Submitted:
21 February 2024
Posted:
22 February 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Quantification of Serum and Synovial Fluid Cytokines by Multiplex Bead Assay
2.3. Statistical Analysis
3. Results
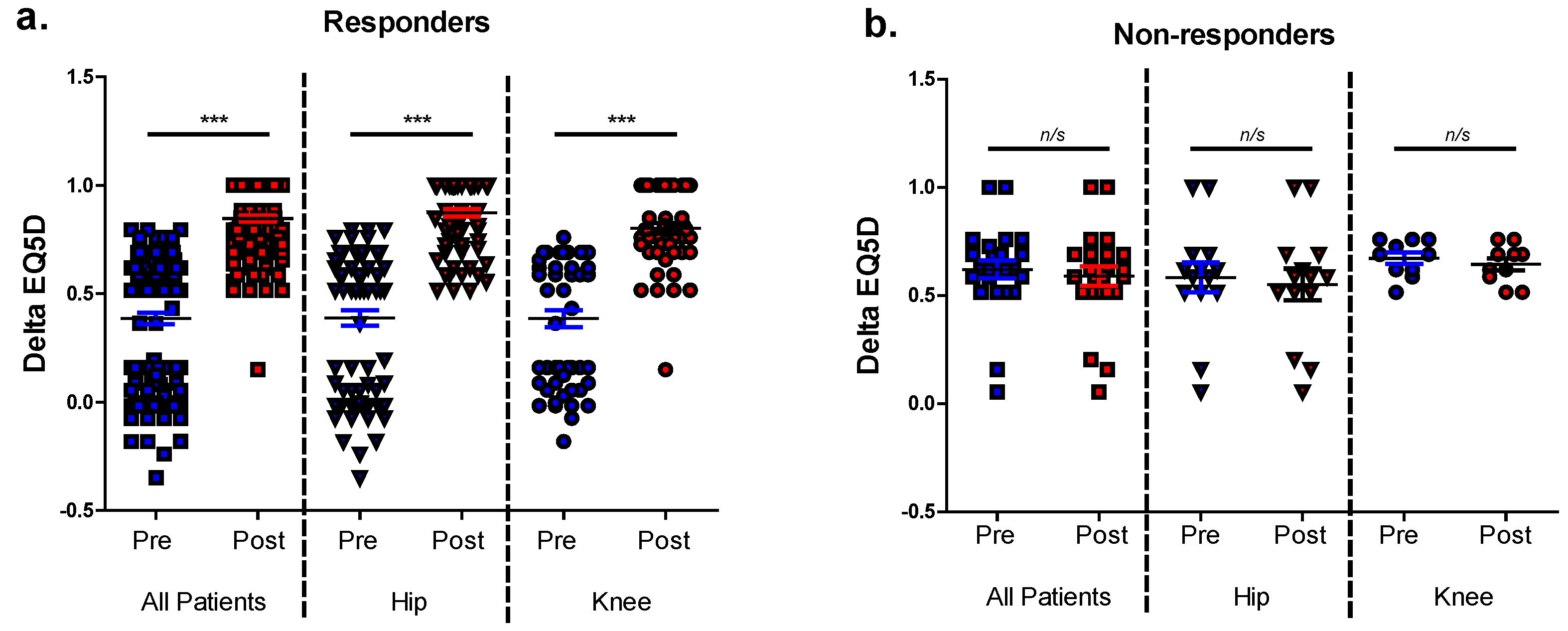
3.1. Identification of Patients with Poor Post-Operative Outcomes and Analysis of EQ5D Index Components
3.2. EQ5D Non-Responders Exhibited Greater Pre-Operative Adiposity and Differential Concentrations of Peri-Operative Synovial Fluid Inflammatory Cytokines
3.3. The Relationship between Pre-Operative Anthropometric Data and Post-Operative Change in EQ5D
3.4. The Relationship between Pre-Operative Serum and Synovial Fluid Cytokines and Post-Operative Change in EQ5D
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Matharu, G. S.; Culliford, D. J.; Blom, A. W.; Judge, A. , Projections for primary hip and knee replacement surgery up to the year 2060: an analysis based on data from The National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. Ann R Coll Surg Engl 2022, 104, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Verhaar, J. , Patient satisfaction after total knee replacement-still a challenge. Acta Orthop 2020, 91, 241–242. [Google Scholar] [CrossRef] [PubMed]
- Kahlenberg, C. A.; Nwachukwu, B. U.; McLawhorn, A. S.; Cross, M. B.; Cornell, C. N.; Padgett, D. E. , Patient Satisfaction After Total Knee Replacement: A Systematic Review. HSS J 2018, 14, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Thudium, C. S.; Lofvall, H.; Karsdal, M. A.; Bay-Jensen, A. C.; Bihlet, A. R. , Protein biomarkers associated with pain mechanisms in osteoarthritis. J Proteomics 2019, 190, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Bas, S.; Finckh, A.; Puskas, G. J.; Suva, D.; Hoffmeyer, P.; Gabay, C.; Lubbeke, A. , Adipokines correlate with pain in lower limb osteoarthritis: different associations in hip and knee. Int Orthop 2014, 38, 2577–2583. [Google Scholar] [CrossRef]
- Miller, R. E.; Miller, R. J.; Malfait, A. M. , Osteoarthritis joint pain: the cytokine connection. Cytokine 2014, 70, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Orita, S.; Koshi, T.; Mitsuka, T.; Miyagi, M.; Inoue, G.; Arai, G.; Ishikawa, T.; Hanaoka, E.; Yamashita, K.; Yamashita, M.; Eguchi, Y.; Toyone, T.; Takahashi, K.; Ohtori, S. , Associations between proinflammatory cytokines in the synovial fluid and radiographic grading and pain-related scores in 47 consecutive patients with osteoarthritis of the knee. BMC Musculoskelet Disord 2011, 12, 144. [Google Scholar] [CrossRef] [PubMed]
