1. Introduction
Tooth extraction (
exodontia) is one of the oldest and most well-known surgical procedures in dental medicine. It is still routinely performed to date by both general practitioners, oral surgeons, and dental undergraduates[
1]. Dental implantology has also become a prime solution for treatment of partial or complete tooth loss. Teeth, which would otherwise be saved by some dubious or hard to perform conservative treatment techniques are now considered for extraction and implant replacement[
2].
The classical means for tooth extraction – forceps and elevators – do not make it impossible to perform an atraumatic extraction. However, their use oftentimes leads to unexpected complications and unplanned difficulties during the procedure. Even for the more experienced practitioners this may easily turn out to be a challenging extraction, requiring a not so atraumatic approach to fully complete. This leads to a varying extent to postoperative defects in the alveolar bone of the extraction site[
3,
4].
Post extraction wound healing is a great indicator of how well the body recovers from the damage caused. This can occur with mild to no discomfort at all but can also be delayed and accompanied by different symptoms such as swelling, trismus, infection and a varying degree of pain, all of which can be signs of postoperative complications[
5]. Decreasing the degree of trauma can not only prevent complications but is necessary to preserve bone and soft tissues[
6].
The Benex extraction system allows for the extraction of teeth in vertical direction, which avoids most, if not all, trauma against the surrounding alveolar bone and soft tissues[
7]. This can potentially allow for more bone to be preserved, due to the limited loss of osteoblast cells[
8]. The Benex system is quite different from the instruments most people are used to and consists of the Benex extractor itself, diamond burs, pull strings, self-tapping screws, and sectional impression trays[
9].
2. Materials and Methods
2.1. Study Design
This study was a double randomized control trial.
2.2. Subjects and Sample
The study included 56 patients who were recruited from the department of Oral Surgery at the Faculty of Dental Medicine, Medical University – Plovdiv and Center of Dental Implantology, Research Institute Medical University - Plovdiv. The study was approved by the ethical committee of the Medical University – Plovdiv.
The participants were divided into two groups with equal numbers of patients. Group I (control group) consisted of 28 patients who had an extraction with forceps and was considered the control group. Group II (study group) consisted of 28 patients who were treated with the Benex extraction system and were considered the study group.
