Submitted:
26 March 2024
Posted:
27 March 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Distribution of Canine Visceral Leishmaniasis in the World
2.1. Africa
The Americas
Asia
Europe
| Continent | Country | Location | Parasite species | % of dogs positive for Leishmania (diagnostic test used) | References |
| África | Ethiopia | Amhara region | L. donovani Complex* | 3.8% (RIFI and ELISA); 2.8% (PCR) | [173] |
| Kafta Humera district | L. donovani | 27.7% (DAT); 14.8% (KDRT) | [174] | ||
| Amhara region | L. donovani | 40% (DAT) | [175] | ||
| Addis Zemen, Humera, and Sheraro |
L. donovani Complex* |
5.9% (PCR) | [176] | ||
| Benishangul-Gumuz region | NA | 13.9% (rK39 ICT); 5.6 (DAT) | [177] | ||
| Ambo, Ejaji, and Weliso | L. infantum | 84.24% (ELISA) | [178] | ||
| Burkina-Faso | Bobo-Dioulasso | L. infantum | 5.88% (Serological test) | [39] | |
| Côte d’Ivoire | Abidjan and Yamoussoukro cities | L. infantum | 8.9% (PCR or IFAT) | [40] | |
| Nigeria | Oyo, Ogun, and Kwara | NA | 4.4% (ELISA) | [41] | |
| Senegal | Mont Rolland | L. infantum | 46.3% (PCR) | [42] | |
| Zambia | Southern Province | L. infantum | NA (Serological tests and PCR) | [43] | |
| Asia |
Iran |
Meshkin-Shahr district | L. infantum | 15.8% (DAT) | [179] |
| Boyer Ahmad district | L. infantum | 10% (DAT) | [180] | ||
| Kouhsar district | L. infantum | 3.6% (DAT) | [181] | ||
| Khorasan Razavi province | L. infantum | 7.6% (IFAT) | [182] | ||
| Kerman province | L. infantum | 11.25% (DAT) | [183] | ||
| Kerman and Sistan-Baluchestan provinces | L. infantum | 15.4% (ELISA) | [184] | ||
| Tehran and Alborz provinces | L. infantum | 4.9% (DAT) | [185] | ||
| Meshkin-Shahr district | L. infantum | 23.4% (DAT) | [186] | ||
| Hamedan province | L. infantum | 3.95% (ELISA) | [187] | ||
| Jiroft district | L. infantum | 7.9% (DAT) | [188] | ||
| Ardabil, Alborz, and East-Azerbaijan provinces | L. infantum | 100% (DAT, rK39, and PCR) | [102] | ||
| Alborz province | L. infantum | 2.97% (DAT) | [189] | ||
| Golestan province | L. infantum | 18% (PCR) | [190] | ||
| Nepal | Kathmandu |
L. donovani Complex* |
18.57% (PCR) | [113] | |
| Pakistan | Chilas, Abbotabad, Bagh, Poonch, and Muzafarabad districts |
L. donovani Complex* |
18% (DAT); 26.6% (ELISA) | [114] | |
| Philippines | NA | L. infantum | NA | [120] | |
| Vietnam | NA | L. infantum | NA | [120] | |
| Europe | Bulgaria | Petrich | L. infantum | NA (IFAT, PCR) | [160] |
| Georgia | Tbilisi and Kutaisi |
L. donovani Complex* |
20% (rK39 test) | [161] | |
| Kvareli and Sagarejo districts | 19.5% and 11.4% (rK39 test) | [162] | |||
| Germany | NA | NA | 11.8% (ELISA) | [163] | |
| Hungary | Tolna province | L. infantum | 30% (IFAT, PCR) | [164] | |
| Kosovo | Prizren, Gjakova, Rahovec, and Deçan | L. infantum | 18.49% (ELISA) | [165] | |
| The Netherlands | NA | NA | 32.4% (ELISA) | [163] | |
| North Macedonia | Skopje and Prilep | L. infantum | 2.5% (PCR) | [166] | |
| Romania | Vâlcea County | L. infantum | NA (FASTest®LEISH) | [167] | |
| Ramnicu Vâlcea | L. infantum | 8.75% (ELISA);10% (PCR) | [168] | ||
| Galați | NA | 8.33% (ELISA) | [169] | ||
| Argeș County | L. infantum | 20.1% (PCR) | [170] | ||
| Slovenia | Kostelo | L. infantum | NA (IFAT) | [171] | |
| Switzerland | NA | NA | 12.2% (ELISA) | [163] | |
| United Kingdom | NA | L. infantum | NA (ELISA, PCR | [172] |
3. Factors Influencing the Territorial Expansion and Transmission Maintenance of Visceral Leishmaniasis
4. The Dog’s Role in the Visceral Leishmaniasis Transmission Cycle
5. The Challenges of Controlling the Spread of Canine Visceral Leishmaniasis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alves, F.; Bilbe, G.; Blesson, S.; Goyal, V.; Monnerat, S.; Mowbray, C.; Muthoni Ouattara, G.; Pécoul, B.; Rijal, S.; Rode, J.; et al. Recent Development of Visceral Leishmaniasis Treatments: Successes, Pitfalls, and Perspectives. Clin Microbiol Rev 2018, 31. [Google Scholar] [CrossRef]
- Alvar, J.; Vélez, I.D.; Bern, C.; Herrero, M.; Desjeux, P.; Cano, J.; Jannin, J.; Boer, M. den Leishmaniasis Worldwide and Global Estimates of Its Incidence. PLoS One 2012, 7, e35671. [Google Scholar] [CrossRef]
- Alemayehu, B.; Alemayehu, M. Leishmaniasis: A Review on Parasite, Vector and Reservoir Host. Health Science Journal 2017, 11. [Google Scholar] [CrossRef]
- Rossi, M.; Fasel, N. How to master the host immune system? Leishmania parasites have the solutions! Int Immunol 2018, 30, 103–111. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/leishmaniasis. (accessed on 1 March 2022).
- McGwire, B.S.; Satoskar, A.R. Leishmaniasis: clinical syndromes and treatment. QJM 2014, 107, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Organização Panamericana da Saúde Leishmanioses: Informe Epidemiológico Das Américas; 2021.
- Maurı́cio, I.L.; Stothard, J.R.; Miles, M.A. The Strange Case of Leishmania chagasi. Parasitology Today 2000, 16, 188–189. [Google Scholar] [CrossRef] [PubMed]
- Lukeš, J.; Mauricio, I.L.; Schönian, G.; Dujardin, J.-C.; Soteriadou, K.; Dedet, J.-P.; Kuhls, K.; Tintaya, K.W.Q.; Jirků, M.; Chocholová, E.; et al. Evolutionary and geographical history of the Leishmania donovani complex with a revision of current taxonomy. Proceedings of the National Academy of Sciences 2007, 104, 9375–9380. [Google Scholar] [CrossRef]
- Roque, A.L.R.; Jansen, A.M. Wild and synanthropic reservoirs of Leishmania Species in the Americas. Int J Parasitol Parasites Wildl 2014, 3, 251–262. [Google Scholar] [CrossRef]
- Roatt, B.M.; de Aguiar-Soares, R.D.O.; Coura-Vital, W.; Ker, H.G.; das Moreira, N.D.; Vitoriano-Souza, J.; Giunchetti, R.C.; Carneiro, C.M.; Reis, A.B. Immunotherapy and immunochemotherapy in visceral leishmaniasis: promising treatments for this neglected disease. Front Immunol 2014, 5, 272. [Google Scholar] [CrossRef]
- Burza, S.; Croft, S.L.; Boelaert, M. Leishmaniasis. Lancet 2018, 392, 951–970. [Google Scholar] [CrossRef] [PubMed]
- Moreno, J. Assessment of Vaccine-Induced Immunity Against Canine Visceral Leishmaniasis. Front Vet Sci 2019, 6, 168. [Google Scholar] [CrossRef]
- Solano-Gallego, L.; Koutinas, A.; Miró, G.; Cardoso, L.; Pennisi, M.G.; Ferrer, L.; Bourdeau, P.; Oliva, G.; Baneth, G. Directions for the diagnosis, clinical staging, treatment and prevention of canine leishmaniosis. Vet Parasitol 2009, 165, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Dantas-Torres, F.; Solano-Gallego, L.; Baneth, G.; Ribeiro, V.M.; de Paiva-Cavalcanti, M.; Otranto, D. Canine Leishmaniosis in the Old and New Worlds: unveiled similarities and differences. Trends Parasitol 2012, 28, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Ulchar, I.; Celeska, I.; Stefanovska, J.; Jakimovska, A. Hematological and Biochemical Parameters in Symptomatic and Asymptomatic Leishmania-Seropositive Dogs. Maced Vet Rev 2015, 38, 175–182. [Google Scholar] [CrossRef]
- Gonçalves, A.A.M.; Leite, J.C.; Resende, L.A.; da Mariano, R.M.S.; Silveira, P.; de Melo-Júnior, O.A.O.; Ribeiro, H.S.; de Oliveira, D.S.; Soares, D.F.; Santos, T.A.P.; et al. An Overview of Immunotherapeutic Approaches Against Canine Visceral Leishmaniasis: What Has Been Tested on Dogs and a New Perspective on Improving Treatment Efficacy. Front Cell Infect Microbiol 2019, 9, 427. [Google Scholar] [CrossRef] [PubMed]
- Ready, P. Epidemiology of visceral leishmaniasis. Clin Epidemiol 2014, 6, 147. [Google Scholar] [CrossRef]
- Kabbout, N.; Merzoug, D.; Chenchouni, H. Ecological Status of Phlebotomine Sandflies (Diptera: Psychodidae) in Rural Communities of Northeastern Algeria. J Arthropod Borne Dis 2016, 10, 24–38. [Google Scholar]
- Harrat, Z.; Belkaid, M. Les Leishmanioses Dans l’Algérois. Données Épidémiologiques. 6ème congrès international francophone de médecine tropicale “Santé et urbanisation en Afrique” 2002.
