Submitted:
18 March 2024
Posted:
19 March 2024
You are already at the latest version
Abstract
Keywords:
1. Background
2. Methods
3. Results
3.1. Pervasiveness of High Blood Glucose and High blood Pressure
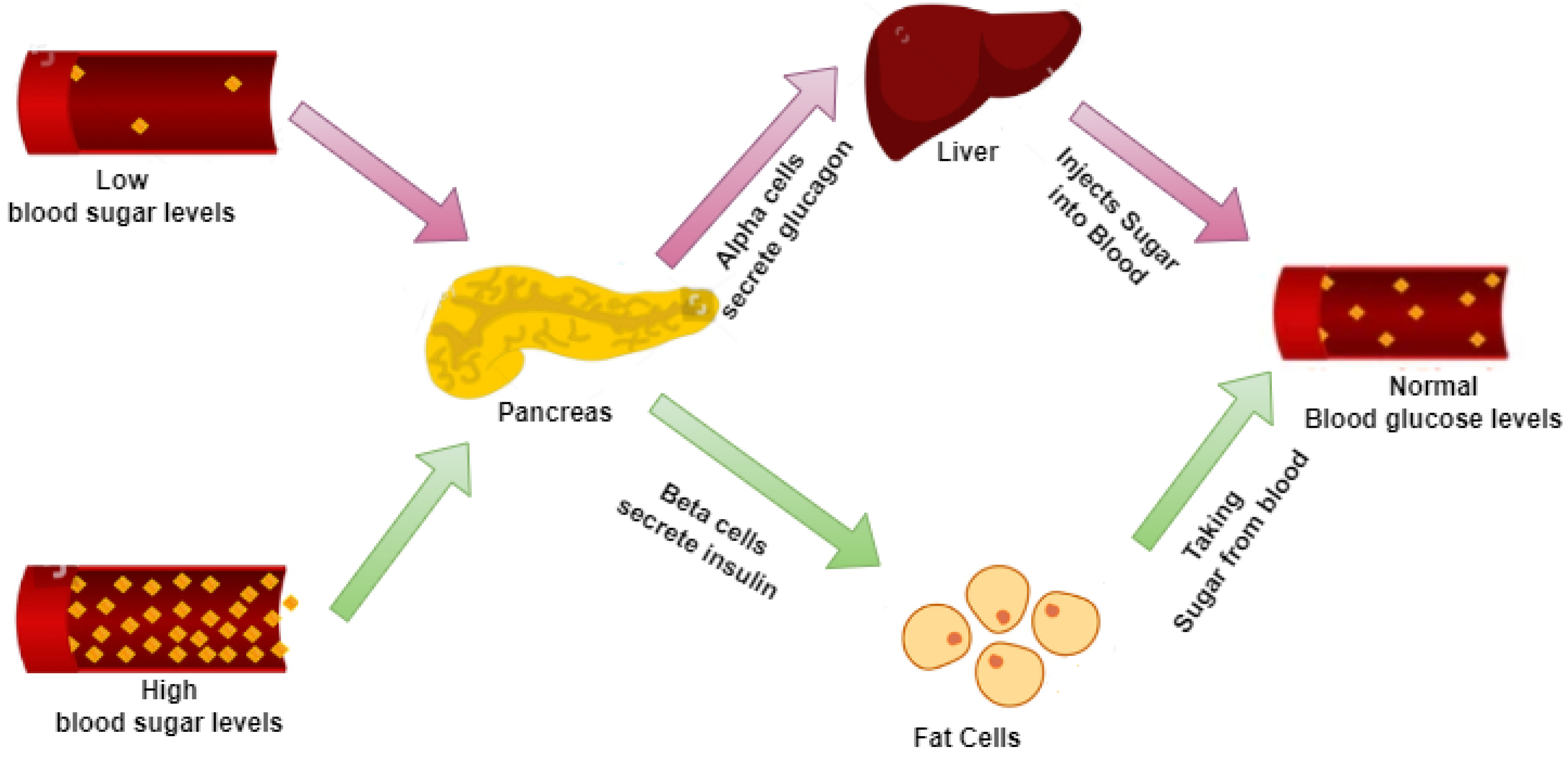
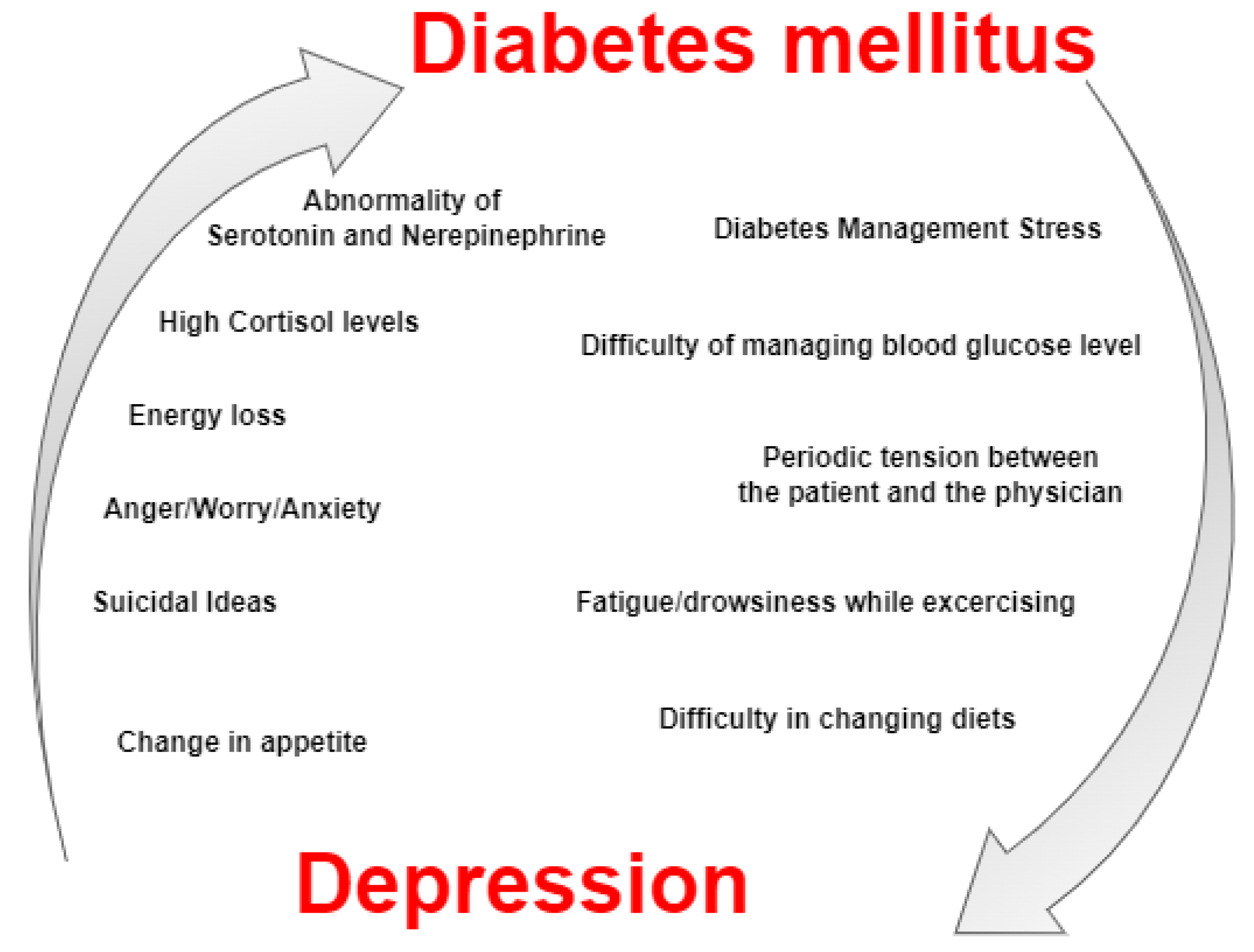
3.2. Bifacial Relationship between Blood Glucose and BP
3.3. Prior Research on Blood Glucose and Blood Pressure
4. Limitations
5. Conclusion
Funding
Data Availability Statement
References
- A. Pan, Q. Sun, O. I. Okereke, K. M. Rexrode, and F. B. Hu. Depression and risk of stroke morbidity and mortality: A meta-analysis and systematic review. JAMA 2011, 306, 1241–1249. [Google Scholar] [CrossRef] [PubMed]
- G. Swapna, K. P. Soman, and R. Vinayakumar. Diabetes Detection Using ECG Signals: An Overview. in Studies in Big Data 2020, 68, 299–327. [CrossRef]
- H. Wu, S. Yang, Z. Huang, J. He, and X. Wang. Type 2 diabetes mellitus prediction model based on data mining. Inform Med Unlocked 2018, 10, 100–107. [Google Scholar] [CrossRef]
- D. Boiroux et al. Overnight glucose control in people with type 1 diabetes. Biomed Signal Process Control 2018, 39, 503–512. [Google Scholar] [CrossRef]
