1. Introduction
There are many techniques for restoring tooth structure lost due to caries. The most common procedure is a filling, using amalgam or a composite resin material. More complicated and costly procedure such as crowns, laminates, ceramic fillings, or gold or ceramic inlays are also performed. The decision of restoration type is usually made after the advantages and disadvantages of each procedure: appearance, cost, length of the procedure, complications, if any, longevity, health hazards, etc. are discussed with the patient. The provider often explains which procedure they have more experience with, and possibly which procedure involves higher success rate.
Although providers emphasise primary prevention, this is often not achieved, and the consequences are dental decay or gum disease. To prevent worsening of the carious lesion and progression toward the nerve of the tooth necessitating root canal therapy, providers use fillings as a secondary prevention technique. As mentioned, the most common restorative materials used for "simple" fillings are amalgam and composite resin.
In the United States, 100 million people have amalgam fillings, and 100 million amalgams are placed yearly [1]. According to a 2019 publication [2], dental amalgam remains a predictable, cost-effective, and safe means for the restoration of posterior teeth. It is important to note that amalgam has been used for the last 150 years and only gold alloys have been used in the restoration of teeth for longer [3]. Alloys of mercury with metals such as silver, copper, tin, and zinc [4] have been used in the restorative material amalgam [5]. Dental amalgam has been studied and reviewed extensively and has an established record of safety and effectiveness [6]. An FDA 2004 report stated that "The current data are insufficient to support an association between mercury release from dental amalgam and the various complaints that have been attributed to this restoration material" [7]. In an article in JAMA from 2006 [8] the authors concluded that "there were no statistically significant differences in adverse neuropsychological or renal effects observed over the 5-year period in children using dental amalgam or composite materials". In 2009 the FDA literature supported the position that "amalgam is a valuable, viable, and safe choice for dental patients" [9].
On the other hand, at the 2013 Minamata Convention [10], (named after the bay in Japan where in the mid-20th century, mercury-tainted industrial wastewater poisoned thousands of people), the most recent global agreement on environment and health was reached. A decision was made to reduce all forms of mercury use. One of the outcomes of this decision adopted in the US was to phase-down dental amalgam use by increasing use of other restorative materials [11]. Concerns have also been raised about the potential of composite resin compounds to cause toxicity [12].
The superior longevity of amalgam has been demonstrated in several publications [13–15]. A meta-analysis from 2016 [16] concluded that composite restorations showed less longevity and higher secondary caries rates compared to amalgam restorations, and this was echoed in the study published in Evidence-Based Dentistry journal [17]. A 2023 study in the U.S [18] showed that the rate of amalgam restorations declined from a mean of 6.29 per 100 patients in 2017 to 4.78 per 100 patients in 2019, while composite resin restorations increased from 27.6 per 100 patients in 2017 to 28.8 per 100 in 2019. The mean number of amalgam restorations placed per person was lower in females than males. Another study [19] in 2023 indicated that non-amalgam restorations were the most common in the primary teeth of children older than 5 years and in the permanent teeth of adults younger than 40 years.
It seems as if the question of survival of amalgam versus composite resin has no universally accepted answer, yet based on the best available evidence, the International Association for Dental Research affirms the safety of dental amalgam, while supporting the phase-down strategy [20].
Our study based on a large data set focuses on the continuing amalgam longevity debate.
2. Materials & Methods
This retrospective study used data from the computerized database of Maccabi Dent, the second largest dental healthcare provider in Israel, with approximately 650,000 dental patients out the 2.5 million members of the Maccabi Health Fund. This database includes all information on dental treatments and medical data from Maccabi Dent’s nationwide dental clinics since 2014.
In addition to data regarding dental treatments, where each procedure has a unique identifying code, data regarding the age and gender of the patient, and the clinic location (an indication of socioeconomic status) were also examined. Only restorations on posterior teeth i.e., molars and premolars were studied, as amalgam is not used as a restorative material in anterior teeth.
The percentage of failures per year using the annual failure rate formula, was calculated using the following steps:
Determine the ratio of failures in n years to the number of restorations in n years.
Take this ratio to the power of 1 divided by n.
Subtract the result obtained from 1.