- Adel, A.; Saegerman, C.; Speybroeck, N.; Praet, N.; Victor, B.; De Deken, R.; Soukehal, A.; Berkvens, D. Canine leishmaniasis in Algeria: True prevalence and diagnostic test characteristics in groups of dogs of different functional type. Vet Parasitol 2010, 172, 204–213. [Google Scholar] [CrossRef]
- Adel, A.; Abatih, E.; Speybroeck, N.; Soukehal, A.; Bouguedour, R.; Boughalem, K.; Bouhbal, A.; Djerbal, M.; Saegerman, C.; Berkvens, D. Estimation of Canine Leishmania Infection Prevalence in Six Cities of the Algerian Littoral Zone Using a Bayesian Approach. PLoS One 2015, 10, e0117313. [Google Scholar] [CrossRef]
- Medkour, H.; Laidoudi, Y.; Lafri, I.; Davoust, B.; Mekroud, A.; Bitam, I.; Mediannikov, O. Canine vector-borne protozoa: Molecular and serological investigation for Leishmania spp., Trypanosoma spp., Babesia spp., and Hepatozoon spp. in dogs from Northern Algeria. Vet Parasitol Reg Stud Reports 2020, 19, 100353. [Google Scholar] [CrossRef]
- Bia, T.; Sanchez, C.; Zait, H.; Kouidri, M.; Mabrouk, S.K.; Nieto, J.; Ammar, S.S.M.; Moreno, J.; Ahlem, B.N. Diagnosis and prevalence of canine leishmaniasis in the Atlas shepherd dog. Vet Parasitol Reg Stud Reports 2022, 36, 100787. [Google Scholar] [CrossRef] [PubMed]
- Jeaume, G. Un Cas de Leishmaniose Naturelle Généralisée Chez Le Chien Au Maroc. Bulletiin de la Société de Pathologie Exotique 1932, 25, 225–227. [Google Scholar]
- Kahime, K.; Boussaa, S.; Nhammi, H.; Boumezzough, A. Urbanization of human visceral leishmaniasis in Morocco. Parasite Epidemiol Control 2017, 2, 1–6. [Google Scholar] [CrossRef]
- Idrissi, H.; Hakkour, M.; Duchateau, L.; Zanatta, R.; Kachani, M.; Azrib, R.; Daminet, S.; Kichou, F.; El Asatey, S.; Tazi, N.; et al. Canine Leishmaniasis in Morocco: A Descriptive Prospective Clinical Study. Vet Med Int 2021, 2021, 6304127. [Google Scholar] [CrossRef] [PubMed]
- Nicolle, C.; Comte, C. Origine Canine Du Kala-Azar. Bulletin of the Societe Pathology Exotique 1908, 1, 299–301. [Google Scholar]
- Diouani, M.F.; Ben Alaya Bouafif, N.; Bettaib, J.; Louzir, H.; Jedidi, S.; Ftaiti, A.; Zaatour, A.; Jomaa, I.; Dellagi, K.; Ben Ismail, R.; et al. Dogs L. infantum Infection from an Endemic Region of the North of Tunisia: A Prospective Study. Arch Inst Pasteur Tunis 2008, 85, 55–61. [Google Scholar] [PubMed]
- Chargui, N.; Haouas, N.; Gorcii, M.; Akrout Messaidi, F.; Zribi, M.; Babba, H. Increase of Canine Leishmaniasis in a Previously Low-Endemicity Area in Tunisia. Parasite 2007, 14, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Chargui, N.; Haouas, N.; Gorcii, M.; Lahmar, S.; Guesmi, M.; Ben Abdelhafidh, A.; Mezhoud, H.; Babba, H. Use of PCR, IFAT and in vitro Culture in the Detection of Leishmania infantum Infection in Dogs and Evaluation of the Prevalence of Canine Leishmaniasis in a Low Endemic Area in Tunisia. Parasite 2009, 16, 65–69. [Google Scholar] [CrossRef]
- Zoghlami, Z.; Chouihi, E.; Barhoumi, W.; Dachraoui, K.; Massoudi, N.; Helel, K. Ben; Habboul, Z.; Hadhri, M.H.; Limam, S.; Mhadhbi, M.; et al. Interaction between canine and human visceral leishmaniases in a holoendemic focus of Central Tunisia. Acta Trop 2014, 139, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Bouattour, A.; Amri, A.; Belkhiria, J.A.; Rhim, A.; Fezaa, O.; Gantier, J.-C.; M’ghirbi, Y. Canine leishmaniosis in Tunisia: Growing prevalence, larger zones of infection. PLoS Negl Trop Dis 2021, 15, e0009990. [Google Scholar] [CrossRef]
- Selim, A.; Shoulah, S.; Abdelhady, A.; Alouffi, A.; Alraey, Y.; Al-Salem, W. Seroprevalence and Risk Factors Associated with Canine Leishmaniasis in Egypt. Vet Sci 2021, 8, 236. [Google Scholar] [CrossRef] [PubMed]
- Leta, S.; Dao, T.H.T.; Mesele, F.; Alemayehu, G. Visceral Leishmaniasis in Ethiopia: An Evolving Disease. PLoS Negl Trop Dis 2014, 8, e3131. [Google Scholar] [CrossRef] [PubMed]
- Dereure, J.; Boni, M.; Pratlong, F.; el Hadi Osman, M.; Bucheton, B.; el-Safi, S.; Feugier, E.; Musa, M.K.; Davoust, B.; Dessein, A.; et al. Visceral leishmaniasis in Sudan: first identifications of Leishmania from dogs. Trans R Soc Trop Med Hyg 2000, 94, 154–155. [Google Scholar] [CrossRef]
- Dereure, J.; El-Safi, S.H.; Bucheton, B.; Boni, M.; Kheir, M.M.; Davoust, B.; Pratlong, F.; Feugier, E.; Lambert, M.; Dessein, A.; et al. Visceral leishmaniasis in eastern Sudan: parasite identification in humans and dogs; host-parasite relationships. Microbes Infect 2003, 5, 1103–1108. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.M.; Osman, O.F.; El-Raba’a, F.M.; Schallig, H.D.; Elnaiem, D.-E.A. Role of the domestic dog as a reservoir host of Leishmania donovani in eastern Sudan. Parasit Vectors 2009, 2, 26. [Google Scholar] [CrossRef]
- Sangare, I.; Djibougou, A.; Koudraogo, B.; Drabo, F.; Diabate, A.; Laure Banu, A.; Fournet, F.; Price, H.; Tinga Guig, R.; Kounbobr, D.R. First Detection of Leishmania infantum in Domestic Dogs from Burkina Faso (West Africa). Research Journal of Parasitology 2016, 12, 27–32. [Google Scholar] [CrossRef]
- Medkour, H.; Laidoudi, Y.; Athias, E.; Bouam, A.; Dizoé, S.; Davoust, B.; Mediannikov, O. Molecular and serological detection of animal and human vector-borne pathogens in the blood of dogs from Côte d’Ivoire. Comp Immunol Microbiol Infect Dis 2020, 69, 101412. [Google Scholar] [CrossRef]
- Adediran, O.A.; Kolapo, T.U.; Uwalaka, E.C. Seroprevalence of canine leishmaniasis in Kwara, Oyo and Ogun states of Nigeria. Journal of Parasitic Diseases 2016, 40, 510–514. [Google Scholar] [CrossRef]
- Faye, B.; Bañuls, A.L.; Bucheton, B.; Dione, M.M.; Bassanganam, O.; Hide, M.; Dereure, J.; Choisy, M.; Ndiaye, J.L.; Konaté, O.; et al. Canine visceral leishmaniasis caused by Leishmania infantum in Senegal: Risk of Emergence in Humans? Microbes Infect 2010, 12, 1219–1225. [Google Scholar] [CrossRef]
- Squarre, D.; Chambaro, H.M.; Hayashida, K.; Moonga, L.C.; Qiu, Y.; Goto, Y.; Oparaocha, E.; Mumba, C.; Muleya, W.; Bwalya, P.; et al. Autochthonous Leishmania infantum in Dogs, Zambia, 2021. Emerg Infect Dis 2022, 28, 888–890. [Google Scholar] [CrossRef] [PubMed]
- Kuhls, K.; Alam, M.Z.; Cupolillo, E.; Ferreira, G.E.M.; Mauricio, I.L.; Oddone, R.; Feliciangeli, M.D.; Wirth, T.; Miles, M.A.; Schönian, G. Comparative Microsatellite Typing of New World Leishmania infantum Reveals Low Heterogeneity among Populations and Its Recent Old World Origin. PLoS Negl Trop Dis 2011, 5, e1155. [Google Scholar] [CrossRef] [PubMed]
- Organização Pan-Americada da Saúde Leishmanioses: Informe Epidemiológico nas Américas; 2020.
- Salomon, O.; Sinagra, A.; Nevot, M.; Barberian, G.; Paulin, P.; Estevez, J.; Riarte, A.; Estevez, J. First visceral leishmaniasis focus in Argentina. Mem Inst Oswaldo Cruz 2008, 103, 109–111. [Google Scholar] [CrossRef]
- Acardi, S.A.; Liotta, D.J.; Santini, M.S.; Romagosa, C.M.; Salomón, O.D. Detection of Leishmania infantum in naturally infected Lutzomyia longipalpis (Diptera: Psychodidae: Phlebotominae) and Canis familiaris in Misiones, Argentina: the first report of a PCR-RFLP and sequencing-based confirmation assay. Mem Inst Oswaldo Cruz 2010, 105, 796–799. [Google Scholar] [CrossRef]
- Cruz, I.; Acosta, L.; Gutiérrez, M.N.; Nieto, J.; Cañavate, C.; Deschutter, J.; Bornay-Llinares, F.J. A canine leishmaniasis pilot survey in an emerging focus of visceral leishmaniasis: Posadas (Misiones, Argentina). BMC Infect Dis 2010, 10, 342. [Google Scholar] [CrossRef] [PubMed]
- Acosta, L.; Díaz, R.; Torres, P.; Silva, G.; Ramos, M.; Fattore, G.; Deschutter, E.J.; Bornay-Llinares, F.J. IDENTIFICATION OF Leishmania infantum IN PUERTO IGUAZÚ, MISIONES, ARGENTINA. Rev Inst Med Trop Sao Paulo 2015, 57, 175–176. [Google Scholar] [CrossRef] [PubMed]
- Fujisawa, K.; Silcott-Niles, C.; Simonson, P.; Lamattina, D.; Humeres, C.A.; Bhattacharyya, T.; Mertens, P.; Thunissen, C.; O’Rourke, V.; Pańczuk, M.; et al. Emergent canine visceral leishmaniasis in Argentina: Comparative diagnostics and relevance to proliferation of human disease. PLoS Negl Trop Dis 2021, 15, e0009552. [Google Scholar] [CrossRef]
- Lamattina, D.; Berrozpe, P.E.; Casas, N.; Moya, S.L.; Giuliani, M.G.; Costa, S.A.; Arrabal, J.P.; Martínez, M.F.; Rivero, M.R.; Salas, M.; et al. Twice upon a time: The progression of canine visceral leishmaniasis in an Argentinean city. PLoS One 2019, 14, e0219395. [Google Scholar] [CrossRef]
- Barroso, P.A.; Marco, J.D.; Locatelli, F.M.; Cardozo, R.M.; Hoyos, C.L.; Mora, M.C.; García Bustos, M.F.; López-Quiroga, I.; Mimori, T.; Gentile, A.G.; et al. Visceral Leishmaniasis Caused by Leishmania infantum in Salta, Argentina: Possible Reservoirs and Vectors. Am J Trop Med Hyg 2015, 93, 334–339. [Google Scholar] [CrossRef]
- Le Pont, F.; Mollinedo, S.; Mouchet, J.; Desjeux, P. Leishmaniose en Bolivie. IV. Le chien dans les cycles des leishmanioses en Bolivie. Mem. Inst. Oswaldo Cruz 1989, 84, 417–421. [Google Scholar] [CrossRef]
- del Zambrano Hernandez, C.P.; Ayala Sotelo, M.S.; Fuya Oviedo, O.P.; Montenegro Puentes, C.A.; Aya Vanegas, N.M.; Rodriguez Toro, J.G.; Becerra Osorio, S.L.; Aguilera Jaramillo, G.; Lozano Polanco, C.A.; Rojas Garcia, M.C.; et al. Brote urbano de leishmaniasis visceral en Neiva (Huila), 2012. Revista de Salud Pública 2015, 17, 514–527. [Google Scholar] [CrossRef]
- Picón, Y.; Almario, G.; Rodríguez, V.; Garcia, N.V. Seroprevalence, clinical, and pathological characteristics of canine leishmaniasis in a central region of Colombia. J Vet Res 2020, 64, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Arbeláez, N.; Moreno, J.; Murillo, J.; Montoya, A.; Robledo, S.M.; Vélez, A.; Vélez, I.D. First Report of an Urban Case of Canine Visceral Leishmaniasis in the Municipality of Cali, Colombia. Am J Trop Med Hyg 2020, 102, 289–293. [Google Scholar] [CrossRef]
- Rueda-Concha, K.L.; Payares-Mercado, A.; Guerra-Castillo, J.; Melendrez, J.; Arroyo-Munive, Y.; Martínez-Abad, L.; Cochero, S.; Bejarano, E.E.; Paternina, L.E. Circulación de Leishmania infantum y Trypanosoma cruzi en perros domésticos de áreas urbanas de Sincelejo, región Caribe de Colombia. Biomédica 2022, 42, 633–649. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Ramírez, R.D.; Lugo-Vargas, R.; Petano-Duque, J.M.; Cruz-Méndez, J.S.; Rondón-Barragán, I.S. First study on microscopic and molecular detection of Acanthocheilonema reconditum and Leishmania infantum coinfection in dogs in Southwest Colombia. Vet World 2023, 16, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Medkour, H.; Davoust, B.; Dulieu, F.; Maurizi, L.; Lamour, T.; Marié, J.-L.; Mediannikov, O. Potential animal reservoirs (dogs and bats) of human visceral leishmaniasis due to Leishmania infantum in French Guiana. PLoS Negl Trop Dis 2019, 13, e0007456. [Google Scholar] [CrossRef] [PubMed]