2.3. Clinical Procedure
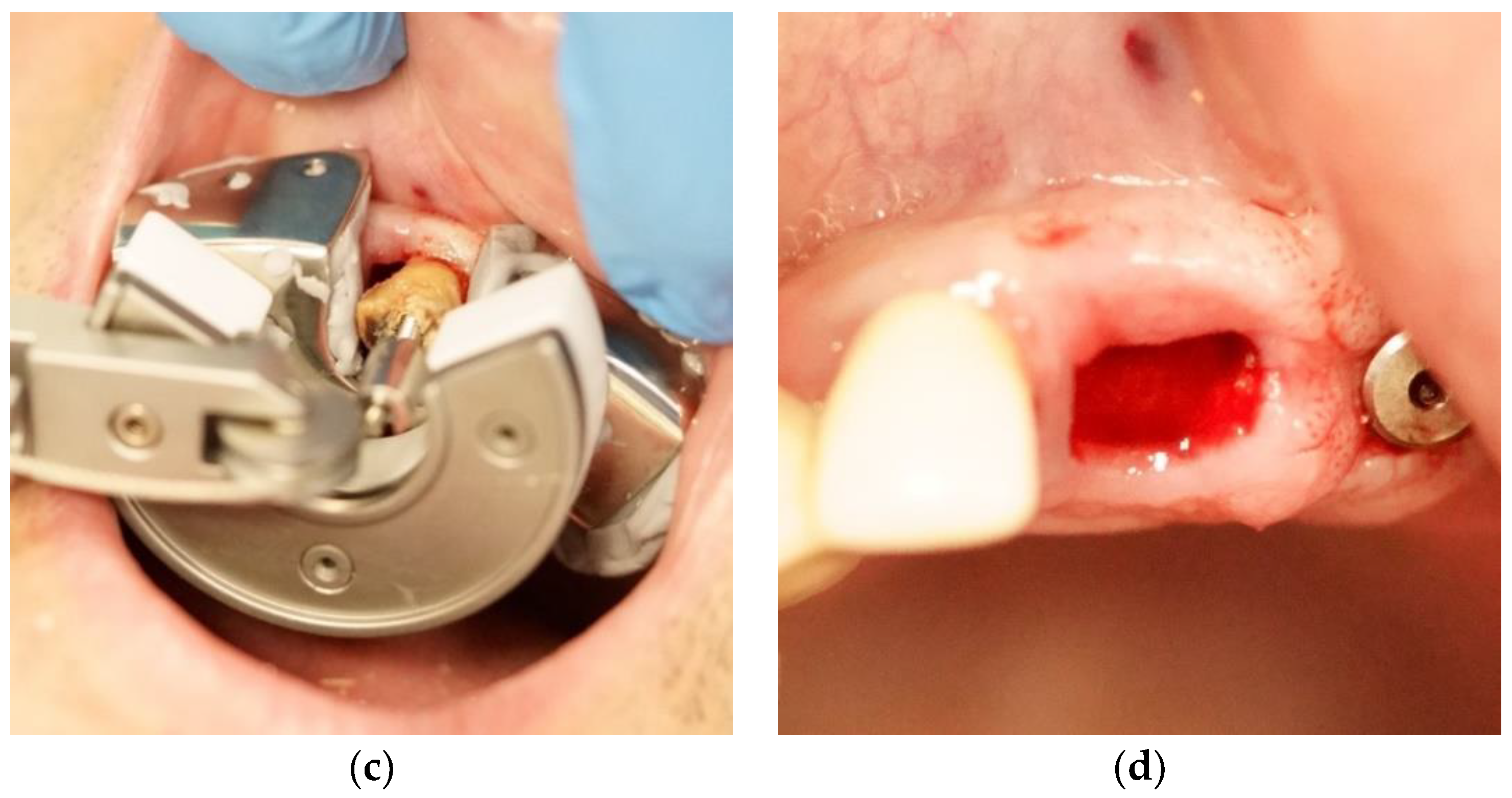
Anaesthesia was performed under infiltration with 4% articaine hydrochloride with adrenaline (dilution, 1:100000; Septodont, Saint-Maur-des-Fossés, France). An impression with Zetaplus putty C-silicon Zetaplus (Zermack, Badia Polesine (Rovigo), Italy) was made with the impression tray included in the Benex extraction kit. Periodontal ligament fibers were cut using a scalpel blade #15. Drilling was performed on the long axis of the tooth with the diamond-coated twist drill from the kit. The screw was inserted, and the impression tray repositioned as a support disk. Then the traction rope was attached to the extraction screw, passed over the roller and fixed in an appropriate notch of the extractor. Extraction was accomplished by gradually turning the hand screw in a clockwise direction. Debridement of the wound was then done, as needed. No sutures were placed over the wounds (
Figure 1).
2.4. Evaluation Method
2.4.1. Extraction Success
Extraction success was graded from 1 to 5 based scale of Choi et al.[
10] and its later modification by Patel et al.[
11]:
Complete success (Score 5): extraction without crown and root fracture;
Limited success with root tip fracture (Score 4): extraction involving root tip fracture;
Limited success with root fracture (Score 3): extraction involving root one or more root fracture or crown fracture;
Limited success with osteotomy (Score 2): fracture-free extraction and partial osteotomy in case divergent roots and thick cortical bone was present;
Failure (Score 1): Failure to extract.
A failed extraction was every extraction, which was not finished of with the instruments for the given group and/or resulted in an open flap extraction. The results between the different groups were compared using independent-samples t-test. The results are presented as mean-and-individual-value.
2.4.2. Buccal Cortical Plate Preservation
The preservation of the buccal cortical plate was rated as preserved (no difference), partially preserved (<4mm) and missing (>4mm). The difference was calculated based on the preoperative and postoperative probing distance on the buccal side of the socket (
Figure 2). This is part of the newly suggested single-rooted extraction wound classification by Hamoun et al.[
12] where they measure the missing buccal cortical plate in percentages. Our results were aggregated in cross-tabulations and were analyzed with a Chi-square test.
