Submitted:
08 February 2024
Posted:
09 February 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Anaplasmosis
3. Human Monocytotropic Ehrlichiosis
4. Human Babesiosis
5. Conclusions
References
- Family Anaplasmataceae (Anaplasmosis, Ehrlichiosis, Neorickettsiosis, and Neoehrlichiosis) - William L. Nicholson, in Principles and Practice of Pediatric Infectious Diseases (Fifth Edition), 2018. [CrossRef]
- Khatat, S.E.H.; Daminet, S.; Duchateau, L.; Elhachimi, L.; Kachani, M.; Sahibi, H. Epidemiological and Clinicopathological Features of Anaplasma phagocytophilum Infection in Dogs: A Systematic Review. Front. Veter.-Sci. 2021, 8, 686644. [Google Scholar] [CrossRef]
- Matei, I.A.; Estrada-Peña, A.; Cutler, S.J.; Vayssier-Taussat, M.; Castro, L.V.; Potkonjak, A.; Zeller, H.; Mihalca, A.D. A review on the eco-epidemiology and clinical management of human granulocytic anaplasmosis and its agent in Europe. Parasites Vectors 2019, 12, 599. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Cui, F.; Wang, L.; Zhang, L.; Zhang, J.; Wang, S.; Yang, S. Investigation of anaplasmosis in Yiyuan County, Shandong Province, China. Asian Pac. J. Trop. Med. 2011, 4, 568–572. [Google Scholar] [CrossRef]
- Gettings, J.R.; Self, S.C.W.; McMahan, C.S.; Brown, D.A.; Nordone, S.K.; Yabsley, M.J. Local and regional temporal trends (2013–2019) of canine Ehrlichia spp. seroprevalence in the USA. Parasites Vectors 2020, 13, 153. [Google Scholar] [CrossRef]
- Paddock CD, Suchard DP, Grumbach KL, et al. Brief report: fatal seronegative ehrlichiosis in a patient with HIV infection. N Engl J Med 1993;329:1164–1167. [PubMed: 8377780]. [CrossRef]
- Olano JP, Hogrefe W, Seaton B, et al. Clinical manifestations, epidemiology, and laboratory diagnosis of human monocytotropic ehrlichiosis in a commercial laboratory setting. Clin Diagn Lab Immunol 2003;10:891 896. [PubMed: 12965923]. [CrossRef]
- Olano JP, Masters E, Hogrefe W, et al. Human monocytotropic ehrlichiosis, Missouri. Emerg Infect Dis 2003;9:1579–1586. [PubMed: 14720399]. [CrossRef]
- Carpenter CF, Gandhi TK, Kong LK, et al. The incidence of ehrlichial and rickettsial infection in patients with unexplained fever and recent history of tick bite in central North Carolina. J Infect Dis 1999;180:900–903. [PubMed: 10438390]. [CrossRef]
- Chapman AS, Bakken JS, Folk SM, et al. Diagnosis and management of tickborne rickettsial diseases: Rocky Mountain spotted fever, ehrlichioses, and anaplasmosis-United States: a practical guide for physicians and other health-care and public health professionals. MMWR Recomm Rep 2006;55 (RR-4):1–27. [CrossRef]
- Caldwell CW, Everett ED, McDonald G, et al. Lymphocytosis of gamma/delta T cells in human ehrlichiosis. Am J Clin Pathol 1995;103:761–766. [PubMed: 7785663]. [CrossRef]
- Paddock CD, Childs JE. Ehrlichia chaffeensis: a Prototypical Emerging Pathogen. Clin Microbiol Rev 2003;16:37–64. [PubMed: 12525424]. [CrossRef]
- Lin M, den Dulk-Ras A, Hooykaas PJ. Anaplasma phagocytophilum AnkA secreted by the type IV secretion system is tyrosine phosphorylated by Abl-1 to facilitate infection. Cell Microbiol 2007;9:2644–2657. [PubMed: 17587335]. [CrossRef]
- Dumler JS, Barat NC, Barat CE, et al. Human granulocytic anaplasmosis and macrophage activation. Clin Infect Dis 2007; 45:199–204. [PubMed: 17578779]. [CrossRef]
- Bakken JS, Dumler JS. Ehrlichiosis and anaplasmosis. Infect Med 2004; 21:433–51.
- Marty AM, Dumler JS, Imes G, et al. Ehrlichiosis mimicking thrombotic thrombocytopenic purpura. Case report and pathological correlation. Human Pathol 1995; 26:920–025. [PubMed: 7635455]. [CrossRef]
- https://www.cdc.gov/ticks/tickbornediseases/ehrlichiosis.
- https://www.cdc.gov/ticks/tickbornediseases/anaplasmosis.
- Ehrlichioses in Humans: Epidemiology, Clinical Presentation, Diagnosis, and Treatment - J. Stephen Dumler, John E. Madigan, Nicola Pusterla, and Johan S. Bakken. [CrossRef]
- Fichtenbaum CJ, Peterson LR, Weil GJ. Ehrlichiosis presents as a life-threatening illness with features of toxic shock syndrome. Am J Med 1993;95:351–357. [PubMed: 8213865]. [CrossRef]
- Walker DH, Dumler JS. Human monocytic and granulocytic ehrlichioses discovery and diagnosis of emerging tick-borne infections and the critical role of the pathologist. Arch Pathol Lab Med 1997;121:785–791. [PubMed: 9278605].
