Submitted:
22 March 2024
Posted:
25 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
Definitions
Search Strategy
Selection Criteria
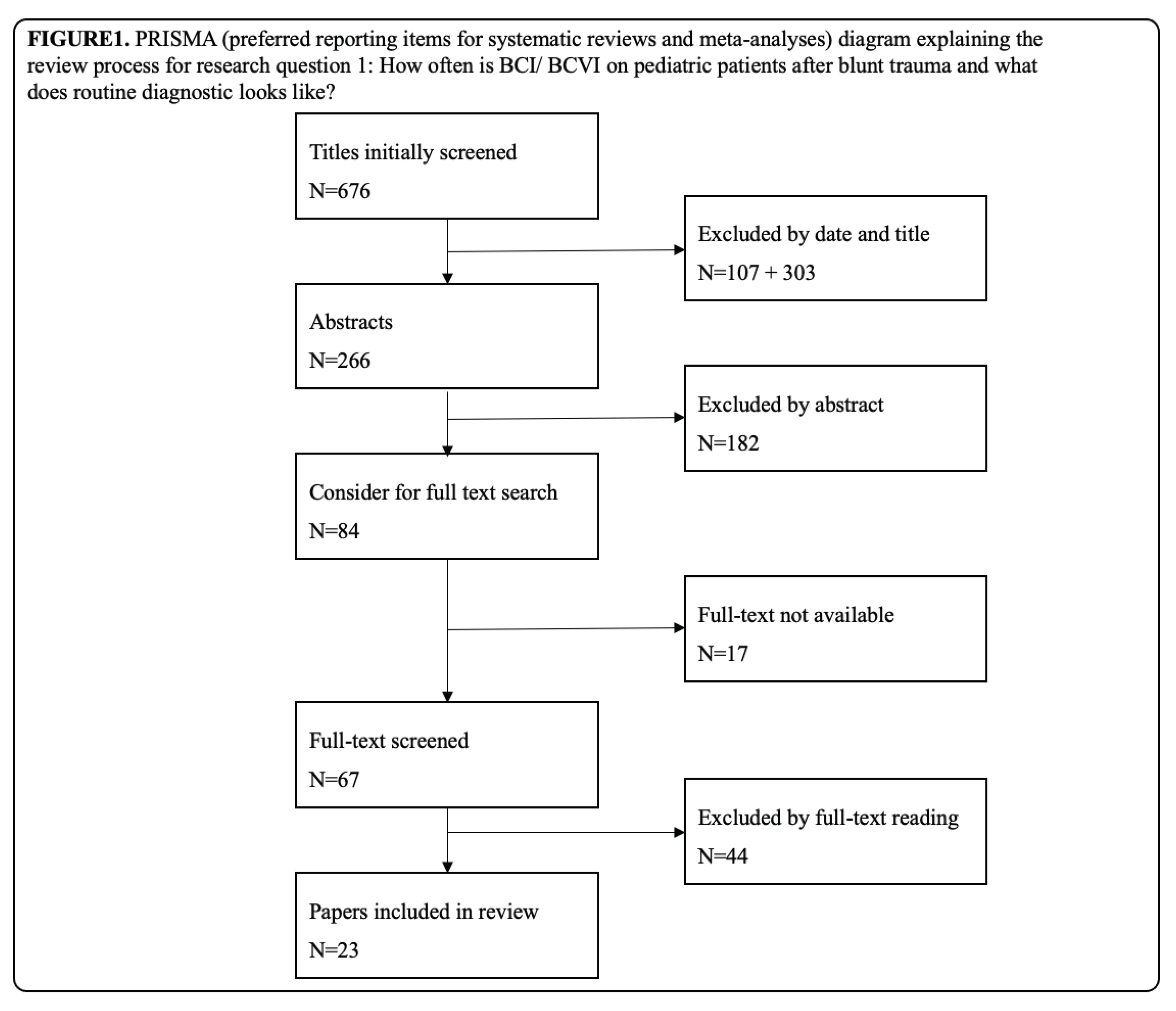
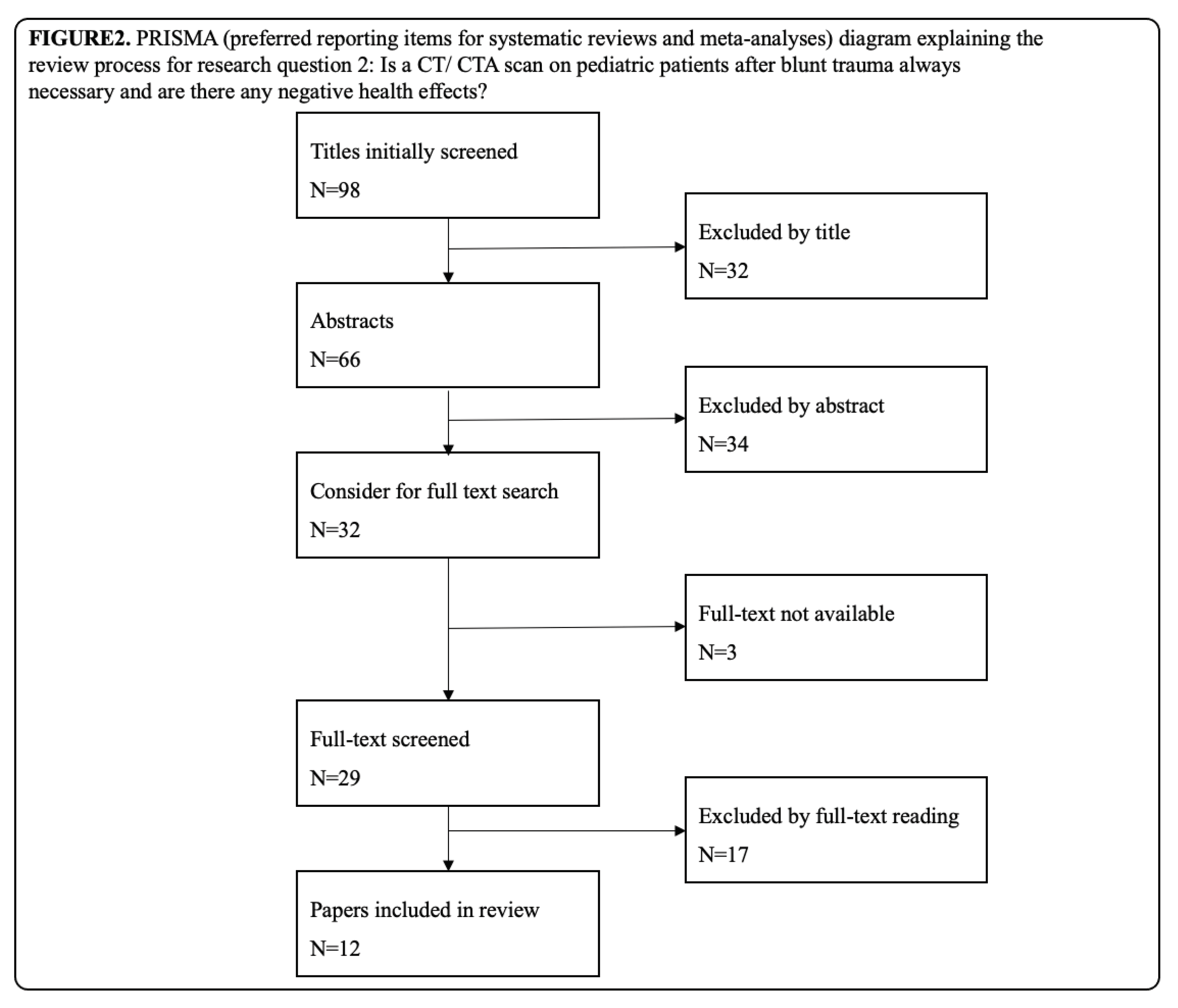
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lew, S. M.; Frumiento, C.; Wald, S. L. Pediatric blunt carotid injury: a review of the National Pediatric Trauma Registry. Pediatr Neurosurg 1999, 30, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Weber, C. D.; Lefering, R.; Weber, M. S.; Bier, G.; Knobe, M.; Pishnamaz, M.; Kobbe, P.; Hildebrand, F. Predictors for Pediatric Blunt Cerebrovascular Injury (BCVI): An International Multicenter Analysis. World J Surg 2019, 43, 2337–2347. [Google Scholar] [CrossRef] [PubMed]
- Azarakhsh, N.; Grimes, S.; Notrica, D. M.; Raines, A.; Garcia, N. M.; Tuggle, D. W.; Maxson, R. T.; Alder, A. C.; Recicar, J.; Garcia-Filion, P.; et al. Blunt cerebrovascular injury in children: underreported or underrecognized?: A multicenter ATOMAC study. J Trauma Acute Care Surg 2013, 75, 1006–1011; [Google Scholar] [CrossRef]
- Herbert, J. P.; Venkataraman, S. S.; Turkmani, A. H.; Zhu, L.; Kerr, M. L.; Patel, R. P.; Ugalde, I. T.; Fletcher, S. A.; Sandberg, D. I.; Cox, C. S.; et al. Pediatric blunt cerebrovascular injury: the McGovern screening score. J Neurosurg Pediatr 2018, 21, 639–649. [Google Scholar] [CrossRef] [PubMed]
- Cuff, R. F.; Thomas, J. H. Pediatric blunt carotid injury from low-impact trauma: a case report and review of the literature. J Trauma 2005, 58, 620–623. [Google Scholar] [CrossRef] [PubMed]
