1. Introduction
Myopia or near-sightedness is a growing public health concern [
1] and is predicted to affect half of the world's population by 2050 [
2]. The prevalence of myopia among urban Indian children is likewise expected to rise from 21.2% in 2019 to 48.1% by 2050 [
3]. Myopia has significant social, educational, and economic consequences, reducing the quality of life [
1], with high myopia (spherical equivalent ≤ -6.00 D) increasing the risk of sight-threatening complications and irreversible vision loss [
4].
There is an increasing interest in myopia management and control among practitioners worldwide [
5]. An array of childhood myopia control options exists, including glasses (single, bifocal, multifocal), contact lenses (soft, rigid, orthokeratology, peripheral defocus), pharmacological (topical atropine), and lifestyle changes (increased outdoor time) [
6,
7,
8]. Emerging myopia control treatments have raised interest in the prevention and control of childhood myopia. Without clinical guidelines, effective strategies remain underused, with over 95% of practitioners relying on non-evidence-based single-vision glasses and advice on visual hygiene [
9]. This highlights the urgent need for global clinical guidelines on myopia management [
5,
10,
11,
12]. Furthermore, little is known about eye-care practitioners' understanding of the consequences of myopia, diagnostic procedures, and treatment approaches for childhood myopia in India. The previous study done nearly two years ago [
13] on childhood myopia practice patterns in India is limited to inexperienced optometrists (~80% with < 5 years of clinical experience) and only from a pocket in northern India (regional), not reflecting the diverse practice patterns throughout the country [
14].
This survey aims to explore and provide updated information on practising optometrists' knowledge, perspective, and practices in diagnosing and managing childhood myopia in India. Furthermore, it assesses the evidence guiding optometric practice and the involvement of adult caregivers in decisions regarding myopia in children.
2. Methods
An online survey using Google Forms (Google Inc., CA, USA) was administered to practising optometrists in India between 27 March 2021 and 27 September 2022. Ethics approval for the study was obtained from the Mangala Institutional Ethical Committee, and the study complied with the tenets of the Declaration of Helsinki.
2.1. Practitioner's survey
The questionnaire used in this study was adapted from a survey conducted among Australian optometrists [
11]. Following a focus group discussion comprising four optometrists with experience of > 5 years in clinical practice, the questionnaire was adopted to fit the scope and context of Indian optometric practice. The content validity was kept the same through a focused group discussion that resulted in the final version of the survey. We omitted the question about therapeutic endorsement, as it is not recognized in Indian optometry. The draft was piloted among five optometrists and five final-year optometry students to ensure the questions' relevance, accuracy, clarity, and interpretation. The required time to complete the survey was approximately 7 – 10 minutes. The survey was distributed to optometrists working in India through state and national optometric associations via email, WhatsApp, Telegram, Facebook, and India Vision Institute's E-Newsletter. Reminders to fill in the survey were sent via email and social media every two weeks during the study period. The survey consisted of a statement at the beginning that the participation is voluntary, and their submission of responses reflects their consent.
We included demographic questions (education and occupation) to filter out opticians and students. Only responses from optometrists practising in India were considered—the survey aimed to understand their childhood myopia knowledge and practices. Duplicates were prevented with email address restrictions and questions on prior survey participation. Participation was voluntary, with no incentives. Responses were kept anonymous and treated confidentially. Sample size
The survey reached approximately ~10,000 optometrists. To ensure a representative response with a margin of error of ±5% and a confidence level of 95%, a sample size of 370 responses was deemed necessary [
15].
2.2. Questionnaire design
This survey was a 26-item questionnaire which is described in detail elsewhere [
11], mainly aimed to understand the practicing optometrists’:
Understanding of the natural history and ocular complications associated with myopia.
Clinical practice behavior related to the diagnosis and management of myopia in children aged 16 years or younger.
Potential barriers to providing optimal myopia care.
Source of evidence that clinicians use as a guide to their practice.
Extent to which adult caregivers are involved during the decision-making process in treating childhood myopia.
Out of the 26 questions, there were 8 × multiple choice questions, 6 × matrix, 3 × open-ended, 3 × closed-ended, 3 × dropdown, 1 × Likert scale, 1 × ranking, and 1 × mixed type question (provided as supplementary material).
The definition of myopia was set at a spherical equivalent of -0.50 D or higher. Respondents were expected to complete the survey questions in the order provided by the authors and had no option to change the answer after submission.
The Checklist for Reporting Results of Internet E-Surveys (CHERRIES) guidelines was used to prepare the survey (Table 1) [
16].
Table 1.
Summary of the survey methodology.
Table 1.
Summary of the survey methodology.
| S.no |
Description |
Survey report |
| 1 |
Survey development |
A pre-validated questionnaire was revised after a focus group discussion among four optometrists to finalize the questionnaire's items |
| 2 |
Number and nature of items in the questionnaire |
A 26-item questionnaire with a mix of open and close-ended questions |
| 3 |
Reliability |
Not determined |
| 4 |
Mode of survey |
Internet-based |
| 5 |
Survey period |
27 March 2021 to 27 September 2022 |
| 6 |
Sample frame |
Open survey: Open for all optometrists across India |
| 7 |
Target population |
Optometrists practicing in India |
| 8 |
Recruitment process |
Open invitations over social media, namely Facebook, WhatsApp, E-Newsletter, and Telegram, in a target group with reminder messages every 2 weeks |
| 9 |
Participation |
Voluntary participation |
| 10 |
Survey administration |
Sequential questions administered using Google forms |
| 11 |
Informed consent |
E-consent |
| 12 |
Incentives |
None |
| 13 |
Randomization of items or questionnaires |
No randomization of items or questions |
| 14 |
Use of adoptive questions |
Yes |
| 15 |
Number of screens |
5 |
| 16 |
Review step |
Review with a back button, no alteration was possible after submission |
| 17 |
Preventing multiple entries from a single respondent, e.g., cookies used |
Limited to one response per email and one item in the questions asked for their previous participation in the survey. |
| 18 |
Data capturing |
Automatic conversion into a spreadsheet |
| 19 |
Data analysis |
Proportions of each response were calculated, and the odds were determined (p value of <0.05 was considered statistically significant) |
| 20 |
Software used for statistical analysis |
GraphPad Prism (version 6.04 for Windows, GraphPad Software, La Jolla, CA, and IBM SPSS Statistics for Windows, Version 28.0, IBM Corp |
2.3. Data analysis
The online responses from Google Forms were imported into a Microsoft Office Excel 365 spreadsheet for analysis. Statistical analyses were performed using Statistical Package for Social Sciences [IBM SPSS Statistics for Windows, Version 28.0, IBM Corp], and graphs were plotted in GraphPad Prism version 6.04 (GraphPad Software Inc.). Only completed responses were considered for analysis, and the normality of data was tested as appropriate using the Shapiro-Wilk test. Descriptive statistics method was used to calculate the percentage of responses for each question. Charts and tables were plotted in Microsoft Office Excel 365 according to data availability. Likert scales were analyzed using ordinal logistic regression, with stratification of years of practice, mode of practice and others as independent factors to model the responses. Dichotomous survey questions were analyzed using binomial logistic regression. The significance level for all statistical tests was set at p < 0.05.
3. Results
Of the 462 responses obtained, 393 (85%) were valid. Invalid data excluded were 55 (12%) respondents with duplicate responses, 8 (1.7%) were undergraduate/diploma students, and 6 (1.3%) of the responses had missing items. Among the included responses, 49.4% (n = 194) were male, and 50.6% (n = 199) were female, with distribution spread across India (North 18%, South 50%, East 10%, and West 22%). Though respondents had a wide range of clinical experience, half of the participating optometrists were within their first five years (50.9%) of clinical practice.
