Submitted:
20 March 2024
Posted:
21 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Blood Sampling and Analysis
2.3. Statistical Analysis
3. Results
3.1. Statistical Analysis of Demographic Characteristics of Cases and Controls
3.2. Statistical Analysis of Genotype and Allele Distribution of Three SNPs of Genes IL-10, IL-6 and TNFα in Various Inheritance Models between Cases and Controls
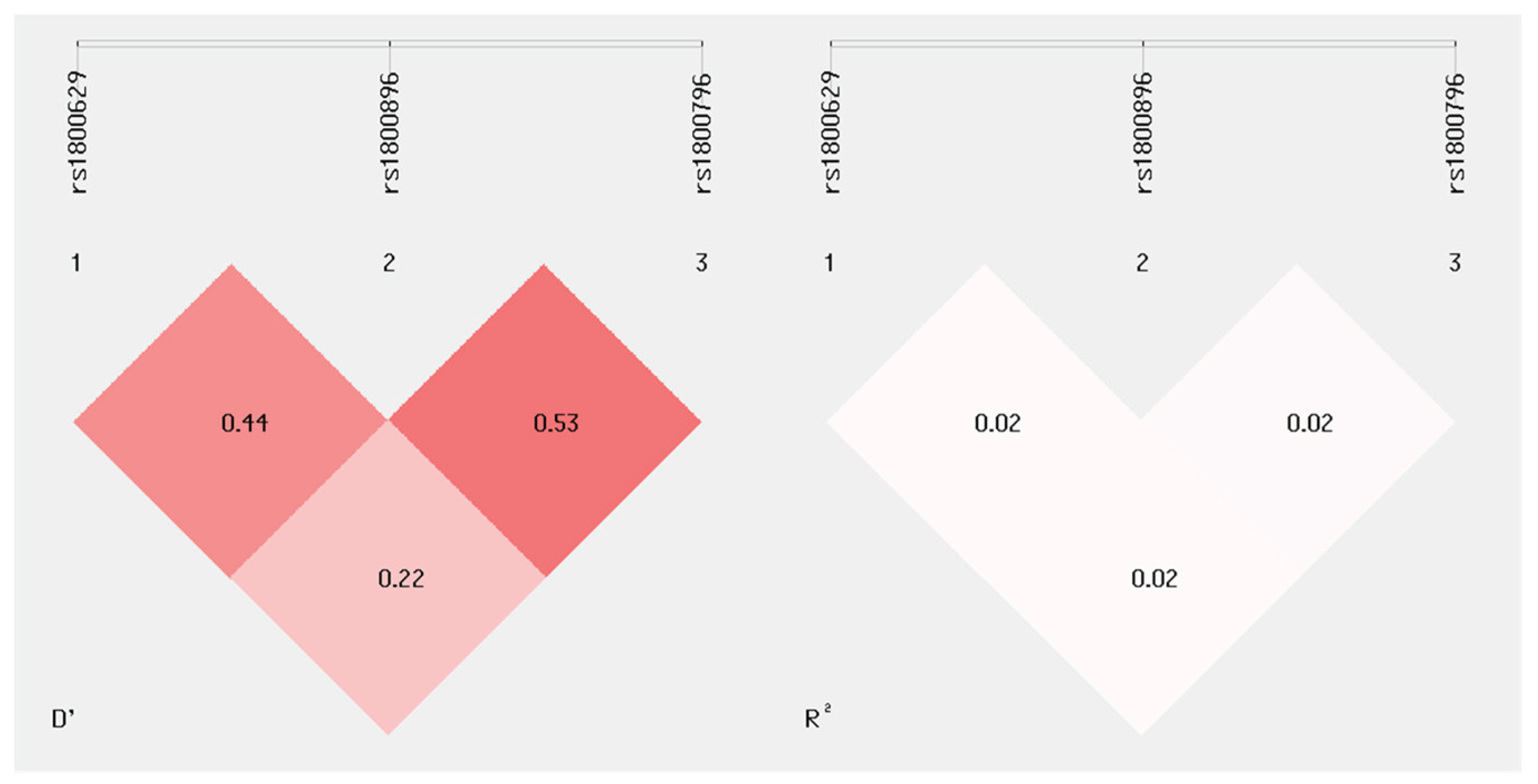
3.3. Statistical Analysis of Linkage Disequilibrium(LD) and Haplotypes Analysis of 3 SNPs of Genes IL-10, IL-6 and TNFα
3.4. Prediction of Probability forPTB by Bivariate and Multivariate Logistic Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. Born Too Soon: The Global Action Report on Preterm Birth. WHO 2014. Available online: (accessed on 8th of March 2024).
