Submitted:
26 February 2024
Posted:
27 February 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
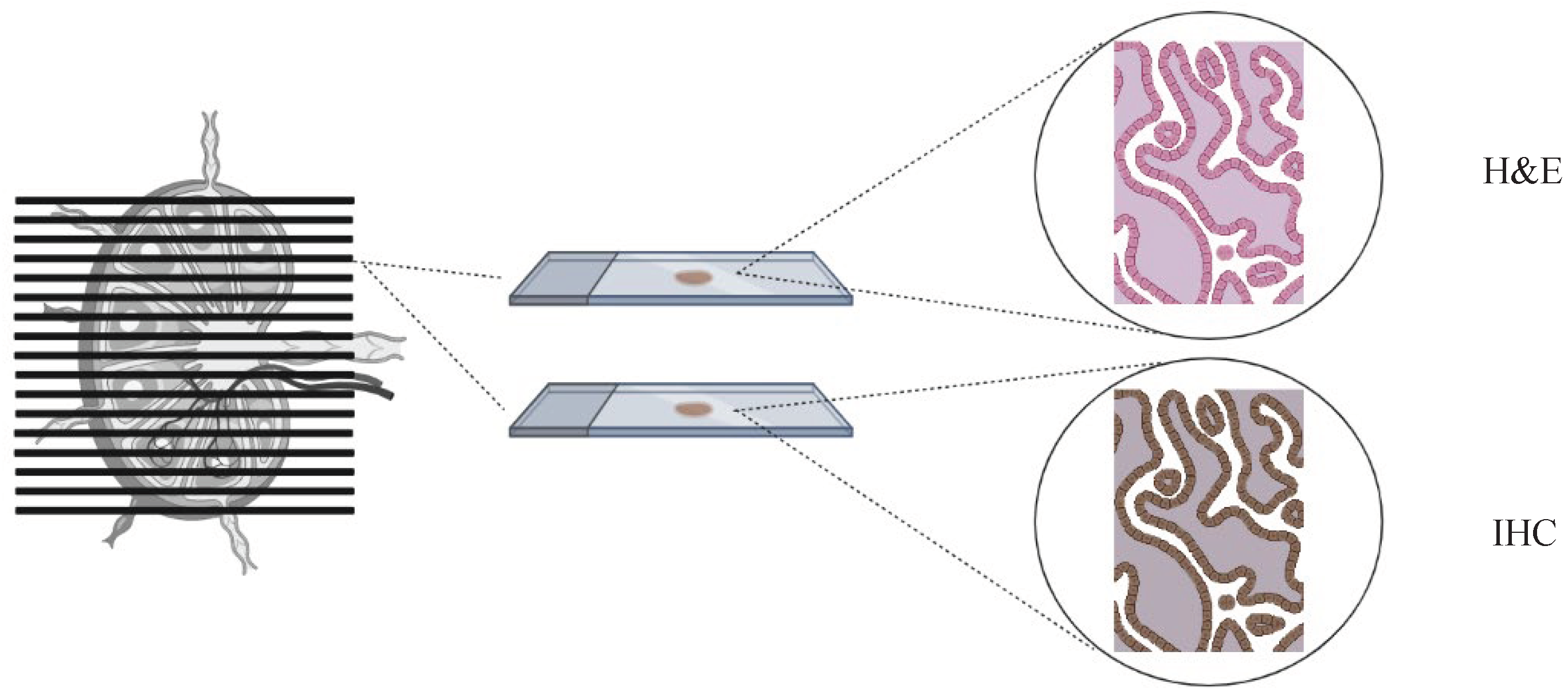
2. Sentinel Lymph Node Assessment: How Low-Volume Metastases are Detected
3. Are Low-Volume Metastases Clinically Meaningful? Controversies of Current Evidence
3.1. Macrometastases, Micrometastases, Isolated Tumor Cells. A matter of Size?
3.2. Impact of Adjuvant Therapy and Complementary PLND
3.3. The Site of Recurrence: Is It Negligible?
4. Present and Future Challenges
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cibula D, Raspollini MR, Planchamp F, et al. ESGO/ESTRO/ESP Guidelines for the management of patients with cervical cancer - Update 2023. Int J Gynecol Cancer. 2023, 33, 649–666. [Google Scholar] [CrossRef] [PubMed]
- Stehman FB, Bundy BN, DiSaia PJ, et al. Carcinoma of the cervix treated with radiation therapy. A multi-variate analysis of prognostic variables in the Gynecologic Oncology Group. Cancer. 1991, 67, 2776–2785. [Google Scholar] [CrossRef]
- Lécuru F, Mathevet P, Querleu D, et al. Bilateral negative sentinel nodes accurately predict absence of lymph node metastasis in early cervical cancer: results of the SENTICOL study. J Clin Oncol. 2011, 29, 1686–1691. [Google Scholar] [CrossRef] [PubMed]
- Mathevet P, Lécuru F, Uzan C, et al. Sentinel lymph node biopsy and morbidity outcomes in early cervical cancer: Results of a multicentre randomised trial (SENTICOL-2). Eur J Cancer 2021, 148, 307–315. [CrossRef] [PubMed]
- Cibula D, Dusek J, Jarkovsky J, et al. A prospective multicenter trial on sentinel lymph node biopsy in patients with early-stage cervical cancer (SENTIX). Int J Gynecol Cancer. 2019, 29, 212–215. [Google Scholar] [CrossRef] [PubMed]
- Lecuru FR, McCormack M, Hillemanns P, et al. SENTICOL III: an international validation study of sentinel node biopsy in early cervical cancer. A GINECO, ENGOT, GCIG and multicenter study. Int J Gynecol Cancer. 2019, 29, 829–834. [Google Scholar] [CrossRef] [PubMed]
- Zhu H, Doğan BE. American Joint Committee on Cancer’s Staging System for Breast Cancer, Eighth Edition: Summary for Clinicians. Eur J Breast Health. 2021, 17, 234–238. [Google Scholar] [CrossRef]
- Cibula D, Kocian R, Plaikner A, et al. Sentinel lymph node mapping and intraoperative assessment in a prospective, international, multicentre, observational trial of patients with cervical cancer: The SENTIX trial. Eur J Cancer 2020, 137, 69–80. [CrossRef]
