Submitted:
12 February 2024
Posted:
13 February 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Diagnostic Assessment of Nerve Repair
3. The Problem of Neuropathic Pain
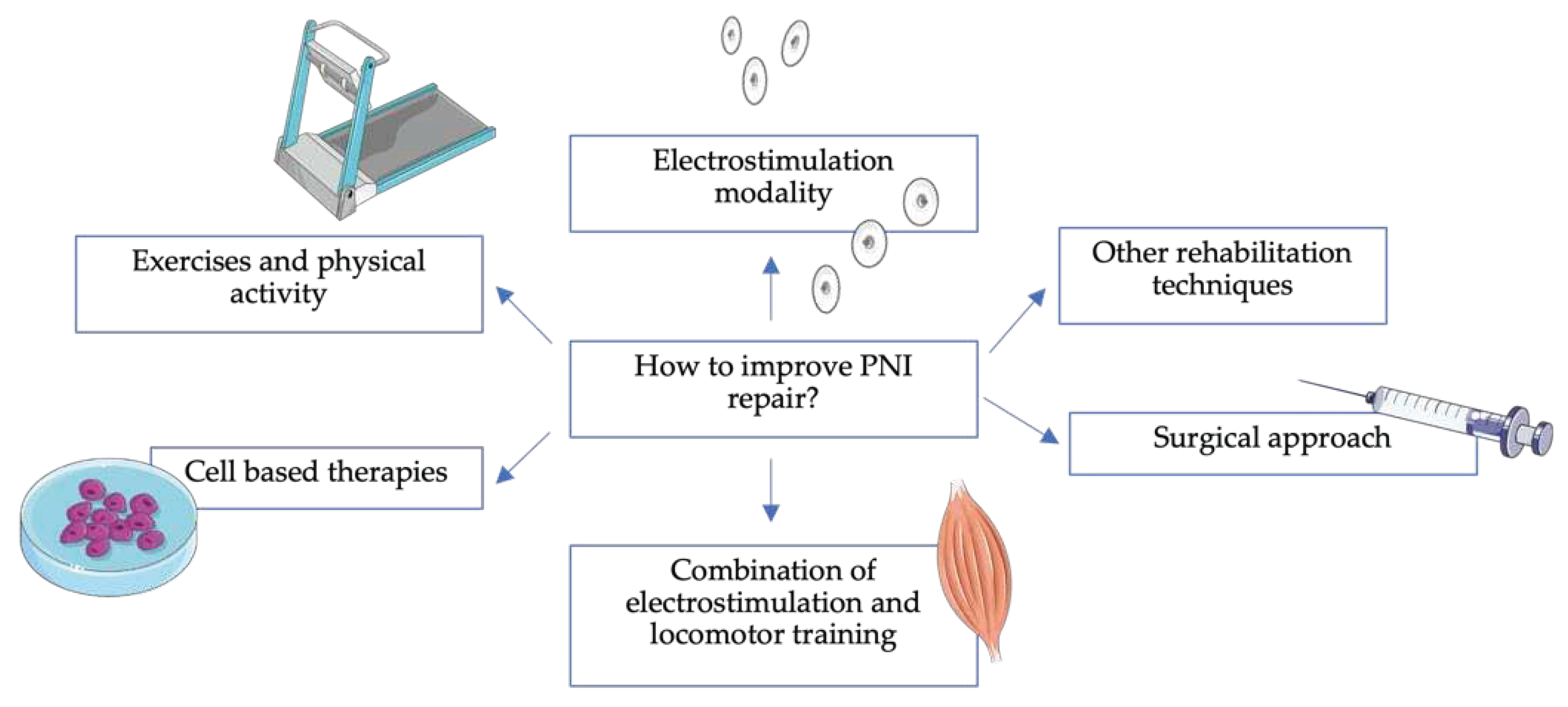
4. How to Improve PNI repair?
4.1. Surgical Approach
4.2. Electrostimulation Modality

4.3. Exercises and Physical Activity
4.4. Combination of Electrical Stimulation and Locomotor Training
4.5. Other Rehabilitation Modalities
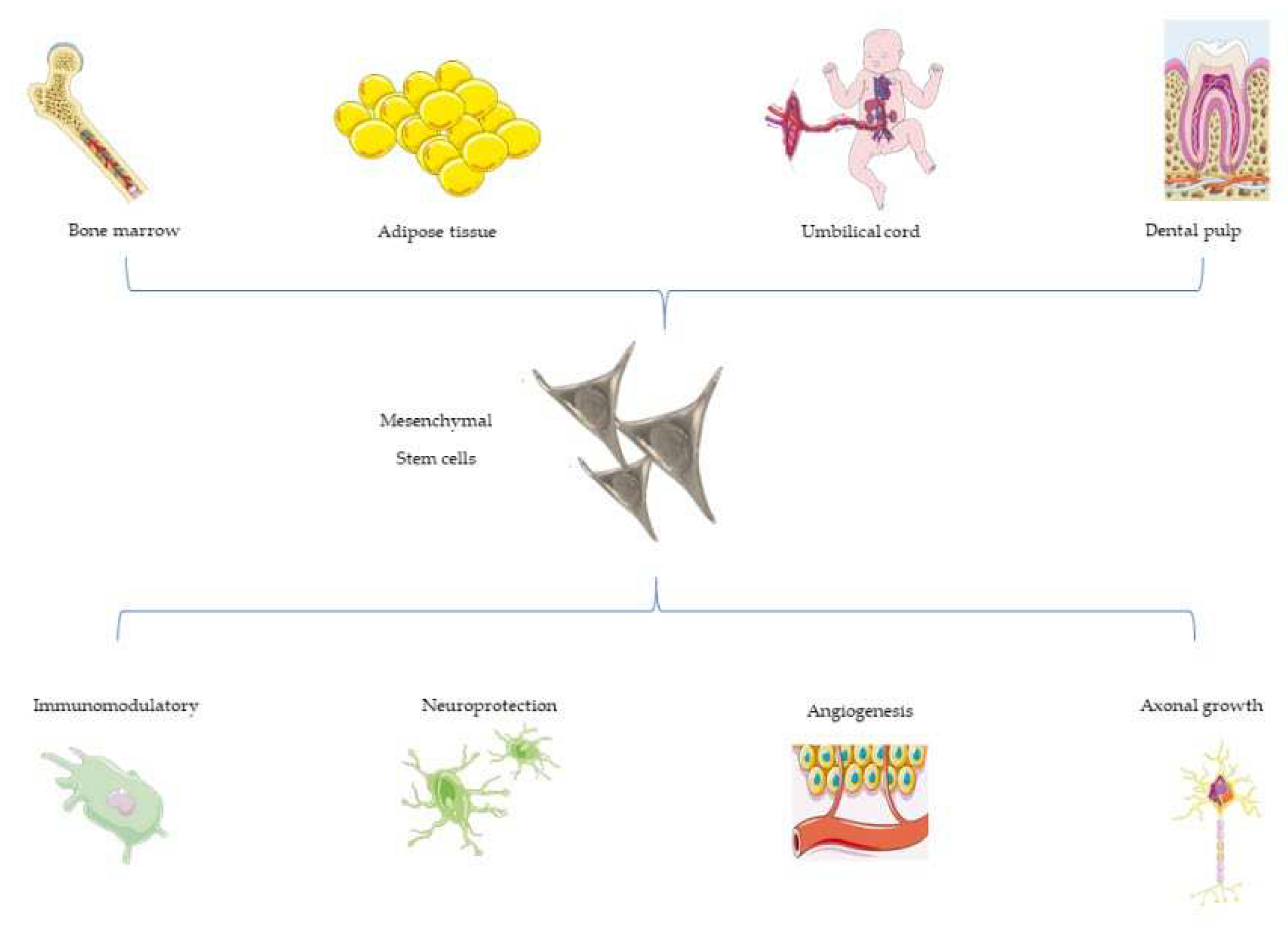
4.6. Cell-Based Therapies and PNI
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgements
Conflicts of Interest
References
- Lavorato, A.; Raimondo, S.; Boido, M.; Muratori, L.; Durante, G.; Cofano, F.; Vincitorio, F.; Petrone, S.; Titolo, P. Tartara, F., et al. Mesenchymal stem cell treatment perspectives in peripheral nerve regeneration: systematic review. Int J Mol Sci. 2021, 22, 572. [Google Scholar] [CrossRef]
- Tremp, M.; Zu Schwabedissen, M.M.; Kappos, E.A.; Engels, P.E.; Fischmann, A.; Scherberich, A.; Schaefer, D.J.; Kalbermatten, D.F. The Regeneration Potential after Human and Autologous Stem Cell Transplantation in a Rat Sciatic Nerve Injury Model can be Monitored by MRI. Cell Transplant. 2015, 24, 203–211. [Google Scholar] [CrossRef]
- Matthes, S.M.; Reimers, K.; Janssen, I.; Liebsch, C.; Kocsis, J.D.; Vogt, P.M.; Radtke, C. Intravenous Transplantation of Mesenchymal Stromal Cells to Enhance Peripheral Nerve Regeneration. BioMed Res. Int. 2013, 2013, 1–6. [Google Scholar] [CrossRef]
- Yousefi, F.; Arab, F.L.; Nikkhah, K.; Amiri, H.; Mahmoudi, M. Novel approaches using mesenchymal stem cells for curing peripheral nerve injuries. Life Sci. 2019, 221, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Moattari, M.; Kouchesfehani, H.M.; Kaka, G.; Sadraie, S.H.; Naghdi, M. Evaluation of nerve growth factor (NGF) treated mesenchymal stem cells for recovery in neurotmesis model of peripheral nerve injury. J. Cranio-Maxillofac. Surg. 2018, 46, 898–904. [Google Scholar] [CrossRef]
- Menchetti, M.; Gandini, G.; Bravaccini, B.; Dondi, M.; Gagliardo, T.; Bianchi, E. Clinical and electrodiagnostic findings and quality of life of dogs and cats with brachial plexus injury. Vet Sci. 2020, 7, 101. [Google Scholar] [CrossRef] [PubMed]
- Lopes, B.; Sousa, P.; Alvites, R.; Branquinho, M.; Sousa, A.C.; Mendonça, C.; Atayde, L.M.; Luís, A.L.; Varejão, A.S.P.; Maurício, A.C. Peripheral Nerve Injury Treatments and Advances: One Health Perspective. Int. J. Mol. Sci. 2022, 23, 918. [Google Scholar] [CrossRef] [PubMed]
- Ribitsch, I.; Baptista, P.M.; Lange-Consiglio, A.; Melotti, L.; Patruno, M.; Jenner, F.; Schnabl-Feichter, E.; Dutton, L.C.; Connolly, D.J.; van Steenbeek, F.G.; et al. Large Animal Models in Regenerative Medicine and Tissue Engineering: To Do or Not to Do. Front. Bioeng. Biotechnol. 2020, 8, 972. [Google Scholar] [CrossRef]
- Maugeri, G.; D’Agata, V.; Trovato, B.; Roggio, F.; Castorina, A.; Vecchio, M.; Di Rosa, M.; Musumeci, G. The role of exercise on peripheral nerve regeneration: From animal model to clinical application. Heliyon. 2021, 7, e08281. [Google Scholar] [CrossRef]
- Seddon, H.J. Three types of nerve injury. Brain. 1943, 66, 237. [Google Scholar] [CrossRef]
- Khaled, M.M.; Ibrahium, A.M.; Abdelgalil, A.I.; El-Saied, M.A.; El-Bably, S.H. Regenerative strategies in treatment of peripheral nerve injuries in different animal models. Tissue Eng Regen Med. 2023, 20, 839–877. [Google Scholar] [CrossRef]
