1. Introduction
Asthma some many different possible reasons and illnesses that can lead to chronic upper airway inflammation, which includes chronic otitis media, chronic rhinitis, chronic sinusitis, chronic pharyngitis, and chronic laryngitis While chronic inflammation of the lower respiratory tract is more broadly defined, “Asthma” still refers to a varied group of clinical disorders with differences in severity, onset, risk factors, triggers, response to therapy, genetics, and natural history Furthermore, it’s frequently difficult to distinguish between asthma and other diagnoses including bronchiolitis and reactive airway disease
The National Institute of Health Guidelines on Asthma (NIH Guidelines) define asthma as follows in their editions from 1991, 1997, and 2007 Asthma is a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role: in particular, mast cells, eosinophils, T lymphocytes, macrophages, neutrophils, and epithelial cells In susceptible individuals, this inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning These episodes are usually associated with widespread but variable airflow obstruction that is often reversible either spontaneously or with treatment The inflammation also causes an associated increase in the existing bronchial hyperresponsiveness to a variety of stimuli The reversibility of airflow limitation may be incomplete in some patients with asthma Like chronic sinusitis, this definition emphasizes the existence of inflammation and the accompanying symptoms without addressing the origin, which is unknown, or the natural history, which is unpredictable.
Epidemiology
One of the most prevalent chronic diseases in the world, asthma affects about 300 million individuals worldwide While the disease is well-known throughout the world, asthma is most common in nations with high GDPs In the majority of rural and low-income countries, the prevalence of asthma is typically less than 1%, which is far lower than the 10% typically observed in industrialized Western nations The prevalence of asthma follows an urban-rural gradient and a weak latitudinal gradient within populations of a given gross domestic product, meaning that asthma is more prevalent in urban regions and that illness prevalence increases with distance from the equator Although the prevalence of asthma is low in low- and middle-income nations, significant and possibly preventable disease morbidity and mortality occur due to underdiagnosis, misdiagnosis, and insufficient treatment in these areas Over the past few decades, asthma has become more commonplace in many parts of the world Until recently, wealthy Western countries saw an annual increase in the prevalence of asthma The origin of the epidemic that started in the late 1970s is unknown, although an increase in the prevalence of asthma is in line with an increase in other immune-mediated conditions such as multiple sclerosis, inflammatory bowel disease, and type 1 diabetes Recent studies in epidemiology have concentrated on how a mother’s nutrition changes during pregnancy — with a focus on the gut and airway microbiota, prematurity, maternal paracetamol usage throughout pregnancy, and the levels of micronutrients including ω-3 fatty acids, folate, and vitamin D (the latter two affecting methylation), and therefore fetal programming The development of asthma is influenced by age, sex, and immunological variables.
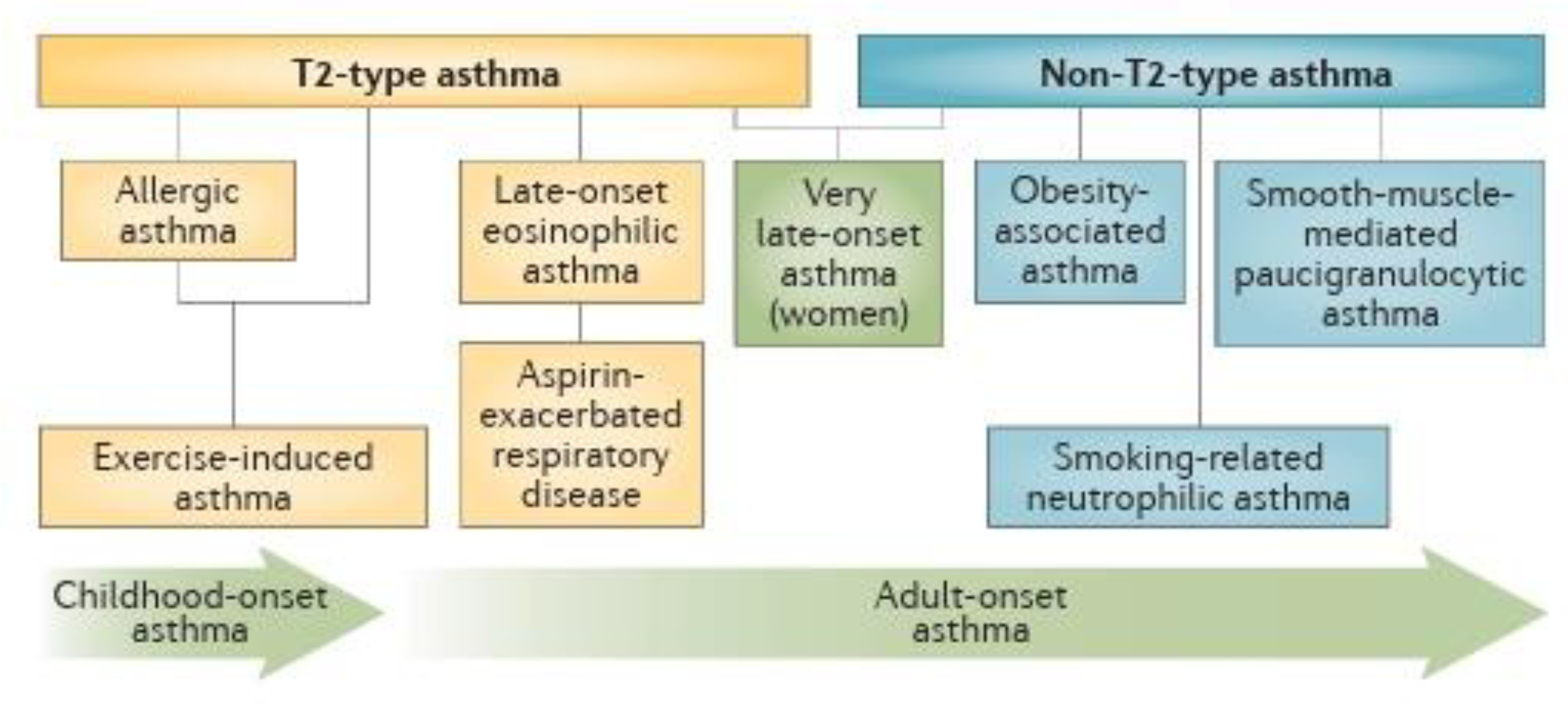
Figure 1.
