1. Introduction
Gestational diabetes mellitus (GDM) is defined as hyperglycemia diagnosed during pregnancy that does not meet the criteria for overt diabetes. It is a highly prevalent condition and is associated with adverse maternal-fetal outcomes [
1]. The most widely accepted diagnostic criteria are based on those defined by the HAPO study, and screening for the disease is recommended for all pregnant women [
2].
The treatment of the disease includes nutritional counseling, physical activity, glycemic control, and pharmacological therapy when indicated. However, adherence to the diet is challenging. Understanding the need to adapt habits, consistency, and adjustment according to cultural, socioeconomic, and lifestyle issues are common challenges, often with a frustrating approach [
3].
In recent decades, the use of digital media has spread in every corner of the world. Digital media are tools that facilitate interaction among people of various age groups, allowing individuals to share information, ideas, images, and form teams by adding other users simultaneously. They are also involved in healthcare delivery and health promotion [
4].
Using these means within nutritional education can strengthen the professional-patient relationship and increase adherence to recommended guidelines. However, what has been observed is that the spread of lay content can complicate and confuse nutritional treatment since there's a lot of false content and misinformation [
5]. Nutritionists, therefore, play a crucial role in disseminating reliable information and enhancing their relationship with patients.
For diabetic pregnant women, the obstetric outcome is directly related to glycemic control. The most commonly used method for monitoring blood glucose is self-monitoring using daily capillary blood glucose. Dietary adjustments, physical activity, and blood glucose monitoring contribute to improved maternal and perinatal outcomes [
6,
7].
With the rapid advancement of technology and the subsequent widespread use of smartphones, there has been a significant increase in the number of smartphone apps available in the market for various purposes, including interventions for diabetes. A quick online search can uncover various health-related smartphone apps, ranging from those assisting in the management of specific diseases, such as diabetes, to others monitoring sleep quality, providing healthy living tips, aiding in diet execution, assisting with physical activities, or even following the day-to-day journey of pregnant women from the beginning to the end of their pregnancy [
8]. Apps can, therefore, be allies in implementing treatments and adopting a healthy lifestyle, and many have been studied in diabetic patient care [
9,
10].
One of the most popular and widely used apps is WhatsApp, an instant messaging application considered a straightforward, affordable, and effective means of communication. Hence, if nutritional care mediated by digital media tools could improve the diet and glycemic control of women with GDM, we proposed this research. The primary objective was to evaluate the use of digital media as a complementary strategy to outpatient nutritional counseling in women with GDM. We assessed glycemic control, the need for pharmacological treatment, and dietary intake.
2. Materials and Methods
Randomized clinical trial, blinded for the patient, carried out at the Diabetes and Pregnancy Outpatient Clinic of Hospital São Paulo – Paulista School of Medicina / Federal University of São Paulo (EPM-UNIFESP) - from February 2021 to January 2023. Pregnant women who met the GDM diagnosis criteria according to the International Association of the Diabetes and Pregnancy Study Groups (IADPSG) (11), defined by: fasting glucose ≥92 mg/dl and <126 mg/dl at the start of prenatal care, or at least one altered point in the 75g OGTT performed between 24 and 28 weeks, namely: fasting ≥92 mg/dl, one hour ≥180mg/dl, or two-hour value ≥153mg/dl were invited. Inclusion criteria were: gestation between 24 and 34 weeks at the time of study entry, forecasted follow-up at the clinic for at least 4 weeks, single gestation with a living fetus, personal mobile phone, literate patient, and capable of using the WhatsApp app. Exclusions were women who could not recall consumed food, pregnant women prescribed drug treatment at the first consultation, patients with digestive system pathologies, a history of any type of bariatric surgery, or those who discontinued clinic follow-up in less than 4 weeks. All women were informed about the study and signed the Informed Consent Form. This study was approved by the Ethics Committee for Research of UNIFESP (CAAE: 30104820.6.0000.5505).