Among the 393 respondents, 171 (43.6%) were undergraduate optometrists, 144 (36.6%) were postgraduate optometrists, 57 (14.5%) had diploma in optometry, and 20 (5.2%) were PhD scholars/completed PhD. The majority of the respondents practised at hospitals (40.4%, n = 159), with most of the optometrists (40.2%, n = 158) managing a maximum of five young children (< 16 years of age) every week. The detailed characteristics of the respondents are listed in
Table 2.
Table 2.
Demographics of the survey responders.
Table 2.
Demographics of the survey responders.
| Characteristic |
Respondents (n=393) |
| Sex (male/female): n (%) |
194/199(49.4%/50.6%) |
| Optometric practice experience: n (%) |
0–5 years
5–10 years
10–15 years
15–20 years
> 20 years |
200 (50.9%)
62 (15.8%)
40 (10.2%)
44 (11.2%)
47 (12.0%) |
| Primary place of optometric practice: n (%) |
Hospital
Academic Institution
Independent (private) practice
Corporate practice
Optometrist pursuing post-graduation |
159 (40.4%)
63 (16.0%)
82 (20.9%)
52 (13.2%)
37 (9.5%) |
| Possess a clinical or research interest in managing childhood myopia (yes/no): n (%) |
352/41
(89.6%/10.4%) |
| Number of myopic patients under 16 years of age provided care to in a typical week: n (%) |
0–5 6–10 11–15 16–20 21–25 26–30 >30 |
158 (40.2%)
114 (29.0%)
46 (11.7%)
16 (4.1%)
18 (4.6%)
9 (2.3%)
32 (8.1)
- |
3.1. Knowledge of childhood myopia and its complications
Almost 90% of respondents indicated having a clinical/research interest in managing childhood myopia. The majority (45.3%) responded -0.50 D as the minimum correction in spherical equivalent prescribed for myopic patients. Most of the optometrists’ responses were retinal breaks (67.4%), followed by rhegmatogenous retinal detachment (45.3%) and cataracts (44.8%) as ocular pathologies associated with high myopia > -6 D (
Table 3). Identification of retinal break was statistically significant among experienced respondents (≥ ten years) (odds ratio (OR) 2.23, 95% confident Interval (CI): 1.53–3.25,
p < 0.001, whereas it was not the case among respondents with interest in myopia management (OR 1.57, 95% CI: 0.60–4.05,
p = 0.35). When stratified based on the primary place of practice, the odds of knowing retinal tear were equal within all practice patterns (Academic institution (OR 2.14, 95%CI: 1.49–3.06,
p < 0.001), corporate practice (OR 2.14, 95%CI: 1.53–2.99,
p < 0.001), hospital (OR 1.79, 95%CI: 1.17–2.74,
p = 0.007), Independent practice (OR 2.11, 95%CI: 1.48–3.01,
p < 0.001) and public health clinic (OR 1.98, 95%CI: 1.43–2.75,
p < 0.001).
Table 3.
Perspective on the associated ocular pathologies with high myopia (-6.00 D or greater).
Table 3.
Perspective on the associated ocular pathologies with high myopia (-6.00 D or greater).
| Ocular conditions |
Percentage of respondents (%) |
| Retinal breaks |
67.4 |
| Rhegmatogenous Retinal Detachment |
45.3 |
| Cataract |
44.8 |
| Exudative Retinal Detachment |
30.8 |
| Primary Open Angle Glaucoma |
29.7 |
| Primary Angle Closure Glaucoma |
18.6 |
| Age-Related Macular Degeneration |
16.9 |
| Diabetic Retinopathy |
7.6 |
3.2. Clinical workup and diagnosis of childhood myopia
Table 4 summarizes the responses to clinical procedures used to examine children with myopia for the first time. Over 75% of the respondents considered taking the family history, performing cycloplegic retinoscopy, dilated retinal examination, and cover test during the first visit. Respondents with myopia management interest and experience (≥ ten years) were more likely to note the family history of myopia (OR 3.50, 95% CI: 1.15–10.6,
p = 0.02 and OR 4.45, 95% CI: 2.81–7.07,
p < 0.001) and perform cycloplegic refraction (OR 3.50, 95% CI: 1.15–10.60,
p = 0.02 and OR 9.00, 95% CI: 4.96–16.30,
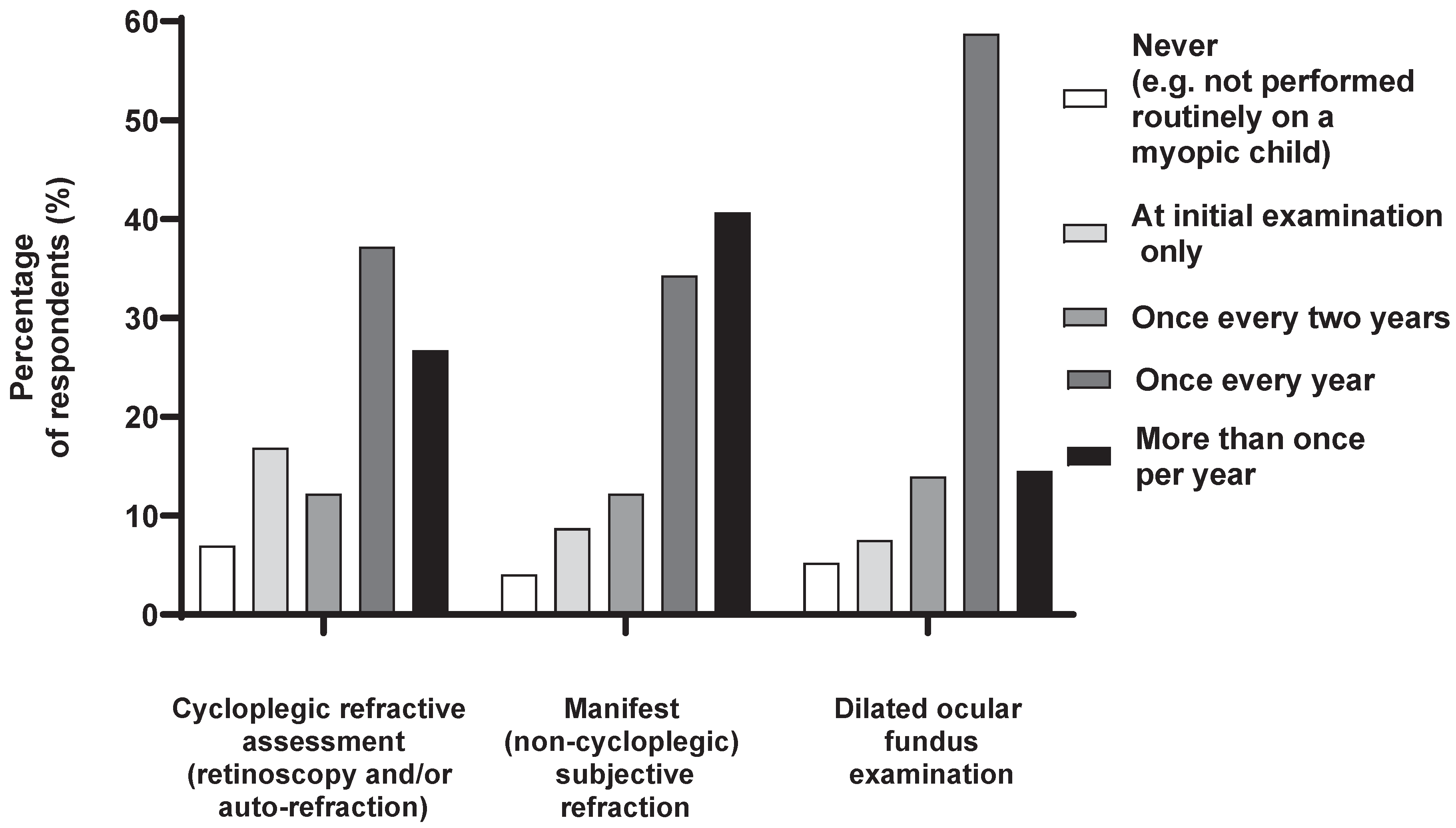
p < 0.001). Ocular biometry is performed by 46.5% of practitioners in clinical practice. Notably, 7%, 4.1%, and 5.2% responded that they never performed cycloplegic, non-cycloplegic, and dilated fundus examination procedures in the routine clinical practice on a myopic child (Fig. 1).
