providers (CELHIN, 2023). This approach not only facilitates in-home services, it promotes elders’ freedom of choice and ties into their existing caregiver network. We wholeheartedly advocate for this approach to become the rule rather than the exception.
Paid home care and self-directed funding. Home care may be the most important route to preventing people with dementia’s institutionalization (Zabalegui et al., 2014). It is far cheaper to initiate and operate than institutions (Drummond et al., 2020). Canadians, however, lack access to community services, given their underfunding and scarcity compared to socioeconomically similar countries (MacAdam, 2011). Because of this disadvantage, the proportion of Canadians over 65 remaining at home is far lower than that of Switzerland, Germany, Norway, Denmark, New Zealand, and the Netherlands (Drummond et al., 2020).
An American pilot project in Connecticut exemplifies a paradigm shift in funding, where 156 unpaid caregivers were funded to return their family members from LTC into their communities. Under Medicaid’s Money Follows the Person (MFP) program, the project significantly increased caregiver satisfaction and strengthened community partnerships (Kristof et al., 2016). Furthermore, the MFP program directly funds seniors (SSAO, February 23, 2021). They and their family members choose where to spend the money: on institutions, home care or other non-institutional alternatives, whichever best suits their needs and values.
In Canada a model for elder self-directed funding already exists. Younger people with physical (but not mental or psychiatric) disabilities can receive provincial funds to hire and manage personal attendants (Kelly, 2016). Wheelchair users lobbied for this funding as part of Canada’s independent-living movement, beginning in the 1980s (Cranford, 2020). In Ontario at least, funding recipients can hire attendants themselves or through an agency (Cranford, 2020). However, Ontario limits self-directed funding to those under 65. If this limit disappeared, as it has in Saskatchewan (Government of Saskatchewan, 2023), self-directed funding could include seniors with dementia. However, the Saskatchewan Government expects seniors to manage their attendants as employees, as it expects younger recipients to do, limiting the program’s usefulness for people with dementia (personal communication, Katherine Ottley, Canadian Association on Gerontology conference, October 26, 2023).
Reablement. Rehabilitation involves using physical, occupational, and speech-therapy techniques to remedy impairments. In contrast, reablement (restorative care) focuses on increasing independence. Practitioners focus on building strength and confidence in abilities, promoting self-care, regaining skills, preventing hospital readmission, and, crucially, postponing institutionalization (Rostgaard, Parsons, & Tuntland, 2023; SSAO, November 21, 2022). Reablement is also particularly useful to dispel the assumption that people with dementia will only decline (First author, 2022). Poulos and colleagues (2017) argue:
The message for policy makers, practitioners, families, and persons with dementia needs to be “living well with dementia,” with a focus on maintaining function for as long as possible, regaining lost function when there is the potential to do so, and adapting to lost function that cannot be regained. (p. 450)
Given the immense stigma surrounding dementia and degeneration, finding reliable, affordable reablement for people with dementia is challenging. Most dementia-oriented services ignore prospects for improving independence, considering people with dementia a homogenous and near-hopeless population (Keyes et al., 2016). Yet reablement holds significant promise, having been shown to reduce healthcare and support use, thus lower costs (Aspinal et al., 2016). Encouraging elders to regain some independence is more fruitful than helping unpaid caregivers cope with their distress at watching elders struggle (Poulos et al., 2017).
Healthcare cooperatives. With government-funded elder home care being insufficient, community-initiated alternatives have emerged. Healthcare cooperatives are one example. One type, worker cooperatives, are owned by personal support workers. A second type of healthcare cooperative is owned by its consumers, a group of elders or families who want better home care. Each member contributes a certain amount per month to jointly hire a personal-support worker (SSAO, December 5, 2022). With illness prevention and client responsibility as central tenets (Craddock & Vayid, 2004), healthcare cooperatives’ services range from supporting activities of daily living to intensive medical assistance, thus narrowing the significant gap in community-based geriatric services (Craddock & Vayid, 2004).
Although Canadian healthcare cooperatives started in Saskatchewan in 1962, they are not yet the go-to option for aging in place (Craddock & Vayid, 2004). Nevertheless, their number appears to be growing nationally. Quebec has integrated healthcare cooperatives into its social economy as a relief valve for government-funded home-care services. The former are regarded more favorably than for-profit agencies, known to cut corners on services or underpay workers to maximize their profit (Craddock & Vayid, 2004). Although healthcare-cooperative services are not usually free, fees are kept reasonable with supplemental government funding.
