Introduction
Since the initial outbreak of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in late December 2019, more than 703 million people have been infected with Coronavirus disease 2019 (COVID-19), which led to an estimated 6.9 million deaths.[
1,
2] While the virus primarily targets the respiratory system, its impact on coagulopathy triggering thrombosis and the direct and indirect insult on the cardiovascular system can also provoke a higher risk of acute myocardial infarction (AMI).[
3,
4]
Over the course of the pandemic, many drastic measures and changes were brought forward to reduce the impact of the virus, such as lockdown protocols and vaccinations. While past studies from the National Inpatient Sample(NIS) have evaluated different aspects of how the virus influenced the odds and outcomes of AMI patients in 2020[
5,
6,
7,
8], at present, there are none comparing how COVID-19 patients with AMI fared between the two years of the pandemic. Therefore, we propose a retrospective study to improve our understanding of potential differences.
Materials and Methods
Data Source
We evaluated patients with a primary diagnosis code for COVID-19 in 2020 and 2021 via the NIS. The NIS is produced each year under the supervision of the Healthcare Cost Utilization Project(HCUP) and the Agency for Healthcare Research and Quality(AHRQ). The de-identified data from the NIS covers around 20% of hospital records across 48 states in the United States. The use of the discharge code “DISCWT” allows users to estimate more than 97% of the population.[
9,
10]
The 2021 NIS was released in 2024 and is, to date, the most recent national data covering COVID-19 hospitalization by HCUP. The NIS contains multiple patient records at a de-identified level, along with up to 40 clinical diagnoses and 25 procedures that can be evaluated using International Classification of Diseases (ICD) codes. For the NIS 2020 and 2021, users are required to use ICD-10 codes. In addition, the NIS also contains hospital characteristics such as location/teaching status, region, and bed size.[
9]
Sample and Statistical Analysis
The ICD-10 diagnosis code for COVID-19, “U071”, was started on April 1
st, 2020, and as per HCUP’s recommendations, we only retained patients from April 1st, 2020, till December 31st, 2021, for our study.[
9]
First, all cases of COVID-19 with a primary diagnosis were extracted. We excluded those of ages <18 years. The month-to-month event of AMI among COVID-19 hospitalizations was evaluated using linear-by-linear association.