Selected asthma subphenotypes New subphenotypes and associated causal pathways, or endotypes, of asthma are being discovered through the application of non-hierarchical statistical analyses of clinical, physiological and laboratory characteristics.
Figure 1.
Selected asthma subphenotypes New subphenotypes and associated causal pathways, or endotypes, of asthma are being discovered through the application of non-hierarchical statistical analyses of clinical, physiological and laboratory characteristics.
Atopic individuals, or those who are genetically predisposed to allergic hypersensitivity, account for 50% of children diagnosed with asthma by the time they are 3 years old and 80% of those diagnosed by the time they are 6 years old The disease is closely associated with the presence of immediate hypersensitivity In children younger than six years old, wheezing is more common than asthma This observation suggests that factors other than asthma, such as physician diagnostic bias and lower respiratory tract infections, can drive the onset and persistence of wheezing Asthma is not constant across the life course of the patient, and patients can experience periods of remission and the onset of new asthma Although boys are more likely than girls to have asthma in early childhood, boys also have a higher likelihood of asthma remission during puberty and the early years of adulthood In addition, females are more likely than boys in this age group to develop asthma As a result, throughout adolescence and early adulthood, the sex ratio of asthma during infancy reverses Although the causes of the patient’s asthma’s variation throughout their life are unknown, there is growing evidence that hormones play a critical part in this process In addition, adolescent asthma remission is linked to a decrease in initial airway hyperresponsiveness and an increase in small airway function when compared to asthma which starts later in life Although the causes of the differences in asthma between those with early and late onsets are likely complicated, it is believed that different environmental exposures, notably those that take place in work environments, have a significant role.
Pathophysiology
The most likely cause of inflammation in the lower respiratory tract is a mix of environmental exposures, genetic predisposition, and potential changes in the microbiome and metabolites (low molecular weight molecules in biological systems) Named for the type 2 T helper cell lymphocyte, type 2 inflammation affects the majority of asthmatics Interleukin [IL]-4, IL-5, and IL-14 are among the cytokine profiles and inflammatory cells linked to type 2 inflammation (eosinophils, mast cells, basophils, type2 T helper lymphocytes, and immunoglobulin E [IgE]-producing plasma cells) Type 2 inflammation is frequently observed in parasite infections, eosinophilic illnesses, and allergy diseases It has also been discovered that cytokines, which control type 2 inflammation, are mostly regulated by airway epithelial cells (IL25, IL-33, and thymic stromal lymphopoietin) It can be challenging to treat asthmatics who do not have a significant predisposition toward type 2 inflammation since they frequently react poorly to corticosteroids.
Challenges in Asthma
An intricate and diverse respiratory ailment is severe asthma Using monoclonal antibody medicines that target the inflammatory aspect of the disease, the management of severe asthma has advanced significantly within the last ten years A major interest in biomarkers to direct treatment has resulted from the fact that patient selection has been critical to the efficacy of these biologicals Several people with severe asthma nevertheless require long-term systemic corticosteroids since their condition is not fully managed even after trying biological treatments To meet this unmet demand, new medicines are presently being developed Nevertheless, it is unclear if these patients could receive better care if innovative biomarkers that objectively quantify disease control and guide the selection of currently accessible biologics were used.
Treatment A heterogeneous airway disease is severe asthma Many severe patient outcomes have been markedly improved by the introduction of biologicals that target specific cytokines, thanks to recent insights into the mechanism of airway inflammation in asthma For predicting the effectiveness of biologicals that target the IL5 pathway, sputum eosinophils seem to be the most informative biomarker Although blood eosinophils can be a helpful proxy, anti-IL5 medication is most likely to assist a significant minority of patients who would otherwise be ignored, especially if they are receiving systemic corticosteroids Additional information is required, however, sputum cytometry can help determine the reason behind a patient’s inadequate response to an anti-IL5 medication and in the process of choosing which patients should get Tezepelumab The best biomarker to identify people who respond to dupilumab appears to be FeNO, while blood eosinophils may be useful in patients who do not take systemic corticosteroids When it comes to selecting between omalizumab and anti-IL5 therapy for patients who are eligible for both medications, there are no reliable clinical or biochemical markers other than the requirement for systemic corticosteroids, which suggests the use of an anti-IL5 medication There is potential for novel biomarkers to support biological selection, including IL13 inducible genes and airway mast cell tryptase Precision medicine in severe asthma will not be able to achieve its goal until new biomarkers are found and validated.