- Sehdev AE, Dumler JS. Hepatic pathology in human monocytic ehrlichiosis. Ehrlichia chaffeensis infection. Am J Clin Pathol 2003;119:859–865. [PubMed: 12817434]. [CrossRef]
- Peters TR, Edwards KM, Standaert SM. Severe ehrlichiosis in an adolescent taking trimethoprim-sulfamethoxazole. Pediatr Infect Dis J 2000;19:170–2. [PubMed: 10694012]. [CrossRef]
- Brantley, RK. Trimethoprim-sulfamethoxazole and fulminant ehrlichiosis [Letter]. Pediatr Infect Dis J 2001;20:231. [PubMed: 11224854]. [CrossRef]
- Dunning Hotopp JC, Lin M, Madupu R, et al. Comparative genomics of emerging human ehrlichiosis agents. PLoS Genet 2006;2:e21. [PubMed: 16482227]. [CrossRef]
- Bakken JS, Dumler JS. Ehrlichiosis and anaplasmosis. Infect Med 2004;21:433–51.
- Katavolos P, Armstrong PM, Dawson JE, Telford SR III. Duration of tick attachment required for transmission of granulocytic ehrlichiosis. J Infect Dis 1998;177:1422–5. [PubMed: 9593039]. [CrossRef]
- des Vignes F, Piesman J, Heffernan R, et al. Effect of tick removal on transmission of Borrelia burgdorferi and Ehrlichia phagocytophila by Ixodes scapularis nymphs. J Infect Dis 2001;183:773– 8. [PubMed: 11181154]. [CrossRef]
- Needham GR. Evaluation of five popular methods of tick removal. Pediatrics 1985;75:997–1002. [PubMed: 4000801]. [CrossRef]
- Babes, V. “Sur l’hemoglobinurie bacterienne du boeuf.” CR Acad. Sci 107 (1888): 692-694.9.
- Skrabalo, Z.; Deanovic, Z. Piroplasmosis in man; report of a case. Doc. Med. Geogr. Trop. 1957, 9, 11–16 9. [Google Scholar]
- Hildebrandt, A.; Zintl, A.; Montero, E.; Hunfeld, K.-P.; Gray, J. Human Babesiosis in Europe. Pathogens 2021, 10, 1165. [Google Scholar] [CrossRef] [PubMed]
- Bakken JS, Dumler JS. Human granulocytic ehrlichiosis. Clin Infect Dis. 2000; 31:554-560. [CrossRef]
- Horowitz HW, Marks SJ, Weintraub M, et al. Brachial plexopathy associated with human granulocytic ehrlichiosis. Neurology. 1996; 46:1026-1029. [CrossRef]
- Chen SM, Dumler JS, Bakken JS, Walker DH. Identification of a granulocytotropic Ehrlichia species as the etiologic agent of human disease. J Clin Microbiol. 1994;32:589–95. [CrossRef]
- Petrovec M, Furlan SL, Zupanc TA, Strle F, Brouqui P, Roux V, Dumler JS. Human disease in Europe is caused by a granulocytic Ehrlichia species. J Clin Microbiol. 1997;35:1556-9. [CrossRef]
- Brouqui PH, Dumler JS, Lienhard R, Brossard M, Raoult D. Human granulocytic ehrlichiosis in Europe. Lancet. 1995;346:782–3. [CrossRef]
- Sumption KJ, Wright D Sumption KJ, Wright DJ, Cutler SJ. Human ehrlichiosis in the UK. Lancet. 1995;346:1487–8. [CrossRef]
- Woldehiwet, Z., Horrocks, B. K., Scaife, H., Ross, G., Munderloh, U. G., Bown, K., et al. (2002). Cultivation of an ovine strain of Ehrlichia phagocytophila in tick cell cultures. J. Comp. Pathol. 127, 142–149. [CrossRef]
- Medlock JM, Hansford KM, Bormane A, Derdakova M, Estrada-Peña A, George JC, et al. Driving forces for changes in the geographical distribution of Ixodes ricinus ticks in Europe. Parasit Vectors. 2013;6:1. [CrossRef]
- Jahfari S, Coipan EC, Fonville M, Van Leeuwen AD, Hengeveld P, Heylen D, et al. Circulation of four Anaplasma phagocytophilum ecotypes in Europe. Parasit Vectors. 2014;7:365. [CrossRef]
- Krücken J, Schreiber C, Maaz D, Kohn M, Demeler J, Beck S, et al. A novel high-resolution melt PCR assay discriminates Anaplasma phagocyt- ophilum and “Candidatus Neoehrlichia mikurensis”. J Clin Microbiol. 2013;51:1958–61.
