Submitted:
04 March 2024
Posted:
05 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
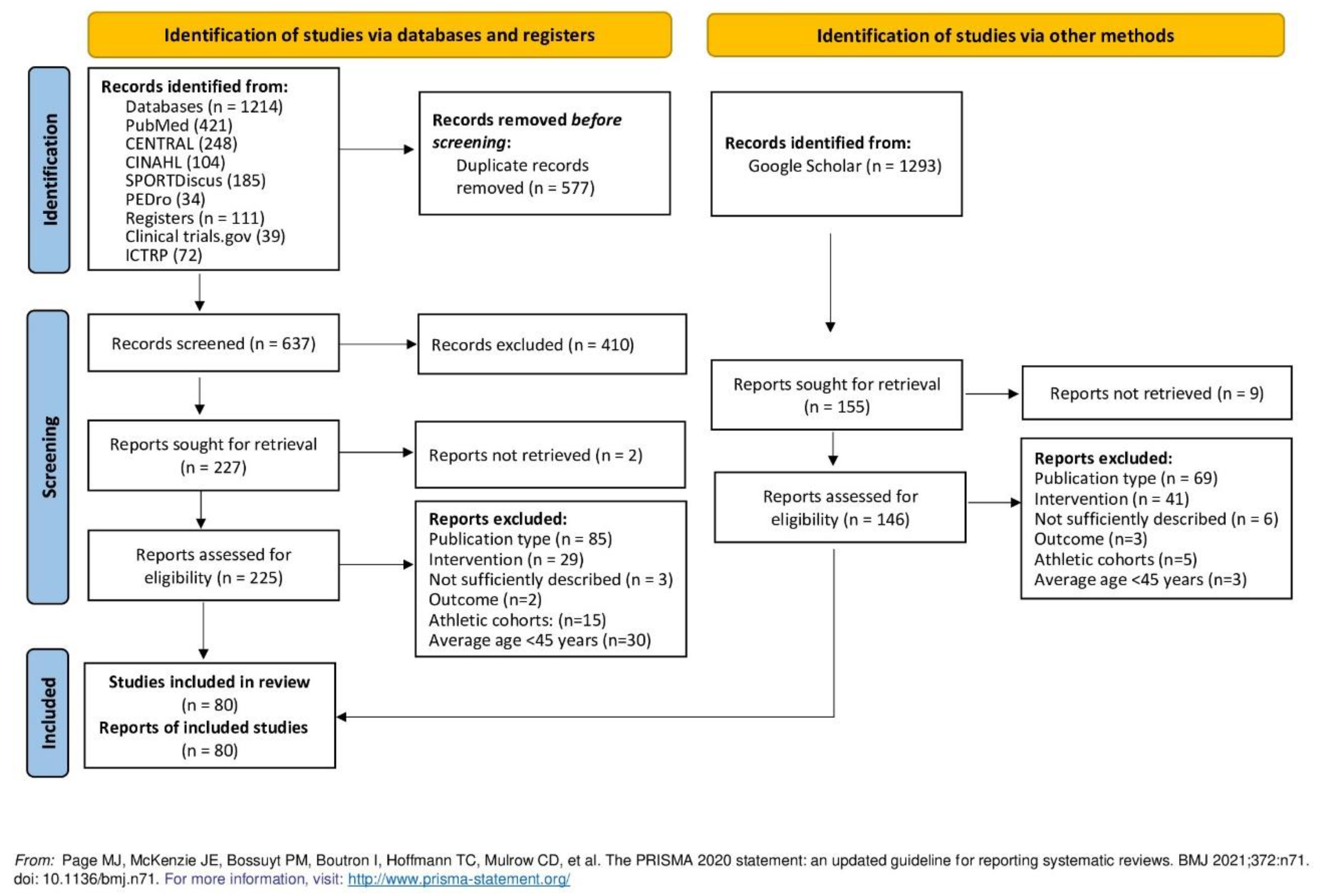
2. Methods
Eligibility criteria
Study design
Population
Comparators
Intervention
Outcomes
Selection process
Data management
Data items
Quality assessment
Data synthesis
3. Results
Publication, study and participant characteristics
Intervention characteristics
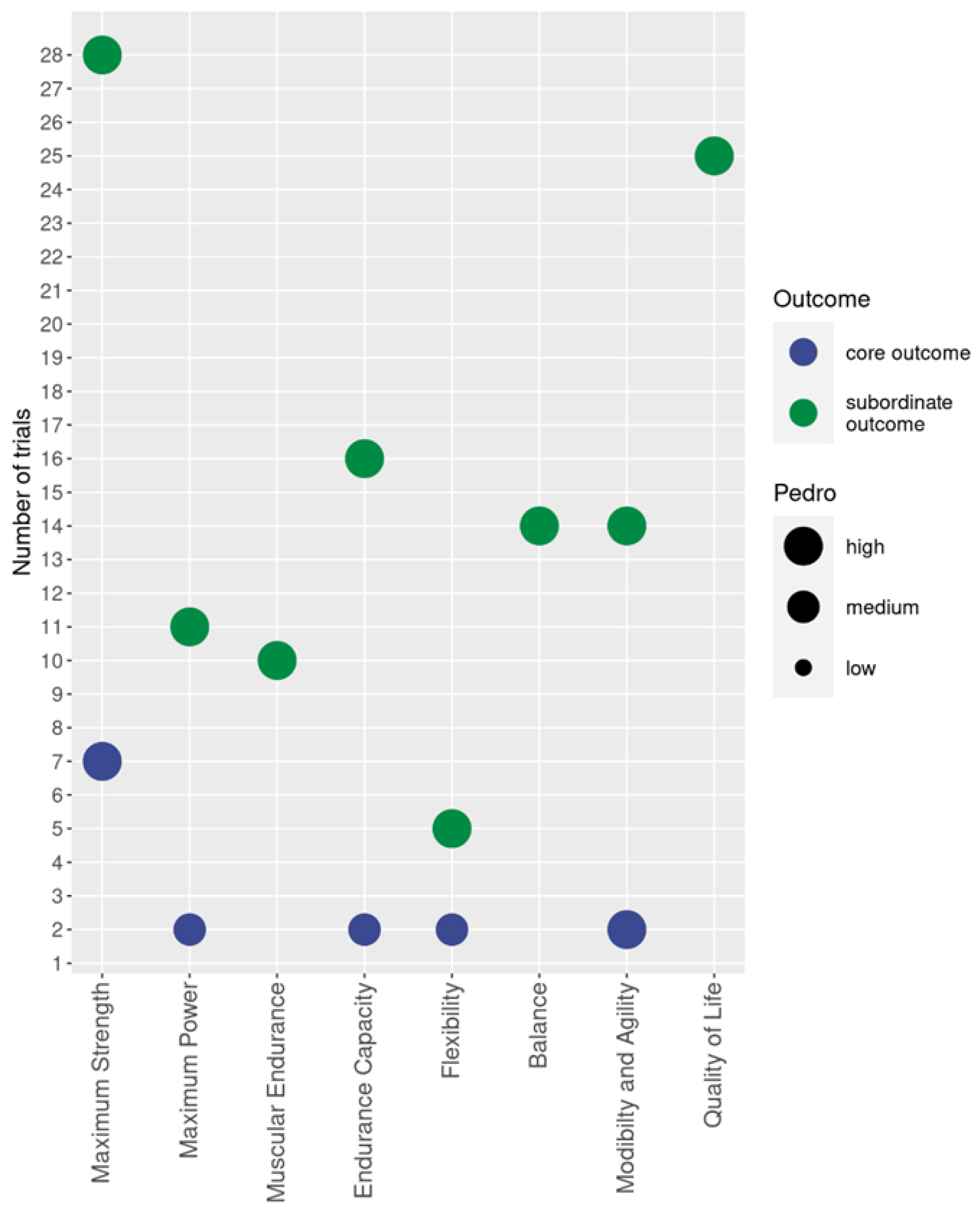
Outcomes: Physical function and fitness domain
Maximum strength
Power
Strength endurance
Endurance
Flexibility
Balance
Mobility, Agility
Quality of life domain
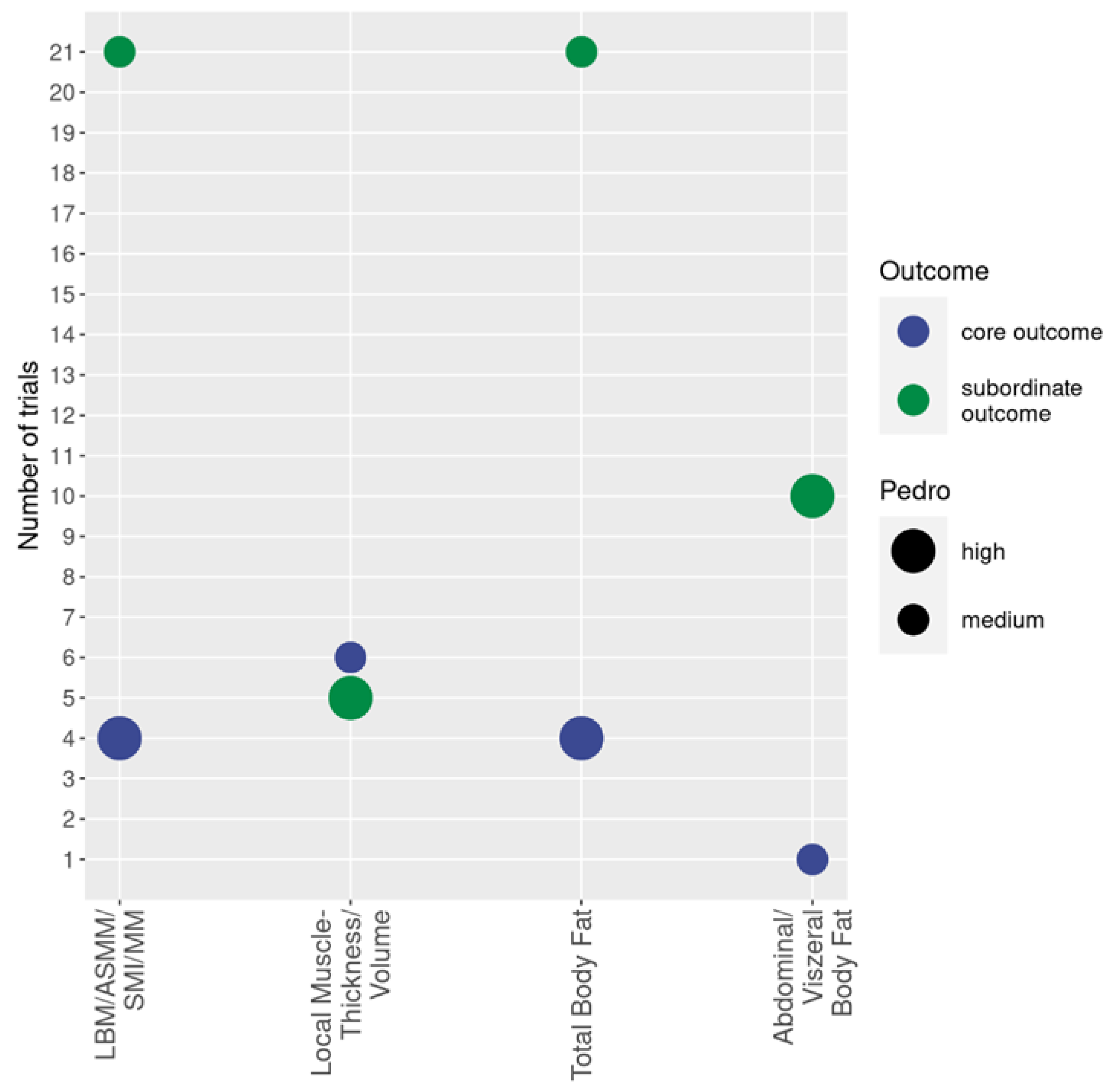
Body composition and anthropometry
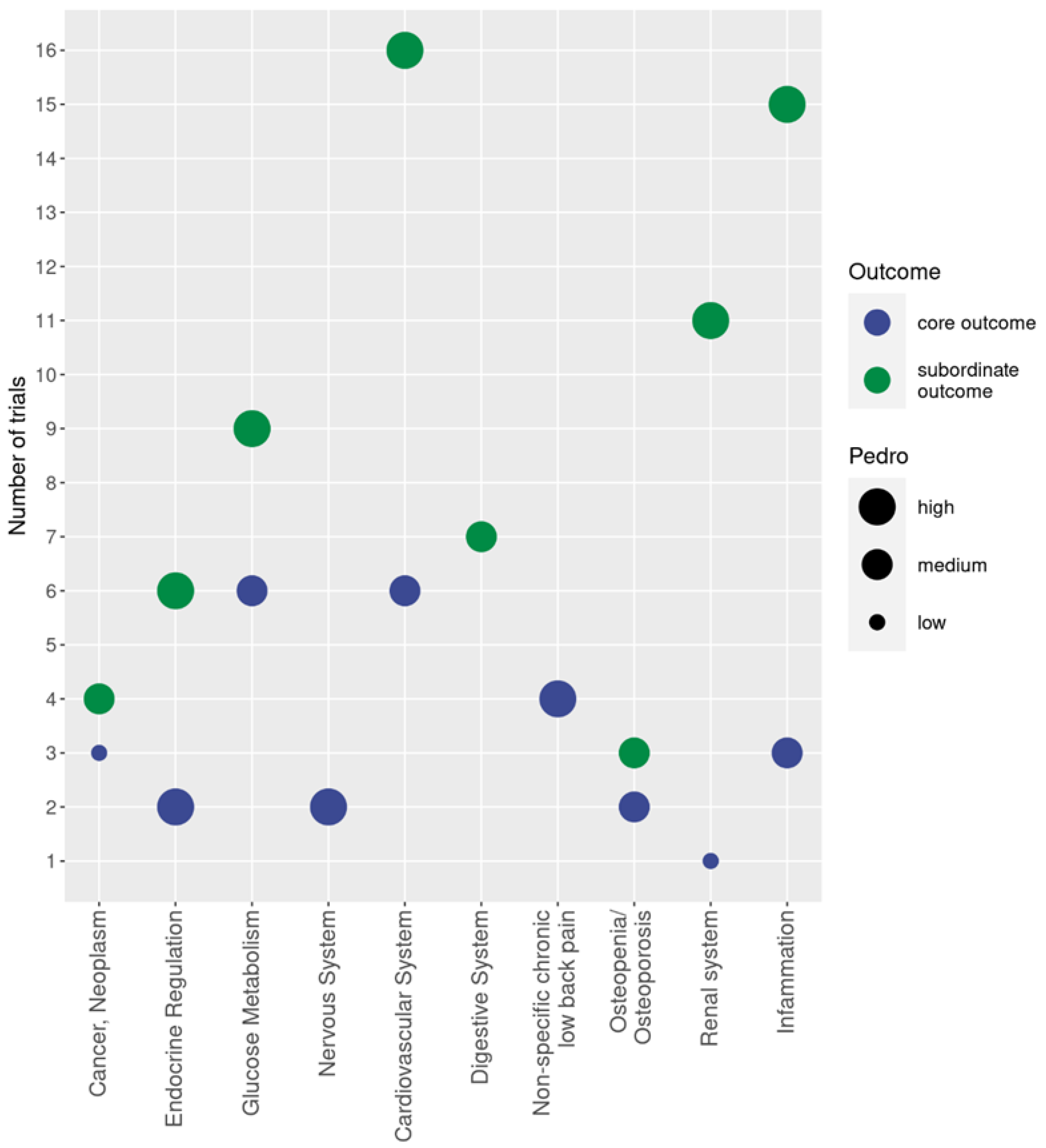
Neoplasm
Endocrine regulation
Diabetes mellitus and the metabolic syndrome
Diseases of the nervous system
Cardiovascular diseases
Diseases of the respiratory system
Diseases of the digestive system
Diseases of the musculoskeletal system
Diseases of the genitourinary system
Inflammation
Adverse effects
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data availability
Acknowledgments
Conflicts of Interest
References
- Kemmler, W.; Kleinoder, H.; Fröhlich, M. Editorial: Whole-Body Electromyostimulation: A Training Technology to Improve Health and Performance in Humans? Frontiers in physiology. 2020, 11, 523. [Google Scholar] [CrossRef]
- Kemmler, W.; Kleinoder, H.; Fröhlich, M. Editorial: Whole-body electromyostimulation: A training technology to improve health and performance in humans? volume II. Frontiers in physiology. 2022, 13, 972011. [Google Scholar] [CrossRef]
