Submitted:
20 March 2024
Posted:
21 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
Data Collection and Analysis
3. Results
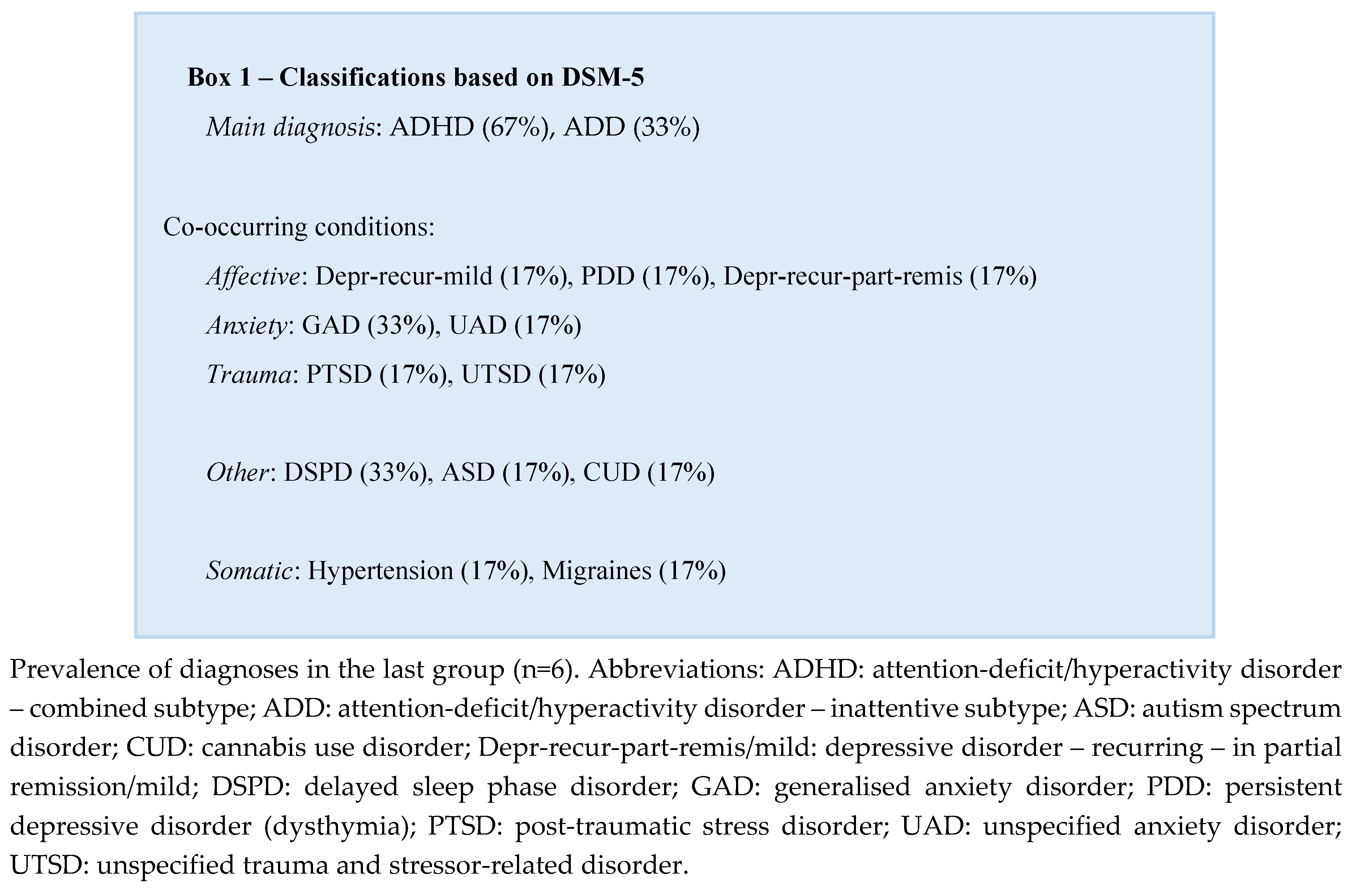
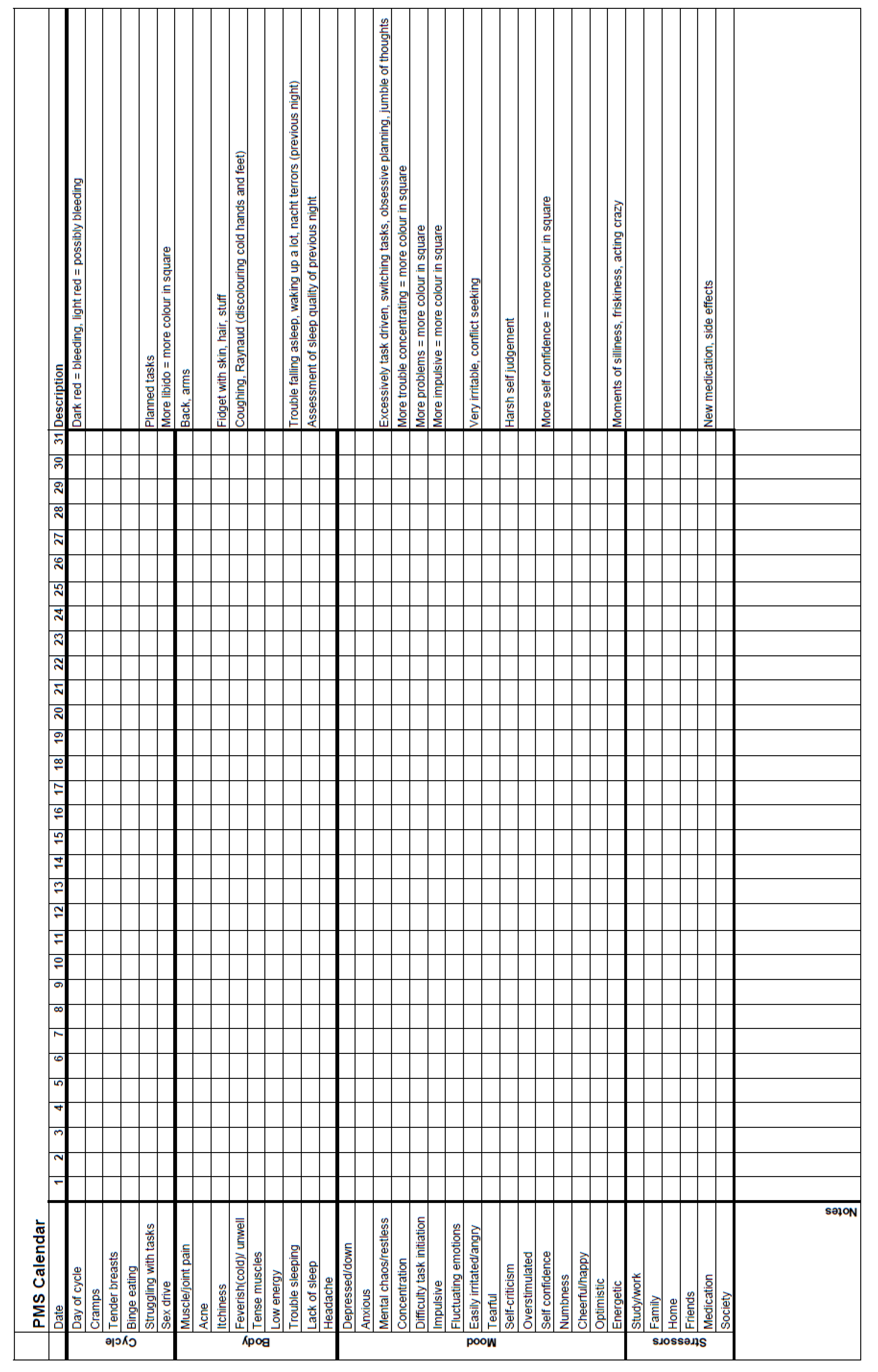
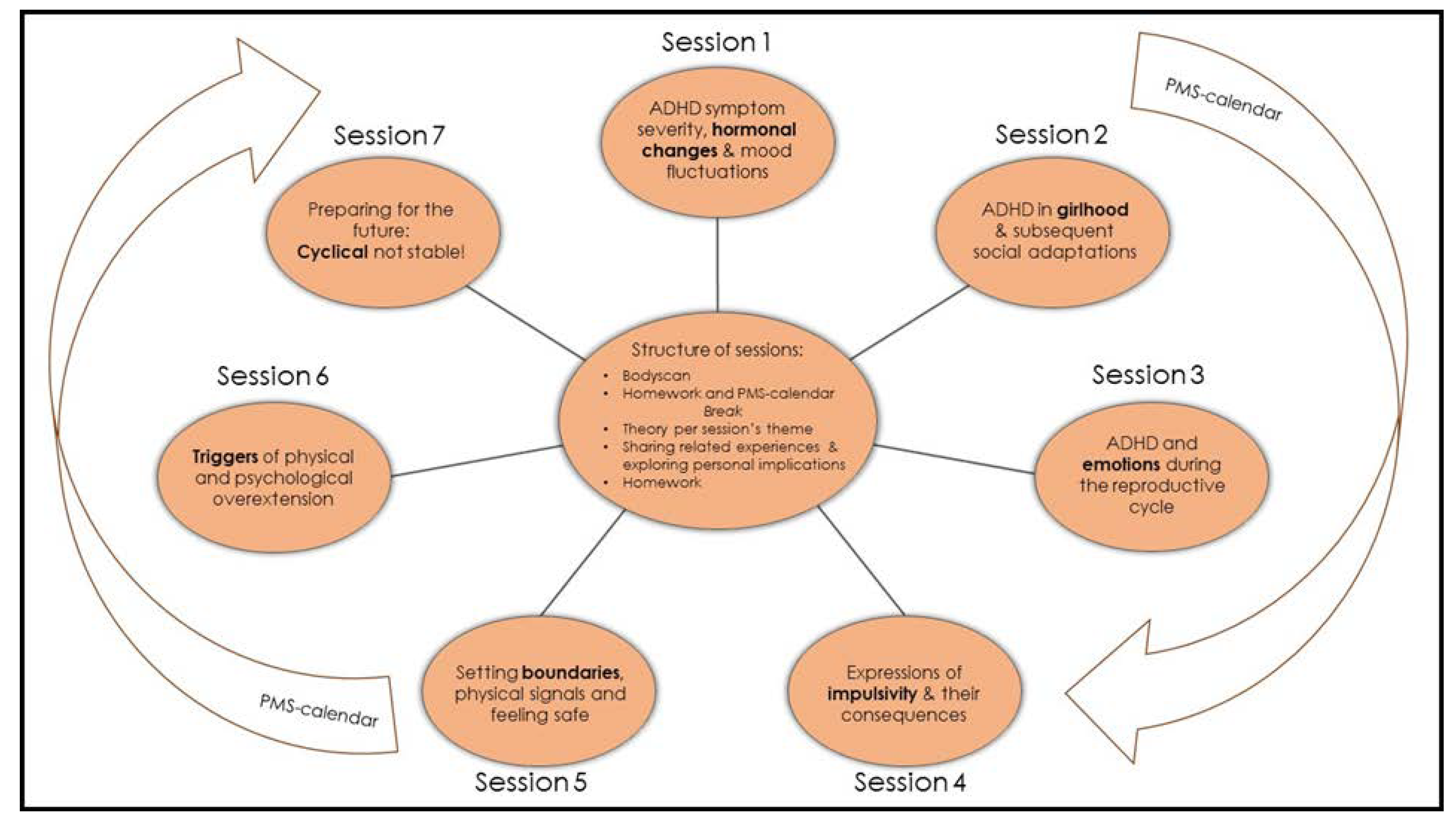
3.1. The Group Programme
3.1.1. Session 1: The Menstrual Cycle
3.1.2. Session 2: ADHD in Childhood for Girls
3.1.3. Session 3: ADHD and Emotionality
3.1.4. Session 4: ADHD and Impulsivity
3.1.5. Session 5: ADHD, Boundaries and Safety
3.1.6. Session 6: ADHD and Triggers
3.1.7. Session 7: The Future
3.2. Experiences
Evaluation
4. Discussion
4.1. Merging Practice and Research
4.2. A Group Setting
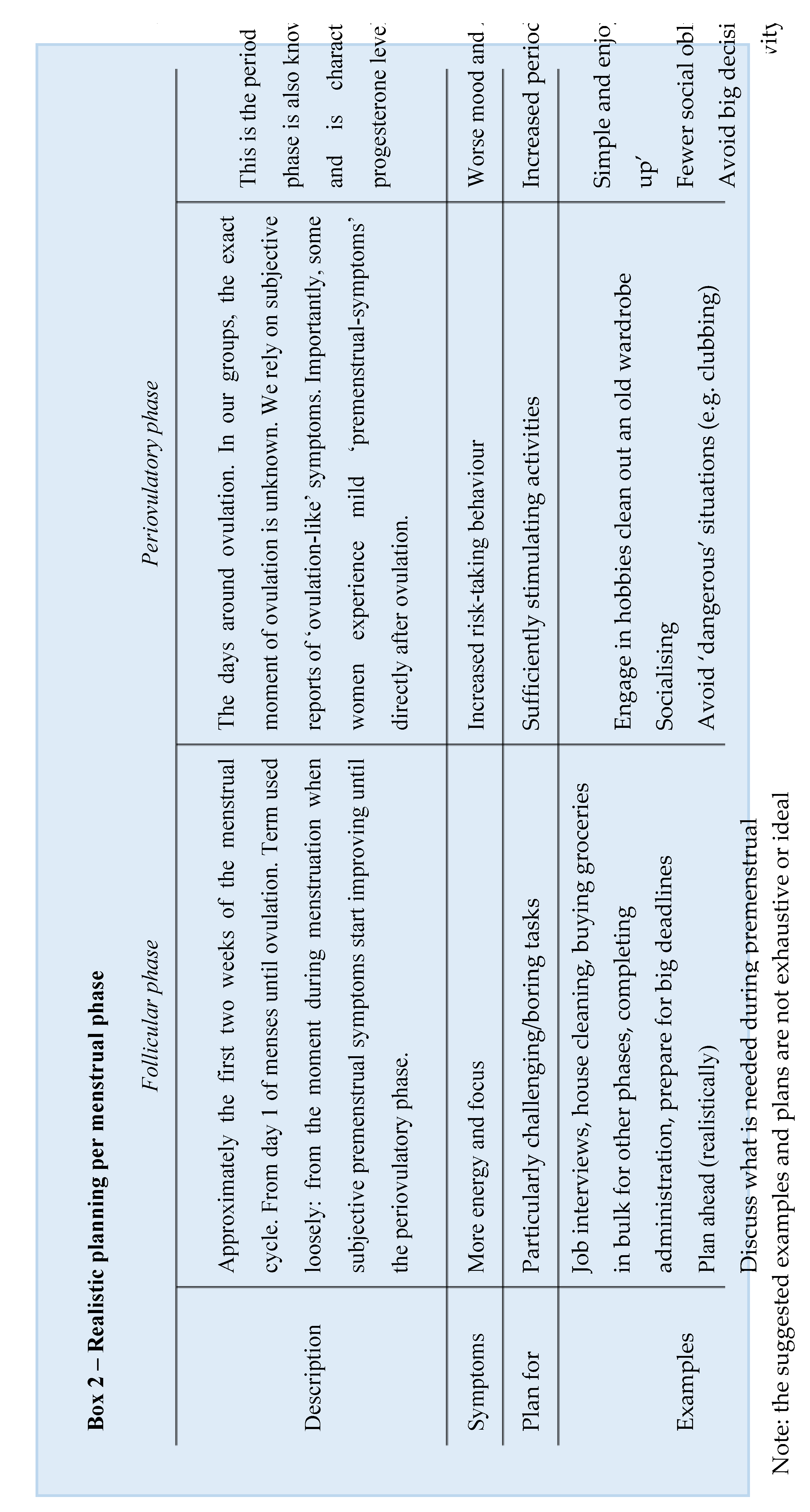