- Rivas, A.K.; Alcover, M.M.; Martínez-Orellana, P.; Montserrat-Sangrà, S.; Nachum-Biala, Y.; Fisa, R.; Riera, C.; Baneth, G.; Solano-Gallego, L. Serological and molecular survey of Leishmania infection in dogs from Venezuela. Vet Parasitol Reg Stud Reports 2020, 21, 100420. [Google Scholar] [CrossRef] [PubMed]
- Segura, G.B.R.; Ochoa, W.H.S.; Matta, V.L.R. da; Martínez, M.; Tercero, C.R.; Gonzalez, R.R.; Pacheco, C.M.S.; Flores, G.V.A.; Silveira, F.T.; Henriquez, M.M.R.; et al. Can domestic dogs be considered a good reservoir of Leishmania (L.) infantum chagasi in an endemic area of nonulcerated cutaneous leishmaniasis in Southern Honduras? Rev Inst Med Trop Sao Paulo 2023, 65, e24. [Google Scholar] [CrossRef]
- Maia-Elkhoury, A.N.S.; Alves, W.A.; Sousa-Gomes, M.L. de; Sena, J.M. de; Luna, E.A. Visceral leishmaniasis in Brazil: trends and challenges. Cad Saude Publica 2008, 24, 2941–2947. [Google Scholar] [CrossRef]
- Harhay, M.O.; Olliaro, P.L.; Costa, D.L.; Costa, C.H.N. Urban parasitology: visceral leishmaniasis in Brazil. Trends Parasitol 2011, 27, 403–409. [Google Scholar] [CrossRef]
- Silva, E.S.; Gontijo, C.M.; Pacheco, R.S.; Fiuza, V.O.; Brazil, R.P. Visceral Leishmaniasis in the Metropolitan Region of Belo Horizonte, State of Minas Gerais, Brazil. Mem Inst Oswaldo Cruz 2001, 96, 285–291. [Google Scholar] [CrossRef]
- Alves Souza, N.; Souza Leite, R.; de Oliveira Silva, S.; Groenner Penna, M.; Figueiredo Felicori Vilela, L.; Melo, M.N.; de Andrade, A.S.R. Detection of mixed Leishmania infections in dogs from an endemic area in Southeastern Brazil. Acta Trop 2019, 193, 12–17. [Google Scholar] [CrossRef]
- Guerra, J.A.O.; Barros, M.L.B.; Fé, N.F.; Guerra, M.V.F.; Castellon, E.; Paes, M.G.; Sherlock, Í.A. Leishmaniose visceral entre índios no Estado de Roraima, Brasil: Aspectos clínicoepidemiológicos de casos observados no período de 1989 a 1993. Rev Soc Bras Med Trop 2004, 37, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Furlan, M.B.G. Epidemia de leishmaniose visceral no município de Campo Grande-MS, 2002 a 2006. Epidemiologia e Serviços de Saúde 2010, 19, 15–24. [Google Scholar] [CrossRef]
- Dias, A.F.L.R.; Almeida, A.B.P.F.; Rodrigues, J.Y.; Nakazato, L.; Fujimori, M.; Sousa, V.R.F. Cytological and molecular detection of Leishmania spp. in different biological tissues of dogs in areas endemic for visceral leishmaniasis. Arq Bras Med Vet Zootec 2019, 71, 2103–2106. [Google Scholar] [CrossRef]
- Menegatti, J.A.; Oliveira Júnior, G.J.; Silva, L.C.F.; Oliveira, A.; Bica, D.L.C.; Santos, P.V.B.A.; Cunha Filho, L.F.C.; Lunardi, M. Fauna flebotomínica e soroprevalência para leishmaniose visceral canina em área urbana na região Centro-Oeste do Brasil. Arq Bras Med Vet Zootec 2020, 72, 1197–1205. [Google Scholar] [CrossRef]
- Steindel, M.; Menin, Á.; Evangelista, T.; Stoco, P.H.; Marlow, M.A.; Fleith, R.C.; Pilati, C.; Grisard, E.C. Outbreak of autochthonous canine visceral leishmaniasis in Santa Catarina, Brazil. Pesquisa Veterinária Brasileira 2013, 33, 490–496. [Google Scholar] [CrossRef]
- Rodrigues, A.C.M.; Melo, A.C.F.L.; Júnior, A.D.S.; Franco, S.O.; Rondon, F.C.M.; Bevilaqua, C.M.L. Epidemiologia da leishmaniose visceral no município de Fortaleza, Ceará. Pesquisa Veterinária Brasileira 2017, 37, 1119–1124. [Google Scholar] [CrossRef]
- Moreno, E.S.; Sabioni, L.A.; de Seixas, M.M.M.; de Souza Filho, J.A.; Marcelino, A.P.; Shimabukuro, P.H.F. Evidence of a sylvatic enzootic cycle of Leishmania infantum in the State of Amapá, Brazil. Rev Soc Bras Med Trop 2020, 53, e20190169. [Google Scholar] [CrossRef]
- Rocha, M.A.N.; Matos-Rocha, T.J.; Ribeiro, C.M.B.; Abreu, S.R.O. Epidemiological aspects of human and canine visceral leishmaniasis in State of Alagoas, Northeast, Brazil. Brazilian Journal of Biology 2018, 78, 609–614. [Google Scholar] [CrossRef]
- Queiroz, P.V.S.; Monteiro, G.R.G.; Macedo, V.P.S.; Rocha, M.A.C.; Batista, L.M.M.; Queiroz, J.W.; Jerônimo, S.M.B.; Ximenes, M.F.F.M. Canine visceral leishmaniasis in urban and rural areas of Northeast Brazil. Res Vet Sci 2009, 86, 267–273. [Google Scholar] [CrossRef]
- de Oliveira, A.C.; Figueiredo, F.B.; Silva, V.L.; Santos, F.N.; de Souza, M.B.; de Madeira, M.F.; Abrantes, T.R.; Périssé, A.R.S. CANINE VISCERAL LEISHMANIASIS CASE INVESTIGATION IN THE JACARE REGION OF NITEROI, RIO DE JANEIRO, BRAZIL. Rev Inst Med Trop Sao Paulo 2015, 57, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Riboldi, E.; Carvalho, F.; Romão, P.R.T.; Barcellos, R.B.; Bello, G.L.; Ramos, R.R.; de Oliveira, R.T.; Júnior, J.P.A.; Rossetti, M.L.; Dallegrave, E. Molecular Method Confirms Canine Leishmania Infection Detected by Serological Methods in Non-Endemic Area of Brazil. Korean J Parasitol 2018, 56, 11–19. [Google Scholar] [CrossRef] [PubMed]
- de Marzochi, M.C.A.; Coutinho, S.G.; Sabroza, P.C.; de Souza, M.A.; de de Souza, P.P.M.; Toledo, L.; Rangel Filho, F.B. Leishmaniose visceral canina no Rio de Janeiro - Brasil. Cad Saude Publica 1985, 1, 432–446. [Google Scholar] [CrossRef]
- Figueiredo, F.B.; de Barbosa Filho, C.J.L.; Schubach, E.Y.P.; Pereira, S.A.; Nascimento, L.D.; de Madeira, M.F. Relato de caso autóctone de leishmaniose visceral canina na zona sul do município do Rio de Janeiro. Rev Soc Bras Med Trop 2010, 43, 98–99. [Google Scholar] [CrossRef] [PubMed]
- Barboza, D.C.P.M.; Leal, D.C.; da Souza, B.M.P.S.; Carneiro, A.J.B.; de Gomes Neto, C.M.B.; de Alcântara, A.C.; da Julião, F.S.; de Moura, S.A.B.; Peralva, L.M.P.; Ferreira, F.; et al. Inquérito epidemiológico da leishmaniose visceral canina em três distritos sanitários do Município de Salvador, Bahia, Brasil. Rev. Bras. Saúde Prod. An. 2009, 10, 434–447. [Google Scholar]
- Tonini, M.A.L.; Lemos, E.M.; Reis, A.B.; Vital, W.C.; Dias, E.S.; Dietze, R. First description of autochthonous canine visceral leishmaniasis in the metropolitan region of Vitória, State of Espírito Santo, Brazil. Rev Soc Bras Med Trop 2012, 45, 754–756. [Google Scholar] [CrossRef] [PubMed]
- Costa, D.N.C.C.; Bermudi, P.M.M.B.; Rodas, L.A.C.; Nunes, C.M.; Hiramoto, R.M.; Tolezano, J.E.; Cipriano, R.S.; Cardoso, G.C.D.; Codeço, C.T.; Chiaravalloti-Neto, F. Human visceral leishmaniasis and relationship with vector and canine control measures. Rev Saude Publica 2018, 52, 92. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, T.F.; do Benitez, A.N.; da Sevá, A.P.; Okamura, L.H.; Galvão, A.B.; Gomes, J.F.; Bresciani, K.D.S.; Cardoso, T.C. Spatial and seroepidemiology of canine visceral leishmaniasis in an endemic Southeast Brazilian area. Rev Soc Bras Med Trop 2020, 53, e20190525. [Google Scholar] [CrossRef]
- Teixeira-Neto, R.G.; da Silva, E.S.; Nascimento, R.A.; Belo, V.S.; di de Oliveira, C.L.; Pinheiro, L.C.; Gontijo, C.M.F. Canine visceral leishmaniasis in an urban setting of Southeastern Brazil: an ecological study involving spatial analysis. Parasit Vectors 2014, 7, 485. [Google Scholar] [CrossRef]
- Barata, R.A.; Peixoto, J.C.; Tanure, A.; Gomes, M.E.; Apolinário, E.C.; Bodevan, E.C.; de Araújo, H.S.; Dias, E.S.; da Pinheiro, A.C. Epidemiology of Visceral Leishmaniasis in a Reemerging Focus of Intense Transmission in Minas Gerais State, Brazil. Biomed Res Int 2013, 2013, 1–6. [Google Scholar] [CrossRef]
- da Pinheiro, A.C.; da Costa, A.S.V.; de Oliveira, R.S.; Reis, M.L.C. Epidemiological aspects and spatial distribution of visceral leishmaniasis in Governador Valadares, Brazil, between 2008 and 2012. Rev Soc Bras Med Trop 2020, 53. [Google Scholar] [CrossRef] [PubMed]
- Brito, F.G.; Langoni, H.; da Silva, R.C.; de Rotondano, T.E.F.; de Melo, M.A.; da Paz, G.S. Canine visceral leishmaniasis in the Northeast Region of Brazil. Journal of Venomous Animals and Toxins including Tropical Diseases 2016, 22, 15. [Google Scholar] [CrossRef]
- Carvalho, A.G. de; Luz, J.G.G.; Rodrigues, L.D.; Dias, J.V.L.; Fontes, C.J.F. High seroprevalence and peripheral spatial distribution of visceral leishmaniasis among domestic dogs in an emerging urban focus in Central Brazil: a cross-sectional study. Pathog Glob Health 2018, 112, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Valadas, S.; Minervino, A.H.H.; Lima, V.M.F.; Soares, R.M.; Ortolani, E.L.; Gennari, S.M. Occurrence of antibodies anti-Neospora caninum, anti-Toxoplasma gondii, and anti-Leishmania chagasi in serum of dogs from Pará State, Amazon, Brazil. Parasitol Res 2010, 107, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Costa, D.N.C.C.; Blangiardo, M.; Rodas, L.A.C.; Nunes, C.M.; Hiramoto, R.M.; Tolezano, J.E.; Bonfietti, L.X.; Bermudi, P.M.M.; Cipriano, R.S.; Cardoso, G.C.D.; et al. Canine visceral leishmaniasis in Araçatuba, State of São Paulo, Brazil, and its relationship with characteristics of dogs and their owners: a cross-sectional and spatial analysis using a geostatistical approach. BMC Vet Res 2018, 14, 229. [Google Scholar] [CrossRef] [PubMed]
- Satragno, D.; Faral-Tello, P.; Canneva, B.; Verger, L.; Lozano, A.; Vitale, E.; Greif, G.; Soto, C.; Robello, C.; Basmadjián, Y. Autochthonous Outbreak and Expansion of Canine Visceral Leishmaniasis, Uruguay. Emerg Infect Dis 2017, 23, 536–538. [Google Scholar] [CrossRef]
- Gaskin, A.A.; Schantz, P.; Jackson, J.; Birkenheuer, A.; Tomlinson, L.; Gramiccia, M.; Levy, M.; Steurer, F.; Kollmar, E.; Hegarty, B.C.; et al. Visceral Leishmaniasis in a New York Foxhound Kennel. J Vet Intern Med 2002, 16, 34. [Google Scholar] [CrossRef]
- Schantz, P.M.; Steurer, F.J.; Duprey, Z.H.; Kurpel, K.P.; Barr, S.C.; Jackson, J.E.; Breitschwerdt, E.B.; Levy, M.G.; Fox, J.C. Autochthonous visceral leishmaniasis in dogs in North America. J Am Vet Med Assoc 2005, 226, 1316–1322. [Google Scholar] [CrossRef]
- Duprey, Z.H.; Steurer, F.J.; Rooney, J.A.; Kirchhoff, L.V.; Jackson, J.E.; Rowton, E.D.; Schantz, P.M. Canine Visceral Leishmaniasis, United States and Canada, 2000–2003. Emerg Infect Dis 2006, 12, 440–446. [Google Scholar] [CrossRef]
- Gibson-Corley, K.N.; Hostetter, J.M.; Hostetter, S.J.; Mullin, K.; Ramer-Tait, A.E.; Boggiatto, P.M.; Petersen, C.A. Disseminated Leishmania infantum infection in two sibling foxhounds due to possible vertical transmission. Can Vet J 2008, 49, 1005–1008. [Google Scholar]
