Introduction
Large to massive rotator cuff tears pose a challenging condition, and various treatment methods have been proposed [
1,
2,
3]. Among them, partial repair is a convenient technique that can be performed without the use of additional synthetic tissue, yielding favorable outcomes. However, it has the drawback of a high retear rate [
4]. In an effort to overcome this, Lee et al. reported reducing the retear rate by medializing the footprint attachment site [
5]. Nevertheless, this procedure also has the limitation of not adequately covering and exposing the humerus greater tuberosity footprint [
1,
2,
3].
Among various surgical procedures, superior capsular reconstruction (SCR) is one of the most commonly employed techniques. In order to address the drawbacks associated with the use of the Tensor Fascia Lata in the origin technique and to circumvent donor site issues, the method utilizing acellular dermis matrix (ADM) has become increasingly popular in recent times [
1,
6].
However, the SCR technique inevitably poses the risk of graft failure as it involves connecting the glenoid and humerus. Mirzayan et al. and others have reported satisfactory outcomes by performing a biologic tuberosity interpositioning solely on the humerus tuberosity when graft failure occurs on the glenoid side. They based their findings on favorable results similar to patients with healed grafts [
7,
8]. However, a limitation of the biologic tuberosity is that it exposes the humerus head.
Therefore, as the application sites of medialization repair and biologic tuberosity are separate, combining these procedures is believed to complement the limitations of each technique. The authors aim to introduce this surgical method with the expectation that it can address the shortcomings of each procedure when used in combination.
Surgical Technique
All patients underwent the application of regional anesthesia, and the procedures were performed in the beach chair position. After performing diagnostic arthroscopy, intraarticular single-row repair using the in-box technique was conducted up to Lafosse classification IV subscapularis tear. For Lafosse classification V subscapularis tear, a double-row repair was performed using the out-box technique.
When the biceps was preserved, anterior cable reconstruction using the biceps was performed.
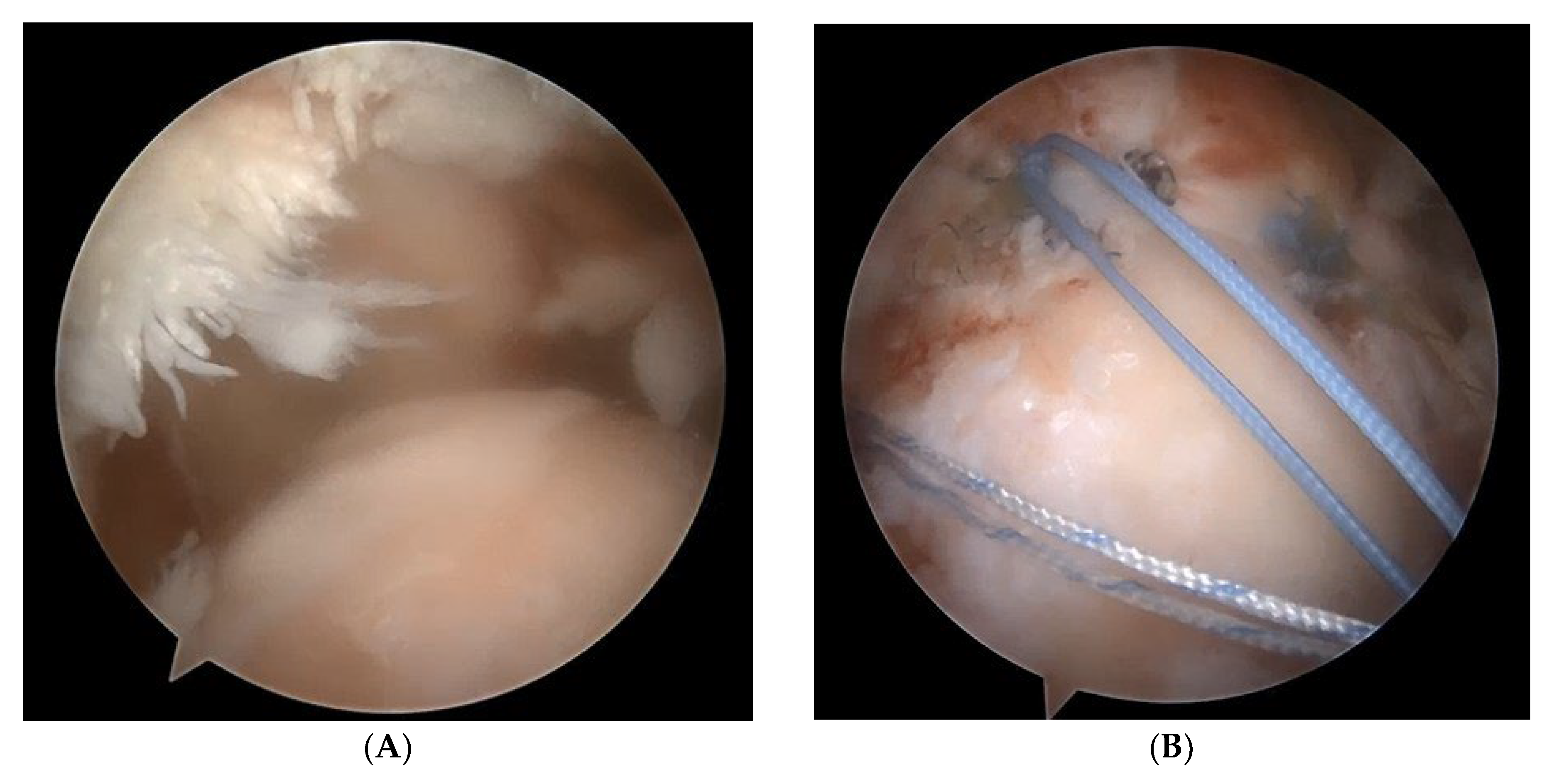
3 Subsequently, the medialization position was determined for the appropriate tension-free repair of the retracted cuff tendon. Single-row repair was conducted using 2-3 medial anchors. Following this, the most anterior and posteriorly tied FiberWire strands were left in place for biologic tuberoplasty (
Figure 1).
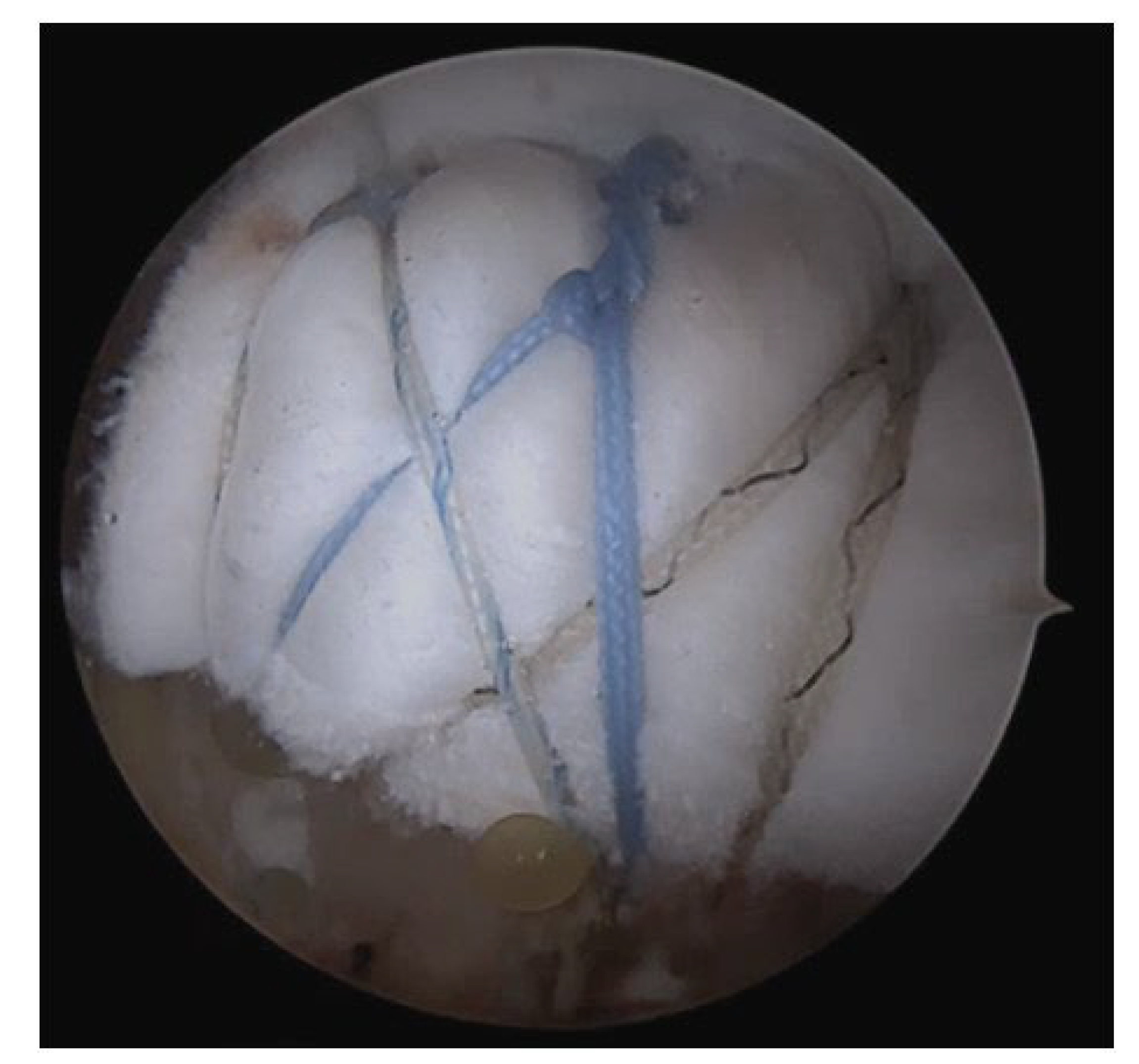
Subsequently, the anterior-posterior and medial-to-lateral distances of the exposed tuberosity were measured. After medialization, the remaining gap was addressed by securing the medial side of a 4mm-thick acellular dermal matrix (BellaCell; Hans Biomed Corporation, Daejeon, Korea) using the residual tissue. Subsequently, a biologic interpositioning tuberoplasty was performed utilizing the suture bridge technique. (
Figure 2)
Postoperative management