To assess the effectiveness of digital media in the glycemic control of women with GDM, two groups were formed, termed the Intervention Group (IG) and the Control Group (CG). Randomization was done by drawing lots. Upon entering the study, all patients completed a sociodemographic questionnaire, attended an initial lecture on nutrition and glycemic control in GDM, and performed the first standardized 24-hour dietary recall (R24), termed R24 baseline (T0).
Patients in the intervention group (IG), in addition to outpatient guidance, also received six daily reminders with nutritional tips via the WhatsApp app at mealtimes: breakfast, mid-morning snack, lunch, afternoon snack, dinner, and supper. We did not use WhatsApp groups; messages were sent individually. Reminders varied daily but always covered the same topics, were sent at the same times, and could repeat over time. No response was requested, and no message viewing control was implemented. This intervention lasted 4 to 8 weeks, depending on the patient's follow-up duration at the clinic. Reminders were sent until the end of prenatal care. CG patients did not receive reminders, but all women had in-person nutritional consultations as needed, either indicated by the multidisciplinary team or sought spontaneously. Consultations evaluated the diet and clarified doubts.
Following the initial 24-hour recall (T0), new recalls were made at intervals 1,2,3,4, and 5, on average ten days apart, through phone calls by the researcher. Patients reported their previous day's intake, and the researcher noted the type and quantity of food consumed. The number of recalls depended on the patient's follow-up duration at the clinic, with recalls named after each follow-up week: T1 for the 1st week, T2 for the 2nd week, and so on up to T5.
Caloric intake, macronutrients, and fiber were calculated using DietPro software, referencing the Brazilian Table of Food Chemical Composition (TACO), the Food Composition Table of the Brazilian Institute of Geography and Statistics (IBGE), and the United States Department of Agriculture (USDA) Table. Initially, this calculation was performed for T0 and then weekly, based on follow-up recalls. Calculations were conducted identically for both study groups.
Glycemic control was assessed by the outpatient clinic's obstetricians and endocrinologists during weekly or bi-weekly returns, depending on each patient's needs. Home-recorded capillary blood glucose levels were considered. Glycemic control targets were fasting glucose up to 95 mg/dl and 1h post-meal up to 140 mg/dl, with 4 daily readings advised. Control was deemed adequate if at least 80% of measurements met targets. If targets were not met or if there were signs of fetal hyperglycemia, drug treatment was indicated, and the patient continued regular follow-up. The number of follow-up weeks varied based on gestational age at study entry and each woman's individual needs. The last assessment was made during the last prenatal consultation before delivery.
For sociodemographic variable analysis, factors as age, number of pregnancies, initial body mass index (BMI), race, marital status, smoking, alcohol consumption, and physical activity were considered. The outcomes analyzed were glycemic control, the need for drug treatment, and food intake.
Glycemic control was deemed adequate when at least 80% of measurements met targets, inadequate if less than 80%, or not performed if the patient had completed fewer than 50% of the recommended readings. Drug treatment was categorized as "yes" or "no", depending on whether the patient was prescribed insulin at any point during follow-up. For food intake assessment, caloric intake, proteins, lipids, carbohydrates, and fiber were calculated. The sample was of convenience. For sample size calculation, a statistical significance of 5% was considered, with an 80% test power and an effect size of 0.65. This led to a minimum sample size of 78 women. Data were tabulated in Excel 2010 (Microsoft Corp. Redmond, WA, USA) and analyzed using the SPSS version 22.0 (SPSS Inc., Chicago, IL, USA). For result analysis, numerical variables were presented: mean and standard deviation, median, and range (interquartile range). Categorical ones were presented in absolute (n) and relative (%) frequencies. Normality was verified using the Kolmogorov–Smirnov test. To compare numerical variables between groups, the Mann-Whitney test was applied, and for categories, the Fisher's Exact Test or Chi-squared Test, depending on frequency distribution. Values of p≤0.05 were considered significant. To compare nutritional intake variables at T0 and during follow-up, the paired Wilcoxon Test was used.