- Petersen, C.A. Leishmaniasis, an Emerging Disease Found in Companion Animals in the United States. Top Companion Anim Med 2009, 24, 182–188. [Google Scholar] [CrossRef]
- Boggiatto, P.M.; Gibson-Corley, K.N.; Metz, K.; Gallup, J.M.; Hostetter, J.M.; Mullin, K.; Petersen, C.A. Transplacental Transmission of Leishmania infantum as a Means for Continued Disease Incidence in North America. PLoS Negl Trop Dis 2011, 5, e1019. [Google Scholar] [CrossRef]
- Gin, T.E.; Lashnits, E.; Wilson, J.M.; Breitschwerdt, E.B.; Qurollo, B. Demographics and travel history of imported and autochthonous cases of leishmaniosis in dogs in the United States and Canada, 2006 to 2019. J Vet Intern Med 2021, 35, 954–964. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.Z.; Kovalenko, D.A.; Kuhls, K.; Nasyrova, R.M.; Ponomareva, V.I.; Fatullaeva, A.A.; Razakov, S.A.; Schnur, L.F.; Schönian, G. Identification of the agent causing visceral leishmaniasis in Uzbeki and Tajiki foci by analysing parasite DNA extracted from patients’ Giemsa-stained tissue preparations. Parasitology 2009, 136, 981–986. [Google Scholar] [CrossRef] [PubMed]
- Akter, S.; Alam, M.Z.; Nakao, R.; Yasin, G.; Kato, H.; Katakura, K. Molecular and Serological Evidence of Leishmania Infection in Stray Dogs from Visceral Leishmaniasis–Endemic Areas of Bangladesh. Am J Trop Med Hyg 2016, 95, 795–799. [Google Scholar] [CrossRef]
- Karunaweera, N.D.; Ferreira, M.U. Leishmaniasis: current challenges and prospects for elimination with special focus on the South Asian region. Parasitology 2018, 145, 425–429. [Google Scholar] [CrossRef]
- Sharifi, I.; Aflatoonian, M.R.; Daei Parizi, M.H.; Hosseininasab, A.; Mostafavi, M.; Bamorovat, M.; Aghaei Afshar, A.; Mohebali, M.; Keshavarz, H.; Daneshvar, H.; et al. Visceral Leishmaniasis in Southeastern Iran: A Narrative Review. Iran J Parasitol 2017, 12, 1–11. [Google Scholar]
- Dalimi, A.; Mohammadiha, A.; Mohebali, M.; Mirzaei, A.; Mahmoudi, M. Molecular Identification and Intra-Species Variations among Leishmania infantum Isolated from Human and Canine Visceral Leishmaniasis in Iran. Iran J Parasitol 2018, 13, 567–576. [Google Scholar] [PubMed]
- Baneth, G.; Dank, G.; Keren-Kornblatt, E.; Sekeles, E.; Adini, I.; Eisenberger, C.L.; Schnur, L.F.; King, R.; Jaffe, C.L. Emergence of visceral leishmaniasis in Central Israel. Am J Trop Med Hyg 1998, 59, 722–725. [Google Scholar] [CrossRef] [PubMed]
- Nasereddin, A.; Baneth, G.; Schönian, G.; Kanaan, M.; Jaffe, C.L. Molecular Fingerprinting of Leishmania infantum Strains Following an Outbreak of Visceral Leishmaniasis in Central Israel. J Clin Microbiol 2005, 43, 6054–6059. [Google Scholar] [CrossRef]
- Hamarsheh, O.; Nasereddin, A.; Damaj, S.; Sawalha, S.; Al-Jawabreh, H.; Azmi, K.; Amro, A.; Ereqat, S.; Abdeen, Z.; Al-Jawabreh, A. Serological and molecular survey of Leishmania parasites in apparently healthy dogs in the West Bank, Palestine. Parasit Vectors 2012, 5, 183. [Google Scholar] [CrossRef] [PubMed]
- Baneth, G.; Nachum-Biala, Y.; Adamsky, O.; Gunther, I. Leishmania tropica and Leishmania infantum infection in dogs and cats in Central Israel. Parasit Vectors 2022, 15, 147. [Google Scholar] [CrossRef] [PubMed]
- Ozbel, Y.; Oskam, L.; Ozensoy, S.; Turgay, N.; Alkan, M.Z.; Jaffe, C.L.; Ozcel, M.A. A survey on canine leishmaniasis in western Turkey by parasite, DNA and antibody detection assays. Acta Trop 2000, 74, 1–6. [Google Scholar] [CrossRef]
- Toz, S.O.; Culha, G.; Zeyrek, F.Y.; Ertabaklar, H.; Alkan, M.Z.; Vardarlı, A.T.; Gunduz, C.; Ozbel, Y. A Real-Time ITS1-PCR Based Method in the Diagnosis and Species Identification of Leishmania Parasite from Human and Dog Clinical Samples in Turkey. PLoS Negl Trop Dis 2013, 7, e2205. [Google Scholar] [CrossRef]
- Koenhemsi, L.; Fabrizio, V.; Mariella, P.; Antonella, M.; Or, E. Seroprevalence of Leishmaniosis Among Healthy Dogs in Istanbul. Israel Journal of Veterinary Medicine 2020, 75. [Google Scholar]
- Strelkova, M.V.; Ponirovsky, E.N.; Morozov, E.N.; Zhirenkina, E.N.; Razakov, S.A.; Kovalenko, D.A.; Schnur, L.F.; Schönian, G. A narrative review of visceral leishmaniasis in Armenia, Azerbaijan, Georgia, Kazakhstan, Kyrgyzstan, Tajikistan, Turkmenistan, Uzbekistan, the Crimean Peninsula and Southern Russia. Parasit Vectors 2015, 8, 330. [Google Scholar] [CrossRef] [PubMed]
- Sundar, S.; Mondal, D.; Rijal, S.; Bhattacharya, S.; Ghalib, H.; Kroeger, A.; Boelaert, M.; Desjeux, P.; Richter-Airijoki, H.; Harms, G. Implementation research to support the initiative on the elimination of kala azar from Bangladesh, India and Nepal - the challenges for diagnosis and treatment. Tropical Medicine & International Health 2008, 13, 2–5. [Google Scholar] [CrossRef]
- Jambulingam, P.; Pradeep Kumar, N.; Nandakumar, S.; Paily, K.P.; Srinivasan, R. Domestic dogs as reservoir hosts for Leishmania donovani in the southernmost Western Ghats in India. Acta Trop 2017, 171, 64–67. [Google Scholar] [CrossRef]
- Díaz-Regañón, D.; Agulla, B.; Piya, B.; Fernández-Ruiz, N.; Villaescusa, A.; García-Sancho, M.; Rodríguez-Franco, F.; Sainz, Á. Stray dogs in Nepal have high prevalence of vector-borne pathogens: a molecular survey. Parasit Vectors 2020, 13, 174. [Google Scholar] [CrossRef]
- Rab, M.A.; Frame, I.A.; Evans, D.A. The role of dogs in the epidemiology of human visceral leishmaniasis in northern Pakistan. Trans R Soc Trop Med Hyg 1995, 89, 612–615. [Google Scholar] [CrossRef]
- Alam, M.Z.; Yasin, G.; Kato, H.; Sakurai, T.; Katakura, K. PCR-Based Detection of Leishmania donovani DNA in a Stray Dog from a Visceral Leishmaniasis Endemic Focus in Bangladesh. J Vet Med Sci 2013, 75, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Hossen, M.A. DETECTION OF LEISHMANIA INFECTION IN STRAY DOGS IN HUMAN LEISHMANIASIS ENDEMIC AREA IN MYMENSINGH DISTRICT WITH ITS POSSIBLE PUBLIC HEALTH SIGNIFICANCE IN BANGLADESH. Journal of Veterinary Medical and One Health Research 2019, 1, 99–109. [Google Scholar] [CrossRef]
- Shang, L.; Peng, W.; Jin, H.; Xu, D.; Zhong, N.; Wang, W.; Wu, Y.; Liu, Q. The prevalence of canine Leishmania infantum infection in Sichuan Province, southwestern China detected by real time PCR. Parasit Vectors 2011, 4, 173. [Google Scholar] [CrossRef]
- Wang, J.-Y.; Ha, Y.; Gao, C.-H.; Wang, Y.; Yang, Y.-T.; Chen, H.-T. The prevalence of canine Leishmania infantum infection in western China detected by PCR and serological tests. Parasit Vectors 2011, 4, 69. [Google Scholar] [CrossRef]
- Sandy, J.; Matthews, A.; Nachum-Biala, Y.; Baneth, G. First Report of Autochthonous Canine Leishmaniasis in Hong Kong. Microorganisms 2022, 10, 1873. [Google Scholar] [CrossRef]
- Colella, V.; Nguyen, V.L.; Tan, D.Y.; Lu, N.; Fang, F.; Zhijuan, Y.; Wang, J.; Liu, X.; Chen, X.; Dong, J.; et al. Zoonotic Vectorborne Pathogens and Ectoparasites of Dogs and Cats in Eastern and Southeast Asia. Emerg Infect Dis 2020, 26, 1221–1233. [Google Scholar] [CrossRef]
- Dujardin, J.-C.; Campino, L.; Cañavate, C.; Dedet, J.-P.; Gradoni, L.; Soteriadou, K.; Mazeris, A.; Ozbel, Y.; Boelaert, M. Spread of Vector-Borne Diseases and Neglect of Leishmaniasis, Europe. Emerg Infect Dis 2008, 14, 1013–1018. [Google Scholar] [CrossRef]
- Velo, E.; Bongiorno, G.; Kadriaj, P.; Myrseli, T.; Crilly, J.; Lika, A.; Mersini, K.; Di Muccio, T.; Bino, S.; Gramiccia, M.; et al. The current status of phlebotomine sand flies in Albania and incrimination of Phlebotomus neglectus (Diptera, Psychodidae) as the main vector of Leishmania infantum. PLoS One 2017, 12, e0179118. [Google Scholar] [CrossRef]
- Colella, V.; Hodžić, A.; Iatta, R.; Baneth, G.; Alić, A.; Otranto, D. Zoonotic Leishmaniasis, Bosnia and Herzegovina. Emerg Infect Dis 2019, 25, 385–386. [Google Scholar] [CrossRef]
- Živičnjak, T.; Martinković, F.; Marinculić, A.; Mrljak, V.; Kučer, N.; Matijatko, V.; Mihaljević, Ž.; Barić-Rafaj, R. A seroepidemiologic survey of canine visceral leishmaniosis among apparently healthy dogs in Croatia. Vet Parasitol 2005, 131, 35–43. [Google Scholar] [CrossRef]
- Živičnjak, T.; Martinković, F.; Khoury, C.; Bongiorno, G.; Bosnić, S.; Lukačević, D.; Maroli, M. Serological and entomological studies of canine leishmaniosis in Croatia. Vet Arh 2011, 81, 99–110. [Google Scholar]
- Deplazes, P.; Grimm, F.; Papaprodromou, M.; Cavaliero, T.; Gramiccia, M.; Christofi, G.; Christofi, N.; Economides, P.; Eckert, J. Canine leishmaniosis in Cyprus due to Leishmania infantum MON 1. Acta Trop 1998, 71, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Mazeris, A.; Soteriadou, K.; Dedet, J.P.; Haralambous, C.; Tsatsaris, A.; Moschandreas, J.; Messaritakis, I.; Christodoulou, V.; Papadopoulos, B.; Ivović, V.; et al. Leishmaniases and the Cyprus Paradox. Am J Trop Med Hyg 2010, 82, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Ruh, E.; Taylan Ozkan, A. Leishmaniasis in Northern Cyprus. European Journal of Therapeutics 2019, 25, 1–5. [Google Scholar] [CrossRef]
- Chamaillé, L.; Tran, A.; Meunier, A.; Bourdoiseau, G.; Ready, P.; Dedet, J.-P. Environmental risk mapping of canine leishmaniasis in France. Parasit Vectors 2010, 3, 31. [Google Scholar] [CrossRef]
- Pomares, C.; Marty, P.; Bañuls, A.L.; Lemichez, E.; Pratlong, F.; Faucher, B.; Jeddi, F.; Moore, S.; Michel, G.; Aluru, S.; et al. Genetic Diversity and Population Structure of Leishmania infantum from Southeastern France: Evaluation Using Multi-Locus Microsatellite Typing. PLoS Negl Trop Dis 2016, 10, e0004303. [Google Scholar] [CrossRef] [PubMed]
- Lachaud, L.; Chabbert, E.; Dubessay, P.; Dereure, J.; Lamothe, J.; Dedet, J.-P.; Bastien, P. Value of two PCR methods for the diagnosis of canine visceral leishmaniasis and the detection of asymptomatic carriers. Parasitology 2002, 125, 197–207. [Google Scholar] [CrossRef]
- Aoun, O.; Mary, C.; Roqueplo, C.; Marié, J.-L.; Terrier, O.; Levieuge, A.; Davoust, B. Canine leishmaniasis in south-east of France: screening of Leishmania infantum antibodies (western blotting, ELISA) and parasitaemia levels by PCR quantification. Vet Parasitol 2009, 166, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Le Rutte, E.A.; van der Wilt, L.S.; Bulstra, C.A.; Nieboer, D.; Kontoroupis, P.; de Vlas, S.J.; Richardus, J.H. Incidence and geographical distribution of canine leishmaniosis in 2016—2017 in Spain and France. Vet Parasitol Reg Stud Reports 2021, 25, 100613. [Google Scholar] [CrossRef]