- Quinn, J.A.; Munoz, F.M.; Gonik, B.; Frau, L.; Cutland, C.; Mallett-Moore, T.; Kissou, A.; Wittke, F.; Das, M.; Nunes, T.; Pye,S.; Watson, V.; Alguacil Ramos, A.M.; Cordero, J.F.; Huang, W.T.; Kochhar, S.; Buttery, J. Preterm Birth: Case Definition & Guidelines for Data Collection, Analysis, and Presentation of Immunisation Safety Data. Vaccine 2016, 34(49), 6046-6056. [CrossRef]
- Blencowe, H.; Cousens, S.; Oestergaard, M.Z.; Chou, D.; Moller, A.B.; Narwal, R.; Adler, A.; Vera Garcia, C.; Rohde, S.; Say, L.; Lawn, J.E. National, Regional, and Worldwide Estimates of Preterm Birth Rates in the Year 2010 With Time Trends Since 1990 for Selected Countries. Lancet 2012, 379(9832)(9832), 2162–2172. [Google Scholar] [CrossRef]
- Ðelmiš, J.; Juras, J.; Rodin, U. Perinatalni Mortalitet u Republici Hrvatskoj u 2015. Godini. Gynaecol Perinatol 2016, 24 (Suppl 1), 3–18. [Google Scholar]
- Wen, S.W.; Smith, G.; Yang, Q.; Walker, M. Epidemiology of Preterm Birth and Neonatal Outcome. Semin Fetal Neonatal Med 2004, 9(6), 429–435. [Google Scholar] [CrossRef] [PubMed]
- Swaggart, K.A.; Pavlicev, M.; Muglia, L.J. Genomics of Preterm Birth. Cold Spring Harb Perspect Med 2015, 5(2). [Google Scholar] [CrossRef]
- York, T.P.; Eaves, L.J.; Lichtenstein, P.; Neale, M.C.; Svensson, A.; Latendresse, S.; Långström, N.; Strauss, J.F. Fetal and Maternal Genes’ Influence on Gestational Age in a Quantitative Genetic Analysis of 244,000 Swedish Births. Am J Epidemiol 2013, 178(4), 543–550. [Google Scholar] [CrossRef] [PubMed]
- Boyd, H.A.; Poulsen, G.; Wohlfahrt, J.; Murray, J.C.; Feenstra, B.; Melbye, M. Maternal Contributions to Preterm Delivery. Am J Epidemiol 2009, 170, 1358. [Google Scholar] [CrossRef] [PubMed]
- Boyle, A.K.; Rinaldi, S.F.; Norman, J.E.; Stock, S.J. Preterm Birth: Inflammation, Fetal Injury and Treatment Strategies. J Reprod Immunol 2017, 119, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Rinaldi, S.F.; Hutchinson, J.L.; Rossi, A.G.; Norman, J.E. Anti-Inflammatory Mediators as Physiological and Pharmacological Regulators of Parturition. Expert Rev Clin Immunol 2011, 7, 675–696. [Google Scholar] [CrossRef]
- Seematter, G.; Binnert, C.; Martin, J.L.; Tappy, L. Relationship between Stress, Inflammation and Metabolism. Curr Opin Clin Nutr Metab Care 2004, 7, 169–173. [Google Scholar] [CrossRef]
- Osman, I.; Young, A.; Ledingham, M.A.; Thomson, A.J.; Jordan, F.; Greer, I.A.; Norman, J.E. Leukocyte Density and Pro-inflammatory Cytokine Expression in Human Fetal Membranes, Decidua, Cervix and Myometrium before and during Labour at Term. Mol Hum Reprod 2003, 9, 41–45. [Google Scholar] [CrossRef]
- Barata, H.; Thompson, M.; Zielinska, W.; Han, Y.S.; Mantilla, C.B.; Prakash, Y.S.; Feitoza, S.; Sieck, G.; Chini, E.N. The Role of Cyclic-ADP-Ribose-Signaling Pathway in Oxytocin-Induced Ca2+ Transients in Human Myometrium Cells. Endocrinology 2004, 145, 881–889. [Google Scholar] [CrossRef]
- Törnblom, S.A.; Klimaviciute, A.; Byström, B.; Chromek, M.; Brauner, A.; Ekman-Ordeberg, G. Non-Infected Preterm Parturition Is Related to Increased Concentrations of IL-6, IL-8 and MCP-1 in Human Cervix. 2005, 3, 1-10. [CrossRef]
- Larsen, B.; Hwang, J. Progesterone Interactions with the Cervix: Translational Implications for Term and Preterm Birth. Infect Dis Obstet Gynecol 2011, 2011, 13. [Google Scholar] [CrossRef] [PubMed]
- Belfer, I.; Buzas, B.; Hipp, H.; Dean, M.; Evans, C.; Lorincz, I.; Max, M.B.; Goldman, D. Haplotype Structure of Inflammatory Cytokines Genes (IL1B, IL6 and TNF/LTA) in US Caucasians and African Americans. Genes & Immunity 2004, 5(6), 505–512. [CrossRef]
- Zare-Bidaki, M.; Sadrinia, S.; Erfani, S.; Afkar, E.; Ghanbarzade, N. Antimicrobial Properties of Amniotic and Chorionic Membranes: A Comparative Study of Two Human Fetal Sacs. J Reprod Infertil 2017, 18, 218. [Google Scholar] [PubMed]
- Keelan, J.A. Pharmacological Inhibition of Inflammatory Pathways for the Prevention of Preterm Birth. J Reprod Immunol 2011, 88, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Romero, R.; Espinoza, J.; Gonçalves, L.F.; Kusanovic, J.P.; Friel, L.; Hassan, S. The Role of Inflammation and Infection in Preterm Birth. Semin Reprod Med 2007, 25, 21–39. [Google Scholar] [CrossRef] [PubMed]
- Velez, D.R.; Fortunato, S.J.; Williams, S.M.; Menon, R. Interleukin-6 (IL-6) and Receptor (IL6-R) Gene Haplotypes Associate with Amniotic Fluid Protein Concentrations in Preterm Birth. Hum Mol Genet 2008, 17, 1619–1630. [Google Scholar] [CrossRef]
- Menon, R.; Fortunato, S.J.; Edwards, D.R.V.; Williams, S.M. Association of Genetic Variants, Ethnicity, and Preterm Birth with Amniotic Fluid Cytokine Concentrations. Ann Hum Genet 2010, 74, 165–183. [Google Scholar] [CrossRef]
- Velez, D.R.; Fortunato, S.; Thorsen, P.; Lombardi, S.J.; Williams, S.M.; Menon, R. Spontaneous Preterm Birth in African Americans Is Associated with Infection and Inflammatory Response Gene Variants. Am J Obstet Gynecol 2009, 200(2), 209-e1. [Google Scholar] [CrossRef]