- James CA, Pearl DL, Lindsay LR, Peregrine AS, Jardine CM. Risk factors associated with the carriage of Ixodes scapularis relative to other tick species in a population of pet dogs from southeastern Ontario, Canada. Ticks Tick Borne Dis. 2019 Feb;10(2):290-298. [PubMed: 30466965]. [CrossRef]
- Dahlgren FS, Heitman KN, Drexler NA, Massung RF, Behravesh CB. Human granulocytic anaplasmosis in the United States from 2008 to 2012: a summary of national surveillance data. Am J Trop Med Hyg. 2015; 93:66–72. [CrossRef]
- Stuen S, Granquist EG, Silaghi C. Anaplasma phagocytophilum—a widespread multi-host pathogen with highly adaptive strategies. Front Cell Infect Microbiol. 2013;3:31. [CrossRef]
- Lee EH, Rikihisa Y. Anti-Ehrlichia chaffeensis antibody complexed with E. chaffeensis induces potent proinflammatory cytokine mRNA expression in human monocytes through sustained reduction of IkappaB-alpha and activation of NF-kappaB. Infect Immun. 1997; 65:2890-2897. [CrossRef]
- Ismail N, Walker DH, Ghose P, et al. Immune mediators of protective and pathogenic immune responses in patients with mild and fatal human monocytotropic ehrlichiosis. BMC Immunol. 2012; 13:26. [CrossRef]
- Ismail N, Crossley EC, Stevenson HL, et al. The relative importance of T-cell subsets in monocytotropic ehrlichiosis: a novel effector mechanism involved in Ehrlichia-induced immunopathology in murine ehrlichiosis. Infect Immun. 2007; 75:4608-4620. [CrossRef]
- Nadelman RB, Horowitz HW, Hsieh TC, et al. Simultaneous- ous human granulocytic ehrlichiosis and Lyme borreliosis. N Engl J Med. 1997;337:27-30. [CrossRef]
- Nilmarie Guzman; Siva Naga S. Yarrarapu; Sary O. Beidas Anaplasma Phagocytophilum.
- Diuk-Wasser MA, Vannier E, Krause PJ. Coinfection by Ixodes tick-borne pathogens: ecological, epidemiological, and clinical consequences. Trends Parasitol. 2016;32: 30–42. [CrossRef]
- Bakken JS, Dumler S. Human granulocytic anaplasmosis. Infect Dis Clin. 2008;22:433–48. [CrossRef]
- Jereb M, Pecaver B, Tomazic J, Muzlovic I, Avsic-Zupanc T, Premru-Srsen T, et al. Severe human granulocytic anaplasmosis transmitted by blood transfusion. Emerg Infect Dis. 2012;18:1354–7. [CrossRef]
- Shields K, Cumming M, Rios J, Wong MT, Zwicker JI, Stramer SL, Alonso CD. Transfusion-associated Anaplasma phagocytophilum infection in a pregnant patient with thalassemia trait: a case report. Transfusion. 2015;55:719–25. [CrossRef]