- Ntais, P.; Sifaki-Pistola, D.; Christodoulou, V.; Messaritakis, I.; Pratlong, F.; Poupalos, G.; Antoniou, M. Leishmaniases in Greece. Am J Trop Med Hyg 2013, 89, 906–915. [Google Scholar] [CrossRef]
- Symeonidou, I.; Angelou, A.; Theodoridis, A.; Sioutas, G.; Papadopoulos, E. Canine Leishmaniosis in Greece: An Updated Countrywide Serological Study and Associated Risk Factors. Pathogens 2021, 10, 1129. [Google Scholar] [CrossRef]
- Tamponi, C.; Scarpa, F.; Carta, S.; Knoll, S.; Sanna, D.; Gai, C.; Pipia, A.P.; Dessì, G.; Casu, M.; Varcasia, A.; et al. Seroprevalence and risk factors associated with Leishmania infantum in dogs in Sardinia (Italy), an endemic island for leishmaniasis. Parasitol Res 2021, 120, 289–300. [Google Scholar] [CrossRef]
- Orndorff, G.R.; Cooper, B.A.; Smith, W.; Ryan, J.R. Canine Visceral Leishmaniasis in Sicily. Mil Med 2000, 165, 29–32. [Google Scholar] [CrossRef]
- Lisi, O.; D’Urso, V.; Vaccalluzzo, V.; Bongiorno, G.; Khoury, C.; Severini, F.; Di Muccio, T.; Gramiccia, M.; Gradoni, L.; Maroli, M. Persistence of phlebotomine Leishmania vectors in urban sites of Catania (Sicily, Italy). Parasit Vectors 2014, 7, 560. [Google Scholar] [CrossRef] [PubMed]
- Foglia Manzillo, V.; Gizzarelli, M.; Vitale, F.; Montagnaro, S.; Torina, A.; Sotera, S.; Oliva, G. Serological and entomological survey of canine leishmaniasis in Lampedusa island, Italy. BMC Vet Res 2018, 14, 286. [Google Scholar] [CrossRef]
- Sauda, F.; Malandrucco, L.; Macrì, G.; Scarpulla, M.; De Liberato, C.; Terracciano, G.; Fichi, G.; Berrilli, F.; Perrucci, S. Leishmania infantum, Dirofilaria spp. and other endoparasite infections in kennel dogs in central Italy. Parasite 2018, 25, 2. [Google Scholar] [CrossRef] [PubMed]
- De Massis, F.; Ippoliti, C.; Iannetti, S.; Tittarelli, M.; Pelini, S.; Giansante, D.; Ciarrocchi, A. Canine Leishmaniasis: Serological Results in Private and Kennel Dogs Tested over a Six-Year Period (2009–2014) in Abruzzo and Molise Regions, Italy. Microorganisms 2020, 8, 1915. [Google Scholar] [CrossRef] [PubMed]
- Mendoza-Roldan, J.; Benelli, G.; Panarese, R.; Iatta, R.; Furlanello, T.; Beugnet, F.; Zatelli, A.; Otranto, D. Leishmania infantum and Dirofilaria immitis infections in Italy, 2009–2019: changing distribution patterns. Parasit Vectors 2020, 13, 193. [Google Scholar] [CrossRef] [PubMed]
- Ferroglio, E.; Maroli, M.; Gastaldo, S.; Mignone, W.; Rossi, L. Canine Leishmaniasis, Italy. Emerg Infect Dis 2005, 11, 1618–1620. [Google Scholar] [CrossRef]
- Baldelli, R.; Piva, S.; Salvatore, D.; Parigi, M.; Melloni, O.; Tamba, M.; Bellini, R.; Poglayen, G. Canine leishmaniasis surveillance in a northern Italy kennel. Vet Parasitol 2011, 179, 57–61. [Google Scholar] [CrossRef]
- Santi, A.; Renzi, M.; Baldelli, R.; Calzolari, M.; Caminiti, A.; Dell’Anna, S.; Galletti, G.; Lombardini, A.; Paternoster, G.; Tamba, M. A Surveillance Program on Canine Leishmaniasis in the Public Kennels of Emilia-Romagna Region, Northern Italy. Vector-Borne and Zoonotic Diseases 2014, 14, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Moirano, G.; Zanet, S.; Giorgi, E.; Battisti, E.; Falzoi, S.; Acquaotta, F.; Fratianni, S.; Richiardi, L.; Ferroglio, E.; Maule, M. Integrating environmental, entomological, animal, and human data to model the Leishmania infantum transmission risk in a newly endemic area in Northern Italy. One Health 2020, 10, 100159. [Google Scholar] [CrossRef] [PubMed]
- Salvatore, D.; Di Francesco, A.; Parigi, M.; Poglayen, G.; Battistini, M.; Baldelli, R. Programma di sorveglianza della leishmaniosi canina in un canile della Repubblica di San Marino. Vet Ital 2013, 49, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Headington, C.E.; Barbara, C.H.; Lambson, B.E.; Hart, D.T.; Barker, D.C. Diagnosis of leishmaniasis in Maltese dogs with the aid of the polymerase chain reaction. Trans R Soc Trop Med Hyg 2002, 96, S195–S197. [Google Scholar] [CrossRef]
- Cardoso, L.; Mendão, C.; Madeira de Carvalho, L. Prevalence of Dirofilaria immitis, Ehrlichia canis, Borrelia burgdorferi sensu Lato, Anaplasma spp. and Leishmania infantum in apparently healthy and CVBD-suspect dogs in Portugal - a national serological study. Parasit Vectors 2012, 5, 62. [Google Scholar] [CrossRef]
- Maia, C.; Dionisio, L.; Afonso, M.O.; Neto, L.; Cristovao, J.M.; Campino, L. Leishmania infection and host-blood feeding preferences of phlebotomine sandflies and canine leishmaniasis in an endemic European area, the Algarve Region in Portugal. Mem Inst Oswaldo Cruz 2013, 108, 481–487. [Google Scholar] [CrossRef]
- Maia, C.; Coimbra, M.; Ramos, C.; Cristóvão, J.; Cardoso, L.; Campino, L. Serological investigation of Leishmania infantum, Dirofilaria immitis and Angiostrongylus vasorum in dogs from southern Portugal. Parasit Vectors 2015, 8, 152. [Google Scholar] [CrossRef] [PubMed]
- Schallig, H.D.; Cardoso, L.; Semião-Santos, S.J. Seroepidemiology of canine leishmaniosis in Évora (southern Portugal): 20-Year Trends. Parasit Vectors 2013, 6, 100. [Google Scholar] [CrossRef]
- Maia, C.; Altet, L.; Serrano, L.; Cristóvão, J.M.; Tabar, M.D.; Francino, O.; Cardoso, L.; Campino, L.; Roura, X. Molecular detection of Leishmania infantum, filariae and Wolbachia spp. in dogs from southern Portugal. Parasit Vectors 2016, 9, 170. [Google Scholar] [CrossRef]
- Maia, C.; Alwassouf, S.; Cristóvão, J.M.; Ayhan, N.; Pereira, A.; Charrel, R.N.; Campino, L. Serological association between Leishmania infantum and sand fly fever Sicilian (but not Toscana) virus in sheltered dogs from southern Portugal. Parasit Vectors 2017, 10, 92. [Google Scholar] [CrossRef]
- Almeida, M.; Maia, C.; Cristóvão, J.M.; Morgado, C.; Barbosa, I.; Ibars, R.F.; Campino, L.; Gonçalves, L.; Cortes, S. Seroprevalence and Risk Factors Associated with Leishmania Infection in Dogs from Portugal. Microorganisms 2022, 10, 2262. [Google Scholar] [CrossRef] [PubMed]
- Montoya-Alonso, J.A.; Morchón, R.; Costa-Rodríguez, N.; Matos, J.I.; Falcón-Cordón, Y.; Carretón, E. Current Distribution of Selected Vector-Borne Diseases in Dogs in Spain. Front Vet Sci 2020, 7. [Google Scholar] [CrossRef] [PubMed]
- Gálvez, R.; Montoya, A.; Cruz, I.; Fernández, C.; Martín, O.; Checa, R.; Chicharro, C.; Migueláñez, S.; Marino, V.; Miró, G. Latest trends in Leishmania infantum infection in dogs in Spain, Part I: mapped seroprevalence and sand fly distributions. Parasit Vectors 2020, 13, 204. [Google Scholar] [CrossRef]
- Montoya, A.; Gálvez, R.; Checa, R.; Sarquis, J.; Plaza, A.; Barrera, J.P.; Marino, V.; Miró, G. Latest trends in L. infantum infection in dogs in Spain, Part II: current clinical management and control according to a national survey of veterinary practitioners. Parasit Vectors 2020, 13, 205. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Regañón, D.; Roura, X.; Suárez, M.L.; León, M.; Sainz, Á. Serological evaluation of selected vector-borne pathogens in owned dogs from northern Spain based on a multicenter study using a commercial test. Parasit Vectors 2020, 13, 301. [Google Scholar] [CrossRef]
- Tsatchev, I.; Kyriazis, I.D.; Boutsini, S.; Karagouni, E.; Dotsika, E. First report of canine visceral leishmaniasis in Bulgaria. Turk J Vet Anim Sci 2010, 34, 465–469. [Google Scholar] [CrossRef]
- Babuadze, G.; Alvar, J.; Argaw, D.; de Koning, H.P.; Iosava, M.; Kekelidze, M.; Tsertsvadze, N.; Tsereteli, D.; Chakhunashvili, G.; Mamatsashvili, T.; et al. Epidemiology of Visceral Leishmaniasis in Georgia. PLoS Negl Trop Dis 2014, 8, e2725. [Google Scholar] [CrossRef] [PubMed]
- Babuadze, G.; Farlow, J.; de Koning, H.P.; Carrillo, E.; Chakhunashvili, G.; Murskvaladze, M.; Kekelidze, M.; Karseladze, I.; Kokaia, N.; Kalandadze, I.; et al. Seroepidemiology and molecular diversity of Leishmania donovani complex in Georgia. Parasit Vectors 2016, 9, 279. [Google Scholar] [CrossRef]
- Miró, G.; Wright, I.; Michael, H.; Burton, W.; Hegarty, E.; Rodón, J.; Buch, J.; Pantchev, N.; von Samson-Himmelstjerna, G. Seropositivity of main vector-borne pathogens in dogs across Europe. Parasit Vectors 2022, 15, 189. [Google Scholar] [CrossRef]
- Tánczos, B.; Balogh, N.; Király, L.; Biksi, I.; Szeredi, L.; Gyurkovsky, M.; Scalone, A.; Fiorentino, E.; Gramiccia, M.; Farkas, R. First Record of Autochthonous Canine Leishmaniasis in Hungary. Vector-Borne and Zoonotic Diseases 2012, 12, 588–594. [Google Scholar] [CrossRef]
- Xhekaj, B.; Alishani, M.; Rexhepi, A.; Jakupi, X.; Sherifi, K. Serological survey of Canine leishmaniasis in Southwestern Region of Kosovo. Vet Ital 2020, 56, 47–50. [Google Scholar] [CrossRef]
- Tasić-Otašević, S.; Savić, S.; Jurhar-Pavlova, M.; Stefanovska, J.; Stalević, M.; Ignjatović, A.; Ranđelović, M.; Gajić, B.; Cvetkovikj, A.; Gabrielli, S. Molecular Survey of Dirofilaria and Leishmania Species in Dogs from Central Balkan. Animals 2022, 12, 911. [Google Scholar] [CrossRef]
- Mircean, V.; Dumitrache, M.O.; Mircean, M.; Bolfa, P.; Györke, A.; Mihalca, A.D. Autochthonous canine leishmaniasis in Romania: neglected or (re)emerging? Parasit Vectors 2014, 7, 135. [Google Scholar] [CrossRef] [PubMed]
- Dumitrache, M.O.; Nachum-Biala, Y.; Gilad, M.; Mircean, V.; Cazan, C.D.; Mihalca, A.D.; Baneth, G. The quest for canine leishmaniasis in Romania: the presence of an autochthonous focus with subclinical infections in an area where disease occurred. Parasit Vectors 2016, 9, 297. [Google Scholar] [CrossRef]
- Cîmpan, A.A.; Diakou, A.; Papadopoulos, E.; Miron, L.D. SEROLOGICAL STUDY OF EXPOSURE TO LEISHMANIA IN DOGS LIVING IN SHELTERS, IN SOUTH-EAST ROMANIA. Rev Rom Med Vet 2019, 29, 54–58. [Google Scholar]
- Cazan, C.D.; Ionică, A.M.; Matei, I.A.; D’Amico, G.; Muñoz, C.; Berriatua, E.; Dumitrache, M.O. Detection of Leishmania infantum DNA and antibodies against Anaplasma spp., Borrelia burgdorferi s.l. and Ehrlichia canis in a dog kennel in South-Central Romania. Acta Vet Scand 2020, 62, 42. [Google Scholar] [CrossRef] [PubMed]
- Kotnik, T. Dog leishmaniasis in Slovenia: a probable creation of the first enzootic focus - a case report. Vet Arh 2020, 90, 317–322. [Google Scholar] [CrossRef]
- McKenna, M.; Attipa, C.; Tasker, S.; Augusto, M. Leishmaniosis in a dog with no travel history outside of the UK. Veterinary Record 2019, 184, 441–441. [Google Scholar] [CrossRef]