3. Results
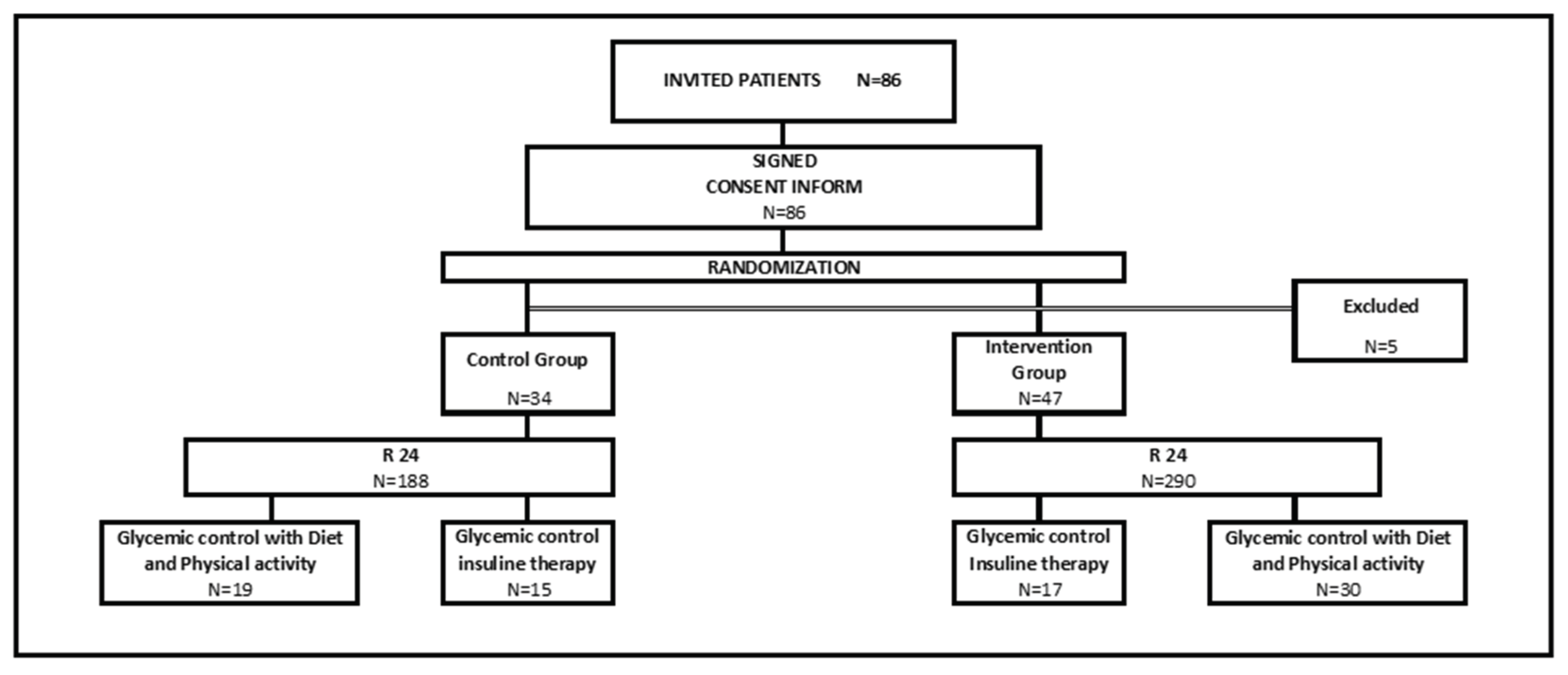
Eighty-six women agreed to participate in the study, but 5 were excluded for not meeting the minimum follow-up criteria. Thirty-four were randomized to the IG and 47 to the CG. A total of 188 24-hour dietary recalls (R24) were conducted in the control group and 290 in the intervention group. All the pregnant women were followed until the last consultation before delivery. This data is represented in
Figure 1.
The age of the patients ranged from 18 to 46 years, with an average of 34.3 years (SD 5.6). The majority identified themselves as mixed race (39.5%) and were married (55.6%). The number of pregnancies ranged from 1 to 8, with an average of 3.1 pregnancies (SD 1.5). The patients in the IG were slightly younger (33.4 vs. 35.5) and slimmer (BMI 28.8 vs. 31.1) than those in the CG, but there were no statistically significant differences in sociodemographic variables between the two groups. This data is represented in
Table 1. The majority were non-smokers (92.6%), non-drinkers (95.1%), and did not engage in physical activity (75.3%), with no differences between the two groups.