2.4.3. Pain Intensity Score
Pain was scored on a linear VAS scale and measured in centimeters on the day of extraction (day 0), 1st, 3rd, and 7th day after the extraction. Participants were asked to place a cross on the linear scale where pain grows from left to right, based on their pain experience on the given day. The results were analyzed with a single-factor repeated measures ANOVA model.
2.4.4. Early Wound Healing
Wound healing was assessed on the 3rd, 7th, and 10th day after the extraction. Scoring was based on Landry’s index (LWHI - Landry Wound Healing Index, also known as Landry, Turnbull, and Howley index).[
13] The index evaluates the extraction socket in regard to wound size, tissue colour, bleeding on palpation, presence of granulation tissue, presence of pus, and gingival margin status. Results were compared using the nonparametric Mann-Whitney U test.
3. Results
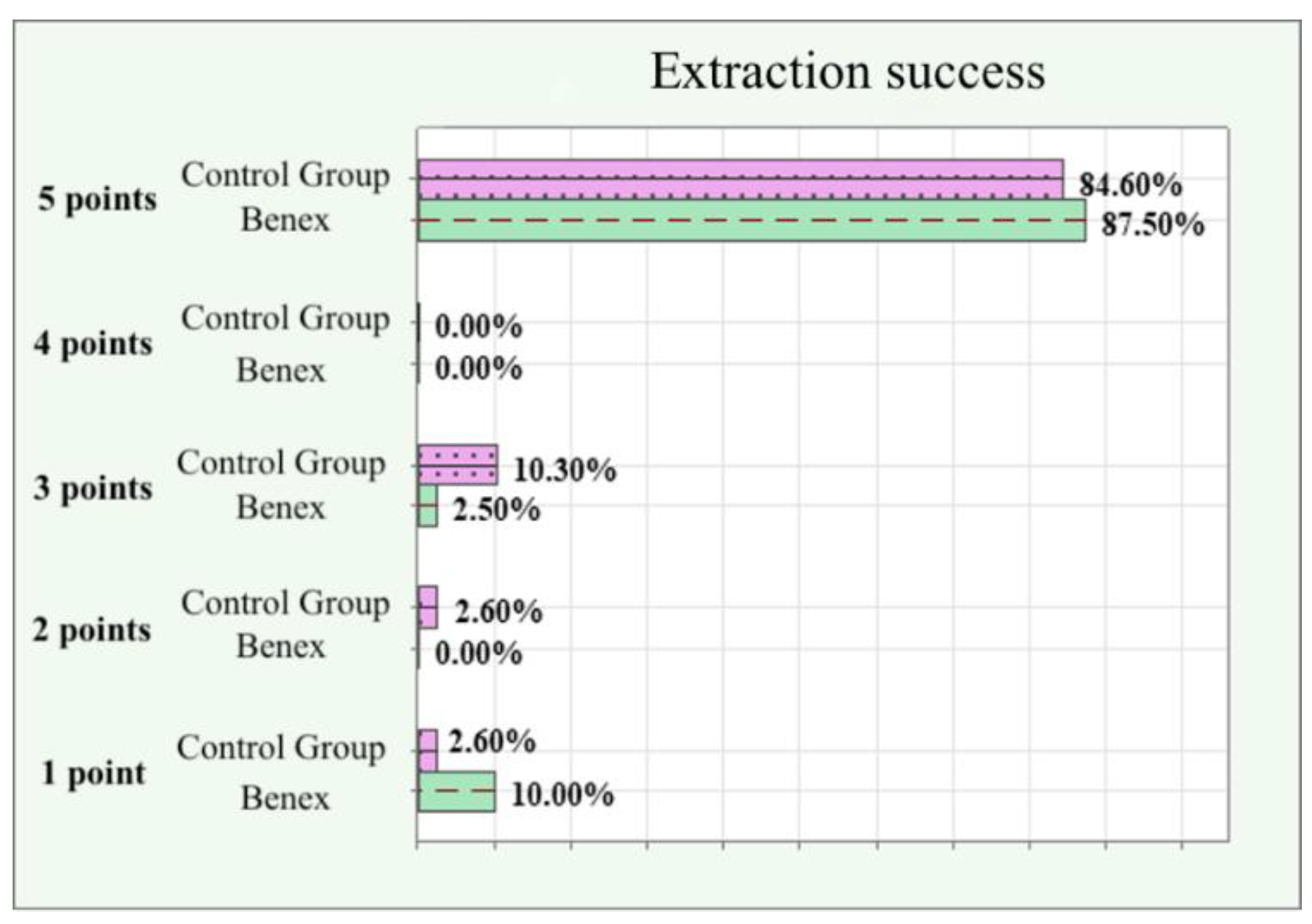
Figure 3 presents the success of extractions in the control group and the study group graded on a scale from 1 (unsuccessful) to 5 (full success). The number of completely successful extractions (5 points) is almost equal in both groups. There were slightly more failures (1 point) in the study group, but there were equally as many partial failures (2-4 points) in the control group. The average success of the extractions with the Benex extractor was 4.61 points while the average for the classical instruments was 4.55 points. There was no statistical significance between the two groups in the number of successful and failed extractions.