- Zack-Williams, S.D.; Butler, P.E.; Kalaskar, D.M. Current progress in use of adipose derived stem cells in peripheral nerve regeneration. World J Stem Cells. 2015, 7, 51. [Google Scholar] [CrossRef]
- Al-Magsoosi, H.H.; Al-Bayati, H.S.; Al-Timmemi, H.A. immuno-hematological response to radial nerve injury and human umbilical cord-mesenchymal stem cells (Huc-MSCS) therapy in dogs. IRAQ Biochem Cell Arch. 2020, 20, 6447–6456. [Google Scholar]
- Modrak, M.; Talukder, M.A.; Gurgenashvili, K.; Noble, M.; Elfar, J.C. Peripheral nerve injury and myelination: potential therapeutic strategies. J Neurosci Res. 2020, 98, 780–795. [Google Scholar] [CrossRef]
- Campbell, W.W. Evaluation and management of peripheral nerve injury. Clin Neurophysiol 2008, 119, 1951–1965. [Google Scholar] [CrossRef] [PubMed]
- Missios, S.; Bekelis, K.; Spinner, R.J. Traumatic peripheral nerve injuries in children: epidemiology and socioeconomics. J Neurosurg Pediatr. 2014, 14, 688–694. [Google Scholar] [CrossRef] [PubMed]
- Javeed, S.; Faraji, A.H.; Dy, C.; Ray, W.Z.; MacEwan, M.R. Application of electrical stimulation for peripheral nerve regeneration: Stimulation parameters and future horizons. Interdiscip. Neurosurg.: Adv. Tech. Case Manag. 2021, 24, 101117. [Google Scholar] [CrossRef]
- Hoke, A.; Brushart, T. Introduction to special issue: challenges and opportunities for regeneration in the peripheral nervous system, Exp. Neurol. 2010, 223, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Pestronk, A.; Drachman, D.B.; Griffin, J.W. Effects of aging on nerve sprouting and regeneration. Exp. Neurol. 1980, 70, 65–82. [Google Scholar] [CrossRef] [PubMed]
- Grinsell, D.; Keating, C.P. Peripheral nerve reconstruction after injury: a review of clinical and experimental therapies. Biomed Res Int. 2014, 698256. [Google Scholar] [CrossRef]
- Smith, J.W. Microsurgery of peripheral nerves. Plast Rec Surg. 1964, 33, 317–329. [Google Scholar] [CrossRef]
- Menorca, R.M.; Fussell, T.S.; Elfar, J. C. Peripheral nerve trauma: mechanisms of injury and recovery. Hand Clin. 2013, 29, 317–330. [Google Scholar] [CrossRef]
- Hussain, G.; Wang, J.; Rasul, A.; Anwar, H.; Qasim, M.; Zafar, S.; Aziz, N.; Razzaq, A.; Hussain, R.; Aguilar, J.; et al. Current status of therapeutic approaches against peripheral nerve injuries: a detailed story from injury to recovery. Intern J Bio Sci. 2020, 16, 116–134. [Google Scholar] [CrossRef] [PubMed]
- Houschyar, K.S.; Momeni, A.; Pyles, M.N.; Cha, J.Y.; Maan, Z.N.; Duscher, D.; Jew, O.S.; Siemers, F.; Schoonhoven, J. The role of current techniques and concepts in peripheral nerve repair. Plastic Surg Intern. 2016, 4175293. [Google Scholar] [CrossRef] [PubMed]
- De Albornoz, P.M.; Delgado, P.J.; Forriol, F.; Maffulli, N. Non-surgical therapies for peripheral nerve injury. Br. Med. Bull. 2011, 100, 73–100. [Google Scholar] [CrossRef]
- Noble J, Munro CA, Prasad VS, Midha R. Analysis of upper and lower extremity peripheral nerve injuries in a population of patients with multiple injuries. J Trauma. 1998, 45, 116–122. [CrossRef]
- Sunderland, S. The anatomy and physiology of nerve injury. Muscle Nerve. 1990, 13, 771–784. [Google Scholar] [CrossRef]
- Post. R.; de Boer, K.S.; Malessy, M.J. Outcome following nerve repair of high isolated clean sharp injuries of the ulnar nerve. PLoS One 2012, 7, e47928.