All patients wore a shoulder abduction brace for 6 weeks post-surgery. Pendulum exercises commenced at 1 week post-surgery, and passive joint exercises were gradually initiated from 2 weeks post-surgery, with restrictions ensuring no more than 120 degrees of forward elevation and 30 degrees of external rotation until 6 weeks post-surgery. Assisted active joint exercises began at 6 weeks post-surgery, followed by active joint exercises at 8 weeks post-surgery, and resistive strengthening exercises at 12 weeks post-surgery. Progressive open and closed chain exercises were implemented, allowing for gradual return to sports activities by the 6-month postoperative mark.
Case
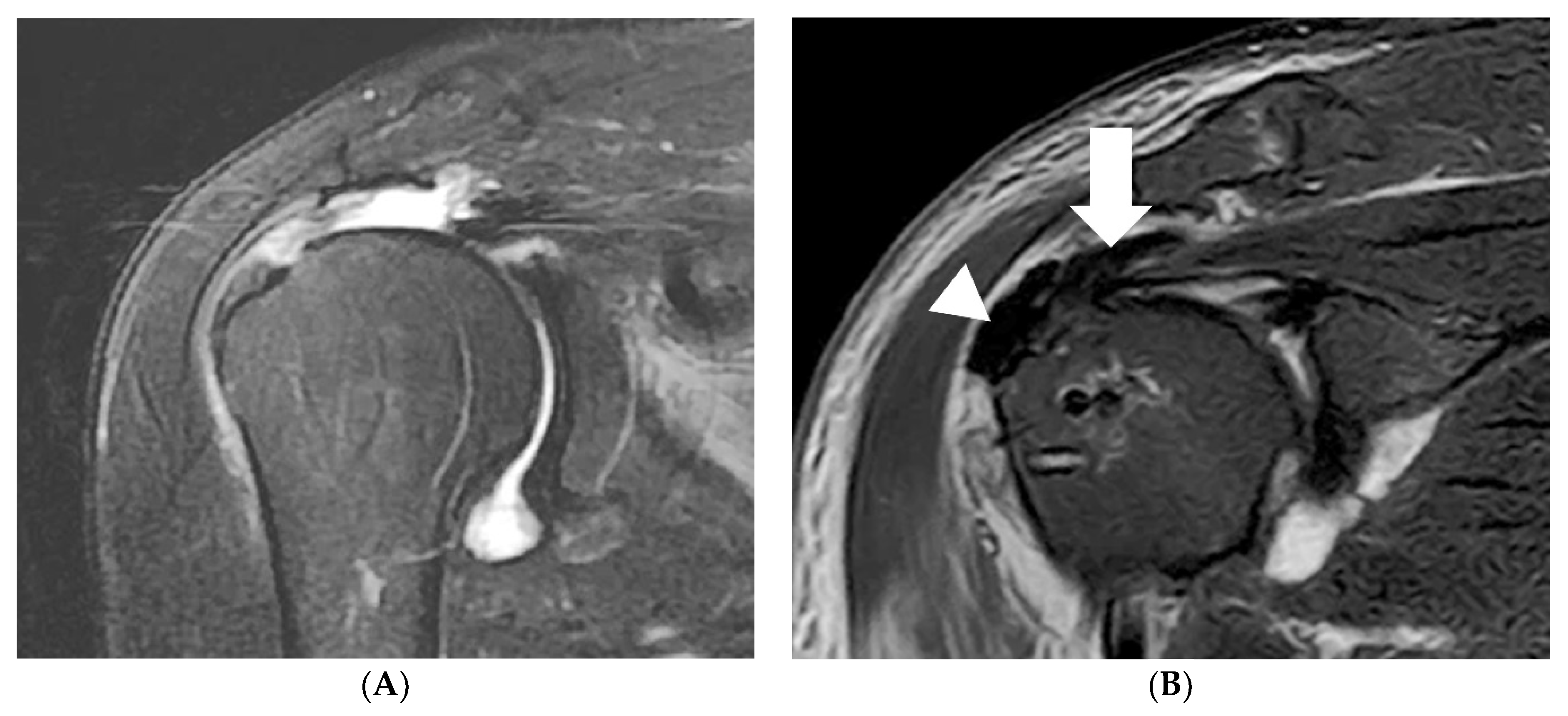
A 71-year-old female patient presented with persistent pain and muscle weakness over several months, leading to a surgical consultation. Preoperative magnetic resonance imaging (MRI) revealed a massive rotator cuff tear. (
Figure 3A) Surgical intervention involved medialization rotator cuff partial repair and biologic tuberoplasty using acellular dermal matrix (ADM). Postoperative MRI demonstrated full coverage from the humeral head to the tuberosity (
Figure 3B).
At the 6-month follow-up, the patient exhibited satisfactory results with pain relief and regained full range of motion (
Figure 4).
Discussion
Large to massive rotator cuff tears are known to be challenging to treat due to chronic tendon wear, severe retraction, and significant fatty degeneration of the muscles [
9,