- Menon, R.; Velez, D.R.; Simhan, H.; Ryckman, K.; Jiang, L.; Thorsen, P.; Vogel, I.; Jacobsson, B.; Merialdi, M.; Williams, S.M.; et al. Multilocus Interactions at Maternal Tumor Necrosis Factor-α, Tumor Necrosis Factor Receptors, Interleukin-6, and Interleukin-6 Receptor Genes Predict Spontaneous Preterm Labor in European-American Women. Am J Obstet Gynecol 2006, 194, 1616–1624. [Google Scholar] [CrossRef]
- Harper, M.; Lilly Zheng, S.; Thom, E.; Klebanoff, M.A.; Thorp, J.; Sorokin, Y.; Varner, M.W.; Iams, J.D.; Dinsmoor, M.; Mercer, B.M.; Rouse, D.J.; Ramin, S.M.; Anderson-Garland, D. Cytokine Gene Polymorphisms and Length of Gestation. Obstet Gynecol 2011, 117(1), 125–130. [Google Scholar] [CrossRef]
- Lyubomirskaya, E.S.; Kamyshnyi, A.M.; Krut, Yu.Ya.; Smiianov, V.A.; Fedoniuk, L.Y.; Romanyuk, L.B.; Kravets, N.Y.; Mochulska, O.M.. Snps and Transcriptional Activity of Genes of Innate and Adaptive Immunity at the Maternal-Fetal Interface in Woman with Preterm Labour, Associated with Preterm Premature Rupture of Membranes. 2020, 73(1), 25-30. [CrossRef]
- Pandey, M.; Awasthi, S.; Singh, U.; Mahdi, A.A. Association of IL-10 Gene Polymorphism (−819C > T, −592C > A and −1082G > A) with Preterm Birth. Indian J Pediatr 2018, 85, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Nuk, M.; Orendi, K.; Rosenberger, S.; Griesbacher, A.; Holzapfel-Bauer, M.; Resch, B.; Lang, U.; Pertl, B. Genetic Variations in Fetal and Maternal Tumor Necrosis Factor-α and Interleukin 10: Is There an Association with Preterm Birth or Periventricular Leucomalacia? J Perinatol 2011, 32(1), 27–32. [Google Scholar] [CrossRef] [PubMed]
- Stonek, F.; Metzenbauer, M.; Hafner, E.; Philipp, K.; Tempfer, C. Interleukin 6 –174 G/C Promoter Polymorphism and Pregnancy Complications: Results of a Prospective Cohort Study in 1626 Pregnant Women. Am J Reprod Immunol 2008, 59, 347–351. [Google Scholar] [CrossRef] [PubMed]
- Amory, J.H.; Adams, K.M.; Lin, M.T.; Hansen, J.A.; Eschenbach, D.A.; Hitti, J. Adverse Outcomes after Preterm Labor Are Associated with Tumor Necrosis Factor-α Polymorphism −863, but Not −308, in Mother-Infant Pairs. Am J Obstet Gynecol 2004, 191, 1362–1367. [Google Scholar] [CrossRef]
- Han, S.H.; Lee, N.R.; Kim, H.J.; Kang, Y.D.; Kim, J.S.; Park, J.W.; Jin, H.J. Association between the IL-6, IL-10 and TNFα Gene Polymorphisms and Preterm-Birth in Korean Women. Genes Genomics 2020, 42, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Liang, M.; Wang, X.; Li, J.; Yang, F.; Fang, Z.; Wang, L.; Hu, Y.; Chen, D. Association of Combined Maternal-Fetal TNF-α Gene G308A Genotypes with Preterm Delivery: A Gene-Gene Interaction Study. J Biomed Biotechnol 2010, 2010, 396184. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, Y.; Verdi, H.; Taneri, A.; Yazici, A.C.; Ecevit, A.N.; Karakaş, N.M.; Tarcan, A.; Haberal, A.; Ozbek, N.; Atac, F.B. Maternal–Fetal Proinflammatory Cytokine Gene Polymorphism and Preterm Birth. 2012, 31, 92–97. [CrossRef]
- Sayaril, N.A.; Bhat, R.S.; Warsy, A.S.; Babay, Z.A.; Addar, M.H.; Shaik, J.; Al-Marry, B.; Al-Daihan, S. Polymorphisms in Proinflammatory Cytokine Genes, Effect on Gene Expression and Association with Preterm Delivery in Saudi Females. Cell Mol Biol 2018, 64, 55–60. [Google Scholar] [CrossRef]
- Andalas, M.; Hakimi, M.; Nurdiati, D.S.; Astuti, I.; Imran, I.; Harapan, H. Association of -308G/A TNF-α Gene Polymorphism and Spontaneous Preterm Birth in Acehnese Ethnic Group, Indonesia: This Polymorphism Is Not Associated with Preterm Birth. Egypt J Med Hum Genet 2016, 17, 33–40. [Google Scholar] [CrossRef]
- Bitner, A.; Kalinka, J. IL-1β, IL-6 Promoter, TNF-α Promoter, and IL-1RA Gene Polymorphisms and the Risk of Preterm Delivery Due to Preterm Premature Rupture of Membranes in a Population of Polish Women. Arch Med Sci 2010, 6(4), 552–557. [Google Scholar] [CrossRef]
- Jones, N.M.; Holzman, C.; Mph, D.; Friderici, K.H.; Jernigan, K.; Chung, H.; Wirth, J.; Fisher, R.; Jones, N. Interplay of Cytokine Polymorphisms and Bacterial Vaginosis in the Etiology of Preterm Delivery. J Reprod Immunol 2010, 87, 82–89. [Google Scholar] [CrossRef]
- Jafarzadeh, L.; Danesh, A.; Sadeghi, M.; Heybati, F.; Hashemzadeh, M. Analysis of Relationship between Tumor Necrosis Factor Alpha Gene (G308A Polymorphism) with Preterm Labor. Int J Prev Med 2013, 4(8), 896. [Google Scholar]
- Mattar, R.; De Souza, E.; Daher, S. Preterm Delivery and Cytokine Gene Polymorphisms. J Reprod Med 2006, 51, 317–320. [Google Scholar] [PubMed]
- Ramos, B.R. de A.; Mendes, N.D.; Tanikawa, A.A.; Amador, M.A.T.; dos Santos, N.P.C. ; dos Santos, S.E.B. ; Castelli, E.C.; Witkin, S.S.; da Silva, M.G. Ancestry Informative Markers and Selected Single Nucleotide Polymorphisms in Immunoregulatory Genes on Preterm Labor and Preterm Premature Rupture of Membranes: A Case Control Study. BMC Pregnancy Childbirth 2016, 16, 1–11. [Google Scholar] [CrossRef]
- GeneCards Human Gene Database. Available online: https://www.genecards.org/ (accessed on 9th March 2024.).