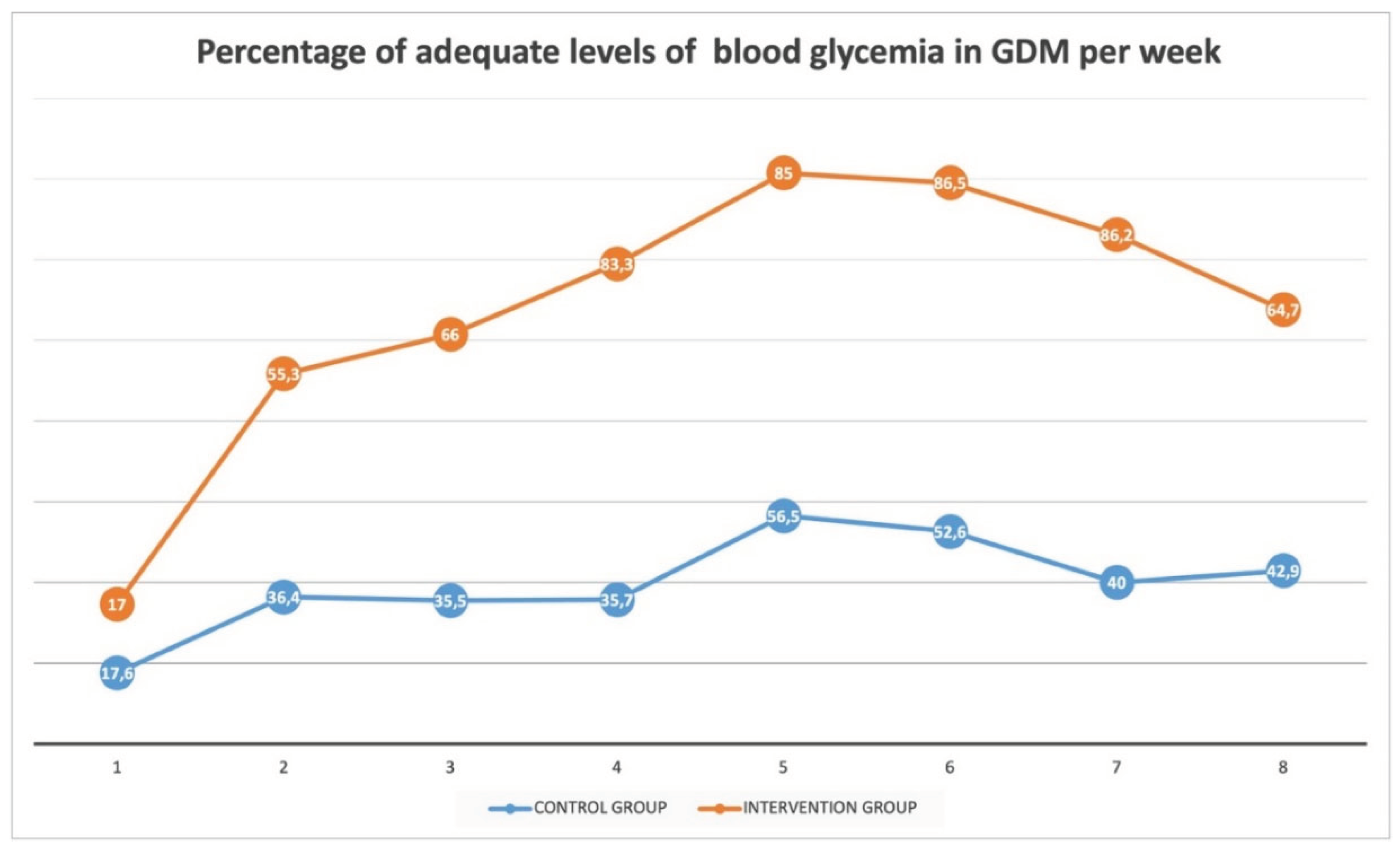
Glycemic control and the need for insulin were evaluated weekly. In the IG, the percentage of women who demonstrated adequate control was higher than in the CG during the third, fourth, fifth, and sixth weeks of follow-up, with a significant difference (p-value < 0.005). This data is represented in the
Table 2. The percentage of patients with adequate glucose blood levels can be accessed in
Figure 2, is possible to observe that the difference is increasing during the study.
