Submitted:
22 February 2024
Posted:
23 February 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
3. Results
3.1. An overview of the studies on digital telerehabilitation
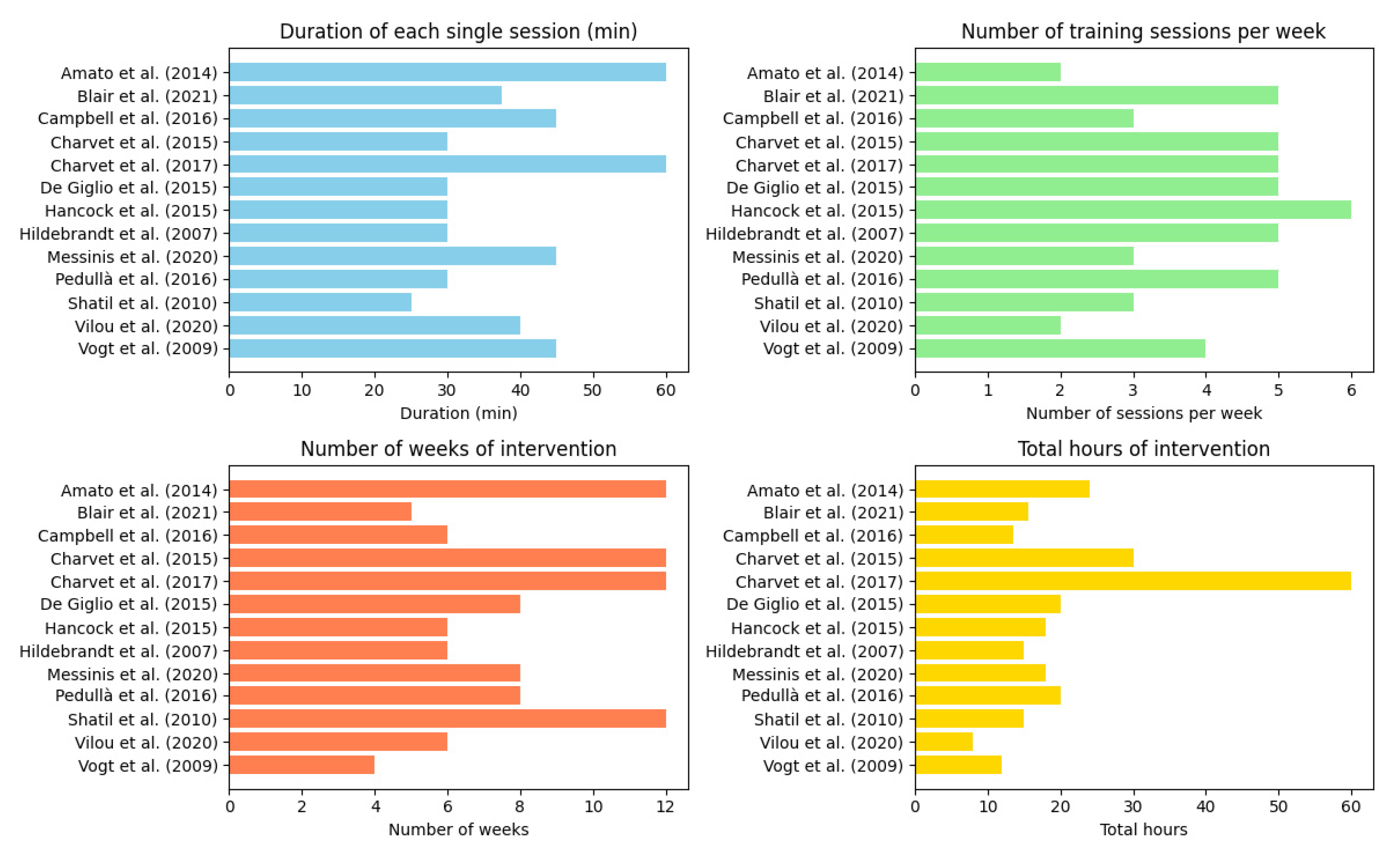
3.2. Training frequency and intensity of digital telerehabilitation.
3.3. Feasibility of digital telerehabilitation
3.4. Efficacy of digital telerehabilitation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ghasemi, N.; Razavi, S.; Nikzad, E. Multiple Sclerosis: Pathogenesis, Symptoms, Diagnoses and Cell-Based Therapy. Cell J 2017, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Stadelmann, C.; Wegner, C.; Brück, W. Inflammation, Demyelination, and Degeneration — Recent Insights from MS Pathology. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease 2011, 1812, 275–282. [Google Scholar] [CrossRef]
- Maggio, M.G.; Russo, M.; Cuzzola, M.F.; Destro, M.; La Rosa, G.; Molonia, F.; Bramanti, P.; Lombardo, G.; De Luca, R.; Calabrò, R.S. Virtual Reality in Multiple Sclerosis Rehabilitation: A Review on Cognitive and Motor Outcomes. Journal of Clinical Neuroscience 2019, 65, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Walton, C.; King, R.; Rechtman, L.; Kaye, W.; Leray, E.; Marrie, R.A.; Robertson, N.; La Rocca, N.; Uitdehaag, B.; van der Mei, I.; et al. Rising Prevalence of Multiple Sclerosis Worldwide: Insights from the Atlas of MS, Third Edition. Mult Scler 2020, 26, 1816–1821. [Google Scholar] [CrossRef]
- Lucchinetti, C.; Brück, W.; Parisi, J.; Scheithauer, B.; Rodriguez, M.; Lassmann, H. Heterogeneity of Multiple Sclerosis Lesions: Implications for the Pathogenesis of Demyelination. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society 2000, 47, 707–717. [Google Scholar] [CrossRef]
- Amato, M.; Goretti, B.; Viterbo, R.; Portaccio, E.; Niccolai, C.; Hakiki, B.; Iaffaldano, P.; Trojano, M. Computer-Assisted Rehabilitation of Attention in Patients with Multiple Sclerosis: Results of a Randomized, Double-Blind Trial. Mult Scler 2014, 20, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.M.; Leo, G.J.; Ellington, L.; Nauertz, T.; Bernardin, L.; Unverzagt, F. Cognitive Dysfunction in Multiple Sclerosis.: II. Impact on Employment and Social Functioning. Neurology 1991, 41, 692–696. [Google Scholar] [CrossRef] [PubMed]
- Achiron, A.; Barak, Y. Cognitive Impairment in Probable Multiple Sclerosis. Journal of Neurology, Neurosurgery & Psychiatry 2003, 74, 443–446. [Google Scholar] [CrossRef]
- Zipoli, V.; Goretti, B.; Hakiki, B.; Siracusa, G.; Sorbi, S.; Portaccio, E.; Amato, M.P. Cognitive Impairment Predicts Conversion to Multiple Sclerosis in Clinically Isolated Syndromes. Mult Scler 2010, 16, 62–67. [Google Scholar] [CrossRef]
- Chiaravalloti, N.D.; DeLuca, J. Cognitive Impairment in Multiple Sclerosis. The Lancet Neurology 2008, 7, 1139–1151. [Google Scholar] [CrossRef]
- Langdon, D.W. Cognition in Multiple Sclerosis. Current Opinion in Neurology 2011, 24, 244. [Google Scholar] [CrossRef]
- Amato, M.P.; Zipoli, V.; Portaccio, E. Cognitive Changes in Multiple Sclerosis. Expert Review of Neurotherapeutics 2008, 8, 1585–1596. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Benito-León, J.; González, J.-M.M.; Rivera-Navarro, J. Quality of Life and Its Assessment in Multiple Sclerosis: Integrating Physical and Psychological Components of Wellbeing. The Lancet Neurology 2005, 4, 556–566. [Google Scholar] [CrossRef]
