Submitted:
09 March 2024
Posted:
11 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Epidemiology
3. Most Common Musculoskeletal Pathologies
4. Clinical Examination
5. Complementary Diagnostic Exams
6. Treatment Options
6.1. Conservative Therapies
6.1.1. Physiotherapeutic Modalities
Physical and Mechanical Agents
Kynesiotape and Bandage
Therapeutic Exercise
Electrotherapy
6.1.2. Pharmacologic Conservative Therapies
Anti-Inflammatories
Hyaluronic Acid (HyA)
Polyacrylamide Hydrogel
Bisphosphonates: Tiludronate and Clodronate
6.1.3. Conservative Surgical Techniques
6.2. Regenerative Therapies
6.2.1. Hemoderivatives
6.2.2. Mesenchymal Stromal/Stem Cell Based Therapies
7. Prognosis
8. Discussion
9. Conclusion and Future Research Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 2D | two-dimensional |
| 3D | three-dimensional |
| ACI | autologous chondrocyte implantation |
| ACS | autologous conditioned serum |
| AFS-MSC | amniotic fluid mesenchymal stromal/stem cell |
| AINEs | non-steroidal anti-inflammatories |
| APS | autologous protein serum |
| AT-MSC | adipose tissue mesenchymal stromal/stem cell |
| BM-MSC | bone marrow mesenchymal stromal/stem cell |
| CD | cluster differentiation |
| CD | complementary diagnostic exams |
| CDET | common digital extensor tendon |
| cm | centimeter |
| CM | conditioned medium |
| cm2 | square centimeter |
| COX | cycloxigenase |
| CSA | cross sectional area |
| CT | Computed Tomography |
| CTA | Computed Tomography Arthrography |
| DDFT | deep digital flexor tendon |
| DNA | desoxyribonucleic acid |
| DP-MSC | dental pulp mesenchymal stromal/stem cell |
| ECM | extracellular matrix |
| ESC | embryonic stem cell |
| ESWT | extracorporeal shock wave therapy |
| EV | extracellular vesicles |
| FEI | Federation Equestre Internationale |
| FGF | fibroblast growth factor |
| FL | forelimbs |
| GAG | glycosaminoglicans |
| GF | growth factor |
| h | hour |
| HILT | high intensity laser therapy |
| HL | hindlimbs |
| HLA | human leucocyte antigen |
| HSC | hematopoietic stem cell |
| HyA | hyaluronic acid |
| Hz | Hertz |
| IA | intra-articular |
| IGF | insulin growth factor |
| IL | Interleukyn |
| IM | intramuscular |
| IPSC | induced pluripotent stem cell |
| IRAP | interleukin-1 receptor antagonist protein |
| IRU | radioisotope uptake |
| IV | endovenous |
| Kg | kilogram |
| KT | Kynesiotaping |
| LLLT | low level laser therapy |
| mg | milligram |
| MHz | megahertz |
| min | minute |
| ml | milliliter |
| MRI | Magnetic Resonance image |
| MSC | mesenchymal stem/stromal cells |
| MT-MSC | muscle tissue mesenchymal stromal/stem cell |
| mW | milliwatts |
| NEMS | Neural electrical muscle stimulation |
| nm | nanometres |
| OA | osteoarthritis |
| oC | Celsius degree |
| PDEGF | platelet derived epidermal growth factor |
| PDGF | platelet derived growth factor |
| PEMF | pulsed electromagnetic frequency |
| PGE2 | Prostaglandin E2 |
| PHyd | Polyacrylamide hydrogel |
| Po -MSC | periosteum mesenchymal stromal/stem cell |
| PO | Per os |
| PSAG | Polysulfated glycosaminoglycan |
| RNA | ribonucleic acid |
| ROM | range of motion |
| SAIDs | steroidal anti-inflammatories |
| SDFT | superficial digital flexor tendon |
| SL | suspensory ligament |
| SM-MSC | synovial membrane mesenchymal stromal/stem cell |
| TENS | transcutaneous electrical nerve stimulation |
| TGF | Transforming growth factor |
| U/S | Ultrasound |
| UC-MSC | umbilical cord derived Whartons jelly mesenchymal stromal/stem cell |
| VEGF | vascular endothelial growth factor |
| VEGF | vascular endothelial growth factor |
| W | Watts |
| WT | water treadmill |
| X-ray | Radiograph |
| α2M | Alfa-2 macroglobulin |
References
- Smith, R.K.W.; McIlwraith, C.W. “One Health” in tendinopathy research: Current concepts. J. Orthop. Res. 2021, 39, 1596–1602. [Google Scholar] [CrossRef]
- Rogers, C.W.; Bolwell, C.F.; Gee, E.K.; Rosanowski, S.M. Equine musculoskeletal development and performance: impact of the production system and early training. Anim. Prod. Sci. 2020, 60, 2069–2079. [Google Scholar] [CrossRef]
- Smith, R.; Webbon, P. Harnessing the stem cell for the treatment of tendon injuries: heralding a new dawn? British journal of sports medicine 2005, 39, 582–584. [Google Scholar] [CrossRef]
- Shokry, M.; Mostafa, A.; Tohamy, A.; El-Sharkawi, M. Autologous mesenchymal stem cells for treatment of acute superficial digital flexor tendonitis in athletic horses: clinical study of 15 cases. Pferdeheilkunde Equine Med. 2020, 36, 43–48. [Google Scholar] [CrossRef]
- Salz, R.O.; Elliott, C.R.B.; Zuffa, T.; Bennet, E.D.; Ahern, B.J. Treatment of racehorse superficial digital flexor tendonitis: A comparison of stem cell treatments to controlled exercise rehabilitation in 213 cases. Equine Veter- J. 2023, 55, 979–987. [Google Scholar] [CrossRef] [PubMed]
- Lim, W.B.; Al-Dadah, O. Conservative treatment of knee osteoarthritis: A review of the literature. World J. Orthop. 2022, 13, 212–229. [Google Scholar] [CrossRef]
- Sutton, J.S.; Muran, A.; Zaslav, K.; Grande, D. Orthobiologics: An Updated Definition. Open Journal of Regenerative Medicine 2023, 12, 36–48. [Google Scholar] [CrossRef]
- De Sousa, N.R.; Luna, S.P.L.; Pizzigatti, D.; Martins, M.T.A.; Possebon, F.S.; Aguiar, A.C.S. Relation between type and local of orthopedic injuries with physical activity in horses. Ciência Rural 2016, 47. [Google Scholar] [CrossRef]
- Lönnell, C. Yard differences in training, management and orthopedic injury in showjumping, riding school, and thoroughbred race horses; Department of Clinical Sciences, Swedish University of Agricultural Sciences: 2012.
- Gramm, M.; Marksteiner, R. The Effect of Age on Thoroughbred Racing Performance. J. Equine Sci. 2010, 21, 73–78. [Google Scholar] [CrossRef]
- Cruz, A.M.; Poljak, Z.; Filejski, C.; Lowerison, M.L.; Goldie, K.; Martin, S.W.; Hurtig, M.B. Epidemiologic characteristics of catastrophic musculoskeletal injuries in Thoroughbred racehorses. Am. J. Veter- Res. 2007, 68, 1370–1375. [Google Scholar] [CrossRef]
- Bertuglia, A.; Bullone, M.; Rossotto, F.; Gasparini, M. Epidemiology of musculoskeletal injuries in a population of harness Standardbred racehorses in training. BMC Veter- Res. 2014, 10, 1–10. [Google Scholar] [CrossRef]
- Bolwell, C.; Rogers, C.; Gee, E.; McIlwraith, W. Epidemiology of Musculoskeletal Injury during Racing on New Zealand Racetracks 2005–2011. Animals 2017, 7, 62. [Google Scholar] [CrossRef] [PubMed]
- Walters, J.M.; Parkin, T.; A Snart, H.; Murray, R.C. Current management and training practices for UK dressage horses. Comp. Exerc. Physiol. 2008, 5, 73–83. [Google Scholar] [CrossRef]
- Murray, R.C.; Dyson, S.J.; Tranquille, C.; Adams, V. Association of type of sport and performance level with anatomical site of orthopaedic injury diagnosis. Equine Veter- J. 2006, 38, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Kaneene, J.B.; Ross, W.A.; Miller, R. The Michigan equine monitoring system. II. Frequencies and impact of selected health problems. Prev. Veter- Med. 1997, 29, 277–292. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, E.; Hassaneen, A.S.A.; Noby, M.A.; Mawas, A.; Abdel-Hady, A.-N.A. Equine osteoarthritis: An overview of different treatment strategies. SVU-International J. Veter- Sci. 2021, 4, 85–96. [Google Scholar] [CrossRef]
- Chen, D.; Shen, J.; Zhao, W.; Wang, T.; Han, L.; Hamilton, J.L.; Im, H.-J. Osteoarthritis: toward a comprehensive understanding of pathological mechanism. Bone Res. 2017, 5, 1–13. [Google Scholar] [CrossRef]
- E Schlueter, A.; Orth, M.W. Equine osteoarthritis: a brief review of the disease and its causes. Equine Comp. Exerc. Physiol. 2004, 1, 221–231. [Google Scholar] [CrossRef]
- Grässel, S.; Zaucke, F.; Madry, H. Osteoarthritis: Novel Molecular Mechanisms Increase Our Understanding of the Disease Pathology. J. Clin. Med. 2021, 10, 1938. [Google Scholar] [CrossRef]
- Grässel, S.; Muschter, D. Recent advances in the treatment of osteoarthritis. F1000Research 2020, 9, 325. [Google Scholar] [CrossRef]
- Ireland, J.L.; Clegg, P.D.; McGOWAN, C.M.; McKANE, S.A.; Chandler, K.J.; Pinchbeck, G.L. Comparison of owner-reported health problems with veterinary assessment of geriatric horses in the United Kingdom. Equine Veter- J. 2012, 44, 94–100. [Google Scholar] [CrossRef]
- Di Filippo, P.A.; Meireles, M.A.D.; Ribeiro, L.M.F.; de Lannes, S.T.; Meireles, N.F.T.; Viana, I.S.; Hokamura, H.K. Influence of Exercise, Age, Body weight, and Growth on the Development of Tarsal Osteoarthritis in Young Mangalarga Marchador Horses. J. Equine Veter- Sci. 2019, 80, 36–39. [Google Scholar] [CrossRef]
- Neundorf, R.H.; Lowerison, M.B.; Cruz, A.M.; Thomason, J.J.; McEwen, B.J.; Hurtig, M.B. Determination of the prevalence and severity of metacarpophalangeal joint osteoarthritis in Thoroughbred racehorses via quantitative macroscopic evaluation. Am. J. Vet. Res. 2010, 71, 1284–1293. [Google Scholar] [CrossRef]
- INVALID CITATION !!!
- Thorpe, C.T.; Godinho, M.S.; Riley, G.P.; Birch, H.L.; Clegg, P.D.; Screen, H.R. The interfascicular matrix enables fascicle sliding and recovery in tendon, and behaves more elastically in energy storing tendons. J. Mech. Behav. Biomed. Mater. 2015, 52, 85–94. [Google Scholar] [CrossRef]
- Zielińska, P.; Nicpoń, J.; Kiełbowicz, Z.; Soroko, M.; Dudek, K.; Zaborski, D. Effects of High Intensity Laser Therapy in the Treatment of Tendon and Ligament Injuries in Performance Horses. Animals 2020, 10, 1327. [Google Scholar] [CrossRef]
- Zielińska, P.; Soroko, M.; Godlewska, M.; Śniegucka, K.; Dudek, K.; Howell, K. Photothermal Effects of High-Intensity Laser Therapy on the Superficial Digital Flexor Tendon Area in Clinically Healthy Racehorses. Animals 2022, 12, 1253. [Google Scholar] [CrossRef] [PubMed]
- Qazi, T.H.; Duda, G.N.; Ort, M.J.; Perka, C.; Geissler, S.; Winkler, T. Cell therapy to improve regeneration of skeletal muscle injuries. J. Cachexia Sarcopenia Muscle 2019, 10, 501–516. [Google Scholar] [CrossRef] [PubMed]
- Piercy, R.J.; Rivero, J. Muscle disorders of equine athletes. Equine Sports Medicine and Surgery E-Book: Basic and clinical sciences of the equine athlete 2013, 109.
- Walmsley, E.; Steel, C.; Richardson, J.; Whitton, R. Muscle strain injuries of the hindlimb in eight horses: diagnostic imaging, management and outcomes. Aust. Veter- J. 2010, 88, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.-Y.; Lee, E.-J.; Park, J.-K.; Park, S.-I.; Cho, S.-G.; Kim, H.K.; Kim, S.-Y.; Jeong, K.-S. Generation of Equine-Induced Pluripotent Stem Cells and Analysis of Their Therapeutic Potential for Muscle Injuries. Cell Transplant. 2016, 25, 2003–2016. [Google Scholar] [CrossRef]
- Redden, R.F. Clinical and radiographic examination of the equine foot. 2003.
- Hinchcliff, K.W.; Kaneps, A.J.; Geor, R.J.; Van Erck-Westergen, E. Equine Sports Medicine and Surgery: Equine Sports Medicine and Surgery-E-Book; Elsevier Health Sciences: 2023.
- Hinchcliff, K.W. Clinical Epidemiology and Evidence-Based Medicine. Equine Internal Medicine-E-Book 2017, 1, 218.