- G. Swapna, K. P. Soman, and R. Vinayakumar. Automated detection of diabetes using CNN and CNN-LSTM network and heart rate signals. in Procedia Computer Science 2018, 132, 1253–1262. [Google Scholar] [CrossRef]
- T. Roy and C. E. Lloyd. Epidemiology of depression and diabetes: A systematic review. J Affect Disord 2012, 142. [Google Scholar] [CrossRef]
- Q. Yang, X. Lang, W. Li, and Y. Liang. The effects of low-fat, high-carbohydrate diets vs. low-carbohydrate, high-fat diets on weight, blood pressure, serum liquids and blood glucose: a systematic review and meta-analysis. European Journal of Clinical Nutrition 2022, 76, 16–27. [Google Scholar] [CrossRef]
- D. Wang et al. Relationship between excess iodine, thyroid function, blood pressure, and blood glucose level in adults, pregnant women, and lactating women: A cross-sectional study. Ecotoxicol Environ Saf 2021, 208. [Google Scholar] [CrossRef]
- J. Liu, L. Liu, Q. Jia, X. Zhang, X. Jin, and H. Shen. Effects of Excessive Iodine Intake on Blood Glucose, Blood Pressure, and Blood Lipids in Adults. Biol Trace Elem Res 2019, 192, 136–144. [Google Scholar] [CrossRef]