- Jiang, L.; Jones, S.; Jia, X. Stem cell transplantation for peripheral nerve regeneration: current options and opportunities. Int J Mol Sci. 2017, 18, 94. [Google Scholar] [CrossRef] [PubMed]
- Burnett, M.G.; Zager, E.L. Pathophysiology of peripheral nerve injury: a brief review. Neurosurg Focus. 2004, 16, E1. [Google Scholar] [CrossRef]
- Takahashi, K.; Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006, 126, 663–676. [Google Scholar] [CrossRef]
- Chiaramonte, R.; Pavone, V.; Testa, G.; Pesce, I.; Scaturro, D.; Musumeci, G.; Mauro, G.; Vecchio, M. The role of physical exercise and rehabilitative implication in the process of nerve repair in peripheral neuropathies: a systematic review. Diagnostics (Basel). 2023, 13, 364. [Google Scholar] [CrossRef]
- Marqueste, T.; Alliez, J.-R.; Alluin, O.; Jammes, Y.; Decherchi, P. Neuromuscular rehabilitation by treadmill running or electrical stimulation after peripheral nerve injury and repair. J. Appl. Physiol. 2004, 96, 1988–1995. [Google Scholar] [CrossRef]
- Asensio-Pinilla, E.; Udina, E.; Jaramillo, J.; Navarro, X. Electrical stimulation combined with exercise increase axonal regeneration after peripheral nerve injury. Exp. Neurol. 2009, 219, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Liao, C.-F.; Yang, T.-Y.; Chen, Y.-H.; Yao, C.-H.; Way, T.-D.; Chen, Y.-S. Effects of swimming exercise on nerve regeneration in a rat sciatic nerve transection model. Biomed. Pharmacother. 2017, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Boeltz, T.; Ireland, M.; Mathis, K.; Nicolini, J.; Poplavski, K.; Rose, S.J.; Wilson, E.; English, A.W. Effects of treadmill training on functional recovery following peripheral nerve injury in rats. J. Neurophysiol. 2013, 109, 2645–2657. [Google Scholar] [CrossRef]
- Kim, H.K.W.; Kerr, R.G.; Turley, C.B.; Evans, P.J.; Jay, V.; Salter, R.B. The Effects of Postoperative Continuous Passive Motion on Peripheral Nerve Repair and Regeneration. J. Hand Surg. 1998, 23, 594–597. [Google Scholar] [CrossRef] [PubMed]
- van Meeteren, N.L.; Brakkee, J.H.; Hamers, F.P.; Helders, P.J.; Gispen, W.H. Exercise training improves functional recovery and motor nerve conduction velocity after sciatic nerve crush lesion in the rat. Arch. Phys. Med. Rehabilitation. 1997, 78, 70–77. [Google Scholar] [CrossRef]
- Huang, J.; Lu, L.; Zhang, J.; Hu, X.; Zhang, Y.; Liang, W.; Wu, S.; Luo, Z. Electrical Stimulation to Conductive Scaffold Promotes Axonal Regeneration and Remyelination in a Rat Model of Large Nerve Defect. PLoS ONE. 2012, 7, e39526. [Google Scholar] [CrossRef] [PubMed]
- Kao, C.-H.; Chen, J.-J.J.; Hsu, Y.-M.; Bau, D.-T.; Yao, C.-H.; Chen, Y.-S. High-Frequency Electrical Stimulation Can Be a Comple- mentary Therapy to Promote Nerve Regeneration in Diabetic Rats. PLoS ONE. 2013, 8, e79078. [Google Scholar] [CrossRef]
- Udina, E.; Puigdemasa, A.; Navarro, X. Passive and active exercise improve regeneration and muscle reinnervation after peripheral nerve injury in the rat. Muscle Nerve. 2011, 43, 500–509. [Google Scholar] [CrossRef]
- Cobianchi, S.; Marinelli, S.; Florenzano, F.; Pavone, F.; Luvisetto, S. Short- but not long-lasting treadmill running reduces allodynia and improves functional recovery after peripheral nerve injury. Neuroscience. 2010, 168, 273–287. [Google Scholar] [CrossRef]
- Cobianchi, S.; de Cruz, J.; Navarro, X. Assessment of sensory thresholds and nociceptive fiber growth after sciatic nerve injury reveals the differential contribution of collateral reinnervation and nerve regeneration to neuropathic pain. Exp. Neurol. 2014, 255, 1–11. [Google Scholar] [CrossRef]
- Herbison, G.J.; Jaweed, M.M.; Ditunno, J.F. Electrical stimulation of sciatic nerve of rats after partial denervation of soleus muscle. Arch. Phys. Med. Rehabilitation. 1986, 67, 79–83. [Google Scholar] [CrossRef]
- Jaweed, M.; Herbison, G.J.; Ditunno, J.F. Direct electrical stimulation of rat soleus during denervation-reinnervation. Exp. Neurol. 1982, 75, 589–599. [Google Scholar] [CrossRef]
- Marqueste, T.; Decherchi, P.; Desplanches, D.; Favier, R.; Grelot, L.; Jammes, Y. Chronic electrostimulation after nerve repair by self-anastomosis: Effects on the size, the mechanical, histochemical and biochemical muscle properties. Acta Neuropathol. 2006, 111, 589–600. [Google Scholar] [CrossRef]
- Michel, R.N.; Gardiner, P.F. Influence of overload on recovery of rat plantaris from partial denervation. J. Appl. Physiol. 1989, 66, 732–740. [Google Scholar] [CrossRef] [PubMed]
- Eisen, A.A.; Carpenter, S.; Karpati, G.; Bellavance, A. The effect of muscle hyper- and hypoactivity upon fibre diameters of intact and regenerating nerves. J. Neurol. Sci. 1973, 20, 457–469. [Google Scholar] [CrossRef] [PubMed]
- Herbison, G.J.; Jaweed, M.; Ditunno, J.F.; Scott, C.M. Effect of overwork during reinnervation of rat muscle. Exp. Neurol. 1973, 41, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Herbison, G.J.; Jaweed, M.M.; Ditunno, J.F. Effect of swimming on reinnervation of rat skeletal muscle. J. Neurol. Neurosurg. Psychiatry. 1974, 37, 1247–1251. [Google Scholar] [CrossRef] [PubMed]
- Sobral, L.L.; Oliviera, L.S.; Takeda, S.Y.M.; Somazz, M.C.; Montebelo, M.I.L.; Teodori, R.M. Immediate versus later exercises for rat sciatic nerve regeneration after axonotmesis: Histomorphometric and functional analyses. Rev. Bras. Fisioter. 2008, 12, 311–316. [Google Scholar] [CrossRef]
- Teodori, R.M.; Betini, J.; de Oliveira, L.S.; Sobral, L.L.; Takeda, S.Y.M.; Montebelo, M.I.D.L. Swimming Exercise in the Acute or Late Phase after Sciatic Nerve Crush Accelerates Nerve Regeneration. Neural Plast. 2011, 783901. [Google Scholar] [CrossRef]
- Skouras, E.; Merkel, D.; Grosheva, M.; Angelova, S.K.; Schiffer, G.; Thelen, U.; Kaidoglou, K.; Sinis, N.; Igelmund, P.; Dunlop, S.A.; et al. Manual stimulation, but not acute electrical stimulation prior to reconstructive surgery, improves functional recovery after facial nerve injury in rats. Restor. Neurol. Neurosci. 2009, 27, 237–251. [Google Scholar] [CrossRef]
- Costa, L.M.; Simões, M.J.; Maurício, A.C.; Varejão, A.S. Methods and protocols in peripheral nerve regeneration experimental research: part IV - Kinematic gait analysis to quantify peripheral nerve regeneration in the rat. Int Rev Neurobiol. 2009, 87, 127–139. [Google Scholar]
- Bozkurt, A.; Deumens, R.; ScheVel, J.; O’Dey, D. M.; Weis, J.; Joosten, E. A.; Fu ̈hrmann, T.; Brook, G. A.; Pallua, N. CatWalk gait analysis in assessment of functional recovery after sciatic nerve injury. J. Neurosci. Methods. 2008, 173, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Schweizer, R.; Schnider J.T.; Fanzio, P.M.; Tsuji, W.; Kostereva, N.; Solari, M.G. Plock, J.A.; Gorantla, V.S. Effect of systemic adipose-derived stem cell therapy on functional nerve regeneration in a rodent model. PRS Global Open. 2020, 1-10. [CrossRef]
- Targosinksi, S.; Henzi, A.; Engmann, A.K.; Rushing, E.J.; Barth, A.A.; Klein, H.J.; Kim, B.; Giovanoli, P. Schwab, M.E.; Plock, J.A., et al. A swim test for functional assessment of rodent peripheral nerve regeneration. J Neurosci Met. 2022, 379, 109663.