- Zhang L, Liu Y, Ni D, Li Q, Yu Y, Yu XJ, et al. Nosocomial transmission of human granulocytic anaplasmosis in China. JAMA. 2008;300:2263–70. [CrossRef]
- Krause PJ, Wormser GP. Nosocomial transmission of human granulocytic anaplasmosis? JAMA. 2008;300:2308–9. [CrossRef]
- Bouchard C, Dibernardo A, Koffi J, Wood H, Leighton PA, Lindsay LR. Increased risk of tick-borne diseases with climate and environmental changes. Can Commun Dis Rep 2019;45(4):81–89. [CrossRef]
- Daszak P, Cunningham AA, Hyatt AD. Anthropogenic environmental change and the emergence of infectious diseases in wildlife. Acta Trop 2001;78:103–116. [CrossRef]
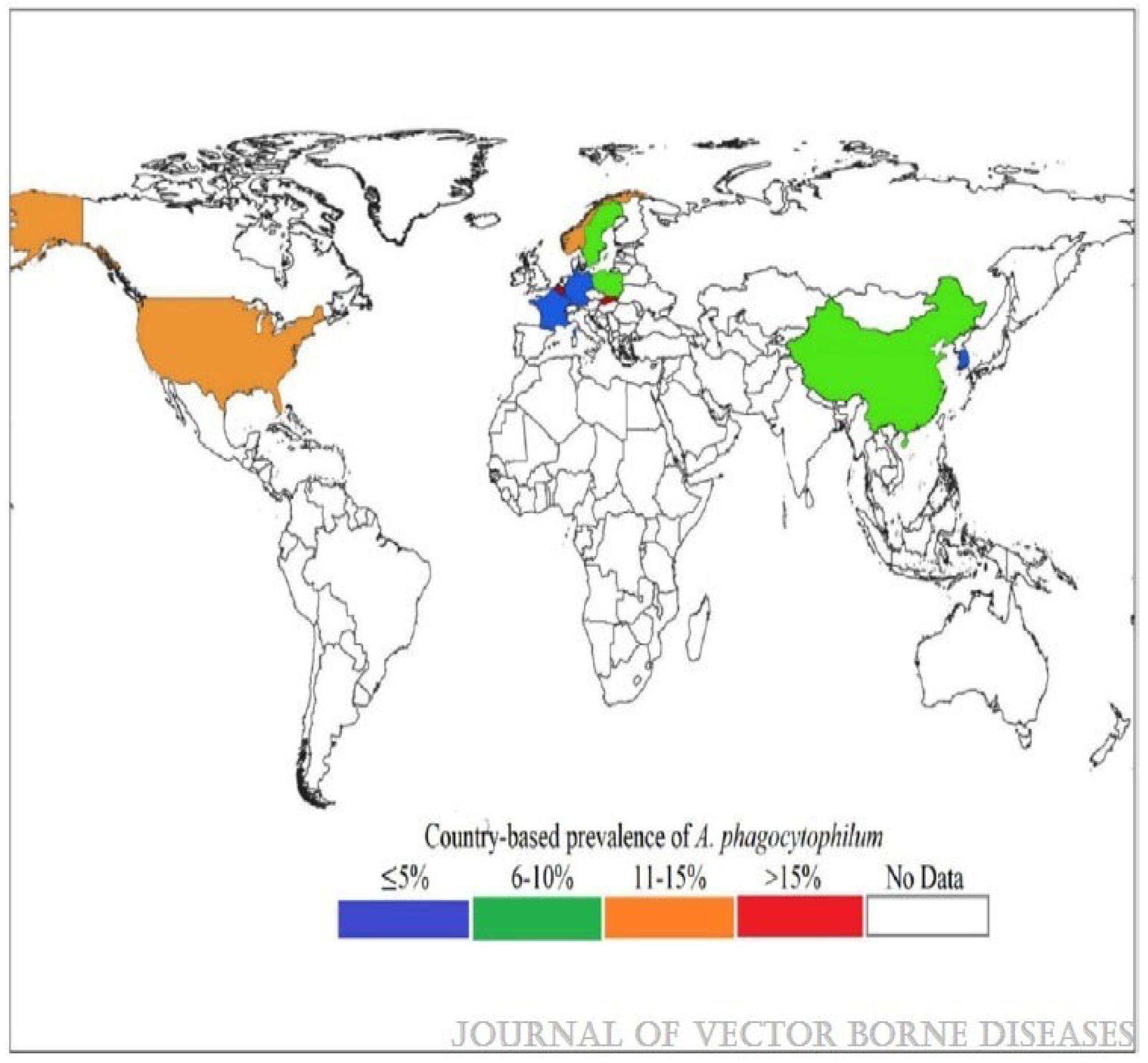
- Global status of Anaplasma phagocytophilum infections in human population: A 50-year (1970–2020) meta-analysis - Karshima, Solomon Ngutor1; Ahmed, Musa Isiyaku2; Mohammed, Kaltume Mamman1; Pam, Victoria Adamu Journal of Vector Borne Diseases 60(3):p 265-278, Jul–Sep 2023. [CrossRef]
- Dumler JS, Choi KS, Garcia-Garcia JC, Barat NS, Scorpio DG, Garyu JW, et al. Human granulocytic anaplasmosis and Anaplasma phagocytophilum. Emerg Infect Dis. 2005;11:1828–34. [CrossRef]
- Nordberg M. Tick-borne infections in humans: aspects of immunopathogenesis, diagnosis, and co-infections with Borrelia burgdorferi and Anaplasma phagocytophilum. Ph.D thesis, Linköping University, Sweden; 2012.
- Dumler JS, Barbet AF, Bekker CP, Dasch GA, Palmer GH, Ray SC, et al. Reorganization of genera in the families Rickettsiaceae and Anaplasmataceae in the order Rickettsiales: unification of some species of Ehrlichia with Anaplasma, Cowdria with Ehrlichia and Ehrlichia with Neorickettsia, descriptions of six new species combinations and designation of Ehrlichia equi and HGE agent as subjective synonyms of Ehrlichia phagocytophila. Int J Syst Evol Microbiol 2001;51:2145–2165. [CrossRef]
- Dumler JS, Choi KS, Garcia-Garcia JC, et al. (December 2005). “Human granulocytic anaplasmosis and Anaplasma phagocytophilum”. Emerging Infect. Dis. 11 (12): 1828. PMC 3367650. PMID 16485466. [CrossRef]
- Nilmarie Guzman; Siva Naga S. Yarrarapu; Sary O. Beidas-Anaplasma Phagocytophilum.
- Anaplasma Phagocytophilum-Nilmarie Guzman; Siva Naga S. Yarrarapu; Sary O. Beidas.
- Shah JS, Horowitz R, Harris NS. Human babesiosis and ehrlichiosis–current status. Eur Infect Dis 2012;6:49–56.