The formula can be expressed as follows:
Percentage of failures per year = 1 - ((number of failures in n years / number of restorations in n years) ^(1/n))
Three types of follow-up treatments indicated restoration failure:
We analysed the proportions of each of these follow-up treatments after amalgam and composite restorations. In order to determine the relationship between restoration size and failure rate, we considered the 5 surfaces of the tooth (occlusal, buccal, lingual, mesial and distal) and classified the original restorations as follows:
single surface restoration;
Restoration of 2-3 surfaces;
restoration of 4-5 surfaces;
two restorations on the same tooth.
Exclusion criteria were:
Incomplete data from 2022.
Data related to children under the age of 12.
Treatment entries with missing or invalid tooth numbers.
For records showing two restorations on the same tooth on the same day, only the first restoration was included in the analysis.
Restorations performed on the same day with different codes.
To assess the association between treatment type and failure rate, a generalized estimating equation (GEE) analysis was performed, which included adjustments for potential confounding variables and clustering effects caused by repeated observations within the same subject. A robust estimator covariance matrix, an exchangeable correlation matrix, and a binary logistic model were used. These parameters allow fit for the binary outcome and assume that the within-subject correlation is constant across all pairs of observations and uses robust standard errors in the estimation to address potential violations of the assumption of independence or heteroscedasticity in the data. This analysis helps ensure that the statistical inference is valid and reliable, even in the presence of correlated or heteroscedastic data.
The variables extracted from the analysis are the odds ratio (OR) which represents the likelihood of failure of one treatment type compared to the reference treatment type; confidence interval (CI) which provides a range of values within which the true odds ratio is likely to fall; and p-value that indicates the statistical significance of the association between the treatment type and failure rate.
IRB: This study was approved by the ethics committees of (0002-21 ASMC, 0019-22 MHC).
3. Results
Maccabi Dent’s data includes information from over 650,000 patients and 260,905 patients (146,315 females; 114,590 males) were treated between 2014 – 2021. Of the 260,905 patients in the cohort, 158,940 had repeated treatments. 84.7% of all treatments (566,987/668,952) were performed on these patients.
The present study had three major outcomes: amalgam, composite or mixed re-restoration, root canal treatment or extraction.
Figure 1 illustrates restoration failure and includes the initial restoration treatment code (amalgam or composite) and subsequent treatments on the same tooth i.e., amalgam, composite or mixed restoration, root canal treatment or extraction.
Table 1 shows analysis of the Odds Ratio (OR), and all comparisons were statistically significant regarding the main effect size (OR=1.25).
As seen in
Table 2, 668,952 restorations were performed for the first time on molars or premolars, 113,281 (16.9%) amalgam, 555,671 (83.1%) composite resin, and 85,635 (12.8%) were categorized as failures. Analysis of failure percentage based on treatment type revealed a significantly higher percentage of failed amalgams compared to composite restorations in all years examined. Specifically, 19,692 out of 113,281 first amalgam restorations failed (17.38%) all years, whereas 65,943 out of 555,671 composite restorations failed (11.87%) all years. It is interesting to note that the total number of amalgam restorations decreased in this period, while the number of composite fillings increased. (
Table 1).