Public community-based-care insurance plans. National long-term-care insurance plans have been implemented in Japan, Germany, France, the Netherlands, and South Korea, among others. They cover not only institutional care but home and nursing care. Japan’s plan, an international model of best practice, emphasizes community-based supports while facilitating familial caregiving (Tlumacki, 2020).
Long-term-care-insurance plans can be financed by employer and employee contributions, income taxes, and pension deductions. These plans borrow from the self-directed-funding model, with one exception: they are federal, not provincial. Thus they implement national policy standards, equalizing resources across the country. This option is not yet available to Canadians. Canada’s overspending on institutional geriatric care and underspending on home care, compared to other OECD countries (Drummond, 2020), supports calls for abandoning this funding imbalance and switching to publicly funded insurance plans. When Réjean Hébert was Quebec’s Minister of Health, he proposed such a plan. Although the project was not implemented, its design covered all “legal, administrative, funding, training and contractual” (Hébert, 2016, p. 45) conditions required for its application and thus could have become a model for Canada. We advocate such an initiative, as public community-based-care-insurance plans show great promise for allowing elders to choose where and how to receive care.
Short-stay care. Short-stay care allows family caregivers who live with disabled adults to take breaks or vacations while care recipients occupy bedrooms in group homes, supported apartments, or LTC facilities (CLT, 2022). Short-stay care can also provide regular respite when caregivers feel burned out, have limited resources at home, or need more community support. Crucially, short-stay care can, together with other interventions, significantly reduce negative caregiving experiences and delay the institutionalization of people with dementia (Etters et al., 2008).
More broadly, respite care frees up ALC beds (Drummond et al., 2020), allowing hospitals to admit more patients from emergency departments (Affleck et al., 2013). Although family caregivers have been hesitant to request short-stay care and thus relinquish their caregiving to strangers (Strang & Haughey, 1998), respite care can allow elders to try out institutions without the trauma of forced transitions, accompanied by the stripping of civic freedoms (First author, 2022). Although we advocate community-based-care options, respite care can help elders make more informed choices about institutional care before agreeing to move, should they prefer that option. Conversely, short-stay care can facilitate hospital-to-home transition, while elders recover, and in-home services are arranged.
Ottawa has a guest house for people with dementia, a seniors-village bungalow containing 12 private rooms with private baths, common living room, kitchen, dining area, and secure courtyard. The bungalow is dementia safe (e.g., all hallways lead to common rooms, soft floors). Fees are low, and guests can participate in a day program and household tasks (Cleary, 2020).
Paying family caregivers. When elders need extensive healthcare and/or domestic services, unpaid caregiving may become nearly impossible to juggle with full-time employment. Raising children, being poor, living far from the elder, and lacking community support makes unpaid caregiving impossible. The impossibility may threaten the person with dementia’s safety and well-being. Accessing paid leave from employers and/or being paid to give care are two ways to solve this problem. Either way, family caregivers can better support their family members, instead of grieving their placement in institutions when no other options were available.
Some federal programs pay family caregivers.3 However, these programs are insufficient and/or incomplete. From employment insurance, caregivers may receive 55% of their earnings (up to $650 a week) for 15 weeks under the family-caregiver-for-adults benefit, or for 26 weeks under the compassionate-care benefit (Government of Canada, 2023a). Only family caregivers of critically ill or near-death individuals are eligible however, ignoring care needs before death approaches. This is especially true for family members of people with dementia who die of other causes.
Canada also offers a caregiver tax credit, where citizens can claim either $2,350 or $7,525, depending on their relationship to the cared-for person (Government of Canada, 2023b). If that person pays taxes, they can also reduce them through the disability tax credit (Carl, 2023). Although a step in the right direction, these tax credits are nonrefundable and therefore irrelevant to most low-income Canadians who pay little to no income tax (First author, 2022).
