1. Introduction
Microvascular free flap reconstructions are key procedures in treating various conditions in pediatric and adolescent patients, including congenital defects, traumatic injuries, malignancies, and issues caused by other medical procedures. These complex surgeries have been well-established in the pediatric population, but there's still a notable lack of detailed research focused on how these procedures affect younger patients [1-4]. The physiological and developmental characteristics of children and adolescents necessitate specialized approaches, distinct from those used in adult patients.
The present study seeks to address this gap by understanding the impact of various factors such as age, sex, etiology of the maxillofacial defect, graft source, and recipient site location on the success of these surgeries. A detailed analysis of 136 pediatric and adolescent patients who underwent maxillofacial microvascular free flap reconstructions was performed to highlight these key variables, providing a foundation for future research. Identifying these factors is critical for enhancing the success rates of these procedures in children and adolescents, thereby improving their post-surgical quality of life
2. Materials and Methods
This is a retrospective chart review from August 2011 to June 2023. Data was collected from Maxillofacial Surgery for Children and Young Adults Division in the Head and Neck Clinic, Regional Specialized Children’s Hospital in Olsztyn, Poland. The study included patients from 1 to 25 years of age. Patients were categorized by recipient site anatomical location, and major complications were recorded.
2.1. Procedures and Techniques
This study initially assessed 206 patients (n=206), of which 136 patients who underwent 136 procedures with complete medical records were eligible for inclusion (n=136). In contrast, 70 patients with incomplete medical records were excluded from the analysis. Thus, a total of 136 procedures were analyzed.
The free flap auto-transplantation procedure began with the resection of pathology, resulting in tissue loss in the recipient site. Next, the flap was harvested from the donor site but remained connected to surrounding tissue by at least one artery and one vein. Simultaneously, the recipient site was surgically dissected to prepare the recipient vein and artery for reattachment with the vascular pedicle of the free flap. Then, the vasculature of the flap was detached, leading to the separation of the free flap from the rest of the tissue, creating a vascular pedicle. The free flap was brought to the defect area and the vessels of the flap were anastomosed with the vessels of the recipient site under the control of a microscope. After reconnection, the free flap was sutured to the defect, while the medical team monitored blood flow in the anastomosed vessels to ensure patency. Meanwhile, the donor site was closed with sutures
2.2. Terms
Definition of terms used in this study are listed in table below.
Table 1.
Terms used in study and their definitions.
Table 1.
Terms used in study and their definitions.
| Term |
Definition |
| |
Etiology of underlying pathology |
| Tumor |
Any malignant or benign mass, which required reconstructive surgical intervention to treat. |
| Congenital defect |
Any harmful condition resulting from either hereditary or environmental factors that is present at birth, which caused loss of function or structural integrity of tissue and required reconstructive surgical intervention to treat. |
| Trauma |
Any injury (such as a wound) to living tissue caused by an extrinsic agent, which required reconstructive surgical intervention to treat. |
| Iatrogenic |
Any harmful condition resulting from medical intervention and required reconstructive surgical intervention to treat. |
| |
Donor flaps |
| Free flap |
A piece of tissue that is disconnected from its original blood supply and is moved a significant distance to be reconnected to a new blood supply. |
| Fibula flap |
A free flap containing bone tissue acquired from fibula. |
| Iliac crest flap |
A free flap containing bone tissue acquired from iliac crest. |
| Medial condyle flap |
A free flap containing bone tissue acquired from medial condyle of femur. |
| Anterolateral thigh flap |
A free flap containing skin, subcutaneous tissue with or without muscles acquired from anterolateral portion of thigh. |
| Forearm flap |
A free flap containing skin, subcutaneous tissue with or without muscles acquired from forearm. |
| Lower limb nerve |
A free flap containing skin, subcutaneous tissue with or without muscles and sural or tibial nerve acquired from the lower limb. |
| |
Recipient site complications |
| Total flap loss |
A state of free flap, when flap necrosis involves 100% of flap volume. |
| Partial flap loss |
A state of free flap, when flap necrosis involved <100% of flap volume. |
| Flap necrosis |
Irreversible cell injury and eventual cell death due to pathological processes of free flap. |
| Flap survival |
A state of free flap, when there is no total flap loss reported. |
| |
Indicators |
| Success rate |
Ratio of number of procedures that resulted in flap survival to number of all procedures shown as a percentage. |
| Complication rate |
Ratio of number of procedures in which complications defined in study (except for TFL) occurred to number of all procedures. |
2.3. Data collection and statistical analysis
Data for this study were extracted from electronic health records. A database was established for analysis. Recorded parameters included gender, age, etiology of the condition, recipient and donor sites, as well as postoperative complications.