Table 4.
Percentage of respondents who indicated performing each clinical procedure routinely on all school-aged children (5–16 years) with myopia on initial presentation.
Table 4.
Percentage of respondents who indicated performing each clinical procedure routinely on all school-aged children (5–16 years) with myopia on initial presentation.
| Clinical Procedures |
Percentage of respondents (%) |
| Cycloplegic retinoscopy |
86.6 |
| Note patient family history of myopia |
83.7 |
| Dilated retinal fundus examination |
76.7 |
| Cover test (distance and near phoria) |
75.0 |
| Cycloplegic subjective refraction |
70.9 |
| Non-cycloplegic retinoscopy |
62.8 |
| Non-cycloplegic subjective refraction |
62.2 |
| Cycloplegic autorefraction |
52.3 |
| Intraocular pressure |
47.1 |
| Axial length measurement |
46.5 |
| Dynamic retinoscopy (e.g., MEM, NOTT Retinoscopy) |
39.5 |
| AC/A ratio |
35.5 |
| Non-cycloplegic autorefraction and stereopsis |
34.3 |
| Measurement of pupil size |
32.6 |
| Corneal topography |
21.5 |
| Retinal fundus photography – posterior pole |
14.5 |
| Retinal fundus photography – periphery |
11.6 |
| Peripheral defocus |
8.7 |
| Others |
11.2 |
Figure 1.
Percentage (%) of respondents who indicated performing each clinical procedure on a school-aged child with myopia at the nominated frequency.
Figure 1.
Percentage (%) of respondents who indicated performing each clinical procedure on a school-aged child with myopia at the nominated frequency.
3.3. Perception on intervention
Table 5 presents the perspective on the most effective management options other than single-vision distance spectacles (full correction) for myopia management. Experienced practitioners prioritized increasing time spent outdoors (OR 2.33, 95% CI: 1.58–3.45,
p < 0.001), low-moderate dose atropine (OR 2.24, 95% CI: 1.52–3.30,
p < 0.001) and visual hygiene (OR 1.93, 95% CI: 1.32–2.81,
p < 0.001) than the inexperienced ones. Practitioners with an interest in myopia management were less likely to prescribe bifocal spectacle lenses with prism (OR 0.05, 95% CI: 0.01–0.44,
p = 0.005), peripheral defocus soft contact lenses (OR 0.05, 95% CI: 0.01–0.44,
p = 0.005) and progressive addition lenses (OR 0.20, 95% CI: 0.05–0.69,
p = 0.01). The likelihood of advising increased time spent outdoors was significantly higher among academic, corporate, hospital, independent and public health practices (OR 2.45–2.92,
p < 0.001). Equally, low-moderate dose atropine and visual hygiene were a preferred mode of advice among all the practices (OR 1.82–3.23,
p < 0.001 and OR 1.93–2.04,
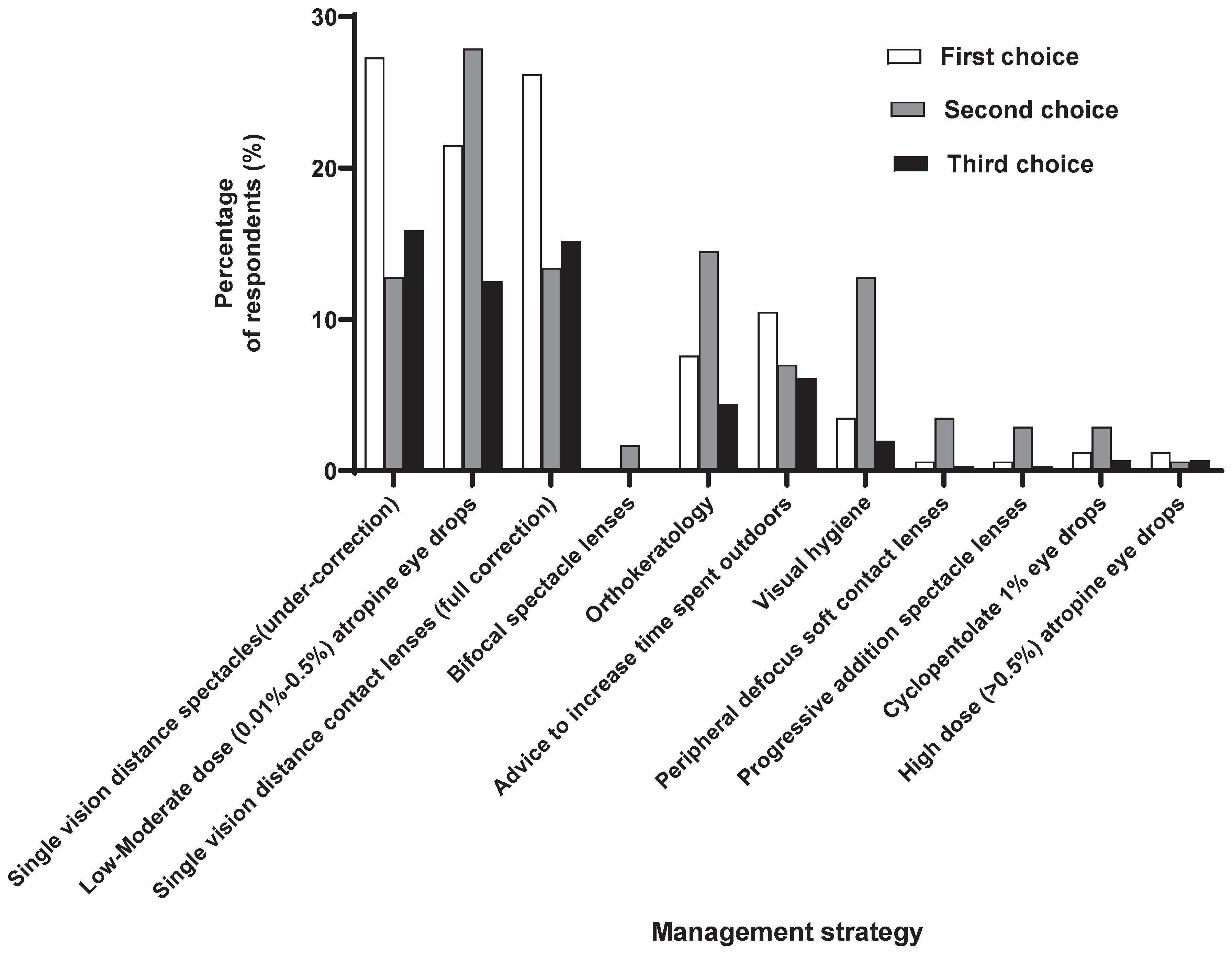
p < 0.01, respectively). When asked about their perspective on the alternative to prescribing single-vision distance spectacles (full correction), practitioners opted for single-vision (under-correction) as their next choice, followed by single-vision contact lenses (full-correction), low-moderate dose atropine (0.01%‒0.5%) eye drops, advice to increase the outdoor time, and Ortho-K (Fig. 2).