Nova Scotia and Newfoundland and Labrador are the only provinces that fund family caregivers directly. The latter’s Paid Family Caregiver Program funds 4-5 hours of personal assistance/day/eligible person, with additional funding for homemaking and respite care (SSAO, February 25, 2021). Nova Scotia pays caregivers only $400 a month, which renders its policy largely ineffective (Carl, 2023). Notably, most provinces offer some form of funding for home adaptations to bolster independence and respite care. Although these programs cut some costs, they hardly replace employed caregivers’ full-time salaries. Most Canadians are hence forced to delegate family-member care to publicly funded strangers.
Out-of-Home Supports
When all options that enable the person with dementia to remain at home have been exhausted, if the person does not want to live alone, or if unpaid caregiving is no sufficient, it is time to look for community-based housing that provides more supports.
Community-based supportive housing. Our rationale for replacing LTC facilities with community-based alternatives echoes a movement from the 1960s to the 2000s called ‘deinstitutionalization’ that challenged the institutional model of care for younger disabled people (Kelly, 2016). An alternative, community-based supportive housing (CBSH) was built for people with developmental, psychiatric, and other disabilities while institutions closed—although not in all provinces/territories.
As currently with LTC, calls to improve institutions preceded calls to replace them, but deinstitutionalization advocates quickly recognized that institutions were ineffective and dehumanizing (Panitch, 2008). The movement ultimately enabled younger disabled people to live in CBSH or their own homes with supports (Cranford, 2020). Similar 20th-century movements closed other institutions, such as orphanages and Indigenous residential schools. Deinstitutionalization-history lessons apply to creating sustainable LTC alternatives.
CBSH for people with developmental disabilities is generally owned and run by non-profit organizations. The first CBSH developed was group homes. Unlike LTC facilities, group homes are not modelled on hospitals (Second author, 2019) but on family homes. These existing houses, renovated perhaps with added ramps and bathrooms, visually integrate into neighborhoods. Group homes house from 4-10 residents with 24-hour staff support. Most bedrooms are private, with some shared with one other person, and decorated to residents’ tastes with their own belongings. Welcome to visit, family and friends do not have to sign in or wear badges as in institutions. Staff and residents may cook meals together, do laundry, and clean. Staff accompany residents on outings of residents’ choosing, to medical appointments, help with personal care, and provide emotional support. More recently, supported-apartment living was developed, where several people share an apartment and staff rotate among apartments.
CBSH is purposefully located in neighborhoods housing people of varying age, close to schools, day cares, shopping, and community centres. This housing thus does not segregate people in large buildings because of their age and disability. Since CBSH is small, it can operate less bureaucratically than institutions. Institutional time4 does not predominate, with more time for relational care (Second author, 2019), and it is easier for residents to engage with surrounding communities. Staff can prioritize residents’ wishes through routines that follow their rhythms; in other words, residents time (Second author, 2019). CBSH is an indispensable shift toward better quality of life and civic engagement for older adults with disabilities, including dementia, while also being cheaper to operate than LTC (Robison et al., 2011).
In their systematic review, Pywell et al. (2023) found that small-scale homelike elder-care settings (SSHS) consistently improved outcomes, compared with institutional settings. SSHS had better care quality, functional-decline rates, social stimulation, emotional wellbeing, quality of life, and lower restraint use than institutional settings. Some outcomes lowered healthcare (e.g., fewer hospital admissions). Residents reported more freedom, privacy, and stronger relationships. Staff seemed more comfortable encouraging independence and felt more motivated to stay, lowering turnover. Pywell et al. (2023) concluded that SSHS achieves superior results across many areas without inflating costs. Crucially, CBSH is safer, both physically and psychologically. During the Covid-19 pandemic, elders in LTC were 13 times more likely to die than their community-dwelling peers (Fisman et al., 2020). Under a social model of care, CBSH staff are expected to focus on building residents’ existing strengths, while encouraging choice and independence (SSAO, March 31, 2021). Although in Canada, the CBSH model has been applied on a small scale to serve elders, including those with dementia, it has been applied more widely in the United States, Sweden, Germany, and Japan (SSAO, March 31, 2021). CBSH is a very good option for elders who do not want to live alone or with family, or who do not have unpaid caregivers such as adult children to offer necessary supports.