We then proceeded to retain only COVID-19 cases with a coexisting code for AMI, and two groups were made: patients admitted in 2020 vs. those admitted in 2021. Additional comorbidities, diagnoses, and procedures were included via their ICD-10 codes.[
10,
11,
12,
13,
14,
15,
16,
17,
18,
19,
20,
21,
22] Cells missing data for month or year were excluded from this study. The characteristics of the two groups were compared using Chi-Square tests for categorical variables (reported as frequency (%)) and T-tests(or Mann-Whitney U tests) for continuous variables (reported as mean ± SD).[
9]
Our primary outcome was the all-cause mortality among COVID-19 patients with AMI. We further explored the use of CABG, PCI, mechanical ventilation, IABP, and events of AKI, cardiogenic shock, cardiac arrest, and cardiac arrhythmias (atrial fibrillation, ventricular fibrillation, and supraventricular tachycardia) in these patients. The mean length of stay(LOS) and their mean hospital charges were also compared. The complications and outcomes were evaluated via multivariable regression analyses as an adjusted odds ratio (aOR), along with their 95% confidence interval (95% CI), and p-value. We retained statistical significance for p<0.05 throughout our study. The analyses were performed using SPSS 29.0 (IBM Corp., Armonk, New York, USA) and STATA 18.0 MP (StataCorp LLC).
As HCUP provided the data in de-identified form, we were exempted from any ethical or IRB approval. We also adhered strictly to the guidelines and rules of HCUP in the use of these databases. All cases <11 were not included in our results.[
9]
Results
In the United States, an estimated 2,541,992 adult cases of COVID-19 were found between April 2020- December 2021, with 1,019,860 cases between April to December 2020 and 1,522,131 cases between January to December 2021.
AMI Trend among COVID-19 Cases
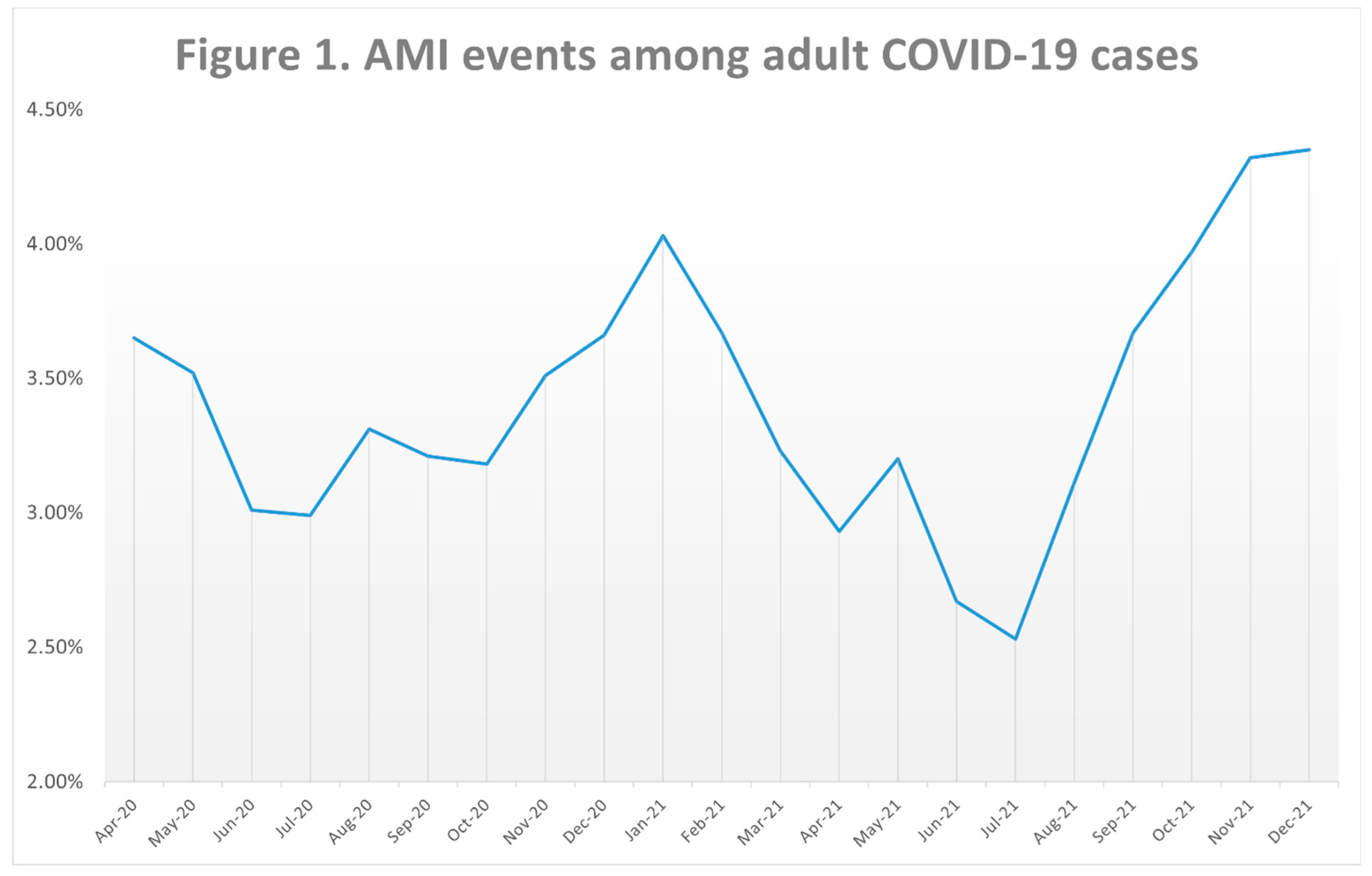
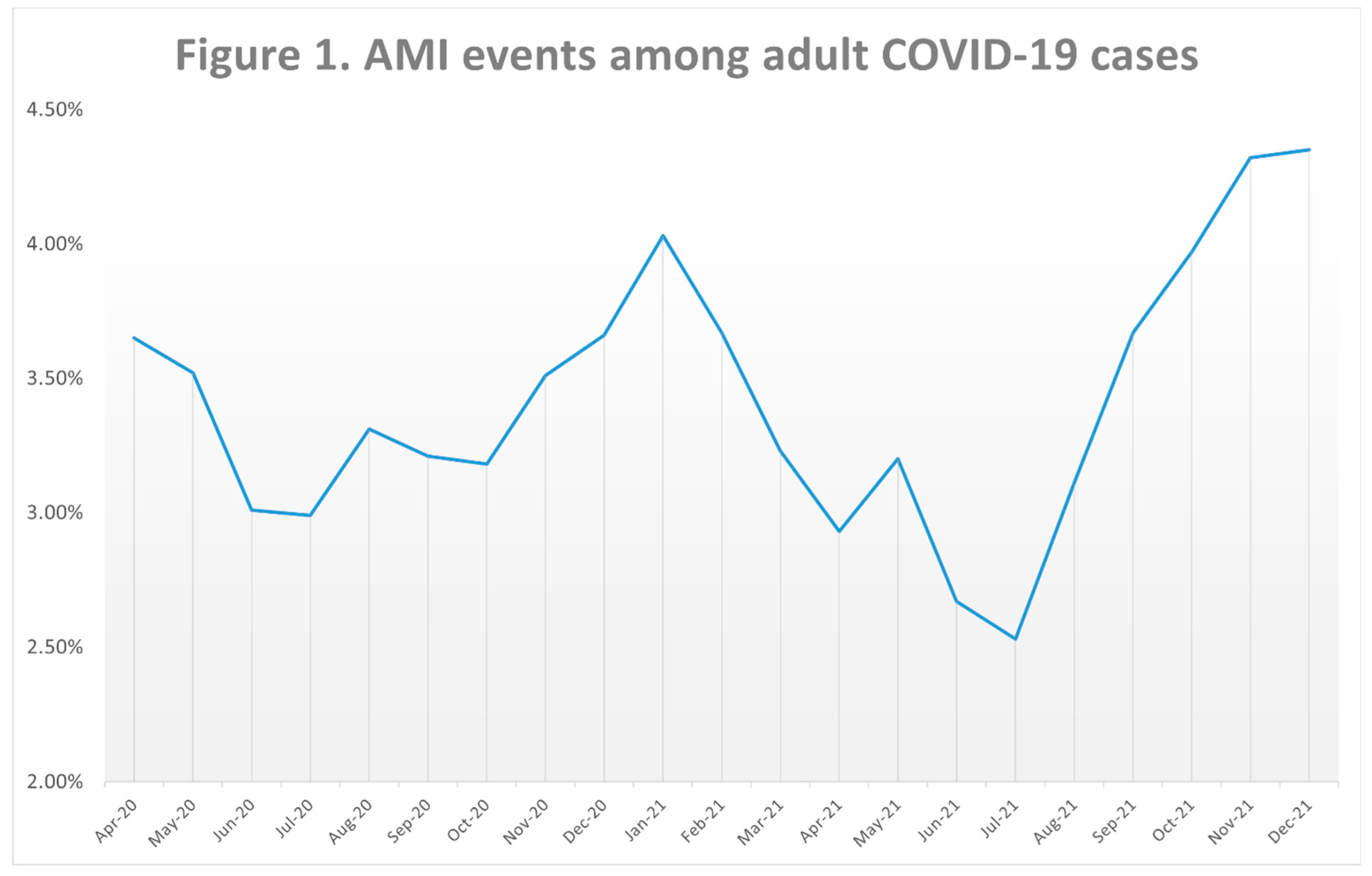
The incidence of AMI among COVID-19 cases fluctuated across the 21 months of our study. Between April and July 2020, it dropped from 3.65% to 2.99%, followed by a rise till January 2021(4.03%). From January 2021 to July 2021, a drop was seen as it reached 2.53%, which was followed by a sharp rise till December 2021(4.35%) (p
trend<0.01). The overall rate of AMI across these 21 months was 3.55% (
Table 1, Figure 1).