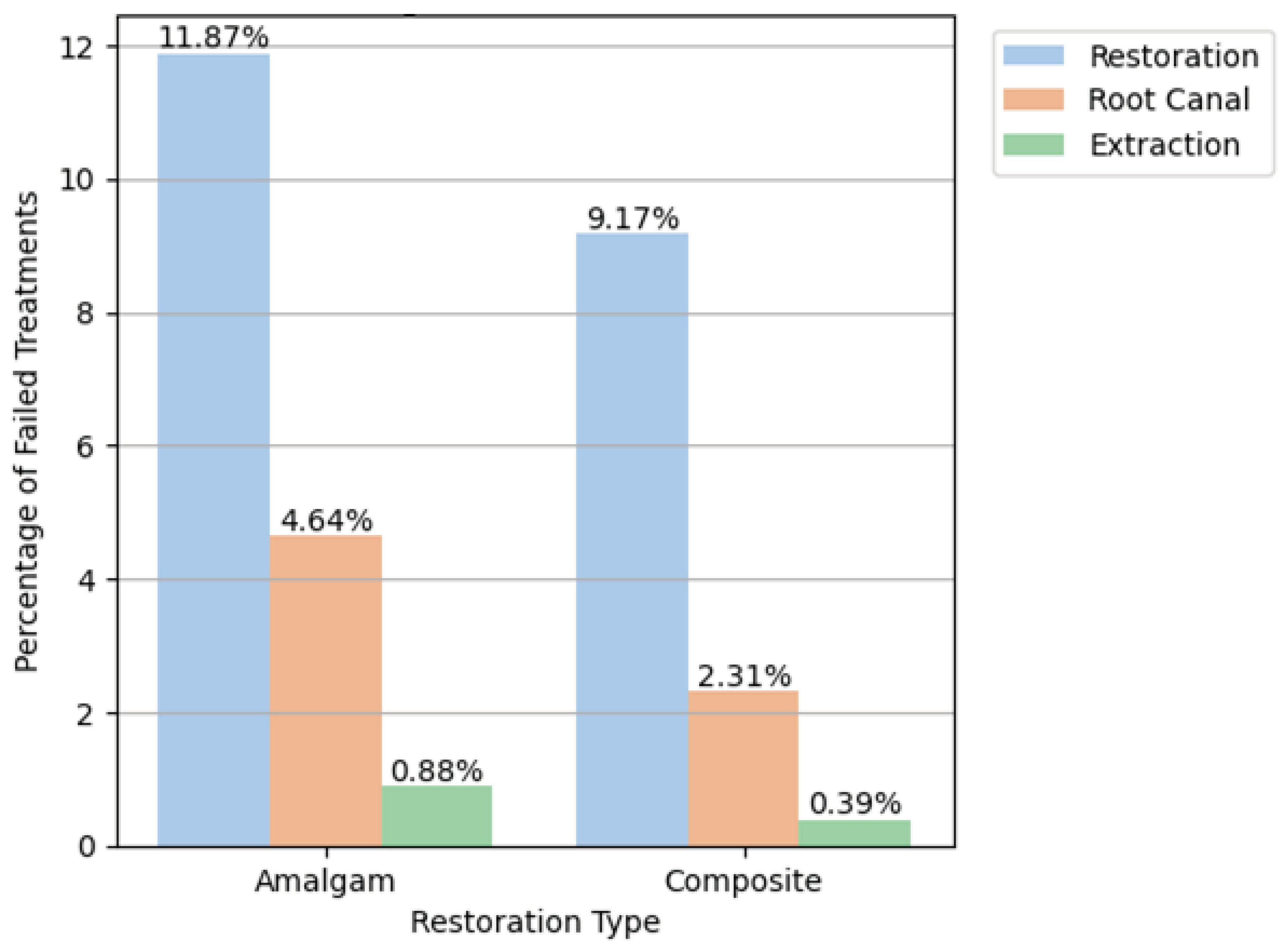
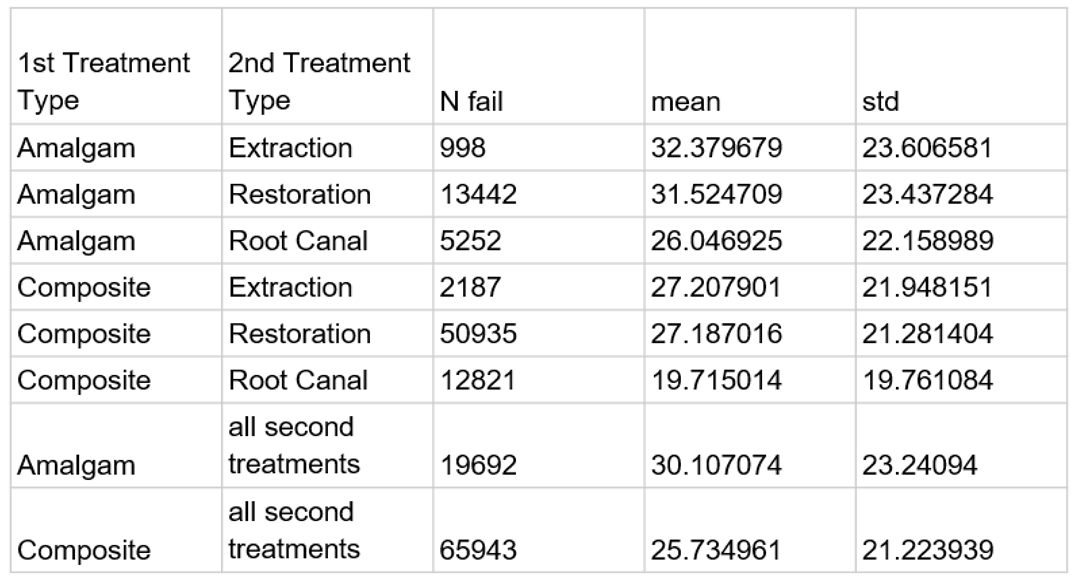
Examining the follow-up treatments indicative of amalgam restoration failure, revealed that the portion of a repeat restoration was the largest, with 13,442 repeated restorations (11.87% failure), 5,252 root canals (4.64%), and 998 extractions (0.88%). The follow-up treatments indicative of composite restoration failures showed that 50,935 (9.17% failure) underwent repeated restoration, 12,821 required root canal treatment (2.31%), and 2,187 (0.39%) required extraction (
Table 3,
Figure 1).