Multigenerational housing. When elders with dementia have immediate family to rely on, multigenerational housing can provide safety while they not only remain in the community but also close to their families. Homes can be expanded into multigenerational dwellings in multiple ways. The first is accessory dwellings (also called granny flats and laneway homes). These are small, self-contained houses constructed in the backyards of family homes or replacing garages. Homeowners can build them for their parents or, when the homeowners are elderly, they can build and occupy the accessory dwellings while their children and grandchildren occupy the main house. When grandparents no longer need the accessory dwellings, they can be rented out for income. Second, homeowners with smaller lots can construct accessory units inside their houses (e.g., in-law suites in basement or home extensions). Both parties have separate spaces with reliable supports nearby when needed; for example, childcare for parents, domestic and other support for grandparents, and companionship for all.
Third, suburban developers are constructing large multigenerational houses to serve immigrant families, in which elderly parents customarily live with their children in a family model of care. These new houses incorporate parents’ suites that, later, can be offered to extended family members or rented out for income. Hence, even if a multigenerational house is purchased to serve family members’ needs, it remains a potentially revenue-generating investment.
Although increasingly common across Canada, retrofitting houses into multigenerational homes may face systemic barriers. Zoning bylaws meant to exclude multifamily housing may only allow single-family dwellings, with accessory buildings without a construction permit limited to a maximum 100 sq. ft. Permits may require separate electrical hookups to the power grid for accessory dwellings, increasing their costs. However, many cities have changed planning regulations and zoning to allow these accessory dwellings (Benzie et al., 2020). Not only do they benefit elders who wish to live with their families, for cities wanting to increase density, these dwellings do so without visibly changing neighborhoods and generating backlash from the surrounding homeowners.
Cohousing. Co-housing is a type of communal living in which single houses, apartments or townhouse clusters are designed to facilitate activities among residents by, for example, sharing dining rooms and gardens. Individual units can be owned privately or by an organization and rented out. Buyers or renters agree to support each other socially and instrumentally and may also share operation, maintenance and pool resources (e.g., through bulk purchasing). This cost minimization and the collective approach are advantages of cohousing.
There are two potential drawbacks to cohousing: (a) conflicts may affect the community’s operation and volunteer-task allocation (Benzie et al., 2020) and (b) because cohousing often requires residents to buy their units or contribute to a house purchase, it may not be affordable for low-income seniors (Poulin, 2022).
Another form of cohousing is where middle-aged people and/or elders purchase a home together. They care for each other and, when they no longer can, jointly hire personal service workers (PSWs) and homemakers. Notably, these are not informal communities. Prospective buyers must draw up and sign legal contracts regarding how they will jointly own the house, operate it, and share expenses. According to communal agreements, this form of cohousing can be managed by family or friends to accommodate physical and cognitive impairments that arise with ageing (Lord, March 8, 2022). Overall, seniors’ cohousing focuses on social and health-related support, with either accessible designs or budget allocations to retrofit units for accessibility that reduce the need for institutional care (Poulin, 2022).
Nonprofit housing cooperatives. These are apartment buildings or townhouse clusters collectively owned by all resident members. Member volunteers democratically run each cooperative through boards of directors and committees, and large cooperatives often have paid staff to manage and maintain property. Rents remain affordable since they only increase with the cooperative’s budget, which members must approve collectively; there is no profit (Harahan et al., 2006). Wheelchair-accessible units in some cooperatives house members who may receive attendant care. Elder members may receive home care.
Because housing cooperatives are more secure and affordable than private-market housing, members may stay for decades, their cooperatives becoming de facto NORCs. To facilitate aging in place, members can use co-operative funds to retrofit units, apply for grants as non-profit organizations, and neighbors may become unpaid caregivers (Harahan et al., 2006). Given cooperatives’ collective structure, services arranged by individual members can be coordinated to improve service-delivery efficiency. Coordination can improve flexibility for care recipients, along with working conditions and job security for workers (Cranford, 2020).
Pocket neighborhoods. These are small car-free neighborhoods comprising 6 to12 dwellings clustered around an open area. Entrances face other, fostering interaction among neighbors. The dwellings may include bedrooms for caregivers (Benzie et al., 2020). Pocket neighborhoods can minimize isolation, a strong predictor of declining health in old age (Freedman & Nicolle, 2020). However, there is little research on how well pocket neighborhoods serve elders with high or rapidly changing care needs (Benzie et al., 2020). At least, when elders with dementia live in small neighborhoods well connected with community services, they are less likely to “fall between the cracks” when their needs surpass available services. For seniors whose dementia progresses slowly, is well managed and/or are frequently visited by unpaid caregivers, pocket neighborhoods are an excellent option for maintaining meaningful community engagement.