- Senger, J.B.; Rabey, K.N.; Morhart, M.J.; Chan, K.M.; Webber, C.A. Conditioning electrical stimulation accelerates regeneration in nerve transfers. Ann Neurol. 2020, 88, 363–374. [Google Scholar] [CrossRef] [PubMed]
- Molteni, R.; Zheng, J.-Q.; Ying, Z.; Gomez-Pinilla, F.; Twiss, J.L. Voluntary exercise increases axonal regeneration from sensory neurons. Proc. Natl. Acad. Sci. USA. 2004, 101, 8473–8478. [Google Scholar] [CrossRef]
- Al-Majed, A.; Brushart, T.M.; Gordon, T. Electrical stimulation accelerates and increases expression of BDNF and trkB mRNA in regenerating rat femoral motoneurons. Eur. J. Neurosci. 2000, 12, 4381–4390. [Google Scholar] [CrossRef]
- English, A.W.; Schwartz, G.; Meador, W.; Sabatier, M.J.; Mulligan, A. Electrical stimulation promotes peripheral axon regeneration by enhanced neuronal neurotrophin signaling. Dev. Neurobiol. 2007, 67, 158–172. [Google Scholar] [CrossRef]
- Martins, D.F.; Mazzardo-Martins, L.; Gadotti, V.M.; Nascimento, F.P.; Lima, D.A.; Speckhann, B.; Favretto, G.A.; Bobinski, F.; Cargnin-Ferreira, E.; Bressan, E.; et al. Ankle joint mobilization reduces axonotmesis-induced neuropathic pain and glial activation in the spinal cord and enhances nerve regeneration in rats. Pain. 2011, 152, 2653–2661. [Google Scholar] [CrossRef] [PubMed]
- Ying, Z.; Roy, R.R.; Edgerton, V.; Gómez-Pinilla, F. Voluntary exercise increases neurotrophin-3 and its receptor TrkC in the spinal cord. Brain Res. 2003, 987, 93–99. [Google Scholar] [CrossRef]
- Seo, T.B.; Oh, M.-J.; You, B.-G.; Kwon, K.-B.; Chang, I.-A.; Yoon, J.-H.; Lee, C.Y.; Namgung, U. ERK1/2-Mediated Schwann Cell Proliferation in the Regenerating Sciatic Nerve by Treadmill Training. J. Neurotrauma. 2009, 26, 1733–1744. [Google Scholar] [CrossRef] [PubMed]
- Ahlborn, P.; Schachner, M.; Irintchev, A. One hour electrical stimulation accelerates functional recovery after femoral nerve repair. Exp. Neurol. 2007, 208, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Pinilla, F.; Ying, Z.; Roy, R.R.; Molteni, R.; Edgerton, V.R. Voluntary Exercise Induces a BDNF-Mediated Mechanism That Promotes Neuroplasticity. J. Neurophysiol. 2002, 88, 2187–2195. [Google Scholar] [CrossRef] [PubMed]
- Troupel, T.; Caenegem, N.V.; Jeandel, A.; Thibaud, J.; Nicolle, A.; Blot, S. Epidemiological, clinical, and electrophysiological findings in dogs and cats with traumatic brachial plexus injury: a retrospectove study of 226 cases. J Vet Intern Med. 2021, 35, 2837–2845. [Google Scholar] [CrossRef]
- Griffiths, I.R.; Duncan, I.D.; Lawson, D.D. Avulsion of the brachial plexus-2. Clinical aspects. J Small Anim Pract. 1974, 15, 177–183. [Google Scholar] [CrossRef]
- Wood, M.D.; Kemp, S.W.; Weber, C.; Borschel, G.H.; Gordon, T. Outcome measures of peripheral nerve regeneration. Annals of Anatomy. 2011, 193, 321–333. [Google Scholar] [CrossRef]
- Belviso, I.; Palermi, S.; Sacco, A.M.; Romano, V.; Corrado, B.; Zappia, M.; Sirico, F. Brachial plexus injuries in sport medicine: Clinical evaluation, diagnostic approaches, treatment options and rehabilitative interventions. J Funct Morphol Kinesiol. 2020, 5, 22. [Google Scholar] [CrossRef]
- Preston, D.C.; Shapiro, B.E. Needle electromyography. Fundamentals, normal and abnormal patterns. Neurol. Clin. 2002, 20, 361–396. [Google Scholar] [CrossRef]
- Anson, A.; Gil, F.; Laredo, F.G.; Soler, M.; Belda, E.; Ayala, M.D.; Agut, A. Correlative ultrasound anatomy of the feline brachial plexus and major nerves of the thoracic limb. Vet Radiol Ultrasound. 2013, 54, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Benecke, R.; Berthold, A.; Conrad, B. Denervation activity in the EMG of patients with upper motor neuron lesions: Time course, local distribution and pathogenetic aspects. J. Neurol. 1983, 230, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Effron, C.R.; Beasley, R.W. Compression neuropathies in the upper limb and electrophysiological studies. In Grabb and Smith’s Plastic Surgery. Thorne, C.H., Bartlett, S.P., Beasley, R.W., Aston, S.J., Gurtner, G.C., Spear, S.L., eds. Philadelphia, USA: Lippincott Williams & Wilkins; 2006, pp. 86.
- Robinson, L.R. Traumatic injury to peripheral nerves. Muscle Nerve. 2000, 23, 863–87. [Google Scholar] [CrossRef]
- Teixeira, M.J.; da Paz, M.G.D.S.; Bina, M.T.; Santos, S.N.; Raicher, I.; Galhardoni, R.; Fernandes, D.T.; Yeng, L.T.; Baptista, A.F.; de Andrade, D.C. Neuropathic pain after brachial plexus avulsion-central and peripheral mechanisms. BMC Neurol. 2015, 15, 73. [Google Scholar] [CrossRef] [PubMed]
- Sadosky, A.; McDermott, A. A review of the epidemiology of painful diabetic peripheral neuropathy, postherpetic neuralgia, and less commonly studied neuropathic pain conditions. Pain Practice. 2008, 8, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Flor, H., Nikolajsen, L., Staehelin, T. Phantom limb pain: a case of maladaptive CNS plasticity? Nature reviews. Neuroscience. 2006, 7, 873–81.
- Flor, H.; Elbert, T.; Knecht, S.; Wienbruch, C.; Pantev, C.; Birbaumer, N.; et al. Phantom-limb pain as a perceptual correlate of cortical reorganization following arm amputation. Nature 1995, 375, 482–4. [Google Scholar] [CrossRef]
- Flor, H.; Nikolajsen, L.; Staehelin Jensen, T. Phantom limb pain: A case of maladaptive CNS plasticity? Nat. Rev. Neurosci. 2006, 7, 873–881. [Google Scholar] [CrossRef]
- Menchetti, M.; Gandini, G.; Gallucci, A.; Della Rocca, G.; Matiasek, L.; Matiasek, K.; Gentilini, F.; Rosati, M. Approaching phantom complex after limb amputation in the canine species. J. Vet. Behav. 2017, 22, 24–28. [Google Scholar] [CrossRef]
- Melzack, R. Phantom limbs. Scientific American. 1992, 90–6. [Google Scholar] [CrossRef]
- Ehde. D.M.; Czerniecki, J.M.; Smith, D.G.; Campbell, K.M.; Edwards, W.T.; Jensen, M.P. et al. Chronic phantom sensations, phantom pain, residual limb pain, and other regional pain after lower limb amputation. Arch Phys Med Rehabil. 2000, 81, 1039–44.
- Probstner, D.; Thuler, L.C.; Ishikawa, N.M.; Alvarenga, R.M. Phantom limb phenomena in cancer amputees. Pain Pract. 2010, 10, 249–256. [Google Scholar] [CrossRef]
- Varejão, A.S.P.; Cabrita, A.M.; Geuna, S.; Melo-Pinto, P.; Filipe, V.M.; Gramsbergen, A.; Meek, M.F. Toe out angle: a functional index for the evaluation of sciatic nerve recovery in the rat model. Exp Neurol. 2003, 183. [Google Scholar] [CrossRef]
- M. Vivo ́, A.; Puigdemasa, L.; Casals, E.; Asensio, E.: Udina, X. Navarro, Immediate electrical stimulation enhances regeneration and reinnervation and modulates spinal plastic changes after sciatic nerve injury and repair. Exp. Neurol. 2008, 211, 180–193.
