Submitted:
21 March 2024
Posted:
22 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
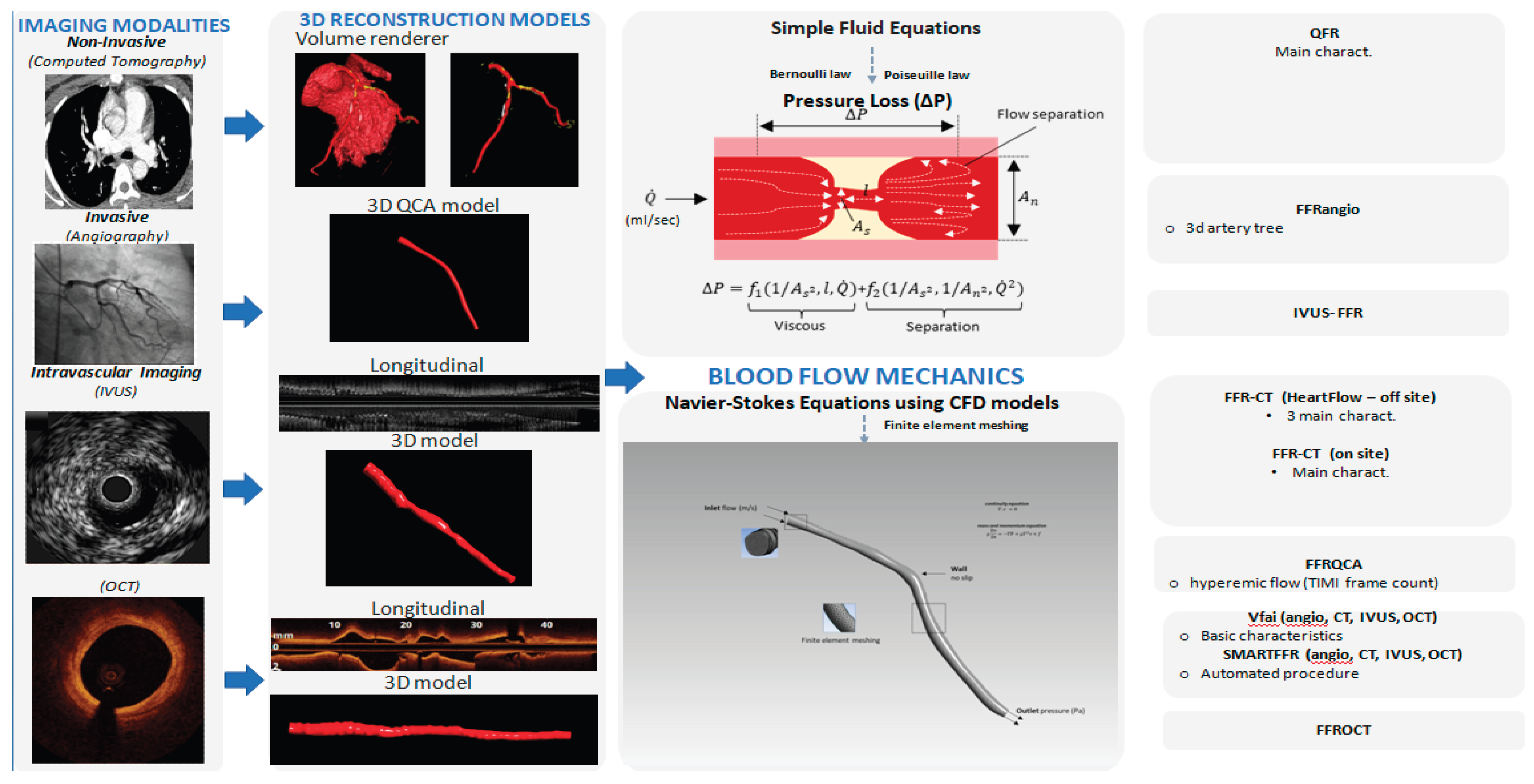
2. Fluid Mechanics and Computational Fluid Dynamics
3. Virtual FFR Based on Non-Invasive Imaging
3.1. FFRCT® by HeartFlow: Offsite Computations
3.2. FFRCT by Other Groups: Onsite Studies
3.3. FFR-CT and Impact on the Decision Making Process
4. Virtual FFR Based on Invasive Imaging
4.1. Invasive Angiography Derived Virtual FFR
4.1.1. Early Pioneer Studies
4.1.2. Large Clinical Studies (QFR, FFRangio)
4.1.3. Outcome-Based Studies
4.1.4. Discrepancy Versus FFR
4.2. Virtual FFR Based on Intravascular Imaging
5. Functional Angiography and Coronary Imaging: Future Perspectives
6. Conclusions
Funding
Conflicts of Interest
References
- Mangla A, Oliveros E, Williams KA, Sr., Kalra DK. Cardiac Imaging in the Diagnosis of Coronary Artery Disease. Current Problems in Cardiology 2017, 42, 316–366. [Google Scholar] [CrossRef] [PubMed]
- McCullough, P.A. Coronary artery disease. Clin J Am Soc Nephrol. 2007, 2, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef] [PubMed]
- Zhang R, Dou K, Guan C, Zou T, Zhang M, Yuan S; et al. Outcomes of quantitative flow ratio-based percutaneous coronary intervention in an all-comers study. EuroIntervention 2022, 17, 1240–1251. [Google Scholar] [CrossRef] [PubMed]
- Schampaert E, Kumar G, Achenbach S, Galli S, Tanaka N, Teraphongphom T; et al. A global registry of fractional flow reserve (FFR)-guided management during routine care: Study design, baseline characteristics and outcomes of invasive management. Catheter Cardiovasc Interv. 2020, 96, E423–E431. [Google Scholar]
- Parikh RV, Liu G, Plomondon ME, Sehested TSG, Hlatky MA, Waldo SW; et al. Utilization and Outcomes of Measuring Fractional Flow Reserve in Patients With Stable Ischemic Heart Disease. J Am Coll Cardiol. 2020, 75, 521. [Google Scholar]
- Fearon WF, Bornschein B, Tonino PA, Gothe RM, Bruyne BD, Pijls NH; et al. Economic evaluation of fractional flow reserve-guided percutaneous coronary intervention in patients with multivessel disease. Circulation 2010, 122, 2545–2550. [Google Scholar] [CrossRef]
- Carvalho V, Pinho D, Lima RA, Teixeira JC, Teixeira SJF. Blood Flow Modeling in Coronary Arteries: A Review. Fluids 2021, 6, 53. [Google Scholar] [CrossRef]
- Kannojiya V, Das AK, Das PK. Simulation of Blood as Fluid: A Review From Rheological Aspects. IEEE Rev Biomed Eng. 2021, 14, 327–341. [Google Scholar] [CrossRef]
- Papafaklis MI, Mavrogiannis MC, Siogkas PK, Lakkas LS, Katsouras CS, Fotiadis DI; et al. Functional assessment of lesion severity without using the pressure wire: Coronary imaging and blood flow simulation. Expert Review of Cardiovascular Therapy 2017, 15, 863–877. [Google Scholar] [CrossRef]
- Vardhan M, Randles AJBR. Application of physics-based flow models in cardiovascular medicine: Current practices and challenges. Biophysics Reviews 2021, 2, 011302. [Google Scholar]