- Macones, G.A.; Parry, S.; Elkousy, M.; Clothier, B.; Ural, S.H.; Strauss, J.F. A Polymorphism in the Promoter Region of TNF and Bacterial Vaginosis: Preliminary Evidence of Gene-Environment Interaction in the Etiology of Spontaneous Preterm Birth. Am J Obstet Gynecol 2004, 190, 1504–1508. [Google Scholar] [CrossRef] [PubMed]
- Moura, E.; Mattar, R.; de Souza, E.; Torloni, M.R.; Gonçalves-Primo, A.; Daher, S. Inflammatory Cytokine Gene Polymorphisms and Spontaneous Preterm Birth. J Reprod Immunol 2009, 80, 115–121. [Google Scholar] [CrossRef] [PubMed]
- De Waal Malefyt, R.; Abrams, J.; Bennett, B.; Figdor, C.G.; De Vries, J.E. Interleukin 10(IL-10) Inhibits Cytokine Synthesis by Human Monocytes: An Autoregulatory Role of IL-10 Produced by Monocytes. J Exp Med 1991, 174(5), 1209–1220. [Google Scholar] [CrossRef] [PubMed]
- Fortunato, S.J.; Menon, R.; Lombardi, S.J. Interleukin-10 and Transforming Growth Factor-β Inhibit Amniochorion Tumor Necrosis Factor-α Production by Contrasting Mechanisms of Action: Therapeutic Implications in Prematurity. Am J Obstet Gynecol 1997, 177, 803–809. [Google Scholar] [CrossRef]
- Pomini, F.; Caruso, A.; Challis, J.R.G. Interleukin-10 Modifies the Effects of Interleukin-1 and Tumor Necrosis Factor-on the Activity and Expression of Prostaglandin H Synthase-2 and the NAD-Dependent 15-Hydroxyprostaglandin Dehydrogenase in Cultured Term Human Villous Trophoblast and Chorion Trophoblast Cells. J Clin Endocrinol Metab 1999, 84, 4645–4651. [Google Scholar]
- Turner, D.M.; Williams, D.M.; Sankaran, D.; Lazarus, M.; Sinnott, P.J.; Hutchinson, I. V. An Investigation Of Polymorphism In The Interleukin-10 Gene Promoter. Eur J Immunogen 1997, 24, 1–8. [Google Scholar] [CrossRef]
- Luppi, P.; Tse, H.; Lain, K.Y.; Markovic, N.; Piganelli, J.D.; DeLoia, J.A. Preeclampsia Activates Circulating Immune Cells with Engagement of the NF-ΚB Pathway. Am J Reprode Immunol 2006, 56, 135–144. [Google Scholar] [CrossRef]
- Blondel, B.; Morin, I.; Platt, R.W.; Kramer, M.S.; Usher, R.; Bréart, G. Algorithms for Combining Menstrual and Ultrasound Estimates of Gestational Age: Consequences for Rates of Preterm and Postterm Birth. BJOG 2002, 109, 718–720. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.Y.; Liu, J. Bin; Liu, X.; Qian, L.X. Association of Interleukin 10 Rs1800896 Polymorphism with Susceptibility to Breast Cancer: A Meta-Analysis. J Int Med Res 2020, 48, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Sun, J.; Chen, Y. Preterm Birth and Single Nucleotide Polymorphisms in Cytokine Genes. Transl Pediatr 2014, 3, 12034–12134. [Google Scholar] [CrossRef]
- Jie, P.; Wei-yue, Z. Relationship among TNF-Alpha Gene Promoter -308 Site Polymorphism, the Levels of Maternal Serum TNF-Alpha, and the MRNA Expression Placental TNF-Alpha in Preterm Labor. J Sichuan Univ 2009, 40, 77–80. [Google Scholar]
- Drews-Piasecka, E.; Seremak-Mrozikiewicz, A.; Barlik, M.; Kurzawińska, G.; Wolski, H.; Woyciechowska, A.; Czerny, B.; Drews, K. The Significance of TNF-α Gene Polymorphisms in Preterm Delivery. Ginekol Pol 2014, 85, 428–434. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Hu, Y.; Wu, B.; Chen, L.; Fang, Z.; Yang, F.; Wang, L. Tumor Necrosis Factor-Alpha Gene G308A Polymorphism Is Associated with the Risk of Preterm Delivery. J Peking Univ. Health Sci. 2003, 35, 377–381. [Google Scholar]
- Wagner, J.; Štibi, S.; Selak, N.; Alvir, I.; Mamić, I.; Marcelić, L.; Šušnjar, L.; Puljiz, M.; Heffer, M.; Danolić, D. Interleukin 10 Rs1800896 and Interleukin 1B Rs16944 Polymorphisms and the Risk of Cervical Cancer. Wien Medizin Wochensch 2023, 173, 57–61. [Google Scholar] [CrossRef]
- Khorrami, S.; Zamani, H.; Hasanzadeh, M.; Mehramiz, M.; Soleimani, A.; Zare Marzouni, H.; Ferns, G.A.; Esmaeili, H.; Avan, A. Association of a Genetic Variant in Interleukin-10 Gene with Increased Risk and Inflammation Associated with Cervical Cancer. Gene 2022, 807, 145933. [Google Scholar] [CrossRef]
- Culjak, M.; Perkovic, M.N.; Uzun, S.; Strac, D.S.; Erjavec, G.N.; Leko, M.B.; Simic, G.; Tudor, L.; Konjevod, M.; Kozumplik, O.; Mimica,N. ; Pivac, N. The Association between TNF-Alpha, IL-1 Alpha and IL-10 with Alzheimer’s Disease. Curr Alzheimer Res 2020, 17, 972–984. [Google Scholar] [CrossRef]
- Cao, X.L.; Zhou, X.Y.; Xu, N.X.; Chen, S.C.; Xu, C.M. Association of IL-4 and IL-10 Polymorphisms With Preterm Birth Susceptibility: A Systematic Review and Meta-Analysis. Front Immunol 2022, 13, 917838. [Google Scholar]
- Shao, M.; Xie, H.; Yang, H.; Xu, W.; Chen, Y.; Gao, X.; Guan, S.; Xu, S.; Shuai, Z.; Pan, F. Association of Interleukin-6 Promoter Polymorphism with Rheumatoid Arthritis: A Meta-Analysis with Trial Sequential Analysis. Clin Rheumatol 2022, 41, 411–419. [Google Scholar] [CrossRef]
- Kaanane, H.; Senhaji, N.; Berradi, H.; Benchakroun, N.; Benider, A.; Karkouri, M.; El Attar, H.; Flores, O.; Khyatti, M.; Nadifi, S. The Influence of Interleukin-6, Interleukin-8, Interleukin-10, Interleukin-17, TNF-A, MIF, STAT3 on Lung Cancer Risk in Moroccan Population. Cytokine 2022, 151, 155806. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.P.; Pereira, J.N.; Delabio, R.W.; Smith, M.A.C.; Payão, S.L.M.; Carneiro, L.C.; Barbosa, M.S.; Rasmussen, L.T. Increased Expression of Interleukin-6 Gene in Gastritis and Gastric Cancer. Braz J Med Biol Res 2021, 54, e10687. [Google Scholar] [CrossRef] [PubMed]
- Hou, Z.F.; Yuan, Z.H.; Chang, K.; Cao, Y.H.; Guan, F.X.; Gao, Y. NLRP3 Rs1539019 Is Significantly Associated with Chronic Obstructive Pulmonary Disease in a Chinese Han Population: A Case-Control Study. Eur Rev Med Pharmacol Sci 2022, 26, 5821–5828. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Wang, Y.; Wang, Y.; Hu, J.; Di, W.; Liu, S.; Zeng, X.; Yu, G.; Wang, Y.; Wang, Z. The IL-6 Rs1800795 and Rs1800796 Polymorphisms Are Associated with Coronary Artery Disease Risk. J Cell Mol Med 2020, 24, 6191–6207. [Google Scholar] [CrossRef] [PubMed]
- Malkki, M.; Petersdorf, E.W. Genotyping of Single Nucleotide Polymorphisms by 5′ Nuclease Allelic Discrimination. In: Immunogenetics. Methods in Molecular Biology, 1st ed.; Christiansen, F., Tait, B., eds.; Humana Press, Totowa, NJ, 2012; vol. 882, pp. 173-182. [CrossRef]
- Applied Biosystems 7500/7500 Fast Real-Time PCR System. Genotyping Experiments Getting Started Guide. Foster City, California, USA; Applied Biosystem, 2010.