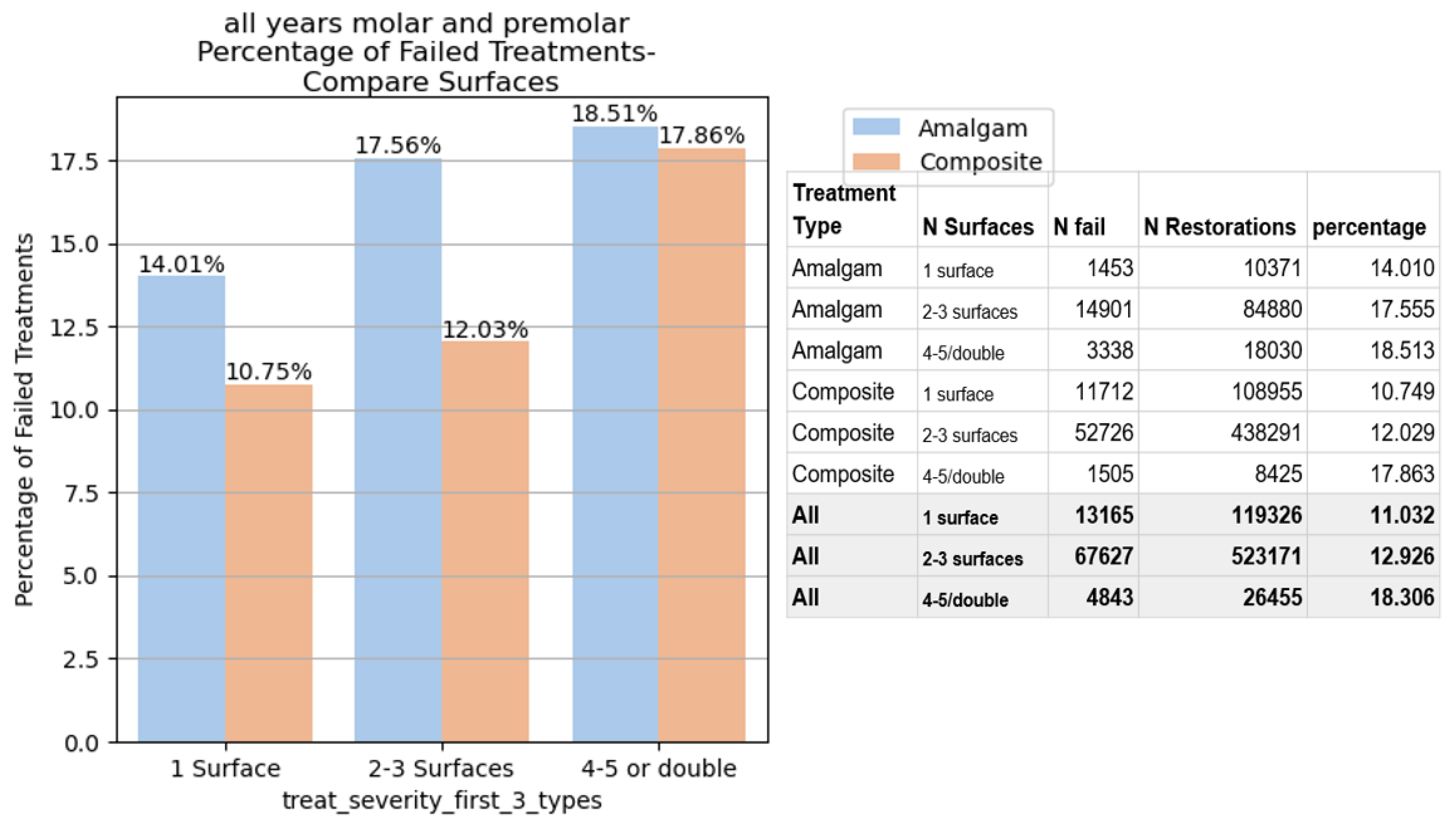
When examining the failure rates of amalgam and composite restorations based on the number of surfaces involved in the initial restoration, single-surface amalgam restorations 14.01% failed compared to 10.75% in composite. For restorations with 2-3 or and 4-5 surfaces, the failure rate was 17.54% and 18.51% in amalgam, compared to 12.07% and 17.86% in composite resin, (
Figure 2).