- M. Rizka, R. L. Ambardini, L. O. A. Virama, and D. Yudhistira. The Effect of Walking Exercise on Blood Pressure and Blood Glucose in the Elderly. International Journal of Kinesiology and Sports Science 2022, 10, 30–35. [Google Scholar] [CrossRef]
- A. Alloubani, A. Saleh, and I. Abdelhafiz. Hypertension and diabetes mellitus as a predictive risk factors for stroke. Diabetes and Metabolic Syndrome: Clinical Research and Reviews 2018, 12, 577–584. [Google Scholar] [CrossRef] [PubMed]
- L. Schinckus, F. Dangoisse, S. van den Broucke, and M. Mikolajczak. When knowing is not enough: Emotional distress and depression reduce the positive effects of health literacy on diabetes self-management. Patient Educ Couns 2018, 101, 324–330. [Google Scholar] [CrossRef] [PubMed]
- N. H. Cho et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 2018, 138, 271–281. [Google Scholar] [CrossRef] [PubMed]
- M. Yu, X. Zhang, F. Lu, and L. Fang. Depression and Risk for Diabetes: A Meta-Analysis. Can J Diabetes 2015, 39, 266–272. [Google Scholar] [CrossRef] [PubMed]
- R. M. Harbord and J. P. T. Higgins. Meta-regression in Stata. 2008.