- Ozakbas, S.; Cagiran, I.; Ormeci, B.; Idiman, E. Correlations between Multiple Sclerosis Functional Composite, Expanded Disability Status Scale and Health-Related Quality of Life during and after Treatment of Relapses in Patients with Multiple Sclerosis. Journal of the Neurological Sciences 2004, 218, 3–7. [Google Scholar] [CrossRef]
- Shevil, E.; Finlayson, M. Perceptions of Persons with Multiple Sclerosis on Cognitive Changes and Their Impact on Daily Life. Disability and Rehabilitation 2006, 28, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Schultheis, M.T.; Garay, E.; DeLuca, J. The Influence of Cognitive Impairment on Driving Performance in Multiple Sclerosis. Neurology 2001, 56, 1089–1094. [Google Scholar] [CrossRef] [PubMed]
- Schultheis, M.T.; Garay, E.; Millis, S.R.; DeLuca, J. Motor Vehicle Crashes and Violations among Drivers with Multiple Sclerosis. Archives of Physical Medicine and Rehabilitation 2002, 83, 1175–1178. [Google Scholar] [CrossRef] [PubMed]
- Amato, M.P.; Langdon, D.; Montalban, X.; Benedict, R.H.B.; DeLuca, J.; Krupp, L.B.; Thompson, A.J.; Comi, G. Treatment of Cognitive Impairment in Multiple Sclerosis: Position Paper. J Neurol 2013, 260, 1452–1468. [Google Scholar] [CrossRef] [PubMed]
- Sandroff, B.M.; DeLuca, J. Will Behavioral Treatments for Cognitive Impairment in Multiple Sclerosis Become Standards-of-Care? International Journal of Psychophysiology 2020, 154, 67–79. [Google Scholar] [CrossRef] [PubMed]
- Chiaravalloti, N.D.; Moore, N.B.; Nikelshpur, O.M.; DeLuca, J. An RCT to Treat Learning Impairment in Multiple Sclerosis: The MEMREHAB Trial. Neurology 2013, 81, 2066–2072. [Google Scholar] [CrossRef]
- Filippi, M.; Riccitelli, G.; Mattioli, F.; Capra, R.; Stampatori, C.; Pagani, E.; Valsasina, P.; Copetti, M.; Falini, A.; Comi, G.; et al. Multiple Sclerosis: Effects of Cognitive Rehabilitation on Structural and Functional MR Imaging Measures—An Explorative Study. Radiology 2012, 262, 932–940. [Google Scholar] [CrossRef]
- Chiu, C.; Bishop, M.; Pionke, J.J.; Strauser, D.; Santens, R.L. Barriers to the Accessibility and Continuity of Health-Care Services in People with Multiple Sclerosis: A Literature Review. International Journal of MS Care 2017, 19, 313–321. [Google Scholar] [CrossRef]
- Buchanan, R.J.; Stuifbergen, A.; Chakravorty, B.J.; Wang, S.; Zhu, L.; Kim, M. Urban/Rural Differences in Access and Barriers to Health Carefor People with Multiple Sclerosis. Journal of Health and Human Services Administration 2006, 29, 360–375. [Google Scholar]
- Scheer, J.; Kroll, T.; Neri, M.T.; Beatty, P. Access Barriers for Persons with Disabilities: The Consumer’s Perspective. Journal of Disability Policy Studies 2003, 13, 221–230. [Google Scholar] [CrossRef]
- Minden, S.L.; Frankel, D.; Hadden, L.; Hoaglin, D.C. Access to Health Care for People with Multiple Sclerosis. Mult Scler 2007, 13, 547–558. [Google Scholar] [CrossRef]
- McDoom, M.M.; Koppelman, E.; Drainoni, M.-L. Barriers to Accessible Health Care for Medicaid Eligible People with Disabilities: A Comparative Analysis. Journal of Disability Policy Studies 2014, 25, 154–163. [Google Scholar] [CrossRef]