- de Oliveira, T.M.D.; Felicio, D.C.; Filho, J.E.; et al. Effects of whole-body electromyostimulation on function, muscle mass, strength, social participation, and falls-efficacy in older people: A randomized trial protocol. PLoS One. 2021, 16, e0245809. [Google Scholar] [CrossRef]
- Eifler, C. Marktsituation, Trends und Entwicklungen. In Ganzkörper-EMS, Kemmler, W.; Fröhlich, M.; Eifler, C. Eds.; Vol. Essentials Springer Spektrum, 2022.
- Beier, M.; Schoene, D.; Kohl, M.; von Stengel, S.; Uder, M.; Kemmler, W. Non-athletic cohorts enrolled in longitudinal whole-body electromyostimulation trials - An evidence map. Sensors (Basel). 2024, 24, 972. [Google Scholar] [CrossRef]
- Miake-Lye, I.M.; Hempel, S.; Shanman, R.; Shekelle, P.G. What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Syst Rev. 2016, 5, 28. [Google Scholar] [CrossRef]
- Thiese, M.S. Observational and interventional study design types; an overview. Biochem Med (Zagreb). 2014, 24, 199–210. [Google Scholar] [CrossRef]
- Bramer, W.M.; Giustini, D.; de Jonge, G.B.; Holland, L.; Bekhuis, T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. 2016, 104, 240–243. [Google Scholar] [CrossRef]
- Mages, M.; Shojaa, M.; Kohl, M.; et al. Exercise Effects on Bone Mineral Density in Men. Nutrients. 2021, 13, 4244. [Google Scholar] [CrossRef]
- Mohebbi, R.; Shojaa, M.; Kohl, M.; et al. Exercise training and bone mineral density in postmenopausal women: An updated systematic review and meta-analysis of intervention studies with emphasis on potential moderators. Osteo Int. 2023, 4, 1145–1178. [Google Scholar] [CrossRef]
- ICD-10-GM. International Statistical Classification of Diseases and Related Health Problems, 10. Revision, German Modification. In https://www.bfarm.de/EN/Code-systems/Classifications/ICD/ICD-10-GM/_node.html, 2022.