10] It is known that attempting to repair severely retracted tendons with excessive tension is closely associated with a high rate of re-tear. Therefore, methods aimed at reducing tension, such as footprint medialization repair, have been reported to decrease re-tear rates [
5,
11] However, although medialization partial repair reduces re-tear rates, complete prevention of re-tear is still not possible. Additionally, because exposure of the humerus greater tuberosity (GT) cannot be addressed, preventing bone-to-bone contact between the GT and acromion, there is a drawback in that pain relief or functional improvement cannot be expected.
Mirzayan et al. introduced biologic interpositioning tuberoplasty to prevent inevitable re-tears occurring in Superior Capsular Reconstruction (SCR) and reported satisfactory outcomes [
7,
8]. Seo et al. also reported a re-tear rate of 0% by simultaneously performing biologic interpositioning tuberoplasty and bursal acromial reconstruction. They observed prevention of bone-to-bone contact between the greater tuberosity (GT) and acromion, along with an increase in acromiohumeral distance, resulting in pain relief and functional improvement [
12] However, one drawback of biologic tuberoplasty is that it positions tissue from the medial aspect of the footprint rather than from the glenoid, leaving the medial aspect of the humeral head exposed. Additionally, for severely retracted tendons, adhesiolysis and medialization often allow for adequate repair. Since the repair locations of medialization and biologic tuberosity do not overlap and complement each other in terms of exposed areas, both techniques were applied together, resulting in complete resolution of humeral exposure post-surgery.