- Kroll, T.; Jones, G.C.; Kehn, M.; Neri, M.T. Barriers and Strategies Affecting the Utilisation of Primary Preventive Services for People with Physical Disabilities: A Qualitative Inquiry. Health & social care in the community 2006, 14, 284–293. [Google Scholar] [CrossRef]
- Morrison, E.H.; George, V.; Mosqueda, L. Primary Care for Adults with Physical Disabilities: Perceptions from Consumer and Provider Focus Groups. Family medicine 2008, 40, 645–651. [Google Scholar] [PubMed]
- Peretti, A.; Amenta, F.; Tayebati, S.K.; Nittari, G.; Mahdi, S.S. Telerehabilitation: Review of the State-of-the-Art and Areas of Application. JMIR Rehabilitation and Assistive Technologies 2017, 4, e7511. [Google Scholar] [CrossRef]
- Grippo, A.; Assenza, G.; Scarpino, M.; Broglia, L.; Cilea, R.; Galimberti, C.A.; Lanzo, G.; Michelucci, R.; Tassi, L.; Vergari, M.; et al. Electroencephalography during SARS-CoV-2 Outbreak: Practical Recommendations from the Task Force of the Italian Society of Neurophysiology (SINC), the Italian League Against Epilepsy (LICE), and the Italian Association of Neurophysiology Technologists (AITN). Neurol Sci 2020, 41, 2345–2351. [Google Scholar] [CrossRef]
- Karakas, H.; Seebacher, B.; Kahraman, T. Technology-Based Rehabilitation in People with Multiple Sclerosis: A Narrative Review. JOURNAL OF MULTIPLE SCLEROSIS RESEARCH 2021, 1, 54–68. [Google Scholar] [CrossRef]
- Charvet, L.; Shaw, M.; Haider, L.; Melville, P.; Krupp, L. Remotely-Delivered Cognitive Remediation in Multiple Sclerosis (MS): Protocol and Results from a Pilot Study. Multiple Sclerosis Journal - Experimental, Translational and Clinical 2015, 1, 2055217315609629. [Google Scholar] [CrossRef] [PubMed]
- Cacciante, L.; Pietà, C. della; Rutkowski, S.; Cieślik, B.; Szczepańska-Gieracha, J.; Agostini, M.; Kiper, P. Cognitive Telerehabilitation in Neurological Patients: Systematic Review and Meta-Analysis. Neurol Sci 2022, 43, 847–862. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, A.R.; Chiaravalloti, N.; Goverover, Y.; DeLuca, J. Evidenced-Based Cognitive Rehabilitation for Persons With Multiple Sclerosis: A Review of the Literature. Archives of Physical Medicine and Rehabilitation 2008, 89, 761–769. [Google Scholar] [CrossRef]
- Mitolo, M.; Venneri, A.; Wilkinson, I.D.; Sharrack, B. Cognitive Rehabilitation in Multiple Sclerosis: A Systematic Review. Journal of the Neurological Sciences 2015, 354, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Goverover, Y.; Chiaravalloti, N.D.; O’Brien, A.R.; DeLuca, J. Evidenced-Based Cognitive Rehabilitation for Persons With Multiple Sclerosis: An Updated Review of the Literature From 2007 to 2016. Archives of Physical Medicine and Rehabilitation 2018, 99, 390–407. [Google Scholar] [CrossRef] [PubMed]
- Brochet, B. Cognitive Rehabilitation in Multiple Sclerosis in the Period from 2013 and 2021: A Narrative Review. Brain Sciences 2022, 12, 55. [Google Scholar] [CrossRef]
- Nair, R. das; Martin, K.-J.; Lincoln, N.B. Memory Rehabilitation for People with Multiple Sclerosis. Cochrane Database of Systematic Reviews 2016. [Google Scholar] [CrossRef]
- Hildebrandt, H.; Lanz, M.; Hahn, H.K.; Hoffmann, E.; Schwarze, B.; Schwendemann, G.; Kraus, J.A. Cognitive Training in MS: Effects and Relation to Brain Atrophy. Restorative Neurology and Neuroscience 2007, 25, 33–43. [Google Scholar]