- de Lange-Brokaar, B. J.; Ioan-Facsinay, A.; Yusuf, E.; Visser, A. W.; Kroon, H. M.; van Osch, G. J.; Zuurmond, A. M.; Stojanovic-Susulic, V.; Bloem, J. L.; Nelissen, R. G.; Huizinga, T. W.; Kloppenburg, M. , Association of pain in knee osteoarthritis with distinct patterns of synovitis. Arthritis Rheumatol 2015, 67, 733–740. [Google Scholar] [CrossRef]
- Nanus, D. E.; Badoume, A.; Wijesinghe, S. N.; Halsey, A. M.; Hurley, P.; Ahmed, Z.; Botchu, R.; Davis, E. T.; Lindsay, M. A.; Jones, S. W. , Synovial tissue from sites of joint pain in knee osteoarthritis patients exhibits a differential phenotype with distinct fibroblast subsets. EBioMedicine 2021, 72, 103618. [Google Scholar] [CrossRef]
- Gandhi, R.; Santone, D.; Takahashi, M.; Dessouki, O.; Mahomed, N. N. , Inflammatory predictors of ongoing pain 2 years following knee replacement surgery. Knee 2013, 20, 316–318. [Google Scholar] [CrossRef]
- Hall, G. M.; Peerbhoy, D.; Shenkin, A.; Parker, C. J.; Salmon, P. , Hip and knee arthroplasty: a comparison and the endocrine, metabolic and inflammatory responses. Clin Sci (Lond) 2000, 98, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Wailoo, A.; Hernandez Alava, M.; Escobar Martinez, A. , Modelling the relationship between the WOMAC Osteoarthritis Index and EQ-5D. Health Qual Life Outcomes 2014, 12, 37. [Google Scholar] [CrossRef] [PubMed]
- Jayadev, C.; Rout, R.; Price, A.; Hulley, P.; Mahoney, D. , Hyaluronidase treatment of synovial fluid to improve assay precision for biomarker research using multiplex immunoassay platforms. J Immunol Methods 2012, 386, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Nanus, D. E.; Wijesinghe, S. N.; Pearson, M. J.; Hadjicharalambous, M. R.; Rosser, A.; Davis, E. T.; Lindsay, M. A.; Jones, S. W. , Regulation of the Inflammatory Synovial Fibroblast Phenotype by Metastasis-Associated Lung Adenocarcinoma Transcript 1 Long Noncoding RNA in Obese Patients With Osteoarthritis. Arthritis Rheumatol 2020, 72, 609–619. [Google Scholar] [CrossRef] [PubMed]
- Pearson, M. J.; Herndler-Brandstetter, D.; Tariq, M. A.; Nicholson, T. A.; Philp, A. M.; Smith, H. L.; Davis, E. T.; Jones, S. W.; Lord, J. M. , IL-6 secretion in osteoarthritis patients is mediated by chondrocyte-synovial fibroblast cross-talk and is enhanced by obesity. Sci Rep 2017, 7, 3451. [Google Scholar] [CrossRef] [PubMed]