The statistical analysis was performed using STATGRAPHICS Centurion 19 (StatPoint, Tulsa, US). The ANOVA test was utilized to determine relations between age and recipient site complications, etiology and total flap loss. The χ² test of independence was applied to assess relationships among categorical variables, including age groups, gender, recipient site complications, donor site, etiology, and the incidence of total flap loss. Age groups were categorized as follows: less than 5 years, 5 to 10 years, 11 to 15 years, 16 to 20 years, and over 20 years. A threshold of p<0.05 was set to determine statistical significance.
3. Results
This study included 136 young patients who underwent microvascular free flap reconstructions, comprising 76 females and 60 males. The median age was 14 years, ranging from 1 to 25 years.
Table 2 categorically delineates demographic and clinical data, illustrating gender distribution, etiology, recipient and donor sites, and recipient site complications. The predominant etiology of the underlying pathology was neoplastic in nature, accounting for 82 out of 136 cases (60.3%), followed by congenital defects in 39 cases (28.7%). The most frequently reconstructed sites were the maxilla (56 out of 136 cases, 41.2%) and mandible (55 out of 136 cases, 40.4%). The fibula (47 out of 136 cases, 34.6%) and iliac crest (44 out of 136 cases, 32.4%) were the most harvested flaps. Out of the 136 procedures performed, 122 resulted in successful free flap survival, while 14 cases experienced total flap loss, yielding an overall success rate of 89.7%. Postoperative complications included total flap necrosis in 14 cases (10.3%), partial flap necrosis in 11 cases (8.1%), abscess formation in 4 cases (2.9%), and nerve palsy in 1 case (0.7%). The distribution of total flap necrosis was 11 in maxillary reconstructions and 3 in mandibular reconstructions. Within the maxillary reconstruction group, the total flap loss was distributed among donor sites as follows: 5 cases from the iliac crest (representing 20.8% of all iliac crest flaps transplanted to the maxilla), 5 from the fibula (35.7% of all fibular flaps to the maxilla), and 1 from the medial condyle of the femur (constituting 7% of all such flaps to the maxilla). Within the mandibular reconstruction group, the total flap loss was distributed among donor sites as follows: 2 cases from the fibula (6,1% of all fibular flaps to the mandible), 1 case from the iliac crest (representing 5% of all such flaps to the mandible).
Table 2.
Demographics.