- Vogt, A.; Kappos, L.; Calabrese, P.; Stöcklin, M.; Gschwind, L.; Opwis, K.; Penner, I.-K. Working Memory Training in Patients with Multiple Sclerosis – Comparison of Two Different Training Schedules. Restorative Neurology and Neuroscience 2009, 27, 225–235. [Google Scholar] [CrossRef]
- Shatil, E.; Metzer, A.; Horvitz, O.; Miller, A. Home-Based Personalized Cognitive Training in MS Patients: A Study of Adherence and Cognitive Performance. NeuroRehabilitation 2010, 26, 143–153. [Google Scholar] [CrossRef]
- Charvet, L.; Shaw, M.; Haider, L.; Melville, P.; Krupp, L. Remotely-Delivered Cognitive Remediation in Multiple Sclerosis (MS): Protocol and Results from a Pilot Study. Multiple Sclerosis Journal - Experimental, Translational and Clinical 2015, 1, 2055217315609629. [Google Scholar] [CrossRef] [PubMed]
- De Giglio, L.; De Luca, F.; Prosperini, L.; Borriello, G.; Bianchi, V.; Pantano, P.; Pozzilli, C. A Low-Cost Cognitive Rehabilitation With a Commercial Video Game Improves Sustained Attention and Executive Functions in Multiple Sclerosis: A Pilot Study. Neurorehabil Neural Repair 2015, 29, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Hancock, L.M.; Bruce, J.M.; Bruce, A.S.; Lynch, S.G. Processing Speed and Working Memory Training in Multiple Sclerosis: A Double-Blind Randomized Controlled Pilot Study. Journal of Clinical and Experimental Neuropsychology 2015, 37, 113–127. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.; Langdon, D.; Cercignani, M.; Rashid, W. A Randomised Controlled Trial of Efficacy of Cognitive Rehabilitation in Multiple Sclerosis: A Cognitive, Behavioural, and MRI Study. Neural plasticity 2016, 2016. [Google Scholar] [CrossRef] [PubMed]
- Pedullà, L.; Brichetto, G.; Tacchino, A.; Vassallo, C.; Zaratin, P.; Battaglia, M.A.; Bonzano, L.; Bove, M. Adaptive vs. Non-Adaptive Cognitive Training by Means of a Personalized App: A Randomized Trial in People with Multiple Sclerosis. Journal of NeuroEngineering and Rehabilitation 2016, 13, 88. [Google Scholar] [CrossRef]
- Charvet, L.E.; Yang, J.; Shaw, M.T.; Sherman, K.; Haider, L.; Xu, J.; Krupp, L.B. Cognitive Function in Multiple Sclerosis Improves with Telerehabilitation: Results from a Randomized Controlled Trial. PLOS ONE 2017, 12, e0177177. [Google Scholar] [CrossRef]
- Messinis, L.; Kosmidis, M.H.; Nasios, G.; Konitsiotis, S.; Ntoskou, A.; Bakirtzis, C.; Grigoriadis, N.; Patrikelis, P.; Panagiotopoulos, E.; Gourzis, P.; et al. Do Secondary Progressive Multiple Sclerosis Patients Benefit from Computer- Based Cognitive Neurorehabilitation? A Randomized Sham Controlled Trial. Multiple Sclerosis and Related Disorders 2020, 39, 101932. [Google Scholar] [CrossRef]
- Vilou, I.; Bakirtzis, C.; Artemiadis, A.; Ioannidis, P.; Papadimitriou, M.; Konstantinopoulou, E.; Aretouli, E.; Messinis, L.; Nasios, G.; Dardiotis, E.; et al. Computerized Cognitive Rehabilitation for Treatment of Cognitive Impairment in Multiple Sclerosis: An Explorative Study. Journal of integrative neuroscience 2020, 19, 341–347. [Google Scholar] [CrossRef]
- Blair, M.; Goveas, D.; Safi, A.; Marshall, C.; Rosehart, H.; Orenczuk, S.; Morrow, S.A. Does Cognitive Training Improve Attention/Working Memory in Persons with MS? A Pilot Study Using the Cogmed Working Memory Training Program. Multiple Sclerosis and Related Disorders 2021, 49, 102770. [Google Scholar] [CrossRef]