- Solé, X.; Guinó, E.; Valls, J.; Iniesta, R.; Moreno, V. SNPStats: A Web Tool for the Analysis of Association Studies. Bioinformatics 2006, 22, 1928–1929. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Zhang, Z.; He, Z.; Tang, W.; Li, T.; Zeng, Z.; He, L.; Shi, Y. A Partition-Ligation-Combination-Subdivision Em Algorithm for Haplotype Inference with Multiallelic Markers: Update of the SHEsis (Http://Analysis.Bio- x.Cn). Cell Res 2009, 19, 519–523. [Google Scholar] [CrossRef]
- Shi, Y.Y.; He, L. SHEsis, a Powerful Software Platform for Analyses of Linkage Disequilibrium, Haplotype Construction, and Genetic Association at Polymorphism Loci. Cell Res 2005, 15, 97–98. [Google Scholar] [CrossRef]
- Sugita, N.; Kobayashi, T.; Kikuchi, A.; Shimada, Y.; Hirano, E.; Sasahara, J.; Tanaka, K.; Yoshie, H. Immunoregulatory Gene Polymorphisms in Japanese Women with Preterm Births and Periodontitis. J Reprod Immunol 2012, 93, 94–101. [Google Scholar] [CrossRef]
- Roberts, A.K.; Monzon-Bordonaba, F.; Van Deerlin, P.G.; Holder, J.; Macones, G.A.; Morgan, M.A.; Strauss, J.F.; Parry, S. Association of Polymorphism within the Promoter of the Tumor Necrosis Factor α Gene with Increased Risk of Preterm Premature Rupture of the Fetal Membranes. Am J Obstet Gynecol 1999, 180, 1297–1302. [Google Scholar] [CrossRef]
- Dizon-Townson, D.S.; Major, H.; Varner, M.; Ward, K. A Promoter Mutation That Increases Transcription of the Tumor Necrosis Factor-α Gene Is Not Associated with Preterm Delivery. Am J Obstet Gynecol 1997, 177, 810–813. [Google Scholar] [CrossRef]
- Belousova, V.S.; Svitich, O.A.; Timokhina, E. V.; Strizhakov, A.N.; Bogomazova, I.M. Polymorphism of the IL-1β, TNF, IL-1RA and IL-4 Cytokine Genes Significantly Increases the Risk of Preterm Birth. Biochemistry (Moscow) 2019, 84, 1040–1046. [Google Scholar] [CrossRef] [PubMed]
- So, T.; Ito, A.; Sato, T.; Mori, Y.; Hirakawa, S. Tumor Necrosis Factor-α Stimulates the Biosynthesis of Matrix Metalloproteinases and Plasminogen Activator in Cultured Human Chorionic Cells. Biol Reprod 1992, 46, 772–778. [Google Scholar] [CrossRef] [PubMed]
- Jeong, P.; Kim, E.J.; Kim, E.G.; Byun, S.S.; Kim, C.S.; Kim, W.J. Association of Bladder Tumors and GA Genotype of -308 Nucleotide in Tumor Necrosis Factor-Alpha Promoter with Greater Tumor Necrosis Factor-Alpha Expression. Urology 2004, 64, 1052–1056. [Google Scholar] [CrossRef]
- Weiyuan, Z.; Li,W. Study of Interleukin-6 and Tumor Necrosis Factor-Alpha Levels in Maternal Serum and Amniotic Fluid of Patients with Premature Rupture of Membranes. J Perinat Med 1998, 26, 491–494. [Google Scholar] [CrossRef] [PubMed]
- Sata, F.; Toya, S.; Yamada, H.; Suzuki, K.; Saijo, Y.; Yamazaki, A.; Minakami, H.; Kishi, R. Proinflammatory Cytokine Polymorphisms and the Risk of Preterm Birth and Low Birthweight in a Japanese Population. Mol Hum Reprod 2009, 15, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Manuck, T.A. Racial and Ethnic Differences in Preterm Birth: A Complex, Multifactorial Problem. Semin Perinatol 2017, 41, 511–518. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA - J Am Med Assoc 2013, 310(20), 2191–2194. [CrossRef]
| SNP | Location | Gene region | Base change | Citation | Related phenotype |
|---|---|---|---|---|---|
| TNFα (rs1800629) | Chr 6:31575254 (GRCh38.p14) |
Promoter region |
G/A | Velez et al.[20] Yilmaz et al.[32] Jones et al.[36] Han et al.[30] Jie et al.[51] Drew.Piasecka et al.[52] Zhu et al.[50] Chen et al.[53] |
Recurrent pregnancy loss Premature birth |
| IL – 10 (rs1800896) | chr 1:206773552 (GRCh38.p14) | Promoter region |
T/C | Wagner et al.[54] Khorrami et al.[55] Čuljak et al.[56] Zhu et al. [49] Pandey et al.[26] Menon et al.[21] Lyubomirskaya et al.[25] Cao et al.[57] |
Cervical cancer Alzheimer’s disease Breast cancer Preterm birth |
| IL – 6 (rs1800796) | Chr7: 22726627 (GRCh38.p14) |
Promoter region | G/A | Shao et al.[58] Kaanene et al.[59] Santos et al.[60] Hou et al.[61] Luai et al.[62] Han et al.[30] Lyubomirskaya et al.[25] |