| |
Frequency |
Percent |
Sex
Female
Male
|
76
60 |
55.9%
44.1% |
Etiology
Congenital
Oncological
Traumatic
Iatrogenic
|
39
82
5
10
|
28.7%
60.3%
3.7%
7.4%
|
Recipient Site
Mandible
Maxilla
Soft tissue
Orbit
Facial nerve |
55
56
17
4
4
|
40.4%
41.2%12.5%
2.9%
2.9%
|
Donor Site
Iliac crest
Medial condyle of Femur
Fibula
Antero-lateral thigh
Forearm
Gracilis muscle
Lower limb nerve |
44
15
47
17
7
4
2
|
32.4%
11.0%
34.6%
12.5%
5.1%
2.9%
1.5%
|
Recipient Site Complications
Nerve palsy
Abscess
Partial flap necrosis
Total flap necrosis
None |
1
4
11
14
106
|
0,7%
2,9%
8,1%
10,3%
78%
|
| Total |
136
|
100%
|
3.1. Patient’s age at the time of surgery and total flap loss.
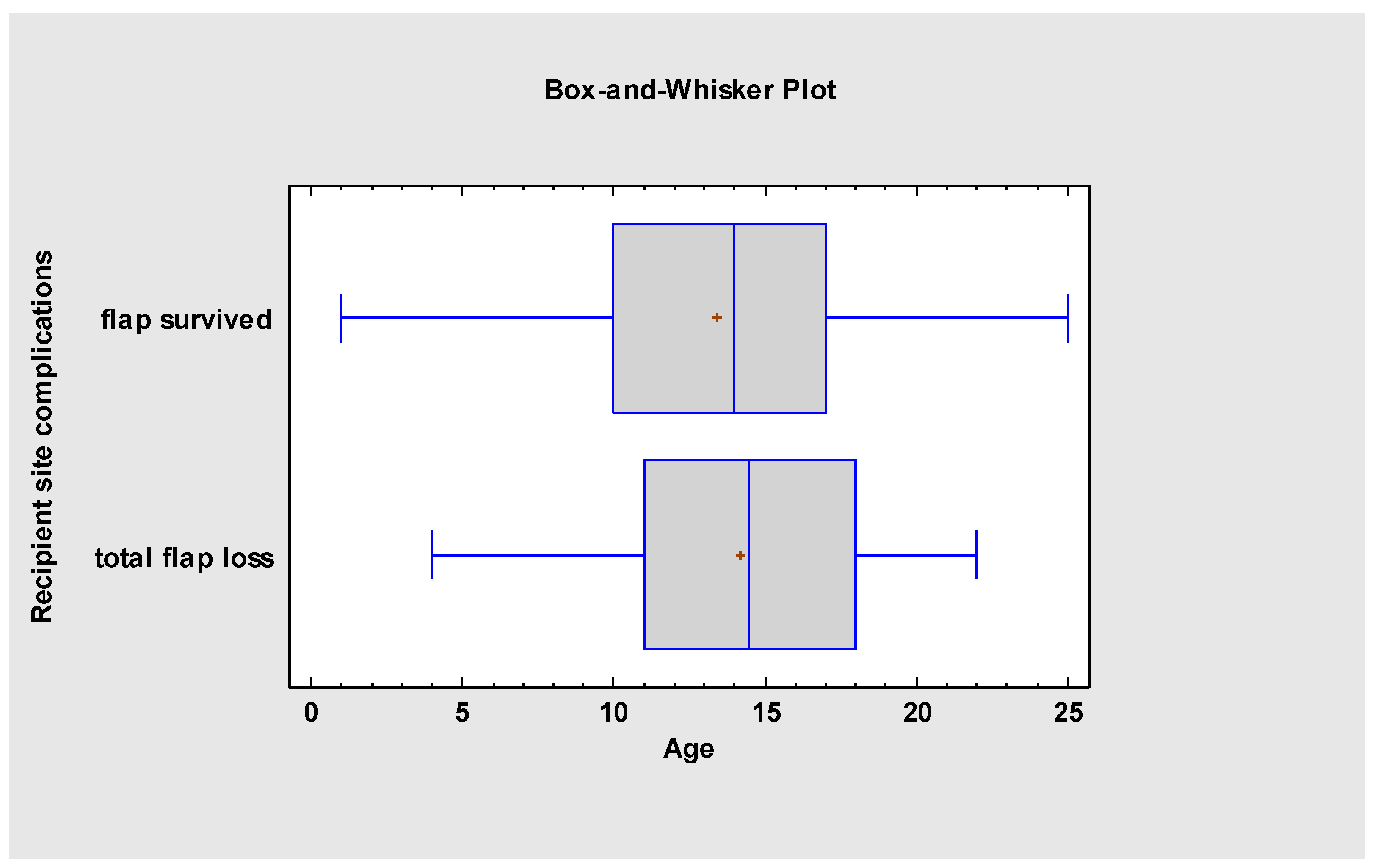
The mean age at the time of microsurgical reconstruction was 13.5 (± 4.98), with a median of 14 years. For patients who had a successful procedure, the mean age was 13.4 (± 5.0), with a median of 14 years. In contrast, the mean age for those with flap failure was 14.2 (± 4.95), with a median of 14.5 years. Statistical analysis indicated no significant age difference between the patients with flap survival and those with flap loss (F = 0.33, p = 0.57).
Figure 1.
There is no age-dependent relation of total flap loss.
Figure 1.
There is no age-dependent relation of total flap loss.
Table 3.
Summary statistics of patient's age by flap survival or total flap loss.
Table 3.
Summary statistics of patient's age by flap survival or total flap loss.