- Dundr P, Cibula D, Němejcová K, et al. Pathologic Protocols for Sentinel Lymph Nodes Ultrastaging in Cervical Cancer. Arch Pathol Lab Med. Published. 2019.
- Cibula D, Abu-Rustum NR, Dusek L, et al. Bilateral ultrastaging of sentinel lymph node in cervical cancer: Lowering the false-negative rate and improving the detection of micrometastasis. Gynecol Oncol. 2012, 127, 462–466. [Google Scholar] [CrossRef]
- Guani B, Balaya V, Magaud L, et al. The Clinical Impact of Low-Volume Lymph Nodal Metastases in Early-Stage Cervical Cancer: The Senticol 1 and Senticol 2 Trials. Cancers. 2020, 12, 1061. [Google Scholar] [CrossRef] [PubMed]
- Stany MP, Stone PJ, Felix JC, et al. Lymph Node Micrometastases in Early-Stage Cervical Cancer are Not Predictive of Survival. Int J Gynecol Pathol. 2015, 34, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Buda A, Casarin J, Mueller M, et al. The impact of low-volume metastasis on disease-free survival of women with early-stage cervical cancer. J Cancer Res Clin Oncol. 2021, 147, 1599–1606. [Google Scholar] [CrossRef] [PubMed]
- Grassi T, Dell’Orto F, Jaconi M, et al. Two ultrastaging protocols for the detection of lymph node metastases in early-stage cervical and endometrial cancers. Int J Gynecol Cancer. 2020, 30, 1404–1410. [Google Scholar] [CrossRef] [PubMed]
- Cibula D, Abu-Rustum NR, Dusek L, et al. Prognostic significance of low volume sentinel lymph node disease in early-stage cervical cancer. Gynecol Oncol. 2012, 124, 496–501. [Google Scholar] [CrossRef] [PubMed]
- Kocian R, Slama J, Fischerova D, et al. Micrometastases in Sentinel Lymph Nodes Represent a Significant Negative Prognostic Factor in Early-Stage Cervical Cancer: A Single-Institutional Retrospective Cohort Study. Cancers. 2020, 12, 1438. [Google Scholar] [CrossRef] [PubMed]
- Colturato LF, Signorini Filho RC, Fernandes RC, et al. Lymph node micrometastases in initial stage cervical cancer and tumoral recurrence. Int J Gynaecol Obstet. 2016, 133, 69–75. [Google Scholar] [CrossRef]
- Fregnani JH, Latorre MR, Novik PR, et al. Assessment of pelvic lymph node micrometastatic disease in stages IB and IIA of carcinoma of the uterine cervix. Int J Gynecol Cancer. 2006, 16, 1188–1194. [Google Scholar] [CrossRef]
- Marchiolé P, Buénerd A, Benchaib M, et al. Clinical significance of lympho vascular space involvement and lymph node micrometastases in early-stage cervical cancer: a retrospective case-control surgico-pathological study. Gynecol Oncol. 2005, 97, 727–732. [Google Scholar] [CrossRef]