- Teschler, M.; Heimer, M.; Schmitz, B.; Kemmler, W.; Mooren, F.C. Four weeks of electromyostimulation improves muscle function and strength in sarcopenic patients: a three-arm parallel randomized trial. J Cachexia Sarcopenia Muscle. 2021, 12, 843–854. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Physical therapy. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Ribeiro de Avila, V.; Bento, T.; Gomes, W.; Leitao, J.; Fortuna de Sousa, N. Functional Outcomes and Quality of Life After Ankle Fracture Surgically Treated: A Systematic Review. J Sport Rehabil. 2018, 27, 274–283. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J. E.; Bossuyt, P.M.; et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021, 372, 71. [Google Scholar] [CrossRef]
- Amaro-Gahete, F.J.; De-la, O.A.; Jurado-Fasoli, L.; et al. Changes in Physical Fitness After 12 Weeks of Structured Concurrent Exercise Training, High Intensity Interval Training, or Whole-Body Electromyostimulation Training in Sedentary Middle-Aged Adults: A Randomized Controlled Trial. Frontiers in physiology. 2019, 10, 451. [Google Scholar] [CrossRef]
- Amaro-Gahete, F.J.; De-la, O.A.; Jurado-Fasoli, L.; et al. Exercise training increases the S-Klotho plasma levels in sedentary middle-aged adults: A randomised controlled trial. The FIT-AGEING study. J Sports Sci. 2019, 37, 2175–2183. [Google Scholar] [CrossRef]
- Amaro-Gahete, F.J.; De-la, O.A.; Jurado-Fasoli, L.; Martinez-Tellez, B.; Ruiz, J.R.; Castillo, M.J. Exercise Training as a Treatment for Cardiometabolic Risk in Sedentary Adults: Are Physical Activity Guidelines the Best Way to Improve Cardiometabolic Health? The FIT-AGEING Randomized Controlled Trial. J Clin Med. 2019, 8. [Google Scholar] [CrossRef]
- Amaro-Gahete, F.J.; De-la, O.A.; Jurado-Fasoli, L.; Ruiz, J.R.; Castillo, M.J.; Gutierrez, A. Effects of different exercise training programs on body composition: A randomized control trial. Scand J Med Sci Sports. 2019, 29, 968–979. [Google Scholar] [CrossRef]
- Amaro-Gahete, F.J.; De-la, O.A.; Jurado-Fasoli, L.; Sanchez-Delgado, G.; Ruiz, J.R.; Castillo, M.J. Metabolic rate in sedentary adults, following different exercise training interventions: The FIT-AGEING randomized controlled trial. Clin Nutr. 2020, 39, 3230–3240. [Google Scholar] [CrossRef]
- Bellia, A.; Ruscello, B.; Bolognino, R.; et al. Whole-body Electromyostimulation plus Caloric Restriction in Metabolic Syndrome. Int J Sports Med. 2020, 41, 751–758. [Google Scholar] [CrossRef]
- Bloeckl, J.; Raps, S.; Weineck, M.; et al. Feasibility and Safety of Whole-Body Electromyostimulation in Frail Older People-A Pilot Trial. Frontiers in physiology. 2022, 13, 856681. [Google Scholar] [CrossRef]
- Boutry-Regard, C.; Vinyes-Pares, G.; Breuille, D.; Moritani, T. Supplementation with Whey Protein, Omega-3 Fatty Acids and Polyphenols Combined with Electrical Muscle Stimulation Increases Muscle Strength in Elderly Adults with Limited Mobility: A Randomized Controlled Trial. Nutrients. 2020, 12, 1866. [Google Scholar] [CrossRef]
- De-la, O.A.; Jurado-Fasoli, L.; Castillo, M.J.; Gutierrez, A.; Amaro-Gahete, F.J. Effect of Exercise Training on 1,25(OH)(2)D Levels: The FIT-AGEING Randomized Controlled Trial. Sports Health. 2022, 14, 518–526. [Google Scholar] [CrossRef]
- di Cagno, A.; Buonsenso, A.; Centorbi, M.; et al. Whole body-electromyostimulation effects on serum biomarkers, physical performances and fatigue in Parkinson’s patients: A randomized controlled trial. Front Aging Neurosci. 2023, 15, 1086487. [Google Scholar] [CrossRef]
- Dote-Montero, M.; De-la, O.A.; Jurado-Fasoli, L.; Ruiz, J.R.; Castillo, M.J.; Amaro-Gahete, F.J. The effects of three types of exercise training on steroid hormones in physically inactive middle-aged adults: a randomized controlled trial. Eur J Appl Physiol. 2021, 121, 2193–2206. [Google Scholar] [CrossRef]
- Evangelista, A.L.; Alonso, A.C.; Ritti-Dias, R.M.; et al. Effects of Whole Body Electrostimulation Associated With Body Weight Training on Functional Capacity and Body Composition in Inactive Older People. Frontiers in physiology. 2021, 12, 638936. [Google Scholar] [CrossRef]
- Fritzsche, D.; Fruend, A.; Schenk, S.; et al. Elektromyostimulation (EMS) bei kardiologischen Patienten. Wird das EMS-Training bedeutsam für die Sekundärprävention? Herz. 2010, 35, 34–40. [Google Scholar] [CrossRef]
- Hamada, R.; Sato, S.; Miyasaka, J.; et al. Belt Electrode-Skeletal Muscle Electrical Stimulation During Early Hematopoietic Post-Transplantation To Prevent Skeletal Muscle Atrophy and Weakness. Transplant Cell Ther. 2023, 29, 51 e51–51 e57. [Google Scholar] [CrossRef]
- Homma, M.; Miura, M.; Hirayama, Y.; et al. Belt Electrode-Skeletal Muscle Electrical Stimulation in Older Hemodialysis Patients with Reduced Physical Activity: A Randomized Controlled Pilot Study. J Clin Med. 2022, 11, 622–630. [Google Scholar] [CrossRef]
- Houdijk, A.P.J.; Bos, N.; Verduin, W.M.; Hijdendaal, M.M.; Zwartkruis, M.A.L. Visceral fat loss by whole-body electromyostimulation is attenuated in male and absent in female older Non-Insulin-Dependent diabetes patients. Endocrinol Diabetes Metab. 2022, 5, e377. [Google Scholar] [CrossRef]
- Imaoka, S.; Kudou, G.; Tsugiyama, K.; et al. Efficacy of Belt Electrode Skeletal Muscle Electrical Stimulation in the Postoperative Rest Period in Patients with Diabetes who Have Undergone minor Amputations: A Randomized Controlled Trial. Int J Low Extrem Wounds. 2022, 15347346221077491. [Google Scholar] [CrossRef]
- Jurado-Fasoli, L.; Amaro-Gahete, F.J.; De-la, O.A.; Castillo, M.J. Impact of different exercise training modalities on energy and nutrient intake and food consumption in sedentary middle-aged adults: a randomised controlled trial. J Hum Nutr Diet. 2020, 33, 86–97. [Google Scholar] [CrossRef]
- Jurado-Fasoli, L.; De-la, O.A.; Molina-Hidalgo, C.; Migueles, J.H.; Castillo, M.J.; Amaro-Gahete, F.J. Exercise training improves sleep quality: A randomized controlled trial. Eur J Clin Invest. 2020, 50, e13202. [Google Scholar] [CrossRef]
- Jurado-Fasoli, L.; Yang, W.; Kohler, I.; et al. Effect of Different Exercise Training Modalities on Fasting Levels of Oxylipins and Endocannabinoids in Middle-Aged Sedentary Adults: A Randomized Controlled Trial. Int J Sport Nutr Exerc Metab. 2022, 32, 275–284. [Google Scholar] [CrossRef]
- Kataoka, H.; Nakashima, S.; Aoki, H.; et al. Electrical stimulation in addition to passive exercise has a small effect on spasticity and range of motion in bedridden elderly patients: A pilot randomized crossover study. Health. 2019, 11, 1072–1086. [Google Scholar] [CrossRef]
- Kemmler, W.; Schliffka, R.; Mayhew, J.L.; von Stengel, S. Effects of Whole-Body-Electromyostimulation on Resting Metabolic Rate, Anthropometric and Neuromuscular Parameters in the Elderly. The Training and ElectroStimulation Trial (TEST). J Strength Cond Res. 2010, 24, 1880–1886. [Google Scholar] [CrossRef]
- Kemmler, W.; Teschler, M.; Von Stengel, S. Effekt von Ganzkörper-Elektromyostimulation – „A series of studies“. Osteologie 2015, 23, 20–29. [Google Scholar]
- Kemmler, W.; Birlauf, A.; von Stengel, S. Einfluss von Ganzkörper-Elektromyostimulation auf das Metabolische Syndrom bei älteren Männern mit metabolischem Syndrom. Dtsch Z Sportmed. 2010, 61, 117–123. [Google Scholar]
- Kemmler, W.; von Stengel, S. Alternative Exercise Technologies to Fight against Sarcopenia at Old Age: A Series of Studies and Review. J Aging Res. 2012, 2012, 109013. [Google Scholar] [CrossRef]
- Kemmler, W.; Bebenek, M.; Engelke, K.; von Stengel, S. Impact of whole-body electromyostimulation on body composition in elderly women at risk for sarcopenia: the Training and ElectroStimulation Trial (TEST-III). Age. 2014, 36, 395–406. [Google Scholar] [CrossRef]
- Kemmler, W.; Engelke, K.; Von Stengel, S. Ganzkörper-Elektromyostimulation zur Prävention der Sarkopenie bei einem älteren Risikokollektiv. Die TEST-III Studie. Dtsch Z Sportmed. 2012, 63, 16–23. [Google Scholar]
- Kemmler, W.; von Stengel, S. Whole-body electromyostimulation as a means to impact muscle mass and abdominal body fat in lean, sedentary, older female adults: subanalysis of the TEST-III trial. Clinical interventions in aging. 2013, 8, 1353–1364. [Google Scholar] [CrossRef]