- S. K. Mohapatra, J. K. Swain, and M. N. Mohanty. Detection of Diabetes Using Multilayer Perceptron. in Advances in Intelligent Systems and Computing 2019, 846, 109–116. [CrossRef]
- R. B. Pachori, M. Kumar, P. Avinash, K. Shashank, and U. R. Acharya. An improved online paradigm for screening of diabetic patients using RR-interval signals. J Mech Med Biol 2016, 16. [Google Scholar] [CrossRef]
- L. W. Jian and T. C. Lim. Automated detection of diabetes by means of higher order spectral features obtained from heart rate signals. J Med Imaging Health Inform 2013, 3, 440–447. [Google Scholar] [CrossRef]
- U. Rajendra Acharya, O. Faust, N. Adib Kadri, J. S. Suri, and W. Yu. Automated identification of normal and diabetes heart rate signals using nonlinear measures. Comput Biol Med 2013, 43, 1523–1529. [Google Scholar] [CrossRef]
- M. Eadie and R. J. Steele. Non-invasive blood glucose monitoring and data analytics. in ACM International Conference Proceeding Series 2017, F130280, 138–142. [CrossRef]
- P. J. Tully et al. Elucidating the biological mechanisms linking depressive symptoms with type 2 diabetes in men: The longitudinal effects of inflammation, microvascular dysfunction, and testosterone. Psychosom Med 2016, 78, 221–232. [Google Scholar] [CrossRef]
- M. Kivimäki and A. Singh-Manoux. Depressive symptoms, antidepressant use, and the incidence of Diabetes in the black women’s health study. Diabetes care 2014, 37, 2211-2217. Diabetes Care 2015, 38, e22–e23. [Google Scholar] [CrossRef]
- A. G. Logan et al. Mobile Phone-Based Remote Patient Monitoring System for Management of Hypertension in Diabetic Patients. Am J Hypertens 2007, 20, 942–948. [Google Scholar] [CrossRef] [PubMed]
- M. L. Litchman, E. Rothwell, and L. S. Edelman. The diabetes online community: Older adults supporting self-care through peer health. Patient Educ Couns 2018, 101, 518–523. [Google Scholar] [CrossRef] [PubMed]
- G. Swapna, R. Vinayakumar, and K. P. Soman. Diabetes detection using deep learning algorithms. ICT Express 2018, 4, 243–246. [Google Scholar] [CrossRef]
- R. I. G. Holt, D. I. W. Phillips, K. A. Jameson, C. Cooper, E. M. Dennison, and R. C. Peveler. The relationship between depression and diabetes mellitus: Findings from the Hertfordshire Cohort Study. Diabetic Medicine 2009, 26, 641–648. [Google Scholar] [CrossRef] [PubMed]
- E. H. B. Lin et al. Depression and increased mortality in diabetes: Unexpected causes of death. Ann Fam Med 2009, 7, 414–421. [Google Scholar] [CrossRef] [PubMed]
- N. Gendelman et al. Prevalence and correlates of depression in individuals with and without type 1 diabetes. Diabetes Care 2009, 32, 575–579. [Google Scholar] [CrossRef]
- M. M. Collins, P. Corcoran, and I. J. Perry. Anxiety and depression symptoms in patients with diabetes: Original Article: Psychology. Diabetic Medicine 2009, 26, 153–161. [Google Scholar] [CrossRef]
- A. Nouwen et al. Type 2 diabetes mellitus as a risk factor for the onset of depression: A systematic review and meta-analysis. Diabetologia 2010, 53, 2480–2486. [Google Scholar] [CrossRef]
- F. Pouwer et al. Prevalence of comorbid depression is high in out-patients with Type 1 or Type 2 diabetes mellitus. Results from three out-patient clinics in the Netherlands. Diabetic Medicine 2010, 27, 217–224. [Google Scholar] [CrossRef]
- A. Pan et al. Bidirectional association between depression and type 2 diabetes mellitus in women. Arch Intern Med 2010, 170, 1884–1891. [Google Scholar] [CrossRef]
- N. Renn, L. Feliciano, and D. L. Segal. The bidirectional relationship of depression and diabetes: A systematic review. Clinical Psychology Review 2011, 31, 1239–1246. [Google Scholar] [CrossRef] [PubMed]
- A. M. Paddison et al. Predictors of anxiety and depression among people attending diabetes screening: A prospective cohort study embedded in the ADDITION (Cambridge) randomized control trial. Br J Health Psychol 2011, 16, 213–226. [Google Scholar] [CrossRef] [PubMed]
- R. C. Hermida, D. E. Ayala, A. Mojoń, and J. R. Fernańdez. Influence of time of day of blood pressure-lowering treatment on cardiovascular risk in hypertensive patientswith type 2 diabetes. Diabetes Care 2011, 34, 1270–1276. [Google Scholar] [CrossRef] [PubMed]