- Morulae in neutrophils: A diagnostic clue for human granulocytic anaplasmosis Sungim Choia, Young-Uk Chob, Sung-Han Kima. [CrossRef]
- Davies RS, Madigan JE, Hodzic E, et al. Dexamethasone- induced cytokine changes associated with diminished disease severity in horses infected with Anaplasma phagocytophilum. Clin Vaccine Immunol. 2011;18:1962–1968. [CrossRef]
- Dumler JS, Madigan JE, Pusterla N, et al. Ehrlichioses in humans: epidemiology, clinical presentation, diagnosis, and treatment. Clin Infect Dis. 2007;45(suppl 1):S45–S51. [CrossRef]
- Bakken JS, Dumler JS. Clinical diagnosis and treatment of human granulocytotropic anaplasmosis. Ann N Y Acad Sci 2006;1078:236–247. [CrossRef]
- Guo WP, Huang B, Zhao Q, Xu G, Liu B, Wang YH, Zhou EM. Human-pathogenic Anaplasma spp., and Rickettsia spp. in animals in Xi’an, China. PLoS Negl Trop Dis. 2018 Nov;12(11): e 0006916. [PMC free article: PMC6258427] [PubMed: 30419024]. [CrossRef]
- Kim SW, Kim CM, Kim DM, Yun NR. Manifestation of anaplasmosis as cerebral infarction: a case report. BMC Infect Dis. 2018 Aug 17;18(1):409. [PMC free article: PMC6098650] [PubMed: 30119642]. [CrossRef]
- Goel R, Westblade LF, Kessler DA, Sfeir M, Slavinski S, Backenson B, Gebhardt L, Kane K, Laurence J, Scherr D, Bussel J, Dumler JS, Cushing MM. Death from Transfusion-Transmitted Anaplasmosis, New York, USA, 2017. Emerg Infect Dis. 2018 Aug;24(8):1548-1550. [PMC free article: PMC6056119] [PubMed: 30016241]. [CrossRef]
- Kobayashi KJ, Weil AA, Branda JA. Case 16-2018: A 45-Year-Old Man with Fever, Thrombocytopenia, and Elevated Aminotransferase Levels. N Engl J Med. 2018 May 24;378(21):2023-2029. [PubMed: 29791814]. [CrossRef]
- Manifestation of anaplasmosis as cerebral infarction: a case report - Seok Won Kim, Choon-Mee Kim, Dong-Min Kim and Na Ra Yun. [CrossRef]
- Grant, L.; Mohamedy, I.; Loertscher, L. One man, three tick-borne illnesses. BMJ Case Rep. 2021, 14, e241004. [Google Scholar] [CrossRef] [PubMed]
- Halasz, C.L.G.; Niedt, G.W.; Kurtz, C.P.; Scorpio, D.G.; Bakken, J.S.; Dumler, J.S. A case of sweet syndrome associated with human granulocytic anaplasmosis. Arch. Dermatol. 2005, 141, 887–889. [Google Scholar] [CrossRef] [PubMed]
- Eldaour, Y.; Hariri, R.; Yassin, M. Severe Anaplasmosis presenting as possible CVA: Case report and 3-year Anaplasma infection diagnosis data is based on PCR testing and serology. IDCases 2021, 24, e01073. [Google Scholar] [CrossRef] [PubMed]
- Khatri, A.; Lloji, A.; Doobay, R.; Wang, G.; Knoll, B.; Dhand, A.; Nog, R. Anaplasma phagocytophilum presenting with orchitis in a renal transplant recipient. Transpl. Infect. Dis. 2019, 21, e13129. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.W.; Kim, C.M.; Kim, D.M.; Yun, N.R. Manifestation of anaplasmosis as cerebral infarction: A case report. BMC Infect. Dis. 2018, 18, 409. [Google Scholar] [CrossRef] [PubMed]
- Young, N.P.; Klein, C.J. Encephalopathy with seizures having PCR-positive Anaplasma phagocytophilum and Ehrlichia chaffeensis. Eur. J. Neurol. 2007, 14, 2006–2007. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T.; Brown, M.; Rabbat, M.; Slim, J. Hemophagocytic Lymphohistiocytosis Associated with Anaplasmosis. J. Glob. Infect. Dis. 2017, 9, 76–78. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.; Jameel, M.N.Q.; Ali, S.S.; Mir, S. Human granulocytic anaplasmosis affecting the myocardium. J. Gen. Intern. Med. 2005, 20, 958. [Google Scholar] [CrossRef]
- Dahlgren FS, Mandel EJ, Krebs JW, Massung RF, McQuiston JH. Increasing incidence of Ehrlichia chaffeensis and Anaplasma phagocytophilum in the United States, 2000-2007. Am J Trop Med Hyg 2011;85(1):124–231. [CrossRef]
- Assi MA, Yao JD, Walker RC. Lyme disease followed by human granulocytic anaplasmosis in a kidney transplant recipient. Transpl Infect Dis 2007; 9: 66-72 [PMID: 17313478]. [CrossRef]
- Khatri A, Lloji A, Doobay R, Wang G, Knoll B, Dhand A, Nog R. Anaplasma phagocytophilum presenting with orchitis in a renal transplant recipient. Transpl Infect Dis 2019; 21: e13129 [PMID: 31215144]. [CrossRef]
- Dana A, Antony A, Patel MJ. Vector-borne infections in solid organ transplant recipients. Int J Dermatol 2012; 51: 1-11 [PMID: 22182371]. [CrossRef]
- Aguero-Rosenfeld ME, Horowitz HW, Wormser GP, et al. Human granulocytic ehrlichiosis: a case series from a medical center in New York State. Ann Intern Med. 1996;125:904–908. [CrossRef]
- Bakken JS, Krueth J, Wilson-Nordskog C, et al. Clinical and laboratory characteristics of human granulocytic ehrlichiosis. JAMA. 1996;275:199–205. [CrossRef]
- Schotthoefer AM, Schrodi SJ, Meece JK, et al. Pro-inflammatory immune responses are associated with clinical signs and symptoms of human anaplasmosis. PLoS ONE. 2017;12:e0179655. [CrossRef]
- Lotric-Furlan S, Petrovec M, Avsic-Zupanc T, et al. Epidemiological, clinical and laboratory distinction between human granulocytic ehrlichiosis and the initial phase of tick-borne encephalitis. Wien Klin Wochenschr. 2002;114:636–640.