Conclusion
The institutional model of dementia care—locked wards in long-term-care facilities—is not only rife with problems but unanimously repudiated as a last resort and unimaginable end of life (First author, 2022). Segregating disabled people, including those with dementia, in institutions is against the United Nations Convention on Rights of Persons with Disabilities, a treaty that Canada signed. Yet Canada’s dementia care remains clouded by systemic ageism and ableism, with institutions as the default option irrespective of elders’ overwhelming preference for ageing in place. Decades of deinstitutionalization enabled younger disabled people to live in the community with supports. Do elders with dementia and other chronic conditions not deserve the same?
In this article, we contribute to dementia-care literature in multiple ways. We describe a plethora of more humane alternatives to institutional dementia care that exist, or could exist, in Canada. We present a roadmap for professionals to consider all relevant care options when helping clients with dementia and their families plan service trajectories that keep clients out of institutions. Our roadmap incorporates supported decision-making, an underapplied approach in dementia care that empowers people to preserve their agency, rather than the substitute decision-making that currently dominates the institutional landscape. As such, both our alternatives-to-institutions descriptions and roadmap contribute to the growing practice of advanced care planning.
Given the strong evidence in support of community-based alternatives for dementia care presented above, we argue that politicians’ continued funding of institutions and reluctance to fund non-institutional alternatives—which are cheaper, safer and have higher rates of satisfaction (Estabrooks et al., 2020)—is inexcusable. We hope that this article will be useful to professionals, their associations, and dementia advocates in lobbying governments to reallocate our tax dollars to expand existing community-centered options and create new ones. We also hope that this article contributes to a paradigm shift in how Canada serves its citizens with dementia. As we have shown throughout, this paradigm shift is possible. Spreading the word about non-institutional alternatives can pressure politicians to change their actions and even create alternatives at the community level.
Endnotes
1. Pay rates are unknown.
3. Although federal benefits are standard across Canada, other benefits vary between provinces and territories and should be researched by professionals familiar with the province/territory.
4. As Second Author (2019) explains, institutional time is the dominant force structuring daily life for LTC staff and residents. Residents’ time is how residents would prefer to structure their daily lives.
Author Contributions
Conceptualization, Margaret Oldfield and Maude Lévesque; methodology, Margaret Oldfield; software, N/A; validation, Margaret Oldfield and Maude Lévesque; formal analysis, Margaret Oldfield; investigation, Margaret Oldfield and Maude Lévesque; resources, N/A; data curation, Margaret Oldfield and Maude Lévesque; writing—original draft preparation, Maude Lévesque; writing—review and editing, Margaret Oldfield; visualization, N/A; supervision, N/A; project administration, N/A; funding acquisition, N/A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Acknowledgments
We thank peer reviewers for their suggestions to improve our article, along with Poland Lai and Katherine Ottley, whose critical feedback improved the draft manuscript. Margaret Oldfield is grateful to advocates of living well with dementia, including people with the condition, for inspiring the guide that preceded this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Aaltonen, M., El Adam, S., Martin-Matthews, A., Sakamoto, M., Strumpf, E., & McGrail, K. (2021). Dementia and poor continuity of primary care delay hospital discharge in older adults: A population-based study from 2001 to 2016. Journal of the American Medical Directors Association, 22(7), 1484-1492. 1492. [CrossRef]
- Araten-Bergman, T., & Bigby, C. (2022). Forming and supporting circles of support for people with intellectual disabilities – A comparative case analysis. Journal of Intellectual & Developmental Disability, 47(2), 177-189. [CrossRef]
- Banerjee, Albert & Armstrong, Pat (2015, Spring). Centring care: Explaining regulatory tensions in residential care for older persons. Studies in Political Economy, 95, 7-28. [CrossRef]
- Béland, F., Bergman, H., Lebel, P., Clarfield, M., Tousignant, P., Contandriopoulos, A.-P., & Dallaire, L. (2006). A system of integrated care for older persons with disabilities in Canada: Results from a randomized controlled trial. The Journals of Gerontology, 61(4), 367-373. [CrossRef]
- Bodkin, H., & Saxena, P. (2017). Exploring home sharing for elders. Journal of Housing for the Elderly, 31(1), 47-56. [CrossRef]
- Carette, J. (2021). Manquer de respect. Les Cahiers de Lectures de l’Action nationale, XV(3), 31-32.