Comparing AMI Cases in COVID-19 Patients in 2020 vs. 2021
We evaluated 90,180 AMI cases among COVID-19 patients. 34,735 were in our 2020 cohort, while 55,445 were in hospitalizations of COVID-19 cases in 2021.
Baseline Characteristics
AMI cases in COVID-19 patients were younger in 2021 as compared to 2020, with a mean age of 70.31 vs. 72.38 years(p<0.01) (
Table 2).
Both groups involved mostly males, with a slightly higher presence of females in 2021 vs. 2020 (40.5% vs. 39.3%, p<0.01). In addition, we found that Medicare covered 69.9% of cases in 2020 and 66.1% of cases in 2021(p<0.01). Racially, Whites formed the biggest part of the AMI cases as 55.6% in 2020 and 65.0% in 2021 were Whites. Most cases were also in the 0-25th household income percentile in both groups (36.8% in 2020 and 36.8% in 2021, p<0.01), and the patients were treated in large bed-size hospitals (46.6% in 2020 and 44.6% in 2021), and hospitals classified as urban teaching centers(71.2% in 2020, 68.3% in 2021, p<0.01). Geographically, most cases were from the southern regions of the US(38.7% in 2020, 42.8% in 2021, p<0.01).
We found that cases in 2020 had higher prevalence of hypothyroidism (14.1%vs. 13.2%, p<0.01), dyslipidemia (53.2% vs. 49.4%, p<0.01), diabetes (49.0% vs. 45.9%, p<0.01), chronic kidney disease (40.5% vs. 39.2%, p<0.01), prior CABG (8.4% vs. 7.6%, p<0.01), prior PCI (10.7% vs. 9.2%, p<0.01), family history of CAD (4.5% vs. 4.0%, p<0.01), prior stroke (8.3% vs. 7.6%, p<0.01), and prior myocardial infarction(9.4% vs. 8.8%, p<0.01). On the contrary, 2020 cases had fewer smokers (28.1% vs. 30.1%, p<0.01), cases with liver cirrhosis (5.2% vs. 5.8%, p<0.01), alcohol abuse (1.8% vs. 2.4%, p<0.01), obesity (20.4% vs. 25.5%, p<0.01), drug abuse (2.0% vs. 2.8%, p<0.01), and COPD (20.7% vs. 21.9%, p<0.01).
The overall mean Charlson Comorbidity (CCI) score was higher in the 2020 cohort (5.04 vs. 4.91. p<0.01). 2021 admissions were longer (11.20 days vs. 9.95 days, p<0.01), with a higher mean hospital charge ($155587 vs. $130538, p<0.01).
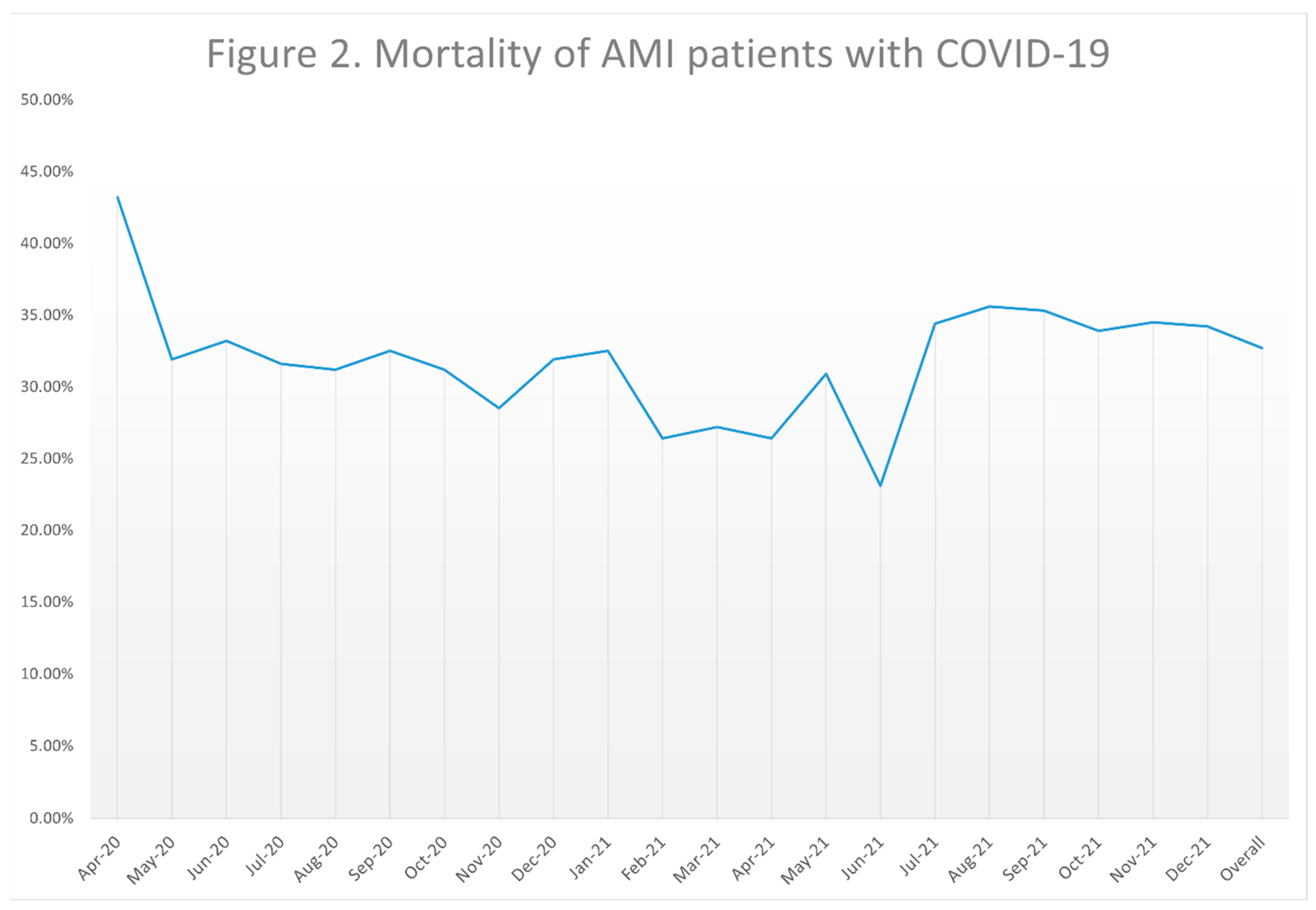
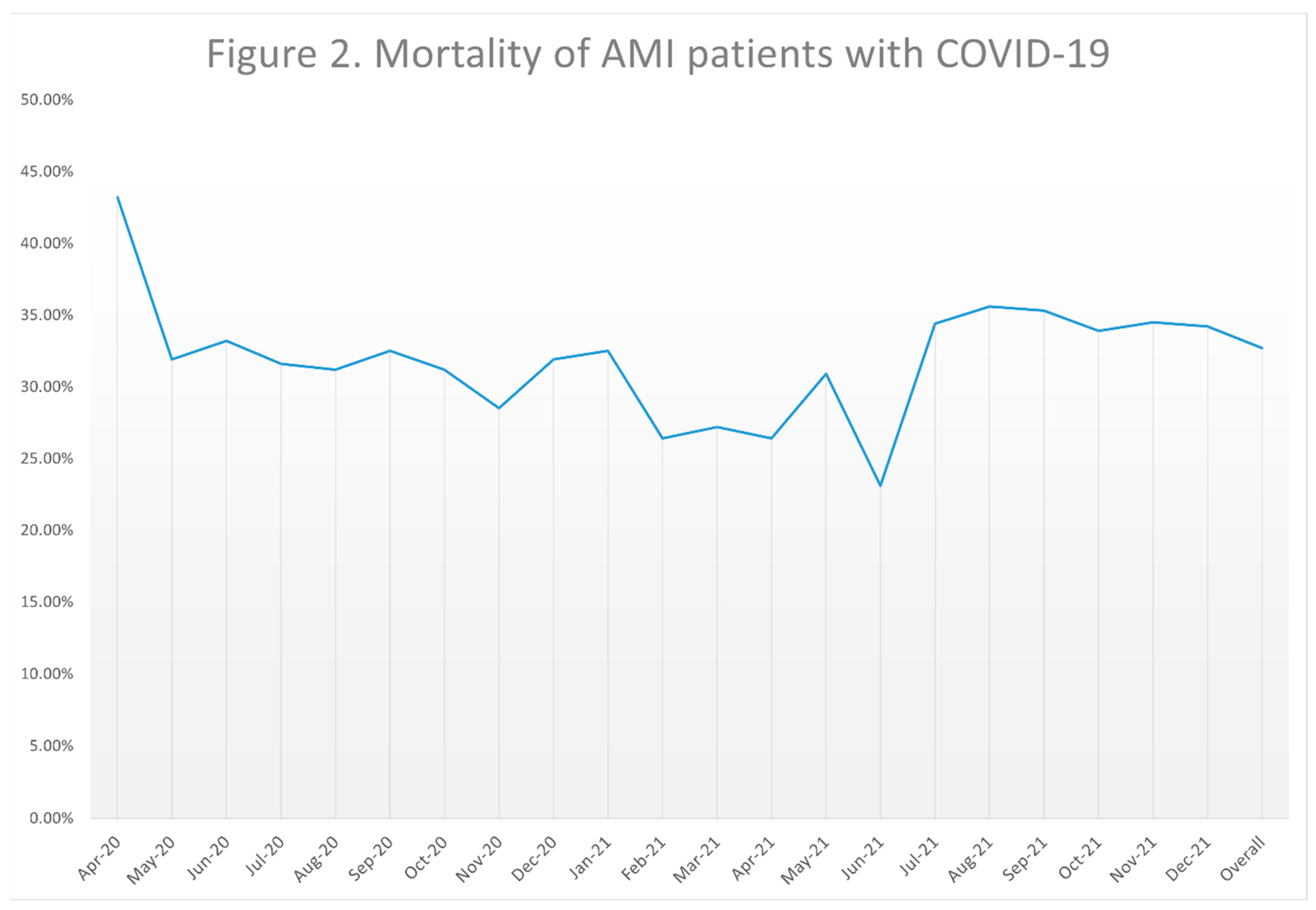
Trends in Mortality
The overall mortality rate fluctuated between the 21 months of our study, with a maximum of 43.2% observed in April 2020 and a minimum of 23.1% in June 2021. The trend was not statistically significant (p
trend =0.103)(
Table 3, Figure 2).