Figure 2.
Perspective on the first three options for effective management other than single vision spectacle (full correction).
Figure 2.
Perspective on the first three options for effective management other than single vision spectacle (full correction).
3.4. Influential factors on management approach
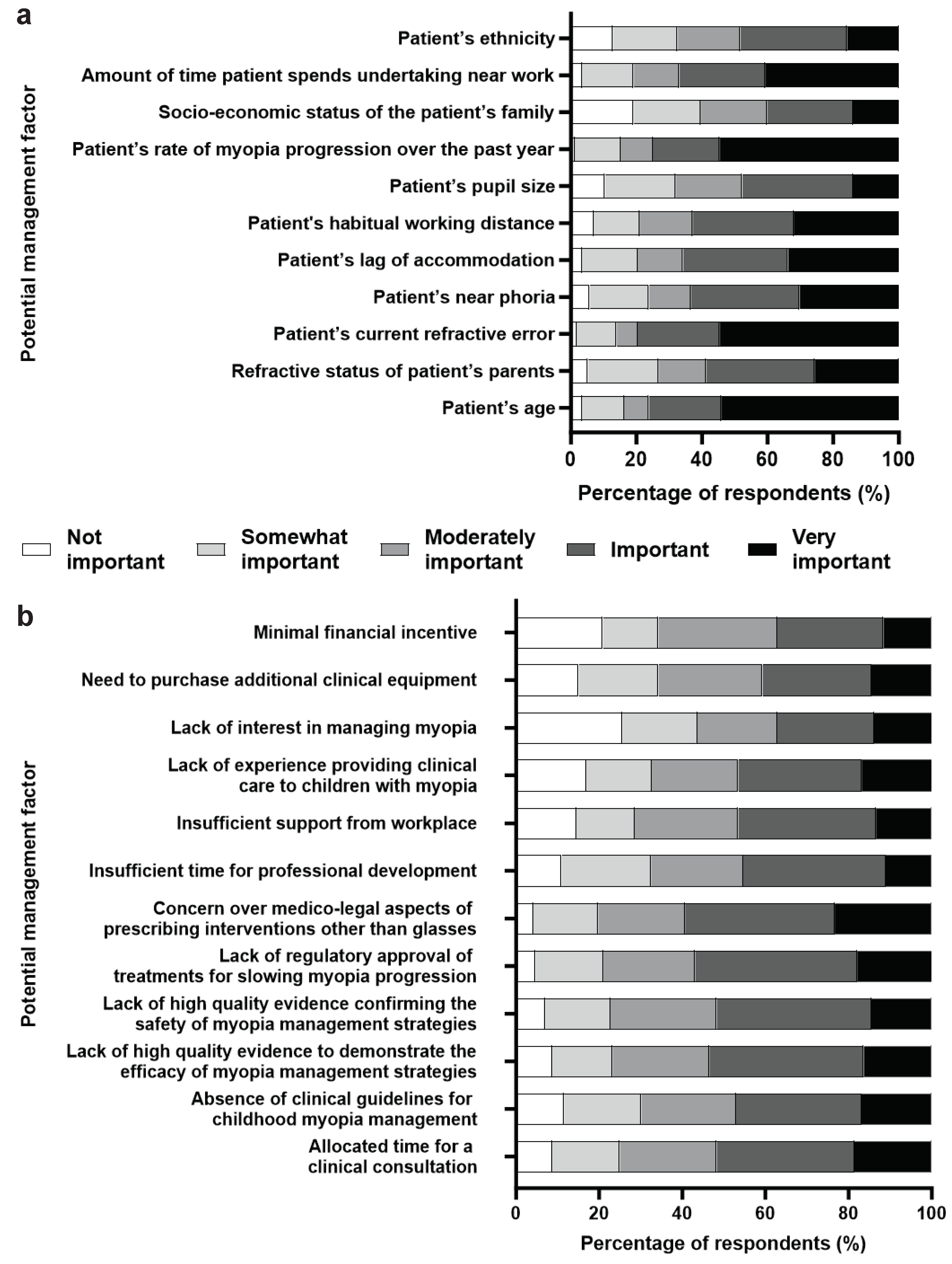
Several clinical features of the myopic patient are deemed necessary by practitioners while managing myopes (Fig. 3a). Over 50% of participants indicated that the age, current refractive error, and myopia progression over the past year are 'very important' followed by time spent in near work (40.7%).
Among the potential factors and barriers that influence optimal myopia care were concerns about the medico-legal implications of administering interventions, lack of regulatory approval of those treatments, scarcity of high-quality evidence backing up the effectiveness, inadequate consultation time, absence of clinical practice guidelines, safety of myopia management techniques which were considered 'very important' or 'important' (Fig. 3b). Experienced practitioners reported insufficient support at the workplace as a potential barrier (OR 1.88, 95% CI: 1.04–3.44, p = 0.03). Lack of minimal financial incentive in hospital-based practice (OR 1.77, 95% CI: 1.03–3.04, p = 0.03) was a barrier, whereas, for the independent practice, allotted time for consultation (OR 0.46, 95% CI: 0.23–0.95, p = 0.03), time for professional development (OR 0.47, 95% CI: 0.24–0.94, p = 0.03) and need for new equipment (OR 0.43, 95% CI: 0.21–0.86, p = 0.01) were not barriers for myopia management.
Figure 3.
Percentage of respondents (%) who rated the relative importance of each: (a) potential factor when deciding upon the management approach for a child with myopia. (b) barrier limiting their ability to provide optimal clinical care to children with myopia.
Figure 3.
Percentage of respondents (%) who rated the relative importance of each: (a) potential factor when deciding upon the management approach for a child with myopia. (b) barrier limiting their ability to provide optimal clinical care to children with myopia.