- Dumler JS, Barat NC, Barat CE, et al. Human granulocytic anaplasmosis and macrophage activation. Clin Infect Dis. 2007;45:199–204. [CrossRef]
- Jiao XY, Fan ZC, Li YZ, et al. Clinical and laboratory features parameters of human granulocytic anaplasmosis (HGA) in patients admitted to hospital in Guangdong Province, China. Trop Doct. 2015;45:209–213. [CrossRef]
- Snorre Stuen, Erik G. Granquist, and Cornelia Silaghi - Anaplasma phagocytophilum - a widespread multi-host pathogen with highly adaptive strategies. [CrossRef]
- CDC. Statistics | Ehrlichiosis |. CDC. Available at https://www.cdc.gov/ehrlichiosis/stats/. March 26, 2020; Accessed: May 25, 2021.
- Rikihisa, Y. 1991. The tribe Ehrlichieae and ehrlichial diseases. Clin. Microbiol Rev. 4:286–308. [CrossRef]
- Tick-borne zoonoses in Europe - Marta Granström. [CrossRef]
- Morais JD, Dawson JE, Green C et al. - First European case of ehrlichiosis. Lancet. 1991; 338: 633-634. [CrossRef]
- Pierard D, Levtchenko E, Dawson JE, Lauwers S - Ehrlichiosis in Belgium. Lancet. 1995; 346: 1233-1234. 1234. [CrossRef]
- Brouqui P, Raoult D, Durand JM - Ehrlichia species as possible causative agents of blood culture-negative. [CrossRef]
- Paddock, C. D., S. M. Folk, G. M. Shore, L. J. Machado, M. M. Huycke, L. N. Slater, A. M. Liddell, R. S. Buller, G. A. Storch, T. P. Monson, D. Rimland, J. W. Sumner, J. Singleton, K. C. Bloch, Y. W. Tang, S. M. Standaert, and J. E. Childs. 2001. Infections with Ehrlichia chaffeensis and Ehrlichia ewingii in persons coinfected with human immunodeficiency virus. Clin. Infect. Dis. 33:1586–1594. [CrossRef]
- https://www.cdc.gov/ehrlichiosis/symptoms/index.html - Ehrlichiosis.
- Nichols Heitman K, Dahlgren FS, Drexler NA, et al. Increasing incidence of ehrlichiosis in the United States: a summary of national surveillance of Ehrlichia chaffeensis and Ehrlichia ewingii infections in the United States, 2008-2012. Am J Trop Med Hyg. 2016;94:52–60. [CrossRef]
- Dunn BE, Monson TP, Dumler JS, et al. Identification of Ehrlichia chaffeensis morulae in cerebrospinal fluid mononuclear cells. J Clin Microbiol. 1992;30:2207–2210. [CrossRef]
- Ismail N, Walker DH, Ghose P, et al. Immune mediators of protective and pathogenic immune responses in patients with mild and fatal human monocytotropic ehrlichiosis. BMC Immunol. 2012;13:26. [CrossRef]
- Dumler JS, Madigan JE, Pusterla N, et al. Ehrlichioses in humans: epidemiology, clinical presentation, diagnosis, and treatment. Clin Infect Dis. 2007;45(suppl 1):S45–S51. [CrossRef]
- Fishbein DB, Dawson JE, Robinson LE. Human ehrlichiosis in the United States, 1985 to 1990. Ann Intern Med. 1994;120:736–743. [CrossRef]
- Schutze GE, Buckingham SC, Marshall GS, et al. Human monocytic ehrlichiosis in children. Pediatr Infect Dis J. 2007;26:475–479. [CrossRef]
- Kumar N, Goyal J, Goel A, et al. Macrophage activation syndrome secondary to human monocytic ehrlichiosis. Indian J Hematol Blood Transfus. 2014;30:145–147. [CrossRef]
- Abbott KC, Vukelja SJ, Smith CE, et al. Hemophagocytic syndrome: a cause of pancytopenia in human ehrlichiosis. Am J Hematol. 1991;38:230–234. [CrossRef]
- Burns S, Saylors R, Mian A. Hemophagocytic lymphohistiocytosis secondary to Ehrlichia chaffeensis infection: a case report. J Pediatr Hematol Oncol. 2010;32:e142–e143. [CrossRef]
- Cheng A, Williams F, Fortenberry J, et al. Use of extracorporeal support in hemophagocytic lymphohistiocytosis secondary to ehrlichiosis. Pediatrics. 2016;138. [CrossRef]
- Hanson D, Walter AW, Powell J. Ehrlichia-induced hemophagocytic lymphohistiocytosis in two children. Pediatr Blood Cancer. 2011;56:661–663. [CrossRef]
- Hamburg BJ, Storch GA, Micek ST, et al. The importance of early treatment with doxycycline in human ehrlichiosis. Medicine (Baltimore). 2008;87:53–60. [CrossRef]
- Paddock CD, Folk SM, Shore GM, et al. Infections with Ehrlichia chaffeensis and Ehrlichia ewingii in persons coinfected with human immunodeficiency virus. Clin Infect Dis. 2001;33:1586–1594. [CrossRef]
- Thomas LD, Hongo I, Bloch KC, et al. Human ehrlichiosis in transplant recipients. Am J Transplant. 2007;7:1641–1647. [CrossRef]
- Paddock, C. D., S. M. Folk, G. M. Shore, L. J. Machado, M. M. Huycke, L. N. Slater, A. M. Liddell, R. S. Buller, G. A. Storch, T. P. Monson, D. Rimland, J. W. Sumner, J. Singleton, K. C. Bloch, Y. W. Tang, S. M. Standaert, and J. E. Childs. 2001. Infections with Ehrlichia chaffeensis and Ehrlichia ewingii in persons coinfected with human immunodeficiency virus. Clin. Infect. Dis. 33:1586–1594. [CrossRef]
- 273/ Walker, D. H. 2000. Diagnosing human ehrlichioses: current status and recommendations. ASM News 66:287–291.
