1. Introduction
The removal of impacted third molars (Ms3) is one of the most common surgical interventions performed in dentistry [
1]. In Norway alone, approximately 75,000 Ms3 are removed annually, often by oral surgeons [
2,
3]. Impacted Ms3 may necessitate a removal procedure that frequently involves a surgical flap, ostectomy, and occasionally odontotomy, as well as soft tissue suturing. Unfortunately, manipulation of both soft and hard tissues can cause post-surgical swelling and pain, postoperative bleeding, hematomas, oral antral communications, reduced masticatory ability, trismus, and periodontal diseases at the distal aspect of the maxillary second molar (M2) [
1,
4,
5,
6,
7]. The surgical M3 removal procedure employed has been found to have conflicting results, with varying outcomes in adjacent M2 [
5,
8]. Despite the existence of multiple standards, there are conflicting data on the effect of surgical removal of Ms3, with differing outcomes for postoperative reinjury [
5]. It is evident from this context that surgeons are still struggling to manage the optimal approach of impacted Ms3, and predict the postoperative complications [
9]. Among the complications, bear importance mandibular fractures [
10], lesions to the inferior alveolar nerve [
11,
12,
13], and alveolar osteitis [
14,
15,
16]. Methods have been introduced aiming to control complications, such as drainage [
17], or application of platelet-rich fibrin [
18], gauzes soaked with cortisone [
19], or ozone [
20]. Surgery was also implemented with the use of Er:YAG Laser [
21] and coronectomy to avoid inferior alveolar nerve lesions [
22].
Nevertheless, maxillary wisdom tooth removal is normally considered not to be a very demanding type of surgery. This is because most of the time in that region, only the soft trabecular bone has to be removed to reach the impacted wisdom tooth. Therefore, no rotary instruments are used, but only hand instruments such as thin levers and no odontotomy are performed. As stated earlier, this situation is a common occurrence, but it is not a universal axiom. It's not difficult to describe some of the constant difficulties and complications, such as the difficulty in accessing that region, which affects visibility. The more the patient opens the mouth, the more the coronoid process, together with the surrounding soft tissues and mussels, covers the wisdom region. Therefore, to access the surgical area with surgical instruments like a scalpel, elevator, and levers, upper wisdom tooth extractions are usually performed through a partially closed mouth. Mainly because of this reason, the surgeon's touch-sensitive abilities often allow to extract the wisdom teeth without seeing them beforehand. The operator draws an incision line with the scalpel, elevates a full-thickness flap, and then enters the region with an elevator trying to achieve the cervical area of the impacted wisdom tooth distally to the second molar only through tactile sensitivity. Then, by making lever movements, the tooth is dislocated distobuccally out of the bone. All these surgical semi-blinded maneuvers might be difficult to perform.
One of the most common adverse events after surgery for a mandibular impacted wisdom tooth is swelling, accompanied by various degrees of pain. The most accredited hypothesis for this side effect can be attributed to full-thickness flap elevation to expose and remove the retained tooth [
23,
24].
In the typical procedure for the extraction of the maxillary impacted wisdom tooth, the surgery ends by repositioning the elevated flap to its original position and maintaining it through a surgical suture. Sutures stabilize the mobilized flap in its original position, guarantee proper hemostasis, and close possible oral antral communication that might occur after the extraction when the upper wisdom teeth are in direct contact with the maxillary sinus. Based on the previously described flap for removing mandibular impacted wisdom teeth [
23], a new flap design was created to remove maxillary impacted wisdom teeth. The extension of bone exposure was reduced by this flap, which could possibly reduce the negative effects of postoperative swelling and pain. Hence, this study aimed to assess the occurrence of adverse events after extraction of maxillary-impacted wisdom teeth using a traditional access (TA) or a new technique (NT).
2. Materials and Methods
2.1. Ethical Statements
This study followed the Declaration of Helsinki regarding medical protocol and ethics, and the CERA (Comitato Etico per la ricerca di Ateneo) of the University of Genoa approved the study on November 16, 2023 (protocol #2023/79). Written informed consent was obtained from all patients who voluntarily agreed to undergo the procedure and were willing to return for evaluation at regular intervals. Signed patient releases were obtained for imaging use.
2.2. Study Design
In this retrospective case-control study, we selected thirty documented cases from the Department of Surgical and Diagnostic Sciences (DISC) database at the University of Genoa in Italy. Each case involved a patient who underwent two different surgical techniques. The traditional technique (TA; control) was characterized by a standard incision made in the middle of the crest of the maxillary tuber, full-thickness flap elevation, and wound closure with sutures. In contrast, the new technique (NT; test) involved a single oblique incision, no flap and periosteum elevation, and wound closure with glue. Despite the retrospective nature of our study, we adhered to rigorous standards to ensure the reliability and transparency of our research.
2.3. Inclusion and Exclusion Criteria
All selected patients were treated for bilateral maxillary third molar extractions (Ms3). To be included in the study sample, patients had to meet the following inclusion criteria: (1) bilateral extraction of impacted upper Ms3; (2) availability of clinical and radiographic data.