3.5. Management approaches to myopia in children
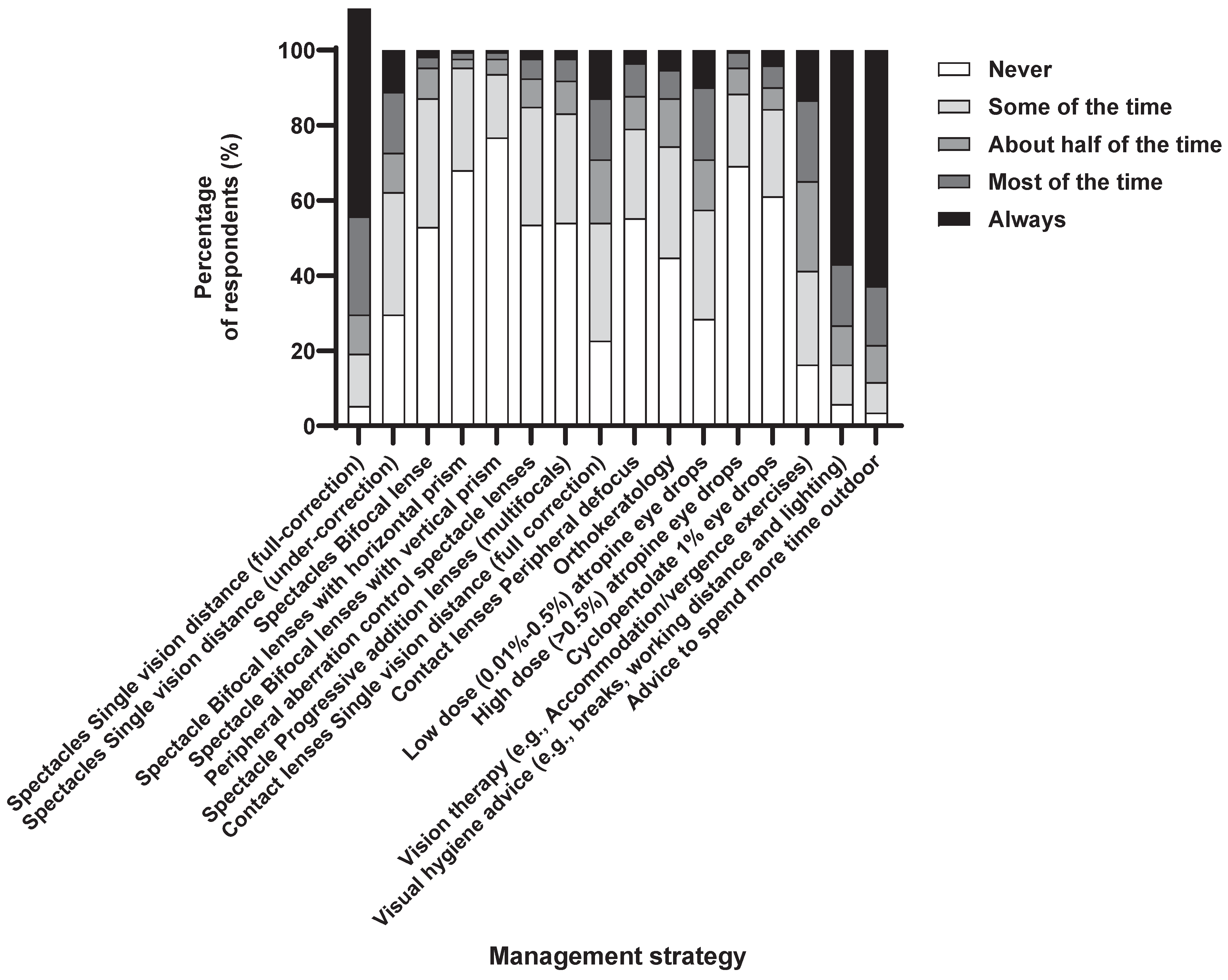
Single-vision distance (full-correction) spectacles were the most prescribed method of optical correction, with about 70.3% of respondents suggesting that they would ‘always’ or ‘mostly’ recommend this modality (Fig. 4). Visual hygiene and increased outdoor time were equally prescribed as the management strategy to children with myopia.
Figure 4.
Percentage of respondents (%) who rated the frequency with which they prescribe each management strategy to children with myopia.
Figure 4.
Percentage of respondents (%) who rated the frequency with which they prescribe each management strategy to children with myopia.
Though the perception for low-moderate dose atropine is effective (68.6%) in myopia management, it was prescribed relatively infrequently, with only 29.1% of practitioners reporting they would ‘always’ or ‘mostly’ recommend it. However, it was less likely that experienced optometrists would prescribe high-dose atropine (OR 0.40, 95% CI: 0.17–0.85, p = 0.02) and cyclopentolate (OR 0.49, 95% CI: 0.23–0.96, p = 0.04). In addition, the majority (>70%) of respondents indicated they would ‘mostly’ or ‘always’ advise on visual hygiene and increasing time spent outdoors. However, experienced optometrists were less likely to advise visual hygiene (OR 0.51, 95% CI: 0.27–0.95, p = 0.03).
Participants were asked to envision a clinical scenario for myopia management and specify when they would cease the intervention (patient age and prescription stability). Responses varied widely, with 16 years (14.5%) as the most common age criterion, and discontinuation was suggested if there was no progression in myopia for 12 months.
3.6. Source of Information
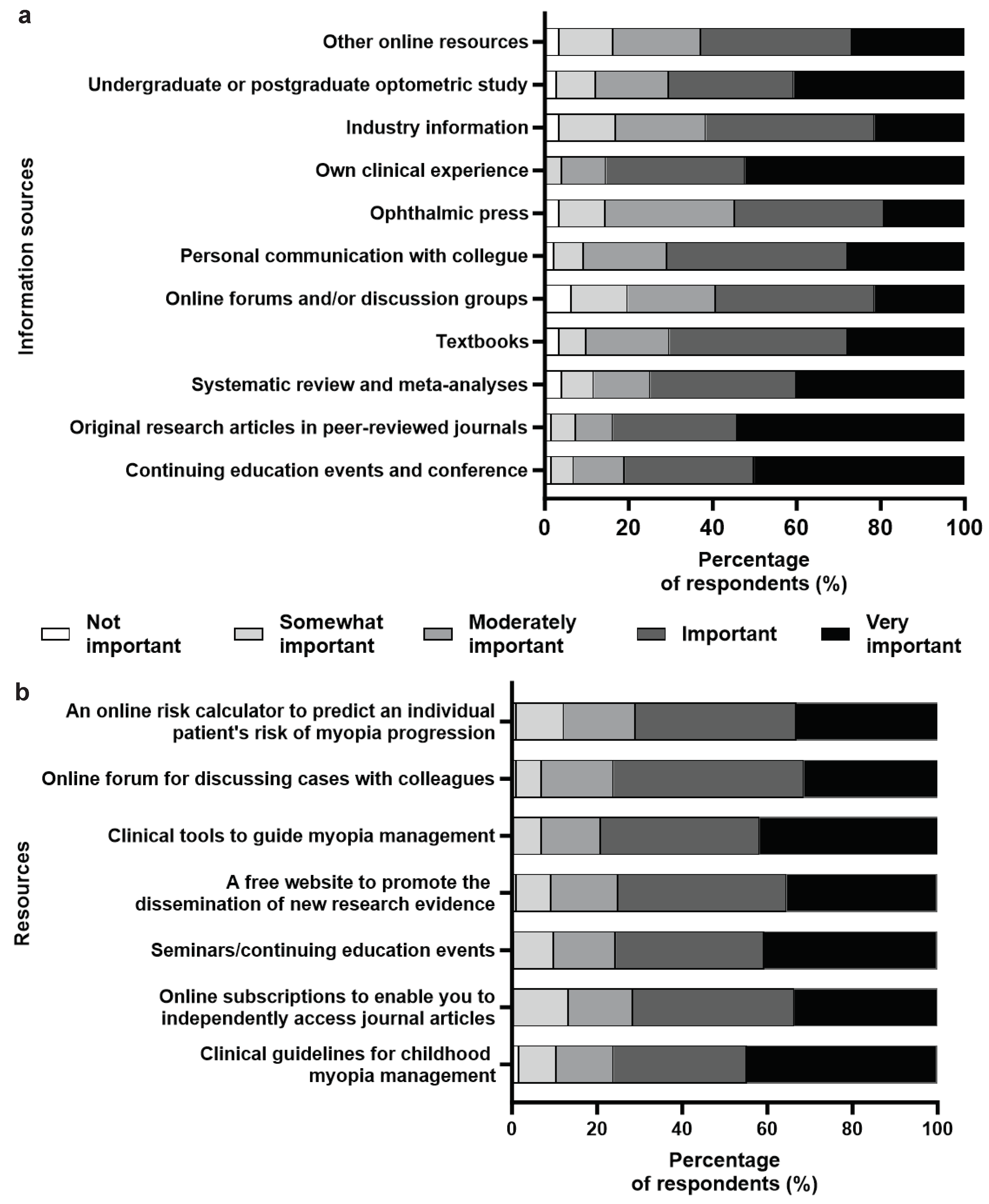
For more than half of the respondents (54.1%), the source of information for clinical management was original peer-reviewed articles, followed by their own clinical experience (52.3%), continuing medical education (CME) and conferences (50%). The least opted sources were industry information (21.5%), online forums, and resources like artificial intelligence (AI) (~20%) and ophthalmic press (19.2%) (Fig. 5a).