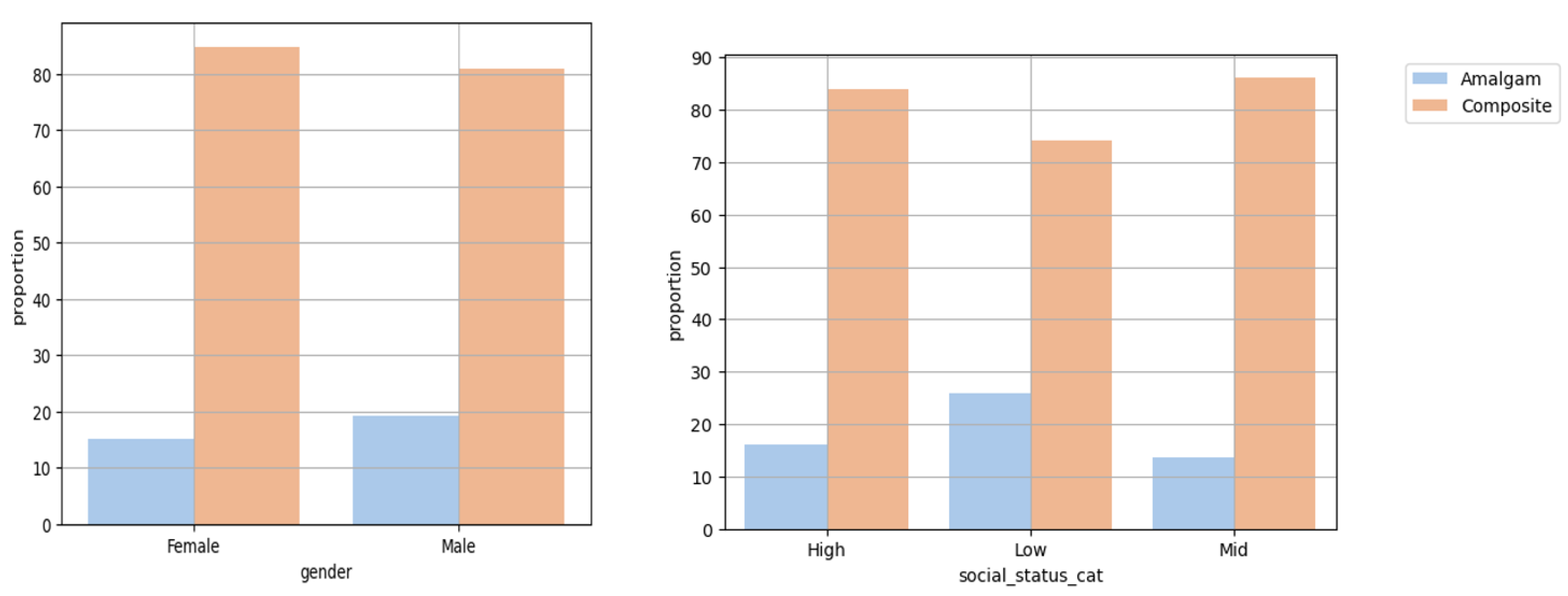
There were significantly less amalgam than composite restorations in males compared to females (p<0.0001) and in individuals of all socio-economic statuses (p<0.0001) (
Figure 3).