Events of Cardiac Arrhythmias
Multivariable regression models for cardiac arrhythmias found that in 2021, there were higher odds of events of ventricular tachycardia (aOR1.126, 95% CI 1.062-1.194, p<0.01) among COVID-19-positive patients who experienced AMI than those in 2020. No differences were seen for atrial fibrillation or supraventricular tachycardia (
Table 4).
Complications and Outcomes
Our study found several differences in outcomes between the two years of the pandemic. In 2021, patients with AMI while admitted for COVID-19 had a higher likelihood of having a PCI (aOR 1.627, 95% CI 1.454-1.822, p<0.01), while also reporting more complications such as acute kidney injury (aOR 1.078, 95% CI 1.047-1.110, p<0.01), acute ischemic stroke (aOR 1.215, 95% CI 1.113-1.328, p<0.01), events of cardiac arrest (aOR 1.106, 95% CI 1.050-1.166, p<0.01), need for mechanical ventilation (aOR 1.133, 95% CI 1.096-1.172, p<0.01), and all-cause mortality (aOR 1.032, 95% CI 1.001-1.064, p=0.043). We found no statistically significant results for events of cardiogenic shock and the need for IABP between these two years. (
Table 3).
Discussions
In our study, there were several key differences in incidence of AMI among COVID-19 patients, patient characteristics, and outcomes of the AMI cases between the first two years of the pandemic in the United States.
We found that AMI events among COVID-19 cases reached an initial peak during January 2021. This corresponds to another peak previously reported among the daily deaths during that same month, which to date was the highest number of COVID-related deaths reported in the United States and worldwide.[
23,
24] Our analysis also confirmed a continuous drop in AMI cases between January to July 2021, which could also correlate to the introduction of vaccination access to the general public and expansion of vaccination campaigns in the United States. However, we further noticed that from July 2021, the incidence of AMI among COVID-19 patients rose constantly till the end of our study (December 2021). This may be linked to the waning levels of antibodies following vaccination, the changes in preventive protocols to prevent infection in at-risk groups, and the impact of viral mutations(such as Delta, Omicron, Alpha, Gamma, and Beta) and their pathophysiological impact on the cardiovascular system.[
25,
26,
27,
28,
29,
30,
31,
32] Further studies exploring the hesitancy of patients with AMI symptoms to seek medical care due to fear of being infected with COVID-19 while being hospitalized should also be explored.[
33,
34]
There were also some discrepancies in the patient demographics between the AMI patients in our two groups. AMI patients were younger in 2021, with varying differences in several comorbidities between the two groups, and expressed a lower mean CCI score in 2021 as compared to 2020. Based on the data provided by the CDC, the mortality rates of all COVID-19 cases among various younger adult groups also rose in 2021; for example the mortality among COVID-19 patients of ages 35-44 and 45-54 rose from 16.0 and 45.2 per 100,000 standard population to 40.6 and 97.9 per 100,000 standard population in 2021, while the rise in much older groups was less drastic; from 644.4 to 649.3 among patients ages 75-84.[
35] Furthermore, vaccination hesitancy among younger population may have predisposed them to worse outcomes following COVID-19.[
36] We therefore encourage additional retrospective studies to identify the factors associated with the differences seen, as it can be utilized as a model to improve the outcomes in any future pandemics.[
37]
Finally, our study also found several differences in the outcomes between the 2021 and 2020 AMI cases in COVID-19 patients. The CDC has confirmed that there was a higher mortality rate among COVID-19 patients in 2021, as the overall deaths rose from 93.2 per 100,000 individuals to 111.4 per 100,000 individuals. A similar rise was seen as 2021 AMI cases reported higher odds of death in our study.[
35] Furthermore, we also found various complications such as events of cardiac arrest, ventricular tachycardia, acute ischemic stroke, acute kidney injury and need for mechanical ventilation, which can predispose to a higher mortality rate.[
38] The higher use of PCI in 2021 could correlate with the improvement in the access of care and distribution of resources as compared to the first year of the pandemic.[
39,
40]
As our study relies on the NIS, there are several associated limitations that can be addressed in future studies. The 2021 NIS does not have data on the vaccination status of the patients, which could influence outcomes. In addition, the NIS does not include details about their medication history and treatment plans during their hospitalization. Our study could not include critical physical examination, laboratory test results, and radiographic findings that could help categorize and study the patients based on severity. Mistakes in codes and inputs at physician level may also influence our results.[
6,
41]
Conclusion
Our retrospective study, via one of the biggest hospitalization records, has shown that incidence of AMI among COVID-19 patients between April 2020 to July 2021 was highest in January 2021, and from July 2021 the numbers rose constantly till December to reach a new peak. Differences in the comorbidities and characteristics existed in the COVID-19 positive adults with AMI between the two years, who also experienced more complications in 2021, and a higher adjusted odds ratio of mortality.
Author Contributions
Conceptualization, Jasninder Dhaliwal, Manraj S Sekhon, Arush Rajotia, Ashujot K Dang, 5. Prabh Partap Singh, Hemamalini Sakthivel, Raheel Ahmed, Renuka Verma, Kamleshun Ramphul and Prabhdeep S Sethi; Methodology, Hemamalini Sakthivel; Validation, Kamleshun Ramphul; Formal analysis, Hemamalini Sakthivel, Renuka Verma and Kamleshun Ramphul; Investigation, Jasninder Dhaliwal, Manraj S Sekhon, Kamleshun Ramphul and Prabhdeep S Sethi; Data curation, Hemamalini Sakthivel, Renuka Verma and Kamleshun Ramphul; Writing – original draft, Jasninder Dhaliwal, Manraj S Sekhon, Arush Rajotia, Ashujot K Dang and Prabhdeep S Sethi; Writing – review & editing, Jasninder Dhaliwal, Arush Rajotia, 5. Prabh Partap Singh, Hemamalini Sakthivel, Raheel Ahmed, Renuka Verma, Kamleshun Ramphul and Prabhdeep S Sethi; Supervision, Kamleshun Ramphul and Prabhdeep S Sethi. All authors read and approved the final draft.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study, due to the de-identified nature of the database(waived by the data provider for all users).