Of the total women evaluated, 39.5% required insulin therapy, with 44.1% from the CG and 36.2% from the IG, with no differences between the groups (p-value = 0.498), despite a slightly lower percentage of women from the intervention group requiring drug treatment. No woman was treated with oral antidiabetic drugs.
To assess dietary intake, the groups were compared at each evaluation point. The intake at baseline was labeled T0, and subsequent ones were named according to the follow-up week, generating recalls from T0 to T5. The average recalls of all patients at each evaluation point were calculated for each variable analyzed: calories, proteins, carbohydrates, lipids, and fibers. Moreover, we assessed consumption in the last recall made by each woman, regardless of the follow-up week it was conducted, and termed it Final Time (FT). There was no difference in caloric intake between the two groups at any follow-up point. There were some differences in macronutrient consumption: higher protein intake at T4 and TF in the IG; higher carbohydrate intake at T1 and T4 in the IG; Higher lipid intake at T4, T5, and TF in the IG; higher fiber intake at T1 and TF in the intervention group, although the IG already had a higher fiber intake at the time of study inclusion. The dietary intake data is represented in
Table 3.
To assess if patients altered their dietary patterns during pregnancy, we compared caloric and macronutrient consumption at two points: baseline (T0) and the last recall conducted (FT), within each group and between the two groups. The data were expressed as mean and median. The IG decreased carbohydrate and fiber intake, and both groups increased lipid consumption during the follow-up, with this increase being more pronounced in the IG (
Table 3). When comparing the two groups regarding the change in consumption throughout the follow-up, we noted that the lipid intake increase in the IG was significantly greater than in the CG. There were no differences for the other parameters.
4. Discussion
A higher percentage of pregnant women showed adequate glycemic control in the third, fourth, fifth, and sixth weeks of follow-up, with no statistically significant difference regarding the need for insulin. Concerning dietary intake, both groups increased lipid consumption, and the IG consumed more proteins and carbohydrates at specific weeks. There were no differences in caloric intake. The groups were homogeneous in terms of clinical and sociodemographic characteristics, which were consistent with the risk factors associated with GDM [
12].
Conducting R24 by phone is plausible and had been evaluated even before the widespread use of smartphones [
13]. It's a practical and straightforward tool, which nowadays can be even more reliable through photo documentation. It was a valuable method, especially since this research was mostly conducted during the COVID-19 pandemic, with phone or virtual contact being strongly recommended during this period [
14].
Furthermore, the COVID-19 pandemic profoundly influenced the population's habits in several respects: family routine, confinement, loss of income, fear of the disease, and restricted access to health services. Stressful situations, like the one experienced during the pandemic, can lead to overeating and anxiety, increasing the consumption of certain foods, especially those high in sugars [
15]. Chinese researchers have shown that pregnant women from areas heavily affected by COVID-19 underwent a significant change in dietary patterns, which they termed "emotional eating," characterized by an increase in cereal and fat consumption and a decrease in fish and seafood consumption. Additionally, the change in family routine likely influenced meal patterns, increasing the intake of ultra-processed foods and sugary beverages [
16]. In our sample, we noted an increase in lipid consumption in both groups. We did not make a temporal correlation of our findings with the pandemic situation, primarily because it was not the scope of our study. However, it's possible that the increase in fat consumption reflected the COVID-19 pandemic, which profoundly impacted population habits over the past three years.
Despite the challenges, the use of technology to enhance health guidelines occupied a significant space during the COVID-19 era. The study of a tool that could be used remotely, encouraging, and advising on diet, was even more promising. WhatsApp is a practical, inexpensive, and widely accessible tool. Moreover, the ubiquity of platforms like WhatsApp in daily communication offers a unique opportunity for health professionals. Its real-time messaging capabilities, combined with features such as voice messages, video calls, and document sharing, provide a multifaceted platform for remote patient management. Especially in contexts where face-to-face consultations might be challenging or risky, as was the case during the height of the COVID-19 pandemic, tools like this become indispensable [
17,
18].