- Sohn, D. H.; Sokolove, J.; Sharpe, O.; Erhart, J. C.; Chandra, P. E.; Lahey, L. J.; Lindstrom, T. M.; Hwang, I.; Boyer, K. A.; Andriacchi, T. P.; Robinson, W. H. , Plasma proteins present in osteoarthritic synovial fluid can stimulate cytokine production via Toll-like receptor 4. Arthritis Res Ther 2012, 14, R7. [Google Scholar] [CrossRef] [PubMed]
- Cicuttini, F. M.; Baker, J. R.; Spector, T. D. , The association of obesity with osteoarthritis of the hand and knee in women: a twin study. J Rheumatol 1996, 23, 1221–1226. [Google Scholar]
- Holliday, K. L.; McWilliams, D. F.; Maciewicz, R. A.; Muir, K. R.; Zhang, W.; Doherty, M. , Lifetime body mass index, other anthropometric measures of obesity and risk of knee or hip osteoarthritis in the GOAL case-control study. Osteoarthritis Cartilage 2011, 19, 37–43. [Google Scholar] [CrossRef]
- Wijesinghe, S. N.; Badoume, A.; Nanus, D. E.; Sharma-Oates, A.; Farah, H.; Certo, M.; Alnajjar, F.; Davis, E. T.; Mauro, C.; Lindsay, M. A.; Jones, S. W. , Obesity defined molecular endotypes in the synovium of patients with osteoarthritis provides a rationale for therapeutic targeting of fibroblast subsets. Clin Transl Med 2023, 13, e1232. [Google Scholar] [CrossRef]
- Philp, A. M.; Butterworth, S.; Davis, E. T.; Jones, S. W. , eNAMPT Is Localised to Areas of Cartilage Damage in Patients with Hip Osteoarthritis and Promotes Cartilage Catabolism and Inflammation. Int J Mol Sci 2021, 22. [Google Scholar] [CrossRef]
- Philp, A. M.; Collier, R. L.; Grover, L. M.; Davis, E. T.; Jones, S. W. , Resistin promotes the abnormal Type I collagen phenotype of subchondral bone in obese patients with end stage hip osteoarthritis. Sci Rep 2017, 7, 4042. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, T.; Church, C.; Tsintzas, K.; Jones, R.; Breen, L.; Davis, E. T.; Baker, D. J.; Jones, S. W. , Vaspin promotes insulin sensitivity of elderly muscle and is upregulated in obesity. J Endocrinol 2019. [Google Scholar] [CrossRef] [PubMed]
- Wilhelmsen, A.; Tsintzas, K.; Jones, S. W. , Recent advances and future avenues in understanding the role of adipose tissue cross talk in mediating skeletal muscle mass and function with ageing. Geroscience 2021, 43, 85–110. [Google Scholar] [CrossRef] [PubMed]
- Pozzobon, D.; Ferreira, P. H.; Blyth, F. M.; Machado, G. C.; Ferreira, M. L. , Can obesity and physical activity predict outcomes of elective knee or hip surgery due to osteoarthritis? A meta-analysis of cohort studies. BMJ Open 2018, 8, e017689. [Google Scholar] [CrossRef] [PubMed]
- Bachmeier, C. J.; March, L. M.; Cross, M. J.; Lapsley, H. M.; Tribe, K. L.; Courtenay, B. G.; Brooks, P. M.; Arthritis, C.; Outcome Project, G. , A comparison of outcomes in osteoarthritis patients undergoing total hip and knee replacement surgery. Osteoarthritis Cartilage 2001, 9, 137–146. [Google Scholar] [CrossRef] [PubMed]