The exclusion criteria were as follows: (1) monolateral extraction of impacted upper Ms3; (2) lack of clinical or radiographic data sufficient to harvest all necessary information needed for the study.
2.4. Sample Size Calculation
The sample calculation was based on the results of a previous study on the extraction of mandibular wisdom teeth performed by the same research group [
23]. A power of 0.95 and α error probability of 0.05, with a correlation between groups of 1.00 for edema, and 1.040 for pain, yielded a sample of 16 and 15, respectively. However, given that the extraction of maxillary wisdom teeth generally results in a lower degree of edema and pain compared to the mandibular wisdom teeth, it was decided to increase the sample to about double.
2.5. Presurgical Evaluations and Treatments
Before scheduling the patient for surgery, adequate professional hygiene and a review of oral maintenance were performed to achieve optimal plaque control with an average F.M.P.S. of < 20% in the study population. The participants were radiologically screened using an orthopanoramic radiograph (Planmeca ProMax® with a one-shot cephalostat; Helsinki, Finland).
2.6. Surgical Procedures
All surgeries were performed by the same surgeon (A.Mat.) and all patients underwent bilateral surgery on the same visit. Two cartridges of local anesthetic (2x1.8 ml of articaine 4% with adrenaline 1:100.000) were injected per side, buccal and palatal. The surgeon always started on the right side of the patient at tooth 1.8 and as second on the left side at tooth 2.8.
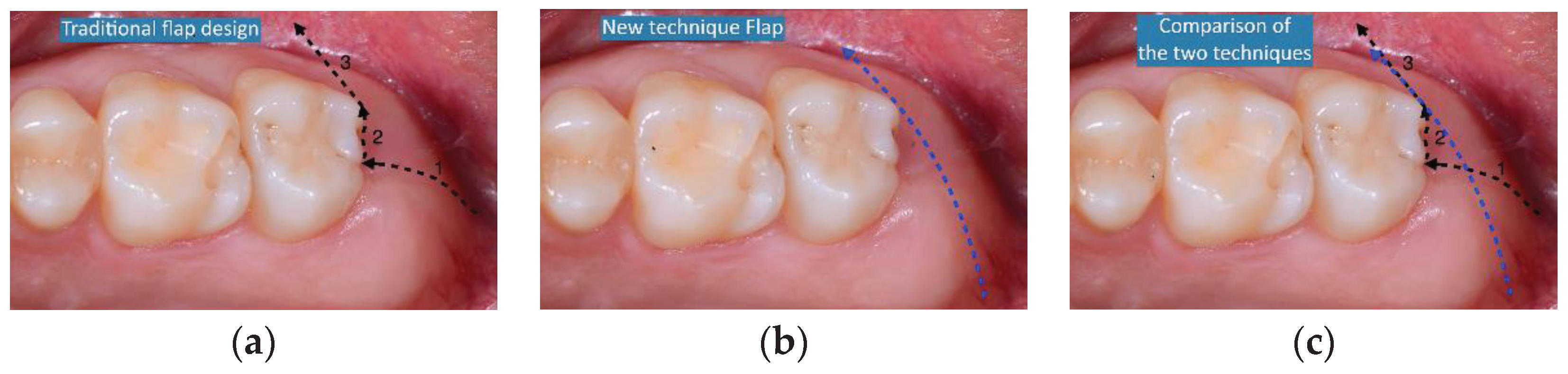
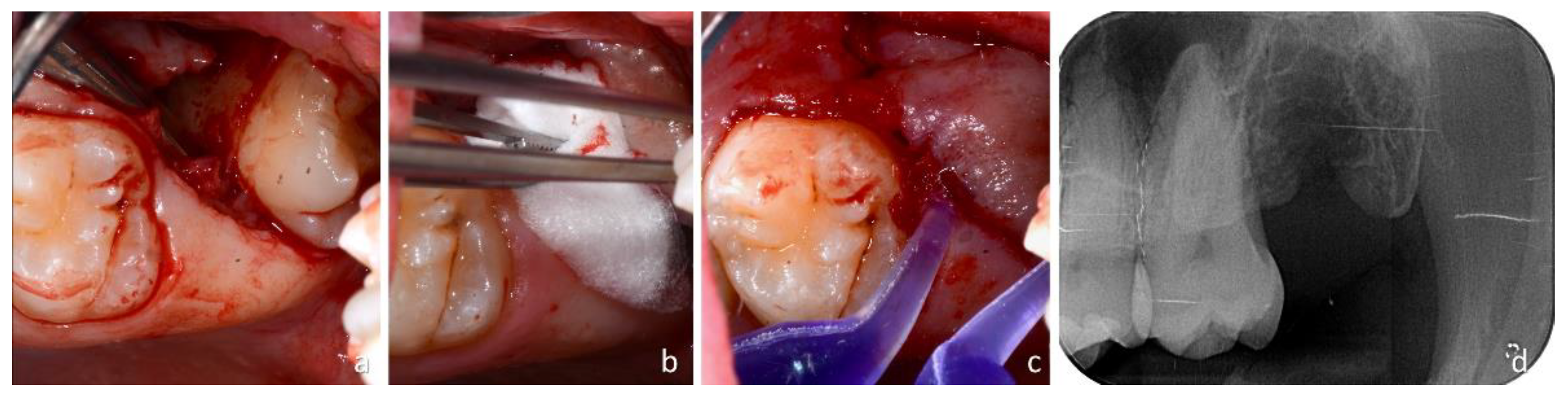
The two surgical techniques were compared (
Figure 1a-c).