4.3. Time and Planning
4.4. Masking the Menstrual Cycle
4.5. Physically Stressed
4.6. Understanding and Connection
4.7. Limitations and Strengths
4.8. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Dorani, F.; Bijlenga, D.; Beekman, A.T.F.; van Someren, E.J.W.; Kooij, J.J.S. Prevalence of hormone-related mood disorder symptoms in women with ADHD. J Psychiatr Res 2021, 133, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Berry, C.A.; Shaywitz, S.E.; Shaywitz, B.A. Girls with attention deficit disorder: a silent minority? A report on behavioral and cognitive characteristics. Pediatrics 1985, 76, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Waite, R. Women and attention deficit disorders: a great burden overlooked. J Am Acad Nurse Pract 2007, 19, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Williamson, D.; Johnston, C. Gender differences in adults with attention-deficit/hyperactivity disorder: A narrative review. Clin Psychol Rev 2015, 40, 15–27. [Google Scholar] [CrossRef] [PubMed]
- Cortese, S.; Faraone, S.V.; Bernardi, S.; Wang, S.; Blanco, C. Gender differences in adult attention-deficit/hyperactivity disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). J Clin Psychiatry 2016, 77, e421–428. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.; Malloy-Diniz, L.; Garcia, M.; Rocha, R. Attention-Deficit/Hyperactivity Disorder and Women. 2020; pp. 215-219.