- Singh, R. R.; Barry, M. C.; Ireland, A.; Bouchier Hayes, D. Current diagnosis and management of blunt internal carotid artery injury. Eur J Vasc Endovasc Surg 2004, 27, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Brenner, D. J.; Hall, E. J. Computed tomography--an increasing source of radiation exposure. N Engl J Med 2007, 357, 2277–2284. [Google Scholar] [CrossRef] [PubMed]
- Kleinerman, R. A. Cancer risks following diagnostic and therapeutic radiation exposure in children. Pediatr Radiol 2006, 36 (Suppl 2), 121–125. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; D’Ayala, M.; Hirshberg, A.; Briggs, W.; Wise, L.; Tortolani, A. Comparison of conservative and operative treatment for blunt carotid injuries: analysis of the National Trauma Data Bank. J Vasc Surg 2010, 51, 593-599, 599.e591-592. [Google Scholar] [CrossRef]
- Jones, T. S.; Burlew, C. C.; Kornblith, L. Z.; Biffl, W. L.; Partrick, D. A.; Johnson, J. L.; Barnett, C. C.; Bensard, D. D.; Moore, E. E. Blunt cerebrovascular injuries in the child. Am J Surg 2012, 204, 7–10. [Google Scholar] [CrossRef]
- Kraus, R. R.; Bergstein, J. M.; DeBord, J. R. Diagnosis, treatment, and outcome of blunt carotid arterial injuries. Am J Surg 1999, 178, 190–193. [Google Scholar] [CrossRef] [PubMed]
- Wei, C. W.; Montanera, W.; Selchen, D.; Lian, J.; Stevens, C.; de Tilly, L. N. Blunt cerebrovascular injuries: diagnosis and management outcomes. Can J Neurol Sci 2010, 37, 574–579. [Google Scholar] [CrossRef] [PubMed]