- Dahlke, S., Hunter, K. F., Fox, M. T., Davidson, S., Perry, N., Watts, L. T., ... & Moody, E. (2021). Awakening Canadians to ageism: A study protocol. BMC Nursing, 20(1), 1-10. [CrossRef]
- Davis, K. (2005). Creating a circle of support. IRCA Articles, 1-4.
- Drummond, D., Sinclair, D., Bergen, R., and COVID-19 Health Policy Working Group. (2020). Ageing well. Kingston, ON: School of Policy Studies, Queens University.
- Estabrooks, C. A., Straus, S. E., Flood, C. M., Keefe, J., Armstrong, P., Donner, G. J., ... et Wolfson, M. C. (2020). Restoring trust: COVID-19 and the future of long-term care in Canada. FACETS, 5(1), 651-691. [CrossRef]
- Fisman, D. N., Bogoch, I., Lapointe-Shaw, L., McCready, J. & Tuite, A. R. (2020). Risk factors associated with mortality among residents with coronavirus disease 2019 (COVID-19) in long-term care facilities in Ontario, Canada. JAMA Network Open, 3(7), e2015957-e2015957. [CrossRef]
- Forbes, D. A., Markle-Reid, M., Hawranik, P., Peacock, S., Kingston, D., Morgan, D., ... & Jansen, S. L. (2008). Availability and acceptability of Canadian home and community-based services: Perspectives of family caregivers of persons with dementia. Home health care services quarterly, 27(2), 75-99. [CrossRef]
- Freedman, V. A. Freedman, V. A., Bandeen-Roche, K., Cornman, J. C., Spillman, B. C., Kasper, J. D., & Wolff, J. L. (2022). Incident care trajectories for older adults with and without dementia. The Journals of Gerontology: Series B, 77(Supplement_1), S21-S30. [CrossRef]
- Harahan, M. F., Sanders, A., & Stone, R. (2006). Inventory of affordable housing plus services initiatives for low-and modest-income seniors. U. S. Department of Health and Human Services.
- Heggestad, A K. T., Nortvedt, P., & Slettebø, Å. (2013). ‘Like a prison without bars’: Dementia and experiences of dignity. Nursing Ethics, 20(8), 881-892. [CrossRef]
- Kelly, C., Dansereau, L., FitzGerald, M., Lee, Y., & Williams, A. (2023). Inequities in access to directly-funded home care in Canada: A privilege only afforded to some. BMC Health Services Research, 23(1), 1-11. [CrossRef]
- Keyes, S. E., Clarke, C. L., Wilkinson, H., Alexjuk, E. J., Wilcockson, J., Robinson, L., ... & Cattan, M. (2016). “We’re all thrown in the same boat…”: A qualitative analysis of peer support in dementia care. Dementia, 15(4), 560-577. [CrossRef]
- Koncul, A., Kelly, C., Aubrecht, K., & Bartlett, R. (2023). Long-term care homes: Carceral spaces in times of crisis or perpetually? Space and Culture, 1-14. [CrossRef]
- Lai, P. (2022, September). A longer view: Human rights and safeguards for long-term care residents. Windsor Review of Legal and Social Issues, 43, 36-75.
- Lai, P. (2023). Autonomous care decisions: What can Article 12 of the CRPD offer to older disabled adults and their supporters? Disability & Society [online]. [CrossRef]
- Lévesque, M. (2022). Vieillir en centre de soins de longue durée : vue convergente d’un système mis en faute. Unpublished doctoral dissertation, School of Social Work, University of Ottawa. Retrieved from http://hdl.handle.net/10393/44146.
- Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., Brayne, C., Burns, A., Cohen-Mansfield, J., Cooper, C., Costafreda, S. G., Dias, A., Fox, N., Gitlin, L. N., Howard, R., Kales, H. C., Kivimäki, M., Larson, E. B., Ogunniyi, A., Orgeta, V., Ritchie, K., Rockwood, K., Sampson, E. L., Samus, Q., Schneider, L. S., Selbæk, G., Teri, L., & Mukadam, N. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet, 396(10248), 413-446. [CrossRef]
- Lloyd, L., Banerjee, A., Harrington, C., Jacobsen, F. F., & Szebehely, M. (2014). It is a scandal! Comparing the causes and consequences of nursing home media scandals in five countries. International Journal of Sociology and Social Policy, 34(1/2), 2-18. [CrossRef]
- Oldfield, M. (2019). “You have to wait!” Time as an instrument of power in a nursing home [preprint]. https://www.researchgate.net/publication/333811513_You_Have_to_Wait_Time_as_an_Instrument_of_Power_in_a_Nursing_Home.
- Oldfield, M. (2021). “Nothing about us without us”: Involving people with dementia in qualitative research. Review of Disability Studies International, 17(2). https://rdsjournal.org/index.php/journal/article/view/1034.
- Panitch, M. (2008). Disability, mothers, and organization: Accidental activists. New York: Routledge.
- Peterson, A., Karlawish, J., & Largent, E. (2020). Supported decision making with people at the margins of autonomy. The American Journal of Bioethics, 21(11), 4-18. [CrossRef]
- Poulin, L. I. L. (2022). University-integrated seniors village: Environmental scan report. Peterborough: Trent Centre for Aging & Society, Trent University.
- Poulos, C. J., Bayer, A., Beaupre, L., Clare, L., Poulos, R. G., Wang, R. H., ... & McGilton, K. S. (2017). A comprehensive approach to reablement in dementia. Alzheimer's & Dementia: Translational Research & Clinical Interventions, 3(3), 450-458. [CrossRef]
- Robison, J., Shugrue, N., Reed, I., Thompson, N., Smith, P., & Gruman, C. (2011). Community-based versus institutional supportive housing: Perceived quality of care, quality of life, emotional well-being, and social interaction. Journal of Applied Gerontology, 30(3), 275-303. [CrossRef]
- Rostgaard, T., Parsons, J., & Tuntland, H. (Eds.). (2023, January). Reablement in long-term care for older people: International perspectives and future directions. Bristol, UK: Bristol University Press.
- Shakespeare, T., Zeilig, H., & Mittler, P. (2017). Rights in mind: Thinking differently about dementia and disability. Dementia, 18(3), 1-14. [CrossRef]
- Slaughter, S., Ickert, C., Carrier, N., Lengyel, C., & Keller, H. (2017). Identifying priority areas for improving food and fluid intake in long-term care: Multi-professional views. Journal of Nursing Home Research Sciences, 3, 43-45. [CrossRef]
- Steele, L., Carr, R., Swaffer, K., Phillipson, L., & Fleming, R. (2020). Human rights and the confinement of people living with dementia in care homes. Health and Human Rights, 22(1), 7. 22.
- Tufford, F., Lowndes, R., Struthers, J., & Chivers, S. (2017, June 1). ‘Call security’: Locks, risk, privacy and autonomy in long-term residential care. Ageing International [online]. [CrossRef]
- Valluru, G., Yudin, J., Patterson, C. L., Kubisiak, J., Boling, P., Taler, G., ... & Kinosian, B. (2019). Integrated home-and community-based services improve community survival among Independence at Home Medicare beneficiaries without increasing Medicaid costs. Journal of the American Geriatrics Society, 67(7), 1495-1501. [CrossRef]
- Weiner, A. S., & Ronch, J. L. (Eds.). (2003). Culture change in long-term care. New York: Routledge.
- Williams, V. & Porter, S. (2015). The meaning of ‘choice and control’ for people with intellectual disabilities who are planning their social care and support. Journal of Applied Research in Intellectual Disabilities, 30, 11-12. [CrossRef]
- Yoon, M. N., Ickert, C., Slaughter, S. E., Lengyel, C., Carrier, N., & Keller, H. (2018). Oral health status of long-term care residents in Canada: Results of a national cross-sectional study. Gerodontology, 35(4), 359-364. [CrossRef]
- Zabalegui, A., Hamers, J. P., Karlsson, S., Leino-Kilpi, H., Renom-Guiteras, A., Saks, K., ... & Cabrera, E. (2014). Best practices interventions to improve quality of care of people with dementia living at home. Patient Education and Counseling, 95(2), 175-184. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).