Rheumatoid arthritis Lung cancer Gastritis and gastric cancer Chronic obstructive pulmonary disease Coronary artery disease Preterm birth |
| Term birth (n = 200) |
PTB (n = 199) | Total (n = 399) |
P | |
|---|---|---|---|---|
| Mother’s age [years]) [Median (IQR)] | 30 (26 – 34) | 31 (27 – 35) | 0.20‡ | |
| BMI (kg/m2) [Median (IQR)] | 27.4 (24.5 – 30.6) | 26.7 (24.2 – 30.1) | 0.35‡ | |
| Underweight [n (%) ] | 2 (1) | 0 | 2 (0.5) | 0.15† |
| Normal weight [n (%) ] | 54 (27) | 66 (33) | 120 (30.1) | |
| Overweight [n (%) ] | 144 (72) | 133 (67) | 277 (69.4) | |
| Coffee consumption [n(%)] | 167 (83.5) | 155 (77.9) | 322 (80.7) | 0.17* |
| Smoking habit [n(%)] | 52 (25.9) | 63 (31.5) | 115 (28.7) | 0.21* |
| Pregnancy complications [n(%)] | 104 (51.7) | 150 (75.4) | 254 (63.7) | <0.001* |
| Uroinfection [n(%)] | 18 (9) | 27 (13.5) | 45 (11.2) | 0.15* |
| Positive cervical swabs [n(%)] | 44 (21.9) | 35 (17.5) | 79 (19.7) | 0.27* |
| Vaginal bleeding during pregnancy [n(%)] | 14 (7) | 45 (22.6) | 59 (14.8) | <0.001* |
| PPROM [n(%)] | 47 (23.4) | 118 (59.6) | 165 (41.4) | <0.001* |
| Number of previous births [Median (IQR)] |
2 (1 – 2) | 1 (1 – 2) | 0.27‡ | |
| PB in family anamnesis [n(%)] | 0 | 33 (16.5) | 33 (8,2) | <0.001* |
| Number of previous PB (n=32) [Median (IQR)] | 1 (n = 1) | 1 (min 1 – max 3) | - | |
| Gestational age [Median (IQR)] | 39+4 (39 – 40+3) | 34+6 (32 – 36) | <0.001‡ | |
| Mode of delivery [n(%)] | ||||
| Vaginal birth | 195 (98) | 142 (71) | 337 (84) | <0.001* |
| Cesarean section | 5 (2) | 57 (29) | 62 (16) | |
| Premature birth [n(%)] | ||||
| Extremely early PB | - | 16 (8) | - | - |
| Early PB | - | 32 (16) | - | - |
| Late PB | - | 151 (76) | - | - |
| Birth weight of infants [g] | 3450 (3123 – 3800) | 2430 (1816 – 2780) | <0.001‡ | |
| Infant gender | ||||
| Male | 100 (50) | 117 (59) | 217 (54) | 0.07* |
| Female | 100 (50) | 81 (41) | 181 (46) |
| SNP/inheritance models | Genotip [n (%)] | OR (95 % CI) |
P* | ||
| Term birth (n = 200) |
PTB (n = 199) |
||||
| a TNFα (rs1800629) | G/G | 154 (77) | 149 (74.9) | 1 | 0.22 |
| A/G | 44 (22) | 43 (21.6) | 1.01 (0.63 – 1.63) | ||
| A/A | 2 (1) | 7 (3.5) | 3.62 (0.74 – 17.7) | ||
| Alelles | G | 352 (88) | 341 (86) | 0.82 (0.54 – 1.23) | 0.3 |
| A | 48 (12) | 57 (14) | |||
| Dominant inheritance model | G/G | 154 (77) | 149 (74.9) | 1 | 0.62 |
| A/G – A/A | 46 (23) | 50 (25.1) | 1.12 (0.71-1.78) | ||
| Recessive inheritance model | G/G – A/G | 198 (99) | 192 (96.5) | 1 | 0.08 |
| A/A | 2 (1) | 7 (3.5) | 3.61 (0.74-17.59) | ||
| Superdominant inheritance model | G/G – A/A | 156 (78) | 156 (78.4) | 1 | 0.92 |
| A/G | 44 (22) | 43 (21.6) | 0.98 (0.61 – 1.57) | ||
| bIL – 10 (rs1800896) | A/A | 68 (34) | 62 (31) | 1 | 0.05 |
| A/G | 88 (44) | 109 (55) | 1,36 (0.87 – 2.12) | ||
| G/G | 44 (22) | 28 (14) | 0,70 (0.39 – 1.25) | ||
| Alelles | A | 224 (56) | 233 (59) | 1,11 (0,84 – 1,47) | 0.47 |
| G | 176 (44) | 165 (41) | |||
| Dominant inheritance model | A/A | 68 (34) | 62 (31.2) | 1 | 0.54 |
| A/G – G/G | 132 (66) | 137 (68.8) | 1,14 (0,75 - 1,73) | ||
| Recessive inheritance model | A/A – A/G | 156 (78) | 171 (85.9) | 1 | 0.04 |
| G/G | 44 (22) | 28 (14.1) | 0.58 (0.34-0.98) | ||
| Superdominant inheritance model | A/A – G/G | 112 (56) | 90 (45.2) | 1 | 0.03 |
| A/G | 88 (44) | 109 (54.8) | 1.54 (1.04-2.29) | ||
| cIL – 6 (rs1800796) | G/G | 176 (88) | 176 (88.4) | 1 | 0.99 |
| C/G | 23 (11.5) | 22 (11.1) | 0.96 (0,51 – 1.78) | ||
| C/C | 1 (0.5) | 1 (0.5) | 1.00 (0.06 – 16.11) | ||
| Alelles | G | 375 (94) | 374 (94) | 1.04 (0.58 – 1.85) | 0.90 |
| C | 25 (6) | 24 (6) | |||
| Dominant inheritance model | G/G | 176 (88) | 176 (88.4) | 1 | 0.89 |
| C/G – C/C | 24 (12) | 23 (11.6) | 0.96 (0.52-1.76) | ||
| Recessive inheritance model | G/G – C/G | 199 (99.5) | 198 (99.5) | 1 | >0.99 |
| C/C | 1 (0.5) | 1 (0.5) | 1.01 (0.06-16.18) | ||
| Superdominant inheritance model | G/G – C/C | 177 (88.5) | 177 (88.9) | 1 | 0.89 |