- Zhong L, Zhang JM, Su B, Tan RS, Allen JC, Kassab GS. Application of Patient-Specific Computational Fluid Dynamics in Coronary and Intra-Cardiac Flow Simulations: Challenges and Opportunities. Front Physiol. 2018, 9, 742. [Google Scholar] [CrossRef]
- Kim HJ, Vignon-Clementel IE, Coogan JS, Figueroa CA, Jansen KE, Taylor CA. Patient-specific modeling of blood flow and pressure in human coronary arteries. Ann Biomed Eng. 2010, 38, 3195–3209. [Google Scholar] [CrossRef] [PubMed]
- Chinnaiyan KM, Safian RD, Gallagher ML, George J, Dixon SR, Bilolikar AN; et al. Clinical Use of CT-Derived Fractional Flow Reserve in the Emergency Department. JACC: Cardiovascular Imaging 2020, 13, 452–461. [Google Scholar]
- Koo BK, Erglis A, Doh JH, Daniels DV, Jegere S, Kim HS; et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol. 2011, 58, 1989–1997. [Google Scholar]
- Nakazato R, Park HB, Berman DS, Gransar H, Koo BK, Erglis A; et al. Noninvasive fractional flow reserve derived from computed tomography angiography for coronary lesions of intermediate stenosis severity: Results from the DeFACTO study. Circulation: Cardiovascular Imaging 2013, 6, 881–889. [Google Scholar]
- Gaur S, Achenbach S, Leipsic J, Mauri L, Bezerra HG, Jensen JM; et al. Rationale and design of the HeartFlowNXT (HeartFlow analysis of coronary blood flow using CT angiography: NeXt sTeps) study. J Cardiovasc Comput Tomogr. 2013, 7, 279–288. [Google Scholar] [CrossRef]
- Nørgaard BL, Leipsic J, Gaur S, Seneviratne S, Ko BS, Ito H; et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: The NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). Journal of the American College of Cardiology 2014, 63, 1145–1155. [Google Scholar] [CrossRef]
- Zhuang B, Wang S, Zhao S, Lu M. Computed tomography angiography-derived fractional flow reserve (CT-FFR) for the detection of myocardial ischemia with invasive fractional flow reserve as reference: Systematic review and meta-analysis. European Radiology 2020, 30, 712–725. [Google Scholar] [CrossRef]
- Hecht HS, Narula J, Fearon WF. Fractional Flow Reserve and Coronary Computed Tomographic Angiography: A Review and Critical Analysis. Circulation Research 2016, 119, 300–316. [Google Scholar] [CrossRef]
- Siogkas PK, Anagnostopoulos CD, Liga R, Exarchos TP, Sakellarios AI, Rigas G; et al. Noninvasive CT-based hemodynamic assessment of coronary lesions derived from fast computational analysis: A comparison against fractional flow reserve. European Radiology 2019, 29, 2117–2126. [Google Scholar] [CrossRef]
- Renker M, Schoepf UJ, Wang R, Meinel FG, Rier JD, Bayer RR, 2nd; et al. Comparison of diagnostic value of a novel noninvasive coronary computed tomography angiography method versus standard coronary angiography for assessing fractional flow reserve. Am J Cardiol. 2014, 114, 1303–1308. [Google Scholar] [CrossRef]
- Kruk M, Wardziak Ł, Demkow M, Pleban W, Pręgowski J, Dzielińska Z; et al. Workstation-Based Calculation of CTA-Based FFR for Intermediate Stenosis. JACC: Cardiovascular Imaging 2016, 9, 690–699. [Google Scholar]