- Savoie, K. B.; Shi, J.; Wheeler, K.; Xiang, H.; Kenney, B. D. Pediatric blunt cerebrovascular injuries: A national trauma database study. J Pediatr Surg 2020, 55, 917–920. [Google Scholar] [CrossRef] [PubMed]
- Acker, S. N.; Kulungowski, A. M. Error traps and culture of safety in pediatric trauma. Semin Pediatr Surg 2019, 28, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Kerwin, A. J.; Bynoe, R. P.; Murray, J.; Hudson, E. R.; Close, T. P.; Gifford, R. R.; Carson, K. W.; Smith, L. P.; Bell, R. M. Liberalized screening for blunt carotid and vertebral artery injuries is justified. J Trauma 2001, 51, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Ugalde, I. T.; Claiborne, M. K.; Cardenas-Turanzas, M.; Shah, M. N.; Langabeer, J. R., 2nd; Patel, R. Risk Factors in Pediatric Blunt Cervical Vascular Injury and Significance of Seatbelt Sign. West J Emerg Med 2018, 19, 961–969. [Google Scholar] [CrossRef] [PubMed]
- Biffl, W. L.; Ray, C. E., Jr.; Moore, E. E.; Franciose, R. J.; Aly, S.; Heyrosa, M. G.; Johnson, J. L.; Burch, J. M. Treatment-related outcomes from blunt cerebrovascular injuries: importance of routine follow-up arteriography. Ann Surg 2002, 235, 699–706; [Google Scholar] [CrossRef]
- Ciapetti, M.; Circelli, A.; Zagli, G.; Migliaccio, M. L.; Spina, R.; Alessi, A.; Acquafresca, M.; Bartolini, M.; Peris, A. Diagnosis of carotid arterial injury in major trauma using a modification of Memphis criteria. Scand J Trauma Resusc Emerg Med 2010, 18, 61. [Google Scholar] [CrossRef]
- Cothren, C. C.; Moore, E. E. Blunt cerebrovascular injuries. Clinics (Sao Paulo) 2005, 60, 489–496. [Google Scholar] [CrossRef]