| C/G | 23 (11.5) | 22 (11.1) | 0.96 (0.51-1.78) | ||
| SNP | Genotype [n (%)] | P* | |||
| Extremely early PTB (n = 16) | Early PTB (n = 32) |
Late PTB (n = 151) |
|||
| TNFα (rs1800629) | A/A | 0 | 0 | 7 (5) | 0,91 |
| A/G | 3 (19) | 7 (22) | 33 (22) | ||
| G/G | 13 (81) | 25 (78) | 111 (73) | ||
| IL – 10 (rs1800896) | A/A | 5 (31) | 12 (38) | 45 (30) | 0,10 |
| A/G | 6 (38) | 19 (59) | 84 (56) | ||
| G/G | 5 (31) | 1 (3) | 22 (14) | ||
| IL – 6 (rs1800796) | C/C | 0 | 0 | 1 (1) | 0,89 |
| C/G | 1 (6) | 4 (13) | 17 (11) | ||
| G/G | 15 (94) | 28 (88) | 133 (88) | ||
| SNP/Inheritance model | Genotype [n (%)] | OR (95 % CI) |
P* | ||
| Term birth (n = 200) |
Extremely early PTB (n = 16) |
||||
| TNFα (rs1800629) | G/G | 154 (77) | 13 (81.2) | 1 | 0.81 |
| A/G | 44 (22) | 3 (18.8) | 0.81 (0.22 – 2.96) | ||
| A/A | 2 (1) | 0 | 0 (0 – NA) | ||
| Alelle | G | 352 (88) | 29 (91) | 1.32 (0.39 – 4.49) | 0.66 |
| A | 48 (12) | 3 (9) | |||
| Dominant model of inheritance | G/G | 154 (77) | 13 (81.2) | 1 | 0.69 |
| A/G – A/A | 46 (23) | 3 (18.8) | 0.77 (0.21 – 2.83) | ||
| Recessive model of inheritance | G/G – A/G | 198 (99) | 16 (100) | 1 | 0.58 |
| A/A | 2 (1) | 0 | 0 (0 – NA) | ||
| Superdominant model of inheritance | G/G – A/A | 156 (78) | 13 (81.2) | 1 | 0.76 |
| A/G | 44 (22) | 3 (18.8) | 0.82 (0.22 – 3.0) | ||
| IL – 10 (rs1800896) | A/A | 68 (34) | 5 (31.2) | 1 | 0.71 |
| A/G | 88 (44) | 6 (37.5) | 0.93 (0.27 – 3.17) | ||
| G/G | 44 (22) | 5 (31.2) | 1.55 (0.42 – 5.65) | ||
| Alelle | A | 224 (56) | 16 (50) | 0.79 (0.38 – 1.62) | 0.51 |
| G | 176 (44) | 16 (50) | |||
| Dominant model of inheritance | A/A | 68 (34) | 5 (312) | 1 | 0.82 |
| A/G – G/G | 132 (66) | 11 (68.8) | 1.13 (0.38 – 3.39) | ||
| Recessive model of inheritance | A/A – A/G | 156 (78) | 11 (68,8) | 1 | 0.41 |
| G/G | 44 (22) | 5 (31.2) | 1.61 (0.53 – 4.88) | ||
| Superdominant model of inheritance | A/A – G/G | 112 (56) | 10 (62.5) | 1 | 0.61 |
| A/G | 88 (44) | 6 (37.5) | 0.76 (0.27 – 2.18) | ||
| IL – 6 (rs1800796) | G/G | 176 (88) | 15 (93.8) | 1 | 0.73 |
| C/G | 23 (11.5) | 1 (6.2) | 0.51 (0.06 – 4.04) | ||
| C/C | 1 (0.5) | 0 | 0 (0 – NA) | ||
| Alelle | G | 375 (94) | 31 (97) | 2,07 (0.27 – 15.77) | 0.48 |
| C | 25 (6) | 1 (3) | |||
| Dominant model of inheritance | G/G | 176 (88) | 15 (93.8) | 1 | 0.46 |
| C/G – C/C | 24 (12) | 1 (6.2) | 0.49 (0.06 – 3.87) | ||
| Recessive model of inheritance | G/G – C/G | 199 (99.5) | 16 (100) | 1 | 0.69 |
| C/C | 1 (0.5) | 0 | 0 (0 – NA) | ||
| Superdominant model of inheritance | G/G – C/C | 177 (88.5) | 15 (93.8) | 1 | 0.44 |
| C/G | 23 (11.5) | 1 (6.2) | 0,51 (0.06 – 4.07) | ||
| G/G | 176 (88) | 15 (93.8) | 1 | ||
| SNP/inheritance models | Genotype [n (%)] | OR (95 % CI) |
P* | ||
| Term birth (n = 200) |
Early PTB (n = 32) |
||||
| TNFα (rs1800629) | G/G | 154 (77) | 25 (78.1) | 1 | .,74 |
| A/G | 44 (22) | 7 (21.9) | 0.98 (0.40 – 2.42) | ||
| A/A | 2 (1) | 0 | 0 (0 – NA) | ||
| Alelle | G | 352 (88) | 57 (89) | 1.11 (0.48 – 2.57) | 0.81 |
| A | 48 (12) | 7 (11) | |||
| Dominant inheritance model | G/G | 154 (77) | 25 (78.1) | 1 | 0.89 |
| A/G – A/A | 46 (23) | 7 (21.9) | 0-94 (0.38-2.31) | ||
| Recessive inheritance model | G/G – A/G | 198 (99) | 32 (100) | 1 | 0.44 |
| A/A | 2 (1) | 0 | 0 (0 - NA) | ||
| Superdominant inheritance model | G/G – A/A | 156 (78) | 25 (78.1) | 1 | 0.99 |
| A/G | 44 (22) | 7 (21.9) | 0.99 (0.40-2.45) | ||
| IL – 10 (rs1800896) | A/A | 68 (34) | 12 (37,5) | 1 | 0.01 |
| A/G | 88 (44) | 19 (59,4) | 1.22 (0.56 – 2.69) | ||
| G/G | 44 (22) | 1 (3,1) | 0.13 (0.02 – 1.03) | ||
| Alelle | A | 224 (56) | 43 (67) | 1.61 (0.92 – 2.81) | 0.09 |
| G | 176 (44) | 21 (33) | |||
| Dominant inheritance model | A/A | 68 (34) | 12 (37.5) | 1 | 0.70 |
| A/G – G/G | 132 (66) | 20 (62.5) | 0.86 (0.40-1.86) | ||
| Recessive inheritance model | A/A – A/G | 156 (78) | 31 (96.9) | 1 | 0.003 |
| G/G | 44 (22) | 1 (3.1) | 0.11 (0.02-0.86) | ||