- Bashaye, S.; Nombela, N.; Argaw, D.; Mulugeta, A.; Herrero, M.; Nieto, J.; Chicharro, C.; Cañavate, C.; Aparicio, P.; Vélez, I.D.; et al. Risk Factors for Visceral Leishmaniasis in a New Epidemic Site in Amhara Region, Ethiopia. Am J Trop Med Hyg 2009, 81, 34–39. [Google Scholar] [CrossRef]
- Kalayou, S.; Tadelle, H.; Bsrat, A.; Abebe, N.; Haileselassie, M.; Schallig, H.D.F.H. Serological Evidence of Leishmania donovani Infection in Apparently Healthy Dogs Using Direct Agglutination Test (DAT) and Rk39 Dipstick Tests in Kafta Humera, north-west Ethiopia. Transbound Emerg Dis 2011, 58, 255–262. [Google Scholar] [CrossRef]
- Kenubih, A.; Dagnachew, S.; Almaw, G.; Abebe, T.; Takele, Y.; Hailu, A.; Lemma, W. Preliminary survey of domestic animal visceral leishmaniasis and risk factors in north-west Ethiopia. Tropical Medicine & International Health 2015, 20, 205–210. [Google Scholar] [CrossRef]
- Rohousova, I.; Talmi-Frank, D.; Kostalova, T.; Polanska, N.; Lestinova, T.; Kassahun, A.; Yasur-Landau, D.; Maia, C.; King, R.; Votypka, J.; et al. Exposure to Leishmania spp. and sand flies in domestic animals in northwestern Ethiopia. Parasit Vectors 2015, 8, 360. [Google Scholar] [CrossRef] [PubMed]
- Bejano, S.; Shumie, G.; Kumar, A.; Asemahagn, E.; Damte, D.; Woldie, S.; Mulugeta, A.; Manaye, N.; Genetu, A.; Gadisa, E.; et al. Prevalence of asymptomatic visceral leishmaniasis in human and dog, Benishangul Gumuz regional state, western Ethiopia. Parasit Vectors 2021, 14, 39. [Google Scholar] [CrossRef]
- Gebremedhin, E.Z.; Weya, W.; Dima, C.; Zewde, D.; Lo Presti, V.D.M.; Vitale, M. High seroprevalence of Leishmania infantum infection in dogs and its associated risk factors in selected towns of Southwest and West Shewa zones of Oromia, Ethiopia. Vet Med Sci 2022, 8, 2319–2328. [Google Scholar] [CrossRef] [PubMed]
- Sharifdini, M.; Mohebali, M.; Keshavarz, H.; Hosseininejad, M.; Hajjaran, H.; Akhoundi, B.; Foroushani, A.R.; Zarei, Z.; Charehdar, S. Neospora caninum and Leishmania infantum Co-Infection in Domestic Dogs (Canis familiaris) in Meshkin-Shahr District, Northwestern Iran. Iran J Arthropod Borne Dis 2011, 1, 60–68. [Google Scholar]
- Moshfe, A.; Mohebali, M.; Afshoun, E.; Mousavizadeh, A.; Zarei, Z.; Abidi, H.; Akhoundi, B.; Barati, V.; Joukar, S. Canine Visceral Leishmaniasis in Boyer Ahmad District, Kohgiluyeh & Boyer Ahmad Province, Southwest of Iran. Iran J Parasitol 2012, 7, 75–81. [Google Scholar] [PubMed]
- Haddadzade, H.; Fattahi, R.; Mohebali, M.; Akhoundi, B.; Ebrahimzade, E. Seroepidemiologcal Investigation of Visceral Leishmaniasis in Stray and Owned Dogs in Alborz Province, Central Iran Using Direct Agglutination Test. Iran J Parasitol 2013, 8, 152–157. [Google Scholar]
- Sabzevari, S.; Razmi, G.R.; Naghibi, A.; Khoshnegah, J. A Serological study of Leishmania infantum in dogs of Khorasan Razavi province, Iran. Journal of Parasitic Diseases 2013, 37, 189–191. [Google Scholar] [CrossRef] [PubMed]
- Bamorovat, M.; Sharifi, I.; Mohammadi, M.A.; Fasihi Harandi, M.; Mohebali, M.; Malekpour Afshar, R.; Babaei, Z.; Ziaali, N.; Aflatoonian, M.R. Canine Visceral Leishmaniasis in Kerman, Southeast of Iran: A Seroepidemiological, Histopathological and Molecular Study. Iran J Parasitol 2014, 9, 342–349. [Google Scholar]
- Mahshid, M.; Baharak, A.; Iraj, S.; Sina, K.; Javad, K.; Mehdi, B. Seroprevalence of canine visceral leishmaniasis in southeast of Iran. Journal of Parasitic Diseases 2014, 38, 218–222. [Google Scholar] [CrossRef]
- Malmasi, A.; Janitabar, S.; Mohebali, M.; Akhoundi, B.; Maazi, N.; Aramoon, M.; Khorrami, N.; Seifi, H.A. Seroepidemiologic Survey of Canine Visceral Leishmaniasis in Tehran and Alborz Provinces of Iran. J Arthropod Borne Dis 2014, 8, 132–138. [Google Scholar] [PubMed]
- Barati, M.; Mohebali, M.; Alimohammadian, M.H.; Khamesipour, A.; Akhoundi, B.; Zarei, Z. Canine visceral leishmaniasis: seroprevalence survey of asymptomatic dogs in an endemic area of northwestern Iran. Journal of Parasitic Diseases 2015, 39, 221–224. [Google Scholar] [CrossRef] [PubMed]
- Gharekhani, J.; Heidari, H.; Hajian-Bidar, H.; Abbasi-Doulatshahi, E.; Edalati-Shokat, H. Prevalence of anti-Leishmania infantum antibodies in dogs from West of Iran. Journal of Parasitic Diseases 2016, 40, 964–967. [Google Scholar] [CrossRef] [PubMed]
- Afshar, M.J.A.; Sharifi, I.; Bamorovat, M.; Mohebali, M.; Bahreini, M.S.; Naderi, A. Canine Visceral Leishmaniasis; A Seroepidemiological Survey in Jiroft District, Southern Kerman Province, Southeastern Iran in 2015. Iran J Parasitol 2018, 13, 67–71. [Google Scholar]
- Heidari, A.; Mohebali, M.; Vahed, M.; Kabir, K.; Zarei, Z.; Akhoundi, B.; Elikaee, S.; Barati, H.; Sezavar, M.; Keshavarz, H.; et al. Molecular and Seroepidemiological Survey of Visceral Leishmaniasis in Owned Dogs (Canis familiaris) in New Foci of Rural Areas of Alborz Province, Central Part of Iran: A Cross-Sectional Study in 2017. J Arthropod Borne Dis 2020, 14, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Fakhar, M.; Derakhshani-nia, M.; Gohardehi, S.; Karamian, M.; Hezarjaribi, H.Z.; Mohebali, M.; Akhoundi, B.; Sharbatkhori, M. Domestic dogs carriers of Leishmania infantum, Leishmania Tropica and Crithidia Fasciculata as potential reservoirs for human visceral leishmaniasis in northeastern Iran. Vet Med Sci 2022, 8, 2329–2336. [Google Scholar] [CrossRef] [PubMed]
- Marcondes, M.; Rossi, C.N. Leishmaniose visceral no Brasil. Braz J Vet Res Anim Sci 2013, 50, 341–352. [Google Scholar] [CrossRef]
- Desjeux, P. The increase in risk factors for leishmaniasis worldwide. Trans R Soc Trop Med Hyg 2001, 95, 239–243. [Google Scholar] [CrossRef]
- Barbosa, I.R.; Carlota, F.C.; Andrade-Neto, V.F. de Seroepidemiological Survey of Canine Leishmania Infections from Peripheral Areas in Natal, Northeast Brazil. Open Microbiol J 2015, 9, 43–47. [Google Scholar] [CrossRef]
- Ready, P.D. Leishmaniasis emergence and climate change. Rev Sci Tech 2008, 27, 399–412. [Google Scholar] [CrossRef]
- El Omari, H.; Chahlaoui, A.; Talbi, F.Z.; El Mouhdi, K.; El Ouali Lalami, A. Impact of Climatic Factors on the Seasonal Fluctuation of Leishmaniasis Vectors in Central Morocco (Meknes Prefecture). Canadian Journal of Infectious Diseases and Medical Microbiology 2020, 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gramiccia, M.; Gradoni, L. The current status of zoonotic leishmaniases and approaches to disease control. Int J Parasitol 2005, 35, 1169–1180. [Google Scholar] [CrossRef]
- Ready, P.D. Leishmaniasis emergence in Europe. Euro Surveill 2010, 15, 19505. [Google Scholar] [CrossRef] [PubMed]
- Koch, L.K.; Kochmann, J.; Klimpel, S.; Cunze, S. Modeling the climatic suitability of leishmaniasis vector species in Europe. Sci Rep 2017, 7, 13325. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, A.Y.M.; Dewan, A.; Shogib, M.R.I.; Rahman, M.M.; Hossain, M.F. Environmental factors associated with the distribution of visceral leishmaniasis in endemic areas of Bangladesh: modeling the ecological niche. Trop Med Health 2017, 45, 13. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, C.V.B.; da Sevá, A. P.; Werneck, G.L.; Struchiner, C.J. Does deforestation drive visceral leishmaniasis transmission? A causal analysis. Proceedings of the Royal Society B: Biological Sciences 2021, 288, 20211537. [Google Scholar] [CrossRef]
- El-Sayed, A.; Kamel, M. Climatic changes and their role in emergence and re-emergence of diseases. Environmental Science and Pollution Research 2020, 27, 22336–22352. [Google Scholar] [CrossRef]
- Al-Salem, W.; Herricks, J.R.; Hotez, P.J. A review of visceral leishmaniasis during the conflict in South Sudan and the consequences for East African countries. Parasit Vectors 2016, 9, 460. [Google Scholar] [CrossRef] [PubMed]
- Sunyoto, T.; Potet, J.; Boelaert, M. Visceral leishmaniasis in Somalia: A review of epidemiology and access to care. PLoS Negl Trop Dis 2017, 11, e0005231. [Google Scholar] [CrossRef]
- Carvalho, A.G. de; Luz, J.G.G.; Rodrigues, L.D.; Dias, J.V.L.; Fontes, C.J.F. High seroprevalence and peripheral spatial distribution of visceral leishmaniasis among domestic dogs in an emerging urban focus in central Brazil: a cross-sectional study. Pathog Glob Health 2018, 112, 29–36. [Google Scholar] [CrossRef]
- Carvalho, A.G.; Luz, J.G.G.; Rodrigues, L.D.; Dias, J.V.L.; Fontes, C.J.F. Factors associated with Leishmania spp. infection in domestic dogs from an emerging area of high endemicity for visceral leishmaniasis in Central-Western Brazil. Res Vet Sci 2019, 125, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Luz, J.G.G.; Carvalho, A.G.; Naves, D.B.; Dias, J.V.L.; Fontes, C.J.F. Are backyard characteristics relevant factors for the occurrence of human visceral leishmaniasis in Central-Western Brazil? Trans R Soc Trop Med Hyg 2020, 114, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, A.I.P.; Silva, D.M.; de Freitas, L.R.S.; Romero, G.A.S. A cross-sectional approach including dog owner characteristics as predictors of visceral leishmaniasis infection in dogs. Mem Inst Oswaldo Cruz 2020, 115. [Google Scholar] [CrossRef]
- Cortes, S.; Afonso, M.O.; Alves-Pires, C.; Campino, L. Stray Dogs and Leishmaniasis in Urban Areas, Portugal. Emerg Infect Dis 2007, 13, 1431–1432. [Google Scholar] [CrossRef] [PubMed]
- Martín-Sánchez, J.; Morales-Yuste, M.; Acedo-Sánchez, C.; Barón, S.; Díaz, V.; Morillas-Márquez, F. Canine Leishmaniasis in Southeastern Spain. Emerg Infect Dis 2009, 15, 795–798. [Google Scholar] [CrossRef] [PubMed]
- Coura-Vital, W.; Marques, M.J.; Veloso, V.M.; Roatt, B.M.; de Aguiar-Soares, R.D.O.; Reis, L.E.S.; Braga, S.L.; Morais, M.H.F.; Reis, A.B.; Carneiro, M. Prevalence and Factors Associated with Leishmania infantum Infection of Dogs from an Urban Area of Brazil as Identified by Molecular Methods. PLoS Negl Trop Dis 2011, 5, e1291. [Google Scholar] [CrossRef]
- Melo, S.N.; Teixeira-Neto, R.G.; Werneck, G.L.; Struchiner, C.J.; Ribeiro, R.A.N.; Sousa, L.R.; de Melo, M.O.G.; Carvalho Júnior, C.G.; Penaforte, K.M.; Manhani, M.N.; et al. Prevalence of visceral leishmaniasis in a population of free-roaming dogs as determined by multiple sampling efforts: a longitudinal study analyzing the effectiveness of euthanasia. Prev Vet Med 2018, 161, 19–24. [Google Scholar] [CrossRef]
- Werneck, G.L.; Costa, C.H.N.; Walker, A.M.; David, J.R.; Wand, M.; Maguire, J.H. Multilevel modelling of the incidence of visceral leishmaniasis in Teresina, Brazil. Epidemiol Infect 2007, 135, 195–201. [Google Scholar] [CrossRef]