Figure 5.
Percentage of respondents (%) who rated the relative importance of each: (a) information source in guiding their current approach to managing childhood myopia. (b) potential resources for supporting their future clinical management of children with myopia.
Figure 5.
Percentage of respondents (%) who rated the relative importance of each: (a) information source in guiding their current approach to managing childhood myopia. (b) potential resources for supporting their future clinical management of children with myopia.
Among the resources that support the respondents' future clinical management (Fig. 5b), over 40% of the respondents mentioned clinical guidelines for childhood myopia management, seminars/continuing education events, and clinical tools to guide myopia management based upon the best available research evidence are very useful. Most (> 70%) marked all listed items as 'useful' or 'very useful'. The results were similar when categorized based on interest, practice, and experience, without any significant difference.
3.7. Engagement with caregivers
Over 40% emphasized discussing myopia's nature, long-term eye disease risks, and potential myopia progression with adult caregivers (Fig. 6). Over 70% found it essential to explain myopia, its physical changes, possible causes, increasing severity, and treatment benefits versus risks for a child. There were no significant differences based on experience or practice patterns, except for discussing treatment options. Regarding caregiver involvement in myopia management decisions, over 72% consider caregiver opinions or decide collaboratively after discussing management options.
Figure 6.
Percentage of respondents (%) who rated the relative importance of each potential topic to discuss with an adult caregiver of a child with myopia.
Figure 6.
Percentage of respondents (%) who rated the relative importance of each potential topic to discuss with an adult caregiver of a child with myopia.
4. Discussion
This survey provides an update and insight into the knowledge, perspective, and practice pattern of Indian optometrists towards childhood myopia management. This is the first study to analyze data from Indian optometrists with a diverse range of practice patterns and clinical experience with equal representation of gender. Even the proportional distribution of the survey responses followed the distribution of optometry colleges across India [
17]. The response rate achieved a representative response rate for Indian optometrists, encompassing practitioners from all states and union territories of India.
4.1. Complications of high myopia
Overall, the knowledge level and awareness of Indian optometrists on the natural history of childhood myopia were comparable with their Australian and Spanish counterparts [
11,
12]. Though children and young teenagers with high myopia are at risk of developing visual impairment later in life due to the associated ocular pathologies [
18], the survey shows a significant proportion (32.6%–92.4%) of respondents were unaware of the risk of ocular complications due to high myopia (
Table 3). The awareness of the association of ocular pathologies with high myopia was underwhelming, with only 7.6%–67.4% of Indian optometrists aware of the ocular complications, whereas it was 8.0%–96.7% in Australia [
11]. Lack of awareness about myopia complications, even among practitioners with an interest in myopia, implies that 'interest' and 'expertise' (knowledge) can be disconnected domains [
19].
4.2. Risk factors
The consideration of the child's age, current refractive status, and rate of progression over the past year as 'very important' or 'important' by the majority (> 70%) of the participants was consistent with the evidence available on the factors influencing myopia development [
20,
21]. However, to consider the ethnicity, parents' refractive status, and time spent on near work as 'moderate/somewhat important' was contrary and dismissive of the available evidence. The rate of myopia progression is faster among younger Asian children compared to other ethnicities [
22], the risk of myopia is higher with one or more myopic parents [
23], and clinical trials on increasing time spent outdoors can reduce the development of myopia [
24].
4.3. Clinical assessment
There is an improved acceptance of cycloplegic refraction, with the majority of the participants performing it on initial examination from the study nearly two years ago (86.6% versus 55.6%) [
13]. Cycloplegic and non-cycloplegic (manifest) subjective refraction was done yearly by 37.2% and 34.3% of the respondents, respectively, and more than once per year by 26.7% and 40.7%, respectively. Evidence suggests that cycloplegic refraction is the best practice to assess refractive error in children, and failure to do so will lead to overestimation of myopic refraction [
25]. Over 85% of the respondents were aware of the clinical relevance of cycloplegic refraction. Almost 35% of the respondents performed cycloplegic and non-cycloplegic refraction yearly, and 40% performed non-cycloplegic refraction more than once a year. Six per cent of respondents reported not performing cycloplegic refraction, and 4% did not perform manifest refraction. The importance of pupil dilation and retinal examination, especially in high myopes, has also improved from the previous study conducted two years ago (76% versus 53%) [
13].
Ocular biometry in pediatric myopes is extremely important to estimate the progression and understand treatment efficacy [
6]. Ocular axial length (AL) elongation has a strong association with axial myopia development [
4] and is known to contribute to degenerative changes and ocular diseases related to pathological myopia [
26]. Nevertheless, there is a gap between the knowledge and application among Indian optometrists, with more than half not measuring the AL.
4.4. Management
From the various management strategies to slow down the progression of myopia in children, the respondents stated single vision spectacle full correction (~70%), visual hygiene (~70%), and advice to spend time outdoors (~76%) as the first three myopia management options (Fig. 4), consistent with reports elsewhere [
5,
10,
11,
12,
27]. Even though optical interventions such as under-correction with single-vision lenses and progressive lenses for myopia control are not evidence-based [
6], a proportion (27.9%‒36.6%) of respondents choose it secondary to single-vision full-distance correction spectacles.
The survey reveals that optometrists are better aware of the efficacy [
28] of low-moderate dose atropine (68.6% versus 49%) and orthokeratology (53% versus 33%) but still differ from practising the same [
13]. This reflects the difference between the level of understanding and practice behaviour/clinical application. Most of the respondents appropriately advised increasing outdoor time for their myopia management option [
29]. However, the reduced likelihood of experienced practitioners advising visual hygiene (i.e., taking visual breaks, having good lighting, and maintaining working distance) may indicate a need for updated knowledge on current management strategies for myopia among relatively older practitioners [
30].
Most respondents reported progressive lenses and peripheral defocus contact lenses to be efficient in myopia management. Although peripheral defocus contact lenses have demonstrated clinical efficacy in reducing myopia progression, progressive lenses demonstrated a sub-clinical difference with single vision lenses and are thus not useful in clinical practice [
25,
31]. The majority cited a lack of clinical recommendations and the absence of a standard practice pattern for managing myopia progression along with the associated medico-legal issues as the main barrier, consistent with the report from Australia [
11], resulting in a deviation from the best available patient care.
4.5. Cessation
Responses considerably varied on the clinical scenario of treatment cessation criteria following myopia control; 16 years was the most common perceived age threshold with no myopia progression for 12 months. Recent evidence suggests that stability should be checked before discontinuation, which includes frequent follow-ups every six months to determine the chances of rebound effect and stability [
32,
33].
4.6. Source of information
Optometrists prefer pre-appraised and synthesized evidence over independently extracting and appraising the literature. This may indicate a need for more confidence and time constraints in appraising the vastly available research evidence among participants [
11,
32]. Participants' preference for resource materials corroborates with the previously available literature [
11,
34,
35]. Notably, despite the extent of its popularity and widespread availability over smartphones, AI chatbots like ChatGPT (online resources) were not named as the common source of scientific information [
36]. This was probably because these large language models are relatively new and have yet to gain trust among the optometric community, with possible awareness of their limitations in providing accurate or updated information [
36].
4.7. Caregiver
Optometrists involve the adult caregiver and consider them essential in their child's myopia management plan. Information of high quality has the potential to influence attitudes, encouraging behavioural change [
37]. Along with a stable attitude, a positive parental attitude originating from information leads to healthy behavioural changes, potentially reducing the prevalence and incidence of childhood myopia [
38,
39].