- Wallin, M.T.; Culpepper, W.J.; Campbell, J.D.; Nelson, L.M.; Langer-Gould, A.; Marrie, R.A.; Cutter, G.R.; Kaye, W.E.; Wagner, L.; Tremlett, H. The Prevalence of MS in the United States: A Population-Based Estimate Using Health Claims Data. Neurology 2019, 92, e1029–e1040. [Google Scholar] [CrossRef] [PubMed]
- Penner, I.; Kobel, M.; Opwis, K. BrainStim–A Recently Developed Tool to Train Different Aspects of Working Memory. In Proceedings of the Proceedings of the INS/GNP Conference; 2006; pp. 17–18. [Google Scholar]
- Shaw, M.T.; Best, P.; Frontario, A.; Charvet, L.E. Telerehabilitation Benefits Patients with Multiple Sclerosis in an Urban Setting. Journal of telemedicine and telecare 2021, 27, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Stirratt, M.J.; Dunbar-Jacob, J.; Crane, H.M.; Simoni, J.M.; Czajkowski, S.; Hilliard, M.E.; Aikens, J.E.; Hunter, C.M.; Velligan, D.I.; Huntley, K. Self-Report Measures of Medication Adherence Behavior: Recommendations on Optimal Use. Translational behavioral medicine 2015, 5, 470–482. [Google Scholar] [CrossRef]
- Nicolson, P.J.; Hinman, R.S.; Wrigley, T.V.; Stratford, P.W.; Bennell, K.L. Self-Reported Home Exercise Adherence: A Validity and Reliability Study Using Concealed Accelerometers. journal of orthopaedic & sports physical therapy 2018, 48, 943–950. [Google Scholar] [CrossRef]
- Furberg, C.D.; Soliman, E.Z. Double-Blindness Protects Scientific Validity. Journal of Thrombosis and Haemostasis 2008, 6, 230–231. [Google Scholar] [CrossRef] [PubMed]
- Boot, W.R.; Simons, D.J.; Stothart, C.; Stutts, C. The Pervasive Problem with Placebos in Psychology: Why Active Control Groups Are Not Sufficient to Rule out Placebo Effects. Perspectives on psychological science 2013, 8, 445–454. [Google Scholar] [CrossRef]
- Hariton, E.; Locascio, J.J. Randomised Controlled Trials—the Gold Standard for Effectiveness Research. BJOG 2018, 125, 1716. [Google Scholar] [CrossRef]
- Cai, Y.; Yang, T.; Yu, X.; Han, X.; Chen, G.; Shi, C. The Alternate-Form Reliability Study of Six Variants of the Brief Visual-Spatial Memory Test-Revised and the Hopkins Verbal Learning Test-Revised. Frontiers in Public Health 2023, 11, 1096397. [Google Scholar] [CrossRef]
- Siciliano, M.; Chiorri, C.; Passaniti, C.; Sant’Elia, V.; Trojano, L.; Santangelo, G. Comparison of Alternate and Original Forms of the Montreal Cognitive Assessment (MoCA): An Italian Normative Study. Neurological Sciences 2019, 40, 691–702. [Google Scholar] [CrossRef]
- McCoy, C.E. Understanding the Intention-to-Treat Principle in Randomized Controlled Trials. West J Emerg Med 2017, 18, 1075–1078. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, N.S.; Truax, P. Clinical Significance: A Statistical Approach to Defining Meaningful Change in Psychotherapy Research. J Consult Clin Psychol 1991, 59, 12–19. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic press, 2013; ISBN 1-4832-7648-1. [Google Scholar] [CrossRef]
- Lin, Y.; Zhu, M.; Su, Z. The Pursuit of Balance: An Overview of Covariate-Adaptive Randomization Techniques in Clinical Trials. Contemporary Clinical Trials 2015, 45, 21–25. [Google Scholar] [CrossRef]