Emerging Drugs for Asthma
Asthma medication treatments currently available reduce airway inflammation and bronchospasm but do not cure the condition; symptoms recur when treatment is stopped the significance of receiving efficient asthma treatment to attain and preserve asthma control is emphasised in asthma management guidelines Controlling asthma is still an unmet requirement for many individuals, despite readily available and efficient therapies.
Significant attempts have been made to distinguish the characteristic symptoms of severe, often uncontrollable asthma from those of mild-to-moderate asthma, paving the way for the creation of novel and even customised treatments of all the novel asthma medications, biologic therapies—more specifically, monoclonal antibodies—are the most intriguing Furthermore, some unique once-daily regimens are being developed that combine inhaled corticosteroids with long-acting b2-agonists.
The complex illness known as asthma is composed of several asthma phenotypes, or ease variations, each with its underlying aetiology It’s important to ascertain each patient’s unique profile of pathophysiological anomalies because different medications target distinct pathways The most significant cytokines are addressed here Several cytokines have been linked to the inflammatory cascades that result in various asthma phenotypes The very variability of asthma poses a hurdle to treatment.
2. Type of Emerging Drug Delivery System
- a)
Nasopulmonary Drug Delivery System
- b)
Pressurized Metered-Dose Inhalers
- c)
Dry powder Inhalers
- d)
Nebulizers
- e)
Nanoparticles
- f)
Liposomes
- g)
Micellar system
- h)
Microparticles
- i)
Dendrimers
- j)
Gene therapy
-
a.
Nasopulmonary Drug Delivery System
One of the most effective medicine delivery methods is via the nose, and it has been utilised recently to treat a variety of illnesses Mucous secretions, ciliated epithelial cells (ie, those in charge of mucociliary clearance), and lung macrophages are only a few of the respiratory system’s (particularly the lungs’) formidable defence mechanisms Applying nasopulmonary medication delivery devices is a little bit difficult because of these defence mechanisms When preparing a nasopulmonary drug delivery system, it is important to consider the parameters of the nano- or microparticles (such as their size, shape, and ability to evade immune clearance mechanisms) that allow them to reach the desired site of action through the nasopulmonary route This research is highly important and provides valuable information In this chapter, the respiratory system’s anatomy and physiology, lung simulation equipment, nasopulmonary drug delivery methods, and factors influencing particle deposition in the deep lung are all summarised Additionally, material selection criteria for nasopulmonary delivery are provided.
-
b.
Pressurized Metered-Dose Inhalers (pMDIs)
When treating respiratory tract conditions including asthma and chronic obstructive pulmonary disease, pressurised metered-dose inhalers are the most often used delivery system pMDIs are available for the administration of all kinds of inhalable medications, either in a single formulation or in combinations containing two or more drugs Patients find it difficult to utilise pMDIs appropriately, even though they are most frequently given for obstructive respiratory conditions The metal canister, metered valve, actuator, and mouthpiece are the structural elements of conventional pMDIs Precise aerosol doses may be administered following each actuation thanks to the metering valve The pMDIs formulation is made up of suspending agents, surfactants, cosolvents, excipients, and propellants in either a suspension or a solution form Aerosolized droplets are created by evaporation when the drug particles enter the air and the formulation’s boiling temperature differs from room temperature Products differ in terms of the size of the aerosolized particles.
Another type of pulmonary delivery device that requires the least amount of coordination between breathing and actuation is the dry powdered inhaler (DPI), which delivers powdered medication directly into the respiratory tract Compared to pMDIs, which are suspensions or solutions of drugs, DPIs offer a higher degree of chemical stability because they contain the medications in a dried state Nevertheless, it is difficult to formulate and produce dry powder particles with the right properties for pulmonary administration and aerosolization Typically, the dry powder is made up of large-sized excipients including lactose, sucrose, and glucose combined with medication particles that have been micronized There are various DPI types available, including multiple reservoirs, single-unit doses, and multiunit doses The patient’s inspiratory attempts provide the DPIs with the energy needed for drug delivery The spiral chamber, manifold, cyclone, and mesh are the structural elements of DPIs These elements need to be able to use the inhaling force to break up the drug-excipient clumps Each product has a different minimum inspiratory force needed, but 30 to 60 L/min is the recommended range.