- S. S. Franklin et al. Masked Hypertension in Diabetes Mellitus: Treatment Implications for Clinical Practice Europe PMC Funders Group. Hypertension 2013, 61, 964–971. [Google Scholar] [CrossRef] [PubMed]
- Or and, D. Tao. A 3-Month Randomized Controlled Pilot Trial of a Patient-Centered, Computer-Based Self-Monitoring System for the Care of Type 2 Diabetes Mellitus and Hypertension. J Med Syst 2016, 40, 1–13. [Google Scholar] [CrossRef]
- W. Katon, M. Y. Fan, J. Unützer, J. Taylor, H. Pincus, and M. Schoenbaum. Depression and diabetes: A potentially lethal combination. J Gen Intern Med 2008, 23, 1571–1575. [Google Scholar] [CrossRef] [PubMed]
- E. Lloyd, G. Pambianco, and T. J. Orchard. Does diabetes-related distress explain the presence of depressive symptoms and/or poor self-care in individuals with Type 1 diabetes? Diabetic Medicine 2010, 27, 234–237. [Google Scholar] [CrossRef]
- M. Yu, X. Zhang, F. Lu, and L. Fang. Depression and Risk for Diabetes: A Meta-Analysis. Can J Diabetes 2015, 39, 266–272. [Google Scholar] [CrossRef]
- Monte-Moreno. Non-invasive estimate of blood glucose and blood pressure from a photoplethysmograph by means of machine learning techniques. Artif Intell Med 2011, 53, 127–138. [Google Scholar] [CrossRef]
- Z. D. Khan, J. Lutale, and S. M. Moledina. Prevalence of Depression and Associated Factors among Diabetic Patients in an Outpatient Diabetes Clinic. Psychiatry J 2019, 2019, 1–6. [Google Scholar] [CrossRef] [PubMed]
- B. Chireh, M. Li, and C. D’Arcy. Diabetes increases the risk of depression: A systematic review, meta-analysis and estimates of population attributable fractions based on prospective studies. Preventive Medicine Reports 2019, 14. [Google Scholar] [CrossRef]
- G. Z. Réus, M. A. B. dos Santos, A. P. Strassi, H. M. Abelaira, L. B. Ceretta, and J. Quevedo. Pathophysiological mechanisms involved in the relationship between diabetes and major depressive disorder. Life Sciences 2017, 183, 78–82. [Google Scholar] [CrossRef]
- M. A. Atkinson, B. O. Roep, A. Posgai, D. C. S. Wheeler, and M. Peakman. The challenge of modulating β-cell autoimmunity in type 1 diabetes. The Lancet Diabetes and Endocrinology 2019, 7, 52–64. [Google Scholar] [CrossRef] [PubMed]
- J. Karduck and K. Chapman-Novakofski. Results of the Clinician Apps Survey, How Clinicians Working With Patients With Diabetes and Obesity Use Mobile Health Apps. J Nutr Educ Behav 2018, 50, 62–69. [Google Scholar] [CrossRef]
- L. Bowman et al. ASCEND: A Study of Cardiovascular Events iN Diabetes: Characteristics of a randomized trial of aspirin and of omega-3 fatty acid supplementation in 15,480 people with diabetes. Am Heart J 2018, 198, 135–144. [Google Scholar] [CrossRef] [PubMed]
- M. Fang. Trends in the Prevalence of Diabetes Among U.S. Adults: 1999–2016. Am J Prev Med 2018, 55, 497–505. [Google Scholar] [CrossRef]
- U. R. Acharya et al. An integrated diabetic index using heart rate variability signal features for diagnosis of diabetes. Comput Methods Biomech Biomed Engin 2013, 16, 222–234. [Google Scholar] [CrossRef]
- O. Faust, U. R. Acharya, F. Molinari, S. Chattopadhyay, and T. Tamura. Linear and non-linear analysis of cardiac health in diabetic subjects. in Biomedical Signal Processing and Control 2012, 7, 295–302. [CrossRef]
- G. Swapna, U. Rajendra Acharya, S. Vinithasree, and J. S. Suri. Automated detection of diabetes using higher order spectral features extracted from heart rate signals. Intelligent Data Analysis 2013, 17, 309–326. [Google Scholar] [CrossRef]
- P. A. Duodu, P. Agbadi, H. O. Duah, E. Darkwah, and J. J. Nutor. Correlates of blood pressure and blood glucose screenings in Cameroon: Insights from the 2018 Demographic and Health Survey. Int Health 2022, 14, 201–210. [Google Scholar] [CrossRef]
- S. Wild et al. Global Prevalence of Diabetes Estimates for the year 2000 and projections for 2030. 2004. [Online]. Available: http://diabetesjournals.org/care/article-pdf/27/5/1047/566025/zdc00504001047.pdf.