- O'Brien, S.; Bennett, D.; Doran, E.; Beverland, D. E. , Comparison of hip and knee arthroplasty outcomes at early and intermediate follow-up. Orthopedics 2009, 32, 168. [Google Scholar]
- Choi, J. K.; Geller, J. A.; Yoon, R. S.; Wang, W.; Macaulay, W. , Comparison of total hip and knee arthroplasty cohorts and short-term outcomes from a single-center joint registry. J Arthroplasty 2012, 27, 837–841. [Google Scholar] [CrossRef]
| All Joints | Hips | Knees | |
|---|---|---|---|
| EQ5Di | |||
| Responders | 87% (139) | 89% (86) | 84% (53) |
| Non-responders | 13% (21) | 11% (11) | 16% (10) |
| Pain/discomfort | |||
| Responders | 72% (123) | 77% (81) | 63% (42) |
| Non-responders | 28% (49) | 23% (24) | 37% (25) |
| Mobility | Self -Care | Usual Activities | Pain/Discomfort | Anxiety/Depression | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | |
| Non-responders | ||||||||||
| All | ||||||||||
| L1 | 19%(14) | 18%(13) | 80%(91) | 75%(86) | 17%(12) | 13%(9) | 4%(2) | 4%(2) | 80%(95) | 77%(92) |
| L2 | 81%(60) | 82%(61) | 20%(23) | 24%(27) | 80%(57) | 83%(59) | 89%(41) | 89%(41) | 19%(23) | 22%(26) |
| L3 | 0%(0) | 0%(0) | 0%(0) | 1%(1) | 3%(2) | 4%(3) | 7(3) | 7(3) | 1%(1) | 1%(1) |
| Hips | ||||||||||
| L1 | 23%(9) | 23%(9) | 75%(45) | 70%(42) | 23%(9) | 21%(8) | 10%(2) | 10%(2) | 79%(54) | 79%(53) |
| L2 | 78%(31) | 78%(31) | 25%(15) | 30%(18) | 74%(29) | 74%(29) | 76%(16) | 76%(16) | 19%(13) | 21%(14) |
| L3 | 0%(0) | 0%(0) | 0%(0) | 0%(0) | 3%(1) | 5%(2) | 14%(3) | 14%(3) | 2%(1) | 2%(1) |
| Knees | ||||||||||
| L1 | 15%(5) | 12%(4) | 85%(46) | 82%(44) | 9%(3) | 3%(1) | 0%(0) | 0%(0) | 80%(41) | 77%(39) |
| L2 | 85%(29) | 88%(30) | 15%(8) | 17%(9) | 88%(28) | 94%(30) | 100%(25) | 100%(25) | 20%(10) | 24%(12) |
| L3 | 0%(0) | 0%(0) | 0%(0) | 2%(1) | 3%(1) | 3%(1) | 0%(0) | 0%(0) | 0%(0) | 0%(0) |
| Responders | ||||||||||
| All | ||||||||||
| L1 | 0%(0) | 100%(91) | 0%(0) | 96%(48) | 0%(0) | 90%(86) | 0%(0) | 76%(93) | 0%(0) | 92%(44) |
| L2 | 100%(91) | 0%(0) | 96%(48) | 4%(2) | 87%(83) | 10%(100 | 54%(66) | 24%(30) | 88(42) | 8%(4) |
| L3 | 0%(0) | 0%(0) | 4%(2) | 0%(0) | 14%(13) | 0%(0) | 46%(57) | 0%(0) | 13%(6) | 0%(0) |
| Hips | ||||||||||
| L1 | 0%(0) | 100%(59) | 0%(0) | 95%(37) | 0%(0) | 89%(55) | 0%(0) | 85%(69) | 0%(0) | 91%(30) |
| L2 | 100%(59) | 0%(0) | 95%(37) | 5%(2) | 86%(53) | 11%(7) | 61%(49) | 15%(12) | 85%(28) | 9%(3) |