- Bromberg, W. J.; Collier, B. C.; Diebel, L. N.; Dwyer, K. M.; Holevar, M. R.; Jacobs, D. G.; Kurek, S. J.; Schreiber, M. A.; Shapiro, M. L.; Vogel, T. R. Blunt cerebrovascular injury practice management guidelines: the Eastern Association for the Surgery of Trauma. J Trauma 2010, 68, 471–477. [Google Scholar] [CrossRef]
- Ravindra, V. M.; Bollo, R. J.; Sivakumar, W.; Akbari, H.; Naftel, R. P.; Limbrick, D. D., Jr.; Jea, A.; Gannon, S.; Shannon, C.; Birkas, Y.; et al. Predicting Blunt Cerebrovascular Injury in Pediatric Trauma: Validation of the “Utah Score”. J Neurotrauma 2017, 34, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Leraas, H. J.; Kuchibhatla, M.; Nag, U. P.; Kim, J.; Ezekian, B.; Reed, C. R.; Rice, H. E.; Tracy, E. T.; Adibe, O. O. Cervical seatbelt sign is not associated with blunt cerebrovascular injury in children: A review of the national trauma databank. Am J Surg 2019, 218, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Grigorian, A.; Dolich, M.; Lekawa, M.; Fujitani, R. M.; Kabutey, N. K.; Kuza, C. M.; Bashir, R.; Nahmias, J. Analysis of blunt cerebrovascular injury in pediatric trauma. J Trauma Acute Care Surg 2019, 87, 1354–1359. [Google Scholar] [CrossRef]
- McGrew, P. R.; Chestovich, P. J.; Fisher, J. D.; Kuhls, D. A.; Fraser, D. R.; Patel, P. P.; Katona, C. W.; Saquib, S.; Fildes, J. J. Implementation of a CT scan practice guideline for pediatric trauma patients reduces unnecessary scans without impacting outcomes. J Trauma Acute Care Surg 2018, 85, 451–458. [Google Scholar] [CrossRef] [PubMed]
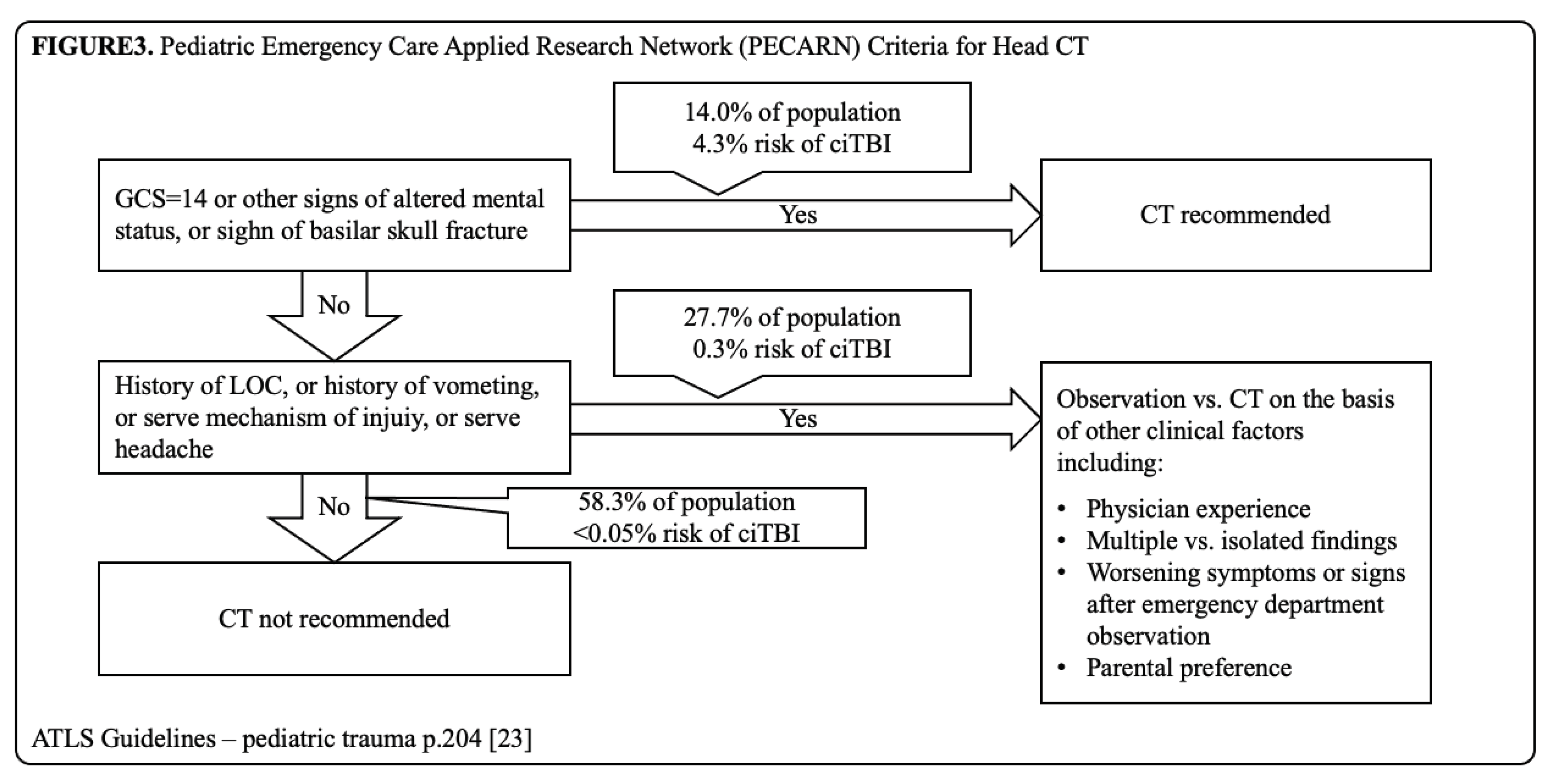