With increasing patient familiarity with digital communication, the integration of such platforms into healthcare can enhance patient engagement and ensure continuous monitoring. The use of images and videos can assist in understanding the dietary habits and physical activities of patients more accurately. For instance, patients could share photos of their meals, facilitating more accurate dietary assessments and enabling healthcare providers to give immediate feedback [
19,
20].
However, it's crucial to note the challenges and potential pitfalls of integrating these platforms into medical practice. Privacy concerns are paramount. WhatsApp, and similar platforms, must adhere to stringent data protection standards to ensure patient information remains confidential. In many jurisdictions, the use of such platforms for medical consultation would require compliance with health information privacy regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States [
21,
22].
Additionally, while digital communication tools offer convenience, they can also lead to miscommunication or misinterpretation of information. Without the nuances available in face-to-face interactions, there's potential for misunderstandings. As a result, clear guidelines and training for healthcare professionals on the effective use of these platforms are essential. It's also vital to ensure that patients are educated about the appropriate use of these tools and the boundaries of digital consultations [
23]. Digital media has presented numerous advantages within the modern healthcare landscape. These benefits range from the seamless exchange of medical information, enhanced patient-doctor interactions, easy access to healthcare data, and an unprecedented platform for social and emotional support. Yet, as with all technology, it carries inherent challenges, such as ensuring patient privacy and the authenticity of disseminated information [
9].
A crucial period where the impact of digital media has been observed is during gestation. Pregnancy offers a unique window for healthcare professionals to influence lifestyle changes. The heightened motivation women experience during this phase, not only for their well-being but also for their unborn child, makes this period opportune for interventions. The frequent prenatal visits and the involvement of multidisciplinary teams, including nutritionists, obstetricians, and endocrinologists, set the stage for impactful and lasting lifestyle shifts. These alterations can potentially influence not only the mother's health trajectory but also set the tone for the family's overall well-being [
24].
In our study, the focus was on leveraging WhatsApp as a communication tool, targeting pregnant patients. However, it's worth noting that diet is intricately linked to family habits. If interventions successfully incorporate familial patterns, the outcomes could be broader and more substantial. A comparative study by Tian et al. [
25] examined glycemic control in diabetic pregnant women, segregating them into groups: those engaged in chat groups and those who weren't. Among the 300 participants, those in the intervention group demonstrated better glycemic control than the control group, though statistical significance wasn't attained. One salient observation was the positive correlation between early intervention and better glycemic control. Nevertheless, a universal trend of deteriorating glycemic control as pregnancy advanced was noted, with no marked difference in perinatal outcomes.
Previous assessments of WhatsApp as an intervention tool have yielded mixed results. For instance, Kennelly et al. [
26] observed no discernible difference between groups of overweight and obese pregnant women given dietary and exercise guidelines via the app. Contrastingly, Al Omar et al. [
10] reported a significant improvement in glycated hemoglobin levels in type 1 and type 2 diabetes mellitus patients following educational guidance delivered through WhatsApp.
Despite these conflicting findings, the overarching consensus remains digital media platforms, including WhatsApp, are viable tools in healthcare, extending to diabetic pregnant patients. The primary challenge lies in refining the intervention delivery method. Some participants in our study voiced discontent with the frequency of messages. A more nuanced approach, possibly fewer daily messages, could be more palatable and effective. Another significant concern in the study was the accuracy of tools measuring dietary intake. The 24-hour recall (R24) is a popular tool, but it's not infallible. Trusting the veracity of patient-reported data can be tricky. This skepticism is particularly pronounced when considering that after medical consultation and guidance, patients may be more conscious of their dietary choices, which might impact their subsequent reports.