While we acknowledge the limitation that self-reporting may not reflect actual practice, the strength of this study is the relatively large sample size and responses from most states and union territories, thus representing the diverse practice pattern in India [
14]. Compared to the previous report two years ago, confined regionally to a few Northern Indian states [
13], the current study utilized a diverse network of state and national optometric associations, trusts, and social media platforms with follow-up reminders sent every two weeks. This ultimately achieved deeper penetration by reaching a varied group of optometrists with wide-ranging years and modes of optometric practice across India. The questionnaire's content was validated beforehand to be contextually relevant, appropriate, and unambiguous. In contrast, the earlier study [
13] was limited by insufficient methodological details of adopting the original Australian questionnaire into Indian optometric practice. The enhanced sampling and inclusion of optometrists from all strata of clinical experience and background of practice in this study might have elucidated a relatively higher proportion of respondents with better knowledge, attitude, and practice patterns. Nevertheless, the electronic questionnaire may have constrained responses to optometrists with digital literacy, and the voluntary nature of the survey likely led to a higher participation of optometrists engaged in myopia management, potentially introducing bias to the results. Finally, although the questionnaire did not include the cost of myopia control, studies in Spain have reported increased financial cost to patients as a significant reason for not prescribing myopia control strategies [
12,
27], which might be the same in the Indian context.
5. Conclusion
This study provides valuable insight into the current knowledge, attitude, and practice of Indian optometrists in managing childhood myopia. The findings highlight the unawareness of high myopia complications, inconsistency in identifying risk factors, and the absence of baseline axial length measurement. Although myopia management perspectives have improved, the uptake of those techniques in clinical practice still needs to improve. While optometrists are aware of emerging myopia interventions, single-vision distance correction remains the primary choice of vision correction. Published literature is the primary source of information for Indian optometrists, not AI chatbots. Barriers to optimal myopia care include medico-legal issues, lack of evidence-based clinical guidelines, and limited consultation time. Myopia rates have risen since COVID-19 due to reduced outdoor activity and increased screen time [
29]. These barriers must be overcome to advance global eye health and put available evidence into clinical practice.
Author Contributions
Conceptualization, S.K.K., C.A.G.; Methodology: A.N., S.K.K., S.H.B.; Software, J.J., S.B.; Validation, S.K.K., S.H.B.; Formal Analysis, A.N., J.J., S.H.B., S.B.; Investigation, A.N., S.K.K., J..J, S.H.B.; Resources, C.A.G.; Data Curation, A.N., S.K.K., J.J., S.H.B., ; Writing – Original Draft Preparation, A.N., S.K.K., J.J., S.H.B., S.B.; Writing – Review & Editing, S.K.K., S.B.; Visualization, S.K.K., J.J.; Supervision, C.A.G., S.B.; Project Administration, S.K.K.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethics approval for the study was obtained from the Mangala Institutional Ethical Committee and our study complied with the tenets of the Declaration of Helsinki.
Informed Consent Statement
The survey consisted of a statement at the beginning of the online form that the participation is voluntary, and their submission of response reflects their consent.
Acknowledgments
We would like to acknowledge Dr. Laura E Downie, Department of Optometry and Vision Sciences, The University of Melbourne, for helping us and providing the survey questionnaire. We thank the Optometric Association of Tamil Nanbargal, India Vision Institute, Tamil Nadu Government Optometry Professionals Association, National Ophthalmic Association, and Association of Schools and Colleges of Optometry (ASCO-India) for helping us circulate the questionnaire. We would like to thank Mr. Vivek Suganthan, Ms. Pooja Nandagopal, and Mr. Anush Nayak for their participation in the focus group discussion.
Conflicts of Interest
The author reports no conflicts of interest in this study.
References
- Sankaridurg, P.; Tahhan, N.; Kandel, H.; Naduvilath, T.; Zou, H.; Frick, K.D.; Marmamula, S.; Friedman, D.S.; Lamoureux, E.; Keeffe, J.; et al. IMI Impact of Myopia. Investigative ophthalmology & visual science 2021, 62, 2. [Google Scholar] [CrossRef]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.J.; Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Priscilla, J.J.; Verkicharla, P.K. Time trends on the prevalence of myopia in India - A prediction model for 2050. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists) 2021, 41, 466–474. [Google Scholar] [CrossRef]
- Ohno-Matsui, K.; Wu, P.C.; Yamashiro, K.; Vutipongsatorn, K.; Fang, Y.; Cheung, C.M.G.; Lai, T.Y.Y.; Ikuno, Y.; Cohen, S.Y.; Gaudric, A.; et al. IMI Pathologic Myopia. Investigative ophthalmology & visual science 2021, 62, 5. [Google Scholar] [CrossRef]
- Wolffsohn, J.S.; Whayeb, Y.; Logan, N.S.; Weng, R. IMI-Global Trends in Myopia Management Attitudes and Strategies in Clinical Practice-2022 Update. Investigative ophthalmology & visual science 2023, 64, 6. [Google Scholar] [CrossRef]
- Gifford, K.L.; Richdale, K.; Kang, P.; Aller, T.A.; Lam, C.S.; Liu, Y.M.; Michaud, L.; Mulder, J.; Orr, J.B.; Rose, K.A.; et al. IMI - Clinical Management Guidelines Report. Investigative ophthalmology & visual science 2019, 60, M184–m203. [Google Scholar] [CrossRef]
- Bullimore, M.A.; Richdale, K. Myopia Control 2020: Where are we and where are we heading? 2020, 40, 254–270. [Google Scholar] [CrossRef]
- Muralidharan, A.R.; Lança, C.; Biswas, S.; Barathi, V.A.; Wan Yu Shermaine, L.; Seang-Mei, S.; Milea, D.; Najjar, R.P. Light and myopia: from epidemiological studies to neurobiological mechanisms. Therapeutic advances in ophthalmology 2021, 13, 25158414211059246. [Google Scholar] [CrossRef]
- Jothi Balaji, J.; Viswanathan, S. Practice patterns in managing myopia differs among Indian eye care practitioners. Indian journal of ophthalmology 2022, 70, 1848–1849. [Google Scholar] [CrossRef]
- Nti, A.N.; Owusu-Afriyie, B.; Osuagwu, U.L.; Kyei, S.; Ovenseri-Ogbomo, G.; Ogbuehi, K.C.; Ouzzani, M.; Agho, K.E.; Mashige, K.P.; Ekure, E.; et al. Trends in myopia management attitudes and strategies in clinical practice: Survey of eye care practitioners in Africa. Contact lens & anterior eye : the journal of the British Contact Lens Association 2023, 46, 101597. [Google Scholar] [CrossRef]
- Douglass, A.; Keller, P.R.; He, M.; Downie, L.E. Knowledge, perspectives and clinical practices of Australian optometrists in relation to childhood myopia. Clinical & experimental optometry 2020, 103, 155–166. [Google Scholar] [CrossRef]
- Di Pierdomenico, J.; González-González, R.; Valiente-Soriano, F.J.; Galindo-Romero, C.; García-Ayuso, D. Attitudes and knowledge of myopia management by Spanish optometrists. International ophthalmology 2023, 43, 4247–4261. [Google Scholar] [CrossRef] [PubMed]
- Chaurasiya, R.K.; Sutar, S.; Gupta, A.; Pandey, R.; Agarwal, P. Knowledge, attitude, and practice of childhood myopia among Indian optometrists: A questionnaire-based study. Indian journal of ophthalmology 2023, 71, 951–956. [Google Scholar] [CrossRef] [PubMed]
- Thite, N.; Jaggernath, J.; Chinanayi, F.; Bharadwaj, S.; Kunjeer, G. Pattern of Optometry Practice and Range of Services in India. Optometry and Vision Science 2015, 92. [Google Scholar] [CrossRef]
- Kotrlik, J.; Higgins, C.J.I.t.; journal, p. Organizational research: Determining appropriate sample size in survey research appropriate sample size in survey research. 19 2001, 19, 43. [Google Scholar]
- Eysenbach, G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). Journal of medical Internet research 2004, 6, e34. [Google Scholar] [CrossRef] [PubMed]
- Optometry in India. An overview of Optometry services in India in terms of optical outlets, eye hospitals and educational institutes, 2016.