| L3 | 0%(0) | 0%(0) | 5%(2) | 0%(0) | 15%(9) | 0%(0) | 40%(32) | 0%(0) | 15%(5) | 0%(0) |
| Knees | ||||||||||
| L1 | 0%(0) | 100%(32) | 0%(0) | 100%(11) | 0%(0) | 91%(31) | 0%(0) | 57%(24) | 0%(0) | 93%(14) |
| L2 | 100%(32) | 0%(0) | 100%(11) | 0%(0) | 88%(30) | 9%(3) | 41%(17) | 43%(18) | 93%(14) | 7%(1) |
| L3 | 0%(0) | 0%(0) | 0%(0) | 0%(0) | 12%(4) | 0%(0) | 60%(25) | 0%(0) | 7%(1) | 0%(0) |
| All Patients | Responders | Non-responders | ||||
|---|---|---|---|---|---|---|
| Age (years) | 70 (62,75) | 70 (62, 75) | 72.5 (63.5, 76.5) | |||
| Height (cm) | 166 (160, 175) | 167 (160, 175) | 163 (160, 173) | |||
| Weight (kg) | 75.7 (67.4, 91.7) | 75.3 (66, 89.9) | 81.4 (73, 93.7) | |||
| BMI (kg/m2) | 27.3 (24.8, 30.7) | 26.8 (24.6, 30,4) | 29.9 (27.5, 33.6)* | |||
| WC (cm) | 96.3 (85.3, 107 ) | 96 (84, 105) | 108 (91, 112)* | |||
| HC (cm) | 107 (99, 113) | 106 (99, 112) | 113 (104, 121)* | |||
| WHR | 0.91 (0.84, 0.96) | 0.91 (0.84, 0.95) | 0.92 (0.88, 0.98) | |||
| Joint Space (mm) | 0 (0,1) | 0 (0, 1) | 0 (0, 3.3) | |||
| KL Grade | 4 (3, 4) | 4 (3, 4) | 4 (2.8, 4) | |||
| Serum | Synovial Fluid | Serum | Synovial Fluid | Serum | Synovial Fluid | |
| TNFα (pg/ml) | 5.1 (4.2, 5.6) | 5.1 (2.8, 9.5) | 5.1 (4.2, 5.6) | 5.1 (2.8, 9.5) | 5.2 (4, 5.6) | 5.1 (1.4, 14.0) |
| Visfatin (ng/ml) | 2.6 (1.8, 3.3) | 0 (0, 32) | 2.6 (1.8, 3.3) | 0 (0, 36) | 2.6 (1.8, 3.3) | 0 (0, 0) |
| IL10 (pg/ml) | 4.81 (4.46, 4.99) | 17.3 (12.2, 22.6) | 4.8 (4.46,4.99) | 17.3 (11.5, 21.6) | 4.7 (4.46, 5.05) | 21.6 (16.1, 31.3) |
| IL1B (pg/ml) | 15.9 (13.7, 17.8) | 25.1 (9.6, 31.6) | 15.9 (13.3, 17.8) | 28.4 (9.0, 31.6) | 16.1 (14.5, 18.2) | 16.3 (7.2, 36.3) |
| DKK1 (ng/ml) | 3.3 (2.3, 4.7) | 0.50 (0.35, 0.71) | 3.3 (2.3, 4.7) | 0.48 (0.35, 0.72) | 3.6 (2.2, 4.7) | 0.53 (0.41, 0.84) |
| MIP1α (ng/ml) | 0.42 (0.03, 0.54) | 0.34 (0.24, 0.39) | 0.42 (0.03, 0.53) | 0.34 (0.24, 0.39) | 0.46 (0.02, 0.60) | 0.43 (0.16, 0.46) |
| gal1 (ng/ml) | 43.9 (31.1, 58.0) | 110 (87, 126) | 40.7 (29.9, 57.7) | 109 (86, 127) | 53.4 (43.2, 67.8) | 111 (90, 125) |
| Chemerin (ng/ml) | 5.6 (3.4, 7.9) | 3.0 (2.4, 3.6) | 5.6 (3.5, 8.0) | 3.0 (2.4, 3.6) | 4.8 (2.7, 6.8) | 3.3 (3.1, 4.0) |
| Eotaxin (pg/ml) | 125 (61, 228) | 28.9 (9.5, 42.6) | 125 (62, 228) | 28.9 (9.5, 42.6) | 82 (61, 214) | 28.9 (9.5, 42.6) |
| gp130 (ng/ml) | 93 (69, 105) | 71.4 (61.6 76.8) | 93 (69, 104) | 71.4 (61.5, 77.2) | 102 (56, 108) | 67.6 (58.9, 76.8) |
| ip10 (pg/ml) | 23.4 (18.4, 32.4) | 104.4 (70.7, 151.4 | 23.9 (18.4, 36.7) | 106.3 (70.4, 152.9) | 22.8 (17.4, 26.6) | 98.9 (73.2, 265.1) |