- Woolf, C.J. Evidence for a central component of post-injury pain hypersensitivity. Nature. 1983, 306, 686–688. [Google Scholar] [CrossRef]
- Finnerup, N.B.; Kuner, R.; Jensen, T.S. Neuropathic pain: from mechanisms to treatment. Physiol Rev. 2021, 101, 259–301. [Google Scholar] [CrossRef] [PubMed]
- Campero, M.; Serra, J.; Marchettini, P.; Ochoa, J.L. Ectopic impulse generation and autoex-citation in single myelinated afferent fibers in patients with peripheral neuropathy andpositive sensory symptoms. Muscle Nerve. 1998, 21, 1661–1667. [Google Scholar] [CrossRef]
- Nordin, M.; Nyström, B.; Wallin, U.; Hagbarth, K.E. Ectopic sensory discharges and pares-thesiae in patients with disorders of peripheral nerves, dorsal roots and dorsal col-umns. Pain. 1984, 20, 231–245. [Google Scholar] [CrossRef] [PubMed]
- Ochoa, J.; Torebjörk, E. Sensations evoked by intraneural microstimulation of C noci-ceptor fibres in human skin nerves. JPhysiol. 1989, 415, 583–599. [Google Scholar]
- Gonçalves, N.P.; Vægter, C.B.; Andersen, H.; Østergaard, L.; Calcutt, N.A. , Jensen, T.S.Schwann cell interactions with axons and microvessels in diabetic neuropathy. Nat RevNeurol. 2017, 13, 135–147. [Google Scholar]
- De Logu, F.; Li Puma, S.; Landini, L.; Portelli, F.; Innocenti, A.; de Araujo, D.S.M.; Janal, M.N.; Patacchini, R.; Bunnett, N.W.; Geppetti, P.; Nassini, R. Schwann cells expressing nociceptivechannel TRPA1 orchestrate ethanol-evoked neuropathic pain in mice. J Clin Invest. 2019, 129, 5424–5441. [Google Scholar] [CrossRef]
- Salter, M.W.; Beggs, S. Sublime microglia: expanding roles for the guardians of the CNS. Cell. 2014, 158, 15–24. [Google Scholar] [CrossRef]
- Moore, S.A. Managing neuropathic pain in dogs. Front Vet Sci. 2016, 22, 3–12. [Google Scholar] [CrossRef]
- Carvalho, G.A.; Nikkhah, G.; Matthies, C.; Penkert, G.; Samii, M. Diagnosis of root avulsions in traumatic brachial plexus injuries: Value of computerized tomography myelography and magnetic resonance imaging. J. Neurosurg. 1997, 86, 69–76. [Google Scholar] [CrossRef]
- Smith, B.W.; Daunter, A.K.; Yang, L.J.S.; Wilson, T.J. An Update on the Management of Neonatal Brachial Plexus Palsy—Replacing Old Paradigms: A Review. JAMA Pediatr. 2018, 172, 585. [Google Scholar] [CrossRef]
- Rich, J.A.; Newell, A.; Williams, T. Traumatic brachial plexus injury rehabilitation using neuromuscular electrical muscle stimulation in a polytrauma patient. BMJ Case Rep. 2019, 12, e232107. [Google Scholar] [CrossRef]
- Abdel-Aziz, S.; Ghaleb, A.H. Cervical Spinal Cord Stimulation for the Management of Pain from Brachial Plexus Avulsion. Pain Med. 2014, 15, 712–714. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Liu, P.; Rui, J.; Zhao, X.; Lao, J. The clinical characteristics of neuropathic pain in patients with total brachial plexus avulsion: A 30-case study. Injury 2016, 47, 1719–1724. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Yuzhou, L.; Yingjie, Z.; Jie, L.; Xin, Z. A new rat model of neuropathic pain: Complete brachial plexus avulsion. Neurosci. Lett. 2015, 589, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, J.R.; Meek, M.; Robinson, P.H.; Gramsbergen, A. Methods to evaluate functional nerve recovery in adult rats: walking track analysis, video analysis and the withdrawal reflex. J Neurosci Met. 2000, 96, 89–96. [Google Scholar] [CrossRef]
- Meek, M.F.; Van Der Werff, J.F.A.; Nicolai, J.P.A.; Gramsbergen, A. Biodegradable p (DLLA-e-CL) Nerve guides versus autologous nerve grafts: electromyographic amd video analysis. Muscle & Nerve. 2001, 24, 753–759. [Google Scholar]
- Watson, N.C.; Jejurikar, S.; Kalliainen, L.K.; Calderon, M.S.; URbanchek, M.G.; Eguchi, T.; Kuzon, J.R. Range of motion physiotherapy reduces the force deficit in antagonists to denervated rat muscles. J Surg Res. 2001, 99, 156–160. [Google Scholar] [CrossRef]
- Du, Z.; Zhang, J.; Han, X.; Yu, W.; Gu, X. Potential novel therapeutic strategies for neuropathic pain. Front Mol Neurosci. 2023, 16, 1138798. [Google Scholar] [CrossRef]
- Chandrashekhar, R.; Wang, H.; Dionne, C.; James, S.; and Burzycki, J. Wearable focal muscle vibration on pain, balance, mobility, and sensation in individuals with diabetic peripheral neuropathy: a pilot study. Int. J. Environ. Res. Public Health. 2021, 18, 2415. [Google Scholar] [CrossRef]
- Heo, J.; Jo, J.; Lee, J.; Kang, H.; Choi, T.; Lee, M.; Kim, J. Electroacupuncture for the treatment of frozen shoulder. Medicine (Baltimore). 2021, 100, e28179. [Google Scholar] [CrossRef]
- Johnson, M. I.; Paley, C. A.; Jones, G.; Mulvey, M. R.; and Wittkopf, P. G. Efficacy and safety of transcutaneous electrical nerve stimulation (TENS) for acute and chronic pain in adults: a systematic review and meta-analysis of 381 studies (the meta-TENS study). BMJ Open. 2022, 12, e051073. [Google Scholar] [CrossRef]
- Martins, Â.; Gouveia, D.; Cardoso, A.; Viegas, I.; Gamboa, Ó.; Ferreira, A. A comparison between body weight-supported treadmill training and conventional over-ground training in dogs with incomplete spinal cord injury. Front Vet Sci. 2021, 8, 597949. [Google Scholar] [CrossRef]
- Lovaglio, A.; Socolovsky, M.; Di Masi, G.; Bonilla, G. Treatment of neuropathic pain after peripheral nerve and brachial plexus traumatic injury. Neurol. India. 2019, 67, 32. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, R.; Dailey, T.; Duncan, K.; Abel, N.; Borlongan, C.V. Peripheral Nerve Injury: Stem Cell Therapy and Peripheral Nerve Transfer. Int J Mol Sci. 2016, 17. [Google Scholar] [CrossRef] [PubMed]
- Blits, B.; Boer, G.J.; Verhaagen, J. Pharmacological, cell, and gene therapy strategies to promote spinal cord regeneration. Cell Transplant. 2002, 11, 593–613. [Google Scholar] [CrossRef] [PubMed]
- Faroni, A.; Mobasseri, S.A.; Kingham, P.J.; Reid, A.J. Peripheral nerve regeneration: experimental strategies and future perspectives. Adv Drug Deliv Rev. 2015, 82–83, 160–167.
- Magnaghi, V.; Procacci, P.; Tata, A.M. Chapter 15: Novel pharmacological approaches to Schwann cells as neuroprotective agents for peripheral nerve regeneration. Int Rev Neurobiol. 2009, 87, 295–315. [Google Scholar]
- Vijayavenkataraman, S. Nerve guide conduits for peripheral nerve injury repair: A review on design, materials and fabrication methods. Acta Biomater. 2020, 106, 54–69. [Google Scholar] [CrossRef] [PubMed]
- Raza, C.; Riaz, H.A.; Anjum, R.; Shakeel, N.U.A. Repair strategies for injured peripheral nerve: Review. Life Sci. 2020, 243, 117308. [Google Scholar] [CrossRef]
- Isvoranu, G.; Manole, E.; Neagu, M. Gait Analysis Using Animal Models of Peripheral Nerve and Spinal Cord Injuries. Biomedicines. 2021, 9, 1050. [Google Scholar] [CrossRef] [PubMed]
- Leite, A.P.S.; Pinto, C.G.; Tiburcio, F.C.; Sartori, A.A.; de Castro Rodrigues, A.; Barraviera, B.; Ferreira, R.S.J.; Filadelpho, A.L.; Matheus, S.M.M. Heterologous fibrin sealant potentiates axonal regeneration after peripheral nerve injury with reduction in the number of suture points. Injury. 2019, 50, 834–847. [Google Scholar] [CrossRef]
- Morris, M.; Brogan, D.M.; Boyer, M.I.; Dy, C.J. Trends in nerve transfer procedures among board-eligible orthopedic hand surgeons. J Hand Surg Global. 2021, 3, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, J.; Mackinnon, S.E.; Watanabe, O.; et al. The effect of duration of muscle denervation on functional recovery in the rat model. Muscle Nerve. 1997, 1997. 20, 858e866. [Google Scholar] [CrossRef]
- Brown, J.M.; Tung, T.H.; Mackinnon, S.E. Median to radial nerve transfer to restore wrist and finger extension: technical nuances. Neurosurgery. 2010, 66(3 Suppl Operative), 75e83. [Google Scholar] [CrossRef]
- Mackinnon, S.E.; Roque, B.; Tung, T.H. Median to radial nerve transfer for treatment of radial nerve palsy: case report. J Neurosurg. 2007, 107, 666e671. [Google Scholar] [CrossRef]
- Dy, C.J.; Aunins, B.; Brogan, D.M. Barriers to epineural scarring: role in treatment of traumatic nerve injury and chronic compressive neuropathy. J Hand Surg Am. 2018, 43, 360–367. [Google Scholar] [CrossRef]
- Kokkalis, Z.T.; Mavrogenis, A.F.; Ballas, E.G.; Papagelopoulos, P.J.; Soucacos, P.N. Collagen nerve wrap for median nerve scarring. Orthopedics. 2015, 38, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Soltani, A.M.; Allan, B.J.; Best, M.J.; Mir, H.S.; Panthaki, Z.J. Revision decompression and collagen nerve wrap for recurrent and persistent compression neuropathies of the upper extremity. Ann Plast Surg. 2014, 72, 572–578. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, L.; Adam, C.; Legagneux, J.; Bruneval, P.; Masmejean, E. Reduction of neural scarring after peripheral nerve suture: an experimental study about collagen membrane and autologous vein wrapping. Chir Main. 2012, 31, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Papatheodorou, L.K.; Williams, B.G.; Sotereanos, D.G. Preliminary results of recurrent cubital tunnel syndrome treated with neurolysis and porcine extracellular matrix nerve wrap. J Hand Surg Am. 2015, 40, 987–992. [Google Scholar] [CrossRef] [PubMed]
- Magill, C.K.; Tuffaha, S.H.; Yee, A.; et al. The short- and long-term effects of Seprafilm on peripheral nerves: a histological and functional study. J Reconstr Microsurg. 2009, 25, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Ozgenel, G.Y.; Filiz, G. Effects of human amniotic fluid on peripheral nerve scarring and regeneration in rats. J Neurosurg. 2003, 98, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Gaspar, M.P.; Abdelfattah, H.M.; Welch, I.W.; Vosbikian, M.M.; Kane, P.M.; Rekant, M.S. Recurrent cubital tunnel syndrome treated with revision neurolysis and amniotic membrane nerve wrapping. J Shoulder Elbow Surg. 2016, 25, 2057–2065. [Google Scholar] [CrossRef]
- Liu, T.; Xu, J.; Pan, X.; Ding, Z.; Xie, H.; Wang, X.; Xie, H. Advances of adipose-derived mesenchymal stem cells-based biomaterial scaffolds for oral and maxillofacial tissue engineering. Bioact Mater. 2021, 6, 2467–2478. [Google Scholar] [CrossRef]
- Zorko, B.; Rozman, J.; Seliškar, A. Influence of electrical stimulation on regeneration of the radial nerve in dogs. Acta Vet. Hung. 2000, 48, 99–105. [Google Scholar] [CrossRef]
- Foecking, E.M.; Fargo, K.N.; Coughlin, L.M.; Kim, J.M.; Sam, J.; Jones, K.J. Crush Injury Enhances Functional Recovery of Rat Facial Nerve, 2012, 49, pp. 451–458.