Nebulizers are machines that produce 1 to 5 μm aerosol droplets for pulmonary administration through inhalation Jet and ultrasonic nebulizers are the two types of nebulizers that are typically employed The force used by these two types of nebulizers to create aerosols from liquid suspension or solution varies Nebulizers can be utilised by a range of patients who are unable to use pMDIs and DPIs since they do not require synchronisation between inspiration and actuation Nebulizers also can deliver high dosages While ultrasonic nebulizers employ sound waves to break big droplets into smaller aerosol droplets, jet nebulizers use a pressure-based process to produce small aerosol particles For best results, nebulizers need to have a few things optimised: air pressure, the mouthpiece being used, and the volume and viscosity of the medication solution that is loaded Compared to the formulation needed for pMDIs and DPIs, the solutions used in nebulizers are simpler and less expensive to make Nebulizers have several drawbacks, one of which is that a patient may find it challenging to build and load the device before each usage and to disassemble and clean it again afterwards if they are not well-trained.
Nanoparticles have been shown to enhance the therapeutic effect by facilitating drug delivery to target tissues, improving the deposition of the drug in the lungs In vitro studies have shown that poly(lactic acid) nanoparticles can co-deliver theophylline and budesonide, which are appropriate drug delivery methods for asthma and COPD treatment In vivo, studies have also investigated the anti-inflammatory activity of quercetin-loaded liquid crystalline NPs (LCN) and surface-modified liquid crystalline NPs (sm-LCN), which can be effective in inhibiting the fabrication of proinflammatory cytokines related to asthma development.
Treatment with lipid nanoparticles has been found to decrease the secretion of proinflammatory cytokines in asthmatic mice and can significantly diminish allergic asthma by hindering the overexpression of proinflammatory cytokines in the airway Nanoparticle administration of LNA oligonucleotides can prevent asthma-induced airway inflammation In vivo, studies have shown that aerosolized liposome formulations for pulmonary delivery of anti-asthmatic treatment show a more prolonged anti-asthma effect than R-TBH solution.
Lymphocyte-loaded chitosan NP (FACHA) aerosolized by vibrating mesh nebulizers have shown greater drug retention time and anti-inflammatory and anti-asthmatic effects compared to the free drug Liposomal budesonide treatment in asthmatic mouse models increased efficacy in the reduction of inflammation and showed fewer side effects compared to steroids.
Bilirubin-based nanoparticles (BRNPs) have been studied as nanomedicine for the treatment of allergic lung inflammatory disease Treatment with BRNPs inhibited the indices of experimental allergic asthma and intensely improved Th2-related allergic lung inflammation Encapsulated andrographolide (AG) in NP (AGNP) showed improved bioavailability upon administration by pulmonary route, and AGNP effectively controlled mild and intense asthma, especially when administered by inhalation Intranasal treatment with NPs targeting IL4Rα to regulate lung inflammation in OVA-sensitized mice has also been tested.
Liposomes, vesicles with a lipid bilayer membrane enclosing an aqueous core, are suitable for encapsulating drugs with various physical properties and drug combinations They have a hydrophilic core and hydrophobic lipid layer membrane, making them suitable for pulmonary delivery Liposomes have been investigated for local delivery of drugs to the lung for the treatment of diseases like pulmonary infections, cystic fibrosis, asthma, and lung cancer Liposomes have been investigated for targeted treatment of pulmonary infectious diseases, such as Asthma, an amikacin-loaded liposomal suspension approved by the FDA for treating infectious lung diseases caused by Mycobacterium avium complex bacteria.
Lung cancer is another respiratory disease where the potential of liposomes for delivery and treatment is being evaluated Many liposomal formulations consisting of chemotherapeutic drugs have been developed in research labs but have been rejected in clinical trials due to toxicity or not exhibiting better effects than the existing formulations Liposomal aerosolized formulations have been shown to improve localized concentration of drugs at the target site, reduce side effects and cytotoxicity, and improve bioavailability in clinical trials The successful development of aerosolized liposomal formulation depends on the ability of the liposome formulation and aerosol delivery device to deliver the drug to the target area in the respiratory tracts in required doses while minimizing side effects.
Polymeric micelles, nanosized colloidal carriers with a core-shell structure, are generated when amphiphilic polymers are dispersed in aqueous solutions above a critical micelle concentration (CMC) and solution temperature These micelles offer advantages like greater physical stability, need-based modification of size, encapsulation efficiency, and hydrophobic drug encapsulation Several micellar systems are being evaluated for their potential in pulmonary drug delivery.
Resveratrol-loaded Chol-PAM micelles exhibited anti-inflammatory effects in vitro and in vivo studies, demonstrating the efficiency of micelles as a carrier for drug and suitability for inhalation-based delivery In vivo studies demonstrated that micelles prolonged pulmonary retention time, localized sustained release for up to 24 hours, and facilitated uptake to pulmonary vascular endothelium.
Peptide conjugate Pluronic and succinylated gelatin-loaded PEG-PLGA micelles were developed and evaluated for the treatment of lung tumours by inhalation The unique property of these micelles was that the release of paclitaxel was triggered by the presence of matrix methacrylate 2/9 (MMP 2/9), with the amount of drug released dependent on the concentration of MMP 2/9 These environment-responsive systems could further be explored for targeted delivery and reduced side effects, especially in cases of lung cancers.