Informed Consent Statement
Not applicable.
Data Availability Statement
Conflicts of Interest
The authors declare no conflict of interest.
References
- COVID-19 CORONAVIRUS PANDEMIC 2023. Available from: https://www.worldometers.info/coronavirus/.
- Ramphul K, Mejias SG. Coronavirus Disease: A Review of a New Threat to Public Health. Cureus. 2020;12(3):e7276. [CrossRef]
- Kumar N, Verma R, Lohana P, Lohana A, Ramphul K. Acute myocardial infarction in COVID-19 patients. A review of cases in the literature. Archives of medical sciences Atherosclerotic diseases. 2021;6:e169-e75. [CrossRef]
- Adla Jala SR, Sanikommu S, Chennapragada SS, Dhillon BK, Aggarwal S, Savani S, et al. Predictors of Immune Thrombocytopenic Purpura in COVID-19 Positive Elderly Admitted in the Pre-Vaccination Era of the Pandemic; An Analysis Via the 2020 National Inpatient Sample. Blood. 2023;142:1263. [CrossRef]
- Moras E, Gandhi KD, Bertasi R, Bertasi T, Dominguez AC. A-32 | The Effect of COVID-19 on Outcomes of Non-ST Elevation Myocardial Infarction (NSTEMI): Results from the National Inpatient Sample Database. Journal of the Society for Cardiovascular Angiography & Interventions. 2023;2(3). [CrossRef]
- Majeed H, Gangu K, Sagheer S, Garg I, Khan U, Shuja H, et al. COVID-19 and NSTEMI Outcomes among Hospitalized Patients in the United States and Racial Disparities in Mortality: Insight from National Inpatient Sample Database. Vaccines. 2022;10(12). [CrossRef]
- Nanavaty D, Sinha R, Kaul D, Sanghvi A, Kumar V, Vachhani B, et al. Impact of COVID-19 on Acute Myocardial Infarction: A National Inpatient Sample Analysis. Curr Probl Cardiol. 2024;49(1 Pt A):102030. [CrossRef]
- Shaka H, Ilelaboye AI, DeAngelo S, Gwira-Tamattey E, Vardar U. Increased national mortality in acute myocardial infarction hospitalization during the COVID-19 pandemic. Proceedings (Baylor University Medical Center). 2023;36(3):298-303. [CrossRef]
- HCUP National Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). 2020-2021. Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/nisoverview.jsp.
- TREND WEIGHTS FOR HCUP NIS DATA. https://hcup-us.ahrq.gov/db/nation/nis/trendwghts.jsp. 2023.
- Ahmed R, Shahbaz H, Ramphul K, Mactaggart S, Dulay MS, Okafor J, et al. Racial disparities among patients with cardiac sarcoidosis and arrhythmias in the United States: A propensity matched-analysis from the national inpatient sample database 2016-2020. Current Problems in Cardiology. 2024;49(4):102450. [CrossRef]
- Sawatari H, Chahal AA, Ahmed R, Collinss GB, Deshpande S, Khanji MY, et al. Impact of Cardiac Implantable Electronic Devices on Cost and Length of Stay in Patients With Surgical Aortic Valve Replacement and Transcutaneous Aortic Valve Implantation. The American journal of cardiology. 2023;192:69-78. [CrossRef]
- Data Organizations Participating in HCUP 2022. Available from: https://www.hcup-us.ahrq.gov/partners.jsp.
- Ramphul K, Kumar N, Verma R, Ramphul Y, Sombans S, Kumari K, et al. Acute myocardial infarction in patients with multiple sclerosis; An insight from 1785 cases in the United States. Multiple sclerosis and related disorders. 2022;68:104140. [CrossRef]
- Deshpande S, Swatari H, Ahmed R, Collins G, Khanji MY, Somers VK, et al. Predictors of morbidity and in-hospital mortality following procedure-related cardiac tamponade. Journal of arrhythmia. 2023;39(5):790-8. [CrossRef]
- Ramphul K, Lohana P, Verma R, Kumar N, Ramphul Y, Lohana A, et al. Cardiac arrhythmias and mortality risk among patients with obstructive sleep apnea following admission for acute myocardial infarction or acute ischemic stroke. Archives of medical sciences Atherosclerotic diseases. 2022;7:e109-e15. [CrossRef]
- Glasheen WP, Cordier T, Gumpina R, Haugh G, Davis J, Renda A. Charlson Comorbidity Index: ICD-9 Update and ICD-10 Translation. American health & drug benefits. 2019;12(4):188-97.