- Brushart, T.M.; Hoffman, P.N.; Royall, R.M.; Murinson, B.B.; Witzel, T. Gordon Electrical stimulation promotes motoneuron regeneration without increasing its speed or conditioning the neuron. J Neurosci. 2002, 22, 6631–6638. [Google Scholar] [CrossRef]
- Geremia, N.M.; Gordon, T.; Brushart, T.M.; Al-Majed, A.A.; Verge, V.M.K. Electrical stimulation promotes sensory neuron regeneration and growth-associated gene expression. Exp Neurol. 2007, 205, 347–359. [Google Scholar] [CrossRef]
- Huang, J.; Lu, L.; Hu, X.; Ye, Z.; Peng, Y.; Yan, X.;Geng, D.; Luo, Z. Electrical stimulation accelerates motor functional recovery in the rat model of 15-mm sciatic nerve gap bridged by scaffolds with longitudinally oriented microchannels, Neurorehabil Neural Repair. 2010, 24, 736–745.
- Ni, L.; Yao, Z.; Zhao, Y.; Zhang, T.; Wang, J; Li, S.; Chen, Z. Electrical stimulation therapy for peripheral nerve injury. Front Neurol. 2023, 14, 1–13.
- Huang, J.; Zhang, Y.; Lu, L.; Hu, X.; Luo, Z. Electrical stimulation accelerates nerve regeneration and functional recovery in delayed peripheral nerve injury in rats. Eur J Neurosci. 2013, 38, 3691–701. [Google Scholar] [CrossRef]
- Song, S.; McConnell, K.W.; Amores, D.; Levinson, A.; Vogel, H.; Quarta, M.; et al. Electrical stimulation of human neural stem cells via conductive polymer nerve guides enhances peripheral nerve recovery. Biomaterials. 2021, 275, 120982. [Google Scholar] [CrossRef]
- Cobianchi, S.; Casals-Diaz, L.; Jaramillo, J.; Navarro, X. Differential effects of activity dependent treatments on axonal regeneration and neuropathic pain after peripheral nerve injury. Exp Neurol. 2013, 240, 157–67. [Google Scholar] [CrossRef]
- Al-Majed, A.A.; Tam, S.L.; Gordon, T. Electrical stimulation accelerates and enhances expression of regeneration-associated genes in regenerating rat femoral motoneurons. Cell Mol Neurobiol. 2004, 24, 379–402. [Google Scholar] [CrossRef] [PubMed]
- Eberhardt, K.A.; Irintchev, A.; Al-Majed, A.A.; Simova, O.; Brushart, T.M.; Gordon, T, et al.. BDNF/TrkB signaling regulates HNK-1 carbohydrate expression in regenerating motor nerves and promotes functional recovery after peripheral nerve repair. Exp Neurol. 2006, 198, 500–10.
- Batty, N.J.; Torres-Espín, A.; Vavrek, R.; Raposo, P.; Fouad, K. Single-session cortical electrical stimulation enhances the efficacy of rehabilitative motor training after spinal cord injury in rats. Exp Neurol. 2020, 324, 113136. [Google Scholar] [CrossRef] [PubMed]
- Martins, A.; Gouveia, D.; Cardoso, A.; Gamboa, Ó.; Millis, D.; Ferreira, A. Nervous system modulation through electrical stimulation in companion animals. Acta Vet Scand. 2021, 63, 22. [Google Scholar] [CrossRef]
- Boyd, J.G.; Gordon, T. Neurotrophic factors and their receptors in axonal regeneration and functional recovery after peripheral nerve injury, Mol Neurobiol. 2003, 27, 277–324.