Discussing macronutrient distribution, the advised distribution during pregnancy is approximately 44-55% carbohydrates, 15-20% proteins, and 30-40% lipids, with a strong emphasis on fiber intake. Caloric and macronutrient intake reported in the R24 remained within these guidelines, although lipid consumption was marginally elevated. Notably, the overall caloric intake was strikingly low, especially given a mean BMI of 29.8 kg/m2 at study entry. This discrepancy might highlight the shortcomings of dietary assessment tools, where underreporting is common, particularly among overweight women dissatisfied with their body image.
One promising strategy to enhance the precision of dietary assessments is the incorporation of meal photographs, allowing for more accurate analysis. Furthermore, as phone-based interventions became paramount during the COVID-19 pandemic [
3], the shift towards such tools seems inevitable.
5. Conclusions
In conclusion, while there are discrepancies in findings regarding the efficacy of digital interventions, platforms like WhatsApp still hold promise in the realm of multidisciplinary healthcare. Our study underscores the need for continued exploration in this domain, especially as telemedicine and remote healthcare burgeons. Digital media's potency lies in its accessibility, catering to remote populations who may otherwise be deprived of specialized care. However, the proliferation of misinformation online necessitates an emphasis on credible communication channels, positioning healthcare providers as trusted information sources. The rapid digitalization of healthcare is undeniable, and with it comes the imperative to adapt and optimize its application, ensuring comprehensive, accurate, and patient-centered care.
Author Contributions
Conceptualization, ET and RM; methodology, MSF; validation, PMD, BAP; formal analysis, VHSS; investigation, MCTV and ET; resources, RG; data curation, MCTV; writing—original draft preparation, MFS; writing—review and editing, EAJ; visualization, MCTV, MFS, RM, RG, PMD, VHSS, BAP, EAJ, and ET; supervision, ET; project administration, RM. All authors have read and agreed to the published version of the manuscript.
Funding
This article was not funded.
Institutional Review Board Statement
Our investigations were carried out following the rules of the Declaration of Helsinki of 1975, revised in 2013. The study was approved by the Ethics Committee of the Federal University of São Paulo (CAAE: CAAE: 30104820.6.0000.5505).
Informed Consent Statement
Informed consent was required by all participants.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors report no conflict of interest.
References
- Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy: a World Health Organization Guideline. Diabetes Res Clin Pract. 2014; 103(3):341–63. [CrossRef]
- HAPO Study Cooperative Research Group; Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR, Hadden DR, McCance DR, Hod M, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008; 358(19):1991–2002. [CrossRef]
- Rasmussen L, Poulsen CW, Kampmann U, Smedegaard SB, Ovesen PG, Fuglsang J. Diet and healthy lifestyle in the management of gestational diabetes mellitus. Nutrients. 2020; 12(10):1–24. [CrossRef]
- Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, Hoving C. A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res. 2013; 15(4):e85. [CrossRef]
- Wang Y, McKee M, Torbica A, Stuckler D. Systematic Literature Review on the Spread of Health-related Misinformation on Social Media. Soc Sci Med. 2019; 240:112552. [CrossRef]
- Lindsay KL, Brennan L, Kennelly MA, Curran S, Coffey M, Smith TP, Foley ME, Hatunic M, McAuliffe FM. Maternal metabolic response to dietary treatment for impaired glucose tolerance and gestational diabetes mellitus. Ir J Med Sci. 2018; 187(3):701-8. [CrossRef]
- American Diabetes Association, Professional Practice Committee. 15. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes—2022. Diabetes Care. 2022; 45:S232–43. [CrossRef]