- Schumacher, J.; Taylor, D.R.; Schramme, M.C.; Schumacher, J. Localization of pain in the equine foot emphasizing the physical examination and analgesic techniques. 2012.
- Park, R.D.; Nelson, T.R.; Hoopes, P.J. Magnetic resonance imaging of the normal equine digit and metacarpophalangeal joint. Veter- Radiol. 1987, 28, 105–116. [Google Scholar] [CrossRef]
- Kraft, S.L.; Gavin, P. Physical Principles and Technical Considerations for Equine Computed Tomography and Magnetic Resonance Imaging. Veter- Clin. North Am. Equine Pr. 2001, 17, 115–130. [Google Scholar] [CrossRef]
- Fraschetto, C.; Dancot, M.; Vandersmissen, M.; Denoix, J.-M.; Coudry, V. Conservative management of equine tarsal collateral ligament injuries may allow return to normal performance. J. Am. Veter- Med Assoc. 2023, 261, 995–1003. [Google Scholar] [CrossRef]
- Coudry, V.; Denoix, J. Ultrasonographic examination of the palmar aspect of the pastern of the horse: Digital flexor tendons and digital sheath. Equine Veter- Educ. 2013, 25, 196–203. [Google Scholar] [CrossRef]
- Denoix, J.-M. Diagnostic Techniques for Identification and Documentation of Tendon and Ligament Injuries. Veter- Clin. North Am. Equine Pr. 1994, 10, 365–407. [Google Scholar] [CrossRef]
- Werpy, N.M.; Denoix, J.-M. Imaging of the Equine Proximal Suspensory Ligament. Veter- Clin. North Am. Equine Pr. 2012, 28, 507–525. [Google Scholar] [CrossRef]
- Garrett, K.S. Ultrasonography of the hock. Atlas of equine ultrasonography 2022, 173-188.
- Dik, K.J. Ultrasonography of the equine tarsus. Veterinary Radiology & Ultrasound 1993, 34, 36–43. [Google Scholar] [CrossRef]
- Denoix, J.-M. Ultrasonographic examination of joints, a revolution in equine locomotor pathology. Bulletin de l’Académie vétérinaire de France 2009, 162, 313–325. [Google Scholar] [CrossRef]
- De Bastiani, G.; de La Côrte, F.D.; Brass, K.E.; Kommers, G.D.; Denoix, J.M. Association of Ultrasound and Anatomopathologic Findings of Equine Metacarpophalangeal Lesions. J. Equine Veter- Sci. 2014, 34, 1218–1225. [Google Scholar] [CrossRef]
- Brommer, H.; Rijkenhuizen, A.B.M.; Brama, P.A.J.; Barneveld, A.; van Weeren, P.R. Accuracy of diagnostic arthroscopy for the assessment of cartilage damage in the equine metacarpophalangeal joint. Equine Veter- J. 2004, 36, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Merkely, G.; Ackermann, J.; Lattermann, C. Articular cartilage defects: incidence, diagnosis, and natural history. Operative techniques in sports medicine 2018, 26, 156–161. [Google Scholar] [CrossRef]
- Ehrle, A.; Lilge, S.; Clegg, P.D.; Maddox, T.W. Equine flexor tendon imaging part 2: Current status and future directions in advanced diagnostic imaging, with focus on the deep digital flexor tendon. Veter- J. 2021, 278, 105763. [Google Scholar] [CrossRef]
- Palmer, A.J.R.; Brown, C.P.; McNally, E.G.; Price, A.J.; Tracey, I.; Jezzard, P.; Carr, A.J.; Glyn-Jones, S.; Ayyar-Gupta, V.; Dutton, S.J.; et al. Non-invasive imaging of cartilage in early osteoarthritis. Bone Jt. J. 2013, 95, 738–746. [Google Scholar] [CrossRef]
- Doll, C.U.; Bohner, M.; Berner, D.; Buettner, K.; Horstmeier, C.; Winter, K.; Burk, J. Approaches to standardising the magnetic resonance image analysis of equine tendon lesions. Veter- Rec. Open 2023, 10, e257. [Google Scholar] [CrossRef] [PubMed]
- Barrett, M.F.; Goorchenko, G.E.; Frisbie, D.D. Comparison of Ultrasound and Magnetic Resonance Imaging for Identifying Soft Tissue Abnormalities in the Palmar Aspect of the Equine Digit. Animals 2023, 13, 2328. [Google Scholar] [CrossRef] [PubMed]
- Mair, T.S.; Kinns, J.; Jones, R.D.; Bolas, N.M. Magnetic resonance imaging of the distal limb of the standing horse. Equine Veter- Educ. 2005, 17, 74–78. [Google Scholar] [CrossRef]
- Vanderperren, K.; Raes, E.; Hoegaerts, M.; Saunders, J.H. Diagnostic imaging of the equine tarsal region using radiography and ultrasonography. Part 1: The soft tissues. Veter- J. 2009, 179, 179–187. [Google Scholar] [CrossRef]
- Biggi, M. Equine scintigraphy: basic principles and interpretation. UK-Vet Equine 2020, 4, 84–86. [Google Scholar] [CrossRef]
- Dyson, S. Musculoskeletal Scintigraphy of the Equine Athlete. Semin. Nucl. Med. 2014, 44, 4–14. [Google Scholar] [CrossRef]
- Denoix, J.-M. Physical Therapy and Massage for the Horse: Biomechanics-Excercise-Treatment; CRC Press: 2021.
- Yang, S.-M.; Chen, W.-S. Conservative treatment of tendon injuries. American Journal of Physical Medicine & Rehabilitation 2020, 99, 550–557. [Google Scholar] [CrossRef]
- Frick, A. Stretching exercises for horses: are they effective? Journal of equine veterinary science 2010, 30, 50–59. [Google Scholar] [CrossRef]
- Kaneps, A.J. Practical Rehabilitation and Physical Therapy for the General Equine Practitioner. Veter- Clin. North Am. Equine Pr. 2016, 32, 167–180. [Google Scholar] [CrossRef]
- van Eps, A.W.; Orsini, J.A. A comparison of seven methods for continuous therapeutic cooling of the equine digit. Equine Veter- J. 2016, 48, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Marlin, D. Evaluation of the cooling efficacy of different equine leg cooling methods. Comp. Exerc. Physiol. 2019, 15, 113–122. [Google Scholar] [CrossRef]
- Montgomery, L.; Elliott, S.B.; Adair, H.S. Muscle and Tendon Heating Rates with Therapeutic Ultrasound in Horses. Veter- Surg. 2013, 42, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Ericson, C.; Stenfeldt, P.; Hardeman, A.; Jacobson, I. The Effect of Kinesiotape on Flexion-Extension of the Thoracolumbar Back in Horses at Trot. Animals 2020, 10, 301. [Google Scholar] [CrossRef] [PubMed]
- GARCIA PIQUERES, M.; FORÉS JACKSON, P. Evaluation of kinesio taping applied to the equine thoracolumbar spine: clinical response and mechanical nociceptive threshold. Journal of Veterinary Medical Research 2021, 28, 1–11. [Google Scholar] [CrossRef]
- de Mattos, L.H.L.; Yamada, A.L.M.; dos Santos, V.H.; Hussni, C.A.; Rodrigues, C.A.; Watanabe, M.J.; Alves, A.L.G. Treatment With Therapeutic Bandages to Control Equine Postarthroscopic Tibio-Patellofemoral Swelling. J. Equine Veter- Sci. 2017, 54, 87–92. [Google Scholar] [CrossRef]
- Practitioners, A.A.o.E. Guide for veterinary service and judging of equestrian events. 1991.
- Davidson, E.J. Controlled Exercise in Equine Rehabilitation. Veter- Clin. North Am. Equine Pr. 2016, 32, 159–165. [Google Scholar] [CrossRef]
- Gillis, C.L. Rehabilitation of tendon and ligament injuries. In Proceedings of the Proc Am Assoc Equine Pract; 1997; pp. 306–309. [Google Scholar]
- Kannus, P.; Jozsa, L.; Natri, A.; Järvinen, M. Effects of training, immobilization and remobilization on tendons. Scandinavian journal of medicine & science in sports 1997, 7, 67–71. [Google Scholar] [CrossRef]
- Sharma, P.; Maffulli, N. Tendon injury and tendinopathy: healing and repair. JBJS 2005, 87, 187–202. [Google Scholar] [CrossRef]
- Muñoz, A.; Saitua, A.; Becero, M.; Riber, C.; Satué, K.; de Medina, A.S.; Argüelles, D.; Castejón-Riber, C. The use of the water treadmill for the rehabilitation of musculoskeletal injuries in the sport horse. J. Veter- Res. 2019, 63, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Nankervis, K.; Tranquille, C.; McCrae, P.; York, J.; Lashley, M.; Baumann, M.; King, M.; Sykes, E.; Lambourn, J.; Miskimmin, K.-A.; et al. Consensus for the General Use of Equine Water Treadmills for Healthy Horses. Animals 2021, 11, 305. [Google Scholar] [CrossRef]
- King, M.R. Principles and Application of Hydrotherapy for Equine Athletes. Veter- Clin. North Am. Equine Pr. 2016, 32, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Kamioka, H.; Tsutani, K.; Okuizumi, H.; Mutoh, Y.; Ohta, M.; Handa, S.; Okada, S.; Kitayuguchi, J.; Kamada, M.; Shiozawa, N.; et al. Effectiveness of Aquatic Exercise and Balneotherapy: A Summary of Systematic Reviews Based on Randomized Controlled Trials of Water Immersion Therapies. J. Epidemiology 2010, 20, 2–12. [Google Scholar] [CrossRef]
- .
- Nankervis, K.J.; Launder, E.J.; Murray, R.C. The Use of Treadmills Within the Rehabilitation of Horses. J. Equine Veter- Sci. 2017, 53, 108–115. [Google Scholar] [CrossRef]
- Tranquille, C.A.; Tacey, J.B.; Walker, V.A.; Nankervis, K.J.; Murray, R.C. International survey of equine water treadmills—Why, when, and how? Journal of Equine Veterinary Science 2018, 69, 34–42. [Google Scholar] [CrossRef]
- Kaneps, A.J.; Beverly, M. THERAPEUTIC ULTRASOUND.
- Porter, M. Equine Rehabilitation Therapy for Joint Disease. Veter- Clin. North Am. Equine Pr. 2005, 21, 599–607. [Google Scholar] [CrossRef]
- Riegel, R.J.; Godbold Jr, J.C. Laser therapy in veterinary medicine: photobiomodulation; John Wiley & Sons: 2017.
- Riegel, R.J.; Godbold Jr, J.C. Fundamental information. Laser Therapy in Veterinary Medicine: Photobiomodulation 2017, 7-18.
- Heiskanen, V.; Hamblin, M.R. Photobiomodulation: lasers vs. light emitting diodes? Photochemical & Photobiological Sciences 2018, 17, 1003–1017. [Google Scholar] [CrossRef]
- Leotty, C.L.R.; Lima, M.M.C.; Araújo, F.X.d. Effect of low-level laser therapy on pain and function of patients with shoulder tendinopathy: A systematic review. Fisioterapia e Pesquisa 2020, 27, 210–217. [Google Scholar] [CrossRef]
- Kaub, L.; Schmitz, C. More than Ninety Percent of the Light Energy Emitted by Near-Infrared Laser Therapy Devices Used to Treat Musculoskeletal Disorders Is Absorbed within the First Ten Millimeters of Biological Tissue. Biomedicines 2022, 10, 3204. [Google Scholar] [CrossRef]
- Jadah, N.A.; Shamkhi, I.A. A comparative study of low-level laser efficacy on autologous activity of PRP injected in knee arthritis, in vivo study. Lasers Med Sci. 2021, 36, 357–363. [Google Scholar] [CrossRef]
- Lyu, K.; Liu, X.; Jiang, L.; Chen, Y.; Lu, J.; Zhu, B.; Liu, X.; Li, Y.; Wang, D.; Li, S. The Functions and Mechanisms of Low-Level Laser Therapy in Tendon Repair (Review). Front. Physiol. 2022, 13, 808374. [Google Scholar] [CrossRef]
- Wu, M.; Luan, L.; Pranata, A.; Witchalls, J.; Adams, R.; Bousie, J.; Han, J. Is high intensity laser therapy more effective than other physical therapy modalities for treating knee osteoarthritis? A systematic review and network meta-analysis. Front. Med. 2022, 9, 956188. [Google Scholar] [CrossRef] [PubMed]
- Berni, M.; Brancato, A.M.; Torriani, C.; Bina, V.; Annunziata, S.; Cornella, E.; Trucchi, M.; Jannelli, E.; Mosconi, M.; Gastaldi, G.; et al. The Role of Low-Level Laser Therapy in Bone Healing: Systematic Review. Int. J. Mol. Sci. 2023, 24, 7094. [Google Scholar] [CrossRef]
- He, K.; Zhou, X.; Zheng, F.; Ju, X.; Fu, S.-N.; Wong, A.Y.L. Histological, Physiological and Biomechanical Effects of Low-Level Laser Therapy on Tendon Healing in Animals and Humans: A Systematic Review. Ann. Biomed. Eng. 2023, 1–49. [Google Scholar] [CrossRef] [PubMed]
- Calatrava, I.R.; Valenzuela, J.M.S.; Gómez-Villamandos, R.J.; Redondo, J.I.; Gómez-Villamandos, J.C.; Jurado, I.A. Histological and clinical responses of articular cartilage to low-level laser therapy: Experimental study. Lasers Med Sci. 1997, 12, 117–121. [Google Scholar] [CrossRef]
- Jankaew, A.; You, Y.-L.; Yang, T.-H.; Chang, Y.-W.; Lin, C.-F. The effects of low-level laser therapy on muscle strength and functional outcomes in individuals with knee osteoarthritis: a double-blinded randomized controlled trial. Sci. Rep. 2023, 13, 165. [Google Scholar] [CrossRef] [PubMed]
- Wyszyńska, J.; Bal-Bocheńska, M. Efficacy of High-Intensity Laser Therapy in Treating Knee Osteoarthritis: A First Systematic Review. Photomed. Laser Surg. 2018, 36, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Angelova, A.; Ilieva, E.M. Effectiveness of High Intensity Laser Therapy for Reduction of Pain in Knee Osteoarthritis. Pain Res. Manag. 2016, 2016, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Stiglić-Rogoznica, N.; Stamenković, D.; Frlan-Vrgoc, L.; Avancini-Dobrović, V.; Vrbanić, T.S.-L. Analgesic effect of high intensity laser therapy in knee osteoarthritis. Coll. Antropol. 2011, 183–185. [Google Scholar]
- Riegel, R.J. Fundamentals of Equine Laser Therapy. Laser Therapy in Veterinary Medicine: Photobiomodulation 2017, 335-343.