| |
Count
|
Average
|
Median
|
Standard deviation
|
Minimum
|
Maximum
|
| Flap survived |
122
|
13.4
|
14.0
|
5.0
|
1.0
|
25.0
|
| Total Flap Loss |
14
|
14.2
|
14.5
|
4.95
|
4.0
|
22.0
|
| Total |
136
|
13.5
|
14.0
|
4.98
|
1.0
|
25.0
|
3.2. Gender, etiology of the underlying pathology and the occurrence of total flap loss.
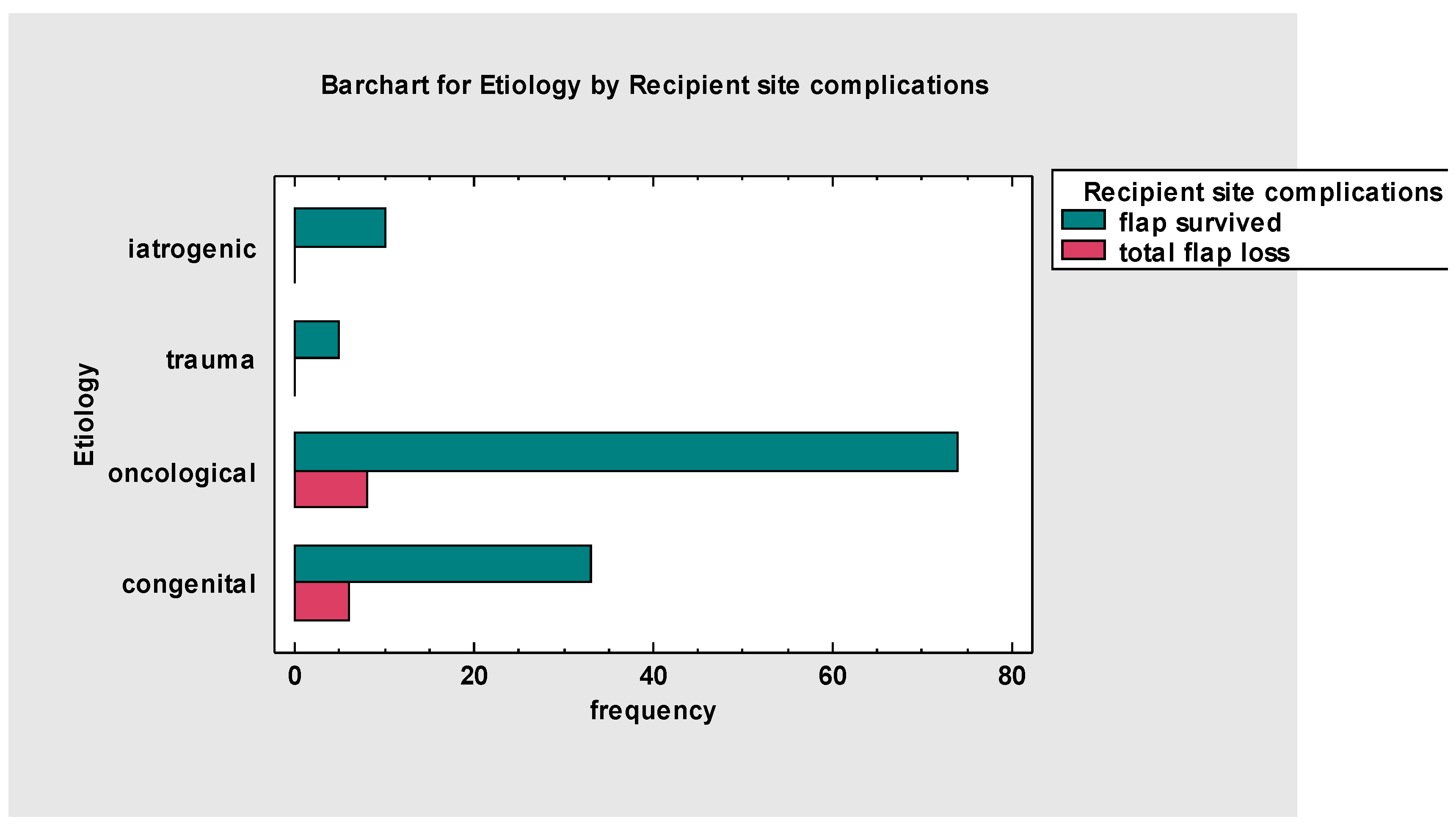
In evaluating the impact of etiology on the incidence of total flap loss and flap survival the oncological group demonstrated a total flap loss in 8 cases, which constituted 5.88% of all 136 cases. Congenital etiologies had a lower incidence of total flap loss, with 6 cases representing 4.41% of all reconstructions performed. Both trauma and iatrogenic categories maintained a 100% flap survival rate with no instances of total flap loss. Statistical analysis revealed no significant differences in the incidence of total flap loss across etiology groups [χ² (3, N = 136) = 2,84, p = 0.42].
Figure 2.
Numbers of total flap losses and flap survival by etiology of reconstruction.
Figure 2.
Numbers of total flap losses and flap survival by etiology of reconstruction.
Table 4.