- U. R. Acharya, H. Fujita, S. L. Oh, Y. Hagiwara, J. H. Tan, and M. Adam. Application of deep convolutional neural network for automated detection of myocardial infarction using ECG signals. Inf Sci (N Y) 2017, 415–416, 190–198. [Google Scholar] [CrossRef]
- M. M. Islam, M. J. Rahman, D. Chandra Roy, and M. Maniruzzaman. Automated detection and classification of diabetes disease based on Bangladesh demographic and health survey data, 2011 using machine learning approach. Diabetes and Metabolic Syndrome: Clinical Research and Reviews 2020, 14, 217–219. [Google Scholar] [CrossRef] [PubMed]
- Z. Xie, O. Nikolayeva, J. Luo, and D. Li. Building risk prediction models for type 2 diabetes using machine learning techniques. Prev Chronic Dis 2019, 16. [Google Scholar] [CrossRef]
- “Diagnosis and classification of diabetes mellitus. Diabetes Care 2010, 33 (Suppl. S1), Suppl–S1. [CrossRef]
- Gahlan, R. Rajput, and V. Singh. Metabolic syndrome in north Indian type 2 diabetes mellitus patients: A comparison of four different diagnostic criteria of metabolic syndrome. Diabetes and Metabolic Syndrome: Clinical Research and Reviews 2019, 13, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Md. A. Uddin. Factors Influencing in Developing Type II Diabetes among Married Women in Bangladesh: Data from Bangladesh Demographic and Health Survey 2011. JOURNAL OF LIFE SCIENCES 2019, 11. [Google Scholar] [CrossRef]
- M. Maniruzzaman et al. Accurate Diabetes Risk Stratification Using Machine Learning: Role of Missing Value and Outliers. J Med Syst 2018, 42. [Google Scholar] [CrossRef]
- M. Maniruzzaman, M. J. Rahman, B. Ahammed, and M. M. Abedin. Classification and prediction of diabetes disease using machine learning paradigm. Health Inf Sci Syst 2020, 8. [Google Scholar] [CrossRef]
- R. Ashisha, X. Anitha Mary, and L. Rose. Design challenges for embedded based wireless postoperative bedside monitoring system. Journal of Interdisciplinary Mathematics 2020, 23, 285–292. [Google Scholar] [CrossRef]
- R. Ashisha, X. Anitha Mary, K. Rajasekaran, and R. Jegan. IoT-Based Continuous Bedside Monitoring Systems. in Advances in Intelligent Systems and Computing 2019, 750, 401–410. [CrossRef]
- M. Gusev et al. Noninvasive Glucose Measurement Using Machine Learning and Neural Network Methods and Correlation with Heart Rate Variability. Journal of Sensors 2020, 2020. [Google Scholar] [CrossRef]
- “Non-invasive blood glucose testing: the horizon. 2016. [Online]. Available: www.hsric.nihr.ac.uk.
- Lee et al. B I O E N G I N E E R I N G Wearable/disposable sweat-based glucose monitoring device with multistage transdermal drug delivery module.” [Online]. Available: http://advances.sciencemag.org/.
- S. Emaminejad et al. Autonomous sweat extraction and analysis applied to cystic fibrosis and glucose monitoring using a fully integrated wearable platform. Proc Natl Acad Sci U S A 2017, 114, 4625–4630. [Google Scholar] [CrossRef] [PubMed]
- C. Todd, P. Salvetti, K. Naylor, and M. Albatat. Towards non-invasive extraction and determination of blood glucose levels. Bioengineering 2017, 4. [Google Scholar] [CrossRef]
- Azhar, S. W. Gillani, G. Mohiuddin, and R. A. Majeed. A systematic review on clinical implication of continuous glucose monitoring in diabetes management. Journal of Pharmacy and Bioallied Sciences 2020, 12, 102–111. [Google Scholar] [CrossRef] [PubMed]
- I. E. Forde, S. Browne, D. Smith, and W. P. Tormey. Glucose sensing technology—current practice? Irish Journal of Medical Science 2019, 188, 125–127. [Google Scholar] [CrossRef] [PubMed]
- H. B. Chandalia and B. R. Boshell. Diagnosis of Diabetes The Size and Nature of Carbohydrate Load.” [Online]. Available: http://diabetesjournals.org/diabetes/article-pdf/19/11/863/345217/19-11-863.pdf.
- O. Schlesinger, N. Vigderhouse, D. Eytan, and Y. Moshe, BLOOD PRESSURE ESTIMATION FROM PPG SIGNALS USING CONVOLUTIONAL NEURAL NETWORKS AND SIAMESE NETWORK. [Online]. Available: http://sipl.technion.ac.il/.