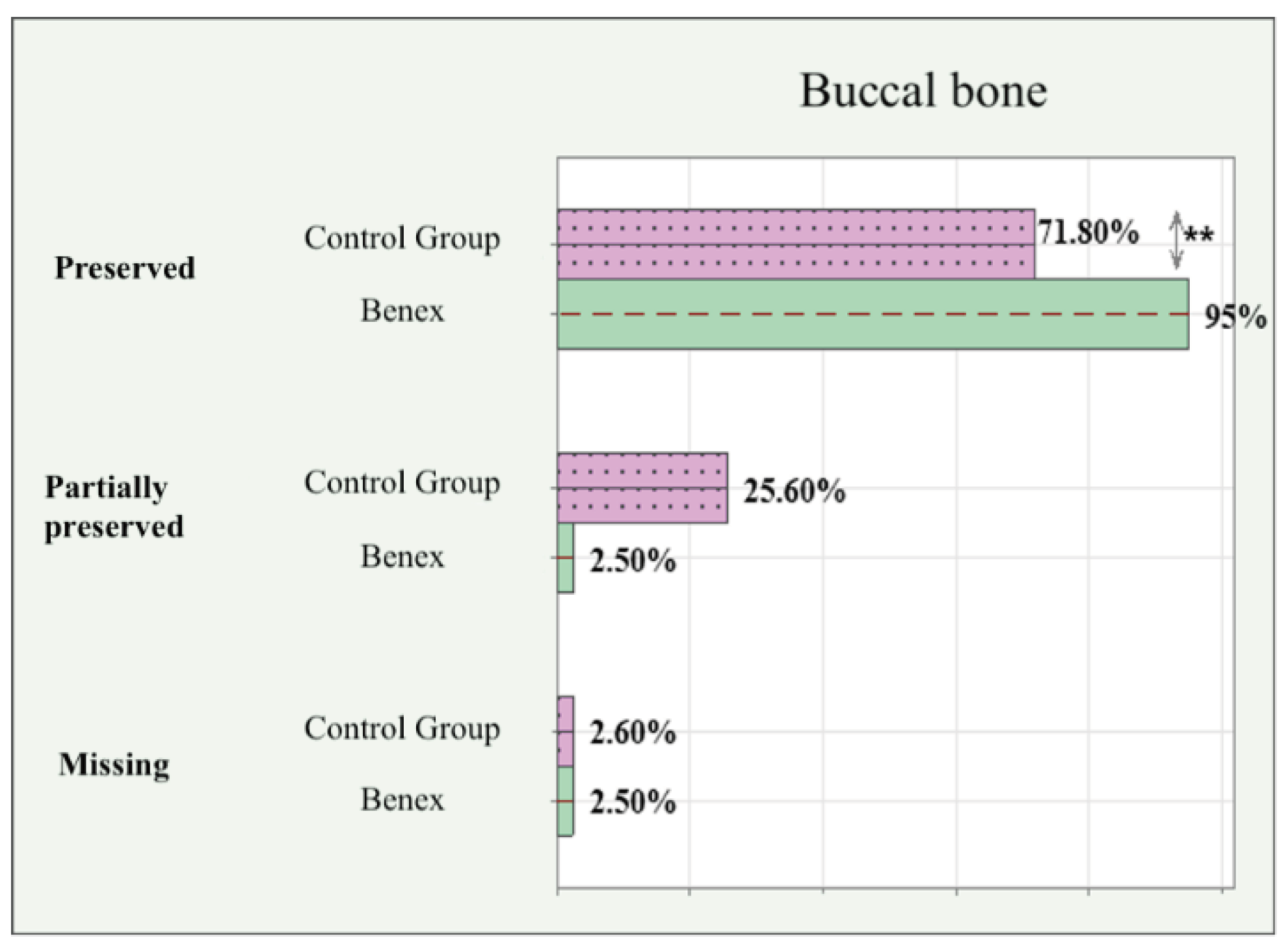
The preservation of buccal cortical bone can be seen in
Figure 4. There was a statistically significant difference in the number of cases where the buccal cortical plate remained intact and completely preserved in the study group. The Benex extractions preserved the buccal cortical plate in 95% of the cases, whereas the forceps extractions only in 71.8%. About one fourth of all extractions in the control group had a partial fracture (<4mm) of the buccal cortical plate. Both groups had and equal number of extractions with completely missing buccal cortical plate (>4mm).