- van Rooden, S.M.; Heiser, W.J.; Kok, J.N.; Verbaan, D.; van Hilten, J.J.; Marinus, J. The Identification of Parkinson’s Disease Subtypes Using Cluster Analysis: A Systematic Review. Movement Disorders 2010, 25, 969–978. [Google Scholar] [CrossRef]
- Feinstein, A.; Amato, M.P.; Brichetto, G.; Chataway, J.; Chiaravalloti, N.D.; Cutter, G.; Dalgas, U.; DeLuca, J.; Farrell, R.; Feys, P. Cognitive Rehabilitation and Aerobic Exercise for Cognitive Impairment in People with Progressive Multiple Sclerosis (CogEx): A Randomised, Blinded, Sham-Controlled Trial. The Lancet Neurology 2023, 22, 912–924. [Google Scholar] [CrossRef]
- Falet, J.-P.R.; Durso-Finley, J.; Nichyporuk, B.; Schroeter, J.; Bovis, F.; Sormani, M.-P.; Precup, D.; Arbel, T.; Arnold, D.L. Estimating Individual Treatment Effect on Disability Progression in Multiple Sclerosis Using Deep Learning. Nature communications 2022, 13, 5645. [Google Scholar] [CrossRef]
- García-Rudolph, A.; García-Molina, A.; Opisso, E.; Tormos, J.M.; Madai, V.I.; Frey, D.; Bernabeu, M. Neuropsychological Assessments of Patients With Acquired Brain Injury: A Cluster Analysis Approach to Address Heterogeneity in Web-Based Cognitive Rehabilitation. Front. Neurol. 2021, 12, 701946. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Rudolph, A.; Garcia-Molina, A.; Opisso, E.; Tormos Muñoz, J. Personalized Web-Based Cognitive Rehabilitation Treatments for Patients with Traumatic Brain Injury: Cluster Analysis. JMIR Medical Informatics 2020, 8, e16077. [Google Scholar] [CrossRef] [PubMed]
- De Meo, E.; Portaccio, E.; Giorgio, A.; Ruano, L.; Goretti, B.; Niccolai, C.; Patti, F.; Chisari, C.G.; Gallo, P.; Grossi, P. Identifying the Distinct Cognitive Phenotypes in Multiple Sclerosis. JAMA neurology 2021, 78, 414–425. [Google Scholar] [CrossRef]
- Whitlock, L.A.; McLaughlin, A.C.; Allaire, J.C. Individual Differences in Response to Cognitive Training: Using a Multi-Modal, Attentionally Demanding Game-Based Intervention for Older Adults. Computers in human behavior 2012, 28, 1091–1096. [Google Scholar] [CrossRef]
- Benedict, R.H.; Amato, M.P.; Boringa, J.; Brochet, B.; Foley, F.; Fredrikson, S.; Hamalainen, P.; Hartung, H.; Krupp, L.; Penner, I. Brief International Cognitive Assessment for MS (BICAMS): International Standards for Validation. BMC neurology 2012, 12, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Baddeley, A. Working Memory. Current biology 2010, 20, R136–R140. [Google Scholar] [CrossRef] [PubMed]
- Baddeley, A. Working Memory. Science 1992, 255, 556–559. [Google Scholar] [CrossRef] [PubMed]
| Study | Groups (N) | Disease Type | Study Aim | Cognitive Domains Targeted | Outcome Measures | Follow-up Assessment |
|---|---|---|---|---|---|---|
|
Hildebrandt et al. (2007) [39] |
IG (17) CG (25) |
RRMS (42) | Explore efficacy of remote cognitive training | Memory, working memory | Disability, motor, cognition, mood, fatigue, quality of life |
No |
|
Vogt et al. (2009) [40] |
IG intensive training (15) IG distributed training (15) CG (15) |
RRMS (36) SPMS (8) Chronic-progressive MS (1) |
Evaluate two different remote training schedules |
Working memory | Cognition, fatigue, mood, quality of life |
No |
|
Shatil et al. (2010) [41] |
IG (59) CG (48) |
RRMS (107) | Explore unprompted adherence to personalised remote cognitive training | Dependent on individual performance on neuropsychological examination | Cognition, mood, disability, fatigue | No |