Summary of number of procedures resulted in flap survival or total flap loss with calculated success rate by gender.
Table 4.
Summary of number of procedures resulted in flap survival or total flap loss with calculated success rate by gender.
| Gender |
Number of procedures with flap survival |
Number of procedures with total flap loss |
Total number of procedures |
Success rate |
| Female |
65 |
11 |
76 |
85.5% |
| Male |
57 |
3 |
60 |
95% |
A higher number of flap transfers was observed in female patients compared to male patients (n=76 vs n=60). There was a larger number of procedures that resulted in total flap loss within the female patient group compared to the male patient group (n=11 vs n=3). The calculated success rates were higher for the male group (95%) than for the female group (86%). However, statistical analysis did not reveal any significant differences between the female and male groups in terms of flap survivability [χ² (1, N = 136) = 3.26, p = 0.07].
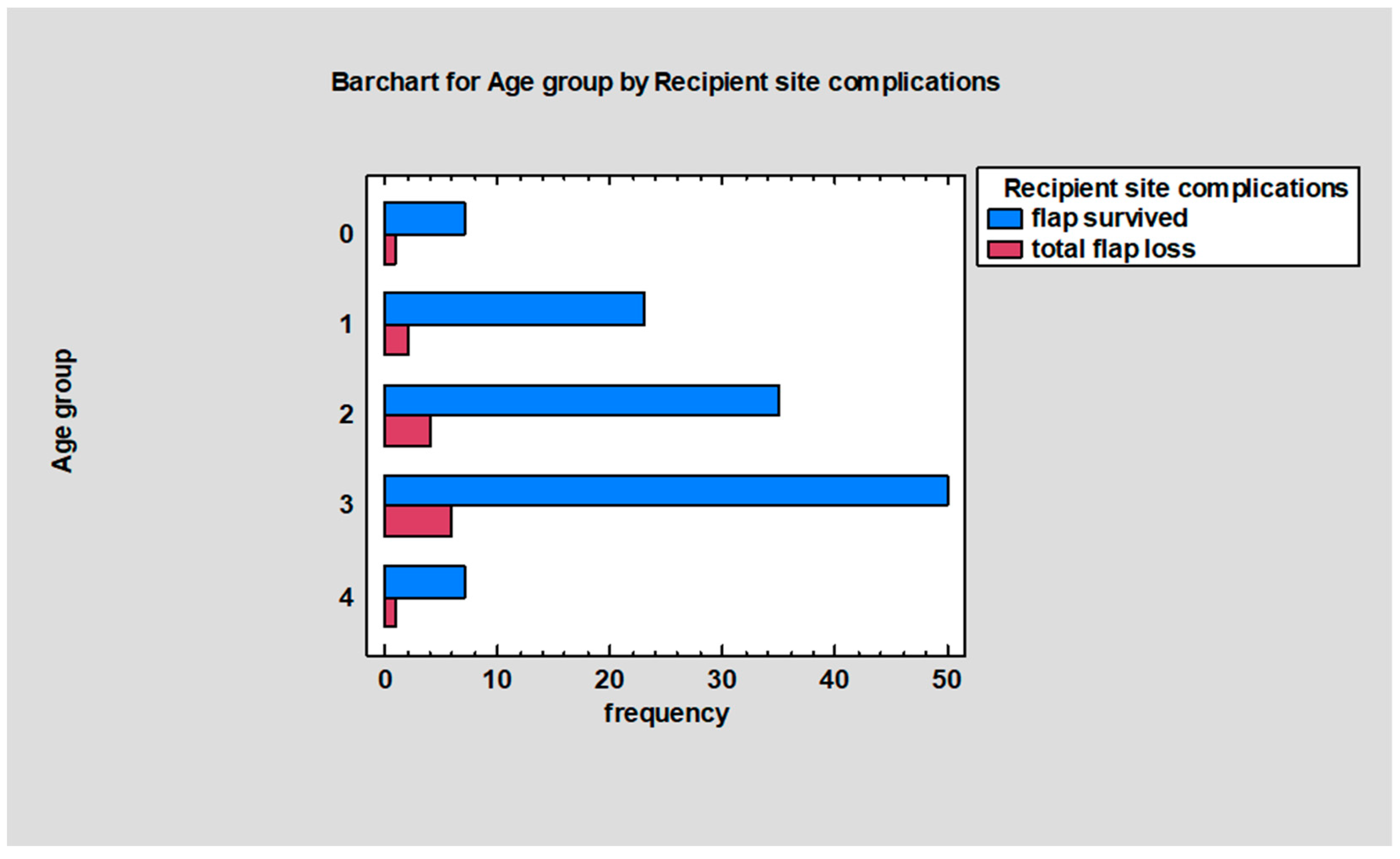
3.3. Occurrence of recipient site complications between age groups and age group specific success rate.
Table 5. provides a summary of recipient site complications categorized by age groups. The 16 to 20-year-old group had the highest incidence of recipient site complications, which also correlated with having the highest number of procedures and the highest number of cases resulting in total flap loss. The fewest complications were noted in patients under 5 years of age, with this group having only one case of total flap loss and no other documented complications. The group aged 6 to 10 years demonstrated the highest success rate at 92%. Statistical analysis revealed no significant differences in the incidence of recipient site complications across age groups [
x2 (16, N = 136) = 7.94, p = 0.95]. Additionally, there was no significant relation between age groups and the number of total flap losses [
x2 (4, N = 136) = 0.24, p = 0.99].
Figure 3.
Number of procedures resulted in flap survival or total flap loss for age groups. Numbers on Y axis are labels of age groups ("0"= less than 5 y.o.; "1"= 6 to 10 y.o.; "2" = 11 to 15 y.o.;"3" = 16 to 20 y.o.; "4" = greater than 20 y.o.).
Figure 3.
Number of procedures resulted in flap survival or total flap loss for age groups. Numbers on Y axis are labels of age groups ("0"= less than 5 y.o.; "1"= 6 to 10 y.o.; "2" = 11 to 15 y.o.;"3" = 16 to 20 y.o.; "4" = greater than 20 y.o.).
3.4. Recipient site, recipient site complication and flap survival.