| MCP1 (ng/ml) | 0.35 (0.25, 0.46) | 0.30 (0.15, 0.61) | 0.35 (0.25, 0.47) | 0.29 (0.15, 0.64) | 0.35 (0.27, 0.41) | 0.30 (0.18, 0.42) |
| IL7 (pg/ml) | 2.7 (1.8, 3.9) | 4.0 (2.8, 5.2) | 2.7 (1.8, 3.4) | 4.0 (2.8, 5.2) | 2.9 (2.2, 4.4) | 4.6 (4.0, 6.3) |
| MIP3α (pg/ml) | 34.4 (8.8, 59.9) | 22.7 (13.1, 42.6) | 33.5 (8.8, 54.7) | 22.9 (13.8, 43.7) | 62.8 (7.1, 71.2) | 9.4 (7.3, 42.1) |
| Amphiregulin (ng/ml) | 0.59 (0.59, 0.59) | 1.36 (0.55, 1.36) | 0.59 (0.48, 0.59) | 1.36 (0.55, 1.36) | 0.59 (0.59, 0.59) | 1.36 (0.78, 1.65) |
| IL15 (pg/ml) | 4.0 (3.0, 4.7) | 31.1 (20.9, 35.2) | 4.0 (3.0, 4.9) | 31.1 (18.8, 34.9) | 3.4 (3.1, 3.8) | 34.9 (27.0, 37.3) |
| Aggrecan (pg/ml) | 163 (116, 217) | 0 (0, 114) | 163 (116, 217) | 0 (0, 114) | 116 (116, 204) | 0 (0, 244) |
| Resistin (ng/ml) | 14.5 (11.2, 18.3) | 2.90 (1.72, 5.19) | 14.5 (11.2, 19.0) | 2.96 (1.99, 5.70) | 14.9 (8.7, 16.2) | 0.97 (0.53, 2.65)* |
| Serpin E1 (ng/ml) | 135 (100, 167) | 15.6 (8.5, 42.7) | 137 (105, 167) | 16.2 (8.4, 49.4) | 113 (19, 165) | 11.0 (6.6, 18.3) |
| Adiponectin(ug/ml) | 9.9 (6.34, 13.5) | 2.7 (2.0, 4.6) | 9.9 (6.8, 14.2) | 2.8 (2.0, 5.3) | 8.5 (1.4, 11.5) | 2.5 (1.6, 3.2) |
| IL6 (pg/ml) | 2.1 (0.0, 2.7) | 132 (57, 453) | 2.1 (0, 2.8) | 175 (64, 577) | 0 (0, 2.0) | 69 (8, 222) |
| Leptin (ng/ml) | 13.1 (6.7, 26.1) | 17.3 (7.1, 54.6) | 12.6 (6.3, 26.1) | 16.3 (6.5, 48.1) | 23.3 (12.7, 27.6) | 54.5 (40.3, 67.9)* |
| FABP4 (ng/ml) | 18.0 (12.6, 28.2) | 16.7 (8.2, 81.4) | 17.9 (11.8, 27.2) | 16.1 (7.7, 66.0) | 18.8 (15.6, 41.0) | 60.1 (11.7, 159.6) |
| MIP1β (ng/ml) | 152 (105, 184) | 55.9 (0, 105.3) | 150 (101, 187) | 55.9 (0, 105.3) | 128 (85, 165) | 0 (0, 80.6) |
| Linear regression coefficient (95% CI) † | r | p-value | |
|---|---|---|---|
| AGE | -0.003 (-0.012, 0.006) | 0.065 | 0.564 |
| Height (cm) | -0.005 (-0.013, 0.003) | 0.137 | 0.228 |
| Weight (kg) | -0.005 (-0.009, -0.00002) | 0.222 | 0.049 |
| BMI | -0.012 (-0.026, 0.003) | 0.181 | 0.108 |
| Waist circumference (cm) | -0.003 (-0.007, 0.0007) | 0.193 | 0.104 |
| Hip circumference (cm) | -0.003 (-0.007, 0.002) | 0.145 | 0.225 |
| WHR | -0.456 (-1.35, 0.440) | 0.121 | 0.313 |
| Joint Space (mm) | -0.023 (-0.075, 0.029) | 0.103 | 0.376 |
| K and L grade | 0.015 (-0.077, 0.106) | 0.037 | 0.751 |
| Linear regression coefficient (95% CI)† | r | p-value | Multiple Linear regression coefficient (95% CI) ‡ | r | p-value | |
|---|---|---|---|---|---|---|
| TNF-α | -0.006 (-0.04, 0.028) | 0.046 | 0.715 | -0.004 (-0.054, 0.046) | 0.293 | 0.872 |