Microparticles are made of either natural or synthetic polymers and range in size from 1 to 1000 μm Due to their enormous size and high porosity, these particles can deposit in deeper lung regions and avoid impaction in the upper tracts because of their tiny aerodynamic diameter High porosity microparticles should be able to evade alveolar macrophage clearance, allowing them to stay at the site longer and administer medications for extended periods Depending on the type of inhaler, the quantity of inhalable mass load at a single time can vary from around 25 to 50 mg The use of polymeric microparticle-based systems for medications that need to be supplied in small quantities is restricted by these constraints.
Dendrimers, sometimes referred to as dendritic polymers, are branched polymers possessing distinct microstructures and many functions The creation of PAMAM-conjugated doxorubicin (DOX) nanocarrier systems was reported by Zhong et al. They also assessed the drug’s efficacy in the lung metastases model and potential for pulmonary delivery The same group conducted a second investigation to assess how PEG surface modification of dendrimers affected their biodistribution and pharmacokinetic profile following systemic and pulmonary injection PEG was conjugated to amine-terminated PAMAM dendrimers on their surface, and additional assessment was conducted The pharmacokinetic profiles revealed that the peak concentration of both PEGylated and non-PEGylated dendrimers was achieved through pharyngeal aspiration within a few hours of administration, ruling out the impact of chemistry on peak plasma concentration.
According to this study, dendrimers’ surfaces can be suitably modified to control their pharmacokinetic profiles, biodistribution, and targeted administration to certain organs There are still issues that need to be resolved regarding the large-scale manufacturing of such dendrimer-based delivery systems that meet the necessary clinical requirements.
It has been investigated for aerosolized delivery targeting illnesses such as cystic fibrosis, lung cancer, alpha-1 antitrypsin deficiency, and asthma using viral and nonviral vectors It was discovered that this inhalable formulation consistently produced proteins after repeated doses without generating systemic or local damage mRNAs can be sent to the lungs via this system to treat conditions such as cystic fibrosis and other illnesses.
Here, it is evident that the polymer was selected for pulmonary distribution due to its capacity to break down at the site and the chemical backbone needed for gene transport This type of strategy can be tested further with various polymers to create the appropriate systems needed to satisfy the therapeutic demand To address clinical needs, more research on the same must be done.
3. Case Studies of HEMA and HPMA
a literature research across medline, biosis and embase databases using the search terms 2-hydroxyethyl methacrylate or 1,2-ethanediol mono(2-methyl propenoate) or glycol methacrylate or HEMA or 2-hydroxypropyl methacrylate or methacrylic acid 2-hydroxypropyl ester or HPMA or and asthma or occupational asthma or respiratory sensitization or respiratory hypersensitive or specific(w)inhalation(w)challenge or respiratory(w) allerg on december 14, 2022 identified 4 published papers: piirila et al. (1998), lindstrom et al. (2002), sauni et al. (2008), moulin et al. (2009).
3.1. Piirila et al. (1998)
The purpose of this study was to report on presumed cases of
respiratory hypersensitivity to
acrylates among dental surgeons and dental nurses in Finland during the period 1992–1997 A total of 12 subjects were examined (6 dentists and 6 dental nurses) with varying lengths of prior professional exposure to acrylic-based dental materials Of the 12 subjects, 9 had a diagnosis of asthma (with or without rhinitis), 2 had
rhinitis, and one had
laryngitis.
The authors concluded that, based on the results of the reported investigations, work-related exposure of these subjects to acrylates and
methacrylates used in dental practice resulted in respiratory hypersensitivity Specific IgE was not measured, and all subjects were uniformly SPT negative when tested with a variety of methacrylates.
The diagnosis of respiratory hypersensitivity to acrylates/methacrylates was based on the results of SIC tests In most instances these challenges were performed with several types of Scotchbond dental adhesives containing a variety of methacrylates (including HEMA), but also several other unrelated ingredients The authors provide some details of the chemical composition of these products More comprehensive information on the chemical composition of these products is detailed in electronic appendix A Two subjects displayed early (immediate) responses following the challenge, and 7 subjects displayed late responses It appears that 3 subjects failed to respond in SIC tests However, these data must be interpreted with considerable caution for two main reasons Firstly, the challenge tests were conducted with Scotchbond™ products that were mixtures containing methacrylates and other unrelated compounds such that responses cannot be ascribed to a single substance Secondly, the strategy used was that if subjects failed to respond to the first challenge (which already employed ten times the quantity of materials than would be encountered when using the recommended amount in the workplace), a second challenge was performed at a later date with twice the volume of the test material (ie, 20 times that recommended (3M Scotch) This use of excessively large quantities of test material for the SIC conflicts with the recommendation to simulate occupational exposure levels and increases the likelihood of non-specific irritation confounding the outcome.
For these reasons, it is very difficult to draw firm conclusions about the specificity of any reactions recorded following the challenge (and whether or not any reaction was indeed triggered by exposure to a methacrylate) Moreover, given the fact that high doses were required (in at least some instances) to elicit a response, the possibility that reactions were the result of non-specific irritancy cannot be excluded.
The authors acknowledge that the challenge tests were performed with dental
acrylate resin products that contained other components as well as impurities They acknowledge also that the reactions observed in SIC tests could be regarded as irritant (although they dispute this without giving adequate justification), and that the results do not indicate the mechanism(s) through which reactions were elicited.