- Kemmler, W.; Teschler, M.; Weissenfels, A.; et al. Whole-body electromyostimulation to fight sarcopenic obesity in community-dwelling older women at risk. Resultsof the randomized controlled FORMOsA-sarcopenic obesity study. Osteoporos Int. 2016, 27, 3261–3270. [Google Scholar] [CrossRef]
- Kemmler, W.; von Stengel, S.; Teschler, M.; et al. Ganzkörper-Elektromyostimulation und Sarcopenic Obesity. Ergebnisse der randomisierten kontrollierten FORMOsASarcopenic Obesity Studie. Osteologie. 2016, 25, 204–211. [Google Scholar]
- Kemmler, W.; Grimm, A.; Bebenek, M.; Kohl, M.; von Stengel, S. Effects of Combined Whole-Body Electromyostimulation and Protein Supplementation on Local and Overall Muscle/Fat Distribution in Older Men with Sarcopenic Obesity: The Randomized Controlled Franconia Sarcopenic Obesity (FranSO) Study. Calcified tissue international. 2018, 103, 266–277. [Google Scholar] [CrossRef]
- Kemmler, W.; Kohl, M.; Freiberger, E.; Sieber, C.; von Stengel, S. Effect of whole-body electromyostimulation and / or protein supplementation on obesity and cardiometabolic risk in older men with sarcopenic obesity: the randomized controlled FranSO trial. BMC geriatrics. 2018, 18, 70. [Google Scholar] [CrossRef]
- Kemmler, W.; von Stengel, S.; Kohl, M.; et al. Safety of a Combined WB-EMS and High-Protein Diet Intervention in Sarcopenic Obese Elderly Men. Clinical interventions in aging. 2020, 15, 953–967. [Google Scholar] [CrossRef]
- Kemmler, W.; Weissenfels, A.; Teschler, M.; et al. Whole-body Electromyostimulation and protein supplementation favorably affect Sarcopenic Obesity in community-dwelling older men at risk. The Randomized Controlled FranSO Study. Clinical interventions in aging. 2017, 12, 1503–1513. [Google Scholar] [CrossRef]
- Kim, J.; Jee, Y. EMS-effect of Exercises with Music on Fatness and Biomarkers of Obese Elderly Women. Medicina (Kaunas). 2020, 56, 156. [Google Scholar] [CrossRef]
- Konrad, K.L.; Baeyens, J.-P.; Birkenmaier, C.; et al. The effects of whole-body electromyostimulation (WB-EMS) in comparison to a multimodal treatment concept in patients with non-specific chronic back pain—A prospective clinical intervention study. PloS one. 2020, 15, e0236780. [Google Scholar] [CrossRef]
- Lukashevich, U. А. , Ponomarev, V.V.; Tarasevich, M.I.; Zhivolupov, S.А.. Functional reciprocal neuromuscular electric stimulation in adaptive kinesitherapy in post-stress patients. Science & Healthcare. 2020, 22, 80–88. [Google Scholar]
- Matsumoto, J.M.; Terabe, S.Y.; Sakaki, R.H. Experience of Belt Electrode Skeletal Muscle Electrical Stimulation Method for Severe Lower Limb Ischemic Patients: A Case Report. Physical Therapy in Clinical Practice, Research & Education. 2020, 27, 81–85. [Google Scholar]
- Matsuo, K.; Yoneki, K.; Tatsuki, H.; et al. Effect of Electrical Muscle Stimulation on the Reduction of Muscle Volume Loss in Acute Heart Failure Patients. Int Heart J. 2022, 63, 1141–1149. [Google Scholar] [CrossRef]
- Micke, F.; Weissenfels, A.; Wirtz, N.; et al. Similar Pain Intensity Reductions and Trunk Strength Improvements following Whole-Body Electromyostimulation vs. Whole-Body Vibration vs. Conventional Back-Strengthening Training in Chronic Non-specific Low Back Pain Patients: A 3-armed randomized controlled trial. Frontiers in physiology. 2021, 13, 664991. [Google Scholar]
- Mori, K.; Tamura, Y.; Deguchi, K.; Miura, Y.; Yura, Y.; KoizumI, T. Effect of belt electrode skeletal muscle electrical stimulation during hemodialysis on the endothelial function in hemodialysis patients [透析患者に対する透析中のベルト電極式骨格筋電気刺激が血管内皮機能に及ぼす影響]. Japanese Journal of Electrophysical Agents. 2020, 27, 78–81. [Google Scholar]
- Müllerová, M.; Vaculíková, P.; Potúčková, A.; Struhár, I.; Balousová, D.N. Impact of Whole-Body Electromyostimulation and Resistance Training Programme on Strength Parameters and Body Composition in Group of Elderly Women at Risk of Sarcopenia. Studia sportiva. 2022, 16, 292–304. [Google Scholar] [CrossRef]
- Nakamura, K.; Kihata, A.; Naraba, H.; et al. Efficacy of belt electrode skeletal muscle electrical stimulation on reducing the rate of muscle volume loss in critically ill patients: A randomized controlled trial. J Rehabil Med. 2019, 51, 705–711. [Google Scholar] [CrossRef]
- Nakamura, K.; Nakano, H.; Naraba, H.; et al. High protein versus medium protein delivery under equal total energy delivery in critical care: A randomized controlled trial. Clin Nutr. 2021, 40, 796–803. [Google Scholar] [CrossRef]
- Navarro-Lomas, G.; Dote-Montero, M.; Alcantara, J.M.A.; Plaza-Florido, A.; Castillo, M.J.; Amaro-Gahete, F.J. Different exercise training modalities similarly improve heart rate variability in sedentary middle-aged adults: the FIT-AGEING randomized controlled trial. Eur J Appl Physiol. 2022, 122, 1863–1874. [Google Scholar] [CrossRef]
- Nejad, M.D.; Nikbakht, M.; Ghanbarzadeh, M.; Ranjbar, R. Effect of Concurrent Training Order With Electromyostimulation on Physical Performance in Young Elderly Women. Archives of Rehabilitation. 2021, 21, 508–525. [Google Scholar] [CrossRef]
- Noguchi, Y.; Hirano, H.; Mizutani, C.; Ito, T.; Kawamura, N. Die Wirkung der elektrischen Stimulation der Skelettmuskulatur mit Gürtelelektroden während der Hämodialyse auf die körperliche Funktion von Hämodialysepatienten [透析中ベルト電極式骨格筋電気刺激法が透析患者の身体機能に与える影響]. Journal of Dialysis Society. 2018, 51, 87–91. [Google Scholar]
- Nonoyama, T.; Shigemi, H.; Kubota, M.; Matsumine, A.; Shigemi, K.; Ishizuka, T. Neuromuscular electrical stimulation in the intensive care unit prevents muscle atrophy in critically ill older patients: A retrospective cohort study. Medicine (Baltimore). 2022, 101, e29451. [Google Scholar] [CrossRef]
- Ochiai, K.; Tamura, Y.; Ehara, K.; Shimizu, R.; Matushita, Y.; Yasu, T. Bridging Therapy Using B-SES for Peripheral Arterial Disease Patients with Severe Lower Limb Ischemia. Journal of Physical Therapy Science. 2018, 33, 545–548. [Google Scholar] [CrossRef]
- Pano-Rodriguez, A.; Beltran-Garrido, J.V.; Hernandez-Gonzalez, V.; Nasarre-Nacenta, N.; Reverter-Masia, J. Impact of Whole Body Electromyostimulation on Velocity, Power and Body Composition in Postmenopausal Women: A Randomized Controlled Trial. Int J Environ Res Public Health. 2020, 17, 4982. [Google Scholar] [CrossRef] [PubMed]
- Pano-Rodriguez, A.; Beltran-Garrido, J.V.; Hernandez-Gonzalez, V.; Reverter-Masia, J. Effects of Whole-Body Electromyostimulation on Physical Fitness in Postmenopausal Women: A Randomized Controlled Trial. Sensors (Basel). 2020, 20. [Google Scholar] [CrossRef]
- Park, S.; Min, S.; Park, S.H.; Yoo, J.; Jee, Y.S. Influence of Isometric Exercise Combined With Electromyostimulation on Inflammatory Cytokine Levels, Muscle Strength, and Knee Joint Function in Elderly Women With Early Knee Osteoarthritis. Frontiers in physiology. 2021, 12, 688260. [Google Scholar] [CrossRef]
- Park, S.; Park, J.; Ham, J.A.; Jee, Y. Effects of aerobic dance with electrical stimulant on body composition and radiological circumference of obese elderly women. Gazzetta Medica Italiana Archivio per le Scienze Mediche. 2021, 180, 000–000. [Google Scholar] [CrossRef]
- Park, W.; Lee, J.; Hong, K.; et al. Protein-Added Healthy Lunch-Boxes Combined with Exercise for Improving Physical Fitness and Vascular Function in Pre-Frail Older Women: A Community-Based Randomized Controlled Trial. Clinical interventions in aging. 2023, 18, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Reljic, D.; Dieterich, W.; Herrmann, H.J.; Neurath, M.F.; Zopf, Y. “HIIT the Inflammation”: Comparative Effects of Low-Volume Interval Training and Resistance Exercises on Inflammatory Indices in Obese Metabolic Syndrome Patients Undergoing Caloric Restriction. Nutrients. 2022, 14. [Google Scholar] [CrossRef]
- Reljic, D.; Herrmann, H.J.; Neurath, M.F.; Zopf, Y. Iron Beats Electricity: Resistance Training but Not Whole-Body Electromyostimulation Improves Cardiometabolic Health in Obese Metabolic Syndrome Patients during Caloric Restriction-A Randomized-Controlled Study. Nutrients. 2021, 13, 1640. [Google Scholar] [CrossRef]