- Lu, B.; Pang, P.T.; Woo, N.H. The yin and yang of neurotrophin action. Nat Rev Neurosci. 2005, 6, 603–614. [Google Scholar] [CrossRef]
- Richner, M.; Ulrichsen, M.; Elmegaard, S.L.; Dieu, R.; Pallesen, L.T.; Vaegter, C.B. Peripheral nerve injury modulates neurotrophin signaling in the peripheral and central nervous system. Mol Neurobiol. 2014, 50, 945–970. [Google Scholar] [CrossRef]
- Gordon, T. Electrical Stimulation to Enhance Axon Regeneration After Peripheral Nerve Injuries in Animal Models and Humans. Neurotherapeutics. 2016, 13, 295–310. [Google Scholar] [CrossRef]
- Dow, D.E.; Dennis, R.G.; Faulkner, J.A. Electrical stimulation attenuates denervation and age-related atrophy in extensor digitorum longus muscles of old rats. J Gerontol A Biol Sci Med Sci. 2005, 60, 416–424. [Google Scholar] [CrossRef] [PubMed]
- Eberstein, A.; Eberstein, S. Electrical stimulation of denervated muscle: is it worthwhile? Med Sci Sports Exerc. 1996, 28, 1463–1469. [Google Scholar] [CrossRef] [PubMed]
- Brushart, T.M.; Jari, R.; Verge, V.; Rohde, C.; Gordon, T. Electrical stimulation restores the specificity of sensory axon regeneration. Exp. Neurol. 2005, 194, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Tam, S.L.; Archibald, V.; Jassar, B.; Tyreman, N.; Gordon, T. Increased Neuromuscular Activity Reduces Sprouting in Partially Denervated Muscles. J. Neurosci. 2001, 21, 654–667. [Google Scholar] [CrossRef] [PubMed]
- Love, F.M.; Son, Y.-J.; Thompson, W.J. Activity alters muscle reinnervation and terminal sprouting by reducing the number of schwann cell pathways that grow to link synaptic sites. J. Neurobiol. 2003, 54, 566–576. [Google Scholar] [CrossRef] [PubMed]
- Alvites, R.; Rita Caseiro, A.; Santos Pedrosa, S.; Vieira Branquinho, M.; Ronchi, G.; Geuna, S.; Varejão, A.S.P.; Colette Maurício, A.; Spurkland, A. Peripheral nerve injury and axonotmesis: State of the art and recent advances. Cogent. Med. 2018, 5, 1466404. [Google Scholar] [CrossRef]
- Bula-Oyola, E.; Belda-Lois, J.; Porcar-Seder, R.; Page, A. Effectiveness of electrophysical modalities in the sensorimotor rehabilitation of radial, ulnar, and median neuropathies: A meta-analysis. Plos One. 2021, 0248484. [Google Scholar] [CrossRef]
- Colbert, A.P.; Markov, M.S.; Carlson, N.; Gregory, W.L.; Carlson, H.; Elmer, P.J. Static Magnetic Field Therapy for Carpal Tunnel Syndrome: A Feasibility Study. Arch Phys Med Rehabil. 2010, 91, 1098–104. [Google Scholar] [CrossRef]
- Ozkan, F.U.; Saygı, E.K.; Senol, S.; Kapcı, S.; Aydeniz, B.; Aktaş, İ.; et al. New treatment alternatives in the ulnar neuropathy at the elbow: ultrasound and low-level laser therapy. Acta Neurol Belg. 2015, 115, 355–60. [Google Scholar] [CrossRef]
- Bilgin Badur, N.; Unlu Ozkan, F.; Aktas, I. Efficacy of shortwave diathermy in ulnar nerve entrapment at the elbow: a double-blind randomized controlled clinical trial. Clin Rehabil. 2020, 34, 1048–55. [Google Scholar] [CrossRef] [PubMed]
- Oshima, C.; Nakazawa, H.; Izukura, H.; Miyagi, M.; Mizutani, A.; Harada, T.; et al. Low Level Laser Therapy for Radial Nerve Palsy Patients: Our Experience. LASER Ther. 2018, 27, 56–60. [Google Scholar] [CrossRef]
- Kim, J.K.; Jeon, S.H. Minimal clinically important differences in the Carpal Tunnel Questionnaire after carpal tunnel release. J Hand Surg. 2013, 38, 75–9. [Google Scholar] [CrossRef]
- Gunter, C.; Delbeke, J.; Ortiz-Catalan, M. Safety of long-term electrical peripheral nerve stimulation: review of the state of the art. J NeuroEng Rehab. 2019, 16. [Google Scholar] [CrossRef] [PubMed]
- Agnew, W.F.; McCreery, D.B. Considerations for safety with chronically implanted nerve electrodes. Epilepsia. 1990, 31, S27–32. [Google Scholar] [CrossRef] [PubMed]
- McCreery, D.B.; Agnew, W.F.; Yuen, T.G.H. Bullara, L.A. Relationship between stimulus amplitude, stimulus frequency and neural damage during electrical stimulation of sciatic nerve of cat. Med Biol Eng Comput. 1995, 33, 426–9. [Google Scholar] [CrossRef]
- Waters, R.L.; McNeal, D.R.; Faloon, W. Clifford B. Functional electrical stimulation of the peroneal nerve for hemiplegia. Long-term clinical follow-up. J Bone Jt Surg. 1985, 67, 792–3. [Google Scholar] [CrossRef]
- Agnew, W.F.; McCreery, D.B.; Yuen, T.G.H.; Bullara, L.A. Histologic and physiologic evaluation of electrically stimulated peripheral nerve: considerations for the selection of parameters. Ann Biomed Eng. 1989, 17, 39–60. [Google Scholar] [CrossRef] [PubMed]
- Hasiba-Pappas, S.; Kamolz, L.; Luze, H.; Nischwitz, S.; Holzer-Geissler, J.; Tuca, A.; Rienmuller, T.; Polz, M.; Ziesel, D.; Winter, R. Does electrical stimulation through nerve conduits improve peripheral nerve regeneration? – A systematic review. J Pers Med. 2023, 13, 414. [Google Scholar] [CrossRef] [PubMed]
- Kubiak, C.A.; Kung, T.A.; Brown, D.L.; Cederna, P.S.; Kemp, S.W.P. State-of-The-Art techniques in treating peripheral nerve injury. Plast. Reconstr. Surg. 2018, 141, 702–710. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.M.; Curran, M.W.T.; Gordon, T. Neuroscience The use of brief post-surgical low frequency electrical stimulation to enhance nerve regeneration in clinical practice. J. Physiol. 2016, 594, 3553–3559. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.C.; Kao, C.H.; Chen, C.C.; Ke, C.J.; Yao, C.H.; Chen, Y.S. Time-course effect of electrical stimulation on nerve regeneration of diabetic rats. PLoS ONE. 2015, 10, e0116711. [Google Scholar] [CrossRef]
- Song, J.; Sun, B.; Liu, S.; Chen, W.; Zhang, Y.; Wang, C.; Mo, X.; Che, J.; Ouyang, Y.; Yuan, W.; et al. Polymerizing pyrrole coated poly (l-lactic acid-co-ε-caprolactone) (PLCL) conductive nanofibrous conduit combined with electric stimulation for long-range peripheral nerve regeneration. Front. Mol. Neurosci. 2016, 9, 117. [Google Scholar] [CrossRef]
- Dorrian, RM.; Berryman, C.F.; Lauto, A.; Leonard, A.V. Electrical stimulation for the treatment of spinal cord injuries: a review of the cellular and molecular mechanisms that drive functional improvements. Front Cell Neurosci. 2023, 17, 1095259. [Google Scholar] [CrossRef]
- Griffin, L.; Decker, M. J.; Hwang, J. Y.; Wang, B.; Kitchen, K.; Ding, Z. , et al. Functional electrical stimulation cycling improves body composition, metabolic and neural factors in persons with spinal cord injury. J. Electromyogr. Kinesiol. 2009, 19, 614–622. [Google Scholar]
- Bakkum, A. J.; Paulson, T. A.; Bishop, N. C.; Goosey-Tolfrey, V. L.; Stolwijk-Swüste, J. M.; van Kuppevelt, D. J. et al. Effects of hybrid cycle and handcycle exercise on cardiovascular disease risk factors in people with spinal cord injury: A randomized controlled trial. J. Rehabil. Med. 2015, 47, 523–530.
- Ayanwuyi, L.; Tokarska, N.; McLean, N. A.; Johnston, J. M.; Verge, V. M. K. Brief electrical nerve stimulation enhances intrinsic repair capacity of the focally demyelinated central nervous system. Neural Regen. Res. 2022, 17, 1042–1050. [Google Scholar] [PubMed]
- Hahm, S.-C.; Yoon, Y. W.; Kim J. High-Frequency transcutaneous electrical nerve stimulation alleviates spasticity after spinal contusion by inhibiting activated microglia in rats. Neurorehabil. Neural Rep. 2014, 29, 370–381.