- Auersperg, V.; Trieb, K. Extracorporeal shock wave therapy: an update. EFORT Open Rev. 2020, 5, 584–592. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-J. Extracorporeal shockwave therapy in musculoskeletal disorders. J. Orthop. Surg. Res. 2012, 7, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, A.N.; Tenforde, A.S.; Jelsing, E.J. Extracorporeal Shockwave Therapy in the Management of Sports Medicine Injuries. Optom. Vis. Sci. 2021, 20, 298–305. [Google Scholar] [CrossRef] [PubMed]
- Stania, M.; Juras, G.; Chmielewska, D.; Polak, A.; Kucio, C.; Król, P. Extracorporeal Shock Wave Therapy for Achilles Tendinopathy. BioMed Res. Int. 2019, 2019, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Ho, K.-D.; Yang, C.-L.; Lo, H.-Y.; Yeh, H.-J. Extracorporeal shockwave therapy with a modified technique on tendon and ligament for knee osteoarthritis: a randomized controlled trial. American Journal of Physical Medicine & Rehabilitation 2022, 101, 11–17. [Google Scholar] [CrossRef]
- Yocom, A.F.; Bass, L.D. Review of the application and efficacy of extracorporeal shockwave therapy in equine tendon and ligament injuries. Equine Veter- Educ. 2019, 31, 271–277. [Google Scholar] [CrossRef]
- Schmitz, C. Improving extracorporeal shock wave therapy with 904 or 905 nm pulsed, high power laser pretreatment. 2021.
- Schlachter, C.; Lewis, C. Electrophysical Therapies for the Equine Athlete. Veter- Clin. North Am. Equine Pr. 2016, 32, 127–147. [Google Scholar] [CrossRef]
- Schils, S.J. Review of electrotherapy devices for use in veterinary medicine. In Proceedings of the Proceedings of the 55th Annual Convention of the American Association of Equine Practitioners, Las Vegas, NV, 2009; pp. 68–73.
- Hyytiäinen, H.K.; Boström, A.; Asplund, K.; Bergh, A. A Systematic Review of Complementary and Alternative Veterinary Medicine in Sport and Companion Animals: Electrotherapy. Animals 2022, 13, 64. [Google Scholar] [CrossRef]
- Lucas, R.G.; Rodríguez-Hurtado, I.; Álvarez, C.T.; Ortiz, G. Effectiveness of Neuromuscular Electrical Stimulation and Dynamic Mobilization Exercises on Equine Multifidus Muscle Cross-Sectional Area. J. Equine Veter- Sci. 2022, 113, 103934. [Google Scholar] [CrossRef]
- Buchner, H.H.F.; Zimmer, L.; Haase, L.; Perrier, J.; Peham, C. Effects of Whole Body Vibration on the Horse: Actual Vibration, Muscle Activity, and Warm-up Effect. J. Equine Veter- Sci. 2017, 51, 54–60. [Google Scholar] [CrossRef]
- Nowlin, C.; Nielsen, B.; Mills, J.; Robison, C.; Schott, H.; Peters, D. Acute and Prolonged Effects of Vibrating Platform Treatment on Horses: A Pilot Study. J. Equine Veter- Sci. 2018, 62, 116–122. [Google Scholar] [CrossRef]
- Sugg, S.J. Effects of Whole Body Vibration on Lameness, Stride Length, Cortisol, and Other Parameters in Healthy Horses. Middle Tennessee State University, 2018.
- Khan, K.M.; Cook, J.L.; Bonar, F.; Harcourt, P.; Åstrom, M. Histopathology of common tendinopathies: update and implications for clinical management. Sports medicine 1999, 27, 393–408. [Google Scholar] [CrossRef]
- Sass, F.A.; Fuchs, M.; Pumberger, M.; Geissler, S.; Duda, G.N.; Perka, C.; Schmidt-Bleek, K. Immunology guides skeletal muscle regeneration. International journal of molecular sciences 2018, 19, 835. [Google Scholar] [CrossRef]
- Coombes, B.K.; Bisset, L.; Vicenzino, B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet 2010, 376, 1751–1767. [Google Scholar] [CrossRef]
- Lin, M.-T.; Chiang, C.-F.; Wu, C.-H.; Huang, Y.-T.; Tu, Y.-K.; Wang, T.-G. Comparative Effectiveness of Injection Therapies in Rotator Cuff Tendinopathy: A Systematic Review, Pairwise and Network Meta-analysis of Randomized Controlled Trials. Arch. Phys. Med. Rehabilitation 2018, 100, 336–349. [Google Scholar] [CrossRef]
- Everhart, J.S.; Cole, D.; Sojka, J.H.; Higgins, J.D.; Magnussen, R.A.; Schmitt, L.C.; Flanigan, D.C. Treatment Options for Patellar Tendinopathy: A Systematic Review. Arthrosc. J. Arthrosc. Relat. Surg. 2017, 33, 861–872. [Google Scholar] [CrossRef]
- da Costa, B.R.; Hari, R.; Jüni, P. Intra-articular Corticosteroids for Osteoarthritis of the Knee. JAMA 2016, 316, 2671–2672. [Google Scholar] [CrossRef]
- Bellamy, N.; Campbell, J.; Welch, V.; Gee, T.L.; Bourne, R.; Wells, G.A. Intraarticular corticosteroid for treatment of osteoarthritis of the knee. Cochrane Database of Systematic Reviews 2006. [CrossRef]
- Shanley, L.C.; Mahon, O.R.; Kelly, D.J.; Dunne, A. Harnessing the innate and adaptive immune system for tissue repair and regeneration: Considering more than macrophages. Acta Biomater. 2021, 133, 208–221. [Google Scholar] [CrossRef]
- Arvind, V.; Huang, A.H. Reparative and Maladaptive Inflammation in Tendon Healing. Front. Bioeng. Biotechnol. 2021, 9. [Google Scholar] [CrossRef]
- Oliva, F.; Marsilio, E.; Asparago, G.; Frizziero, A.; Berardi, A.C.; Maffulli, N. The Impact of Hyaluronic Acid on Tendon Physiology and Its Clinical Application in Tendinopathies. Cells 2021, 10, 3081. [Google Scholar] [CrossRef]
- Lo, G.H.; LaValley, M.; McAlindon, T.; Felson, D.T. Intra-articular hyaluronic acid in treatment of knee osteoarthritis: a meta-analysis. Jama 2003, 290, 3115–3121. [Google Scholar] [CrossRef]
- Han, S.-B.; Seo, I.-W.; Shin, Y.-S. Intra-Articular Injections of Hyaluronic Acid or Steroids Associated With Better Outcomes Than Platelet-Rich Plasma, Adipose Mesenchymal Stromal Cells, or Placebo in Knee Osteoarthritis: A Network Meta-analysis. Arthrosc. J. Arthrosc. Relat. Surg. 2021, 37, 292–306. [Google Scholar] [CrossRef] [PubMed]
- Bowman, S.; Awad, M.E.; Hamrick, M.W.; Hunter, M.; Fulzele, S. Recent advances in hyaluronic acid based therapy for osteoarthritis. Clin. Transl. Med. 2018, 7, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kaux, J.-F.; Samson, A.; Crielaard, J.-M. Hyaluronic acid and tendon lesions. Muscles, ligaments and tendons journal 2015, 5, 264. [Google Scholar] [CrossRef] [PubMed]
- Agostini, F.; de Sire, A.; Paoloni, M.; Finamore, N.; Ammendolia, A.; Mangone, M.; Bernetti, A. Effects of hyaluronic acid injections on pain and functioning in patients affected by tendinopathies: A narrative review. J. Back Musculoskelet. Rehabilitation 2022, 35, 949–961. [Google Scholar] [CrossRef]
- Ning, C.; Li, P.; Gao, C.; Fu, L.; Liao, Z.; Tian, G.; Yin, H.; Li, M.; Sui, X.; Yuan, Z.; et al. Recent advances in tendon tissue engineering strategy. Front. Bioeng. Biotechnol. 2023, 11, 1115312. [Google Scholar] [CrossRef]
- Bannuru, R.; Natov, N.; Dasi, U.; Schmid, C.; McAlindon, T. Therapeutic trajectory following intra-articular hyaluronic acid injection in knee osteoarthritis – meta-analysis. Osteoarthr. Cartil. 2011, 19, 611–619. [Google Scholar] [CrossRef]
- Strauss, E.J.; Hart, J.A.; Miller, M.D.; Altman, R.D.; Rosen, J.E. Hyaluronic acid viscosupplementation and osteoarthritis: current uses and future directions. The American journal of sports medicine 2009, 37, 1636–1644. [Google Scholar] [CrossRef]
- Xavier, A.A.d.S.; da Rosa, P.P.; Mackmill, L.d.B.; Roll, V.F.B. An assessment of the effectiveness of hyaluronic acid and polyacrylamide hydrogel in horses with osteoarthritis: Systematic review and network meta-analysis. Res. Veter- Sci. 2021, 134, 42–50. [Google Scholar] [CrossRef]
- Henrotin, Y.; Raman, R.; Richette, P.; Bard, H.; Jerosch, J.; Conrozier, T.; Chevalier, X.; Migliore, A. Consensus statement on viscosupplementation with hyaluronic acid for the management of osteoarthritis. Semin. Arthritis Rheum. 2015, 45, 140–149. [Google Scholar] [CrossRef]
- Cooper, C.; Rannou, F.; Richette, P.; Bruyère, O.; Al-Daghri, N.; Altman, R.D.; Brandi, M.L.; Basset, S.C.; Herrero-Beaumont, G.; Migliore, A.; et al. Use of Intraarticular Hyaluronic Acid in the Management of Knee Osteoarthritis in Clinical Practice. Arthritis Care Res. 2017, 69, 1287–1296. [Google Scholar] [CrossRef]
- Rydell, N.W.; Butler, J.; Balazs, E.A. yaluronic acid in synovial fluid: VI. Effect of intra-articular injection of hyaluronic acid on the clinical symptoms of arthritis in track horses. Acta Veterinaria Scandinavica 1970, 11, 139. [Google Scholar] [CrossRef]
- Chen, Z.; Wang, C.; You, D.; Zhao, S.; Zhu, Z.; Xu, M. Platelet-rich plasma versus hyaluronic acid in the treatment of knee osteoarthritis: A meta-analysis. Medicine 2020, 99. [Google Scholar] [CrossRef]
- Derwich, M.; Mitus-Kenig, M.; Pawlowska, E. Mechanisms of Action and Efficacy of Hyaluronic Acid, Corticosteroids and Platelet-Rich Plasma in the Treatment of Temporomandibular Joint Osteoarthritis—A Systematic Review. Int. J. Mol. Sci. 2021, 22, 7405. [Google Scholar] [CrossRef]
- Zhao, J.; Huang, H.; Liang, G.; Zeng, L.-F.; Yang, W.; Liu, J. Effects and safety of the combination of platelet-rich plasma (PRP) and hyaluronic acid (HA) in the treatment of knee osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet. Disord. 2020, 21, 1–12. [Google Scholar] [CrossRef]
- Xu, Z.; He, Z.; Shu, L.; Li, X.; Ma, M.; Ye, C. Intra-Articular Platelet-Rich Plasma Combined With Hyaluronic Acid Injection for Knee Osteoarthritis Is Superior to Platelet-Rich Plasma or Hyaluronic Acid Alone in Inhibiting Inflammation and Improving Pain and Function. Arthrosc. J. Arthrosc. Relat. Surg. 2021, 37, 903–915. [Google Scholar] [CrossRef]
- Dovedytis, M.; Liu, Z.J.; Bartlett, S. Hyaluronic acid and its biomedical applications: A review. Eng. Regen. 2020, 1, 102–113. [Google Scholar] [CrossRef]
- Galarraga, J.H.; Locke, R.C.; E Witherel, C.; Stoeckl, B.D.; Castilho, M.; Mauck, R.L.; Malda, J.; Levato, R.; A Burdick, J. Fabrication of MSC-laden composites of hyaluronic acid hydrogels reinforced with MEW scaffolds for cartilage repair. Biofabrication 2021, 14, 014106. [Google Scholar] [CrossRef] [PubMed]