- Ko BS, Cameron JD, Munnur RK, Wong DTL, Fujisawa Y, Sakaguchi T; et al. Noninvasive CT-Derived FFR Based on Structural and Fluid Analysis: A Comparison With Invasive FFR for Detection of Functionally Significant Stenosis. JACC: Cardiovascular Imaging 2017, 10, 663–673. [Google Scholar]
- Donnelly PM, Kolossváry M, Karády J, Ball PA, Kelly S, Fitzsimons D; et al. Experience with an On-Site Coronary Computed Tomography-Derived Fractional Flow Reserve Algorithm for the Assessment of Intermediate Coronary Stenoses. American Journal of Cardiology 2018, 121, 9–13. [Google Scholar] [CrossRef]
- Röther J, Moshage M, Dey D, Schwemmer C, Tröbs M, Blachutzik F; et al. Comparison of invasively measured FFR with FFR derived from coronary CT angiography for detection of lesion-specific ischemia: Results from a PC-based prototype algorithm. Journal of Cardiovascular Computed Tomography 2018, 12, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Wardziak Ł, Kruk M, Pleban W, Demkow M, Rużyłło W, Dzielińska Z; et al. Coronary CTA enhanced with CTA based FFR analysis provides higher diagnostic value than invasive coronary angiography in patients with intermediate coronary stenosis. Journal of Cardiovascular Computed Tomography 2019, 13, 62–67. [Google Scholar] [CrossRef]
- Siogkas PK, Papafaklis MI, Lakkas L, Exarchos TP, Karmpaliotis D, Ali ZA; et al. Virtual Functional Assessment of Coronary Stenoses Using Intravascular Ultrasound Imaging: A Proof-of-Concept Pilot Study. Heart, Lung & Circulation 2019, 28, e33–e36. [Google Scholar]
- Siogkas PK, Lakkas L, Sakellarios AI, Rigas G, Kyriakidis S, Stefanou KA; et al. SmartFFR, a New Functional Index of Coronary Stenosis: Comparison with Invasive FFR Data. Frontiers in Cardiovascular Medicine 2021, 8, 714471. [Google Scholar] [CrossRef] [PubMed]
- Sakellarios AI, Rigas G, Kigka V, Siogkas P, Tsompou P, Karanasiou G; et al. SMARTool: A tool for clinical decision support for the management of patients with coronary artery disease based on modeling of atherosclerotic plaque process. Annu Int Conf IEEE Eng Med Biol Soc. 2017, 2017, 96–99. [Google Scholar]
- Sakellarios A, Correia J, Kyriakidis S, Georga E, Tachos N, Siogkas P; et al. A cloud-based platform for the non-invasive management of coronary artery disease. Enterprise Information Systems 2020, 14, 1102–1123. [Google Scholar] [CrossRef]
- Driessen RS, Danad I, Stuijfzand WJ, Raijmakers PG, Schumacher SP, van Diemen PA; et al. Comparison of Coronary Computed Tomography Angiography, Fractional Flow Reserve, and Perfusion Imaging for Ischemia Diagnosis. Journal of the American College of Cardiology 2019, 73, 161–173. [Google Scholar] [CrossRef]
- Anagnostopoulos CD, Siogkas PK, Liga R, Benetos G, Maaniitty T, Sakellarios AI; et al. Characterization of functionally significant coronary artery disease by a coronary computed tomography angiography-based index: A comparison with positron emission tomography. European Heart Journal Cardiovascular Imaging 2019, 20, 897–905. [Google Scholar] [CrossRef] [PubMed]