The results for the subjective pain intensity score measured in centimeters on VAS are presented in
Table 1. Both groups show a spike in the pain in the first day after the extraction and gradual improvement in the following days. While the study group shows marginally better results, there is no statistically significant difference.
The healing score based on the early wound healing index (LWHI) can be seen in
Table 2. The Benex extractions showed better healing in all periods where 100% of the extraction wounds had healed
Very Good or Excellent. Only 78.6% of the extraction wounds in the control group had healed
Very Good or Excellent.
4. Discussion
Dental specialists are looking for ways to predictably improve the success of their extractions, while reducing the amount of trauma. The latter is directly correlated with how much hard and soft tissues will be affected and lost during the healing period [
14]. A variety of socket and ridge preservation techniques exist, aimed at reducing the overall bone loss after a tooth extraction. They, however, do not overrule the benefits of atraumatic extraction [
15,
16].
Muska et al.[
17] perform 111 extractions with the Benex extractor with an overall success rate of 83%. Furthermore, based on their judgement about 44% of all teeth would have otherwise required a surgical extraction, which is often not a simple procedure. Hong et al.[
7] extracted a total of 323 teeth with Benex, where 46 were included after a previously unsuccessful extraction with extraction forceps and have a success rate of 85.4%. They extended their study further and performed 1719 extractions with extraction forceps and found 1 out of 5 (22%) cases to require surgical extraction, whereas with the use of Benex only 1 of 20 (6%) required a surgical extraction. In our study, we did not limit the inclusion criteria to teeth with tissues above the bone level but did not include teeth which were directly indicated for open flap surgery before the start of the procedure.
The average success of the Benex extractions in our study was calculated to be 4.61 points, while the same for the classical instruments was 4.55. This shows a marginally better outcome for the Benex extractions. Hong's findings may partially explain the greater extraction success of the Benex device in comparison to the classic extraction forceps. It seems that the Benex extractor excels when it comes to difficult to extract teeth with roots below the level of the surrounding bone, or cases of previously failed extraction with the conventional means.
In our study we included both single and multi-rooted teeth. While there was success with maxillary first premolars, the extraction of molars was incredibly difficult, due to the bulk of the Benex device, even after separating their roots. This coincides with the findings of Muska et al.[
17] who report a success rate of 89% success for teeth with a single root, in comparison to only 43% in multi-rooted teeth. Hong et al.[
7] also conclude that the odds of failure in multi-rooted teeth are about 2.2 times greater.
In our study we found that teeth with previous endodontic treatment were more difficult to extract with Benex and had a higher chance of failure. This is possibly because the root canals were already weakened during the endodontic filing and shaping. Furthermore, such teeth were oftentimes left exposed for a long period of time, and decay or caries could be found inside the root canals. This does not allow the Benex extraction post to be firmly screwed inside the prepared root. This is in conclusion with Hong et al.[
7] who reported that failure rate in endodontically treated teeth was 2.1 times higher.