- Z. Taha, L. Shirley, and M. A. Mohd Razman. A review on non-invasive hypertension monitoring system by using photoplethysmography method. Movement, Health & Exercise 2017, 6. [Google Scholar] [CrossRef]
- R. Samria, R. Jain, A. Jha, S. Saini, and S. R. Chowdhury, Noninvasive Cuffless Estimation of Blood Pressure using Photoplethysmography without Electrocardiograph Measurement.
- Liu, L. Liu, Q. Jia, X. Zhang, X. Jin, and H. Shen. Effects of Excessive Iodine Intake on Blood Glucose, Blood Pressure, and Blood Lipids in Adults. Biol Trace Elem Res 2019, 192, 136–144. [Google Scholar] [CrossRef]
- M. Barale, V. Cappiello, E. Ghigo, and M. Procopio. Increased frequency of impaired fasting glucose and isolated systolic hypertension in Paget’s disease of bone. Endocrine 2019, 63, 385–390. [Google Scholar] [CrossRef]
- C. A. Emdin, S. G. Anderson, M. Woodward, and K. Rahimi. Usual Blood Pressure and Risk of New-Onset Diabetes Evidence From 4.1 Million Adults and a Meta-Analysis of Prospective Studies. 2015.
- D. Ettehad et al. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. The Lancet 2016, 387, 957–967. [Google Scholar] [CrossRef]
- I. Zhou, C. Liu, P. Shan, Y. Zhou, E. Xu, and Y. Ji. Prevalence and distinguishing features of masked hypertension in type 2 diabetic patients. J Diabetes Complications 2013, 27, 82–86. [Google Scholar] [CrossRef] [PubMed]
- J. Lee, S. Yang, S. Lee, and H. C. Kim. Analysis of pulse arrival time as an indicator of blood pressure in a large surgical biosignal database: Recommendations for developing ubiquitous blood pressure monitoring methods. J Clin Med 2019, 8. [Google Scholar] [CrossRef]
- P. Muntner et al. Measurement of blood pressure in humans: A scientific statement from the american heart association. Hypertension 2019, 73, E35–E66. [Google Scholar] [CrossRef]
- C. Edeoga et al. Relationships between blood pressure and blood glucose among offspring of parents with type 2 diabetes: Prediction of incident dysglycemia in a biracial cohort. J Diabetes Complications 2017, 31, 1580–1586. [Google Scholar] [CrossRef]
- J. R. Petrie, T. J. 83. J. R. Petrie, T. J. Guzik, and R. M. Touyz. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Canadian Journal of Cardiology 2018, 34, 575–584. [Google Scholar] [CrossRef] [PubMed]
- S. P. Chatrati et al. Smart home health monitoring system for predicting type 2 diabetes and hypertension. Journal of King Saud University - Computer and Information Sciences 2022, 34, 862–870. [Google Scholar] [CrossRef]
- E. A. Graham, S. S. Deschênes, M. N. Khalil, S. Danna, K. B. Filion, and N. Schmitz. Measures of depression and risk of type 2 diabetes: A systematic review and meta-analysis. Journal of Affective Disorders 2020, 265, 224–232. [Google Scholar] [CrossRef]

| Characteristics | T1D | T2D |
| Age | Above 40 years | Above 50 years |
| Length of symptoms | Many weeks | Many weeks to many years |
| Weight | underweight or Normal | Overweight |
| If not treated | death | No immediate death |
| Diabetic family history | Mostly No | Mostly Yes |
| Authors | Blood Glucose Evaluation Methods | Blood Pressure Evaluation Methods | Results |
| Ref [26] | Hospital Anxiety and Depression Scale | WHO standard | The linkage is there between high blood glucose and high blood pressure. The study also finds that there is a association between depression, blood glucose, and insulin concentration in males. High blood pressure can lead to Diabetes. |
| Ref [27] | Patient Health Questionnaire (PHQ-9) | Clinical Records | People with T2D and high blood pressure facing high mortality chances. After adjusting some clinical characteristics, little high pressure is not showing a significant relationship with mortality risk. |
| Ref [28] | Beck Depression Inventory II | Clinical Records | The commonness of high blood pressure is higher in type 1 diabetic patients. The pervasiveness of high blood glucose is significantly high in patients affected by high blood pressure. |
| Ref [29] | Hospital Anxiety and Depression Scale (HADS) | Clinical Records | People having high blood pressure are at a higher chance of getting depression. |
| Ref [30] | Self-report | Self-report, medical record or fasting plasma glucose test (FPG) | Patients with type 2 Diabetes has a 24% risk of getting depression. |
| Ref [31] | World Health Organization-5Well Being Index (WHO-5), Centre for Epidemiologic Studies-Depression scale (CESD), Composite International Diagnostic Interview (CIDI) |