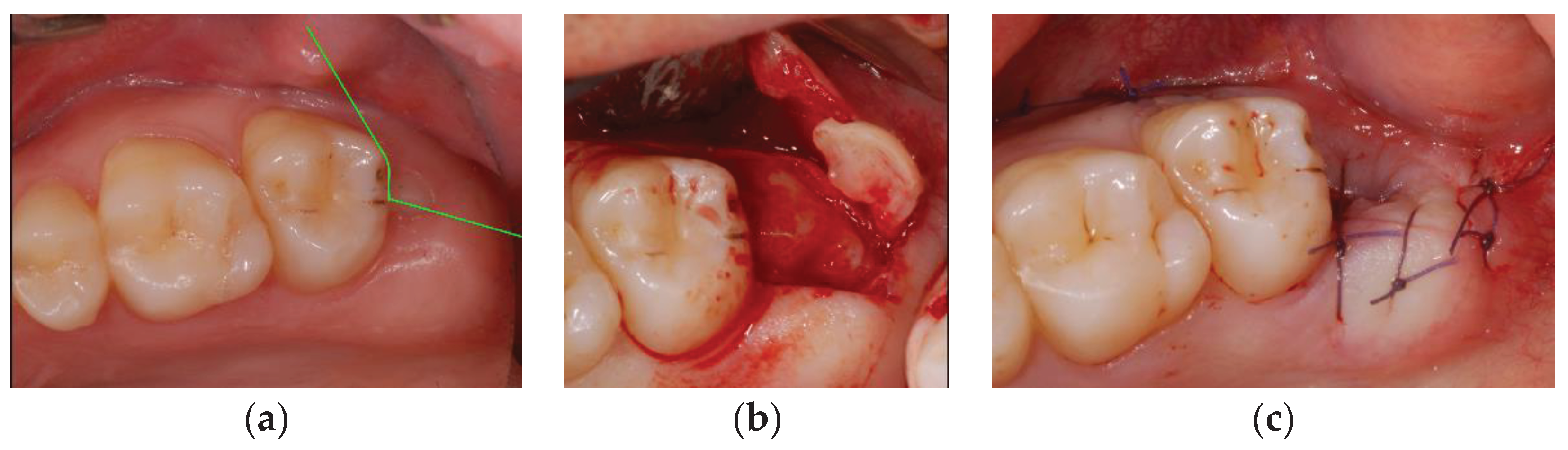
The traditional technique (TA) consists of a straight incision, beginning in the middle of the crest of the tuber maxillae and progressing forward to the middle of the distal surface of M2 (
Figure 2a).
In this region, the second incision began in the distal sulcus of M2 and proceeded buccally intrasulcular of the M2 ending at the distobuccal edge of M2. From this point, a releasing incision through the buccal attached gingiva over the mucogingival line described the third and last incisions. All incisions were made using a 15c Swann-Morton blade (
Figure 2b) and a triangular full-thickness flap, that is including the periosteum, was elevated with a Pritchard elevator (3 Prichard periosteal PPR36, Hu-Friedy Mfg. Co., Chicago, IL, USA). The wisdom tooth area was reachable using a straight 3 mm lever (Luxator Periotome L3S TiN Directa), which was gently pushed between the distal surface of M2 and the mesial surface of M3 to the cementum enamel junction of the impacted M3. When the surgeon felt that position, he began to rotate the lever distobuccal in order to extract the impacted M3. After the removal of M3 with the help of a 3 mm Lucas bone curette, the residual follicle of M3 was gently removed, and the residual thin, poorly attached bony walls of the empty alveolus were removed. A 5 ml sterile physiological solution wash was performed directly inside the wound using a single-use syringe. Subsequently, a resorbable bovine collagen sponge (hemocollagen; SEPTODONT, 58 rue du Pont de Creteil 94100 Saint Maur des Fosses France) was inserted into the wound directly in the superficial portion of the alveolus to stabilize the coagulum. The surgery ended by repositioning the elevated buccal flap in its original position and was secured using a monofilament synthetic absorbable poliglecaprone 4/0 USP surgical PGCL suture (OMNIA S.p.A., Fidenza, Italy). Single sutures were used to close the first distal incision and the buccal area to close the third releasing incision (
Figure 2c).