- Guani B, Mahiou K, Crestani A, et al. Clinical impact of low-volume lymph node metastases in early-stage cervical cancer: A comprehensive meta-analysis. Gynecol Oncol. 2022, 164, 446–454. [Google Scholar] [CrossRef]
- Dostálek L, Benešová K, Klát J, et al. Stratification of lymph node metastases as macrometastases, micrometastases, or isolated tumor cells has no clinical implication in patients with cervical cancer: Subgroup analysis of the SCCAN project. Gynecol Oncol 2023, 168, 151–156. [CrossRef] [PubMed]
- Bhatla N, Berek JS, Cuello Fredes M, et al. Revised FIGO staging for carcinoma of the cervix uteri. Int J Gynaecol Obstet. 2019, 145, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Sedlis A, Bundy BN, Rotman MZ, et al. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: A Gynecologic Oncology Group Study. Gynecol Oncol. 1999, 73, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Bianchi T, Grassi T, Bazzurini L, et al. Radical Hysterectomy in Early-Stage Cervical Cancer: Abandoning the One-Fits-All Concept. J Pers Med. 2023, 13, 1292. [Google Scholar] [CrossRef] [PubMed]
- Ghoniem K, Larish AM, Dinoi G, et al. Oncologic outcomes of endometrial cancer in patients with low-volume metastasis in the sentinel lymph nodes: An international multi-institutional study. Gynecol Oncol. 2021, 162, 590–598. [Google Scholar] [CrossRef] [PubMed]
- A Zaal A, Zweemer RP, Zikán M, et al. Pelvic lymphadenectomy improves survival in patients with cervical cancer with low-volume disease in the sentinel node: a retrospective multicenter cohort study. Int J Gynecol Cancer. 2014, 24, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Ramirez PT, Frumovitz M, Pareja R, et al. Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer. N Engl J Med. 2018, 379, 1895–1904. [Google Scholar] [CrossRef]
- Nica A, Gien LT, Ferguson SE, et al. Does small volume metastatic lymph node disease affect long-term prognosis in early cervical cancer? Int J Gynecol Cancer. 2020, 30, 285–290. [Google Scholar] [CrossRef]
- Cibula D, Borčinová M, Kocian R, et al. CERVANTES: an international randomized trial of radical surgery followed by adjuvant (chemo) radiation versus no further treatment in patients with early-stage, intermediate-risk cervical cancer (CEEGOG-CX-05; ENGOT-CX16). Int J Gynecol Cancer 2022.