- Pontone G, Rabbat MG. The New Era of Computational Fluid Dynamics in CT Angiography: Far Beyond the FFR Number. JACC: Cardiovascular Imaging 2017, 10, 674–676. [Google Scholar]
- Lu MT, Ferencik M, Roberts RS, Lee KL, Ivanov A, Adami E; et al. Noninvasive FFR Derived From Coronary CT Angiography: Management and Outcomes in the PROMISE Trial. JACC Cardiovasc Imaging 2017, 10, 1350–1358. [Google Scholar] [CrossRef]
- CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): An open-label, parallel-group, multicentre trial. Lancet 2015, 385, 2383–2391. [CrossRef]
- Adamson PD, Newby DE, Hill CL, Coles A, Douglas PS, Fordyce CB. Comparison of International Guidelines for Assessment of Suspected Stable Angina: Insights From the PROMISE and SCOT-HEART. JACC: Cardiovascular Imaging 2018, 11, 1301–1310. [Google Scholar]
- Curzen NP, Nolan J, Zaman AG, Nørgaard BL, Rajani R. Does the Routine Availability of CT-Derived FFR Influence Management of Patients With Stable Chest Pain Compared to CT Angiography Alone?: The FFR(CT) RIPCORD Study. JACC Cardiovasc Imaging 2016, 9, 1188–1194. [Google Scholar] [CrossRef]
- Morris PD, Ryan D, Morton AC, Lycett R, Lawford PV, Hose DR; et al. Virtual fractional flow reserve from coronary angiography: Modeling the significance of coronary lesions: Results from the VIRTU-1 (VIRTUal Fractional Flow Reserve From Coronary Angiography) study. JACC: Cardiovascular Interventions 2013, 6, 149–157. [Google Scholar]
- Tu S, Barbato E, Köszegi Z, Yang J, Sun Z, Holm NR; et al. Fractional flow reserve calculation from 3-dimensional quantitative coronary angiography and TIMI frame count: A fast computer model to quantify the functional significance of moderately obstructed coronary arteries. JACC: Cardiovascular Interventions 2014, 7, 768–777. [Google Scholar]
- Papafaklis MI, Muramatsu T, Ishibashi Y, Lakkas LS, Nakatani S, Bourantas CV; et al. Fast virtual functional assessment of intermediate coronary lesions using routine angiographic data and blood flow simulation in humans: Comparison with pressure wire—Fractional flow reserve. EuroIntervention 2014, 10, 574–583. [Google Scholar] [CrossRef]
- Tu S, Westra J, Yang J, von Birgelen C, Ferrara A, Pellicano M; et al. Diagnostic Accuracy of Fast Computational Approaches to Derive Fractional Flow Reserve From Diagnostic Coronary Angiography: The International Multicenter FAVOR Pilot Study. JACC: Cardiovascular Interventions 2016, 9, 2024–2035. [Google Scholar]
- Xu B, Tu S, Qiao S, Qu X, Chen Y, Yang J; et al. Diagnostic Accuracy of Angiography-Based Quantitative Flow Ratio Measurements for Online Assessment of Coronary Stenosis. Journal of the American College of Cardiology 2017, 70, 3077–3087. [Google Scholar] [CrossRef] [PubMed]