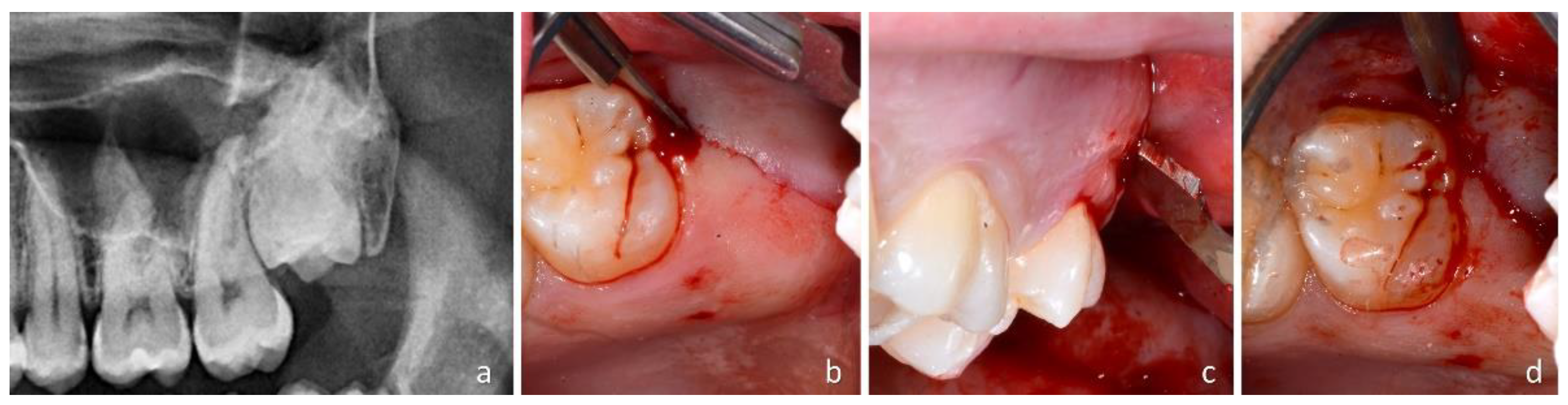
The newly proposed technique (NT) for impacted maxillary wisdom teeth (
Figure 3a) consisted of a single oblique incision that began in the keratinized mucosa on the distal palatal side of the tuber maxillae and crossed from the distopalatal side to the mesiobuccal side (
Figure 3b).
The 15c blade entered the gingival sulcus of M2 at its distal edge and continued its oblique path through the buccal attached gingiva, reaching the mucogingival line at the buccal side of M2 (
Figure 3c). This incision was made straight from the distopalatal portion of the tuber maxilla to the buccal mucogingival line of the buccal surface of M2. No flap was elevated so that the periosteum was not elevated but left adherent to the bone. Through the performed incision, at the distobuccal edge of the M2, a thin 3 mm straight lever (Luxator Periotome L3S TiN Directa) was inserted in the incision entering the tissues in contact with the distal surface of the M2. The lever was gently pushed inside the incision to reach the crown of M3 and subsequently between the crown of M3 and the distal surface of M2 (
Figure 3d).
When, by gently moving the lever, it was deemed that the cementum-enamel junction of M3 had been reached, a rotation of the lever was started to push M3 out of the wound towards the oral cavity. Soft tissues were cut through an oblique incision, and the wound was spread apart by the emerging tooth during extraction (
Figure 4a).
Subsequently, revision of the alveolus was performed using a 3 mm Lucas bone curette to remove the follicle of M3 and possible thin bone walls that were fractured during the extraction of M3. Subsequently, a wash was performed with 5 ml sterile physiological solution directly inside the alveolus using a disposable syringe. An absorbable bovine collagen sponge (Hemocollagene, SEPTODONT; Rue du Pont de Creteil 94100, Saint Maur des Fosses, France) was inserted into the wound directly in the superficial portion of the socket to stabilize the clot (
Figure 4b). As this surgical technique did not involve any flap lifting, the wound was closed using surgical glue (PeriAcry|®90HV Cyanoacrylate Oral scription; GluStitch Inc. 307–7188 Progress Way - Delta, British Columbia V4G 1M6, Canada) directly on the wound (
Figure 4c). A gentle stream of sterile saline solution was used to immediately set the glue, and an X-ray was taken to evaluate the complete extraction of the roots and possible complications, such as fractures of the tuberosity.
2.7. Clinical Evaluations
Patient sex and age were recorded. The following clinical parameters were evaluated and recorded: pocket probing depth distal (PPD-D) and distovestibular (PPD-DV) at the second molar.
Operative parameters evaluated were subjective difficulty encountered during extraction (0, straight through; 1, moments of uncertainty); bleeding within a few minutes after the end of the surgical procedure (0, no bleeding; 1, light bleeding; 2, heavy bleeding); and time for extraction from the first incision to when the last stitch was cut or when the gentle physiological washing of the glue to make it hardened quickly was finished.
Telephone calls were made the following day. At the 1-week visit, a VAS was used for the following evaluations: home bleeding (0, no bleeding; 1, light bleeding; 2, heavy bleeding), pain (0, no pain; 1, bearable pain; 2, significant pain; 3, unbearable pain), edema (0, absent; 1, light; 2, evident; 3, extreme), and hematoma (0, absent; 1, less than 2 cm in diameter; 2, more than 2 cm in diameter). Grade 2 home bleeding, and grade 3 pain and edema were considered complications.