- Araújo, V.E.M. de; Pinheiro, L.C.; de Almeida, M.C.M.; de Menezes, F.C.; Morais, M.H.F.; Reis, I.A.; Assunção, R.M.; Carneiro, M. Relative Risk of Visceral Leishmaniasis in Brazil: A Spatial Analysis in Urban Area. PLoS Negl Trop Dis 2013, 7, e2540. [Google Scholar] [CrossRef]
- Leite, B.M.M.; da Solcà, M.S.; Santos, L.C.S.; Coelho, L.B.; Amorim, L.D.A.F.; Donato, L.E.; de Passos, S.M.S.; de Almeida, A.O.; Veras, P.S.T.; Fraga, D.B.M. The mass use of deltamethrin collars to control and prevent canine visceral leishmaniasis: A field effectiveness study in a highly endemic area. PLoS Negl Trop Dis 2018, 12, e0006496. [Google Scholar] [CrossRef]
- Oliveira, C.D.L.; Assunção, R.M.; Reis, I.A.; Proietti, F.A. Spatial distribution of human and canine visceral leishmaniasis in Belo Horizonte, Minas Gerais State, Brazil, 1994-1997. Cad Saude Publica 2001, 17, 1231–1239. [Google Scholar] [CrossRef] [PubMed]
- Gavgani, A.S.M.; Mohite, H.; Edrissian, G.H.; Mohebali, M.; Davies, C.R. Domestic dog ownership in Iran is a risk factor for human infection with Leishmania infantum. Am J Trop Med Hyg 2002, 67, 511–515. [Google Scholar] [CrossRef] [PubMed]
- França-Silva, J.C.; da Costa, R.T.; Siqueira, A.M.; Machado-Coelho, G.L.L.; da Costa, C.A.; Mayrink, W.; Vieira, E.P.; Costa, J.S.; Genaro, O.; Nascimento, E. Epidemiology of canine visceral leishmaniosis in the endemic area of Montes Claros Municipality, Minas Gerais State, Brazil. Vet Parasitol 2003, 111, 161–173. [Google Scholar] [CrossRef] [PubMed]
- Giorgobiani, E.; Chitadze, N.; Chanturya, G.; Grdzelidze, M.; Jochim, R.C.; Machablishvili, A.; Tushishvili, T.; Zedginidze, Y.; Manjgaladze, M.K.; Iashvili, N.; et al. Epidemiologic Aspects of an Emerging Focus of Visceral Leishmaniasis in Tbilisi, Georgia. PLoS Negl Trop Dis 2011, 5, e1415. [Google Scholar] [CrossRef] [PubMed]
- Palatnik-de-Sousa, C.B.; Day, M.J. One Health: The global challenge of epidemic and endemic leishmaniasis. Parasit Vectors 2011, 4, 197. [Google Scholar] [CrossRef]
- Toepp, A.J.; Monteiro, G.R.G.; Coutinho, J.F. V.; Lima, A.L.; Larson, M.; Wilson, G.; Grinnage-Pulley, T.; Bennett, C.; Mahachi, K.; Anderson, B.; et al. Comorbid infections induce progression of visceral leishmaniasis. Parasit Vectors 2019, 12, 54. [Google Scholar] [CrossRef] [PubMed]
- Belo, V.S.; Werneck, G.L.; Barbosa, D.S.; Simões, T.C.; Nascimento, B.W.L.; da Silva, E.S.; Struchiner, C.J. Factors Associated with Visceral Leishmaniasis in the Americas: A Systematic Review and Meta-Analysis. PLoS Negl Trop Dis 2013, 7, e2182. [Google Scholar] [CrossRef]
- Thomaz Soccol, V.; Pasquali, A.K.S.; Pozzolo, E.M.; de Leandro, A.S.; Chiyo, L.; Baggio, R.A.; Michaliszyn, M.S.; Silva, C.; Cubas, P.H.; Peterlle, R.; et al. More than the eyes can see: The worrying scenario of canine leishmaniasis in the Brazilian side of the triple border. PLoS One 2017, 12, e0189182. [Google Scholar] [CrossRef]
- Cabrera, M.A.A.; Paula, A.A.; Camacho, L.A.B.; Marzochi, M.C.A.; Xavier, S.C.; Silva, A.V.M. da; Jansen, A.M. Canine Visceral Leishmaniasis in Barra de Guaratiba, Rio de Janeiro, Brazil: Assessment of Risk Factors. Rev Inst Med Trop Sao Paulo 2003, 45, 79–83. [Google Scholar] [CrossRef]
- do B.P.F. de Almeida, A.; Mendonça, A.J.; Sousa, V.R.F. Prevalência e epidemiologia da leishmaniose visceral em cães e humanos, na cidade de Cuiabá, Mato Grosso, Brasil. Ciência Rural 2010, 40, 1610–1615. [Google Scholar] [CrossRef]
- dos Santos, J.M.L.; Dantas-Torres, F.; Mattos, M.R.F.; Lino, F.R.L.; Andrade, L.S.S.; de Souza, R.C.A.; da Brito, F.L.C.; de Brito, M.E.F.; Brandão-Filho, S.P.; Simões-Mattos, L. Prevalência de anticorpos antileishmania spp em cães de Garanhuns, Agreste de Pernambuco. Rev Soc Bras Med Trop 2010, 43, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Deane, L.M. Leishmaniose Visceral No Brasil. Estudos sobre reservatórios e transmissores realizados no estado do Ceará. Doutorado em Parasitologia, Universidade de São Paulo: São Paulo, 1956.
- Deane, L.M.; Deane, M.P. Visceral leishmaniosis in Brazil. Geographical distribution and transmission. Rev. Inst. Med. Trop. 1962, 4, 198–212. [Google Scholar]
- Fraga, D.B.M.; Solcà, M.S.; Silva, V.M.G.; Borja, L.S.; Nascimento, E.G.; Oliveira, G.G.S.; Pontes-de-Carvalho, L.C.; Veras, P.S.T.; dos-Santos, W.L.C. Temporal distribution of positive results of tests for detecting Leishmania infection in stray dogs of an endemic area of visceral leishmaniasis in the Brazilian tropics: a 13 years survey and association with human disease. Vet Parasitol 2012, 190, 591–594. [Google Scholar] [CrossRef]
- Miró, G.; Gálvez, R.; Fraile, C.; Descalzo, M.A.; Molina, R. Infectivity to Phlebotomus perniciosus of dogs naturally parasitized with Leishmania infantum after different treatments. Parasit Vectors 2011, 4, 52. [Google Scholar] [CrossRef] [PubMed]
- Courtenay, O.; Carson, C.; Calvo-Bado, L.; Garcez, L.M.; Quinnell, R.J. Heterogeneities in Leishmania infantum Infection: Using Skin Parasite Burdens to Identify Highly Infectious Dogs. PLoS Negl Trop Dis 2014, 8, e2583. [Google Scholar] [CrossRef] [PubMed]
- Maia, C.; Nunes, M.; Cristóvão, J.; Campino, L. Experimental canine leishmaniasis: Clinical, parasitological and serological follow-up. Acta Trop 2010, 116, 193–199. [Google Scholar] [CrossRef]
- Michalsky, É.M.; Rocha, M.F.; da Rocha Lima, A.C.V.M.; França-Silva, J.C.; Pires, M.Q.; Oliveira, F.S.; Pacheco, R.S.; dos Santos, S.L.; Barata, R.A.; Romanha, Á.J.; et al. Infectivity of seropositive dogs, showing different clinical forms of leishmaniasis, to Lutzomyia longipalpis phlebotomine sand flies. Vet Parasitol 2007, 147, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Verçosa, B.; Lemos, C.; Mendonça, I.; Silva, S.; de Carvalho, S.; Goto, H.; Costa, F. Transmission potential, skin inflammatory response, and parasitism of symptomatic and asymptomatic dogs with visceral leishmaniasis. BMC Vet Res 2008, 4, 45. [Google Scholar] [CrossRef] [PubMed]
- Molina, R.; Amela, C.; Nieto, J.; San-Andrés, M.; González, F.; Castillo, J.A.; Lucientes, J.; Alvar, J. Infectivity of dogs naturally infected with Leishmania infantum to colonized Phlebotomus perniciosus. Trans R Soc Trop Med Hyg 1994, 88, 491–493. [Google Scholar] [CrossRef]
- Guarga, J.L.; Lucientes, J.; Peribáñez, M.A.; Molina, R.; Gracia, M.J.; Castillo, J.A. Experimental infection of Phlebotomus perniciosus and determination of the natural infection rates of Leishmania infantum in dogs. Acta Trop 2000, 77, 203–207. [Google Scholar] [CrossRef]
- Solano-Gallego, L.; Morell, P.; Arboix, M.; Alberola, J.; Ferrer, L. Prevalence of Leishmania infantum Infection in Dogs Living in an Area of Canine Leishmaniasis Endemicity Using PCR on Several Tissues and Serology. J Clin Microbiol 2001, 39, 560–563. [Google Scholar] [CrossRef]
- Moshfe, A.; Mohebali, M.; Edrissian, G.; Zarei, Z.; Akhoundi, B.; Kazemi, B.; Jamshidi, S.; Mahmoodi, M. Canine visceral leishmaniasis: Asymptomatic infected dogs as a source of L. infantum infection. Acta Trop 2009, 112, 101–105. [Google Scholar] [CrossRef]
- Coura-Vital, W.; Reis, A.B.; Fausto, M.A.; de Leal, G.G.A.; Marques, M.J.; Veloso, V.M.; Carneiro, M. Risk Factors for Seroconversion by Leishmania infantum in a Cohort of Dogs from an Endemic Area of Brazil. PLoS One 2013, 8, e71833. [Google Scholar] [CrossRef]
- Lopes, J.V.; Michalsky, É.M.; de Lara Silva, F.O.; Lima, A.C.V.M.R.; de Avelar, D.M.; da Costa, A.A.J.; França-Silva, J.C.; Regina-Silva, S.; Fortes-Dias, C.L.; Dias, E.S. Seroprevalence and molecular characterization of Leishmania in dogs from an endemic area of zoonotic visceral leishmaniasis in Brazil. Int J Vet Sci Med 2017, 5, 70–74. [Google Scholar] [CrossRef]
- Miguel, D.C.; Guarnier, D.C. Canine and Human Leishmaniasis: Disease Progression to Brazilian Urbanized Areas. International Journal of Tropical Diseases 2019, 2. [Google Scholar] [CrossRef]
- Travi, B.L.; Cordeiro-da-Silva, A.; Dantas-Torres, F.; Miró, G. Canine visceral leishmaniasis: Diagnosis and management of the reservoir living among us. PLoS Negl Trop Dis 2018, 12, e0006082. [Google Scholar] [CrossRef]
- Dantas-Torres, F.; Miró, G.; Bowman, D.D.; Gradoni, L.; Otranto, D. Culling Dogs for Zoonotic Visceral Leishmaniasis Control: The Wind of Change. Trends Parasitol 2019, 35, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Nunes, C.M.; Lima, V.M.F. de; Paula, H.B. de; Perri, S.H.V.; Andrade, A.M. de; Dias, F.E.F.; Burattini, M.N. Dog culling and replacement in an area endemic for visceral leishmaniasis in Brazil. Vet Parasitol 2008, 153, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Sevá, A.P.; Ovallos, F.G.; Amaku, M.; Carrillo, E.; Moreno, J.; Galati, E.A.B.; Lopes, E.G.; Soares, R.M.; Ferreira, F. Canine-Based Strategies for Prevention and Control of Visceral Leishmaniasis in Brazil. PLoS One 2016, 11, e0160058. [Google Scholar] [CrossRef]
- Grimaldi, G.; Teva, A.; Ferreira, A.L.; dos Santos, C.B.; de-S. Pinto, I.; de-Azevedo, C.T.; Falqueto, A. Evaluation of a novel chromatographic immunoassay based on Dual-Path Platform technology (DPP® CVL Rapid Test) for the serodiagnosis of canine visceral leishmaniasis. Trans R Soc Trop Med Hyg 2012, 106, 54–59. [Google Scholar] [CrossRef]
- Coura-Vital, W.; Ker, H.G.; Roatt, B.M.; Aguiar-Soares, R.D.O.; de Leal, G.G.A.; das Moreira, N.D.; Oliveira, L.A.M.; de Menezes Machado, E.M.; Morais, M.H.F.; Corrêa-Oliveira, R.; et al. Evaluation of Change in Canine Diagnosis Protocol Adopted by the Visceral Leishmaniasis Control Program in Brazil and a New Proposal for Diagnosis. PLoS One 2014, 9, e91009. [Google Scholar] [CrossRef] [PubMed]
- de Sousa-Paula, L.C.; da Silva, L.G.; da Sales, K.G.S.; Dantas-Torres, F. Failure of the dog culling strategy in controlling human visceral leishmaniasis in Brazil: A screening coverage issue? PLoS Negl Trop Dis 2019, 13, e0007553. [Google Scholar] [CrossRef]
- Coura-Vital, W.; Marques, M.J.; Veloso, V.M.; Roatt, B.M.; de Aguiar-Soares, R.D.O.; Reis, L.E.S.; Braga, S.L.; Morais, M.H.F.; Reis, A.B.; Carneiro, M. Prevalence and Factors Associated with Leishmania infantum Infection of Dogs from an Urban Area of Brazil as Identified by Molecular Methods. PLoS Negl Trop Dis 2011, 5, e1291. [Google Scholar] [CrossRef] [PubMed]