Other possibility for failure is improper fixation of the root canal screw-post. Muska et al.[
17] found that the second major type of failure was due to insufficient retention of the screw due to operator misjudgment or previously existing fractures and/or caries. However, we noticed that the odds of success can be somewhat improved if the screw penetrates the entire tooth and reaches or slightly engages the bone on the opposing end. This is also supported by Krug et al.[
18] who found perforation in 3 of 51 cases with no lasting damage and complete healing of the periodontium after the extrusion.
Most dental extractions normally heal with mild to no symptoms. However, sometimes the postoperative period can be accompanied by discomfort and different symptoms, including varying degree of pain, temperature, fever and even lead to life threatening situations. Compromised wound healing will not only result in patient complaints and additional appointments but can complicate and even make a following tooth replacement impossible.[
19]
In our study, we followed up the extractions for up to 10 days and evaluated the extraction wound healing using the LWHI. There was statistically significant difference in favor of the Benex extractions. Makki et al.[
20] use the same index follow the patients up to 4 weeks after and their results at the end of this period show that 94.7% of all Benex extraction wounds had healed with a score of 5 or 4, while the extraction forceps had 47.4%. The difference between the success of the extractions with Benex and extraction forceps matches the findings of our study.
It is a well-established fact that after a tooth extraction, the hard and soft tissues undergo remodeling and are ultimately reduced [
21]. The loss of a tooth leads to the initiation of resorption processes, which mainly affect the bone on the buccal side of the extraction site. This bone loss is correlated with the amount of trauma caused during the extraction and the destruction of the existing stem cells in the periodontal space [
22]. Even with the use of different technique for ridge preservation, the soft tissues, too, do not remain unaffected with a predominant change in their buccal contour [
23]. The following bone loss makes implant placement a challenging endeavor, while a subsequent soft tissue recession may expose an already placed implant and compromise its esthetics and life expectancy.
The fact that the Benex system extracts to tooth in a vertical direction puts out an expectation that it is more sparing to the buccal cortical plate. In our study the buccal cortical plate remains intact in 95% of the Benex extractions, compared with only 71.8% for the extraction forceps. We did not find another study in the available literature to compare our results with. Furthermore, the Benex system requires no luxation motions, which causes no additional compression and expansion of hard tissues, or deformation and tearing of soft tissues. This is backed by the findings that the actual force and bone density are not as important as for the success of a tooth extraction, as much as how this force is applied, and the technique used [24].
5. Conclusions
Atraumatic extractions allow for more hard and soft tissues to be preserved in the extraction site. The Benex extractor is a device, which pulls the tooth or root out of the socket, eliminating any trauma to the surrounding bone, and causing minimal to no effect on the soft tissues and their contour. This is all crucial for the successful outcome and aesthetically pleasing results of a following prosthetic or implant restoration. The Benex device, after some initial getting used to, is a tool to predictably achieve these results, even in cases otherwise considered for open surgical extractions.
Author Contributions
Writing – original draft, Lyubomir Chenchev; Supervision, Vasilena Ivanova and Ivan Chenchev; Methodology, Lyubomir Chenchev and Ivan Chenchev; Visualization, Krikor Giragosyan; Formal Analysis, Tasho Gavrailov. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Medical University - Plovdiv (P-3499/21.09.2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- McKenzie, W.S. Principles of Exodontia. Oral and Maxillofacial Surgery Clinics of North America 2020, 32, 511–517. [Google Scholar] [CrossRef]
- Dym, H.; Weiss, A. Exodontia: Tips and Techniques for Better Outcomes. Dental Clinics of North America 2012, 56, 245–266. [Google Scholar] [CrossRef]
- Rafiq, Z.; Vinayakrishna, K.; Sequeira, J.P. Use of Flexible Periotomes and Conventional Periotomes in Atraumatic Extractions: A Comparative Study. OJST 2023, 13, 134–142. [Google Scholar] [CrossRef]
- Kosinski, T. Use of Innovative Physics Forceps for Extractions in Preparation for Dental Implants. Implant News & Views 14.