- Li P, Lu X, Teng C, Hadley M, Cai P, Dai Q, et al. The Association Between Hyperlipidemia and In-Hospital Outcomes in Takotsubo Cardiomyopathy. Diabetes, metabolic syndrome and obesity : targets and therapy. 2021;14:117-26. [CrossRef]
- Wu J, Fan Y, Zhao W, Li B, Pan N, Lou Z, et al. In-Hospital Outcomes of Acute Myocardial Infarction With Essential Thrombocythemia and Polycythemia Vera: Insights From the National Inpatient Sample. Journal of the American Heart Association. 2022;11(24):e027352. [CrossRef]
- Yang CW, Li S, Dong Y, Paliwal N, Wang Y. Epidemiology and the Impact of Acute Kidney Injury on Outcomes in Patients with Rhabdomyolysis. Journal of clinical medicine. 2021;10(9). [CrossRef]
- Taneja V, Stein DJ, Feuerstein JD. Impact of Cirrhosis on Outcomes in Inflammatory Bowel Disease Hospitalizations. 2022;56(8):718-23. [CrossRef]
- ELIXHAUSER COMORBIDITY SOFTWARE REFINED FOR ICD-10-CM. Available from: https://hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/comorbidity_icd10.jsp.
- COVID-19 CORONAVIRUS PANDEMIC. Available from: https://www.worldometers.info/coronavirus/.
- WORLD/COUNTRIES/UNITED STATES. Available from: https://www.worldometers.info/coronavirus/country/us/.
- Shrotri M, Navaratnam AMD, Nguyen V, Byrne T, Geismar C, Fragaszy E, et al. Spike-antibody waning after second dose of BNT162b2 or ChAdOx1. Lancet (London, England). 2021;398(10298):385-7. [CrossRef]
- COVID-19 restrictions. Available from: https://eu.usatoday.com/storytelling/coronavirus-reopening-america-map/.
- Yao H, Wang J, Liu W. Lockdown Policies, Economic Support, and Mental Health: Evidence From the COVID-19 Pandemic in United States. Frontiers in public health. 2022;10:857444. [CrossRef]
- Li Y, Undurraga EA, Zubizarreta JR. Effectiveness of Localized Lockdowns in the COVID-19 Pandemic. American journal of epidemiology. 2022;191(5):812-24. [CrossRef]
- Glass DH. European and US lockdowns and second waves during the COVID-19 pandemic. Mathematical biosciences. 2020;330:108472. [CrossRef]
- Sheikh A, McMenamin J, Taylor B, Robertson C. SARS-CoV-2 Delta VOC in Scotland: demographics, risk of hospital admission, and vaccine effectiveness. Lancet (London, England). 2021;397(10293):2461-2. [CrossRef]
- Choi JY, Smith DM. SARS-CoV-2 Variants of Concern. Yonsei medical journal. 2021;62(11):961-8. [CrossRef]
- Nyberg T, Twohig KA, Harris RJ, Seaman SR, Flannagan J, Allen H, et al. Risk of hospital admission for patients with SARS-CoV-2 variant B.1.1.7: cohort analysis. BMJ (Clinical research ed). 2021;373:n1412. [CrossRef]
- Gbolahan O, Bonatsos V, Mukherjee S, Raza A. Are patients' fears of catching COVID-19 during an emergency hospital admission with an acute urological problem justified?-A UK epicentre experience. Journal of public health (Oxford, England). 2023;45(2):488-90. [CrossRef]
- Einav S, Tankel J. The unseen pandemic: treatment delays and loss to follow-up due to fear of COVID. Journal of anesthesia, analgesia and critical care. 2022;2(1):5. [CrossRef]
- Provisional Mortality Data — United States, 2021. Available from: https://www.cdc.gov/mmwr/volumes/71/wr/mm7117e1.htm.
- Reece S, CarlLee S, Scott AJ, Willis DE, Rowland B, Larsen K, et al. Hesitant adopters: COVID-19 vaccine hesitancy among diverse vaccinated adults in the United States. Infectious medicine. 2023;2(2):89-95. [CrossRef]
- Ramphul K, Lohana P, Verma R, Sombans S. The impact of COVID-19 on cardiology departments. Archives of medical sciences Atherosclerotic diseases. 2021;6:e1-e2. [CrossRef]
- Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC infectious diseases. 2021;21(1):855. [CrossRef]
- Raisi-Estabragh Z, Mamas MA. Cardiovascular Health Care Implications of the COVID-19 pandemic. Heart failure clinics. 2023;19(2):265-72. [CrossRef]
- Kaplan EF, Strobel RJ, Young AM, Wisniewski AM, Ahmad RM, Mehaffey JH, et al. Cardiac Surgery Outcomes During the COVID-19 Pandemic Worsened Across All Socioeconomic Statuses. The Annals of thoracic surgery. 2023;115(6):1511-8. [CrossRef]
- Ramphul K, Aggarwal S, Verma R, Lohana P, Sombans S, Ramphul Y, et al. Acute myocardial infarction among teenagers in the United States between 2016 and 2020: a retrospective analysis from the National Inpatient Sample. Archives of medical sciences Atherosclerotic diseases. 2023;8:e177-e81. [CrossRef]
Table 1.
AMI cases among adult COVID-19 patients between April 2020 to December 2021 in the United States.
Table 1.
AMI cases among adult COVID-19 patients between April 2020 to December 2021 in the United States.
| Time |
AMI events among COVID-19 cases |
| Apr-20 |
3.65% |
| May-20 |
3.52% |
| Jun-20 |
3.01% |
| Jul-20 |
2.99% |
| Aug-20 |
3.31% |
| Sep-20 |
3.21% |
| Oct-20 |
3.18% |
| Nov-20 |
3.51% |
| Dec-20 |
3.66% |
| Jan-21 |
4.03% |
| Feb-21 |
3.67% |
| Mar-21 |
3.23% |
| Apr-21 |
2.93% |
| May-21 |
3.20% |
| Jun-21 |
2.67% |
| Jul-21 |
2.53% |
| Aug-21 |
3.11% |
| Sep-21 |
3.67% |
| Oct-21 |
3.97% |
| Nov-21 |
4.32% |
| Dec-21 |
4.35% |
| Overall |
3.55% |
Table 2.