- Reljic, D.; Konturek, P.C.; Herrmann, H.J.; Neurath, M.F.; Zopf, Y. Effects of whole-body electromyostimulation exercise and caloric restriction on cardiometabolic risk profile and muscle strength in obese women with the metabolic syndrome: a pilot study. J Physiol Pharmacol. 2020, 71. [Google Scholar]
- Reverter-Masia, J.; Pano-Rodriguez, A.; Beltran-Garrido, J.V.; Lecube, A.; Sánchez, E.; Hernández-González, V. Effect of a Training Program on Hepatic Fat Content and Cardiometabolic Risk in Postmenopausal Women: The Randomized Controlled Trial. Applied Sciences. 2021, 11. [Google Scholar] [CrossRef]
- Richter, H. Effect of electromyostimulation training and high-protein diet on gastrointestinal tumor patients in palliative and curative treatment settings. [Einfluss von Elektromyostimulationstraining und proteinreicher Ernährung auf gastrointestinale Tumorpatienten in palliativer und kurativer Behandlungssituation]. Friedrich-Alexander-University Erlangen-Nürnberg, Germany, Erlangen, 2019.
- Sánchez-Infante, J.; Bravo-Sáncheza, A.; Abiánb, P.; Estebana, P.; Jimeneza, J.; Abián-Vicén, J. The influence of whole-body electromyostimulation training in middle-aged women. Isokinet Exerc Sci 2020, 1, 1–9. [Google Scholar] [CrossRef]
- Schink, K.; Gassner, H.; Reljic, D.; et al. Assessment of gait parameters and physical function in patients with advanced cancer participating in a 12-week exercise and nutrition programme: A controlled clinical trial. Eur J Cancer Care (Engl). 2020, 29, e13199. [Google Scholar] [CrossRef] [PubMed]
- Schink, K.; Herrmann, H.J.; Schwappacher, R.; et al. Effects of whole-body electromyostimulation combined with individualized nutritional support on body composition in patients with advanced cancer: a controlled pilot trial. BMC cancer. 2018, 18, 886. [Google Scholar] [CrossRef] [PubMed]
- Schink, K.; Reljic, D.; Herrmann, H.J.; et al. Whole-Body Electromyostimulation Combined With Individualized Nutritional Support Improves Body Composition in Patients With Hematological Malignancies - A Pilot Study. Frontiers in physiology. 2018, 9, 1808. [Google Scholar] [CrossRef] [PubMed]
- Schwappacher, R.; Dieterich, W.; Reljic, D.; et al. Muscle-Derived Cytokines Reduce Growth, Viability and Migratory Activity of Pancreatic Cancer Cells. Cancers (Basel). 2021, 13, 3820. [Google Scholar] [CrossRef] [PubMed]
- Schwappacher, R.; Schink, K.; Sologub, S.; et al. Physical activity and advanced cancer: evidence of exercise-sensitive genes regulating prostate cancer cell proliferation and apoptosis. J Physiol. 2020, 598, 3871–3889. [Google Scholar] [CrossRef] [PubMed]
- Silvestri, A.; Ruscello, B.; Rosazza, C.; et al. Acute Effects of Whole-Body Electrostimulation Combined with Stretching on Lower Back Pain. Int J Sports Med. 2023, 44, 820–829. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Ikeda, M.; Minami, M.; et al. Beneficial Effect of Intradialytic Electrical Muscle Stimulation in Hemodialysis Patients: A Randomized Controlled Trial. Artif Organs. 2018, 42, 899–910. [Google Scholar] [CrossRef]
- Suzuki, Y.; Suzuki, H.; Yato, S.; et al. Mittelfristige Auswirkungen der Elektrotherapie der Skeletmuskulatur mit Gürtelelektroden auf den Glukose und Fettstoffwechsel die Körperzusammensetzung, die Muskelkraft und die Muskelausdauer bei Patienten mit Typ-2 Diabetes [型糖尿病患者における糖・脂質代謝および体組成, 筋力, 筋持久力に及ぼすベルト電極式骨格筋電気刺激療法の中期的効果]. Physical Therapy Science. 2019, 33, 53–59. [Google Scholar]
- Tanaka, S.; Kamiya, K.; Matsue, Y.; et al. Effects of electrical muscle stimulation on physical function in frail older patients with acute heart failure: a randomized controlled trial. Eur J Prev Cardiol. 2022, 29, e286–e288. [Google Scholar] [CrossRef]
- Tanaka, S.; Kamiya, K.; Matsue, Y.; et al. Efficacy and Safety of Acute Phase Intensive Electrical Muscle Stimulation in Frail Older Patients with Acute Heart Failure: Results from the ACTIVE-EMS Trial. J Cardiovasc Dev Dis. 2022, 9. [Google Scholar] [CrossRef]
- Tsurumi, T.; Tamura, Y.; Nakatani, Y.; et al. Neuromuscular Electrical Stimulation during Hemodialysis Suppresses Postprandial Hyperglycemia in Patients with End-Stage Diabetic Kidney Disease: A Crossover Controlled Trial. J Clin Med. 2022, 11, 6239. [Google Scholar] [CrossRef]
- Vaculíková, P.; Paclíková, A.; Kotková, M.; Struhár, I.; Balousová, D.N. Impact of Whole-Body Electromyostimulation and Resistance Training on Bone Mineral Density in women at risk for Osteopororosis. IJPESS. 2022, 69–79. [Google Scholar] [CrossRef]
- Vaculíková, P.; Paclíková, A.; Kotková, M.; Struhár, I.; Balousová, D.N.; Rozsypal, R. Impact of Whole-Body Electromyostimulation and Resistance Training on the Level of Functional Fitness in Elderly Women. Studia Sportiva. 2023, 16, 115–126. [Google Scholar] [CrossRef]
- van Buuren, F.; Horstkotte, D.; Mellwig, K.; et al. Electrical Myostimulation (EMS) Improves Glucose Metabolism and Oxygen Uptake in Type 2 Diabetes Mellitus Patients—Results from the EMS Study. Diabetes Technol Ther. 2015, 17, 413–419. [Google Scholar] [CrossRef]
- van Buuren, F.; Mellwig, K.P.; Frund, A.; et al. Electromyostimulation: Verbessserung von Lebensqualität, Sauerstoffaufnahme und linksventrikuläerer Funktion bei chronischer Herzinsuffizienz. Rehabilitation. 2014, 53, 321–326. [Google Scholar]
- van Buuren, F.; Mellwig, K.P.; Prinz, C.; et al. Electrical myostimulation improves left ventricular function and peak oxygen consumption in patients with chronic heart failure: results from the exEMS study comparing different stimulation strategies. Clinical research in cardiology : official journal of the German Cardiac Society. 2013, 102, 523–534. [Google Scholar] [CrossRef]
- von Stengel, S.; Bebenek, M.; Engelke, K.; Kemmler, W. Whole-Body Electromyostimulation to Fight Osteopenia in Elderly Females: The Randomized Controlled Training and Electrostimulation Trial (TEST-III). Journal of osteoporosis. 2015, 2015, 643520. [Google Scholar] [CrossRef]
- Weissenfels, A.; Teschler, M.; Willert, S.; et al. Effects of whole-body electromyostimulation on chronic nonspecific low back pain in adults: a randomized controlled study. Journal of pain research. 2018, 11, 1949–1957. [Google Scholar] [CrossRef]
- Wittmann, K.; Sieber, C.; von Stengel, S.; et al. Impact of whole body electromyostimulation on cardiometabolic risk factors in older women with sarcopenic obesity: the randomized controlled FORMOsA-sarcopenic obesity study. Clinical interventions in aging. 2016, 11, 1697–1706. [Google Scholar] [CrossRef]
- Özdal, M.; Bostanci, Ö. Effects of whole-body electromyostimulation with and without voluntary muscular contractions on total and regional fat mass of women. Archives of Applied Science Research. 2016, 8, 75–79. [Google Scholar]
- Stephan, H.; Wehmeier, U.F.; Forster, T.; Tomschi, F.; Hilberg, T. Additional Active Movements Are Not Required for Strength Gains in the Untrained during Short-Term Whole-Body Electromyostimulation Training. Healthcare (Basel). 2023, 11, 741. [Google Scholar] [CrossRef]
- Evangelista, A.L.; Teixeira, C.V.S.; Barros, B.M.; et al. Does whole-body electrical muscle stimulation combined with strength training promote morphofunctional alterations? Clinics (Sao Paulo). 2019, 74, e1334. [Google Scholar] [CrossRef]
- Teschler, M.; Weissenfels, A.; Bebenek, M.; et al. Very high creatine kinase CK levels after WB_EMS. Are there implications for health. Int J Clin Exp Med 2016, 9, 22841–22850. [Google Scholar]
- Bermejo, I.; Carnicero, J.; Garcia, F.; et al. POS1446 CREATINE KINASE COULD BE A MARKER OF CHRONIC INFLAMMATION-INDUCED SARCOPENIA IN FRAIL PATIENTS. Annals of the Rheumatic Diseases 2022, 81, 1067–1068. [Google Scholar] [CrossRef]
- Stollberger, C.; Finsterer, J. Side effects of and contraindications for whole-body electro-myo-stimulation: a viewpoint. BMJ Open Sport Exerc Med. 2019, 5, e000619. [Google Scholar] [CrossRef]
- Kirkham, J.J.; Davis, K.; Altman, D.G.; et al. Core Outcome Set-STAndards for Development: The COS-STAD recommendations. PLoS Med. 2017, 14, e1002447. [Google Scholar] [CrossRef]
- Eriksen, E.F. Cellular mechanisms of bone remodeling. Reviews in endocrine & metabolic disorders. 2010, 11, 219–227. [Google Scholar]
- WHO. Assessment of osteoporotic fracture risk and its application to screening for postmenopausal osteoporosis.; World Health Organization, Geneva, 1994, 1994.