|
Amato et al. (2014) [6] |
IG (55) CG (33) |
RRMS (88) | Explore efficacy of remote cognitive training | Attention | Cognition, depression, fatigue, everyday activities | 6 months |
|
Charvet et al. (2015) [42] |
IG (11) CG (9) |
RRMS (20) | Explore feasibility of remote cognitive training | Processing speed, memory | Cognition, motor | No |
|
De Giglio et al. (2015) [43] |
IG (18) CG (17) |
RRMS (35) | Explore efficacy of remote cognitive training | Attention, processing speed, working memory | Cognition, fatigue, quality of life | No |
|
Hancock et al. (2015) [44] |
IG (15) CG (15) |
RRMS (21) SPMS (5) PPMS (4) |
Explore efficacy of remote cognitive training | Processing speed, working memory | Cognition, mood, fatigue, quality of life | No |
|
Campbell et al. (2016) [45] |
IG (19) CG (19) |
RRMS (27) SPMS (11) |
Explore efficacy of remote cognitive training |
Working memory, visuospatial memory, divided attention | Cognition, quality of life, mood, patient reported chronic illness management, self-efficacy, self-reported cognition, fatigue | 4.5 months |
|
Pedullà et al. (2016) [46] |
IG (14) CG (14) |
RRMS (17) SPMS (11) |
Explore efficacy of remote cognitive training | Working memory | Cognition | 6 months |
|
Charvet et al. (2017) [47] |
IG (74) CG (61) |
RRMS (89) SPMS (35) PPMS (7) |
Explore efficacy of remote cognitive training |
Processing speed, attention, working memory, executive functions | Cognition | No |
|
Messinis et al. (2020) [48] |
IG (19) CG (17) |
SPMS (36) | Explore efficacy of remote cognitive training |
Attention, divided attention, verbal memory, visuospatial memory, executive functions | Cognition, fatigue, mood, quality of life | No |
|
Vilou et al. (2020) [49] |
IG (23) CG (24) |
RRMS (47) | Explore efficacy of remote cognitive training | Episodic memory, attention, processing speed | Cognition | No |
|
Blair et al. (2021) [50] |
IG (15) CG (15) |
RRMS (17) SPMS (12) PPMS (1) |
Explore efficacy of remote cognitive training |
Attention, working memory | Cognition, self-reported cognitive function, mood, pain, quality of life | 6 months |
| Study |
Positive results on NPS measures |
Positive results on other measures | Negative results on NPS measures | Negative results on other measures | Positive results maintained at follow-up | Effect sizes for (immediate) positive results |
|---|---|---|---|---|---|---|
|
Hildebrandt et al. (2007) [39] |
CVLT-II (learning trials & long delay free recall); PASAT |
NHPT | CVLT-II (short delay free recall, cued recall & long delay cued recall); Object alternation RTs & errors; Alertness with & without cueing | EDSS; Timed walked test; SF-12 bodily & mental scores; BDI; FSS | No follow up assessment performed | Not reported |
|
Vogt et al. (2009) [40] |
Corsi blocks backward (only in the distributed training group); Digit span backward; 2-back task omissions; PASAT; FST |
FSMC; MFIS |
Corsi blocks forward; Digit span forward; SDMT |
CES-D; FAMS | No follow up assessment performed | Corsi block backward: ηp2 = 0.08; Digit span backward: ηp2 = 0.11; 2-back task omissions: ηp2 = 0.06; PASAT: ηp2 = 0.10; FST: ηp2 = 0.14 (distributed training group). Digit span backward: ηp2 = 0.11; 2-back task omissions: ηp2 = 0.06; PASAT: ηp2 = 0.10; FST: ηp2 = 0.11 (high intensity training group) |