- Ronald, M. Stewart, M. F. R., Sharon M. Henry, Monique Drago, Advanced Trauma Life Support - Student Course Manual, 2018. [Google Scholar]
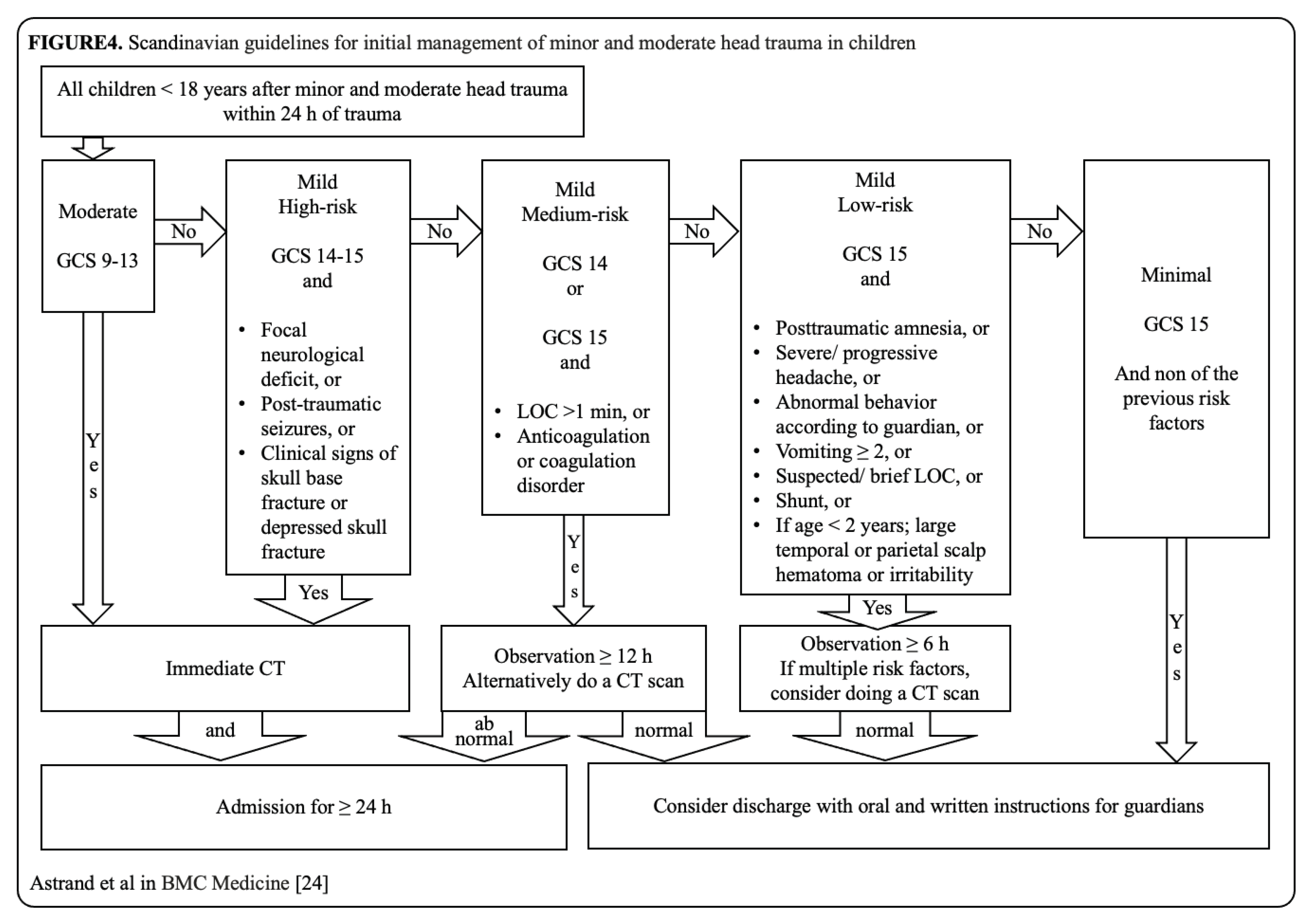
- Astrand, R.; Rosenlund, C.; Undén, J. Scandinavian guidelines for initial management of minor and moderate head trauma in children. BMC Med 2016, 14, 33. [Google Scholar] [CrossRef] [PubMed]
- Sadigh, G.; Kadom, N.; Karthik, P.; Sengupta, D.; Strauss, K. J.; Frush, D.; Applegate, K. E. Noncontrast Head CT in Children: National Variation in Radiation Dose Indices in the United States. AJNR Am J Neuroradiol 2018, 39, 1400–1405. [Google Scholar] [CrossRef] [PubMed]
- Journy, N. M. Y.; Dreuil, S.; Boddaert, N.; Chateil, J. F.; Defez, D.; Ducou-le-Pointe, H.; Garcier, J. M.; Guersen, J.; Habib Geryes, B.; Jahnen, A.; et al. Individual radiation exposure from computed tomography: a survey of paediatric practice in French university hospitals, 2010-2013. Eur Radiol 2018, 28, 630–641. [Google Scholar] [CrossRef]
- Schneider, T.; Wyse, E.; Pearl, M. S. Analysis of radiation doses incurred during diagnostic cerebral angiography after the implementation of dose reduction strategies. J Neurointerv Surg 2017, 9, 384–388. [Google Scholar] [CrossRef]
- Meulepas, J. M.; Ronckers, C. M.; Smets, A.; Nievelstein, R. A. J.; Gradowska, P.; Lee, C.; Jahnen, A.; van Straten, M.; de Wit, M. Y.; Zonnenberg, B.; et al. Radiation Exposure From Pediatric CT Scans and Subsequent Cancer Risk in the Netherlands. J Natl Cancer Inst 2019, 111, 256–263. [Google Scholar] [CrossRef]