Our study concluded that failure over the study period was 17.38% for amalgam restorations and 11.87% for composite resin restorations. mAFR was 3.55% for amalgam restorations and 3.06% for composite resin restorations, (
Table 4).
Figure 2.
Restoration failure rates based on the number of surfaces treated.
Figure 2.
Restoration failure rates based on the number of surfaces treated.
Figure 3.
Proportion of amalgam and composite restorations according to gender and socio-economic status.
Figure 3.
Proportion of amalgam and composite restorations according to gender and socio-economic status.
Table 4.
Mean Annual Failure Rates and Failure Percentage at eight years for restoration type, tooth type, number of surfaces and follow-up treatment.
Table 4.
Mean Annual Failure Rates and Failure Percentage at eight years for restoration type, tooth type, number of surfaces and follow-up treatment.
| Restoration Type |
Failure % at Eight Years |
maen Annual Failure Rates (%) |
| Factor |
Amalgam |
Composite |
Amalgam |
Composite |
| Surfaces: |
|
|
|
|
| 1 Surface |
14.01
|
10.75
|
2.87
|
2.58
|
| 2-3 Surfaces |
17.56
|
12.03
|
3.39
|
2.84
|
| 4-5 Surfaces / Double Restoration |
18.51
|
17.86
|
4.01
|
4.81
|
| Teeth Group: |
|
|
|
|
| Molar |
17.54
|
12.07
|
3.57
|
3.16
|
| Molar Upper jaw |
16.39
|
11.36
|
3.29
|
3.03
|
| Molar Lower jaw |
18.82
|
12.68
|
3.89
|
3.26
|
| Premolar |
16.75
|
11.60
|
3.45
|
2.94
|
| Premolar Upper jaw |
15.51
|
11.02
|
3.14
|
2.82
|
| Premolar Lower jaw |
18.59
|
12.40
|
3.91
|
3.11
|
| Follow-up Indicative Treatment: |
|
|
|
|
| Repeated Restoration |
11.87
|
9.17
|
2.22
|
2.27
|
| Root Canal |
4.64
|
2.31
|
1.05
|
0.63
|
| Extraction |
0.88
|
0.39
|
0.18
|
0.10
|
| All |
17.38 |
11.87 |
3.55 |
3.06 |
4. Discussion
The results of the present study demonstrate a higher survival rate of composite compared to amalgam restorations. These results are based on data from Maccabi Dent the second largest HMO in Israel, with more than 650,000 patients treated in the 58 nationwide dental clinics with 440 dental units. In our eight-year retrospective filling-survival cohort, composite showed an advantage over amalgam in the summation of all years and in cross-sectional analyses across population groups, such as a socioeconomic status. In the last twenty years, recommendations have been made to reduce the use of mercury. International bodies such as the World Health Organization (WHO) made similar recommendations in 1997 [21] and in 2021 [22].
Prospective RCT studies have shown equal survival rates for composite and amalgam fillings [23]. In contrast, some retrospective studies have indicated that amalgam was advantageous for large posterior restorations and posterior composite restorations demonstrated lower survival [24]. The different results of the studies can be explained by the research models employed. One of the shortcomings inherent to RCT studies is the lack of long-term follow-up, these studies are often carried out in uniform groups of low-risk participants, such as dental teams. These groups are not representative and therefore the findings can have errors due to bias. This shortcoming could be overcome by using the pragmatic research approach. According to Opdam et al., [25], in retrospective practice-based studies, differences in reconstruction survivals appear after five years, and then a real-life study is required. The studies that meet these requirements are the big data studies such as the current mega-data study with data from over eight years.
Some of the previous studies categorized types of restoration failure such as restoration fracture or secondary caries. In the current study we compared the survival of two restoration materials based on the need for renewal of the restoration for any reason, root canal treatment, or extraction of the same tooth, the reason for subsequent treatment was not examined.
A recent JADA [26] publication based on 38 trials that evaluated the effectiveness of direct restorative materials to treat caries lesions noted there was limited evidence of clinically important differences between the restorative materials they assessed.