- Hinshaw, S.P.; Nguyen, P.T.; O'Grady, S.M.; Rosenthal, E.A. Annual Research Review: Attention-deficit/hyperactivity disorder in girls and women: underrepresentation, longitudinal processes, and key directions. J Child Psychol Psychiatry 2022, 63, 484–496. [Google Scholar] [CrossRef] [PubMed]
- Nussbaum, N.L. ADHD and Female Specific Concerns:A Review of the Literature and Clinical Implications. Journal of Attention Disorders 2012, 16, 87–100. [Google Scholar] [CrossRef] [PubMed]
- Arnold, L.E.; Hodgkins, P.; Caci, H.; Kahle, J.; Young, S. Effect of treatment modality on long-term outcomes in attention-deficit/hyperactivity disorder: a systematic review. PLoS One 2015, 10, e0116407. [Google Scholar] [CrossRef]
- Faraone, S.V.; Banaschewski, T.; Coghill, D.; Zheng, Y.; Biederman, J.; Bellgrove, M.A.; Newcorn, J.H.; Gignac, M.; Al Saud, N.M.; Manor, I.; et al. The World Federation of ADHD International Consensus Statement: 208 Evidence-based conclusions about the disorder. Neurosci Biobehav Rev 2021, 128, 789–818. [Google Scholar] [CrossRef]
- Young, S.; Adamo, N.; Ásgeirsdóttir, B.B.; Branney, P.; Beckett, M.; Colley, W.; Cubbin, S.; Deeley, Q.; Farrag, E.; Gudjonsson, G.; et al. Females with ADHD: An expert consensus statement taking a lifespan approach providing guidance for the identification and treatment of attention-deficit/ hyperactivity disorder in girls and women. BMC Psychiatry 2020, 20, 404. [Google Scholar] [CrossRef]
- Quinn, P.O.; Madhoo, M. A review of attention-deficit/hyperactivity disorder in women and girls: uncovering this hidden diagnosis. Prim Care Companion CNS Disord 2014, 16. [Google Scholar] [CrossRef] [PubMed]
- Kok, F.M.; Groen, Y.; Fuermaier, A.B.M.; Tucha, O. The female side of pharmacotherapy for ADHD-A systematic literature review. PLoS One 2020, 15, e0239257. [Google Scholar] [CrossRef]
- Camara, B.; Padoin, C.; Bolea, B. Relationship between sex hormones, reproductive stages and ADHD: a systematic review. Arch Womens Ment Health 2022, 25, 1–8. [Google Scholar] [CrossRef]
- Chronis-Tuscano, A. ADHD in girls and women: a call to action - reflections on Hinshaw et al. (2021). J Child Psychol Psychiatry 2022, 63, 497–499. [Google Scholar] [CrossRef]
- Fuller-Thomson, E.; Lewis, D.A.; Agbeyaka, S.K. Attention-deficit/hyperactivity disorder casts a long shadow: findings from a population-based study of adult women with self-reported ADHD. Child Care Health Dev 2016, 42, 918–927. [Google Scholar] [CrossRef] [PubMed]
- Gutman, S.A.; Balasubramanian, S.; Herzog, M.; Kim, E.; Swirnow, H.; Retig, Y.; Wolff, S. Effectiveness of a Tailored Intervention for Women With Attention Deficit Hyperactivity Disorder (ADHD) and ADHD Symptoms: A Randomized Controlled Study. Am J Occup Ther 2020, 74, 7401205010p7401205011–7401205010p7401205011. [Google Scholar] [CrossRef]
- Soares, C.N.; Zitek, B. Reproductive hormone sensitivity and risk for depression across the female life cycle: a continuum of vulnerability? J Psychiatry Neurosci 2008, 33, 331–343. [Google Scholar] [PubMed]
- Roberts, B.; Eisenlohr-Moul, T.; Martel, M.M. Reproductive steroids and ADHD symptoms across the menstrual cycle. Psychoneuroendocrinology 2018, 88, 105–114. [Google Scholar] [CrossRef]
- Barth, C.; Villringer, A.; Sacher, J. Sex hormones affect neurotransmitters and shape the adult female brain during hormonal transition periods. Front Neurosci 2015, 9, 37. [Google Scholar] [CrossRef]
- Steiner, M.; Dunn, E.; Born, L. Hormones and mood: from menarche to menopause and beyond. J Affect Disord 2003, 74, 67–83. [Google Scholar] [CrossRef]
- Hwang, W.J.; Lee, T.Y.; Kim, N.S.; Kwon, J.S. The Role of Estrogen Receptors and Their Signaling across Psychiatric Disorders. Int J Mol Sci 2020, 22. [Google Scholar] [CrossRef] [PubMed]
- Shanmugan, S.; Epperson, C.N. Estrogen and the prefrontal cortex: towards a new understanding of estrogen's effects on executive functions in the menopause transition. Hum Brain Mapp 2014, 35, 847–865. [Google Scholar] [CrossRef] [PubMed]
- Hylan, T.R.; Sundell, K.; Judge, R. The impact of premenstrual symptomatology on functioning and treatment-seeking behavior: experience from the United States, United Kingdom, and France. J Womens Health Gend Based Med 1999, 8, 1043–1052. [Google Scholar] [CrossRef] [PubMed]
- Dubol, M.; Epperson, C.N.; Sacher, J.; Pletzer, B.; Derntl, B.; Lanzenberger, R.; Sundström-Poromaa, I.; Comasco, E. Neuroimaging the menstrual cycle: A multimodal systematic review. Front Neuroendocrinol 2021, 60, 100878. [Google Scholar] [CrossRef] [PubMed]
- Sacher, J.; Okon-Singer, H.; Villringer, A. Evidence from neuroimaging for the role of the menstrual cycle in the interplay of emotion and cognition. Front Hum Neurosci 2013, 7, 374. [Google Scholar] [CrossRef] [PubMed]
- Gervais, N.J.; Mong, J.A.; Lacreuse, A. Ovarian hormones, sleep and cognition across the adult female lifespan: An integrated perspective. Front Neuroendocrinol 2017, 47, 134–153. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo-Lopez, E.; Pletzer, B. Interactive Effects of Dopamine Baseline Levels and Cycle Phase on Executive Functions: The Role of Progesterone. Front Neurosci 2017, 11, 403. [Google Scholar] [CrossRef] [PubMed]