- 61/ Childs, J. E., J. W. Sumner, W. L. Nicholson, R. F. Massung, S. M. Standaert, and C. D. Paddock. 1999. Outcome of diagnostic tests using samples from patients with culture-proven human monocytic ehrlichiosis: implications for surveillance. J. Clin. Microbiol. 37:2997–3000. [CrossRef]
- 73/ Dawson, J. E., B. E. Anderson, D. B. Fishbein, J. L. Sanchez, C. S. Goldsmith, K. H. Wilson, and C. W. Duntley. 1991. Isolation and characterization of an Ehrlichia sp. from a patient diagnosed with human ehrlichiosis. J. Clin. Microbiol. 29:2741–2745. [CrossRef]
- 209/ Paddock, C. D., J. W. Sumner, G. M. Shore, D. C. Bartley, R. C. Elie, J. G. McQuade, C. R. Martin, C. S. Goldsmith, and J. E. Childs. 1997. Isolation and characterization of Ehrlichia chaffeensis strains from patients with fatal ehrlichiosis. J. Clin. Microbiol. 35:2496–2502. [CrossRef]
- 255/ Standaert, S. M., T. Yu, M. A. Scott, J. E. Childs, C. D. Paddock, W. L. Nicholson, J. Singleton, and M. J. Blaser. 2000. Primary isolation of Ehrlichia chaffeensis from patients with febrile illnesses: clinical and molecular characteristics. J. Infect. Dis. 181:1082–1088. [CrossRef]
- 262/ Tan, H. P., J. S. Dumler, W. R. Maley, A. S. Klein, J. F. Burdick, P. F. Fred, P. J. Thuluvath, and J. S. Markowitz. 2001. Human monocytic ehrlichiosis: an emerging pathogen in transplantation. Transplantation 71:1678–1680. [CrossRef]
- 99/ Everett, E. D., K. A. Evans, R. B. Henry, and G. McDonald. 1994. Human ehrlichiosis in adults after tick exposure: diagnosis using polymerase chain reaction. Ann. Intern. Med. 120:730–735. [CrossRef]
- 90/ Dumler, J. S., S. M. Chen, K. Asanovich, E. Trigiani, V. L. Popov, and D. H. Walker. 1995. Isolation and characterization of a new strain of Ehrlichia chaffeensis from a patient with nearly fatal monocytic ehrlichiosis. J. Clin. Microbiol. 33:1704–1711. [CrossRef]
- Gorenflot A, Moubri K, Precigout E, Carcy B, Schetters TP. Human babesiosis. Ann Trop Med Parasitol. 1998. [CrossRef]
- Boeva-Bangyozova, Violina; K.Eneva; Muhtarov, Marin; Dragomirova, Petya. HUMAN BABESIOSIS.JOUR, 2018/02/05.
- Amsden, J. R., Warmack, S., & Gubbins, P. O. (2005). Tick-Borne Bacterial, Rickettsial, Spirochetal, and Protozoal Infectious Diseases in the United States: A Comprehensive Review. Pharmacotherapy, 25(2), 191– 210. [CrossRef]
- Krause PJ, Telford SR, Ryan R, et al. Geographical and temporal distribution of babesial infection in Connecticut. J Clin Microbiol 1991;29:1–4. [CrossRef]
- Rochlin, Ilia, and Alvaro Toledo. “Emerging tick-borne pathogens of public health importance: a mini-review.” Journal of medical microbiology 69.6 (2020): 781. [CrossRef]
- Kumar, A.; O’Bryan, J.; Krause, P.J. The Global Emergence of Human Babesiosis. Pathogens 2021, 10, 1447. [Google Scholar] [CrossRef] [PubMed]
- Jia N, Zheng Y-C, Jiang J-F, Jiang R-R, Jiang B-G et al. Human babesiosis caused by a Babesia crassa Like pathogen: a case series. Clin Infect Dis 2018;67:1110–1119. [CrossRef]
- Homer MJ, Aguilar-Delfin IA, Telford SR, Krause PJ, Persing DH (2000) Babesiosis. Clin Microbiol Rev 13(3):451–469. [CrossRef]
- Laha, Ramgopal, M. Das, and A. Sen. “Morphology, epidemiology, and phylogeny of Babesia: An overview.” Tropical parasitology 5.2 (2015): 94. [CrossRef]
- Madison-Antenucci, Susan, et al. “Emerging tick-borne diseases.” Clinical microbiology reviews 33.2 (2020): 10-1128. [CrossRef]
- Boustani, Maria R., and Jeffrey A. Gelfand. “Babesiosis.” Clinical infectious diseases (1996): 611-614.