- Matas, J.; Orrego, M.; Amenabar, D.; Infante, C.; Tapia-Limonchi, R.; Cadiz, M.I.; Alcayaga-Miranda, F.; González, P.L.; Muse, E.; Khoury, M.; et al. Umbilical Cord-Derived Mesenchymal Stromal Cells (MSCs) for Knee Osteoarthritis: Repeated MSC Dosing Is Superior to a Single MSC Dose and to Hyaluronic Acid in a Controlled Randomized Phase I/II Trial. Stem Cells Transl. Med. 2019, 8, 215–224. [Google Scholar] [CrossRef]
- Yang, Y.; Zhu, Z.; Gao, R.; Yuan, J.; Zhang, J.; Li, H.; Xie, Z.; Wang, Y. Controlled release of MSC-derived small extracellular vesicles by an injectable Diels-Alder crosslinked hyaluronic acid/PEG hydrogel for osteoarthritis improvement. Acta Biomater. 2021, 128, 163–174. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhao, X.; Xu, H.; Xing, Y.; Wu, T.; Sun, X.; Kuang, M.; Ma, X.; Liu, W.; Yang, Q. Wharton's jelly MSC-derived extracellular vehicles—loaded hyaluronic acid-alginate adhesives for treatment of osteoarthritis. J. Mater. Sci. Technol. 2023, 142, 240–252. [Google Scholar] [CrossRef]
- Shekhter, A.B.; Zar, V.V.; Voloshin, V.P.; Lopatin, V.V. issue and cell reaction of the synovial media to intraarticular injection of polymer viscoprosthesis “Noltrex” in experimental conditions. Alm. Clin. Med. 2016, 20–24. [Google Scholar] [CrossRef]
- Christensen, L.; Camitz, L.; Illigen, K.; Hansen, M.; Sarvaa, R.; Conaghan, P. Synovial incorporation of polyacrylamide hydrogel after injection into normal and osteoarthritic animal joints. Osteoarthr. Cartil. 2016, 24, 1999–2002. [Google Scholar] [CrossRef]
- Tnibar, A.; Persson, A.; Jensen, H. Mechanisms of action of an intraarticular 2.5% polyacrylamide hydrogel (Arthramid Vet) in a goat model of osteoarthritis: preliminary observations. SM Journal of Biomedical Engineering 2017, 3, 1022. [Google Scholar]
- Moreau, M.; Rialland, P.; Pelletier, J.-P.; Martel-Pelletier, J.; Lajeunesse, D.; Boileau, C.; Caron, J.; Frank, D.; Lussier, B.; del Castillo, J.R.; et al. Tiludronate treatment improves structural changes and symptoms of osteoarthritis in the canine anterior cruciate ligament model. Arthritis Res. Ther. 2011, 13, R98. [Google Scholar] [CrossRef]
- Fan, T.M.; de Lorimier, L.P.; Charney, S.C.; Hintermeister, J.G. Evaluation of intravenous pamidronate administration in 33 cancer-bearing dogs with primary or secondary bone involvement. Journal of veterinary internal medicine 2005, 19, 74–80. [Google Scholar]
- Richbourg, H.A.; Mitchell, C.F.; Gillett, A.N.; McNulty, M.A. Tiludronate and clodronate do not affect bone structure or remodeling kinetics over a 60 day randomized trial. BMC Veter- Res. 2018, 14, 1–11. [Google Scholar] [CrossRef]
- Tischmacher, A.; Wilford, S.; Allen, K.; Mitchell, R.D.; Parkin, T.; Denoix, J.-M. Retrospective Analysis of the Use of Tiludronate in Equine Practice: Safety on 1804 Horses, Efficacy on 343 Horses. J. Equine Veter- Sci. 2022, 115, 104007. [Google Scholar] [CrossRef]
- Story, M.R.; Haussler, K.K.; Nout-Lomas, Y.S.; Aboellail, T.A.; Kawcak, C.E.; Barrett, M.F.; Frisbie, D.D.; McIlwraith, C.W. Equine Cervical Pain and Dysfunction: Pathology, Diagnosis and Treatment. Animals 2021, 11, 422. [Google Scholar] [CrossRef]
- Denoix, J. .; Thibaud, D.; Riccio, B. Tiludronate as a new therapeutic agent in the treatment of navicular disease: a double-blind placebo-controlled clinical trial. Equine Veter- J. 2003, 35, 407–413. [Google Scholar] [CrossRef]
- Yocom, A.; Contino, E.; Kawcak, C. Review of the Mechanism of Action and Use of Bisphosphonates in Horses. J. Equine Veter- Sci. 2023, 127, 104503. [Google Scholar] [CrossRef]
- Argüelles, D.; Saitua, A.; de Medina, A.S.; Muñoz, J.A.; Muñoz, A. Clinical efficacy of clodronic acid in horses diagnosed with navicular syndrome: A field study using objective and subjective lameness evaluation. Res. Veter- Sci. 2019, 125, 298–304. [Google Scholar] [CrossRef]
- Osborn, M.L.; Cornille, J.L.; Blas-Machado, U.; Uhl, E.W. The equine navicular apparatus as a premier enthesis organ: Functional implications. Veter- Surg. 2021, 50, 713–728. [Google Scholar] [CrossRef]
- Gough, M.R.; Thibaud, D.; Smith, R.K.W. Tiludronate infusion in the treatment of bone spavin: A double blind placebo-controlled trial. Equine Veter- J. 2010, 42, 381–387. [Google Scholar] [CrossRef]
- Dubuc, J. Distal tarsal joints osteoarthritis: Evidence behind bisphosphonates and NSAIDs to improve lameness. Veter- Évid. 2020, 5. [Google Scholar] [CrossRef]
- Soto, S.A.; Barbará, A.C. Bisphosphonates: Pharmacology and Clinical Approach to Their Use in Equine Osteoarticular Diseases. J. Equine Veter- Sci. 2014, 34, 727–737. [Google Scholar] [CrossRef]
- Bertuglia, A.; Basano, I.; Pagliara, E.; Bottegaro, N.B.; Spinella, G.; Bullone, M. Effect of intravenous tiludronate disodium administration on the radiographic progression of osteoarthritis of the fetlock joint in Standardbred racehorses. J. Am. Veter- Med Assoc. 2021, 259, 651–661. [Google Scholar] [CrossRef] [PubMed]
- Vergara-Hernandez, F.B.; Nielsen, B.D.; Colbath, A.C. Is the Use of Bisphosphonates Putting Horses at Risk? An Osteoclast Perspective. Animals 2022, 12, 1722. [Google Scholar] [CrossRef] [PubMed]
- Suva, L.J.; Cooper, A.; Watts, A.E.; Ebetino, F.H.; Price, J.; Gaddy, D. Bisphosphonates in veterinary medicine: The new horizon for use. Bone 2020, 142, 115711. [Google Scholar] [CrossRef]
- Mitchell, A.; Watts, A.E.; Ebetino, F.H.; Suva, L.J. Bisphosphonate use in the horse: what is good and what is not? BMC veterinary research 2019, 15, 1–7. [Google Scholar] [CrossRef]
- Knych, H.K.; Finno, C.J.; Katzman, S.; Ryan, D.; McKemie, D.S.; Kass, P.H.; Arthur, R.M. Clodronate detection and effects on markers of bone resorption are prolonged following a single administration to horses. Equine Veter- J. 2023, 55, 696–706. [Google Scholar] [CrossRef]
- Mama, K.R.; Hector, R.C. Therapeutic developments in equine pain management. Veter- J. 2019, 247, 50–56. [Google Scholar] [CrossRef]
- Krueger, C.R.; Mitchell, C.F.; Leise, B.S.; Knych, H.K. Pharmacokinetics and pharmacodynamics of clodronate disodium evaluated in plasma, synovial fluid and urine. Equine Veter- J. 2020, 52, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Delguste, C.; Amory, H.; Doucet, M.; Piccot-Crézollet, C.; Thibaud, D.; Garnero, P.; Detilleux, J.; Lepage, O. Pharmacological effects of tiludronate in horses after long-term immobilization. Bone 2007, 41, 414–421. [Google Scholar] [CrossRef]
- Kamm, L.; McIlwraith, W.; Kawcak, C. A Review of the Efficacy of Tiludronate in the Horse. J. Equine Veter- Sci. 2008, 28, 209–214. [Google Scholar] [CrossRef]
- Knych, H.K.; Janes, J.; Kennedy, L.; McKemie, D.S.; Arthur, R.M.; Samol, M.A.; Uzal, F.A.; Scollay, M. Detection and residence time of bisphosphonates in bone of horses. J. Veter- Diagn. Investig. 2022, 34, 23–27. [Google Scholar] [CrossRef]
- Ortved, K.F. Regenerative Medicine and Rehabilitation for Tendinous and Ligamentous Injuries in Sport Horses. Veter- Clin. North Am. Equine Pr. 2018, 34, 359–373. [Google Scholar] [CrossRef]
- Fortier, L.A.; Smith, R.K. Regenerative Medicine for Tendinous and Ligamentous Injuries of Sport Horses. Veter- Clin. North Am. Equine Pr. 2008, 24, 191–201. [Google Scholar] [CrossRef]
- Godek, P. Regenerative Medicine and Cell Biology. Regen Med 2022, 1, 1. [Google Scholar]
- Fukuda, K.; Kuwano, A.; Kuroda, T.; Tamura, N.; Mita, H.; Okada, Y.; Kasashima, Y. Optimal double-spin method for maximizing the concentration of platelets in equine platelet-rich plasma. J. Equine Sci. 2020, 31, 105–111. [Google Scholar] [CrossRef]
- Garbin, L.C.; Olver, C.S. Platelet-Rich Products and Their Application to Osteoarthritis. J. Equine Veter- Sci. 2020, 86, 102820. [Google Scholar] [CrossRef]
- Garbin, L.C.; Contino, E.K.; Olver, C.S.; Frisbie, D.D. A safety evaluation of allogeneic freeze-dried platelet-rich plasma or conditioned serum compared to autologous frozen products equivalents in equine healthy joints. BMC Veter- Res. 2022, 18, 141. [Google Scholar] [CrossRef]
- Everts, P.; Onishi, K.; Jayaram, P.; Lana, J.F.; Mautner, K. Platelet-Rich Plasma: New Performance Understandings and Therapeutic Considerations in 2020. Int. J. Mol. Sci. 2020, 21, 7794. [Google Scholar] [CrossRef]
- Marques-Smith, P.; Kallerud, A.S.; Johansen, G.M.; Boysen, P.; Jacobsen, A.M.; Reitan, K.M.; Henriksen, M.M.; Löfgren, M.; Fjordbakk, C.T. Is clinical effect of autologous conditioned serum in spontaneously occurring equine articular lameness related to ACS cytokine profile? BMC veterinary research 2020, 16, 1–9. [Google Scholar] [CrossRef]
- Geburek, F.; Lietzau, M.; Beineke, A.; Rohn, K.; Stadler, P.M. Effect of a single injection of autologous conditioned serum (ACS) on tendon healing in equine naturally occurring tendinopathies. Stem Cell Res. Ther. 2015, 6, 1–14. [Google Scholar] [CrossRef]
- Genc, E.; Yuksel, S.; Caglar, A.; Beytemur, O.; Gulec, M.A. Comparison on effects of platelet-rich plasma versus autologous conditioned serum on Achilles tendon healing in a rat model. Acta Orthop. et Traumatol. Turc. 2020, 54, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Fjordbakk, C.T.; Johansen, G.M.; Løvås, A.C.; Oppegård, K.L.; Storset, A.K. Surgical stress influences cytokine content in autologous conditioned serum. Equine Veter- J. 2015, 47, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Stashak, T.S. Adams’ lameness in horses; Verlag M. & H. Schaper: 2008.