- Westra J, Tu S, Winther S, Nissen L, Vestergaard MB, Andersen BK; et al. Evaluation of Coronary Artery Stenosis by Quantitative Flow Ratio During Invasive Coronary Angiography: The WIFI II Study (Wire-Free Functional Imaging II). Circulation: Cardiovascular Imaging 2018, 11, e007107. [Google Scholar]
- Yazaki K, Otsuka M, Kataoka S, Kahata M, Kumagai A, Inoue K; et al. Applicability of 3-Dimensional Quantitative Coronary Angiography-Derived Computed Fractional Flow Reserve for Intermediate Coronary Stenosis. Circulation Journal 2017, 81, 988–992. [Google Scholar] [CrossRef]
- Siogkas PK, Stefanou KA, Athanasiou LS, Papafaklis MI, Michalis LK, Fotiadis DI. Art care: A multi-modality coronary 3D reconstruction and hemodynamic status assessment software. Technology and Health Care 2018, 26, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Fearon WF, Achenbach S, Engstrom T, Assali A, Shlofmitz R, Jeremias A; et al. Accuracy of Fractional Flow Reserve Derived From Coronary Angiography. Circulation 2019, 139, 477–484. [Google Scholar] [CrossRef]
- Witberg G, De Bruyne B, Fearon WF, Achenbach S, Engstrom T, Matsuo H; et al. Diagnostic Performance of Angiogram-Derived Fractional Flow Reserve: A Pooled Analysis of 5 Prospective Cohort Studies. JACC: Cardiovascular Interventions 2020, 13, 488–497. [Google Scholar]
- Song L, Tu S, Sun Z, Wang Y, Ding D, Guan C; et al. Quantitative flow ratio-guided strategy versus angiography-guided strategy for percutaneous coronary intervention: Rationale and design of the FAVOR III China trial. Am Heart J. 2020, 223, 72–80. [Google Scholar] [CrossRef]
- Seike F, Uetani T, Nishimura K, Kawakami H, Higashi H, Fujii A; et al. Intravascular Ultrasound-Derived Virtual Fractional Flow Reserve for the Assessment of Myocardial Ischemia. Circ J. 2018, 82, 815–823. [Google Scholar] [CrossRef]
- Karanasiou GS, Rigas GA, Kyriakidis SK, Tachos NS, Sakellarios AI, Fotiadis DI. InSilc: 3D Reconstruction and plaque characterization tool. Annu Int Conf IEEE Eng Med Biol Soc. 2018, 2018, 4528–4531. [Google Scholar]
- Zafar H, Sharif F, Leahy MJ. Feasibility of intracoronary frequency domain optical coherence tomography derived fractional flow reserve for the assessment of coronary artery stenosis. Int Heart J. 2014, 55, 307–311. [Google Scholar] [CrossRef]
- Ha J, Kim JS, Lim J, Kim G, Lee S, Lee JS; et al. Assessing Computational Fractional Flow Reserve From Optical Coherence Tomography in Patients with Intermediate Coronary Stenosis in the Left Anterior Descending Artery. Circ Cardiovasc Interv. 2016, 9. [Google Scholar]
- Yu W, Huang J, Jia D, Chen S, Raffel OC, Ding D; et al. Diagnostic accuracy of intracoronary optical coherence tomography-derived fractional flow reserve for assessment of coronary stenosis severity. EuroIntervention 2019, 15, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Poon EKW, Thondapu V, Revalor E, Ooi A, Barlis P. Coronary optical coherence tomography-derived virtual fractional flow reserve (FFR): Anatomy and physiology all-in-one. Eur Heart J. 2017, 38, 3604–3605. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).