- Handy, A.B.; Greenfield, S.F.; Yonkers, K.A.; Payne, L.A. Psychiatric Symptoms Across the Menstrual Cycle in Adult Women: A Comprehensive Review. Harv Rev Psychiatry 2022, 30, 100–117. [Google Scholar] [CrossRef]
- Haimov-Kochman, R.; Berger, I. Cognitive functions of regularly cycling women may differ throughout the month, depending on sex hormone status; a possible explanation to conflicting results of studies of ADHD in females. Front Hum Neurosci 2014, 8, 191. [Google Scholar] [CrossRef]
- Quinn, P.O. Treating adolescent girls and women with ADHD: gender-specific issues. J Clin Psychol 2005, 61, 579–587. [Google Scholar] [CrossRef]
- de Jong, M.; Wynchank, D.S.M.R.; van Andel, E.; Beekman, A.T.F.; Kooij, J.J.S. Female-specific pharmacotherapy in ADHD: premenstrual adjustment of psychostimulant dosage. Frontiers in Psychiatry 2023, 14. [Google Scholar] [CrossRef] [PubMed]
- Kooij, J.J.S.; Bijlenga, D.; Salerno, L.; Jaeschke, R.; Bitter, I.; Balazs, J.; Thome, J.; Dom, G.; Kasper, S.; Nunes Filipe, C.; et al. Updated European Consensus Statement on diagnosis and treatment of adult ADHD. Eur Psychiatry 2019, 56, 14–34. [Google Scholar] [CrossRef]
- Cortese, S.; Moreira-Maia, C.R.; St Fleur, D.; Morcillo-Peñalver, C.; Rohde, L.A.; Faraone, S.V. Association Between ADHD and Obesity: A Systematic Review and Meta-Analysis. Am J Psychiatry 2016, 173, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Katzman, M.A.; Bilkey, T.S.; Chokka, P.R.; Fallu, A.; Klassen, L.J. Adult ADHD and comorbid disorders: clinical implications of a dimensional approach. BMC Psychiatry 2017, 17, 302. [Google Scholar] [CrossRef]
- Attoe, D.E.; Climie, E.A. Miss. Diagnosis: A Systematic Review of ADHD in Adult Women. J Atten Disord 2023, 10870547231161533. [Google Scholar] [CrossRef]
- Rasmussen, K.; Levander, S. Untreated ADHD in Adults: Are There Sex Differences in Symptoms, Comorbidity, and Impairment? Journal of attention disorders 2009, 12, 353–360. [Google Scholar] [CrossRef]
- Groß-Lesch, S.; Dempfle, A.; Reichert, S.; Jans, T.; Geissler, J.; Kittel-Schneider, S.; Nguyen, T.T.; Reif, A.; Lesch, K.-P.; Jacob, C.P. Sex- and Subtype-Related Differences in the Comorbidity of Adult ADHDs. Journal of Attention Disorders 2016, 20, 855–866. [Google Scholar] [CrossRef] [PubMed]
- Faheem, M.; Akram, W.; Akram, H.; Khan, M.A.; Siddiqui, F.A.; Majeed, I. Gender-based differences in prevalence and effects of ADHD in adults: A systematic review. Asian J Psychiatr 2022, 75, 103205. [Google Scholar] [CrossRef]
- Robison, R.J.; Reimherr, F.W.; Marchant, B.K.; Faraone, S.V.; Adler, L.A.; West, S.A. Gender differences in 2 clinical trials of adults with attention-deficit/hyperactivity disorder: a retrospective data analysis. J Clin Psychiatry 2008, 69, 213–221. [Google Scholar] [CrossRef]
- Ahlberg, R.; Du Rietz, E.; Ahnemark, E.; Andersson, L.M.; Werner-Kiechle, T.; Lichtenstein, P.; Larsson, H.; Garcia-Argibay, M. Real-life instability in ADHD from young to middle adulthood: a nationwide register-based study of social and occupational problems. BMC Psychiatry 2023, 23, 336. [Google Scholar] [CrossRef]
- Faraone, S.V.; Rostain, A.L.; Blader, J.; Busch, B.; Childress, A.C.; Connor, D.F.; Newcorn, J.H. Practitioner Review: Emotional dysregulation in attention-deficit/hyperactivity disorder - implications for clinical recognition and intervention. J Child Psychol Psychiatry 2019, 60, 133–150. [Google Scholar] [CrossRef]
- Christiansen, H.; Hirsch, O.; Albrecht, B.; Chavanon, M.L. Attention-Deficit/Hyperactivity Disorder (ADHD) and Emotion Regulation Over the Life Span. Curr Psychiatry Rep 2019, 21, 17. [Google Scholar] [CrossRef]
- El Archi, S.; Barrault, S.; Garcia, M.; Branger, S.; Maugé, D.; Ballon, N.; Brunault, P. Adult ADHD Diagnosis, Symptoms of Impulsivity, and Emotional Dysregulation in a Clinical Sample of Outpatients Consulting for a Behavioral Addiction. J Atten Disord 2023, 27, 731–742. [Google Scholar] [CrossRef]
- Lenzi, F.; Cortese, S.; Harris, J.; Masi, G. Pharmacotherapy of emotional dysregulation in adults with ADHD: A systematic review and meta-analysis. Neurosci Biobehav Rev 2018, 84, 359–367. [Google Scholar] [CrossRef]
- Edel, M.A.; Rudel, A.; Hubert, C.; Scheele, D.; Brüne, M.; Juckel, G.; Assion, H.J. Alexithymia, emotion processing and social anxiety in adults with ADHD. Eur J Med Res 2010, 15, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Eng, A.G.; Nirjar, U.; Elkins, A.R.; Sizemore, Y.J.; Monticello, K.N.; Petersen, M.K.; Miller, S.A.; Barone, J.; Eisenlohr-Moul, T.A.; Martel, M.M. Attention-deficit/hyperactivity disorder and the menstrual cycle: Theory and evidence. Horm Behav 2023, 158, 105466. [Google Scholar] [CrossRef] [PubMed]
- van Vliet, I.M.; de Beurs, E. [The MINI-International Neuropsychiatric Interview. A brief structured diagnostic psychiatric interview for DSM-IV en ICD-10 psychiatric disorders]. Tijdschr Psychiatr 2007, 49, 393–397. [Google Scholar] [PubMed]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998, 59 Suppl 20, 22-33;quiz 34-57.