- Clegg, P. Differential diagnosis of a swollen hock in the horse. Pr. 2003, 25, 328–341. [Google Scholar] [CrossRef]
- Kümmerle, J.M.; Kummer, M.R. Arthroscopically Accessible Anatomy of the Tarsal Collateral Ligaments in the Horse. Veter- Surg. 2013, 42, 267–274. [Google Scholar] [CrossRef]
- Jindal, K.; Patel, S.; Dhillon, M. The future of injectable orthobiologic substances for knee osteoarthritis: Options beyond platelet-rich plasma. J. Musculoskelet. Surg. Res. 2020, 4, 173. [Google Scholar] [CrossRef]
- Kaneps, A.J. A one-health perspective: use of hemoderivative regenerative therapies in canine and equine patients. J. Am. Veter- Med Assoc. 2023, 261, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Linardi, R.L.; Dodson, M.E.; Moss, K.L.; King, W.J.; Ortved, K.F. The Effect of Autologous Protein Solution on the Inflammatory Cascade in Stimulated Equine Chondrocytes. Front. Veter- Sci. 2019, 6, 64. [Google Scholar] [CrossRef]
- Garbin, L.C.; Morris, M.J. A Comparative Review of Autologous Conditioned Serum and Autologous Protein Solution for Treatment of Osteoarthritis in Horses. Front. Veter- Sci. 2021, 8. [Google Scholar] [CrossRef]
- Soontararak, S.; Ardaum, P.; Senarat, N.; Yangtara, S.; Lekcharoensuk, C.; Putchong, I.; Kashemsant, N.; Vijarnsorn, M.; Chow, L.; Dow, S.; et al. In Vitro Anti-Inflammatory and Regenerative Effects of Autologous Conditioned Serum from Dogs with Osteoarthritis. Animals 2022, 12, 2717. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, E.; Ruggeri, M.; Rossi, S.; Vigani, B.; Miele, D.; Bonferoni, M.C.; Sandri, G.; Ferrari, F. Innovative Strategies in Tendon Tissue Engineering. Pharmaceutics 2021, 13, 89. [Google Scholar] [CrossRef] [PubMed]
- Gaesser, A.M.; Underwood, C.; Linardi, R.L.; Even, K.M.; Reef, V.B.; Shetye, S.S.; Mauck, R.L.; King, W.J.; Engiles, J.B.; Ortved, K.F. Evaluation of Autologous Protein Solution Injection for Treatment of Superficial Digital Flexor Tendonitis in an Equine Model. Front. Veter- Sci. 2021, 8. [Google Scholar] [CrossRef]
- Geburek, F.; Gaus, M.; van Schie, H.T.M.; Rohn, K.; Stadler, P.M. Effect of intralesional platelet-rich plasma (PRP) treatment on clinical and ultrasonographic parameters in equine naturally occurring superficial digital flexor tendinopathies – a randomized prospective controlled clinical trial. BMC Veter- Res. 2016, 12, 1–16. [Google Scholar] [CrossRef]
- Peng, C.; Yang, L.; Labens, R.; Gao, Y.; Zhu, Y.; Li, J. A systematic review and meta-analysis of the efficacy of platelet-rich plasma products for treatment of equine joint disease. Equine Veter- J. 2024. [Google Scholar] [CrossRef]
- Abu-Seida, A.M. Regenerative Therapy for Equine Osteoarthritis: A Concise Review. Asian J. Anim. Veter- Adv. 2015, 10, 500–508. [Google Scholar] [CrossRef]
- Pereira, R.C.d.F.; De La Côrte, F.D.; Brass, K.E.; Azevedo, M.d.S.; Gallio, M.; Cantarelli, C.; Dau, S.L.; Cezar, A.S.; Inkelmann, M.A. Evaluation of Three Methods of Platelet-Rich Plasma for Treatment of Equine Distal Limb Skin Wounds. J. Equine Veter- Sci. 2019, 72, 1–7. [Google Scholar] [CrossRef]
- Gottschall, J.; Johnston, V.L.; Rzad, L.; Anderson, A.J.; Aster, R. Importance of white blood cells in platelet storage. Vox sanguinis 1984, 47, 101–107. [Google Scholar] [CrossRef]
- E Giraldo, C.; López, C.; E Álvarez, M.; Samudio, I.J.; Prades, M.; Carmona, J.U. Effects of the breed, sex and age on cellular content and growth factor release from equine pure-platelet rich plasma and pure-platelet rich gel. BMC Veter- Res. 2013, 9, 1–10. [Google Scholar] [CrossRef]
- McCarrel, T.M. Equine Platelet-Rich Plasma. Veterinary Clinics: Equine Practice 2023, 39, 429–442. [Google Scholar] [CrossRef]
- Garbin, L.C.; Lopez, C.; Carmona, J.U. A Critical Overview of the Use of Platelet-Rich Plasma in Equine Medicine Over the Last Decade. Front. Veter- Sci. 2021, 8. [Google Scholar] [CrossRef]
- Bosch, G.; van Schie, H.T.; de Groot, M.W.; Cadby, J.A.; van de Lest, C.H.; Barneveld, A.; van Weeren, P.R. Effects of platelet-rich plasma on the quality of repair of mechanically induced core lesions in equine superficial digital flexor tendons: a placebo-controlled experimental study. Journal of orthopaedic research 2010, 28, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Bosch, G.; Moleman, M.; Barneveld, A.; van Weeren, P.R.; van Schie, H.T.M. The effect of platelet-rich plasma on the neovascularization of surgically created equine superficial digital flexor tendon lesions. Scand. J. Med. Sci. Sports 2011, 21, 554–561. [Google Scholar] [CrossRef] [PubMed]
- Santangelo, K.; Nuovo, G.; Bertone, A. In vivo reduction or blockade of interleukin-1β in primary osteoarthritis influences expression of mediators implicated in pathogenesis. Osteoarthr. Cartil. 2012, 20, 1610–1618. [Google Scholar] [CrossRef] [PubMed]
- Hopper, S.A. Regenerative Medicine–Under-standing IRAP, PRP and stem cell Therapies. Rood and Riddle 2015.
- Crawford, D.C.; Miller, L.E.; Block, J.E. Conservative management of symptomatic knee osteoarthritis: a flawed strategy? Orthopedic reviews 2013, 5. [Google Scholar]
- Rönn, K.; Reischl, N.; Gautier, E.; Jacobi, M. Current Surgical Treatment of Knee Osteoarthritis. Arthritis 2011, 2011, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Genç, E.; Beytemur, O.; Yuksel, S.; Eren, Y.; Çağlar, A.; Küçükyıldırım, B.O.; Güleç, M.A. Investigation of the biomechanical and histopathological effects of autologous conditioned serum on healing of Achilles tendon. Acta Orthop. et Traumatol. Turc. 2018, 52, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Bertone, A.L.; Ishihara, A.; Zekas, L.J.; Wellman, M.L.; Lewis, K.B.; Schwarze, R.A.; Barnaba, A.R.; Schmall, M.L.; Kanter, P.M.; Genovese, R.L. Evaluation of a single intra-articular injection of autologous protein solution for treatment of osteoarthritis in horses. Am. J. Vet. Res. 2014, 75, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Ortved, K.F. Equine Autologous Conditioned Serum and Autologous Protein Solution. Veter- Clin. North Am. Equine Pr. 2023, 39, 443–451. [Google Scholar] [CrossRef]
- Knott, L.E.; Fonseca-Martinez, B.A.; O'Connor, A.M.; Goodrich, L.R.; McIlwraith, C.W.; Colbath, A.C. Current use of biologic therapies for musculoskeletal disease: A survey of board-certified equine specialists. Veter- Surg. 2022, 51, 557–567. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, A.V.; Boone, L.H.; Braim, A.P.; Taintor, J.S.; Caldwell, F.; Wright, J.C.; Wooldridge, A.A. A Survey of Clinical Usage of Non-steroidal Intra-Articular Therapeutics by Equine Practitioners. Front. Veter- Sci. 2020, 7, 579967. [Google Scholar] [CrossRef]
- Wang, S.; Wei, X.; Zhou, J.; Zhang, J.; Li, K.; Chen, Q.; Terek, R.; Fleming, B.C.; Goldring, M.B.; Ehrlich, M.G. Identification of α2-macroglobulin as a master inhibitor of cartilage-degrading factors that attenuates the progression of posttraumatic osteoarthritis. Arthritis & rheumatology 2014, 66, 1843–1853. [Google Scholar] [CrossRef]
- Zhu, M.; Zhao, B.; Wei, L.; Wang, S. alpha-2-Macroglobulin, a Native and Powerful Proteinase Inhibitor, Prevents Cartilage Degeneration Disease by Inhibiting Majority of Catabolic Enzymes and Cytokines. Curr. Mol. Biol. Rep. 2021, 7, 1–7. [Google Scholar] [CrossRef]
- Li, S.; Xiang, C.; Wei, X.; Sun, X.; Li, R.; Li, P.; Sun, J.; Wei, D.; Chen, Y.; Zhang, Y.; et al. Early supplemental α2-macroglobulin attenuates cartilage and bone damage by inhibiting inflammation in collagen II-induced arthritis model. Int. J. Rheum. Dis. 2019, 22, 654–665. [Google Scholar] [CrossRef]
- Szponder, T.; Latalski, M.; Danielewicz, A.; Krać, K.; Kozera, A.; Drzewiecka, B.; Nguyen Ngoc, D.; Dobko, D.; Wessely-Szponder, J. Osteoarthritis: pathogenesis, animal models, and new regenerative therapies. Journal of Clinical Medicine 2022, 12, 5. [Google Scholar] [CrossRef]
- Velloso Alvarez, A.; Boone, L.H.; Pondugula, S.R.; Caldwell, F.; Wooldridge, A.A. Effects of autologous conditioned serum, autologous protein solution, and triamcinolone on inflammatory and catabolic gene expression in equine cartilage and synovial explants treated with IL-1β in co-culture. Frontiers in veterinary science 2020, 7, 323. [Google Scholar] [CrossRef]
- Tokawa, P.K.A.; Brossi, P.M.; Baccarin, R.Y.A. Autologous conditioned serum in equine and human orthopedic therapy: A systematic review. Res. Veter- Sci. 2022, 146, 34–52. [Google Scholar] [CrossRef] [PubMed]
- Hraha, T.H.; Doremus, K.M.; McILWRAITH, C.W.; Frisbie, D.D. Autologous conditioned serum: The comparative cytokine profiles of two commercial methods (IRAP and IRAP II) using equine blood. Equine Veter- J. 2011, 43, 516–521. [Google Scholar] [CrossRef]
- Lasarzik, J.; Bondzio, A.; Rettig, M.; Estrada, R.; Klaus, C.; Ehrle, A.; Einspanier, R.; Lischer, C.J. Evaluation of Two Protocols Using Autologous Conditioned Serum for Intra-articular Therapy of Equine Osteoarthritis—A Pilot Study Monitoring Cytokines and Cartilage-Specific Biomarkers. J. Equine Veter- Sci. 2018, 60, 35–42. [Google Scholar] [CrossRef]
- Voga, M.; Adamic, N.; Vengust, M.; Majdic, G. Stem Cells in Veterinary Medicine—Current State and Treatment Options. Front. Veter- Sci. 2020, 7, 278. [Google Scholar] [CrossRef]
- Prockop, D.J.; Oh, J.Y. Medical therapies with adult stem/progenitor cells (MSCs): A backward journey from dramatic results in vivo to the cellular and molecular explanations. J. Cell. Biochem. 2012, 113, 1460–1469. [Google Scholar] [CrossRef] [PubMed]
- Caplan, A.I. Mesenchymal stem cells: time to change the name! Stem cells translational medicine 2017, 6, 1445–1451. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.-C.; Kim, H.-S.; Shin, T.-H.; Kang, I.; Lee, J.Y.; Kim, J.-J.; Kang, H.K.; Seo, Y.; Lee, S.; Yu, K.-R.; et al. PGE2 maintains self-renewal of human adult stem cells via EP2-mediated autocrine signaling and its production is regulated by cell-to-cell contact. Sci. Rep. 2016, 6, 26298. [Google Scholar] [CrossRef]
- Margiana, R.; Markov, A.; Zekiy, A.O.; Hamza, M.U.; Al-Dabbagh, K.A.; Al-Zubaidi, S.H.; Hameed, N.M.; Ahmad, I.; Sivaraman, R.; Kzar, H.H.; et al. Clinical application of mesenchymal stem cell in regenerative medicine: a narrative review. Stem Cell Res. Ther. 2022, 13, 1–22. [Google Scholar] [CrossRef]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.C.; Krause, D.S.; Deans, R.J.; Keating, A.; Prockop, D.J.; Horwitz, E.M. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef]
- Vizoso, F.J.; Eiro, N.; Cid, S.; Schneider, J.; Perez-Fernandez, R. Mesenchymal Stem Cell Secretome: Toward Cell-Free Therapeutic Strategies in Regenerative Medicine. Int. J. Mol. Sci. 2017, 18, 1852. [Google Scholar] [CrossRef]
- Reis, I.L.; Lopes, B.; Sousa, P.; Sousa, A.C.; Branquinho, M.; Caseiro, A.R.; Pedrosa, S.S.; Rêma, A.; Oliveira, C.; Porto, B.; et al. Allogenic Synovia-Derived Mesenchymal Stem Cells for Treatment of Equine Tendinopathies and Desmopathies—Proof of Concept. Animals 2023, 13, 1312. [Google Scholar] [CrossRef]
- Colbath, A.C.; Dow, S.W.; Phillips, J.N.; McIlwraith, C.W.; Goodrich, L.R. Autologous and Allogeneic Equine Mesenchymal Stem Cells Exhibit Equivalent Immunomodulatory Properties In Vitro. Stem Cells Dev. 2017, 26, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Reis, I.L.; Lopes, B.; Sousa, P.; Sousa, A.C.; Branquinho, M.V.; Caseiro, A.R.; Rêma, A.; Briote, I.; Mendonça, C.M.; Santos, J.M.; et al. Treatment of Equine Tarsus Long Medial Collateral Ligament Desmitis with Allogenic Synovial Membrane Mesenchymal Stem/Stromal Cells Enhanced by Umbilical Cord Mesenchymal Stem/Stromal Cell-Derived Conditioned Medium: Proof of Concept. Animals 2024, 14, 370. [Google Scholar] [CrossRef] [PubMed]
- Reis, I.; Lopes, B.; Sousa, P.; Sousa, A.; Caseiro, A.R.; Briote, I.; Rocha, A.M.; Pereira, J.; Mendonça, C.; Santos, J. Equine Metacarpophalangeal Joint Partial and Full Thickness Defects Treated with Allogenic Equine Synovial Membrane Mesenchymal Stem/Stromal Cell and Umbilical Cord Mesenchymal Stem/Stromal Cell Conditioned Medium: The Proof-of-Concept. 2024.