Self-Report, Diagnostic Interview | Depression is a common problem in Type 1 Diabetes and Type 2 Diabetes. There is an increased risk for women affected by Type 2 Diabetes, uncontrollable Type 1 Diabetic Patients, and those who are with diabetic complications. |
| Ref [32] | 5-item Mental Health Index (MHI-5) | Self-Report, Medical Record Review | In depression patients the risk for T2D is high. Alternatively, patients with high blood glucose have a higher risk of developing high blood pressure. |
| Ref [33] | Psychiatric interview, Self-Report | fasting plasma glucose test (FPG), Self-Report, Medical Records | The association between BP and blood glucose are well explained in the literature, but the exact evidence for the association is unclear. |
| Ref [34] | Hospital Anxiety and Depression Scale | WHO Standards | The diabetes testing result was not associated with depression at a 12-month follow-up. The maximum number of self-reports of high blood glucose symptoms was related to depression. |
| Ref [12] | Diabetes website | Self-Report | The health study and the self-effectiveness have direct positive contact with Diabetes. But this positive impact will disappear if the person is affected by depression or high blood pressure. |
| Ref [35] | Bedtime Treatment | Bedtime Treatment | Bedtime treatment with ≥1 blood pressure-reducing medication, enhance BP control, and also reduces the heart-related risk in any patient affected by hypertension and T2 Diabetes. |
| Ref [6] | Systemic Review | Systemic Review | Depression is developing in patients with high blood glucose. But more studies are needed for providing a clear view of the relationship between DM and high BP. |
| Ref [36] | Population-based 11-country International Database |
Population-based 11-country International Database |
29% untreated diabetic patients having masked hypertension and heart-related issues as stage 1 hypertension patient and they need a reasonable reduction in their blood pressure. |
| Ref [37] | Self-Monitoring | Self-Monitoring | The study of three months about the self-monitoring of T2D and hypertension concludes that by using the computer-based self-monitoring systems hypertension can be controlled. |
| Ref [38] | Health Assessment Questionnaire Survey | Self-Report or Clinical Diagnosis | Comorbid depression creates increasing death rates. There is a need for research to find whether the increase in death rate connected with blood pressure is because of a patient's behavior (poor diet, smoking habit) or physical problems correlated with high blood pressure. |
| Ref [39] | Problem Areas in Diabetes (PAID) scale |
Center for Epidemiologic Studies Depression (CES-D) Scale, Beck Depression Inventory (BDI) |
There may be an important impact of high blood pressure on Diabetes. |
| Ref [40] | Egger regression asymmetry test | Egger regression asymmetry test | The patient with high blood pressure has 41% of increasing risk factors for DM and also 32% of increasing risk factors of T2D. The linkage is not clear and so further research is required to prove this result. |
| Ref [22] | Black Women’s Health Study (BWHS) | Black Women’s Health Study (BWHS) | Depression disorder or depression symptoms and the usage of antidepressants has a relationship with the development of Diabetes. |
| Ref [41] | Photoplethysmograph sensor | Photoplethysmograph sensor | This system detects the blood pressure and blood glucose from s PPG sensor. But in 1.9% of cases this system is not properly detecting blood glucose. |
| Ref [42] | 9-item Patient Health Questionnaire (PHQ 9) scale |
9-item Patient Health Questionnaire (PHQ 9) scale |
A larger number of diabetic patients are with the slightest depression and also about 30% of them had mild or moderate depression. Patients with smoking habits and also patients taking insulin treatment are completely related with experiencing mild or moderate hypertension. |
| Ref [43] | Longitudinal Studies | Longitudinal Studies | High blood glucose is a risk element of developing depression. Depressive disorder is maximum in diabetic patients compared to peope without Diabetes. This depression risk is because of the repetition of depression in patients with depression history or due to diabetes complications. |
| Ref [44] | Longitudinal Studies | Longitudinal Studies | People with Major Depressive Disorder (MDD) are having a higher risk of developing Diabetes mellitus (DM) than those are without MDD. But many diabetic patients will not be diagnosed with depressive disorder. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