Several studies [27–29] found that women prefer composite restorations, whereas men preferred amalgam restorations. They also noted a preference for composite restorations which are generally more expensive in areas with higher socioeconomic status, while amongst those of a lower socioeconomic status, amalgam (which is generally less expensive) was preferred. In the current study, examinations by gender and socioeconomic status, revealed a statistically significant preference for composite over amalgam restorations. The large size of our cohort minimizes the chance of random findings.
5. Conclusions
The current study found no evidence of the superiority of amalgam over composite restorations. At a time when a global environmental decision has been made to reduce the use of mercury, it seems that there are no clinical reasons to continue treatments with amalgam alloy in dentistry. We found that more composite restorations are being placed, this may be due to aesthetic concerns, the generally higher compensation or because some healthcare providers believe that composite is safer. This study, based on big data, indicates that composite restorations have a lower failure rate than amalgams and there is now strong evidence to end the long-standing debate on the longevity of amalgam and composite materials, and hence we can strongly support Minamata recommendations for the use of composite resin materials only.
References
- Elliot V. Feldbau, Jennifer L. FrustinoJe, Steven A. Migliorini; Dental Secrets (Fourth Edition); Amalgam, Mercury, and Health Issues; 2015; pp. 147–200.
- Available online: https://www.sciencedirect.com/science/article/pii/b9780323262781000088.
- Dental Amalgam: Science direct. Dental amalgam remains a predictable, cost-effective, and safe means for the restoration of posterior (and some anterior) teeth that are missing various amounts of tooth structure. From: Sturdevant’s Art and Science of Operative Dentistry, 2019.
- Chadwick, R.G.; Lloyd, C.H. Dental amalgam: the history and legacy you perhaps never knew? Br Dent J 2022, 232, 633–637. [Google Scholar] [CrossRef]
- Leinfelder, K.F. Dental amalgam alloys. Curr Opin Dent 1991, 1, 214–217. [Google Scholar] [PubMed]
- Marshall, S.J.; Marshall, G.W., Jr. Dental amalgam: the materials. Adv Dent Res 1992, 6, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Dental amalgam: update on safety concerns. ADA council on Scientific Affairs. J Am Dent Assoc 1998, 129, 494–503. [CrossRef] [PubMed]
- Bellinger, D.C.; Daniel, D.; Trachtenberg, F.; Tavares, M.; McKinlay, S. Dental amalgam restorations and children’s neuropsychological function: the New England Children’s Amalgam Trial. Environ Health Perspect 2007, 115, 440–446. [Google Scholar] [CrossRef] [PubMed]
- DeRouen, T.A.; Martin, M.D.; Leroux, B.G.; Townes, B.D.; Woods, J.S.; Leitão, J.; Castro-Caldas, A.; Luis, H.; Bernardo, M.; Rosenbaum, G.; Martins, I.P. Neurobehavioral effects of dental amalgam in children: a randomized clinical trial. JAMA 2006, 295, 1784–1792. [Google Scholar] [CrossRef]
- European Commission: Scientific Committee on Emerging and Newly Identified Health Risks. The safety of Dental Amalgam and Alternative Dental Restoration Materials for Patients and Users, 2008.
- Minamata Convention on Mercury. United States Environmental Protection Agency. Available online: https://www.mercuryconvention.org/sites/default/files/2021-06/minamata-convention-booklet-sep-2019-en-pdf.
- Estrich, C.G.; Lipman, R.D.; Araujo, M.W.B. Dental amalgam restorations in nationally representative sample of US population aged ≥15 years: NHANES 2011-2016. J Public Health Dent 2021, 81, 327–330. [Google Scholar] [CrossRef] [PubMed]
- Composite Resin Versus Amalgam for Dental Restorations—CADTH Report/Projects in Briefs. Canadian Agency for Drugs and Technologies in Health: Ottawa, ON, Canada, 2011–2018.
- Available online: https://www.ncbi.nlm.nih.gov/books/NBK535155/.