- Al-Khateeb, T.H.; Alnahar, A. Pain Experience After Simple Tooth Extraction. Journal of Oral and Maxillofacial Surgery 2008, 66, 911–917. [Google Scholar] [CrossRef]
- Kubilius, M.; Kubilius, R.; Gleiznys, A. The preservation of alveolar bone ridge during tooth extraction. 2012, 14, 3–11. [Google Scholar] [PubMed]
- Hong, B.; Bulsara, Y.; Gorecki, P.; et al. Minimally invasive vertical versus conventional tooth extraction. The Journal of the American Dental Association 2018, 149, 688–695. [Google Scholar] [CrossRef] [PubMed]
- Кalyan, S.; Prameela, S.; Bhushan, S.; et al. Clinical and Radiographical Evaluation of the Efficacy of Periotome during Tooth Extractions. IJMSIR 2018, 3, 122–132. [Google Scholar]
- Saund, D.; Dietrich, T. Minimally-invasive tooth extraction: doorknobs and strings revisited! Dental Update 2013, 40, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.-H.; Bae, J.-H. Clinical evaluation of a new extraction method for intentional replantation. JKACD 2011, 36, 211–218. [Google Scholar] [CrossRef]
- Patel, H.S.; Managutti, A.; Menat, S.; et al. Comparative Evaluation of Efficacy of Physics Forceps versus Conventional Forceps in Orthodontic Extractions: A Prospective Randomized Split Mouth Study. JCDR 2016, 10, 41–45. [Google Scholar] [CrossRef]
- Sabri, H.; Barootchi, S.; Heck, T.; et al. Single-rooted extraction socket classification: A systematic review and proposal of a new classification system based on morphologic and patient-related factors. J Esthet Restor Dent 2023, 35, 168–182. [Google Scholar] [CrossRef]
- Lingamaneni, S.; Mandadi, L.; Pathakota, K. Assessment of healing following low-level laser irradiation after gingivectomy operations using a novel soft tissue healing index: A randomized, double-blind, split-mouth clinical pilot study. J Indian Soc Periodontol 2019, 23, 53. [Google Scholar] [CrossRef] [PubMed]
- Menchini-Fabris, G.B.; Toti, P.; Crespi, R.; et al. A Retrospective Digital Analysis of Contour Changing after Tooth Extraction with or without Using Less Traumatic Surgical Procedures. JCM 2022, 11, 922. [Google Scholar] [CrossRef]
- Fickl, S.; Zuhr, O.; Wachtel, H.; et al. Tissue alterations after tooth extraction with and without surgical trauma: a volumetric study in the beagle dog. J Clinic Periodontology 2008, 35, 356–363. [Google Scholar] [CrossRef]
- Oghli, A.A.; Steveling, H. Ridge preservation following tooth extraction: a comparison between atraumatic extraction and socket seal surgery. Quintessence Int 2010, 41, 605–609. [Google Scholar] [PubMed]
- Muska, E.; Walter, C.; Knight, A.; et al. Atraumatic vertical tooth extraction: a proof of principle clinical study of a novel system. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 2013, 116, e303–e310. [Google Scholar] [CrossRef]
- Krug, R.; Connert, T.; Soliman, S.; Syfrig, B.; Dietrich, T.; Krastl, G. Surgical extrusion with an atraumatic extraction system: A clinical study. The Journal of Prosthetic Dentistry 2018, 120, 879–85. [Google Scholar] [CrossRef] [PubMed]
- Makki, A.Z.; Nassar, A.A.; Alharbi, W.M.; et al. Evaluation of post-extraction healing after atraumatic axial tooth extraction using Benex system II versus conventional extraction: Randomized control trial. The Saudi Dental Journal 2021, 33, 923–928. [Google Scholar] [CrossRef]
- Tan, W.L.; Wong, T.L.T.; Wong, M.C.M.; et al. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clinical Oral Implants Res 2012, 23, 1–21. [Google Scholar] [CrossRef]
- Naenni, N. Regeneration von verlorenem Knochen und verlorenem Zahnfleisch. Praxis 2022, 111, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Schneider, D.; Schmidlin, P.R.; Philipp, A.; et al. Labial soft tissue volume evaluation of different techniques for ridge preservation after tooth extraction: a randomized controlled clinical trial. J Clinic Periodontology 2014, 41, 612–617. [Google Scholar] [CrossRef] [PubMed]
- Cicciù, M.; Bramanti, E.; Signorino, F.; et al. Experimental Study on Strength Evaluation Applied for Teeth Extraction: An In Vivo Study. TODENTJ 2013, 7, 20–26. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).