- Pearce, M. S.; Salotti, J. A.; Little, M. P.; McHugh, K.; Lee, C.; Kim, K. P.; Howe, N. L.; Ronckers, C. M.; Rajaraman, P.; Sir Craft, A. W.; et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012, 380, 499–505. [Google Scholar] [CrossRef]
- Goodman, T. R.; Mustafa, A.; Rowe, E. Pediatric CT radiation exposure: where we were, and where we are now. Pediatr Radiol 2019, 49, 469–478. [Google Scholar] [CrossRef] [PubMed]
- Nabaweesi, R.; Ramakrishnaiah, R. H.; Aitken, M. E.; Rettiganti, M. R.; Luo, C.; Maxson, R. T.; Glasier, C. M.; Kenney, P. J.; Robbins, J. M. Injured Children Receive Twice the Radiation Dose at Nonpediatric Trauma Centers Compared With Pediatric Trauma Centers. J Am Coll Radiol 2018, 15, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Purvis, D.; Aldaghlas, T.; Trickey, A. W.; Rizzo, A.; Sikdar, S. A novel decision tree approach based on transcranial Doppler sonography to screen for blunt cervical vascular injuries. J Ultrasound Med 2013, 32, 1023–1031. [Google Scholar] [CrossRef] [PubMed]
- Sönnerqvist, C.; Brus, O.; Olivecrona, M. Validation of the scandinavian guidelines for initial management of minor and moderate head trauma in children. Eur J Trauma Emerg Surg 2021, 47, 1163–1173. [Google Scholar] [CrossRef] [PubMed]
| Denver Criteria | EAST Criteria | Modified Memphis Criteria | Utah Criteria | McGovern Criteria |
|---|---|---|---|---|
| Focal neurological deficit | Cervical hyperextension associated w/ displaced midface or complex mandibular fracture or closed head injury consistent with diffuse axonal injury | Basilar skull fracture with involvement of petrous bone | GCS score ≤8 (1Pt.) | GCS score ≤8 (1Pt.) |