| Superdominant inheritance model | A/A – G/G | 112 (56) | 13 (40.6) | 1 | 0.11 |
| A/G | 88 (44) | 19 (59.4) | 1.86 (0.87-3.97) | ||
| IL – 6 (rs1800796) | G/G | 176 (88) | 28 (87.5) | 1 | 0.85 |
| C/G | 23 (11.5) | 4 (12.5) | 1.09 (0.35 – 3.40) | ||
| C/C | 1 (0.5) | 0 | 0 (0 – NA) | ||
| Alelle | G | 375 (94) | 60 (94) | 1.0 (0.34 – 2.97) | >0.99 |
| C | 25 (6) | 4 (6) | |||
| Dominant inheritance model | G/G | 176 (88) | 28 (87,5) | 1 | 0.94 |
| C/G – C/C | 24 (12) | 4 (12,5) | 1.05 (0.34-3.25) | ||
| Recessive inheritance model | G/G – C/G | 199 (99.5) | 32 (100) | 1 | 0.59 |
| C/C | 1 (0.5) | 0 | 0 (0 - NA) | ||
| Superdominant inheritance model | G/G – C/C | 177 (88.5) | 28 (87.5) | 1 | 0.87 |
| C/G | 23 (11.5) | 4 (12.5) | 1.10 (0.35-3.42) | ||
|
SNP/inheritance models |
Genotype [n (%)] | OR (95 % CI) |
P* | ||
| Term birth (n = 200) |
Late PTB (n = 151) |
||||
| TNFα(rs1800629) | G/G | 154 (77) | 111 (73.5) | 1 | 0.09 |
| A/G | 44 (22) | 33 (21.9) | 1.04 (0.62-1.74) | ||
| A/A | 2 (1) | 7 (4.6) | 4.86 (0.99-23.82) | ||
| Alelle | G | 352 (88) | 255 (84) | 0.69 (0.45 – 1.07) | 0.09 |
| A | 48 (12) | 47 (16) | |||
| Dominant inheritance model | G/G | 154 (77) | 111 (73.5) | 1 | 0.45 |
| A/G – A/A | 46 (23) | 40 (26.5) | 1.21 (0.74-1.97) | ||
| Recessive inheritance model | G/G – A/G | 198 (99) | 144 (95.4) | 1 | 0.03 |
| A/A | 2 (1) | 7 (4.6) | 4.81 (0.99-23.51) | ||
| Superdominant inheritance model | G/G – A/A | 156 (78) | 118 (78.2) | 1 | 0.97 |
| A/G | 44 (22) | 33 (21.9) | 0.99 (0.59-1.65) | ||
| IL – 10 (rs1800896) | A/A | 68 (34) | 45 (29.8) | 1 | 0.07 |
| A/G | 88 (44) | 84 (55.6) | 1.44 (0.89-2.33) | ||
| G/G | 44 (22) | 22 (14.6) | 0.76 (0.40-1.43) | ||
| Alelle | A | 224 (56) | 174 (58) | 1.07 (0.79 – 1.44) | 0.67 |
| G | 176 (44) | 128 (42) | |||
| Dominant inheritance model | A/A | 68 (34) | 45 (29.8) | 1 | 0.40 |
| A/G – G/G | 132 (66) | 106 (70.2) | 1.21 (0.77-1.91) | ||
| Recessive inheritance model | A/A – A/G | 156 (78) | 129 (85.4) | 1 | 0.08 |
| G/G | 44 (22) | 22 (14.6) | 0.60 (0.34-1.06) | ||
| Superdominant inheritance model | A/A – G/G | 112 (56) | 67 (44.4) | 1 | 0.03 |
| A/G | 88 (44) | 84 (55.6) | 1.60 (1.04-2.44) | ||
| IL – 6 (rs1800796) | G/G | 176 (88) | 133 (88.1) | 1 | 0.98 |
| C/G | 23 (11,5) | 17 (11.3) | 0.98 (0.50-1.90) | ||
| C/C | 1 (0.5) | 1 (0.7) | 1.32 (0.08-21.35) | ||
| Alelle | G | 375 (94) | 283 (94) | 0.99 (0.54 – 1.84) | 0.98 |
| C | 25 (6) | 19 (6) | |||
| Dominant inheritance model | G/G | 176 (88) | 133 (88.1) | 1 | 0.98 |
| C/G – C/C | 24 (12) | 18 (11.9) | 0.99 (0.52-1.90) | ||
| Recessive inheritance model | G/G – C/G | 199 (99.5) | 150 (99.3) | 1 | 0.84 |
| C/C | 1 (0.5) | 1 (0.7) | 1.33 (0.08-21.38) | ||
| Superdominant inheritance model | G/G – C/C | 177 (88.5) | 134 (88.7) | 1 | 0.94 |
| C/G | 23 (11.5) | 17 (11.3) | 0.98 (0.50-1.90) | ||
| Haplotype | n (%) | OR (95 %C I) | χ2 | P* | adjP† | |||
| PTB | Term birth | |||||||
| Mothers | χ2 = 2,41 df = 4 P = 0,66 |
|||||||
| rs1800629 | rs1800896 | rs1800796 | ||||||
| G | G | G | 117 (29.3) | 134 (33.5) | 0.83 (0.61 – 1.11) | 1.56 | 0.22 | 0.42 |
| G | A | G | 210 (52.7) | 199 (49.7) | 1.13 (0.85 – 1.49) | 0.73 | 0.21 | 0.55 |
| A | G | G | 29 (7.2) | 25 (6.2) | 1.18 (0.68 – 2.05) | 0.34 | 0.56 | 0.64 |
| A | A | G | 18 (4.5) | 17 (4.2) | 1.07 (0.54 – 2.10) | 0.67 | 0.41 | 0.85 |
| G | G | C | 10 (2.5) | 14 (3.5) | 0.71 (0.31 - 1.62) | 0.04 | 0.85 | 0.85 |
| ß | Wald | P | OR (95 CI%) | |
| * Bivariant logistic regression | ||||
| TNFα (rs1800629) (A/G – A/A vs. G/G) | 0.738 | 5.47 | 0.02 | 2.09 (1.13 – 3.88) |
| IL – 10 (rs1800896) (A/G – G/G vs. A/A) | 0.105 | 0.22 | 0.64 | 1.11 (0.72 – 1.71) |
| IL – 6 (rs1800796) (C/G – C/C vs. G/G) | -0.225 | 0.46 | 0.50 | 0.80 (0.42 – 1.53) |
| * Multivariant logistic regression | ||||
| TNFα (rs1800629) (A/G – A/A vs. G/G) | 0.74 | 5.47 | 0.02 | 2.10 (1.13 to 3.88) |
| Constant | -0.76 | 0.66 | 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