- Knutson, J.S.; Fu, M.J.; Sheffler, L.R.; Chae, J. Neuromuscular Electrical Stimulation for Motor Restoration in Hemiplegia. Phys Med Rehabil Clin N Am. 2015, 26, 729–745. [Google Scholar] [CrossRef]
- Kemmler, W.; Weissenfels, A.; Willert, S.; et al. Recommended Contraindications for the Use of Non-Medical WB-Electromyostimulation. Dtsch Z Sportmed. 2019, 70, 278–281. [Google Scholar] [CrossRef]
- BMU. Regulation on Protection against Harmful Effects of Non-Ionizing Radiation in Human Applications (NiSV) [Verordnung zum Schutz vor schädlichen Wirkungen nichtionisierender Strahlung bei der Anwendung am Menschen (NiSV)]. Bundesministerium-für-Umwelt-Naturschutz-und-nukleare-Sicherheit: Bonn, 2019.
- BMU. Requirements for the acquisition of expertise for applications of non-ionizing radiation sources on humans [Anforderungen an den Erwerb der Fachkunde für Anwendungen nichtionisierender Strahlungsquellen am Menschen]. Bundesministerium-für-Umwelt-Naturschutz-und-nukleare-Sicherheit: Bonn, 2020.
- Berger, J.; Fröhlich, M.; Kemmler, W. WB-EMS Market Development—Perspectives and Threats. Int. J. Environ. Res. Public Health. 2022, 19, 14211. [Google Scholar] [CrossRef] [PubMed]
- Koch, A.J.; Pereira, R.; Machado, M. The creatine kinase response to resistance exercise. Journal of musculoskeletal & neuronal interactions. 2014, 14, 68–77. [Google Scholar]
- Kemmler, W.; Fröhlich, M.; Ludwig, O.; et al. Position statement and updated international guideline for safe and effective whole-body electromyostimulation training-the need for common sense in WB-EMS application. Frontiers in physiology. 2023, 14, 1174103. [Google Scholar] [CrossRef] [PubMed]
- Kemmler, W.; von Stengel, S.; Teschler, M.; et al. Ganzkörper-Elektromyostimulation, Sarkopenie und Adipositas. Ergebnisse der randomisierten kontrollierten “Franconia Sarcopenic Obesity Study” (FRANSO). Osteoporose & Rheuma Aktuell. 2017, 15, 12–18. [Google Scholar]
- Amaro-Gahete, F.J.; De-la, O.A.; Sanchez-Delgado, G.; et al. Functional Exercise Training and Undulating Periodization Enhances the Effect of Whole-Body Electromyostimulation Training on Running Performance. Frontiers in physiology. 2018, 9, 720. [Google Scholar] [CrossRef]
| 1 | ≥50% of skeletal muscle mass |
| 2 | However, two studies [95, 96] additionally implemented a “passive” WB-EMS study arm |
| 3 | Some of these studies listed scores (i.e. Sarcopenie Z-Score) or test batteries (e.g. Senior Fitness Test battery) that included several fitness parameters as the primary or core study outcome. |
| 4 | Maximum strength change was defined as primary outcome in the trials of Suzuki et al., Tanaka et al and Teschler et al. [12, 82, 85] |
| 5 | Changes in endurance were defined as primary outcome by the trials of Homma et al. [30] and Teschler et al. [12]. |
| 6 | Park et al. [69] only published data on short physical performance battery-score |
| 7 | Changes in SPPB (…and 6MWT) was the primary study outcome of the trial of [30]. |
| 8 | E.g. Kim et al. [50] listed “body composition” as the main outcome; Kemmler et al. [44, 49] applied Sarcopenic Obesity as the primary study outcome. |
| 9 | brain derived neurotropic factor, Fibroblast growth factor-21, Nerve Growth Factor |
| 10 | To avoid overlap, corresponding outcomes were given in the “inflammation” section. |
| 11 | Although not explicitly stated, oxygen uptake can be considered the primary outcome of van Buuren et al. [91] |
| 12 | Data of Teschler et al. [98] indicate that CK and Myoglobin peaks occurred 48 to 72 h post-WB-EMS. |
| Author, project | year | country (code) |
study- design |
Number of study arms (n) | total sample size (n) |
gender | age (years) |
Body Mass Index (kg/m2)1 | training-status2 | diseases/ conditions |
methodological quality5 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | FitAging-Project; Amaro-Gahete et al. [16,17,18,19,20,24,26,33,34,35,60] | 2019 | ESP | RCT | 4 | 80-89 | m+w | 53 ± 5 | 26.8 | untrained | no | 6 |
| 2 | Bellia et al. [21] | 2020 | ITA | RCT | 2 | 25 | m+w | 49±7 | 40.1 | moderate | yes | 4 |
| 3 | Blöckl et al. [22] | 2022 | GER | NRCT | 22 | 28 | m+w | 80±4 | 26.23 | untrained | yes | 4 |
| 4 | Bouty-Regard et al. [23] | 2020 | JPN | RCT | 3 | 41 | m+w | 77±2 | 21.5 | untrained | yes | 6 |
| 5 | DiCagno et al. [25] | 2023 | ITA | RCT | 3 | 24 | m+w | 72±6 | n.g. | untrained | yes | 8 |
| 6 | Evangelista et al. [27] | 2021 | BRA | RCT | 2 | 30 | m | 75±7 | n.g. | untrained | no | 5 |
| 7 | Fritzsche et al. [28] | 2010 | GER | No CG | 1 | 15 | m+w | 56±16 | 26.8 | untrained | yes | 2 |
| 8 | Hamada et al. [29] | 2023 | JPN | NRCT | 2 | 49 | m+w | 54±17 | 21.4 | untrained | yes | 3 |
| 9 | Homma et al. [30] | 2022 | JPN | RCT | 2 | 27 | m+w | 79±6 | 22.0 | untrained | yes | 5 |
| 10 | Houdjijk et al. [31] | 2022 | NL | NRCT | 4 | 75 | m+w | 45-75 | 31.84 | untrained | yes | 3 |
| 11 | Imaoka et al. [32] | 2022 | JPN | RCT | 2 | 49 | m+w | 64±7 | 24.2 | untrained | yes | 6 |
| 12 | Kataoka et al. [36] | 2019 | JPN | RCT- | 2 | 16 | m+w | 83±6 | 16.7 | untrained | yes | 5 |