- Iijima, H.; Isho, T.; Kuroki, H.; Takahashi, M.; Aoyama, T. Effectiveness of mesenchymal stem cells for treating patients with knee osteoarthritis: a meta-analysis toward the establishment of effective regenerative rehabilitation. npj Regen. Med. 2018, 3, 15. [Google Scholar] [CrossRef] [PubMed]
- Richardson, S.M.; Kalamegam, G.; Pushparaj, P.N.; Matta, C.; Memic, A.; Khademhosseini, A.; Mobasheri, R.; Poletti, F.L.; Hoyland, J.A.; Mobasheri, A. Mesenchymal stem cells in regenerative medicine: Focus on articular cartilage and intervertebral disc regeneration. Methods 2016, 99, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Ouyang, H.; Dass, C.R.; Xu, J. Current research on pharmacologic and regenerative therapies for osteoarthritis. Bone Res. 2016, 4, 15040. [Google Scholar] [CrossRef] [PubMed]
- Im, G.-I.; Shin, Y.-W.; Lee, K.-B. Do adipose tissue-derived mesenchymal stem cells have the same osteogenic and chondrogenic potential as bone marrow-derived cells? Osteoarthritis and cartilage 2005, 13, 845–853. [Google Scholar] [CrossRef]
- Huang, Y.-Z.; Xie, H.-Q.; Silini, A.; Parolini, O.; Zhang, Y.; Deng, L.; Huang, Y.-C. Mesenchymal Stem/Progenitor Cells Derived from Articular Cartilage, Synovial Membrane and Synovial Fluid for Cartilage Regeneration: Current Status and Future Perspectives. Stem Cell Rev. Rep. 2017, 13, 575–586. [Google Scholar] [CrossRef]
- Song, Y.; Du, H.; Dai, C.; Zhang, L.; Li, S.; Hunter, D.J.; Lu, L.; Bao, C. Human adipose-derived mesenchymal stem cells for osteoarthritis: a pilot study with long-term follow-up and repeated injections. Regen. Med. 2018, 13, 295–307. [Google Scholar] [CrossRef]
- Terada, N.; Hamazaki, T.; Oka, M.; Hoki, M.; Mastalerz, D.M.; Nakano, Y.; Meyer, E.M.; Morel, L.; Petersen, B.E.; Scott, E.W. Bone marrow cells adopt the phenotype of other cells by spontaneous cell fusion. Nature 2002, 416, 542–545. [Google Scholar] [CrossRef]
- Konno, M.; Hamabe, A.; Hasegawa, S.; Ogawa, H.; Fukusumi, T.; Nishikawa, S.; Ohta, K.; Kano, Y.; Ozaki, M.; Noguchi, Y.; et al. Adipose-derived mesenchymal stem cells and regenerative medicine. Dev. Growth Differ. 2013, 55, 309–318. [Google Scholar] [CrossRef]
- Lee, W.-S.; Kim, H.J.; Kim, K.-I.; Kim, G.B.; Jin, W. Intra-Articular Injection of Autologous Adipose Tissue-Derived Mesenchymal Stem Cells for the Treatment of Knee Osteoarthritis: A Phase IIb, Randomized, Placebo-Controlled Clinical Trial. Stem Cells Transl. Med. 2019, 8, 504–511. [Google Scholar] [CrossRef]
- Sakaguchi, Y.; Sekiya, I.; Yagishita, K.; Muneta, T. Comparison of human stem cells derived from various mesenchymal tissues: Superiority of synovium as a cell source. Arthritis Rheum. 2005, 52, 2521–2529. [Google Scholar] [CrossRef] [PubMed]
- To, K.; Zhang, B.; Romain, K.; Mak, C.; Khan, W. Synovium-Derived Mesenchymal Stem Cell Transplantation in Cartilage Regeneration: A PRISMA Review of in vivo Studies. Front. Bioeng. Biotechnol. 2019, 7, 314. [Google Scholar] [CrossRef] [PubMed]
- Zupan, J.; Drobnič, M.; Stražar, K. Synovium-derived mesenchymal stem/stromal cells and their promise for cartilage regeneration. Cell Biology and Translational Medicine, Volume 6: Stem Cells: Their Heterogeneity, Niche and Regenerative Potential 2020, 87-106.
- Kondo, S.; Muneta, T.; Nakagawa, Y.; Koga, H.; Watanabe, T.; Tsuji, K.; Sotome, S.; Okawa, A.; Kiuchi, S.; Ono, H.; et al. Transplantation of autologous synovial mesenchymal stem cells promotes meniscus regeneration in aged primates. J. Orthop. Res. 2017, 35, 1274–1282. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, Y.; Kim, H.; Hwang, K.J.; Kwon, H.C.; Kim, S.K.; Cho, D.J.; Kang, S.G.; You, J. Human amniotic fluid-derived stem cells have characteristics of multipotent stem cells. Cell Prolif. 2007, 40, 75–90. [Google Scholar] [CrossRef]
- De Coppi, P.; Bartsch Jr, G.; Siddiqui, M.M.; Xu, T.; Santos, C.C.; Perin, L.; Mostoslavsky, G.; Serre, A.C.; Snyder, E.Y.; Yoo, J.J. Isolation of amniotic stem cell lines with potential for therapy. Nature biotechnology 2007, 25, 100–106. [Google Scholar] [CrossRef]
- Davies, J.E.; Walker, J.T.; Keating, A. Concise review: Wharton’s jelly: the rich, but enigmatic, source of mesenchymal stromal cells. Stem cells translational medicine 2017, 6, 1620–1630. [Google Scholar] [CrossRef]
- Anzalone, R.; Iacono, M.L.; Corrao, S.; Magno, F.; Loria, T.; Cappello, F.; Zummo, G.; Farina, F.; La Rocca, G. New Emerging Potentials for Human Wharton’s Jelly Mesenchymal Stem Cells: Immunological Features and Hepatocyte-Like Differentiative Capacity. Stem Cells Dev. 2010, 19, 423–438. [Google Scholar] [CrossRef]
- Jiang, S.; Tian, G.; Yang, Z.; Gao, X.; Wang, F.; Li, J.; Tian, Z.; Huang, B.; Wei, F.; Sang, X.; et al. Enhancement of acellular cartilage matrix scaffold by Wharton's jelly mesenchymal stem cell-derived exosomes to promote osteochondral regeneration. Bioact. Mater. 2021, 6, 2711–2728. [Google Scholar] [CrossRef]
- Abbaszadeh, H.; Ghorbani, F.; Derakhshani, M.; Movassaghpour, A.A.; Yousefi, M.; Talebi, M.; Shamsasenjan, K. Regenerative potential of Wharton's jelly-derived mesenchymal stem cells: A new horizon of stem cell therapy. J. Cell. Physiol. 2020, 235, 9230–9240. [Google Scholar] [CrossRef]
- Thitiset, T.; Damrongsakkul, S.; Yodmuang, S.; Leeanansaksiri, W.; Apinun, J.; Honsawek, S. A novel gelatin/chitooligosaccharide/demineralized bone matrix composite scaffold and periosteum-derived mesenchymal stem cells for bone tissue engineering. Biomater. Res. 2021, 25, 19. [Google Scholar] [CrossRef]
- Moon, D.K.; Kim, B.G.; Lee, A.R.; Choe, Y.I.; Khan, I.; Moon, K.M.; Jeon, R.-H.; Byun, J.-H.; Hwang, S.-C.; Woo, D.K. Resveratrol can enhance osteogenic differentiation and mitochondrial biogenesis from human periosteum-derived mesenchymal stem cells. J. Orthop. Surg. Res. 2020, 15, 1–10. [Google Scholar] [CrossRef]
- Masuda, K.; Han, X.; Kato, H.; Sato, H.; Zhang, Y.; Sun, X.; Hirofuji, Y.; Yamaza, H.; Yamada, A.; Fukumoto, S. Dental Pulp-Derived Mesenchymal Stem Cells for Modeling Genetic Disorders. Int. J. Mol. Sci. 2021, 22, 2269. [Google Scholar] [CrossRef]
- Caseiro, A.R.; Pedrosa, S.S.; Ivanova, G.; Branquinho, M.V.; Almeida, A.; Faria, F.; Amorim, I.; Pereira, T.; Maurício, A.C. Mesenchymal Stem/ Stromal Cells metabolomic and bioactive factors profiles: A comparative analysis on the umbilical cord and dental pulp derived Stem/ Stromal Cells secretome. PLOS ONE 2019, 14, e0221378. [Google Scholar] [CrossRef]
- Kern, S.; Eichler, H.; Stoeve, J.; Klüter, H.; Bieback, K. Comparative Analysis of Mesenchymal Stem Cells from Bone Marrow, Umbilical Cord Blood, or Adipose Tissue. Stem Cells 2006, 24, 1294–1301. [Google Scholar] [CrossRef]
- Jin, H.J.; Bae, Y.K.; Kim, M.; Kwon, S.-J.; Jeon, H.B.; Choi, S.J.; Kim, S.W.; Yang, Y.S.; Oh, W.; Chang, J.W. Comparative Analysis of Human Mesenchymal Stem Cells from Bone Marrow, Adipose Tissue, and Umbilical Cord Blood as Sources of Cell Therapy. Int. J. Mol. Sci. 2013, 14, 17986–18001. [Google Scholar] [CrossRef] [PubMed]
- Čamernik, K.; Mihelič, A.; Mihalič, R.; Presen, D.M.; Janež, A.; Trebše, R.; Marc, J.; Zupan, J. Skeletal-muscle-derived mesenchymal stem/stromal cells from patients with osteoarthritis show superior biological properties compared to bone-derived cells. Stem Cell Res. 2019, 38, 101465. [Google Scholar] [CrossRef] [PubMed]
- Godwin, E.E.; Young, N.J.; Dudhia, J.; Beamish, I.C.; Smith, R.K.W. Implantation of bone marrow-derived mesenchymal stem cells demonstrates improved outcome in horses with overstrain injury of the superficial digital flexor tendon. Equine Veter- J. 2012, 44, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Costa-Almeida, R.; Calejo, I.; Gomes, M.E. Mesenchymal Stem Cells Empowering Tendon Regenerative Therapies. Int. J. Mol. Sci. 2019, 20, 3002. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, C.S.; E Saether, E.; Vanderby, R.; Aktas, E. Mesenchymal Stem Cell Therapy on Tendon/Ligament Healing. J. Cytokine Biol. 2017, 2, 1–3. [Google Scholar] [CrossRef]