- Jong, M.; Sankaridurg, P.; Li, W.; Resnikoff, S.; Naidoo, K.; He, M. Reduced vision in highly myopic eyes without ocular pathology: the ZOC-BHVI high myopia study. Clinical and Experimental Optometry 2018, 101, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Fryer, L.K.; Shum, A.; Lee, A.; Lau, P. Mapping students' interest in a new domain: Connecting prior knowledge, interest, and self-efficacy with interesting tasks and a lasting desire to reengage. Learning and Instruction 2021, 75, 101493. [Google Scholar] [CrossRef]
- Morgan, I.G.; Wu, P.C.; Ostrin, L.A.; Tideman, J.W.L.; Yam, J.C.; Lan, W.; Baraas, R.C.; He, X.; Sankaridurg, P.; Saw, S.M.; et al. IMI Risk Factors for Myopia. Investigative ophthalmology & visual science 2021, 62, 3. [Google Scholar] [CrossRef]
- Biswas, S.; El Kareh, A.; Qureshi, M.; Lee, D.M.X.; Sun, C.H.; Lam, J.S.H.; Saw, S.M.; Najjar, R.P. The influence of the environment and lifestyle on myopia. Journal of physiological anthropology 2024, 43, 7. [Google Scholar] [CrossRef]
- Luong, T.Q.; Shu, Y.H.; Modjtahedi, B.S.; Fong, D.S.; Choudry, N.; Tanaka, Y.; Nau, C.L. Racial and Ethnic Differences in Myopia Progression in a Large, Diverse Cohort of Pediatric Patients. Investigative ophthalmology & visual science 2020, 61, 20. [Google Scholar] [CrossRef]
- Mutti, D.O.; Mitchell, G.L.; Moeschberger, M.L.; Jones, L.A.; Zadnik, K. Parental myopia, near work, school achievement, and children's refractive error. Investigative ophthalmology & visual science 2002, 43, 3633–3640. [Google Scholar]
- He, X.; Sankaridurg, P.; Wang, J.; Chen, J.; Naduvilath, T.; He, M.; Zhu, Z.; Li, W.; Morgan, I.G.; Xiong, S.; et al. Time Outdoors in Reducing Myopia: A School-Based Cluster Randomized Trial with Objective Monitoring of Outdoor Time and Light Intensity. Ophthalmology 2022, 129, 1245–1254. [Google Scholar] [CrossRef] [PubMed]
- Wolffsohn, J.S.; Kollbaum, P.S.; Berntsen, D.A.; Atchison, D.A.; Benavente, A.; Bradley, A.; Buckhurst, H.; Collins, M.; Fujikado, T.; Hiraoka, T.; et al. IMI - Clinical Myopia Control Trials and Instrumentation Report. Investigative ophthalmology & visual science 2019, 60, M132–m160. [Google Scholar] [CrossRef]
- Jonas, J.B.; Ohno-Matsui, K.; Holbach, L.; Panda-Jonas, S. Retinal pigment epithelium cell density in relationship to axial length in human eyes. Acta ophthalmologica 2017, 95, e22–e28. [Google Scholar] [CrossRef]
- Martínez-Pérez, C.; Villa-Collar, C.; Santodomingo-Rubido, J.; Wolffsohn, J.S. Strategies and attitudes on the management of myopia in clinical practice in Spain. Journal of Optometry 2023, 16, 64–73. [Google Scholar] [CrossRef]
- Tsai, H.-R.; Wang, J.-H.; Huang, H.-K.; Chen, T.-L.; Chen, P.-W.; Chiu, C.-J. Efficacy of atropine, orthokeratology, and combined atropine with orthokeratology for childhood myopia: A systematic review and network meta-analysis. Journal of the Formosan Medical Association 2022, 121, 2490–2500. [Google Scholar] [CrossRef] [PubMed]
- Karthikeyan, S.K.; Ashwini, D.L.; Priyanka, M.; Nayak, A.; Biswas, S. Physical activity, time spent outdoors, and near work in relation to myopia prevalence, incidence, and progression: An overview of systematic reviews and meta-analyses. Indian journal of ophthalmology 2022, 70, 728–739. [Google Scholar] [CrossRef]
- Tsugawa, Y.; Newhouse, J.P.; Zaslavsky, A.M.; Blumenthal, D.M.; Jena, A.B. Physician age and outcomes in elderly patients in hospital in the US: observational study. BMJ (Clinical research ed.) 2017, 357, j1797. [Google Scholar] [CrossRef]
- Berntsen, D.A.; Sinnott, L.T.; Mutti, D.O.; Zadnik, K. A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Investigative ophthalmology & visual science 2012, 53, 640–649. [Google Scholar] [CrossRef]
- Heiwe, S.; Kajermo, K.N.; Tyni-Lenné, R.; Guidetti, S.; Samuelsson, M.; Andersson, I.L.; Wengström, Y. Evidence-based practice: attitudes, knowledge and behaviour among allied health care professionals. International journal for quality in health care : journal of the International Society for Quality in Health Care 2011, 23, 198–209. [Google Scholar] [CrossRef] [PubMed]
- Brennan, N.A.; Toubouti, Y.M.; Cheng, X.; Bullimore, M.A. Efficacy in myopia control. Progress in retinal and eye research 2021, 83, 100923. [Google Scholar] [CrossRef] [PubMed]
- Downie, L.E.; Keller, P.R.; Vingrys, A.J. An evidence-based analysis of Australian optometrists' dry eye practices. Optometry and vision science : official publication of the American Academy of Optometry 2013, 90, 1385–1395. [Google Scholar] [CrossRef] [PubMed]
- Downie, L.E.; Keller, P.R. The self-reported clinical practice behaviors of Australian optometrists as related to smoking, diet and nutritional supplementation. PloS one 2015, 10, e0124533. [Google Scholar] [CrossRef] [PubMed]
- Biswas, S.; Logan, N.S.; Davies, L.N.; Sheppard, A.L.; Wolffsohn, J.S. Assessing the utility of ChatGPT as an artificial intelligence-based large language model for information to answer questions on myopia. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists) 2023, 43, 1562–1570. [Google Scholar] [CrossRef]
- Glasman, L.R.; Albarracín, D. Forming attitudes that predict future behavior: a meta-analysis of the attitude-behavior relation. Psychological bulletin 2006, 132, 778–822. [Google Scholar] [CrossRef]
- Li, Q.; Guo, L.; Zhang, J.; Zhao, F.; Hu, Y.; Guo, Y.; Du, X.; Zhang, S.; Yang, X.; Lu, C. Effect of School-Based Family Health Education via Social Media on Children's Myopia and Parents' Awareness: A Randomized Clinical Trial. JAMA ophthalmology 2021, 139, 1165–1172. [Google Scholar] [CrossRef]
- Xu, H.; Wen, L.M.; Rissel, C. Associations of parental influences with physical activity and screen time among young children: a systematic review. Journal of obesity 2015, 2015, 546925. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).