Wound closure was evaluated after 4 and 8 weeks (0, closure; 1, no complete closure). At the 8-week visit, pocket probing depth distal (PPD-D) and distovestibular (PPD-DV) at the second molar and complaints (0, no complaints; 1, complaints, reporting type, and degree) were assessed.
2.8. Experimental Outcomes and Statistical Methods
The primary predictor variable of interest is the surgical technique employed, encompassing incision, periosteum elevation, and closure methods. The primary variables were postoperative pain and edema. The secondary variables included bleeding, hematoma, and surgery time. The values obtained are expressed as mean ± standard deviation. The Shapiro-Wilk test was used to determine the normality of data and, according to the results, the differences between the test and control sides were evaluated using a paired t-test or a Wilcoxon matched-pairs signed rank test.
3. Results
3.1. Demographic and Presurgical-Surgical Data
The thirty cases from treatment and follow-up corresponded to the period of 01/04/ 2022 and 31/03/ 2023. The mean age was 32.1 ±10.8 years, 14 were females, and 16 were males. The initial probing depth in the TA group was PPD D= 3.9 ±0.7 mm and PPD DV 2.5 ±0.5 mm. In the NT group, the respective measures were 4.1 ±0.9 and 2.5 ±0.6 (p= 0.109 and p>0.999, respectively).
3.2. Evaluation at the Surgery
The mean time used for all tooth extractions was 07:03” ±02:22” in the NT group and 11:01” ±02:17” in the TA group (p<0.0001). Difficulties during extraction were found in three cases in the NT group, with a mean time of 11:06” ±02:22”, and 3 cases in the TA group, with a mean time of 15:00” ±02:53”. Bleeding was not observed at the end of the surgical procedure.
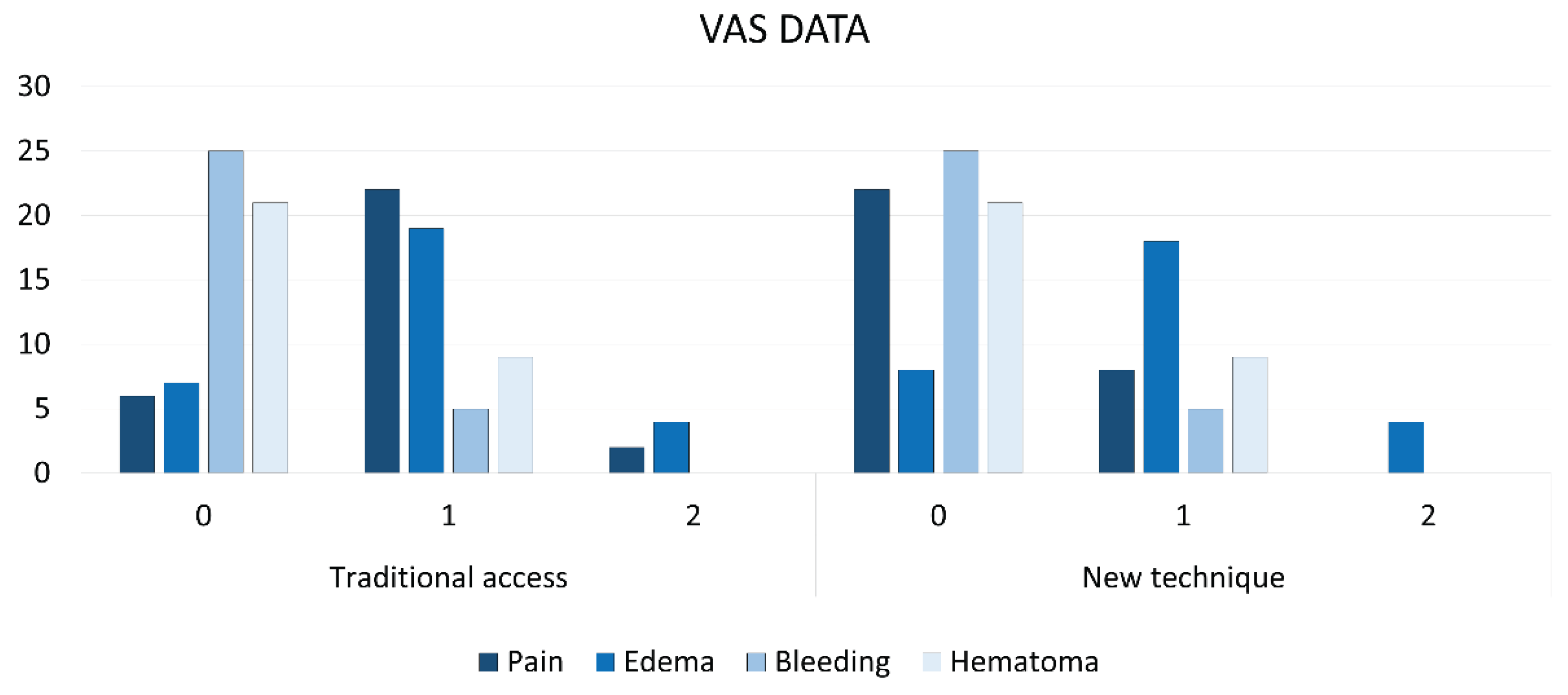
3.3. Evaluation at 1-Week of Healing
No major complications were registered. No pain was reported by 22 patients of the NT group, and only by 6 patients of the TA group; 2 patients in group TA reported significant pain while all remaining patients of both groups reported bearable pain (p<0.0001 between groups). The maximum grade of edema was 2 (evident), reported by four patients in both groups, while in most cases, light edema was reported (p>0.999 between groups). No home bleeding was reported by 25 patients in both groups while five patients in each group reported a grade 1. Hematomas were reported by 9 patients each group (grade 1; p>0.999).