In this context, it is important to consider whether the speed of reaction associated with a positive SIC test (early or late) provides evidence for the nature of the response It has been proposed that early asthmatic reactions (EAR) in SIC tests are indicative of an irritant reaction, and that late asthmatic reactions (LAR) are associated with sensitisation to a chemical allergen and
allergic asthma However, this is not an absolute rule, and LAR has been reported with irritant chemicals Consequently, it has been argued recently that the elicitation of a LAR in a SIC test cannot be regarded as being convincing or conclusive evidence for an allergic mechanism.
Taken together, the significant limitations of the data summarised above do not permit any conclusions to be drawn about the cause or mechanisms of occupational respiratory hypersensitivity, and certainly, there is no basis for identifying any specific chemicals (including HEMA) as being a respiratory sensitiser.
3.2. Lindstrom et al. (2002)
This paper describes the assessment of a dentist diagnosed as having occupational asthma The clinical picture was of normal spirometry, but moderate
bronchial hyperreactivity based on histamine challenge All SPTs were negatives, including those conducted with HEMA either as a free chemical or when conjugated to
human serum albumin Specific inhalation challenge tests were conducted using Scotchbond™ primer containing 40% HEMA and/or adhesive containing 37% HEMA (as well as other uncharacterised components) The first SIC test (using 20 drops of the adhesive) resulted in a very modest decrease in FEV
1 of 10% (that is below the level of 15% proposed for a positive challenge test; A second SIC test was conducted using 40 drops of both the primer and adhesive and this was associated with an ‘early/late’ reduction in FEV.
This case is somewhat unusual because the subject was also
patch test positive indicative of
allergic contact dermatitis (ACD) to both HEMA and HPMA, as well as some other methacrylates and acrylates The authors stated that they had not previously seen concurrent asthma,
rhinoconjunctivitis and ACD associated with methacrylates in the same patient The patient was found to develop eye symptoms during patch testing which is indicative of systemic ACD It is possible, therefore, that the reactions observed following the second SIC test may, at least in part, be a manifestation of systemic ACD
Given the uncertainty about the exact composition of materials used in the SIC tests, the fact that high concentrations of these materials were required to elicit a positive challenge reaction and that responses may be, in part, associated with systemic ACD or non-specific irritation, it is not possible to draw any firm conclusions regarding respiratory sensitisation to HEMA,
HMPA or other methacrylates based on these data.
3.3. Sauni et al. (2008)
This paper describes clinical studies of 2 female nail technicians diagnosed with occupational asthma associated with workplace exposure to artificial sculptured nails and associated products containing methacrylates and
cyanoacrylates.
Patient 1 developed
eczema some months after starting work with artificial nails and was claimed to have ACD to HEMA and EGDMA (ethylene glycol methacrylate) Subsequently, the subject developed respiratory symptoms and was shown to have moderate bronchial hyperresponsiveness in a histamine challenge Skin prick tests with methacrylates (including HEMA and EGDMA) were negative, as was an SPT conducted with HEMA conjugated with human serum albumin.
In a challenge test, the subject simulated attaching the nail with glue and then filing and sculpturing the nails in a challenge chamber A dual reaction was recorded with both an immediate and delayed drop in FEV1 On this basis, occupational asthma resulting from exposure to sculptured nails was diagnosed.
Patient 2 also worked with products similar to those used by patient 1 She presented with allergic rhinitis and reactivity to cat and
pollen allergens In histamine challenges the subject displayed initially mild, and later moderate, bronchial hyperresponsiveness and asthma was diagnosed No SPTs with methacrylates were carried out A SIC test employing challenges with gel nails and gel nail materials was conducted A dual response in the SIC was observed with an immediate reaction 35 min after the initiation of exposure, and a later drop in FEV
1 at 8 h.
The challenge material (which was comprised of a bonding agent, sealing resin, sculpture resin and gel nails) was analysed and found to contain a variety of methacrylates, at differing concentrations, including HEMA and HPMA.
Concerning HEMA this was found to be present in the bonding reagent at 75% (w/w) and HPMA was present in the sculpture resin at 67% (w/w), but in other components of the challenged material (sealing resin and gel nails), the content of these chemicals was either extremely low or absent Other methacrylates and cyanoacrylates were also present in the materials, together with high concentrations of unknown materials For instance, in the bonding agent, unknown components (that is components other than methacrylates) were shown to account for approximately 90% of the mix by weight In all probability, patient 1 was exposed to the challenge of the same, or at least very similar, products and chemicals.
Taken together the data available for the 2 cases reported by Sauni et al. (2008) do not permit identification of the specific chemical(s) that might have been responsible for the diagnosis of occupational asthma Certainly, it is impossible based on the available data to identify any specific chemical, or even groups of chemicals, as the causative agent(s) in these cases.
3.4. Moulin et al. (2009)
This paper describes studies designed to examine cases where there is evidence for simultaneous occupational asthma and ACD to a chemical Two subjects are described that were considered by the authors to have ACD and occupational asthma caused by HEMA.