Table 6 highlights a significant discrepancy in the incidence of total flap loss between the maxilla and mandible groups. The maxilla group, with the highest number of transplants (n=56), also had the highest incidence of total flap loss (n=11), resulting in a success rate of 80.4% for free flap transplants in this group. In contrast, of the 55 free flap transplantations to the mandible, only three resulted in total flap loss, yielding a success rate of 94.6% for mandibular reconstructions. The difference in total flap loss between the two sites was statistically significant (p < 0.05) [χ² (4, N = 136) = 9.56, p = 0.049]. For the maxillary transplants, 24 (42.9%) flaps were harvested from the iliac crest, 14 (25%) from the fibula, 14 (25%) from the medial condyle of the femur, 3 (5.4%) from the anterolateral thigh, and 1 from the forearm. In the 55 mandibular transplants, there were 33 fibula flaps (60%), 20 (36.4%) flaps from the iliac crest and 2 (3.6%) flaps from the medical condyle of femur. In the groups undergoing soft tissue, orbital, and facial nerve microsurgical reconstruction, there were no instances of total flap loss, leading to success rates of 100% in these categories.
Table 7 indicates that the maxilla group experienced the highest number of recipient site complications, followed by the mandible and soft tissue groups. There were no reported complications for free flap transfers to the orbit or facial nerve. Excluding total flap loss, the complication rate for free flap transfers to the maxilla was 10.7%, while transfers to the mandible had a complication rate of 16.4%. The results of the χ² test suggest no significant association between the recipient sites and the occurrence of complications [χ² (4, N = 136) = 7.10, p = 0.13].
4. Discussion
This study conducted an extensive examination of maxillofacial microvascular free flap reconstructions in a pediatric and adolescent cohort, yielding significant insights into the success rates and factors influencing outcomes. The observed success rate of 89.71% in our study, while notable, is somewhat lower compared to the success rates typically reported in existing literature, which often exceed 94% [1-8]. In a study by Liu et al. (2018) focusing on pediatric head and neck reconstruction, a higher success rate of 95.6% was reported. However, it is essential to highlight the differences in the distribution of recipient sites between the two studies. Our research found the maxilla (55 out of 136 cases) and mandible (55 cases) as the most common recipient sites, with maxilla having the highest incidence of total flap loss. Notably, the success rate for mandibular reconstructions in our study was 94.55%, closely aligning with the higher success rates reported in the literature. In contrast, the study by Liu et al. primarily involved mandibular reconstructions (88 out of 135 cases), with only 9 cases of maxillary reconstructions. Despite their conclusion of no significant relation between recipient site and total flap loss, the predominance of mandibular reconstructions in their study, which aligns closely with the higher success rates in our mandibular cases, might partially explain the overall higher success rate observed in their findings.