- Sevinc, G.; Hölzel, B.K.; Hashmi, J.; Greenberg, J.; McCallister, A.; Treadway, M.; Schneider, M.L.; Dusek, J.A.; Carmody, J.; Lazar, S.W. Common and Dissociable Neural Activity After Mindfulness-Based Stress Reduction and Relaxation Response Programs. Psychosom Med 2018, 80, 439–451. [Google Scholar] [CrossRef] [PubMed]
- Zsido, R.G.; Williams, A.N.; Barth, C.; Serio, B.; Kurth, L.; Mildner, T.; Trampel, R.; Beyer, F.; Witte, A.V.; Villringer, A.; et al. Ultra-high-field 7T MRI reveals changes in human medial temporal lobe volume in female adults during menstrual cycle. Nature Mental Health 2023, 1, 761–771. [Google Scholar] [CrossRef]
- Loyer Carbonneau, M.; Demers, M.; Bigras, M.; Guay, M.-C. Meta-Analysis of Sex Differences in ADHD Symptoms and Associated Cognitive Deficits. Journal of Attention Disorders 2021, 25, 1640–1656. [Google Scholar] [CrossRef] [PubMed]
- Mowlem, F.D.; Rosenqvist, M.A.; Martin, J.; Lichtenstein, P.; Asherson, P.; Larsson, H. Sex differences in predicting ADHD clinical diagnosis and pharmacological treatment. Eur Child Adolesc Psychiatry 2019, 28, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Quinn, P.; Wigal, S. Perceptions of girls and ADHD: results from a national survey. MedGenMed 2004, 6, 2. [Google Scholar] [PubMed]
- Rucklidge, J.J. Gender differences in attention-deficit/hyperactivity disorder. Psychiatr Clin North Am 2010, 33, 357–373. [Google Scholar] [CrossRef] [PubMed]
- Zalecki, C.A.; Hinshaw, S.P. Overt and relational aggression in girls with attention deficit hyperactivity disorder. J Clin Child Adolesc Psychol 2004, 33, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Quinn, P.O. Attention-deficit/hyperactivity disorder and its comorbidities in women and girls: an evolving picture. Curr Psychiatry Rep 2008, 10, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Rucklidge, J.J.; Tannock, R. Psychiatric, psychosocial, and cognitive functioning of female adolescents with ADHD. Journal of the American Academy of Child and Adolescent Psychiatry 2001, 40 5, 530–540. [Google Scholar] [CrossRef]
- Rosenthal, E.A.; Hinshaw, S.P. Pubertal timing in adolescents with ADHD: extension and replication in an all-female sample. Eur Child Adolesc Psychiatry 2023. [Google Scholar] [CrossRef] [PubMed]
- Waite, R. Women with ADHD: it is an explanation, not the excuse du jour. Perspect Psychiatr Care 2010, 46, 182–196. [Google Scholar] [CrossRef]
- Holthe, M.E.G.; Langvik, E. The strives, struggles, and successes of women diagnosed with ADHD as adults. Sage Open 2017, 7, 2158244017701799. [Google Scholar] [CrossRef]
- Yonkers, K.A.; O'Brien, P.M.; Eriksson, E. Premenstrual syndrome. Lancet 2008, 371, 1200–1210. [Google Scholar] [CrossRef]
- Halbreich, U.; Borenstein, J.; Pearlstein, T.; Kahn, L.S. The prevalence, impairment, impact, and burden of premenstrual dysphoric disorder (PMS/PMDD). Psychoneuroendocrinology 2003, 28 Suppl 3, 1–23. [Google Scholar] [CrossRef]
- Diekhof, E.K. Be quick about it. Endogenous estradiol level, menstrual cycle phase and trait impulsiveness predict impulsive choice in the context of reward acquisition. Horm Behav 2015, 74, 186–193. [Google Scholar] [CrossRef]
- Crider, A.; Pillai, A. Estrogen Signaling as a Therapeutic Target in Neurodevelopmental Disorders. J Pharmacol Exp Ther 2017, 360, 48–58. [Google Scholar] [CrossRef]
- Lockinger, K.; Gagnon, M.M. Dysmenorrhea and psychological wellbeing among females with attention deficit hyperactivity disorder. J Health Psychol 2023, 13591053231177254. [Google Scholar] [CrossRef] [PubMed]
- Sedgwick, J.A.; Merwood, A.; Asherson, P. The positive aspects of attention deficit hyperactivity disorder: a qualitative investigation of successful adults with ADHD. Atten Defic Hyperact Disord 2019, 11, 241–253. [Google Scholar] [CrossRef] [PubMed]
- Joyce, K.M.; Good, K.P.; Tibbo, P.; Brown, J.; Stewart, S.H. Addictive behaviors across the menstrual cycle: a systematic review. Arch Womens Ment Health 2021, 24, 529–542. [Google Scholar] [CrossRef] [PubMed]
- Kaisari, P.; Dourish, C.T.; Higgs, S. Attention Deficit Hyperactivity Disorder (ADHD) and disordered eating behaviour: A systematic review and a framework for future research. Clin Psychol Rev 2017, 53, 109–121. [Google Scholar] [CrossRef] [PubMed]
- Svedlund, N.E.; Norring, C.; Ginsberg, Y.; von Hausswolff-Juhlin, Y. Symptoms of Attention Deficit Hyperactivity Disorder (ADHD) among adult eating disorder patients. BMC Psychiatry 2017, 17, 19. [Google Scholar] [CrossRef] [PubMed]
- Svedlund, N.E.; Norring, C.; Ginsberg, Y.; von Hausswolff-Juhlin, Y. Are treatment results for eating disorders affected by ADHD symptoms? A one-year follow-up of adult females. Eur Eat Disord Rev 2018, 26, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Halevy-Yosef, R.; Bachar, E.; Shalev, L.; Pollak, Y.; Enoch-Levy, A.; Gur, E.; Weizman, A.; Stein, D. The complexity of the interaction between binge-eating and attention. PLoS One 2019, 14, e0215506. [Google Scholar] [CrossRef]