| 13 | TEST I Project; Kemmler et al. [37,38,40] | 2010 | GER | RCT | 2 | 30 | w | 65±6 | 26.0 | well-train. | yes | 6 |
| 14 | TEST II-Project; Kemmler et al. [38,39,40] | 2012 | GER | RCT | 2 | 28 | m | 69±3 | 28.1 | untrained | yes | 5 |
| 15 | TEST III-Project; Kemmler/von Stengel et al. [41,42,43,92] | 2015 | GER | RCT | 2 | 76 | m+w | >70 | 34.6 | untrained | yes | 7 |
| 16 | TEST III-Sub-Project; Kemmler et al. [43] | 2013 | GER | RCT | 2 | 46 | w | >70 | 22.1 | untrained | yes | 7 |
| 17 | Formosa-Project; Kemmler et al. [44,45,94] | 2016 | GER | RCT | 3 | 75 | w | 77±4 | 25.1 | untrained | yes | 8 |
| 18 | FranSO-Project; Kemmler et al. [46,47,48,49,111]. | 2017 | GER | RCT | 3 | 100 | m | 77±5 | 26.1 | moderate | yes | 8 |
| 19 | Kim et al [50] | 2020 | KOR | RCT | 2 | 25 | w | 71±3 | 30.9 | untrained | yes | 6 |
| 20 | Konrad et al. [51] | 2020 | GER | NRCT | 2 | 128 | m+w | 56±14 | n.g. | untrained | yes | 2 |
| 21 | Lukashevich et al. [52] | 2020 | BLR | RCT | 3 | 52 | w | 45-65 | n.g. | untrained | yes | 4 |
| 22 | Matsumoto et al. [53] | 2020 | JPN | No CG | 1 | 4 | m+w | 66±6 | 24.0 | untrained | yes | 2 |
| 23 | Matsuo et al. [54] | 2022 | JPN | NRCT | 2 | 90 | m+w | 77±11 | 24.0 | untrained | yes | 4 |
| 24 | Micke et al. [55] | 2021 | GER | RCT | 3 | 240 | m+w | 40-70 | 26.3 | moderate | yes | 8 |
| 25 | Mori 2020 et al. [56] | 2020 | JPN | NRCT | 1 | 14 | m | 65±13 | n.g. | untrained | yes | 4 |
| 26 | Müllerova et al. [57] | 2022 | CZE | RCT | 2 | 21 | w | 63±2 | 26.6 | untrained | no | 4 |
| 27 | Nakamura et al. [58] | 2019 | JPN | RCT | 2 | 94 | m+w | 76±12 | 21.0 | untrained | yes | 4 |
| 28 | Nakamura et al. [59] | 2021 | JPN | RCT | 2 | 134 | m+w | 68±15 | 21.4 | untrained | yes | 5 |
| 29 | Nejad et al. [61] | 2021 | IRN | RCT | 5 | 50 | w | 60-70 | 28.2 | untrained | no | 3 |
| 30 | Noguchi et al. [62] | 2017 | JPN | No CG | 1 | 8 | m+w | 69±10 | n.g. | untrained | yes | 1 |
| 31 | Nonoyama et al. [63] | 2022 | JPN | NRCT | 2 | 42 | m+w | 72-84 | 24.4 | untrained | yes | 3 |
| 32 | Ochiai et al. [64] | 2018 | JPN | NRCT | 2 | 6 | m+w | 60-90 | n.g. | untrained | yes | 3 |
| 33 | Leida-Project; Pano-Rodriguez et al. [65,66,73] | 2020 | ESP | RCT | 2 | 34 | w | 61±4 | 26.5 | untrained | no | 7 |
| 34 | Park 2021 et al. [68] | 2021 | Kor | RCT | 2 | 34 | w | 70±4 | 27.5 | untrained | yes | 7 |
| 35 | Park et al. [67] | 2021 | Kor | RCT | 3 | 81 | w | 61-79 | 24.4 | untrained | yes | 7 |
| 36 | Park et al [69] | 2023 | Kor | RCT | 4 | 60 | w | ≥65 | 25.4 | Untrained | yes | 7 |
| 37 | MetS-Project; Reljic el al. [70,71,72] | 2022 | GER | RCT | 4 | 29-118 | m+w | 53±11 | 37.2 | moderate | yes | 6 |
| 38 | Sanchez-Infante et al. [75] | 2020 | ESP | RCT | 2 | 28 | w | 40-60 | 25.5 | moderate | no | 6 |
| 39 | Advanced cancer project; Schink et al. [76,77] | 2018 | GER | NRCT | 2 | 131 | m+w | 60±13 | 25.2 | untrained | yes | 3 |
| 40 | Advanced cancer project; Schink et al. [78] | 2018 | GER | NRCT | 2 | 31 | m+w | 55±15 | 25.4 | untrained | yes | 3 |
| 41 | Advanced cancer project; Richter et al. [74] | 2019 | GER | NRCT | 2 | 75 | m+w | 59±13 | 25.5 | untrained | yes | 4 |
| 42 | Advanced cancer project; Schwappacher et al. [80] | 2020 | GER | NRCT | 2 | 30 | m+w | 63±15 | 28.0 | untrained | yes | 3 |
| 43 | Advanced cancer project, Schwappacher et al. [79] | 2021 | GER | NRCT | 2 | 12 | m+w | 62±9 | 26.8 | untrained | yes | 3 |
| 44 | Silvestri et al. [81] | 2023 | ITA | NRCT | 2 | 52 | m+w | 43-81 | 24.6 | untrained | yes | 3 |
| 45 | Suzuki et al. [82] | 2018 | JPN | RCT | 2 | 29 | w | 66±10 | 23.2 | untrained | no | 4 |
| 46 | Suzuki. et al. [83] | 2018 | JPN | No CG | 1 | 12 | m+w | 65±7 | 23.7 | untrained | yes | 3 |
| 47 | Tanaka et al. [84,85] | 2022 | JPN | RCT | 2 | 39 | m+w | 66±10 | 26.7 | untrained | yes | 7 |
| 48 | Teschler et al. [12] | 2021 | GER | NRCT | 3 | 134 | m+w | 56±8 | 36.2 | untrained | yes | 7 |
| 49 | Tsurumi et al. [86] | 2022 | JPN | RCT | 2 | 11 | m+w | 74±5 | 35.7 | moderate | yes | 5 |
| 50 | Vacoulikova et al. [88] | 2021 | CZE | RCT | 3 | 21 | m+w | 60-65 | 22.7 | untrained | yes | 4 |
| 51 | Vacoulikova et al. [87] | 2021 | CZE | RCT | 3 | 63 | w | 60-65 | 27.1 | untrained | no | 4 |
| 52 | van Buuren et al. [90,91] | 2014 | GER | NRCT | 3 | 60 | w | 61±11 | 27.0 | untrained | yes | 4 |
| 53 | van Buuren et al. [89] | 2015 | GER | No CG | 1 | 15 | m+w | 62±4 | 29.7 | untrained | yes | 4 |
| 54 | Weissenfels et al. [93] | 2018 | GER | RCT | 2 | 60 | w | 57±7 | 22.2 | untrained | yes | 8 |
- CG: control group; IS: Intervention study; m: men, n.a.: not applicable; NRCT: non-randomized controlled trial; RCT: randomized controlled trial; w: women; methodological quality according to PEDro (maximum of 10 score points)
- 1 due to the approach of calculating BMI by body length and mass in case of missing BMI we do not list the SD here; 2 training status: untrained = no regular exercise; moderate = 1 session per week, well-trained = 2-3 sessions per week;3 Blöckl et al.: BMI refer to “frail cohort”;4 Houdjik et al: BMI refer to participants with non-insulin dependent diabetes; 5 according to PEDro.