In our analysis, we specifically examined the relation between patient age and the incidence of total flap loss. It has been observed that children under ten years of age, might be at a heightened risk of lower success rates in these procedures [
1]. The potential underlying factors attributed to this finding include reduced diameter of vasculature in younger patients, arterial vasospasms and heightened complexity in performing surgical techniques on smaller anatomical structures. Regardless of these findings, our data did not demonstrate a significant relation between patient age and the incidence of total flap loss. Interestingly, this result is consistent with another substantial study involving 102 patients, where a similar lack of relation between age and surgical success in microvascular reconstructions was observed [
8]. This parallel outcome in a separate large-scale study reinforces the notion that age, while an important consideration, may not be as critical a determinant of flap survival.
We investigated the potential relation between patient gender and the incidence of total flap loss. Our examination revealed a borderline statistical significance (p=0.071), suggesting a tentative yet not statistically validated trend towards a higher risk of total flap loss in female patients. However, given the marginal nature of this finding, it necessitates further investigation with an expanded pediatric sample size to establish a more definitive conclusion. The literature presents varied perspectives on the influence of gender in head and neck reconstructions. For example, Loupatatzi et al. identified female gender as one of the factors associated with increased complications in head and neck cancer reconstructions, alongside pre-operative radiation therapy and extended surgery duration [
9]. In contrast, Rohleder et al. reported no significant gender-related differences in the postoperative outcomes of free flap reconstructions in the head and neck region [
10]. It is important to note, however, that these studies predominantly involved adult populations, with mean ages notably above the pediatric range, thereby limiting the applicability of their findings to a younger demographic.
A striking finding was the higher incidence of total flap loss in maxillary reconstructions compared to mandibular ones. Specifically, the maxilla experienced 11 cases of total flap necrosis out of 55 reconstructions, translating to a success rate of 80.36%, markedly lower than the 94.55% observed for mandibular reconstructions. This contrast becomes even more pronounced when compared to adult maxillary reconstruction success rates, which typically hover around 95% in the literature [
11,
12]. However, it aligns more closely with recent findings in pediatric patients, such as those reported by Burns et al. (2023), who observed a 23% total flap loss in pediatric maxillary reconstructions [
13].
Noteworthy is the absence of any total flap loss instances in reconstructions involving soft tissues, orbital regions, and facial nerves. The results are consistent with the noted trend that flaps incorporating bone have a nearly fivefold higher failure rate compared to those consisting entirely of soft tissue. This is likely attributable to the fact that in bone defect reconstructions, the positioning of both the flap and its pedicle is dictated by the bony defect, offering limited flexibility for alteration [
14].
5. Conclusions
The aim of our study was to identify key factors influencing the success of maxillofacial microvascular free flap reconstructions in pediatric and adolescent patients. Our findings point towards the importance of the recipient site, particularly the challenges associated with maxillary reconstructions. The lack of significant correlation with age and gender shifts focus to site-specific variables rather than demographic ones. This study, therefore, underscores the need for specialized surgical strategies for maxillary reconstructions in the young population.
Author Contributions
Conceptualization, D.L.; J.M.; R.Maksymowicz., C.S. and K.D.; Data curation, D. L.; J.M.; R.Maksymowicz, C. S. and M. K.; Formal analysis, D. L.; J. M.; R. Maksymowicz., C. S.; R. Marguła, Ł. K.; M. K. and K. D.; Funding acquisition, K. D.; Investigation, D. L.; J. M.; R. Maksymowicz and C. S.; Methodology, D. L.; J. M.; R. Maksymowicz, C. S.; R. Marguła, M. K. and K.D.; Project administration, D.L. and K.D.; Resources, Ł. K.; Software, M. K.; Supervision, Ł. K. and K.D.; Validation, D.L.; J. M.;R. Maksymowicz, C. S.; R. Marguła, Ł. K.; M. K. and K. D.; Visualization, D. L.; R. Maksymowicz and M.K.; Writing – original draft, D. L.; J.M.; R. Maksymowicz, C. S. and R. Marguła; Writing – review & editing, D. L, J. M.; R. Maksymowicz, C. S.; R. Marguła and K. D. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by ChM SP. Z O.O., Poland.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Regional Specialized Children’s Hospital in Olsztyn, (36 ZE//2023/WSSD; 07/12/2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data are available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Liu, S.; Zhang, W.-b. , Yu, Y.; Wang, Y.; Mao, C.; Guo, C.-b., Yu, G.-y., Peng, X. Free Flap Transfer for Pediatric Head and Neck Reconstruction: What Factors Influence Flap Survival? The Laryngoscope 2019;129: 1915-1921.