|
Shatil et al. (2010) [41] |
General memory; Visual working memory; Verbal auditory working memory (N-CPC) | Auditory (non-linguistic) working memory; Awareness divided attention Avoiding distractions; Hand – eye coordination; Inhibition Naming; Planning response time; Shifting attention Spatial perception; Time estimation; Visual perception; Visual scanning (N-CPC) |
Zung depression scale; EDSS; FSS | No follow up assessment performed | General memory: ηp2 = 0.207; Visual working memory: ηp2 = 0.196; Verbal auditory working memory: ηp2 = 0.191. | |
|
Amato et al. (2014) [6] |
PASAT; SDMT (improvement also in the control group) |
ESS (improvement also in the control group); MADRS (improvement also in the control group); VAS (improvement also in the control group) | Visual search; TMT A & B; SRT; SPART; WLG | FSS | PASAT; SDMT (improvement sustained also in the control group) | Not reported |
|
Charvet et al. (2015) [32] |
General composite cognitive score |
Ecog | WAIS-IV letter number sequence; Corsi block; PASAT; SRT; BVMT-R |
No follow up assessment performed | General composite cognitive score: d = 1.11 | |
| De Giglio et al. (2015)[43] | Stroop test; SDMT | MSQoL-54 mental health composite, rolelimitations-emotional, emotional well-being, cognitive function, health distress | PASAT 3 | MFIS; MSQoL-54 physical health composite, physical function, role limitations- physical, pain, energy, health perceptions, social function, sexual function, overall QoL, sexual function | No follow up assessment performed | Stoop test: F2 = 0.210; SDMT: F2 = 0.177 |
|
Hancock et al. (2015) [44] |
PASAT | SDMT; Stroop test; LNS; Digit backward; Raven's APM; BVMT-R; COWAT; CPT-II; AVLT | BDI; STAI; MFIS; MSQOL-54 | No follow up assessment performed | PASAT: d= 0.90 |
|
|
Campbell et al. (2016) [45] |
SDMT | CVLT-II; BVMT-R | EQ-5D; FAMS; PAM-13; USE-MS; HADS; MSNQ; FSS | not significant | Not reported | |
|
Pedullà et al. (2016) [46] |
SRT consistent long-term retrieval & delayed recall; SDMT; PASAT; WLG | SRT long term storage; SPART; WCST | PASAT; SDMT | Not reported | ||
|
Charvet et al. (2017) [47] |
General composite cognitive score |
SRT; BVMT-R; PASAT; TMT; WAIS-IV letter number sequence; WAIS-IV digit span backward; DKEFS | No follow up assessment performed | General composite cognitive score: d = 0.38 |
||
|
Messinis et al. (2020) [48] |
SDMT, GVLT, BVMT-R | MFIS; BDI-FS; EQ-5D | No follow up assessment performed | SDMT: g = 2.980; GVLT: g = 2.898; BVMT-R: g = 1.699 | ||
|
Vilou et al. (2020) [49] |
GVLT; BVMT-R; TMT-A; Stroop test | SDMT; TMT-B | No follow up assessment performed | GVLT: d = 0.6; BVMT-R: d = 0.38; TMT-A: d = 0.15; Stroop test: d = 0.32 | ||
|
Blair et al. (2021) [50] |
DKEFS colour-word interference test; WAIS-III digit span backward | HADS-D | SDMT; PASAT; CVLT-II; BVMT-R; VSVT; WAIS-III spatial span forward and backward, WAIS-III arithmetic; WAIS-III digit span forward; WAIS-III letter-number sequence | BDI-FS; FSS, MSNQ, HADS-A; SF-36; DEX; CFQ; Brief COPE; PDQ; NPRS | HADS-D |
DKEFS colour-word interference test: d = 0.27; WAIS-III digit span backward: d = 0.69 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