- Sala, L.; Martinotti, G.; Carenti, M.L.; Romo, L.; Oumaya, M.; Pham-Scottez, A.; Rouillon, F.; Gorwood, P.; Janiri, L. Attention-deficit/hyperactivity disorder symptoms and psychological comorbidity in eating disorder patients. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity 2018, 23, 513–519. [Google Scholar] [CrossRef]
- El Archi, S.; Cortese, S.; Ballon, N.; Réveillère, C.; De Luca, A.; Barrault, S.; Brunault, P. Negative Affectivity and Emotion Dysregulation as Mediators between ADHD and Disordered Eating: A Systematic Review. Nutrients 2020, 12. [Google Scholar] [CrossRef]
- Biederman, J.; Ball, S.W.; Monuteaux, M.C.; Surman, C.B.; Johnson, J.L.; Zeitlin, S. Are girls with ADHD at risk for eating disorders? Results from a controlled, five-year prospective study. J Dev Behav Pediatr 2007, 28, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Klump, K.L.; Keel, P.K.; Racine, S.E.; Burt, S.A.; Neale, M.; Sisk, C.L.; Boker, S.; Hu, J.Y. The interactive effects of estrogen and progesterone on changes in emotional eating across the menstrual cycle. J Abnorm Psychol 2013, 122, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Hirschberg, A.L. Sex hormones, appetite and eating behaviour in women. Maturitas 2012, 71, 248–256. [Google Scholar] [CrossRef]
- Bijlenga, D.; Tjon-Ka-Jie, J.Y.M.; Schuijers, F.; Kooij, J.J.S. Atypical sensory profiles as core features of adult ADHD, irrespective of autistic symptoms. Eur Psychiatry 2017, 43, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Martin, E.; Dourish, C.T.; Higgs, S. Interoceptive accuracy mediates the longitudinal relationship between attention deficit hyperactivity disorder (ADHD) inattentive symptoms and disordered eating in a community sample. Physiol Behav 2023, 268, 114220. [Google Scholar] [CrossRef] [PubMed]
- Kutscheidt, K.; Dresler, T.; Hudak, J.; Barth, B.; Blume, F.; Ethofer, T.; Fallgatter, A.J.; Ehlis, A.C. Interoceptive awareness in patients with attention-deficit/hyperactivity disorder (ADHD). Atten Defic Hyperact Disord 2019, 11, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Kok, F.M.; Groen, Y.; Fuermaier, A.B.M.; Tucha, O. Problematic Peer Functioning in Girls with ADHD: A Systematic Literature Review. PLOS ONE 2016, 11, e0165119. [Google Scholar] [CrossRef] [PubMed]
- Van Veen, M.M.; Kooij, J.S.; Boonstra, A.M.; Gordijn, M.C.; Van Someren, E.J. Delayed circadian rhythm in adults with attention-deficit/hyperactivity disorder and chronic sleep-onset insomnia. Biological psychiatry 2010, 67, 1091–1096. [Google Scholar] [CrossRef]
- Snitselaar, M.A.; Smits, M.G.; van der Heijden, K.B.; Spijker, J. Sleep and Circadian Rhythmicity in Adult ADHD and the Effect of Stimulants. J Atten Disord 2017, 21, 14–26. [Google Scholar] [CrossRef]
- Baker, F.C.; Lee, K.A. Menstrual Cycle Effects on Sleep. Sleep Med Clin 2022, 17, 283–294. [Google Scholar] [CrossRef]
- Aspesi, D.; Bass, N.; Kavaliers, M.; Choleris, E. The Role of Androgens and Estrogens in Social Interactions and Social Cognition. Neuroscience 2023. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.C.; Peisen, F.; Kogler, L.; Radke, S.; Turetsky, B.; Freiherr, J.; Derntl, B. The Influence of Menstrual Cycle and Androstadienone on Female Stress Reactions: An fMRI Study. Front Hum Neurosci 2016, 10, 44. [Google Scholar] [CrossRef] [PubMed]
- Skoglund, C.; Sundström Poromaa, I.; Leksell, D.; Ekholm Selling, K.; Cars, T.; Giacobini, M.; Young, S.; Kopp Kallner, H. Time after time: failure to identify and support females with ADHD – a Swedish population register study. Journal of Child Psychology and Psychiatry n/a. [CrossRef]
- Fedele, D.A.; Lefler, E.K.; Hartung, C.M.; Canu, W.H. Sex differences in the manifestation of ADHD in emerging adults. J Atten Disord 2012, 16, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Littman, E.; Dean, J.M.; Wagenberg, B.; Wasserstein, J. ADHD in Females Across the Lifespan and the Role of Estrogen. The ADHD Report 2021, 29, 1–8. [Google Scholar] [CrossRef]
- Deecher, D.; Andree, T.H.; Sloan, D.; Schechter, L.E. From menarche to menopause: exploring the underlying biology of depression in women experiencing hormonal changes. Psychoneuroendocrinology 2008, 33, 3–17. [Google Scholar] [CrossRef]
- Epperson, C.N.; Steiner, M.; Hartlage, S.A.; Eriksson, E.; Schmidt, P.J.; Jones, I.; Yonkers, K.A. Premenstrual dysphoric disorder: evidence for a new category for DSM-5. Am J Psychiatry 2012, 169, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Shanmugan, S.; Loughead, J.; Nanga, R.P.; Elliott, M.; Hariharan, H.; Appleby, D.; Kim, D.; Ruparel, K.; Reddy, R.; Brown, T.E.; et al. Lisdexamfetamine Effects on Executive Activation and Neurochemistry in Menopausal Women with Executive Function Difficulties. Neuropsychopharmacology 2017, 42, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Jeanette Wasserstein; Mary Solanto; Gerry A Stefanatos; D.Phil. ADHD During Perimenopause and Menopause. In Proceedings of the APSARD, Orlando, Florida, 12-15 January, 2023.