- Rasines Alcaraz, M.G.; Veitz-Keenan, A.; Sahrmann, P.; Schmidlin, P.R.; Davis, D.; Iheozor-Ejiofor, Z. Direct composite resin fillings versus amalgam fillings for permanent or adult posterior teeth. Cochrane Database Syst Rev 2014, CD005620, Update in Cochrane Database Syst Rev 2021, 8, CD005620. [Google Scholar] [CrossRef]
- . [CrossRef]
- Soares, A.C.; Cavalheiro, A. A review of amalgam and composite longevity of posterior restorations. Revista Portuguesa de Estomatologia, Medicina Dentaria e Cirurgia Maxilofacial 2010, 51, 155–164. [Google Scholar] [CrossRef]
- Bernardo, M.; Luis, H.; Martin, M.D.; Leroux, B.G.; Rue, T.; Leitão, J.; DeRouen, T.A. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J Am Dent Assoc 2007, 138, 775–783. [Google Scholar] [CrossRef]
- Amalgam vs Composite Restoration, Survival, and Secondary Caries. Journal of Evidence-Based Dental Practice 2016, 16, 107–109. [CrossRef] [PubMed]
- Alhareky, M.; Tavares, M. Amalgam vs Composite Restoration, Survival, and Secondary Caries. J Evid Based Dent Pract 2016, 16, 107–109. [Google Scholar] [CrossRef] [PubMed]
- Estrich, C.G.; Eldridge, L.A.; Lipman, R.D.; Araujo, M.W.B. Posterior dental restoration material choices in privately insured people in the United States, 2017 through 2019. J Am Dent Assoc 2023, 154, 393–402. [Google Scholar] [CrossRef]
- Beltrán-Aguilar, E.D.; Thornton-Evans, G.; Wei, L.; Bernal, J. Prevalence and mean number of teeth with amalgam and nonamalgam restorations, United States, 2015 through 2018. J Am Dent Assoc 2023, 154, 417–426. [Google Scholar] [CrossRef] [PubMed]
- Ajiboye, A.S.; Mossey, P.A.; IADR Science Information Committee; Fox, C.H. International Association for Dental Research Policy and Position Statements on the Safety of Dental Amalgam. J Dent Res 2020, 99, 763–768. [Google Scholar] [CrossRef] [PubMed]
- Mjor, I.A.; Pakhomov, G.N. Dental amalgam and alternative direct restorative materials. World Health Organization, 1997; https://apps.who.int/iris/handle/10665/63711.
- Minamata Convention on Mercury. Report 197, Commonwealth of Australia 2021.
- Manhart, J.; Chen, H.; Hamm, G.; Hickel, R. Buonocore Memorial Lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent 2004, 29, 481–508. [Google Scholar] [PubMed]
- Van Nieuwenhuysen, J.P.; D’Hoore, W.; Carvalho, J.; Qvist, V. Long-term evaluation of extensive restorations in permanent teeth. J Dent 2003, 31, 395–405. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.; Bronkhorst, E.M.; Cenci, M.S.; Huysmans, M.C.; Wilson, N.H. Age of failed restorations: A deceptive longevity parameter. J Dent 2011, 39, 225–230. [Google Scholar] [CrossRef]
- Pilcher, L.; Pahlke, S.; Urquhart, O.; O’Brien, K.K.; Dhar, V.; Fontana, M.; González-Cabezas, C.; Keels, M.A.; Mascarenhas, A.K.; Nascimento, M.M.; Platt, J.A.; Sabino, G.J.; Slayton, R.L.; Tinanoff, N.; Young, D.A.; Zero, D.T.; Tampi, M.P.; Purnell, D.; Salazar, J.; Megremis, S.; Bienek, D.; Carrasco-Labra, A. Direct materials for restoring caries lesions: Systematic review and meta-analysis-a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 2023, 154, e1–e98, Erratum in J Am Dent Assoc 2023, 154, A9. [Google Scholar] [CrossRef]
- Willershausen, B.; Witzel, S.; Schuster, S.; Kasaj, A. Influence of gender and social factors on oral health, treatment degree and choice of dental restorative materials in patients from a dental school. Int J Dent Hyg 2010, 8, 116–120. [Google Scholar] [CrossRef]
- Vidnes-Kopperud, S.; Tveit, A.B.; Gaarden, T.; Sandvik, L.; Espelid, I. Factors influencing dentists’ choice of amalgam and tooth-colored restorative materials for Class II preparations in younger patients. Acta Odontol Scand 2009, 67, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Bailey, O.; Stone, S.; Ternent, L.; Vernazza, C.R. Public Valuation of Direct Restorations: A Discrete Choice Experiment. J Dent Res 2022, 101, 1572–1579. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).