- Lee, J.Y.; Zhou, Z.; Taub, P.J.; Ramcharan, M.; Li, Y.; Akinbiyi, T.; Maharam, E.R.; Leong, D.J.; Laudier, D.M.; Ruike, T.; et al. BMP-12 Treatment of Adult Mesenchymal Stem Cells In Vitro Augments Tendon-Like Tissue Formation and Defect Repair In Vivo. PLOS ONE 2011, 6, e17531. [Google Scholar] [CrossRef] [PubMed]
- Docheva, D.; Müller, S.A.; Majewski, M.; Evans, C.H. Biologics for tendon repair. Advanced drug delivery reviews 2015, 84, 222–239. [Google Scholar] [CrossRef]
- Yea, J.-H.; Kim, Y.; Jo, C.H. Comparison of mesenchymal stem cells from bone marrow, umbilical cord blood, and umbilical cord tissue in regeneration of a full-thickness tendon defect in vitro and in vivo. Biochem. Biophys. Rep. 2023, 34, 101486. [Google Scholar] [CrossRef]
- Burk, J.; Gittel, C.; Heller, S.; Pfeiffer, B.; Paebst, F.; Ahrberg, A.B.; Brehm, W. Gene expression of tendon markers in mesenchymal stromal cells derived from different sources. BMC Res. Notes 2014, 7, 1–6. [Google Scholar] [CrossRef]
- Conze, P.; van Schie, H.T.; van Weeren, R.; Staszyk, C.; Conrad, S.; Skutella, T.; Hopster, K.; Rohn, K.; Stadler, P.; Geburek, F. Effect of autologous adipose tissue-derived mesenchymal stem cells on neovascularization of artificial equine tendon lesions. Regen. Med. 2014, 9, 743–757. [Google Scholar] [CrossRef]
- Archer, C.W.; Dowthwaite, G.P.; Francis-West, P. Development of synovial joints. Birth Defects Research Part C: Embryo Today: Reviews 2003, 69, 144–155. [Google Scholar] [CrossRef]
- Koyama, E.; Shibukawa, Y.; Nagayama, M.; Sugito, H.; Young, B.; Yuasa, T.; Okabe, T.; Ochiai, T.; Kamiya, N.; Rountree, R.B.; et al. A distinct cohort of progenitor cells participates in synovial joint and articular cartilage formation during mouse limb skeletogenesis. Dev. Biol. 2008, 316, 62–73. [Google Scholar] [CrossRef]
- Zha, K.; Li, X.; Yang, Z.; Tian, G.; Sun, Z.; Sui, X.; Dai, Y.; Liu, S.; Guo, Q. Heterogeneity of mesenchymal stem cells in cartilage regeneration: from characterization to application. npj Regen. Med. 2021, 6, 14. [Google Scholar] [CrossRef]
- Lam, A.T.; Reuveny, S.; Oh, S.K.-W. Human mesenchymal stem cell therapy for cartilage repair: Review on isolation, expansion, and constructs. Stem Cell Res. 2020, 44, 101738. [Google Scholar] [CrossRef]
- Richter, W. Mesenchymal stem cells and cartilage in situ regeneration. J. Intern. Med. 2009, 266, 390–405. [Google Scholar] [CrossRef]
- Grande, D.A.; Southerland, S.S.; Manji, R.; Pate, D.W.; Schwartz, R.E.; Lucas, P.A. Repair of Articular Cartilage Defects Using Mesenchymal Stem Cells. Tissue Eng. 1995, 1, 345–353. [Google Scholar] [CrossRef]
- Otto, W.R.; Rao, J. Tomorrow's skeleton staff: mesenchymal stem cells and the repair of bone and cartilage. Cell Prolif. 2004, 37, 97–110. [Google Scholar] [CrossRef]
- Koga, H.; Muneta, T.; Nagase, T.; Nimura, A.; Ju, Y.-J.; Mochizuki, T.; Sekiya, I. Comparison of mesenchymal tissues-derived stem cells for in vivo chondrogenesis: suitable conditions for cell therapy of cartilage defects in rabbit. Cell Tissue Res. 2008, 333, 207–215. [Google Scholar] [CrossRef]
- Yoshimura, H.; Muneta, T.; Nimura, A.; Yokoyama, A.; Koga, H.; Sekiya, I. Comparison of rat mesenchymal stem cells derived from bone marrow, synovium, periosteum, adipose tissue, and muscle. Cell Tissue Res. 2007, 327, 449–462. [Google Scholar] [CrossRef]
- Jones, B.A.; Pei, M. Synovium-Derived Stem Cells: A Tissue-Specific Stem Cell for Cartilage Engineering and Regeneration. Tissue Eng. Part B: Rev. 2012, 18, 301–311. [Google Scholar] [CrossRef]
- Hassanzadeh, A.; Vousooghi, N.; Rahimnia, R.; Razeghian, E.; Rajaeian, S.; Seyhoun, I.; Sharif, S.; Verdi, J. Recent advances in mesenchymal stem/stromal cells (MSCs)-based approaches for osteoarthritis (OA) therapy. Cell Biol. Int. 2023, 47, 1033–1048. [Google Scholar] [CrossRef] [PubMed]
- Granero-Molto, F.; A Weis, J.; Longobardi, L.; Spagnoli, A.; D, P. ; Bs; Md Role of mesenchymal stem cells in regenerative medicine: application to bone and cartilage repair. Expert Opin. Biol. Ther. 2008, 8, 255–268. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Stanford, W.L.; Kandel, R.A. Mesenchymal stem and progenitor cells for cartilage repair. Skelet. Radiol. 2007, 36, 909–912. [Google Scholar] [CrossRef] [PubMed]
- Kubosch, E.J.; Lang, G.; Furst, D.; Kubosch, D.; Izadpanah, K.; Rolauffs, B.; Sudkamp, N.P.; Schmal, H. The Potential for Synovium-derived Stem Cells in Cartilage Repair. Curr. Stem Cell Res. Ther. 2018, 13, 174–184. [Google Scholar] [CrossRef]
- Mochizuki, T.; Muneta, T.; Sakaguchi, Y.; Nimura, A.; Yokoyama, A.; Koga, H.; Sekiya, I. Higher chondrogenic potential of fibrous synovium– and adipose synovium–derived cells compared with subcutaneous fat–derived cells: Distinguishing properties of mesenchymal stem cells in humans. Arthritis Rheum. 2006, 54, 843–853. [Google Scholar] [CrossRef]
- Koga, H.; Muneta, T.; Ju, Y.-J.; Nagase, T.; Nimura, A.; Mochizuki, T.; Ichinose, S.; von der Mark, K.; Sekiya, I. Synovial Stem Cells Are Regionally Specified According to Local Microenvironments After Implantation for Cartilage Regeneration. Stem Cells 2006, 25, 689–696. [Google Scholar] [CrossRef]
- De Bari, C.; Dell’Accio, F.; Tylzanowski, P.; Luyten, F.P. Multipotent mesenchymal stem cells from adult human synovial membrane. Arthritis Rheum. 2001, 44, 1928–1942. [Google Scholar] [CrossRef] [PubMed]
- Song, L.; Tuan, R.S. Transdifferentiation potential of human mesenchymal stem cells derived from bone marrow. FASEB J. 2004, 18, 980–982. [Google Scholar] [CrossRef]
- Prockop, D.J.; Gregory, C.A.; Spees, J.L. One strategy for cell and gene therapy: Harnessing the power of adult stem cells to repair tissues. Proc. Natl. Acad. Sci. 2003, 100, 11917–11923. [Google Scholar] [CrossRef]
- Zha, K.; Sun, Z.; Yang, Y.; Chen, M.; Gao, C.; Fu, L.; Li, H.; Sui, X.; Guo, Q.; Liu, S. Recent Developed Strategies for Enhancing Chondrogenic Differentiation of MSC: Impact on MSC-Based Therapy for Cartilage Regeneration. Stem Cells Int. 2021, 2021, 1–15. [Google Scholar] [CrossRef]
- Sadlik, B.; Jaroslawski, G.; Puszkarz, M.; Blasiak, A.; Oldak, T.; Gladysz, D.; Whyte, G.P. Cartilage Repair in the Knee Using Umbilical Cord Wharton's Jelly–Derived Mesenchymal Stem Cells Embedded Onto Collagen Scaffolding and Implanted Under Dry Arthroscopy. Arthrosc. Tech. 2018, 7, e57–e63. [Google Scholar] [CrossRef]
- Liu, T.P.; Ha, P.; Xiao, C.Y.; Kim, S.Y.; Jensen, A.R.; Easley, J.; Yao, Q.; Zhang, X. Updates on mesenchymal stem cell therapies for articular cartilage regeneration in large animal models. Front. Cell Dev. Biol. 2022, 10, 982199. [Google Scholar] [CrossRef]
- Xiang, X.-N.; Zhu, S.-Y.; He, H.-C.; Yu, X.; Xu, Y.; He, C.-Q. Mesenchymal stromal cell-based therapy for cartilage regeneration in knee osteoarthritis. Stem Cell Res. Ther. 2022, 13, 1–20. [Google Scholar] [CrossRef] [PubMed]
- De La Garza-Rodea, A.S.; Van Der Velde-Van Dijke, I.; Boersma, H.; Gonçalves, M.A.; Van Bekkum, D.W.; De Vries, A.A.; Knaän-Shanzer, S. Myogenic properties of human mesenchymal stem cells derived from three different sources. Cell transplantation 2012, 21, 153–173. [Google Scholar] [CrossRef]
- Kim, J.; Park, J.; Song, S.-Y.; Kim, E. Advanced Therapy medicinal products for autologous chondrocytes and comparison of regulatory systems in target countries. Regen. Ther. 2022, 20, 126–137. [Google Scholar] [CrossRef]
- Carballo, C.B.; Nakagawa, Y.; Sekiya, I.; Rodeo, S.A. Basic Science of Articular Cartilage. Clin. Sports Med. 2017, 36, 413–425. [Google Scholar] [CrossRef]
- Welch, T.; Mandelbaum, B.; Tom, M. Autologous chondrocyte implantation: past, present, and future. Sports medicine and arthroscopy review 2016, 24, 85–91. [Google Scholar] [CrossRef]
- Xia, J.; Minamino, S.; Kuwabara, K.; Arai, S. Stem cell secretome as a new booster for regenerative medicine. Biosci. Trends 2019, 13, 299–307. [Google Scholar] [CrossRef]
- Daneshmandi, L.; Shah, S.; Jafari, T.; Bhattacharjee, M.; Momah, D.; Saveh-Shemshaki, N.; Lo, K.W.-H.; Laurencin, C.T. Emergence of the Stem Cell Secretome in Regenerative Engineering. Trends Biotechnol. 2020, 38, 1373–1384. [Google Scholar] [CrossRef]