- Chu, X.; Song, X.; Li, Q.; Li, Y.; He, F.; Gu, X.; Ming, D. Basic mechanisms of peripheral nerve injury and treatment via electrical stimulation. Neural Regen Res. 2022, 17, 2185–2193. [Google Scholar] [PubMed]
- Martins, D.F.; Martins, T.C.; Batisti, A.P.; Leonel, L.D.S.; Bobinski, F.; Belmonte, L.A.O.; Mazzardo-Martins, L.; Cargnin-Ferreira, E.; Santos, A.R.S. Long-Term Regular Eccentric Exercise Decreases Neuropathic Pain-like Behavior and Improves Motor Functional Recovery in an Axonotmesis Mouse Model: The Role of Insulin-like Growth Factor-1. Mol. Neurobiol. 2017, 55, 6155–6168. [Google Scholar] [CrossRef]
- Sobral, L.L.; Oliviera, L.S.; Takeda, S.Y.M.; Somazz, M.C.; Montebelo, M.I.L.; Teodori, R.M. Immediate versus later exercises for rat sciatic nerve regeneration after axonotmesis: Histomorphometric and functional analyses. Rev. Bras. Fisioter 2008, 12, 311–316. [Google Scholar] [CrossRef]
- López-Álvarez, V.M.; Modol, L.; Navarro, X.; Cobianchi, S. Early increasing-intensity treadmill exercise reduces neuropathic pain by preventing nociceptor collateral sprouting and disruption of chloride cotransporters homeostasis after peripheral nerve injury. Pain 2015, 156, 1812–1825. [Google Scholar] [CrossRef]
- de Moraes, A.A.; de Almeida, C.A.S.; Lucas, G.; Thomazini, J.A.; DeMaman, A.S. Effect of swimming training on nerve morphological recovery after compressive injury. Neurol. Res. 2018, 40, 955–962. [Google Scholar] [CrossRef]
- Ilha, J.; Araujo, R.T.; Malysz, T.; Hermel, E.E.S.; Rigon, P.; Xavier, L.L.; Achaval, M. Endurance and Resistance Exercise Training Programs Elicit Specific Effects on Sciatic Nerve Regeneration After Experimental Traumatic Lesion in Rats. Neurorehabilit. Neural Repair 2007, 22, 355–366. [Google Scholar] [CrossRef] [PubMed]
- Pachter, B.R.; Eberstein, A. Passive Exercise and Reinnervation of the Rat Denervated Extensor Digitorum Longus Muscle after Nerve Crush. Am. J. Phys. Med. Rehabilitation 1989, 68, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Florence, S.L.; Boydston, L.A.; Hackett, T.A.; Lachoff, H.T.; Strata, F.; Niblock, M.M. Sensory enrichment after peripheral nerve injury restores cortical, not thalamic, receptive field organization. Eur. J. Neurosci. 2001, 13, 1755–1766. [Google Scholar] [CrossRef]
- Sinis, N.; Guntinas-Lichius, O.; Irintchev, A.; Skouras, E.; Kuerten, S.; Pavlov, S.P.; Schaller, H.E.; Dunlop, S.A.; Angelov, D.N. Manual stimulation of forearm muscles does not improve recovery of motor function after injury to a mixed peripheral nerve. Med. Sci. Sports Exerc. 2006, 38, 1267–1276. [Google Scholar] [CrossRef] [PubMed]
- Cobianchi, S.; de Cruz, J.; Navarro, X. Assessment of sensory thresholds and nociceptive fiber growth after sciatic nerve injury reveals the differential contribution of collateral reinnervation and nerve regeneration to neuropathic pain. Exp. Neurol. 2014, 255, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Pan, B.; Fromholt, S.E.; Hess, E.J.; Crawford, T.O.; Griffin, J.W.; Sheikh, K.A.; Schnaar, R.L. Myelin-associated glycoprotein and complementary axonal ligands, gangliosides, mediate axon stability in the CNS and PNS: neuropathology and behavioral deficits in single- and double-null mice. Exp Neurol. 2005, 195, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Trapp, B.D.; Andrews, S.B.; Cootauco, C.; Quarles, R. The myelin-associated glycoprotein is enriched in multivesicular bodies and periaxonal membranes of actively myelinating oligodendrocytes. J Cell Biol. 1989, 109, 2417–26. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.P.; Taylor, R.S. Guillain-Barre Syndrome. StatPearls. 2022. [Google Scholar]
- Sabatier, M.J.; Redmon, N.; Schwartz, G.; English, A.W. Treadmill training promotes axon regeneration in injured peripheral nerves. Exp. Neurol. 2008, 211, 489–493. [Google Scholar] [CrossRef] [PubMed]
- English, A.W.; Cucoranu, D.; Mulligan, A.; Sabatier, M. Treadmill training enhances axon regeneration in injured mouse peripheral nerves without increased loss of topographic specificity. J. Comp. Neurol. 2009, 517, 245–255. [Google Scholar] [CrossRef]
- Hunter, G.; Sarvestany, A.A.; Roche, S.; Symes, R.; Gillinwater, T.H. SMN-dependent intrinsic defects in Schwann cells in mouse models of spinal muscular atrophy. Hum Mol Genet. 2014, 23, 2235–50. [Google Scholar] [CrossRef]
- Armada-da-Silva, P.; Pereira, C.; Amado, S.; Veloso, A. Role of physical exercise for improving posttraumatic nerve regeneration. Int Ver Neurobiol. 2013, 109, 125–49. [Google Scholar]
- Martins treino locomotor.
- Willand, M.; Nguyen, M.; Borschel, G.; Gordon, T. Electrical stimulation to promote peripheral nerve regeneration. Neurorehabil neural repair. 2016, 30, 30,490–6. [Google Scholar] [CrossRef]
- Thompson, N.J.; Sengelaub, D.R.; English, A.W. Enhancement of peripheral nerve regeneration due to treadmill training and electrical stimulation is dependent on androgen receptor signaling. Dev Neurobiol. 2014, 74, 531–540. [Google Scholar] [CrossRef]
- Elzinga, K.; Tyreman, N.; Ladak, A.; Savaryn, B.; Olson, J.; Gordon, T. Brief electrical stimulation improves nerve regeneration after delayed repair in Sprague Dawley rats. Exp Neurol. 2015. [Google Scholar] [CrossRef]
- Gordon, T.; Amirjani, N.; Edwards, D.C.; Chan, K.M. Brief post-surgical electrical stimulation accelerates axon regeneration and muscle reinnervation without affecting the functional measures in carpal tunnel syndrome patients. Exp Neurol. 2010, 223, 192–202. [Google Scholar] [CrossRef]
- Wong, J.N.; Olson, J.L.; Morhart, M.J.; Chan, K.M. Electrical stimulation enhances sensory recovery: A randomized control trial. Ann Neurol. 2015. [Google Scholar] [CrossRef]
- Juckett, L.; Saffari, T.M.; Ormseth, B.; Senger, J.; Moore, A. The effect of electrical stimulation on nerve regeneration following peripheral nerve injury. Biomolecules. 2022, 12, 1856. [Google Scholar] [CrossRef]
- López-Álvarez, V.M.; Modol, L.; Navarro, X.; Cobianchi, S. Early increasing-intensity treadmill exercise reduces neuropathic pain by preventing nociceptor collateral sprouting and disruption of chloride cotransporters homeostasis after peripheral nerve injury. Pain 2015, 156, 1812–1825. [Google Scholar] [CrossRef]
- Bal-Price, A.; Brown, G.C. Nitric-oxide-induced necrosis and apoptosis in PC12 cells mediated bu mitochondria. J Neurochem. 2000, 75, 1455–64. [Google Scholar] [CrossRef] [PubMed]
- Khalil, Z.; Khodr, B. A role for free radicals and nitric oxide in delayed recovery in aged rats with chronic constriction nerve injury. Free Rad Biol and Med. 2001, 31, 430–439. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, R.I.; Marcolino, A.M.; de Jesus Guirro, R.R.; Mazzer, N.; Barbieri, C.H.; de Cássia Registro Fonseca, M. Comparative effects of wavelengths of low-power laser in regeneration of sciatic nerve in rats following crushing lesion. Lasers Med Sci. 2010, 25, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Gigo-Benato, D.; Geuna, S.; de Castro Rodrigues, A.; Tos, P.; Fornaro, M.; Boux, E.; Battiston, B. Giacobini-Robecchi, M.G. Low-power laser biostimulation enhances nerve repair after end-to-side neurorrhaphy: a double-blind randomized study in the rat median nerve model. Lasers Med Sci. 2004, 19, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.C.; Yang, Y.C.; Liu, B.S. Large-area irradiated low-level laser effect in a biodegradable nerve guide conduit on neural regeneration of peripheral nerve injury in rats. Injury. 2011, 42, 803–13. [Google Scholar] [CrossRef]
- Page, M.; OConnor, D.; Pitt, V.; Massy-Westropp, N. Therapeutic ultrasound for carpal tunnel syndrome. Cochrane Database Syst Rev. 2013, 3, CD009601. [Google Scholar] [CrossRef] [PubMed]
- Bekhet, A.; Ragab, B.; Abushouk, A.; Elgebaly, A.; Ali, O. Efficacy of low-level laser therapy in carpal tunnel syndrome management: a systematic review and meta-analysis. Lasers Med Sci. 2017, 32, 32,1439–1448. [Google Scholar] [CrossRef] [PubMed]
- Cofano, F.; Boido, M.; Monticelli, M.; Zenga, F.; Ducati, A.; Vercelli, A.; Garbossa, D. Mesenchymal Stem Cells for Spinal Cord Injury: Current Options, Limitations, and Future of Cell Therapy. Int. J. Mol. Sci. 2019, 20, 2698. [Google Scholar] [CrossRef] [PubMed]
- Rowland, J.W.; Hawryluk, G.W.; Kwon, B.; Fehlings, M.G. Current status of acute spinal cord injury pathophysiology and emerging therapies: Promise on the horizon. Neurosurg. Focus 2008, 25, E2. [Google Scholar] [CrossRef]
- Gazdic, M.; Volarevic, V.; Harrell, C.R.; Fellabaum, C.; Jovicic, N.; Arsenijevic ́, N.; Stojkovic, M. Stem Cells Therapy for Spinal Cord Injury. Int. J. Mol. Sci. 2018, 19, 1039. [Google Scholar] [CrossRef]
- Kumar, P.; Kandoi, S.; Misra, R.; Vijayalakshmi, S.; Rajagopal, K.; Verma, R.S. The mesenchymal stem cell secretome: A new paradigm towards cell-free therapeutic mode in regenerative medicine. Cytokine Growth Factor Rev. 2019, 46, 1–9. [Google Scholar]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