| Author | NEMS System | Isolated EMS? | Active mode? | Intervention length(months) |
Sessions per week (n) | length of the session (min) | Impulse-frequency (Hz) | Impulse-width (µs) | Impulse-length (s) | Impulse-break (s) | WB-EMS Drop-out (%) | Adherence (%) | Adverse effects | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | FitAging-Project; Amaro-Gaehete et al. [16,17,18,19,20,24,26,33,34,35,60,112] | WB-EMS1 | no | yes | 3 | 2 | 20 or 32.5 | 15-20 or 35-75 |
200 - 400 | 6 | 4 | 17 | 99 | no |
| 2 | Bellia et al. [21] | WB-EMS | yes | yes | 6 | 2 | 20 | 15 or 85 | 400 | 42 | 4 | 23 | 90 | no |
| 3 | Blöckl et al. [22] | WB-EMS | yes | yes | 2 | 1-1.5 | 20 | 85 | 350 | 6 | 4 | 14 | 88 | no |
| 4 | Bouty-Regard et al. [23] | B-SES2 | yes | n.g. | 3 | 2 | 20 | 20 | 250 | 5 | 2 | 0 | 97 | no |
| 5 | DiCagno et al. [25] | WB-EMS | yes | yes | 3 | 2 | 20 | 7 or 85 | 350 | 4 | 4 | 0 | 100 | no |
| 6 | Evangelista et al. [27] | WB-EMS | no | yes | 1.5 | 2 | 20 | 85 | 350 | 4 | 2 | 33 | 100 | no |
| 7 | Fritzsche et al. [28] | WB-EMS | yes | yes | 6 | 2 | 20 | 80 | 300 | 4 | 4 | 0 | n.g. | no |
| 8 | Hamada et al. [29] | B-SES | yes | yes | 1 | 7(?) | 20 | 20 | 250 | 5 | 2 | 12 | 71 | no |
| 9 | Homma et al. [30] | B-SES | yes | no | 3 | 3 | 40 | 20 | 250 | 5 | 2 | 29 | 100 | no |
| 10 | Houdjijk et al. [31] | WB-EMS | yes | yes | 4 | 2 | 20 | 85 | 350 | 4 | 4 | 0 | 95 | no |
| 11 | Imaoka et al. [32] | B-SES | yes | no | 0.5 | 5 | 20 | 20 | 250 | 5 | 2 | 27 | n.g. | no |
| 12 | Kataoka et al. [36] | B-SES | yes | no | 3 | 3 | 20 | 4 | 250 | 1200 | 25 | n.g. | no | |
| 13 | TEST I Project; Kemmler et al. [37,38] | WB-EMS | yes | yes | 3.5 | 2 | 20 | 7 or 85 | 350 | 4 | 4 | 0 | 98 | no |
| 14 | TEST II-Project; Kemmler et al. [38,39] | WB-EMS | yes | yes | 3.5 | 1.50 | 30 | 85 | 350 | 4 | 4 | 7 | 78 | no |
| 15 | TEST-III-Project; Kemmler/von Stengel et al [40,41,42,92] | WB-EMS | yes | yes | 12 | 1.50 | 20 | 85 | 350 | 6 | 4 | 16 | 79 | no |
| 16 | TEST III-Sub-Project; Kemmler et al. [43] | WB-EMS | yes | yes | 12 | 1.50 | 20 | 85 | 350 | 6 | 4 | 16 | 79 | no |
| 17 | Formosa-Project Kemmler et al. [44,94] | WB-EMS | yes | yes | 6 | 1 | 20 | 85 | 350 | 4 | 4 | 10 | 89 | no |
| 18 | FranSO-Project; Kemmler et al. [46,47,48,49,111]. | WB-EMS | yes | yes | 4 | 1.50 | 20 | 85 | 350 | 4 | 4 | 9 | 91 | no |
| 19 | Kim et al. [50] | WB-EMS | no | yes | 2 | 3 | 40 | 85 | 350 | 6 | 4 | 13 | n.g. | no |
| 20 | Konrad et al. [51] | WB-EMS | yes | yes | 1.5 | 1 | 20 | 85 | 350 | 4 | 4 | 27 | 85 | no |
| 21 | Lukashevich et al. [52] | WB-EMS | no | yes | 0.66 | 4 | 20 | Up to 25000 |
Up to 5000 | n.g. | n.g. | n.g. | n.g. | no |
| 22 | Matsumoto et al. [53] | B-SES | yes | no | 1 | 5 | 20 | 20 | 250 | 5 | 2 | n.g. | n.g. | no |
| 23 | Matsuo et al. [54] | B-SES | yes | n.g. | 0.5 | 5 | 20 | 20 | 250 | 5 | 2 | 6 | 94 | no |
| 24 | Micke et al. [55] | WB-EMS | yes | yes | 3 | 1 | 20 | 85 | 350 | 6 | 4 | 9 | 92 | no |
| 25 | Mori 2020 et al. [56] | B-SES | yes | n.g. | 1.5 | 2 | 30 | 20 | 250 | 5 | 2 | n.g. | n.g. | n.g. |
| 26 | Müllerova et al. [57] | WB-EMS | yes | yes | 2.5 | 1 | 20 | 85 | 350 | 4 | 4 | 18 | n.g. | n.g. |
| 27 | Nakamura et al. [58] | B-SES | yes | n.g. | 0.5 | 7 | 20 | 20 | 250 | 5 | 2 | 55 | 100 | no |
| 28 | Nakamura et al. [59] | B-SES | yes | n.g. | 0.5 | 7 | 20 | 20 | 250 | 5 | 2 | 17 | 100 | n.g. |
| 29 | Nejad et al. [61] | WB-EMS | no | yes | 3 | 3 | 20 | 15-33 or 35-75 |
200 and 400 | 6 | 4 | n.g. | n.g. | n.g. |
| 30 | Noguchi et al. [62] | B-SES | yes | n.g. | 3 | 3 | 20 | 20 | 250 | 5 | 2 | 0 | n.g | no |
| 31 | Nonoyama et al. [63] | B-SES | yes | n.g. | 1.30 | 5 | 30 | 20 | 250 | 5 | 2 | n.g. | 97 | no |
| 32 | Ochiai et al. [64] | B-SES | yes | n.g. | 1.10 | 7 | 20 | 20 | 250 | 5 | 2 | 0 | n.g. | no |
| 33 | Leida-Project; Pano-Rodriguez et al. [65,66,73] | WB-EMS | no | yes | 2.5 | 2 | 40 | 7 or 55 | 150 to 350 | 6 | 4 | 6 | 93 | no |
| 34 | Park 2021 et al. [68] | WB-EMS | no | yes | 1.5 | 3 | 40 | 80 | n.g. | 5 | 3 | 6 | 100 | no |
| 35 | Park et al. [67] | WB-EMS | no | yes | 2 | 3 | 20 | 85 | 350 | 6 | 4 | 7 | 92 | no |
| 36 | Park et al. [69] | WB-EMS | no | yes | 2 | 3 | 45 | 4 | n.g. | 2 | 2 | 3 | 97 | no |
| 37 | MetS-Project; Reljic el al. [70,71,72] | WB-EMS | yes | yes | 3 | 2 | 20 | 85 | 350 | 6 | 4 | 23 | 93 | no |
| 38 | Sanchez-Infante et al. [75] | WB-EMS | no | yes | 2 | 1 | 20 | 10 or 85 | 350 | 8/cont. | 4/cont. | 0 | 100 | no |
| 39 | Schink et al. [76,77] | WB-EMS | yes | yes | 3 | 2 | 20 | 85 | 350 | 6 | 4 | 40 | 87 | no |
| 40 | Schink et al. [78] | WB-EMS | yes | yes | 3 | 2 | 20 | 85 | 350 | 6 | 4 | 59 | 77 | no |
| 41 | Richter et al. [74] | WB-EMS | yes | yes | 3 | 2 | 20 | 85 | 350 | 6 | 4 | 19 | 88 | no |
| 42 | Schwappacher et al. [80] | WB-EMS | yes | yes | 3 | 2 | 20 | 85 | 350 | 6 | 4 | n.g. | 88 | no |
| 43 | Schwappacher [79] | WB-EMS | yes | yes | 3 | 2 | 20 | 85 | 350 | 6 | 4 | n.g. | 79 | no |
| 44 | Silvestri et al. [81] | WB-EMS | yes | yes | 2 | 2 | 20 | 85 | 350 | 6 | 4 | 23 | 91 | no |
| 45 | Suzuki et al. [82] | B-SES | yes | n.g. | 2 | 3 | 20 | 20 | 250 | 5 | 2 | 13 | 98 | no |
| 46 | Suzuki. et al. [83] | B-SES | yes | no | 3 | 3 | 30 | 20 | 250 | 5 | 2 | 0 | n.g. | no |
| 47 | Tanaka et al. [84,85] | B-SES | yes | no | 0.30 | 5 | 35 | 20 | 250 | 5 | 2 | 25 | 86 | no |
| 48 | Teschler et al. [12] | WB-EMS | yes | yes | 1 | 1.50 | 20 | 85 | 350 | 4 | 4 | 9 | 98 | no |
| 49 | Tsurumi et al. [86] | B-SES | yes | no | 3 | 3 | 30 | 4 | 250 | 1200 | 0 | 27 | n.g. | n.g. |
| 50 | Vacoulikova et al. [88] | WB-EMS | yes | yes | 2.5 | 1 | 20 | 85 | 350 | 4 | 4 | n.g. | 81 | no |
| 51 | Vacoulikova et al. [87] | WB-EMS | yes | yes | 2.5 | 1 | 20 | 85 | 350 | 4 | 4 | 18 | 100 | no |
| 52 | van Buuren et al. [90,91] | WB-EMS | yes | yes | 2.5 | 2 | 20 | 80 | 350 | 4 | 4 | 0 | 100 | no |
| 53 | van Buuren 2015 et al. [89] | WB-EMS | yes | yes | 2.5 | 2 | 20 | 80 | 350 | 4 | 4 | 0 | 100 | no |
| 54 | Weissenfels et al. [93] | WB-EMS | yes | yes | 3 | 1 | 20 | 85 | 350 | 6 | 4 | 7 | 93 | no |
- 1 WB-EMS: simultaneous application of electric stimuli via at least six current channels or participation of all major muscle groups, with a current impulse effective to trigger muscular adaptations”[1]. In detail: large electrodes embedded in vest and cuffs were used to stimulate both thighs, upper arms, gluteals, lower back, upper back, latissimus area, abdomen and chest (stimulated area up to 2800 cm2)
- 2 B-SES: We are not aware of a dedicated definition of B.SES, however, B-SES focuses on the stimulation of gluteals and lower extremities using belt-electrodes.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