- Park AJ, Maruthur MK, Swerlick RA. Information technologies in health care delivery and policy: giant steps and missteps. Semin Cutan Med Surg. 2019; 38(1):E25–30. [CrossRef]
- Gabarron E, Arsand E, Wynn R. Social media use in interventions for diabetes: Rapid evidence-based review. J Med Internet Res. 2018; 20(8):e10303. [CrossRef]
- Al Omar M, Hasan S, Palaian S, Mahameed S. The impact of a self-management educational program coordinated through WhatsApp on diabetes control. Pharm Pract (Granada). 2020; 18(2):1–9. [CrossRef]
- Metzger BE. International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010; 33(3):676–82. [CrossRef]
- Sweeting A, Wong J, Murphy HR, Ross GP. A Clinical Update on Gestational Diabetes Mellitus. Endocr Rev. 2022; 43(5):763-93. [CrossRef]
- Casey PH, Goolsby SLP, Lensing SY, Perloff BP, Bogle ML. The use of telephone interview methodology to obtain 24-hour dietary recalls. J Am Diet Assoc. 1999; 99(11):1406–11. [CrossRef]
- Guendelman S, Krueger GN, Cruz GI, Trepman PC, Suharwardy SH. Use of Telehealth During the COVID-19 Pandemic Among Practicing Maternal-Fetal Medicine Clinicians. Telemedicine and e-Health. 2023; 29(5):696–707. [CrossRef]
- Ghosh A, Arora B, Gupta R, Anoop S, Misra A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India. Diabetes Metab Syndr. 2020; 14(5):917-920. [CrossRef]
- Pietrobelli A, Pecoraro L, Ferruzzi A, Heo M, Faith M, Zoller T, Antoniazzi F, Piacentini G, Fearnbach SN, Heymsfield SB. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity (Silver Spring). 2020; 28(8):1382–5. [CrossRef]
- Nardo B, Lugaresi M, Doni M, Vulcano I, Piccione D, Paglione D, Stabile G. WhatsApp video call communication between oncological patients and their families during COVID-19 outbreak. Minerva Surg. 2021; 76(2):146-155. [CrossRef]
- Enyama D, Balti EV, Simeni Njonnou SR, Ngongang Ouankou C, Kemta Lekpa F, Noukeu Njinkui D, Fouogue JT, Mayouego Kouam J, Njateng GSS, Kenfack B, et al. Use of WhatsApp®, for distance teaching during COVID-19 pandemic: Experience and perception from a sub-Saharan African setting. BMC Med Educ. 2021; 21(1):517. [CrossRef]
- Ngo J, Engelen A, Molag M, Roesle J, García-Segovia P, Serra-Majem L. A review of the use of information and communication technologies for dietary assessment. Br J Nutr. 2009; 101 Suppl 2:S102-12. [CrossRef]
- Jaichuen N, Vandevijvere S, Kelly B, Vongmongkol V, Phulkerd S, Tangcharoensathien V. Unhealthy food and non-alcoholic beverage advertising on children's, youth and family free-to-air and digital television programmes in Thailand. BMC Public Health. 2018; 18(1):737. [CrossRef]
- Hung M, Lipsky MS, Phuatrakoon TN, Nguyen M, Licari FW, Unni EJ. Teledentistry Implementation During the COVID-19 Pandemic: Scoping Review. Interact J Med Res. 2022; 11(2):e39955. [CrossRef]
- Kanchan S, Gaidhane A. Social Media Role and Its Impact on Public Health: A Narrative Review. Cureus. 2023; 15(1):e33737. [CrossRef]
- Konttila J, Siira H, Kyngäs H, Lahtinen M, Elo S, Kääriäinen M, Kaakinen P, Oikarinen A, Yamakawa M, Fukui S, et al. Healthcare professionals' competence in digitalisation: A systematic review. J Clin Nurs. 2019; 28(5-6):745-761. [CrossRef]
- Smith M, Mitchell AS, Townsend ML, Herbert JS. The relationship between digital media use during pregnancy, maternal psychological wellbeing, and maternal-fetal attachment. PLoS One. 2020; 15(12):e0243898. [CrossRef]
- Tian Y, Zhang S, Huang F, Ma L. Comparing the Efficacies of Telemedicine and Standard Prenatal Care on Blood Glucose Control in Women With Gestational Diabetes Mellitus: Randomized Controlled Trial. JMIR Mhealth Uhealth. 2021; 9(5): e22881. [CrossRef]
- Kennelly MA, Ainscough K, Lindsay K, Gibney E, Mc Carthy M, McAuliffe FM. Pregnancy, exercise and nutrition research study with smart phone app support (Pears): Study protocol of a randomized controlled trial. Contemp Clin Trials. 2016; 46:92–9. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).