- Parpinel G, Laas-Faron E, Balaya V, et al. Survival after sentinel lymph node biopsy for early cervical cancers: a systematic review and meta-analysis. Int J Gynecol Cancer. 2023, 33, 1853–1860. [Google Scholar] [CrossRef]
- Pache B, Tantari M, Guani B, et al. Predictors of Non-Sentinel Lymph Node Metastasis in Patients with Positive Sentinel Lymph Node in Early-Stage Cervical Cancer: A SENTICOL GROUP Study. Cancers. 2023, 15, 4737. [Google Scholar] [CrossRef]
| Author | Date | Study design | Population | FIGO Stage | Prevalence of isolated LVM | Surgical LNtreatment | AdjuvantTreatment | Negative impact of LVM on oncologic outcome* | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LVM | ITC only | MIC only | Node negative | LVM | Endpoint | LVM | MIC | ITC | ||||||
| Marchiolè et al. | 2005 | Retrospective | 52 | IA2-IIB (FIGO 1988) | 12/52 (23%) | 6/52 (11,5%) | 6/52 (11,5%) | PLND | NA | NA | RR | Yes | Yes | Yes |
| Fregnani et al. | 2006 | Retrospective | 289 | IB-IIA (FIGO 1988) | 11/289 (3,8%) | NA | NA | PLND | NA | 4/11 (36%) | DFS | Yes | NA | NA |
| Cibula et al. | 2012 | Retrospective | 645 | IA1-IIB (FIGO 2009) | 71/645 (11%) | 25/645 (4%) | 46/645 (7%) | SLN + PLND | 48/456 (10,5%) | 51/71 (72%) | RFS OS |
NA NA |
Yes Yes |
No No |
| Stany et al. | 2015 | Retrospective | 129 | IA2-IB2 (FIGO 1988) | 26/129 (20%) | NA | NA | PLND | 19/103 (18,5%) | 10/26 (38%) | RFS, OS | No No |
NA | NA |
| Colturato et al. | 2016 | Retrospective | 83 | IB1-IIA (FIGO 2009) | 6/83 (7%) | NA | NA | PLND | 0/77 (0%) | 0/6 (0%) | RR | Yes | NA | NA |
| Guani et al. | 2019 | Prospective | 139 | IA1-IB1 (FIGO 2009) | 13/139 (9%) | 6/139 (4%) | 7/139 (5%) | SLN + PLND | NA | 4/13 (30%) | DFS | No | No | No |
| Nica et al. | 2019 | Prospective | 19 | IA1-IB3 (FIGO 2018) | NA | 9/19 (47%) | 10/19 (53%) | SLN or SLN+PLND |
NA | 14/19 (74%) | RFS | No | No | No |
| Kocian et al. | 2020 | Retrospective | 226 | IA1-IIB (FIGO 2009) | 24/226 (11%) | 8/226 (4%) | 16/226 (7%) | SLN or SLN+PLND |
NA | 17/24 (71%) | DFS OS |
NA NA |
Yes Yes |
No No |
| Buda et al. | 2020 | Retrospective | 573 | IA1-IB2 (FIGO 2018) | 21/573 (3,6%) | 4/573 (0,6%) | 17/573 (3%) | SLN or SLN+PLND |
NA | NA | DFS | No | No | No |
| Guani et al. | 2020 | Prospective | 321 | IA1-IB1 (FIGO 2009) | 24/321 (7%) | 24/321 (4%) | 11/321 (3%) | SLN or SLN+PLND |
NA | 13/24 (54%) | DFS | No | No | No |
| Dostalek et al. | 2023 | Retrospective | 967 | IA1-IIB (FIGO 2018) | 93/967 (10%) | 39/967 (4%) | 54/967 (6%) | SLN or SLN+PLND |
151/795 (19%) | 71/93 (76%) | DFS | NA | Yes | Yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