Subject 1 was a female beautician who developed finger dermatitis and respiratory problems Symptoms began following the introduction of a nail prosthesis method employing new resins and solvents The subject was patch tested positive for HEMA, and a SIC test conducted with a product described as “HEMA without hardener” provoked an early asthmatic reaction The patient was diagnosed as having occupational asthma and ACD to HEMA.
Subject 2 was also a beautician who reported skin and respiratory problems associated with her workplace activities Patch tests with the methacrylate series were negative However, positive patch tests were obtained using activated ultraviolet gel and acrylic liquid According to the authors,
material safety data sheets made available by the manufacturer indicated that these products contained HEMA There is no mention of the concentration of HEMA in these products or the other constituent chemicals The patient declined to undergo any additional respiratory investigations, including a SIC test Nevertheless, based on these data the authors concluded that subject 2 had ACD and occupational asthma to HEMA, although they did acknowledge that the latter diagnosis could not be proven.
These diagnoses of occupational asthma resulting from allergic sensitisation to HEMA are not robust There are two important considerations, as follows: (a) it is entirely possible that the observed respiratory reactions were attributable to irritancy rather than sensitisation, and (b) irrespective of whether the reactions were or were not irritant there appears to be little justification for attributing the causation to HEMA In the case of subject 1, no information about the composition of the challenged material used in the SIC test is available beyond a “HEMA-type resin”, and in the case of subject 2 no A SIC test was performed Taken together there is insufficient information to implicate HEMA as the cause of respiratory effects.
4. Artificial Intelligence in Asthma Management
Artificial intelligence (AI), machine learning, and deep learning are hierarchical concepts that simulate human intelligence by computer systems AI covers tasks such as reasoning, learning, language processing, and knowledge display Machine learning is a subset of AI that aims for computers to automatically handle tasks and improve from experience without explicit programming There are two main types of machine learning: supervised and unsupervised.
Traditionally, statistical methods like calculus and regression modelling were used to establish mathematical equations, but these methods can be limited when dealing with large volumes of data Machine learning can analyze large volumes of data to establish complex, nonlinear relationships, enabling greater accuracy in outcomes.
It also enables the analysis of types of data that were previously unamenable to computational analysis, such as imaging and auditory data Deep learning, a subset of machine learning, has gained popularity due to the rapid increase in data available to researchers It allows algorithms to automatically discover specific features and transformations required for tasks in raw data Deep learning is currently being used in speech recognition, predicting drug molecules’ activity, and predicting non-coding DNA mutations’ effects on gene expression and disease.
Use of Ai in Respiratory Medicine
AI has been used to assess chest CT images for lung cancer, identifying trends in changes in nodule and non-nodule features, as well as changes in temporal and spatial alterations In a longitudinal screening program, this technology has been utilized to guide clinical management and forecast the 3-year risk of lung cancer Using visual localization of anomalies, deep neural networks (DNNs) have been built to identify lung cancer, TB, pneumonia, and pneumothorax on chest radiographs.
High-resolution computed tomography is essential for the accurate identification of fibrotic lung disease Using worldwide diagnostic guideline statements as a reference, a deep learning algorithm has obtained an accuracy of 733% for automated categorization of fibrotic lung disease on high-resolution CT. This accuracy is comparable to the median accuracy of thoracic radiologists for the same cases When compared to qualitative and quantitative data obtained using image analysis tools, the use of deep neural networks (DNNs) in respiratory disease detection, namely in chest radiographs and CT scans, has led to a step change in diagnostic accuracy Compared to manual qualitative or quantitative analysis, DNNs are more accurate since they extract features straight from the data itself.
5. The Global Impact of Asthma
241 million adults and children worldwide suffer from asthma, a common chronic illness that results in 22 million life years lost because of needless incapacity According to the International Study of Asthma and Allergies in Childhood (ISAAC), the majority of individuals live in low- and middle-income countries (LMICs), where asthma prevalence is rising at the quickest rate Several HICs and LMICs have created national or regional asthma strategies or programs to lessen the burden of asthma, which has quickly reduced the negative impacts of asthma.
Finland created the first all-inclusive national asthma policy in 1994, and other nations followed suit Several additional national plans inside the European Union, such as those in France, Portugal, and Spain, have been influenced by this approach Other countries like Australia, El Salvador, Brazil, Canada, Costa Rica, Singapore, Tonga, and Turkey have also employed independent methods with better results There aren’t many reports of these tactics, though, which suggests that many nations lack national asthma plans or implementations.
In 2012, members of the International Society for Acute Care (ISAAC) and the International Union Against Tuberculosis and Lung Disease (The Union) collaborated to create the Global Asthma Network (GAN) With an emphasis on LMICs, its objectives are to improve asthma care globally by increasing capacity building, research collaboration, improved surveillance, and access to necessary medications that are guaranteed to be of high quality It was a good idea to conduct a quick poll to find out if a nation had a national asthma strategy for adults and children because of the vast number of centres and nations participating in GAN.
Conclusion
Asthma is a long-term inflammatory respiratory condition that affects around 300 million people globally Asthma is characterized by a chronic inflammatory condition of the airways that involves mast cells, eosinophils, T lymphocytes, macrophages, neutrophils, and epithelial cells, according to the National Institute of Health Guidelines on Asthma (NIH Guidelines) It is intimately linked to acute hypersensitivity; wheeze is more common than asthma in children under six years old.