Figure 5.
Number of patients presenting various grades of pain, Edema, Bleeding, and Hematoma.
Figure 5.
Number of patients presenting various grades of pain, Edema, Bleeding, and Hematoma.
3.4. Evaluation at the Follow-Ups
After 4 weeks, 25 wounds were closed in the NT group and 17 in the TA group (p<0.01). However, after 6 weeks, all wounds were closed in both groups (
Figure 4d). At 8 weeks, no complaints were reported by any of the patients. The PPD D and PPD DV in the NT group were 3.4 ±0.5 mm and 2.4 ±0.6 mm, respectively. The differences between the preoperative and 8-week postoperative probing depth yielded p<0.01 for PPD D and p=0.500 for PPD DV. In the TA group, the respective probing depths were 3.6 ±0.7 mm and 2.5 ±0.5 mm (p=0.100 and p>0.999, respectively).
4. Discussion
This study aimed to evaluate the postoperative adverse events after maxillary-impacted wisdom tooth extraction using traditional or modified access. The two techniques differ in terms of incision access, flap elevation, and wound closure. Traditional incision includes a straight incision in the middle of the tuber and a releasing incision in the distal aspect of the second molar. A full-thickness including the periosteum will be elevated. The modified access included only an oblique incision from the distal palatal side of the tuber to the distal buccal aspect of the second molar, crossing the attached buccal gingiva to the buccal mucosa. The peculiarity of this modified incision is that, besides allowing access to the impacted tooth with levers, it might be dislocated distobuccally like a trapdoor without elevating the periosteum. Without flap elevation, the elasticity of the flap allows the tooth to be enucleated, and owing to its elastic memory, it will regress to its original position. Therefore, after the placement of a collagen sponge, no sutures are needed to secure the flaps, and only cyanoacrylate glue can be applied.
A modified flap has several advantages. The pain reported by the patients was lower in the modified access group than in the traditional access group (p<0.0001 between groups), even though only two patients in the TA group reported significant pain. However, no differences were reported in edema. Flap design has assumed particular importance in recent years, especially for the extraction of impacted mandibular wisdom teeth. Attention has been paid to improving periodontal healing in the second molar and wound closure [
25,
26,
27]. However, no significant advantages were observed for postoperative pain or edema.
Recently, a modification of the access for the extraction of impacted third mandibular molars has been suggested. Traditional access with flap elevation was compared with complete removal of the oral mucosa above the impacted tooth, which is described as a flapless surgical approach (FSA). A lower degree of pain and edema was observed in the modified FSA approach than in the traditional approach [
23]. A further improvement was subsequently suggested by the same group [
24]. In an RCT study, the FSA technique was compared with a new technique called “single incision access” (SIA), which only included a small semilunar incision above the buccal profile of the impacted tooth. From this “small” access, the wisdom tooth could be extracted. The SIA approach produced results similar to those of the FSA in terms of postoperative pain and edema; however, the recovery of the treated region was faster.
This confirmed that the management of soft tissues is extremely important for postsurgical patient comfort. Applying similar care for soft tissue management for the extraction of maxillary impacted wisdom teeth, the postsurgical period of the patients also improved in quality compared with the traditional technique. After 4 weeks of healing, 25 wounds were closed in the modified flap group and 17 in the traditional flap group (p<0.01). Moreover, the modified surgical procedure used in the present study was faster than that of the traditional flap approach, that is, 7 min compared with 11 min, which is also in favor of the modified access. Some may argue that the use of glue significantly affected the time calculation. However, it is important to note that no flaps were elevated in the NT group, allowing the periosteum to remain adhered to the bone. This resulted in the modified flap tending to regress to its original position, thereby favoring the use of glue over sutures. In contrast, the traditional access (TA), which involved full-thickness flaps and periosteum elevation, did not allow for a secure wound closure using glue, and sutures had to be used to secure the wounds. This implies that the variables to be considered should not be two—incision and sutures—but rather only one, “the technique”, that includes flap and closure. Finally, the difficulties in tooth extraction were similar in both groups, indicating that the new flap did not complicate the surgical procedure.
5. Conclusions
In conclusion, the implementation of the new technique for extracting impacted maxillary wisdom teeth not only resulted in a reduction of post-surgical pain but also led to a decrease in surgical duration. The adoption of a simplified incision did not introduce complexity to the surgical procedure; instead, it facilitated the utilization of adhesive agents in place of sutures, significantly streamlining surgical time. These findings underscore the efficacy and practicality of the new technique, offering a promising avenue for improved outcomes and efficiency in impacted maxillary wisdom teeth extraction procedures.