| Visfatin | 0.001 (-0.006, 0.07) | 0.023 | 0.856 | 0.001 (-0.007, 0.008) | 0.291 | 0.836 |
| IL-10 | -0.0003 (-0.005, 0.005) | 0.013 | 0.92 | -0.001 (-0.006, 0.005) | 0.291 | 0.824 |
| IL-1β | 0.002 (-0.001, 0.006) | 0.174 | 0.165 | 0.003 (-0.001, 0.007) | 0.346 | 0.175 |
| DKK1 | -0.024 (-0.065, 0.017) | 0.147 | 0.243 | -0.031 (-0.082, 0.021) | 0.344 | 0.239 |
| MIP1α | 0.042 (-0.223, 0.306) | 0.04 | 0.754 | 0.014 (-0.307, 0.336) | 0.292 | 0.928 |
| Galectin1 | -0.0008 (-0.003, 0.001) | 0.097 | 0.442 | -0.0001 (-0.003, 0.002) | 0.292 | 0.932 |
| Chemerin | -0.006 (-0.026, 0.013) | 0.079 | 0.531 | -0.007 (-0.032, 0.018) | 0.301 | 0.586 |
| Eotaxin | 0.00014 (-0.00028, 0.00055 ) | 0.082 | 0.519 | 0.00013 (-0.001, 0.001) | 0.284 | 0.968 |
| gp130 | -0.0014 (-0.004, 0.001) | 0.170 | 0.175 | -0.002 (-0.004, 0.001) | 0.336 | 0.230 |
| IP10 | 0.00046 (-0.003, 0.004) | 0.034 | 0.786 | 0.001 (-0.003, 0.005) | 0.297 | 0.679 |
| MCP1 | 0.004 (-0.059, 0.067) | 0.017 | 0.895 | 0.028 (-0.049, 0.104) | 0.308 | 0.472 |
| IL-7 | -0.018 (-0.076, 0.04) | 0.079 | 0.531 | -0.007 (-0.092, 0.078) | 0.293 | 0.872 |
| MIP3α | 6.8x10-6 (-0.00013, 0.00014) | 0.013 | 0.919 | 6.02x10-6 (-0.00016, 0.00014) | 0.292 | 0.936 |
| Amphiregulin | 0.091 (-0.340, 0.522) | 0.054 | 0.674 | 0.240 (-0.301, 0.780) | 0.315 | 0.377 |
| IL-15 | 0.002 (-0.012, 0.016) | 0.034 | 0.788 | 0.001 (-0.016, 0.018) | 0.290 | 0.920 |
| Aggrecan | 7.5x10-5 (-0.00014, 0.00029) | 0.088 | 0.487 | 0.0004 (-0.0001, 0.001) | 0.365 | 0.106 |
| Resistin | 0.007 (-0.001, 0.016) | 0.219 | 0.085 | 0.006 (-0.005, 0.016) | 0.329 | 0.288 |
| Serpin E1 | 0.0005 (-0.0006, 0.0016) | 0.110 | 0.383 | 0.001 (-0.001, 0.002) | 0.318 | 0.361 |
| Adiponectin | 0.008 (-0.004, 0.020) | 0.165 | 0.193 | 0.006 (-0.01, 0.022) | 0.310 | 0.467 |
| IL-6 | 1.9x10-5 (-0.001, 0.009) | 0.005 | 0.970 | -8.3x10-5 (-0.001, 0.001) | 0.293 | 0.881 |
| Leptin | 0.00019 (-0.004, 0.004) | 0.012 | 0.925 | 0.00014 (-0.007, 0.007) | 0.279 | 0.967 |
| FABP4 | 0.001 (-0.001, 0.004) | 0.145 | 0.252 | 0.001 (-0.002, 0.004) | 0.308 | 0.494 |
| MIP1β | 0.0006 (-0.0004, 0.0016) | 0.209 | 0.102 | 0.001 (-0.001, 0.002) | 0.312 | 0.430 |
| Linear regression coefficient (95% CI)† | r | p-value | Multiple Linear regression coefficient (95% CI) ‡ | r | p-value | |
|---|---|---|---|---|---|---|
| TNF-α | 0.001 (-0.018, 0.020) | 0.016 | 0.921 | 0.008 (-0.022, 0.037) | 0.544 | 0.584 |
| Visfatin | 0.001 (-0.001, 0.003) | 0.195 | 0.222 | 0.001 (-0.001, 0.004) | 0.560 | 0.352 |
| IL-10 | -0.0004 (-0.010, 0.009) | 0.012 | 0.940 | -0.001 (-0.016, 0.013) | 0.537 | 0.843 |