By allowing chores to be handled automatically and allowing for experience to be gained without explicit programming, learning has completely changed the way asthma is managed The Global Asthma Network (GAN) was established in 2012 with the goal of enhancing asthma care on a global scale through increased access to high-quality drugs, enhanced surveillance, research collaboration, and capacity building In the past ten years, there has been a tremendous advancement in the care of severe asthma, a complex and multifaceted respiratory condition The fact that patient selection has been crucial to the effectiveness of these biologicals has led to a significant interest in biomarkers for direct treatment Researchers have created a number of drug delivery techniques to solve this, such as nebulizers, nanoparticles, liposomes, dry powdered inhalers (DPIs), pressurized metered-dose inhalers (pMDIs), and liposomes.
It has been demonstrated that nanoparticles improve the delivery of drugs to target tissues and promote their accumulation in the lungs, hence augmenting therapeutic benefits According to research conducted in vitro, poly (lactic acid) nanoparticles have the ability to co-deliver theophylline and budesonide, two medications that are useful for treating Asthma.
References
- Holgate, S T, Wenzel, S, Postma, D S, Weiss, S T, Renz, H, & Sly, P D. Asthma Nature reviews Disease primers, 2015, 1, 15025.
- Adatia, A, & Vliagoftis, H. Challenges in severe asthma: Do we need new drugs or new biomarkers? Frontiers in Medicine, 2022, 9, 921967. [CrossRef]
- Sunkara, K, Mehta, M, Satija, S, Dhanjal, D S, Sharma, P, Shukla, S D, & Allam, V S R R (2022) An introduction to respiratory diseases and an emerging need for efficient drug delivery systems In Advanced Drug Delivery Strategies for Targeting Chronic Inflammatory Lung Diseases (pp 1-24) Singapore: Springer Singapore. [CrossRef]
- Gao, J, Karp, J M, Langer, R, & Joshi, N. The future of drug delivery Chemistry of Materials, 2023, 35, 359-363. [CrossRef]
- Ibrahim, A, Aziz, O A A, Dena, A S A, & El-Sherbiny, I M (2023) Current advancements in nasopulmonary drug delivery systems In Advanced and Modern Approaches for Drug Delivery (pp 91-111) Academic Press. [CrossRef]
- Mishra, B, & Singh, J (2020) Novel drug delivery systems and significance in respiratory diseases In Targeting Chronic Inflammatory Lung Diseases Using Advanced Drug Delivery Systems (pp 57-95) Academic Press.
- Taghavizadeh Yazdi, M E, Qayoomian, M, Beigoli, S, & Boskabady, M H. Recent advances in nanoparticle applications in respiratory disorders: a review Frontiers in pharmacology, 2023, 14, 1059343.
- Pemberton, M A, Kreuzer, K, & Kimber, I. Challenges in the classification of chemical respiratory allergens based on human data: Case studies of 2-hydroxyethylmethacrylate (HEMA) and 2-hydroxypropylmethacrylate (HPMA) Regulatory Toxicology and Pharmacology, 2023, 105404. [CrossRef]
- Kaplan, A, Cao, H, FitzGerald, J M, Iannotti, N, Yang, E, Kocks, J W, & Mastoridis, P. Artificial intelligence/machine learning in respiratory medicine and potential role in asthma and COPD diagnosis The Journal of Allergy and Clinical Immunology: In Practice, 2021, 9, 2255-2261. [CrossRef]
- Enilari, O, & Sinha, S. The global impact of asthma in adult populations Annals of global health, 2019, 85. [CrossRef]
- Asher, I, Haahtela, T, Selroos, O, Ellwood, P, Ellwood, E, & Global Asthma Network Study Group. Global Asthma Network survey suggests more national asthma strategies could reduce burden of asthma Allergologia et immunopathologia, 2017, 45, 105-114. [CrossRef]
- Quirce, S, Bobolea, I, & Barranco, P. Emerging drugs for asthma Expert opinion on emerging drugs, 2012, 17, 219-237.
- Blease, K, Lewis, A, & Raymon, H K. Emerging treatments for asthma Expert opinion on emerging drugs, 2003, 8, 71-81.
- Barnes, P J, & Drazen, J M. Pathophysiology of asthma Asthma and COPD, 2002, 343-359. [CrossRef]
- Chan, H K, & Chew, N Y. Novel alternative methods for the delivery of drugs for the treatment of asthma Advanced drug delivery reviews, 2003, 55, 793-805. [CrossRef]
- Drummond, D, Roukema, J, & Pijnenburg, M. Home monitoring in asthma: towards digital twins Current Opinion in Pulmonary Medicine, 2023, 29, 270-276. [CrossRef]
- Sarangdhar, N, Deshpande, P, Patel, S, Nair, G, Uppe, A, & Moulick, N. Asthma–Current Trends and Management Perspectives Indian Practitioner, 2023, 76.
- Wenzel, S E. Asthma phenotypes: the evolution from clinical to molecular approaches Nature medicine, 2012, 18, 716-725. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).