This version maintains the essence of your original conclusion while refining the language for clarity and impact. Let me know if you need further adjustments or have any other questions!
Author Contributions
Conceptualization, A.Mat. and S.B.; methodology, A.Mat.; formal analysis, K.A.A.A, and D.B.; investigation, A.Mat.; resources, A.Mat. and S.B.; data curation, A.Mat., A.Mal., and D.B.; writing—original draft preparation, Mat.A., K.A.A.A., and D.B.; writing—review and editing, A.Mat., A.Mal., and D.B.; visualization, A.Mal.; supervision, S.B.; project administration, A.Mal.; funding acquisition, A.Mat., and D.B. All authors have read and agreed to the published version of the manuscript.
Funding
No economic support was received by any author.
Institutional Review Board Statement
This study followed the Declaration of Helsinki regarding medical protocol and ethics, and the CERA (Comitato Etico per la ricerca di Ateneo) of the University of Genoa approved the study on November 16, 202 (protocol #2023/79)9.
Informed Consent Statement
Written informed consent was obtained from all patients who voluntarily agreed to undergo the procedure and were willing to return for evaluation at regular intervals. Signed patient releases were obtained for imaging use.
Data Availability Statement
Data is available under reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Barbato, L.; Kalemaj, Z.; Buti, J.; Baccini, M.; La Marca, M.; Duvina, M.; Tonelli, P. Effect of surgical intervention for removal of mandibular third molar on periodontal healing of adjacent mandibular second molar: A systematic review and bayesian network meta-analysis. J. Periodontol. 2016, 87, 291–302. [Google Scholar] [CrossRef] [PubMed]
- Berge, T.I.; Bøe, O.E. Predictor evaluation of postoperative morbidity after surgical removal of mandibular third molars. Acta Odontol. Scand. 1994, 52, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Øyri, H.; Bjørnland, T.; Barkvoll, P.; Jensen, J.L. Mandibular third molar surgery in 396 patients at a Norwegian university-clinic: Morbidity recorded after 1 week utilizing an e-infrastructure for clinical research. Acta Odontol. Scand. 2016, 74, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-W.; Lee, C.-T.; Hum, L.; Chuang, S.-K. Effect of flap design on periodontal healing after impacted third molar ex-traction: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2017, 46, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Khaleelahmed, S.; Alqahtani, N.A.; Desai, F. Evaluation of two flap designs on the mandibular second molar after third molar extractions. J. Oral Maxillofac. Pathol. 2017, 21, 317–318. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Liu, Z.; Shi, Y.; Fang, D.; Li, S.; Zhang, D. A novel orthodontic extraction method for removal of impacted mandibular third molars in close proximity to inferior alveolar nerve. J. Oral. Maxillofac. Surg. 2019, 77, 1575.e1–1575.e6. [Google Scholar] [CrossRef] [PubMed]
- Coulthard, P.; Bailey, E.; Esposito, M.; Furness, S.; Renton, T.F.; Worthington, H.V. Surgical techniques for the removal of mandibular wisdom teeth. Cochrane Database Syst. Rev. 2014, 29, CD004345. [Google Scholar] [CrossRef] [PubMed]
- Suarez-Cunqueiro, M.M.; Gutwald, R.; Reichman, J.; Otero-Cepeda, X.L.; Schmelzeisen, R. Marginal flap versus paramarginal flap in impacted third molar surgery: A prospective study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2003, 95, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Gojayeva G, Tekin G, Saruhan Kose N, Dereci O, Kosar YC, Caliskan G. Evaluation of complications and quality of life of patient after surgical extraction of mandibular impacted third molar teeth. BMC Oral Health. 2024 Jan 25;24(1):131. PMCID: PMC10811863. [CrossRef] [PubMed]
- Libersa, P.; Roze, D.; Cachart, T.; Libersa, J.-C. Immediate and late mandibular fractures after third molar removal. J. Oral Maxillofac. Surg. 2002, 60, 163–165. [Google Scholar] [CrossRef] [PubMed]
- Lu Z, Bingquan H, Jun T, Fei G. Effectiveness of concentrated growth factor and laser therapy on wound healing, inferior alveolar nerve injury and periodontal bone defects post-mandibular impacted wisdom tooth extraction: A randomized clinical trial. Int Wound J. 2024 Jan;21(1):e14651. PMCID: PMC10789919. [CrossRef] [PubMed]