- Djatche, W.H.B.; Zhu, H.; Ma, W.; Li, Y.; Li, Z.; Zhao, H.; Liu, Z.; Qiao, H. Potential of mesenchymal stem cell-derived conditioned medium/secretome as a therapeutic option for ocular diseases. Regen. Med. 2023, 18, 795–807. [Google Scholar] [CrossRef]
- Pawitan, J.A. Prospect of Stem Cell Conditioned Medium in Regenerative Medicine. BioMed Res. Int. 2014, 2014, 965849. [Google Scholar] [CrossRef] [PubMed]
- Jafarinia, M.; Alsahebfosoul, F.; Salehi, H.; Eskandari, N.; Ganjalikhani-Hakemi, M. Mesenchymal Stem Cell-Derived Extracellular Vesicles: A Novel Cell-Free Therapy. Immunol. Investig. 2020, 49, 758–780. [Google Scholar] [CrossRef]
- Yu, H.; Cheng, J.; Shi, W.; Ren, B.; Zhao, F.; Shi, Y.; Yang, P.; Duan, X.; Zhang, J.; Fu, X.; et al. Bone marrow mesenchymal stem cell-derived exosomes promote tendon regeneration by facilitating the proliferation and migration of endogenous tendon stem/progenitor cells. Acta Biomater. 2020, 106, 328–341. [Google Scholar] [CrossRef]
- Kou, M.; Huang, L.; Yang, J.; Chiang, Z.; Chen, S.; Liu, J.; Guo, L.; Zhang, X.; Zhou, X.; Xu, X. Mesenchymal stem cell-derived extracellular vesicles for immunomodulation and regeneration: a next generation therapeutic tool? Cell Death & Disease 2022, 13, 580. [Google Scholar]
- Kwon, S.; Shin, S.; Do, M.; Oh, B.H.; Song, Y.; Bui, V.D.; Lee, E.S.; Jo, D.-G.; Cho, Y.W.; Kim, D.-H.; et al. Engineering approaches for effective therapeutic applications based on extracellular vesicles. J. Control. Release 2021, 330, 15–30. [Google Scholar] [CrossRef]
- Mebarki, M.; Abadie, C.; Larghero, J.; Cras, A. Human umbilical cord-derived mesenchymal stem/stromal cells: a promising candidate for the development of advanced therapy medicinal products. Stem Cell Res. Ther. 2021, 12, 1–10. [Google Scholar] [CrossRef]
- Ni, Z.; Zhou, S.; Li, S.; Kuang, L.; Chen, H.; Luo, X.; Ouyang, J.; He, M.; Du, X.; Chen, L. Exosomes: Roles and therapeutic potential in osteoarthritis. Bone Res. 2020, 8, 25. [Google Scholar] [CrossRef]
- Fan, W.-J.; Liu, D.; Pan, L.-Y.; Wang, W.-Y.; Ding, Y.-L.; Zhang, Y.-Y.; Ye, R.-X.; Zhou, Y.; An, S.-B.; Xiao, W.-F. Exosomes in osteoarthritis: Updated insights on pathogenesis, diagnosis, and treatment. Front. Cell Dev. Biol. 2022, 10, 949690. [Google Scholar] [CrossRef]
- Fang, W.H.; Agrawal, D.K.; Thankam, F.G. “Smart exosomes”: a smart approach for tendon regeneration. Tissue Engineering Part B: Reviews 2022, 28, 613–625. [Google Scholar] [CrossRef]
- Wang, Y.; He, G.; Guo, Y.; Tang, H.; Shi, Y.; Bian, X.; Zhu, M.; Kang, X.; Zhou, M.; Lyu, J.; et al. Exosomes from tendon stem cells promote injury tendon healing through balancing synthesis and degradation of the tendon extracellular matrix. J. Cell. Mol. Med. 2019, 23, 5475–5485. [Google Scholar] [CrossRef]
- Lyu, K.; Liu, T.; Chen, Y.; Lu, J.; Jiang, L.; Liu, X.; Liu, X.; Li, Y.; Li, S. A “cell-free treatment” for tendon injuries: adipose stem cell-derived exosomes. European Journal of Medical Research 2022, 27, 75. [Google Scholar] [CrossRef] [PubMed]
- Iyer, S.R.; Scheiber, A.L.; Yarowsky, P.; Henn III, R.F.; Otsuru, S.; Lovering, R.M. Exosomes isolated from platelet-rich plasma and mesenchymal stem cells promote recovery of function after muscle injury. The American Journal of Sports Medicine 2020, 48, 2277–2286. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Song, W.; Chen, B.; Liu, X.; He, Y. Exosomes Isolated From Adipose-Derived Stem Cells: A New Cell-Free Approach to Prevent the Muscle Degeneration Associated With Torn Rotator Cuffs. Am. J. Sports Med. 2019, 47, 3247–3255. [Google Scholar] [CrossRef]
- Holmes, T.Q.; Brown, A.F. Champing at the Bit for Improvements: A Review of Equine Welfare in Equestrian Sports in the United Kingdom. Animals 2022, 12, 1186. [Google Scholar] [CrossRef]
- Mactaggart, G.; Waran, N.; Phillips, C.J.C. Identification of Thoroughbred Racehorse Welfare Issues by Industry Stakeholders. Animals 2021, 11, 1358. [Google Scholar] [CrossRef]
- Marshall-Gibson, M.E.; Durham, M.G.; Seabaugh, K.A.; Moorman, V.J.; Ferris, D.J. Survey of equine veterinarians regarding primary equine back pain in the United States. Front. Veter- Sci. 2023, 10, 1224605. [Google Scholar] [CrossRef]
- Rhatomy, S.; Prasetyo, T.E.; Setyawan, R.; Soekarno, N.R.; Romaniyanto, F.; Sedjati, A.P.; Sumarwoto, T.; Utomo, D.N.; Suroto, H.; Mahyudin, F.; et al. Prospect of stem cells conditioned medium (secretome) in ligament and tendon healing: A systematic review. Stem Cells Transl. Med. 2020, 9, 895–902. [Google Scholar] [CrossRef]
- Rodríguez-Fuentes, D.E.; Fernández-Garza, L.E.; Samia-Meza, J.A.; Barrera-Barrera, S.A.; Caplan, A.I.; Barrera-Saldaña, H.A. Mesenchymal Stem Cells Current Clinical Applications: A Systematic Review. Arch. Med Res. 2021, 52, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Carter-Arnold, J.; Neilsen, N.; Amelse, L.; Odoi, A.; Dhar, M. In vitro analysis of equine, bone marrow-derived mesenchymal stem cells demonstrates differences within age-and gender-matched horses. Equine veterinary journal 2014, 46, 589–595. [Google Scholar] [CrossRef]
- Colbath, A.C.; Dow, S.W.; McIlwraith, C.W.; Goodrich, L.R. Mesenchymal stem cells for treatment of musculoskeletal disease in horses: Relative merits of allogeneic versus autologous stem cells. Equine Veter- J. 2020, 52, 654–663. [Google Scholar] [CrossRef]
- Jammes, M.; Contentin, R.; Audigié, F.; Cassé, F.; Galéra, P. Effect of pro-inflammatory cytokine priming and storage temperature of the mesenchymal stromal cell (MSC) secretome on equine articular chondrocytes. Front. Bioeng. Biotechnol. 2023, 11, 1204737. [Google Scholar] [CrossRef]
- Broeckx, S.Y.; Seys, B.; Suls, M.; Vandenberghe, A.; Mariën, T.; Adriaensen, E.; Declercq, J.; Van Hecke, L.; Braun, G.; Hellmann, K.; et al. Equine Allogeneic Chondrogenic Induced Mesenchymal Stem Cells Are an Effective Treatment for Degenerative Joint Disease in Horses. Stem Cells Dev. 2019, 28, 410–422. [Google Scholar] [CrossRef]
- Taylor, C.J.; Peter, V.G.; Coleridge, M.O.D.; Bathe, A.P. Immediate pre-operative computed tomography for surgical planning of equine fracture repair: A retrospective review of 55 cases. PLOS ONE 2022, 17, e0278748. [Google Scholar] [CrossRef]
- Sherlock, C.E.; Eggleston, R.B.; Peroni, J.F.; Parks, A.H. Desmitis of the medial tarsal collateral ligament in 7 horses. Equine Veter- Educ. 2011, 24, 72–80. [Google Scholar] [CrossRef]
- Santos, V.H.; Pfeifer, J.P.H.; Rosa, G.S. Synovial-Derived Mesenchymal Stem Cells Encapsulated in Alginate Beads Provide Better Outcomes for Equine Tarsus Chondral Lesions. J. Orthop. Sports Med. 2023, 5, 265–279. [Google Scholar] [CrossRef]
- Rose, P.L.; Moore, I. Imaging diagnosis--avulsion of the medial collateral ligament of the tarsus in a horse. Veterinary Radiology & Ultrasound: The Official Journal of the American College of Veterinary Radiology and the International Veterinary Radiology Association 2003, 44, 657–659. [Google Scholar] [CrossRef]
- Mitchell, R.; DaSilva, D.; Rosenbaum, C.; Blikslager, A.; Edwards III, R. Ultrasound findings in tendons and ligaments of lame sport horses competing or training in South Florida venues during the winter seasons of 2007 through 2016. Equine Veterinary Education 2021, 33, 306–309. [Google Scholar] [CrossRef]
- Roessingh, A.S.d.B.; Laurent, A.; E Darwiche, S.; Hirt-Burri, N.; Scaletta, C.; Michetti, M.; Laurent, P.; Raffoul, W.; Applegate, L.A. Banking Progenitor Cells for Hippiatric Regenerative Medicine: Optimized Establishment of Safe and Consistent Cell Sources for Standardized Veterinary Therapeutic Protocols. Am. J. Biomed. Sci. Res. 2020, 8, 252–271. [Google Scholar] [CrossRef]
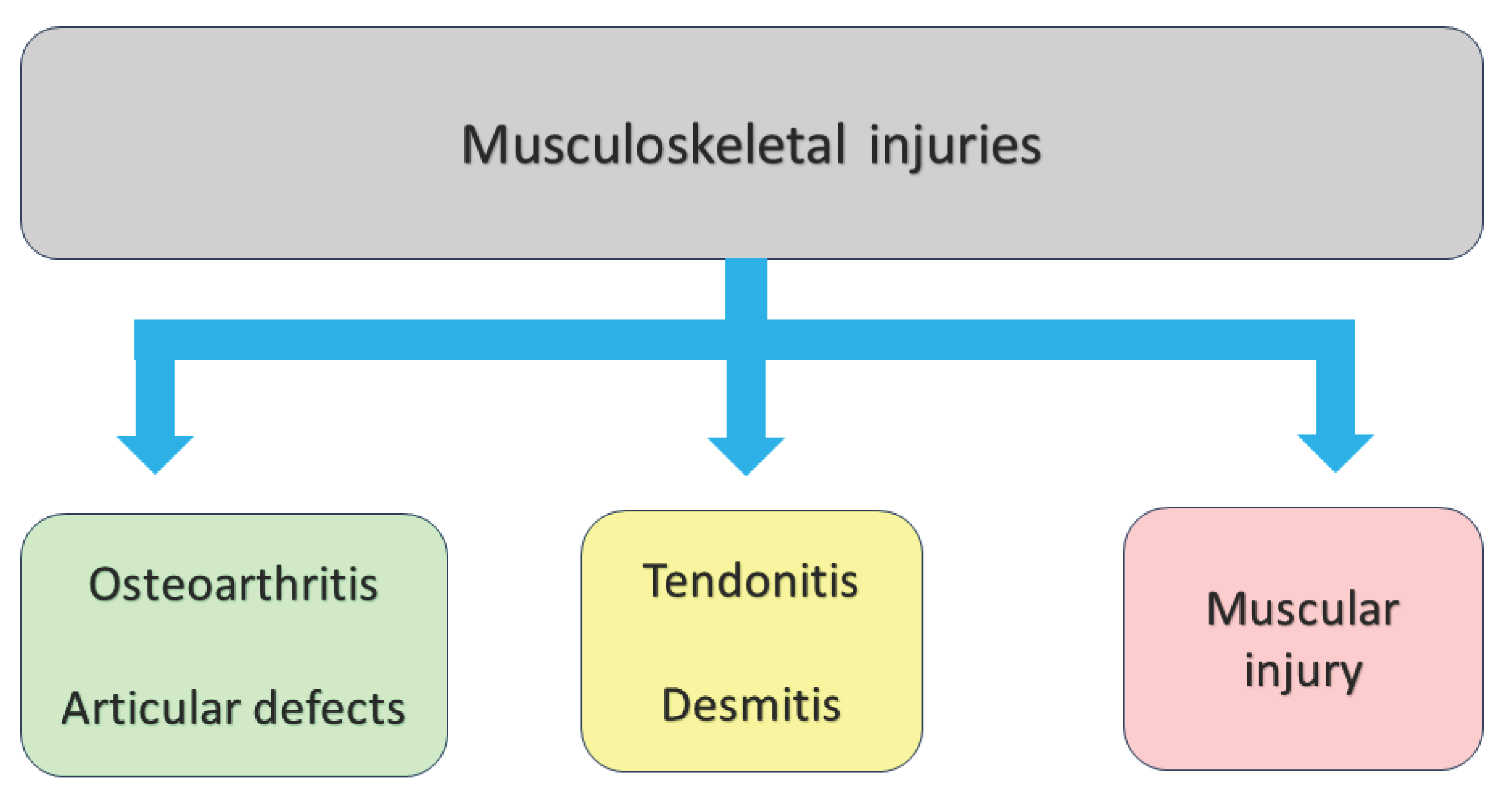
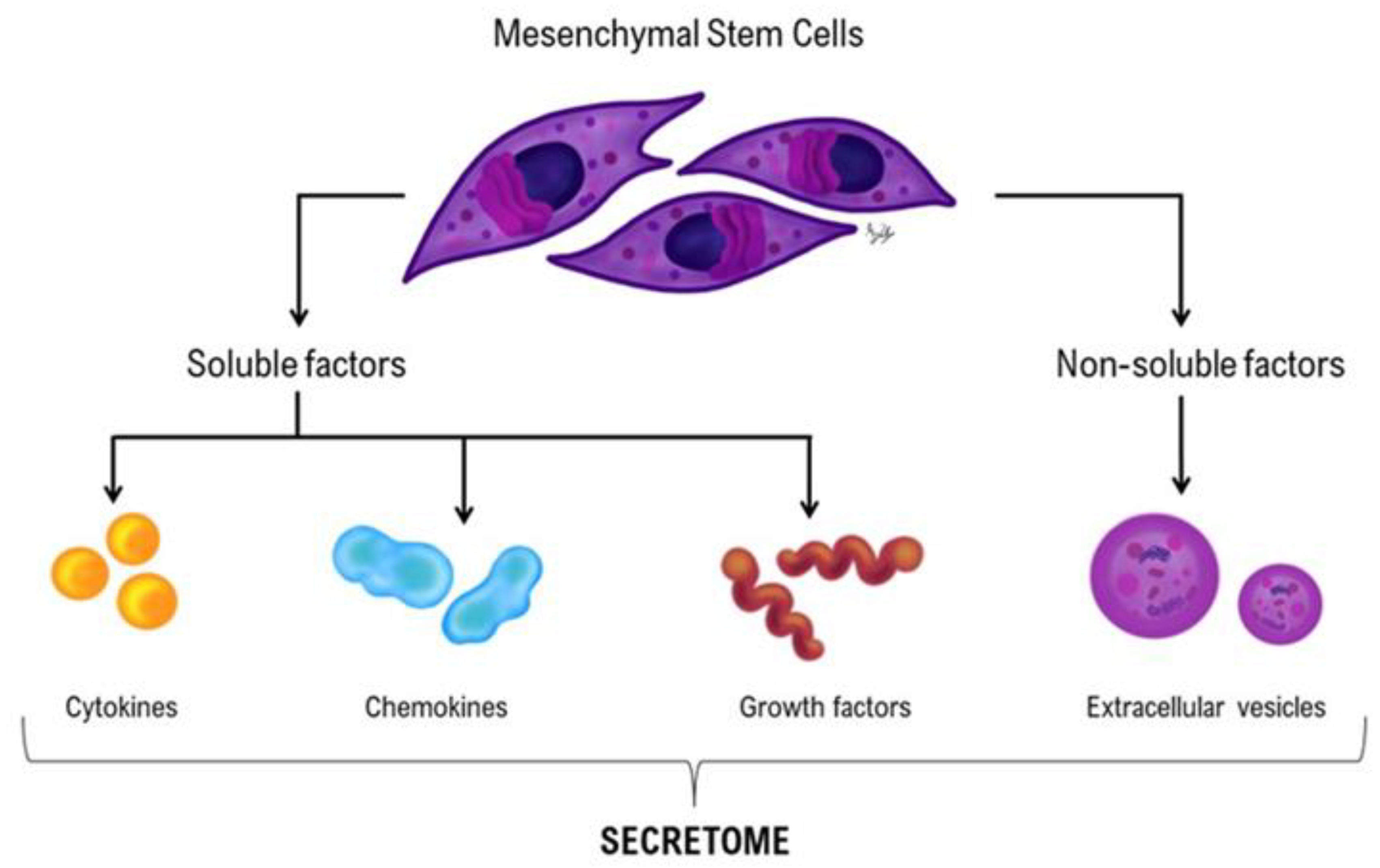
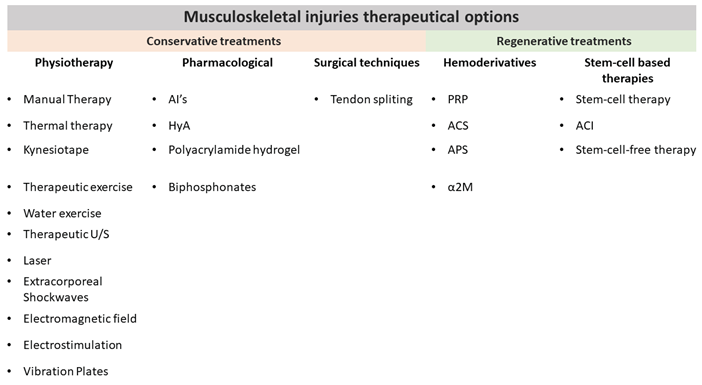 |
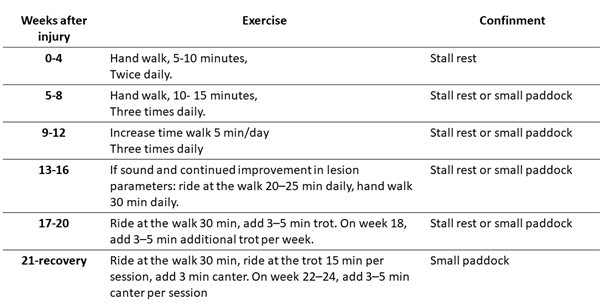 |
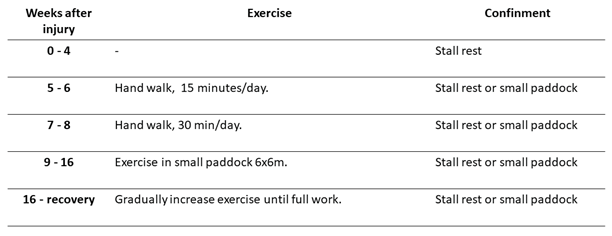 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