- Terner, J.M.; de Wit, H. Menstrual cycle phase and responses to drugs of abuse in humans. Drug Alcohol Depend 2006, 84, 1–13. [Google Scholar] [CrossRef]
- Justice, A.J.; de Wit, H. Acute effects of d-amphetamine during the follicular and luteal phases of the menstrual cycle in women. Psychopharmacology (Berl) 1999, 145, 67–75. [Google Scholar] [CrossRef]
- White, T.L.; Justice, A.J.; de Wit, H. Differential subjective effects of D-amphetamine by gender, hormone levels and menstrual cycle phase. Pharmacol Biochem Behav 2002, 73, 729–741. [Google Scholar] [CrossRef]
- Barkley, R. Why Emotional Impulsiveness Should Be a Central Feature of ADHD. Adhd Report, The 2010, 18, 1–5. [Google Scholar] [CrossRef]
- Kofler, M.J.; Rapport, M.D.; Sarver, D.E.; Raiker, J.S.; Orban, S.A.; Friedman, L.M.; Kolomeyer, E.G. Reaction time variability in ADHD: a meta-analytic review of 319 studies. Clin Psychol Rev 2013, 33, 795–811. [Google Scholar] [CrossRef] [PubMed]
- LaCount, P.A.; Hartung, C.M.; Shelton, C.R.; Stevens, A.E. Efficacy of an Organizational Skills Intervention for College Students With ADHD Symptomatology and Academic Difficulties. J Atten Disord 2018, 22, 356–367. [Google Scholar] [CrossRef] [PubMed]
- Knouse, L.E.; Cooper-Vince, C.; Sprich, S.; Safren, S.A. Recent developments in the psychosocial treatment of adult ADHD. Expert Rev Neurother 2008, 8, 1537–1548. [Google Scholar] [CrossRef] [PubMed]
- Weissenberger, S.; Děchtěrenko, F.; Klicperova-Baker, M.; Vňuková, M.; Zimbardo, P.; Raboch, J.; Anders, M.; Braaten, E.; Ptáček, R. ADHD Symptoms in Adults and Time Perspectives - Findings From a Czech National Sample. Front Psychol 2020, 11, 950. [Google Scholar] [CrossRef] [PubMed]
- Weissenberger, S.; Schonova, K.; Büttiker, P.; Fazio, R.; Vnukova, M.; Stefano, G.B.; Ptacek, R. Time Perception is a Focal Symptom of Attention-Deficit/Hyperactivity Disorder in Adults. Med Sci Monit 2021, 27, e933766. [Google Scholar] [CrossRef] [PubMed]
- Olson, M.M.; Alhelou, N.; Kavattur, P.S.; Rountree, L.; Winkler, I.T. The persistent power of stigma: A critical review of policy initiatives to break the menstrual silence and advance menstrual literacy. PLOS Glob Public Health 2022, 2, e0000070. [Google Scholar] [CrossRef] [PubMed]
- Stenner, P.; O'Dell, L.; Davies, A. Adult women and ADHD: On the temporal dimensions of ADHD identities. Journal for the Theory of Social Behaviour 2019, 49, 179–197. [Google Scholar] [CrossRef]
- Able, S.L.; Haynes, V.; Hong, J. Diagnosis, treatment, and burden of illness among adults with attention-deficit/hyperactivity disorder in Europe. Pragmat Obs Res 2014, 5, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Miklósi, M.; Máté, O.; Somogyi, K.; Szabó, M. Adult Attention Deficit Hyperactivity Disorder Symptoms, Perceived Stress, and Well-Being: The Role of Early Maladaptive Schemata. J Nerv Ment Dis 2016, 204, 364–369. [Google Scholar] [CrossRef]
- Hargitai, L.D.; Livingston, L.A.; Waldren, L.H.; Robinson, R.; Jarrold, C.; Shah, P. Attention-deficit hyperactivity disorder traits are a more important predictor of internalising problems than autistic traits. Scientific Reports 2023, 13, 31. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry 1982, 4, 33–47. [Google Scholar] [CrossRef]
- Saccaro, L.F.; Schilliger, Z.; Perroud, N.; Piguet, C. Inflammation, Anxiety, and Stress in Attention-Deficit/Hyperactivity Disorder. Biomedicines 2021, 9. [Google Scholar] [CrossRef] [PubMed]
- Schnorr, I.; Siegl, A.; Luckhardt, S.; Wenz, S.; Friedrichsen, H.; El Jomaa, H.; Steinmann, A.; Kilencz, T.; Arteaga-Henríquez, G.; Ramos-Sayalero, C.; et al. Inflammatory biotype of ADHD is linked to chronic stress: a data-driven analysis of the inflammatory proteome. Transl Psychiatry 2024, 14, 37. [Google Scholar] [CrossRef]
- Brewerton, T.D.; Duncan, A.E. Associations between Attention Deficit Hyperactivity Disorder and Eating Disorders by Gender: Results from the National Comorbidity Survey Replication. Eur Eat Disord Rev 2016, 24, 536–540. [Google Scholar] [CrossRef]
- Klump, K.L.; Keel, P.K.; Culbert, K.M.; Edler, C. Ovarian hormones and binge eating: exploring associations in community samples. Psychol Med 2008, 38, 1749–1757. [Google Scholar] [CrossRef]
- Lester, N.A.; Keel, P.K.; Lipson, S.F. Symptom fluctuation in bulimia nervosa: relation to menstrual-cycle phase and cortisol levels. Psychol Med 2003, 33, 51–60. [Google Scholar] [CrossRef]
- Steward, R.; Crane, L.; Mairi Roy, E.; Remington, A.; Pellicano, E. "Life is Much More Difficult to Manage During Periods": Autistic Experiences of Menstruation. J Autism Dev Disord 2018, 48, 4287–4292. [Google Scholar] [CrossRef]
- Ray, P.; Mandal, N.; Sinha, V.K. Change of symptoms of schizophrenia across phases of menstrual cycle. Arch Womens Ment Health 2020, 23, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Teatero, M.L.; Mazmanian, D.; Sharma, V. Effects of the menstrual cycle on bipolar disorder. Bipolar Disord 2014, 16, 22–36. [Google Scholar] [CrossRef] [PubMed]

| Mean (range) | |
| Age* | 37,8 year (29-46 years) |
| Time since ADHD diagnosis | 32 months (4 months - 10years) |
| Time since treatment start** | 10 months (2 - 22 months) |
| n⁰ (total=6) | |
| Use of ADHD-medication at start* | 4 |
| Stable medication* | 2 |
| Use of ADHD-medication at end*** | 5 |
| Stable medication*** | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