- Upton, J.; Guo, L. Pediatric Free Tissue Transfer: A 29-Year Experience with 433 Transfers. Plast. Reconstr. Surg. 2008, 121, 1725–1737. [Google Scholar] [CrossRef] [PubMed]
- Bilkay, U.; Tiftikcioglu, Y.O.; Temiz, G.; Ozek, C.; Akin, Y. Free-tissue transfers for reconstruction of oromandibular area in children. Microsurgery 2008, 28, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Markiewicz, M.R.; Ruiz, R.L.; Pirgousis, P.; Bell, R.B.; Dierks, E.J.; Edwards, S.P.; Fernandes, R. Microvascular Free Tissue Transfer for Head and Neck Reconstruction in Children. J. Craniofacial Surg. 2016, 27, 846–856. [Google Scholar] [CrossRef] [PubMed]
- Crosby, M.A.; Martin, J.W.; Robb, G.L.; Chang, D.W. Pediatric mandibular recon- struction using a vascularized fibula flap. Head Neck J. Sci. Spec. 2008, 30, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Warren, S.M.M.; Borud, L.J.M.; Brecht, L.E.D.; Longaker, M.T.M.; Siebert, J.W.M. Microvascular Reconstruction of the Pediatric Mandible. Plast. Reconstr. Surg. 2007, 119, 649–661. [Google Scholar] [CrossRef] [PubMed]
- Wolf, R.; Ringel, B.; Zissman, S.; Shapira, U.; Duek, I.; Muhanna, N.; Horowitz, G.; Zaretski, A.; Yanko, R.; Derowe, A.; et al. Free flap transfers for head and neck and skull base reconstruction in children and adolescents - Early and late outcomes. Int. J. Pediatr. Otorhinolaryngol. 2020, 138, 110299. [Google Scholar] [CrossRef] [PubMed]
- Margaret JS MM, Michael EK, et al. Microsurgical reconstruction following oncologic resection in pediatric patients: a 15-year experience. Ann. Surg. Oncol. 2017, 24, 4009–4016. [Google Scholar] [CrossRef] [PubMed]
- Loupatatzi, A.; Stavrianos, S.D.; Karantonis, F.F.; Machairas, A.; Rapidis, A.D.; Kokkalis, G.; Papadopoulos, O. Are Females Predisposed to Complications in Head and Neck Cancer Free Flap Reconstruction? J. Oral. Maxillofac. Surg. 2014, 72, 178–185. [Google Scholar] [CrossRef] [PubMed]
- Rohleder, N.H.; Heimüller, S.; Wolff, K.D.; Kesting, M.R. Influence of biological sex on intra- and postoperative course of microvascular free flap reconstructive surgery in the head and neck region: A retrospective analysis involving 215 patients. Adv. Oral. Maxillofac. Surg. 2022, 7. [Google Scholar] [CrossRef]
- Costa, H.; Zenha, H.; Sequeira, H.; Coelho, G.; Gomes, N.; Pinto, C.; Martins, J.; Santos, D.; Andresen, C. Microsurgical reconstruction of the maxilla: Algorithm and concepts. J. Plast. Reconstr. Aesthetic Surg. 2015, 68, e89–e104. [Google Scholar] [CrossRef] [PubMed]
- Mücke, T.; Hölzle, F.; Loeffelbein, D.J.; Ljubic, A.; Kesting, M.; Wolff, K.-D.; Mitchell, D.A. Maxillary reconstruction using microvascular free flaps. Oral. Surgery, Oral. Med. Oral. Pathol. Oral. Radiol. Endodontology 2011, 111, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Burns, H.R.; Yim, N.H.; Hashemi, A.S.A.; Upadhyaya, R.M.; Montgomery, A.; Dimachkieh, A.L.; Pederson, W.C.; Buchanan, E.P. Pediatric Maxilla-Mandible Oncoplastic Reconstruction: A 25 Patient Case Series. Face 2023, 4, 495–504. [Google Scholar] [CrossRef]
- Kroll, S.S.; Schusterman, M.A.; Reece, G.P.; Miller, M.J.; Evans, G.R.D.; Robb, G.L.; Baldwin, B.J. Choice of Flap and Incidence of Free Flap Success. Plast. Reconstr. Surg. 1996, 98, 459–463. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).