Characteristics of COVID-19 patients with AMI in 2020 vs 2021 in the United States.
Table 2.
Characteristics of COVID-19 patients with AMI in 2020 vs 2021 in the United States.
| Variable |
AMI among COVID-19 patients in 2020 (n=34735)(%) |
AMI among COVID-19 patients in 2021 (n=55445)(%) |
p-value |
| Mean age (±SD) |
72.38(13.31) |
70.31(13.71) |
<0.01 |
| Weekend admission |
26.8 |
26.7 |
0.766 |
| Female |
39.3 |
40.5 |
<0.01 |
Primary payer
Medicare
Medicaid
Private |
69.9
8.7
15.5 |
66.1
9.4
17.8
|
<0.01 |
Race
White
Black
Hispanic |
55.6
17.8
18.0
|
65.0
16.1
12.4 |
<0.01 |
Median household income
0-25th percentile
26th to 50th percentile (median)
51st to 75th percentile
76th to 100th percentile |
36.8
29.6
20.5
13.1 |
36.8
27.4
21.7
14.1
|
<0.01 |
| Hospital characteristics |
Hospital bed size
Small
Medium
Large |
23.5
29.9
46.6 |
24.7
30.7
44.6 |
<0.01 |
Location/Teaching status
Rural
Urban non-teaching
Urban teaching |
10.9
18.0
71.2 |
13.1
18.5
68.3 |
<0.01 |
Region of hospital
Northeast
Midwest
South
West |
18.7
2.1
38.7
16.5 |
16.6
22.9
42.8
17.7 |
<0.01 |
| Comorbidities |
| Sarcoidosis |
0.3 |
0.3 |
0.791 |
| SLE |
0.6 |
0.5 |
0.495 |
| Rheumatoid arthritis |
2.1 |
2.2 |
0.290 |
| Hyperthyroidism |
0.6 |
0.6 |
0.615 |
| Hypothyroidism |
14.1 |
13.2 |
<0.01 |
| Hypertension |
27.9 |
28.1 |
0.543 |
| Dyslipidemia |
53.2 |
49.4 |
<0.01 |
| Smoking |
28.1 |
30.1 |
<0.01 |
| Diabetes |
49.0 |
45.9 |
<0.01 |
| CKD |
40.5 |
39.2 |
<0.01 |
| Prior CABG |
8.4 |
7.6 |
<0.01 |
| Prior PCI |
10.7 |
9.2 |
<0.01 |
| Family history of CAD |
4.5 |
4.0 |
<0.01 |
| Peripheral vascular disease |
4.4 |
4.3 |
0.604 |
| Prior stroke |
8.3 |
7.6 |
<0.01 |
| Cirrhosis |
5.2 |
5.8 |
<0.01 |
| Alcohol abuse |
1.8 |
2.4 |
<0.01 |
| Prior MI |
9.4 |
8.8 |
<0.01 |
| Obesity |
20.4 |
25.5 |
<0.01 |
| Drug abuse |
2.0 |
2.8 |
<0.01 |
| COPD |
20.7 |
21.9 |
<0.01 |
| Mean CCI Score |
5.04(3.35) |
4.91(3.36) |
<0.01 |
Table 3.
Mortality rates among AMI events in COVID-19 patients between April 2020 to December 2021 in the United States.
Table 3.
Mortality rates among AMI events in COVID-19 patients between April 2020 to December 2021 in the United States.
| Time |
Mortality of AMI patients with COVID-19 |
| Apr-20 |
43.20% |
| May-20 |
31.90% |
| Jun-20 |
33.20% |
| Jul-20 |
31.60% |
| Aug-20 |
31.20% |
| Sep-20 |
32.50% |
| Oct-20 |
31.20% |
| Nov-20 |
28.50% |
| Dec-20 |
31.90% |
| Jan-21 |
32.50% |
| Feb-21 |
26.40% |
| Mar-21 |
27.20% |
| Apr-21 |
26.40% |
| May-21 |
30.90% |
| Jun-21 |
23.10% |
| Jul-21 |
34.40% |
| Aug-21 |
35.60% |
| Sep-21 |
35.30% |
| Oct-21 |
33.90% |
| Nov-21 |
34.50% |
| Dec-21 |
34.20% |
| Overall |
32.70% |
Table 4.
Arrhythmias, procedures, and complications among COVID-19 patients with AMI in 2021 vs. 2020(reference).
Table 4.
Arrhythmias, procedures, and complications among COVID-19 patients with AMI in 2021 vs. 2020(reference).
| Cardiac arrhythmias |
| Variable |
p-value |
aOR |
Lower 95% CI |
Upper 95% CI |
| Atrial fibrillation |
.424 |
1.013 |
.982 |
1.045 |
| Supraventricular tachycardia |
.527 |
1.023 |
.954 |
1.096 |
| Ventricular tachycardia |
<.001 |
1.126 |
1.062 |
1.194 |
| Complications |
| Variable |
p-value |
aOR |
Lower 95% CI |
Upper 95% CI |
| PCI |
<.001 |
1.627 |
1.454 |
1.822 |
| Cardiogenic shock |
.841 |
1.008 |
.931 |
1.092 |
| IABP |
.565 |
.902 |
.636 |
1.281 |
| AKI |
<.001 |
1.078 |
1.047 |
1.110 |
| AIS |
<.001 |
1.215 |
1.113 |
1.328 |
| Cardiac arrest |
<.001 |
1.106 |
1.050 |
1.166 |
| Invasive mechanical ventilation |
<.001 |
1.133 |
1.096 |
1.172 |
| Died |
.043 |
1.032 |
1.001 |
1.064 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).