- Plesman, Joseph, and Andrew Spielman. “Babesia microti: infectivity of parasites from ticks for hamsters and white-footed mice.” Experimental parasitology 53.2 (1982): 242-248. [CrossRef]
- Herwaldt, Barbara L., et al. “Transfusion-associated babesiosis in the United States: a description of cases.” Annals of internal medicine 155.8 (2011): 509-519. [CrossRef]
- Gray, E. B., and B. L. Herwaldt. “Surveillance for babesiosis—United States, 2014.” Division of Parasitic Diseases and Malaria, Centers for Disease Control and Prevention, Atlanta, GA (2016).
- Kletsova, Ekaterina A., et al. “Babesiosis in Long Island: review of 62 cases focusing on treatment with azithromycin and atovaquone.” Annals of clinical microbiology and antimicrobials 16.1 (2017): 1-7. [CrossRef]
- White DJ, Talarico J, Chang HG, Birkhead GS, Heimberger T, Morse DL. 1998. Human babesiosis in New York State: review of 139 hospitalized cases and analysis of prognostic factors. Arch Intern Med 158:2149–2154. [CrossRef]
- Martinot, M.; Zadeh, M.M.; Hansmann, Y.; Grawey, I.; Christmann, D.; Aguillon, S.; Jouglin, M.; Chauvin, A.; De Briel, D. Babesiosis in immunocompetent patients, Europe. Emerg. Infect. Dis. 2011, 17, 114–116. [Google Scholar] [CrossRef] [PubMed]
- Chan, W.Y.; MacDonald, C.; Keenan, A.; Xu, K.; Bain, B.J.; Chiodini, P.L. Severe babesiosis due to Babesia divergens acquired in the United Kingdom. Am. J. Hematol. 2021, 96, 889–890. [Google Scholar] [CrossRef] [PubMed]
- Herwaldt, B.L.; Cacció, S.; Gherlinzoni, F.; Aspöck, H.; Slemenda, S.B.; Piccaluga, P.; Martinelli, G.; Edelhofer, R.; Hollenstein, U.; Poletti, G.; et al. Molecular characterization of a non-Babesia divergens organism causing zoonotic babesiosis in Europe. Emerg. Infect. Dis. 2003, 9, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Li, H.; Gao, X.; Bian, A.; Yan, H.; Kong, D.; Liu, X. Human babesiosisi n China: Asystematic review. Parasitol. Res. 2019, 118, 1103–1112. [CrossRef]
- Rollend, L., S.J. Bent, P.J. Krause, S. et al. Quantitative PCR for detection of Babesia microti in Ixodes scapularis ticks and in human blood. Vector Borne Zoonotic Dis., 2013, 13, 784-90. [CrossRef]
- Krause, P.J., S.R. Telford, R. Ryan et al. Diagnosis of babesiosis: evaluation of a serologic test for the detection of Babesia microti antibody. J. Infect. Dis., 1994, 169, 4, 923-6. [CrossRef]
- Krause, P.J.; McKay, K.; Thompson, C.A.; Sikand, V.K.; Lentz, R.; Lepore, T.; Closter, L.; Christianson, D.; Telford, S.R.; Persing, D.; et al. Disease-specific diagnosis of coinfecting tickborne zoonoses: Babesiosis, human granulocytic ehrlichiosis, and Lyme disease. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2002, 34, 1184–1191. [CrossRef]
- Hunfeld, K.P.; Lambert, A.; Kampen, H.; Albert, S.; Epe, C.; Brade, V.; Tenter, A.M. Seroprevalence of Babesia infections in humans exposed to ticks in midwestern Germany. J. Clin. Microbiol. 2002, 40, 2431–2436. [Google Scholar] [CrossRef] [PubMed]
- Wilson, Melisa, et al. “Development of droplet digital PCR for the detection of Babesia microti and Babesia duncani.” Experimental parasitology 149 (2015): 24-31. [CrossRef]
- Saifee NH, Krause PJ, Wu Y. 2016. Apheresis for babesiosis: therapeutic parasite reduction or removal of harmful toxins or both? J Clin Apher 31:454–458. [CrossRef]
- Krause PJ, Lepore T, Sikand VK, Gadbaw J, Jr, Burke G, Telford SR, III, Brassard P, Pearl D, Azlanzadeh J, Christianson D, McGrath D, Spielman A. 2000. Atovaquone and azithromycin for the treatment of babesiosis. N Engl J Med 343:1454–1458. [CrossRef]
- Brasseur, P.; Lecoublet, S.; Kapel, N.; Favennec, L.; Ballet, J.J. Quinine in the treatment of Babesia divergens infections in humans. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 1996, 15, 840–841. [CrossRef]
- Bläckberg, J.; Lazarevic, V.L.; Hunfeld, K.P.; Persson, K.E.M. Low-virulent Babesia venatorum infection masquerading as hemophagocytic syndrome. Ann. Hematol. 2018, 97, 731–733. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