SCR can address humeral exposure by connecting from the glenoid to the humeral head, but it cannot completely resolve the complication of re-tears. Moreover, re-tears occurring at the GT site lead to unfavorable clinical outcomes, making the postoperative risk higher than that of biologic tuberosity. Performing only biologic tuberosity in groups where partial repair is possible has limitations, as it not only leaves the disadvantage of humeral head exposure but also eliminates the potential secondary functional improvement expected with successful partial repair.
Even with simultaneous medialization and biologic tuberosity procedures, complete prevention of re-tear in the medialized tendon is not guaranteed. However, in cases where tendon re-tear does occur, biologic tuberoplasty maintains an interpositioned state between the GT and acromion. This suggests that compared to SCR or medialization alone, biologic tuberosity can mitigate the risk of re-tear and potentially lead to better functional improvement by promoting healing of the medialized tendon (
Table 1). Therefore, I believe that further comparative studies involving more case outcomes are necessary.
In summary, the combined use of medialization and biologic interpositioning tuberoplasty serves as a surgical approach that complements the limitations of each technique. Due to the anatomical improvements in various areas compared to standalone procedures, better pain relief and functional enhancement are anticipated.
References
- Mihata T, McGarry MH, Pirolo JM, Kinoshita M, Lee TQ. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: a biomechanical cadaveric study. Am J Sports Med. 2012, 40, 2248-2255. [CrossRef]
- Mirzayan R, Abboud JA, Sethi PM; et al. Emerging Treatment Options for Massive Rotator Cuff Tears: Biologic Tuberoplasty, Balloon Arthroplasty, Anterior Cable Reconstruction, Lower Trapezius Transfer. Instr Course Lect. 2023, 72, 223–238. [Google Scholar] [PubMed]
- Seo JB, Kwak KY, Park B, Yoo JS. Anterior cable reconstruction using the proximal biceps tendon for reinforcement of arthroscopic rotator cuff repair prevent retear and increase acromiohumeral distance. J Orthop. 2021, 23, 246–249.
- Yoo JC, Ahn JH, Koh KH, Lim KS. Rotator cuff integrity after arthroscopic repair for large tears with less-than-optimal footprint coverage. Arthroscopy. 2009, 25, 1093–1100. [Google Scholar] [CrossRef] [PubMed]
- Lee KW, Lee GS, Yang DS, Park SH, Chun YS, Choy WS. Clinical Outcome of Arthroscopic Partial Repair of Large to Massive Posterosuperior Rotator Cuff Tears: Medialization of the Attachment Site of the Rotator Cuff Tendon. Clin Orthop Surg. 2020, 12, 353–363. [Google Scholar] [CrossRef]
- Denard PJ, Brady PC, Adams CR, Tokish JM, Burkhart SS. Preliminary Results of Arthroscopic Superior Capsule Reconstruction with Dermal Allograft. Arthroscopy. 2018, 34, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Mirzayan R, Bouz G. Biologic Tuberoplasty With an Acellular Dermal Allograft for Massive Rotator Cuff Tears. Arthrosc Tech. 2021, 10, e1743–e1749. [Google Scholar] [CrossRef] [PubMed]
- Mirzayan R, Stone MA, Batech M, Acevedo DC, Singh A. Failed Dermal Allograft Procedures for Irreparable Rotator Cuff Tears Can Still Improve Pain and Function: The “Biologic Tuberoplasty Effect”. Orthop J Sports Med. 2019, 7, 2325967119863432. [Google Scholar]
- Elhassan BT, Wagner ER, Werthel JD. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J Shoulder Elbow Surg. 2016, 25, 1346–1353. [Google Scholar] [CrossRef]
- Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004, 86, 219–224. [Google Scholar] [CrossRef]
- Jeong JH, Yoon EJ, Kim BS, Ji JH. Biceps-incorporating rotator cuff repair with footprint medialization in large-to-massive rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2022, 30, 2113–2122. [Google Scholar] [CrossRef]
- Seo JB, Jung JW, Yoo JS. Combination of arthroscopic biologic tuberoplasty and bursal acromial reconstruction. J Orthop. 2024, 51, 1–6. [Google Scholar] [CrossRef]
- Tokish JM, Alexander TC, Kissenberth MJ, Hawkins RJ. Pseudoparalysis: a systematic review of term definitions, treatment approaches, and outcomes of management techniques. J Shoulder Elbow Surg. 2017, 26, e177–e187. [Google Scholar] [CrossRef]
- Mihata T, Bui CNH, Akeda M, et al. A biomechanical cadaveric study comparing superior capsule reconstruction using fascia lata allograft with human dermal allograft for irreparable rotator cuff tear. J Shoulder Elbow Surg. 2017, 26, 2158–2166. [Google Scholar] [CrossRef]
- Mihata T, McGarry MH, Kahn T, Goldberg I, Neo M, Lee TQ. Biomechanical Effect of Thickness and Tension of Fascia Lata Graft on Glenohumeral Stability for Superior Capsule Reconstruction in Irreparable Supraspinatus Tears. Arthroscopy. 2016, 32, 418–426. [Google Scholar] [CrossRef]
- Mihata T, Lee TQ, Watanabe C, et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013, 29, 459–470. [Google Scholar] [CrossRef]
- Ohta S, Komai O, Onochi Y. Outcomes of superior capsule reconstruction for massive rotator cuff tears and risk factors for postoperative retear. Arch Orthop Trauma Surg. 2020, 140, 1319–1325. [Google Scholar] [CrossRef]
- Suri M, Parry S, Dham M, Verma A. Arthroscopic Biologic Tuberoplasty for Irreparable Rotator Cuff Tears: An Expedited Technique. Arthrosc Tech. 2022, 11, e2265–e2270. [Google Scholar] [CrossRef]
- David TS, Grotting JA, Bass S. Dermal Tuberoplasty for Irreparable Supraspinatus Tears Using Self-Punching, Knotless Fixation. Arthrosc Tech. 2023, 12, e71–e75. [Google Scholar] [CrossRef]
- Pines Y, Magone KM, Ben-Ari E, et al. Outcomes of arthroscopic tuberoplasty for symptomatic irreparable rotator cuff tendon tear without pseudoparalysis. JSES Int. 2022, 6, 1005–1010. [Google Scholar] [CrossRef]
- Ravenscroft M, Barnes MW, Muench LN, Mazzocca AD, Berthold DP. Bursal Acromial Reconstruction (BAR) Using an Acellular Dermal Allograft as a Surgical Solution for the Treatment of Massive Irreparable Rotator Cuff Tears. Arthrosc Tech. 2021, 10, e877–e885. [Google Scholar] [CrossRef]
- O’Neil S, Marvil S, Lakehomer H, et al. Modified Technique for Arthroscopic Bursal Acromial Reconstruction Utilizing Acellular Dermal Allograft. Arthrosc Tech. 2022, 11, e301–e306. [Google Scholar] [CrossRef]
- Berthold DP, Ravenscroft M, Bell R, et al. Bursal Acromial Reconstruction (BAR) Using an Acellular Dermal Allograft for Massive, Irreparable Posterosuperior Rotator Cuff Tears: A Dynamic Biomechanical Investigation. Arthroscopy. 2022, 38, 297–306.e292. [Google Scholar] [CrossRef]
- Labib M, Amirouche F, Pradhan S, Bobko A, Koh J. A Biomechanical Analysis of Shoulder Muscle Excursions During Abduction, After the Treatment of Massive Irreparable Rotator Cuff Tears Using Superior Capsular Reconstruction (SCR), Bursal Acromial Reconstruction (BAR), and SCR with BAR. J Shoulder Elb Arthroplast. 2022, 6, 24715492221109001. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).