| Arterial hemorrhage | Anoxic brain injury due to hypoxia as a result of squeezed arteries | Basilar skull fracture with involvement of the carotid canal | Focal neurological deficit (2Pt.) | Focal neurological deficit (2Pt.) |
| Cervical bruit in patients <50 yrs | Seatbelt abrasion or other soft-tissue injury resulting in swelling or altered mental status | Le Fort II or III fracture pattern | Carotid canal fracture (2Pt.) | Carotid canal fracture (2Pt.) |
| Expanding neck hematoma | Cervical vertebral body fracture or carotid canal fracture in proximity to the internal$$$carotid or vertebral arteries | Cervical spine fracture | Petrous temporal bone fracture (3Pt.) | Petrous temporal bone fracture (3Pt.) |
| Neurological exam findings inconsistent w/ head CT scan | Horner’s syndrome | Cerebral infarction on CT (3Pt.) | Cerebral infarction on CT (3Pt.) | |
| Cerebrovascular accident on follow-up head CT scan not seen on initial head CT scan | Neck soft-tissue injury (seatbelt sign, hanging or hematoma) | MOI (2Pt.) | ||
| Presence of Le Fort II or III fractures | Focal neurologic deficit not explained by imaging | |||
| Cervical spine fracture w/ subluxation | ||||
| C1–3 cervical spine fracture | ||||
| Cervical spine fracture extending into the transverse foramen | ||||
| Basilar skull fracture w/ carotid involvement | ||||
| Diffuse axonal injury w/ GCS score <6 | ||||
| Hypoxic ischemia due to squeezed arteries |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