- Rieder M, Remschmidt B, Schrempf V, Schwaiger M, Jakse N, Kirnbauer B. Neurosensory Deficits of the Mandibular Nerve Following Extraction of Impacted Lower Third Molars-A Retrospective Study. J Clin Med. 2023 Dec 13;12(24):7661. PMCID: PMC10743649. [CrossRef] [PubMed]
- Kuang S, Liu Y, Zhuang W, Li K, Yang W, Tian Y. The effect of root orientation on inferior alveolar nerve injury after extraction of impacted mandibular third molars based on propensity score-matched analysis: a retrospective cohort study. BMC Oral Health. 2023 Nov 27;23(1):929. PMCID: PMC10680265. [CrossRef] [PubMed]
- Ghosh A, Aggarwal VR, Moore R. Aetiology, Prevention and Management of Alveolar Osteitis-A Scoping Review. J Oral Rehabil. 2022 Jan;49(1):103-113. Epub 2021 Oct 22. [CrossRef] [PubMed]
- Chisci G, Capuano A, Parrini S. Alveolar Osteitis and Third Molar Pathologies. J Oral Maxillofac Surg. 2018 Feb;76(2):235-236. Epub 2017 Nov 16. [CrossRef] [PubMed]
- Daly BJ, Sharif MO, Jones K, Worthington HV, Beattie A. Local interventions for the management of alveolar osteitis (dry socket). Cochrane Database Syst Rev. 2022 Sep 26;9(9):CD006968. PMCID: PMC9511819. [CrossRef] [PubMed]
- Selvaraj S, Periyasamy IK, Elangovan GP, Su A, Srinath K, Sivaragahvi B. Comparative Evaluation of the Placement of Drain Versus Normal Suturing to Eliminate Postoperative Complications After the Surgical Removal of Impacted Third Molar. Cureus. 2024 Jan 2;16(1):e51517. PMCID: PMC10832945. [CrossRef] [PubMed]
- Mathialagan Kalai Selvam L, M A, Lakshmanan S, Kumar SP. Effectiveness of Advanced Platelet-Rich Fibrin on Postoperative Sequelae for Impacted Mandibular Third Molar Surgery: A Prospective Study. Cureus. 2024 Jan 15;16(1):e52297. PMCID: PMC10865923. [CrossRef] [PubMed]
- Krishna S, Bhaskaran R, Kumar SP, Krishnan M. Efficacy of Oxytetracycline Hydrocortisone-Soaked Gauze Pack on Postoperative Sequelae in Lower Third Molar Surgery: A Prospective Study. Cureus. 2024 Jan 14;16(1):e52245. PMCID: PMC10863368. [CrossRef] [PubMed]
- Varghese LJ, Lahiri B, Penumatsa NV, Soans CR, Sekar A, Nasyam FA. Effectiveness of Topical Ozone Gel Application in the Management of Postextraction Wound Healing: An In Vivo Study. J Contemp Dent Pract. 2023 Nov 1;24(11):887-890. [CrossRef] [PubMed]
- Sandhu R, Kumar H, Dubey R, Vyas D, Shahi AK. Comparative Study of the Surgical Excision of Impacted Mandibular Third Molars Using Surgical Burs and an Erbium-Doped Yttrium Aluminum Garnet (Er:YAG) Laser. Cureus. 2023 Dec 2;15(12):e49816. PMCID: PMC10758536. [CrossRef] [PubMed]
- Peixoto AO, Bachesk AB, Leal MOCD, Jodas CRP, Machado RA, Teixeira RG. Benefits of Coronectomy in Lower Third Molar Surgery: A Systematic Review and Meta-analysis. J Oral Maxillofac Surg. 2024 Jan;82(1):73-92. Epub 2023 Oct 6. [CrossRef] [PubMed]
- Materni A, De Angelis N, Di Tullio N, Colombo E, Benedicenti S, Amaroli A. Flapless Surgical Approach to Extract Impacted Inferior Third Molars: A Retrospective Clinical Study. J Clin Med. 2021 Feb 4;10(4):593. PMCID: PMC7914559. [CrossRef] [PubMed]
- Materni A, Pasquale C, Signore A, Benedicenti S, Amaroli A. Comparison between the Flapless Surgical Approach and a Novel Single Incision Access in Terms of Recovery Time and Comfort after Extraction of Impacted Inferior Third Molars: A Ran-domised, Blinded, Split-Mouth Controlled Clinical Trial. J Clin Med. 2023 Mar 2;12(5):1995. PMCID: PMC10004479. [CrossRef] [PubMed]
- Korkmaz, Y.T.; Mollaoglu, N.; Ozmeriç, N. Does Laterally Rotated Flap Design Influence the Short-Term Periodontal Status of Second Molars and Postoperative Discomfort after Partially Impacted Third Molar Surgery? J. Oral Maxillofac. Surg. 2015, 73, 1031–1041. [Google Scholar] [CrossRef] [PubMed]
- Kirtiloğlu, T.; Bulut, E.; Sümer, M.; Cengiz, I. Comparison of 2 Flap Designs in the Periodontal Healing of Second Molars after Fully Impacted Mandibular Third Molar Extractions. J. Oral Maxillofac. Surg. 2007, 65, 2206–2210. [Google Scholar] [CrossRef] [PubMed]
- Choudhury, R.; Rastogi, S.; Rohatgi, R.G.; Abdulrahman, B.I.; Dutta, S.; Giri, K.Y. Does Pedicle Flap Design Influence the Postoperative Sequel of Lower Third Molar Surgery and Quality of Life? J. Oral Biol. Craniofac. Res. 2022, 12, 694–701. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).