| IL-1β | 0.0005 (-0.006, 0.007) | 0.024 | 0.881 | 0.002 (-0.006, 0.011) | 0.544 | 0.589 |
| DKK1 | -0.073 (-0.225, 0.08) | 0.153 | 0.339 | -0.120 (-0.543, 0.302) | 0.545 | 0.562 |
| MIP1α | -0.284 (-0.882, 0.313) | 0.152 | 0.342 | -0.633 (-0.155, 0.283) | 0.587 | 0.166 |
| Galectin1 | 0.0018 (-0.0019, 0.0056) | 0.156 | 0.329 | 0.0003 (-0.006, 0.005) | 0.536 | 0.906 |
| Chemerin | -0.023 (-0.099, 0.052) | 0.100 | 0.534 | 0.004 (-0.117, 0.126) | 0.536 | 0.940 |
| Eotaxin | -0.0007 (-0.002, 0.001) | 0.146 | 0.362 | -0.001 (-0.002, 0.001) | 0.545 | 0.559 |
| gp130 | -0.001 (-0.008, 0.006) | 0.054 | 0.738 | -0.003 (-0.013, 0.007) | 0.545 | 0.565 |
| IP10 | 0.00013 (-0.0005, 0.0007) | 0.069 | 0.670 | 0.000019 (-0.001, 0.001) | 0.535 | 0.960 |
| MCP1 | 0.026 (-0.052, 0.105) | 0.109 | 0.497 | 0.06 (-0.03, 0.155) | 0.582 | 0.193 |
| IL-7 | -0.033 (-0.093, 0.028) | 0.172 | 0.283 | -0.031 (-0.112, 0.05) | 0.533 | 0.438 |
| MIP3α | 0.002 (-0.002, 0.006) | 0.164 | 0.307 | 0.001 (-0.005, 0.007) | 0.541 | 0.654 |
| Amphiregulin | -0.158 (-0.343, 0.026) | 0.268 | 0.09 | -0.24 (-0.5, 0.021) | 0.619 | 0.07 |
| IL-15 | -0.001 (-0.009, 0.008) | 0.020 | 0.90 | -0.003 (-0.016, 0.010) | 0.543 | 0.615 |
| Aggrecan | -0.0005 (-0.0015, 0.0005) | 0.169 | 0.29 | -0.0004 (-0.002, 0.001) | 0.538 | 0.773 |
| Resistin | 0.0011 (-0.008, 0.010) | 0.041 | 0.801 | -0.002 (-0.016, 0.012) | 0.538 | 0.777 |
| Serpin E1 | 0.0018 (-0.0019, 0.0054) | 0.154 | 0.338 | 0.001 (-0.006, 0.007) | 0.537 | 0.808 |
| Adiponectin | 0.032 (-0.004, 0.069) | 0.274 | 0.083 | 0.022 (-0.055, 0.098) | 0.545 | 0.560 |
| IL-6 | 0.0013 (-0.00001, 0.00028) | 0.288 | 0.072 | 0.0001 (-0.00008, 0.0003) | 0.569 | 0.223 |
| Leptin | 0.0002 (-0.0024, 0.0029) | 0.028 | 0.868 | 0.0002 (-0.006, 0.006) | 0.560 | 0.950 |
| FABP4 | 0.00004 (-0.00009, 0.00018) | 0.104 | 0.521 | -0.001 (-0.003, 0.001) | 0.552 | 0.348 |
| MIP1β | 0.00044 (-0.0012, 0.0021) | 0.089 | 0.585 | -0.001 (-0.003, 0.001) | 0.566 | 0.239 |
| r | p-value | Unstandardized Coefficients (B) | ||||
|---|---|---|---|---|---|---|
| Cytokine | BW | Constant | Equation | |||
| Amph, BW | 0.434 | 0.023 | -0.108 | -0.0006 | 1.052 | ΔEQ5D = -0.108 [Amph ng/ml] -0.0006 [BW kg] + 1.053 |
| IL-6, BW | 0.418 | 0.035 | 7.4x10-5 | -0.006 | 0.871 | ΔEQ5D = 7.4x10-5 [IL-6 ng/ml] -0.006 [BW kg] + 0.871 |
| Amph, IL-6, BW | 0.470 | 0.035 | -0.142 (Amph) 8.3x10-5 (IL-6) |
-0.005 | 0.919 | ΔEQ5D = -0.142 [Amph ng/ml] +8.3x10-5 [IL-6 ng/ml] -0.005 [BW kg] + 0.919 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