- Courtenay, O.; Quinnell, R.J.; Garcez, L.M.; Shaw, J.J.; Dye, C. Infectiousness in a Cohort of Brazilian Dogs: Why Culling Fails to Control Visceral Leishmaniasis in Areas of High Transmission. J Infect Dis 2002, 186, 1314–1320. [Google Scholar] [CrossRef] [PubMed]
- Moreira, E.D.; Mendes de Souza, V.M.; Sreenivasan, M.; Nascimento, E.G.; Pontes de Carvalho, L. Assessment of an optimized dog-culling program in the dynamics of canine Leishmania transmission. Vet Parasitol 2004, 122, 245–252. [Google Scholar] [CrossRef]
- Ashford, D.A.; David, J.R.; Freire, M.; David, R.; Sherlock, I.; da Eulálio, M.C.; Sampaio, D.P.; Badaro, R. Studies on control of visceral leishmaniasis: impact of dog control on canine and human visceral leishmaniasis in Jacobina, Bahia, Brazil. American Journal of Tropical Medicine and Hygiene 1998, 59, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.H.N.; Tapety, C.M.M.; Werneck, G.L. Controle da leishmaniose visceral em meio urbano: estudo de intervenção randomizado fatorial. Rev Soc Bras Med Trop 2007, 40, 415–419. [Google Scholar] [CrossRef]
- Nunes, C.M.; Pires, M.M.; da Silva, K.M.; Assis, F.D.; Filho, J.G.; Perri, S.H.V. Relationship between dog culling and incidence of human visceral leishmaniasis in an endemic area. Vet Parasitol 2010, 170, 131–133. [Google Scholar] [CrossRef] [PubMed]
- Costa, D.N.C.C.; Bermudi, P.M.M.B.; Rodas, L.A.C.; Nunes, C.M.; Hiramoto, R.M.; Tolezano, J.E.; Cipriano, R.S.; Cardoso, G.C.D.; Codeço, C.T.; Chiaravalloti-Neto, F. Human visceral leishmaniasis and relationship with vector and canine control measures. Rev Saude Publica 2018, 52, 92. [Google Scholar] [CrossRef]
- Bermudi, P.M.M.; Costa, D.N.C.C.; Nunes, C.M.; Tolezano, J.E.; Hiramoto, R.M.; Rodas, L.A.C.; Cipriano, R.S.; Blangiardo, M.; Chiaravalloti-Neto, F. Canine serological survey and dog culling and its relationship with human visceral leishmaniasis in an endemic urban area. BMC Infect Dis 2020, 20, 401. [Google Scholar] [CrossRef]
- Dietze, R.; Barros, G.B.; Teixeira, L.; Harris, J.; Michelson, K.; Falqueto, A.; Corey, R. Effect of Eliminating Seropositive Canines on the Transmission of Visceral Leishmaniasis in Brazil. Clinical Infectious Diseases 1997, 25, 1240–1242. [Google Scholar] [CrossRef]
- Paranhos-Silva, M.; Nascimento, E.G.; Melro, M.C.B.F.; Oliveira, G.G.S.; dos Santos, W.L.C.; Pontes-de-Carvalho, L.C.; Oliveira-dos-Santos, A.J. Cohort study on canine emigration and Leishmania infection in an endemic area for american visceral leishmaniasis. Implications for the disease control. Acta Trop 1998, 69, 75–83. [Google Scholar] [CrossRef]
- Vaz, T.P.; Gama-Melo, M.O.; Quaresma, P.F.; Gontijo, C.M.F.; Santos, G.; Barbosa, F.S.; Fontes, G. Evaluation of the euthanasia of seropositive dogs for canine visceral leishmaniasis as the only method of controling the disease in the enzootic area in the Midwestern Minas Gerais. Pesquisa Veterinária Brasileira 2020, 40, 107–112. [Google Scholar] [CrossRef]
- Costa, D.N.C.C.; Codeço, C.T.; Silva, M.A.; Werneck, G.L. Culling Dogs in Scenarios of Imperfect Control: Realistic Impact on the Prevalence of Canine Visceral Leishmaniasis. PLoS Negl Trop Dis 2013, 7, e2355. [Google Scholar] [CrossRef] [PubMed]
- França-Silva, J.C.; Giunchetti, R.C.; da Mariano, R.M.S.; Machado-Coelho, G.L.L.; de Teixeira, L.A.S.; Barata, R.A.; Michalsky, É.M.; Rocha, M.F.; Fortes-Dias, C.L.; Dias, E.S. The Program for the Control of Visceral Leishmaniasis in Brazil: The Effect of the Systematic Euthanasia of Seropositive Dogs as a Single Control Action in Porteirinha, a Brazilian City with an Intense Transmission of Visceral Leishmaniasis. Pathogens 2023, 12, 1060. [Google Scholar] [CrossRef]
- Latif, A.A.; Nkabinde, B.; Peba, B.; Matthee, O.; Pienaar, R.; Josemans, A.; Marumo, D.; Labuschagne, K.; Abdelatief, N.A.; Krüger, A.; et al. Risk of establishment of canine leishmaniasis infection through the import of dogs into South Africa. Onderstepoort Journal of Veterinary Research 2019, 86. [Google Scholar] [CrossRef]
- Figueiredo, F.B.; Lima Júnior, F.E.F. de; Tomio, J.E.; de Indá, F.M.C.; Corrêa, G.L.B.; de Madeira, M.F. Leishmaniose Visceral Canina: Dois casos autóctones no município de Florianópolis, estado de Santa Catarina. Acta Sci Vet 2012, 40, 1026. [Google Scholar]
- Vilas, V.J.D.R.; Maia-Elkhoury, A.N.S.; Yadon, Z.E.; Cosivi, O.; Sanchez-Vazquez, M.J. Visceral leishmaniasis: a One Health approach. Veterinary Record 2014, 175, 42–44. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho, F.L.N.; de Riboldi, E.O.; Bello, G.L.; Ramos, R.R.; Barcellos, R.B.; Gehlen, M.; Halon, M.L.; Romão, P.R.T.; Dallegrave, E.; Rossetti, M.L.R. Canine visceral leishmaniasis diagnosis: a comparative performance of serological and molecular tests in symptomatic and asymptomatic dogs. Epidemiol Infect 2018, 146, 571–576. [Google Scholar] [CrossRef]
- Pessoa-e-Silva, R.; Vaitkevicius-Antão, V.; de Andrade, T.A.S.; de Oliveira Silva, A.C.; de Oliveira, G.A.; Trajano-Silva, L.A.M.; Nakasone, E.K.N.; de Paiva-Cavalcanti, M. The diagnosis of canine visceral leishmaniasis in Brazil: confronting old problems. Exp Parasitol 2019, 199, 9–16. [Google Scholar] [CrossRef]
- Coura-Vital, W.; Marques, M.J.; Veloso, V.M.; Roatt, B.M.; de Aguiar-Soares, R.D.O.; Reis, L.E.S.; Braga, S.L.; Morais, M.H.F.; Reis, A.B.; Carneiro, M. Prevalence and Factors Associated with Leishmania infantum Infection of Dogs from an Urban Area of Brazil as Identified by Molecular Methods. PLoS Negl Trop Dis 2011, 5, e1291. [Google Scholar] [CrossRef] [PubMed]
- Lopes, E.G.; Sevá, A.P.; Ferreira, F.; Nunes, C.M.; Keid, L.B.; Hiramoto, R.M.; Ferreira, H.L.; Oliveira, T.M.F.S.; Bigotto, M.F.D.; Galvis-Ovallos, F.; et al. Serological and molecular diagnostic tests for canine visceral leishmaniasis in Brazilian endemic area: one out of five seronegative dogs are infected. Epidemiol Infect 2017, 145, 2436–2444. [Google Scholar] [CrossRef] [PubMed]
- Mendonça, I.L. de; Batista, J.F.; Schallig, H.; do S.P. e Cruz, M.; Alonso, D.P.; Ribolla, P.E.M.; Costa, D.L.; Costa, C.H.N. The performance of serological tests for Leishmania infantum infection screening in dogs depends on the prevalence of the disease. Rev Inst Med Trop Sao Paulo 2017, 59. [Google Scholar] [CrossRef]
- Ribeiro, V.M.; Miranda, J.B.; Marcelino, A.P.; de Andrade, H.M.; Reis, I.A.; Cardoso, M.S.; Gontijo, C.M.F.; Paz, G.F. Performance of different serological tests in the diagnosis of natural infection by Leishmania infantum in dogs. Vet Parasitol 2019, 274, 108920. [Google Scholar] [CrossRef]
- Herrera, G.; Castillo, A.; Ayala, M.S.; Flórez, C.; Cantillo-Barraza, O.; Ramirez, J.D. Evaluation of four rapid diagnostic tests for canine and human visceral Leishmaniasis in Colombia. BMC Infect Dis 2019, 19, 747. [Google Scholar] [CrossRef] [PubMed]
- Salomón, O.D.; Pérez, A.A.; Riarte, A.R.; Casas, N.; Fragueiro-Frías, V.; Negri, V.; Santini, M.S.; Liotta, D.J. Performance of Rapid Tests for Canine Visceral Leishmaniasis Diagnosis in Argentina. Medicina (Buenos Aires) 2020, 80, 103–110. [Google Scholar]
- Teixeira, A.I.P.; Silva, D.M.; Vital, T.; Nitz, N.; de Carvalho, B.C.; Hecht, M.; Oliveira, D.; Oliveira, E.; Rabello, A.; Romero, G.A.S. Improving the reference standard for the diagnosis of canine visceral leishmaniasis: a challenge for current and future tests. Mem Inst Oswaldo Cruz 2019, 114. [Google Scholar] [CrossRef]
- Figueiredo, F.B.; de Vasconcelos, T.C.B.; de Madeira, M.F.; Menezes, R.C.; Maia-Elkhoury, A.N.S.; Marcelino, A.P.; Werneck, G.L. Validation of the Dual-Path Platform chromatographic immunoassay (DPP® CVL Rapid Test) for the serodiagnosis of canine visceral leishmaniasis. Mem Inst Oswaldo Cruz 2018, 113. [Google Scholar] [CrossRef]
- Brasil. Ministério da Saúde Manual de Vigilância e Controle Da Leishmaniose Visceral; Editora MS, 2014; Vol. 1; ISBN 9788533407428.
- Costa, D.N.C.C.; Codeço, C.T.; Bermudi, P.M.M.; Rodas, L.A.C.; Nunes, C.M.; Hiramoto, R.M.; Tolezano, J.E.; Chiaravalloti Neto, F. Controle da leishmaniose visceral canina por eutanásia: estimativa de efeito baseado em inquérito e modelagem matemática. Cad Saude Publica 2020, 36. [Google Scholar] [CrossRef]
- Leite, J.C.; Gonçalves, A.A.M.; de Oliveira, D.S.; Resende, L.A.; Boas, D.F.V.; Ribeiro, H.S.; Pereira, D.F.S.; da Silva, A.V.; da Mariano, R.M.S.; Reis, P.C.C.; et al. Transmission-Blocking Vaccines for Canine Visceral Leishmaniasis: New Progress and Yet New Challenges. Vaccines (Basel) 2023, 11, 1565. [Google Scholar] [CrossRef] [PubMed]
- Oliva, G.; Nieto, J.; Foglia Manzillo, V.; Cappiello, S.; Fiorentino, E.; Di Muccio, T.; Scalone, A.; Moreno, J.; Chicharro, C.; Carrillo, E.; et al. A Randomised, Double-Blind, Controlled Efficacy Trial of the LiESP/QA-21 Vaccine in Naïve Dogs Exposed to Two Leishmania infantum Transmission Seasons. PLoS Negl Trop Dis 2014, 8, e3213. [Google Scholar] [CrossRef] [PubMed]
- Fernández Cotrina, J.; Iniesta, V.; Monroy, I.; Baz, V.; Hugnet, C.; Marañon, F.; Fabra, M.; Gómez-Nieto, L.C.; Alonso, C. A large-scale field randomized trial demonstrates safety and efficacy of the vaccine LetiFend® against canine leishmaniosis. Vaccine 2018, 36, 1972–1982. [Google Scholar] [CrossRef] [PubMed]
- Giunchetti, R.C.; Silveira, P.; Resende, L.A.; Leite, J.C.; de Melo-Júnior, O.A.O.; Rodrigues- Alves, M.L.; Costa, L.M.; Lair, D.F.; Chaves, V.R.; dos Soares, I.S.; et al. Canine visceral leishmaniasis biomarkers and their employment in vaccines. Vet Parasitol 2019, 271, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Velez, R.; Gállego, M. Commercially approved vaccines for canine leishmaniosis: a review of available data on their safety and efficacy. Tropical Medicine & International Health 2020, 25, 540–557. [Google Scholar] [CrossRef]
- de Lana, M.; Giunchetti, R.C. Dogs as a Model for Chemotherapy of Chagas Disease and Leishmaniasis. Curr Pharm Des 2021, 27, 1741–1756. [Google Scholar] [CrossRef]
- Ribas, L.M.; Zaher, V.L.; Shimozako, H.J.; Massad, E. Estimating the Optimal Control of Zoonotic Visceral Leishmaniasis by the Use of a Mathematical Model. The Scientific World Journal 2013, 2013, 1–6. [Google Scholar] [CrossRef]
- Ministério da Saúde, Brasil; Secretaria de Vigilância em Saúde. Nota Técnica No 5/2021-CGZV/DEIDT/SVS/MS; Ministério da Saúde: Brasília, Brasil, 2021; Available online: https://www.gov.br/saude/pt-br/assuntos/saude-de-a-a-z/l/leishmaniose-visceral/arquivos/sei_ms-nota-tecnica-n-5_leishpdf.pdf (accessed on 14 October 2022).
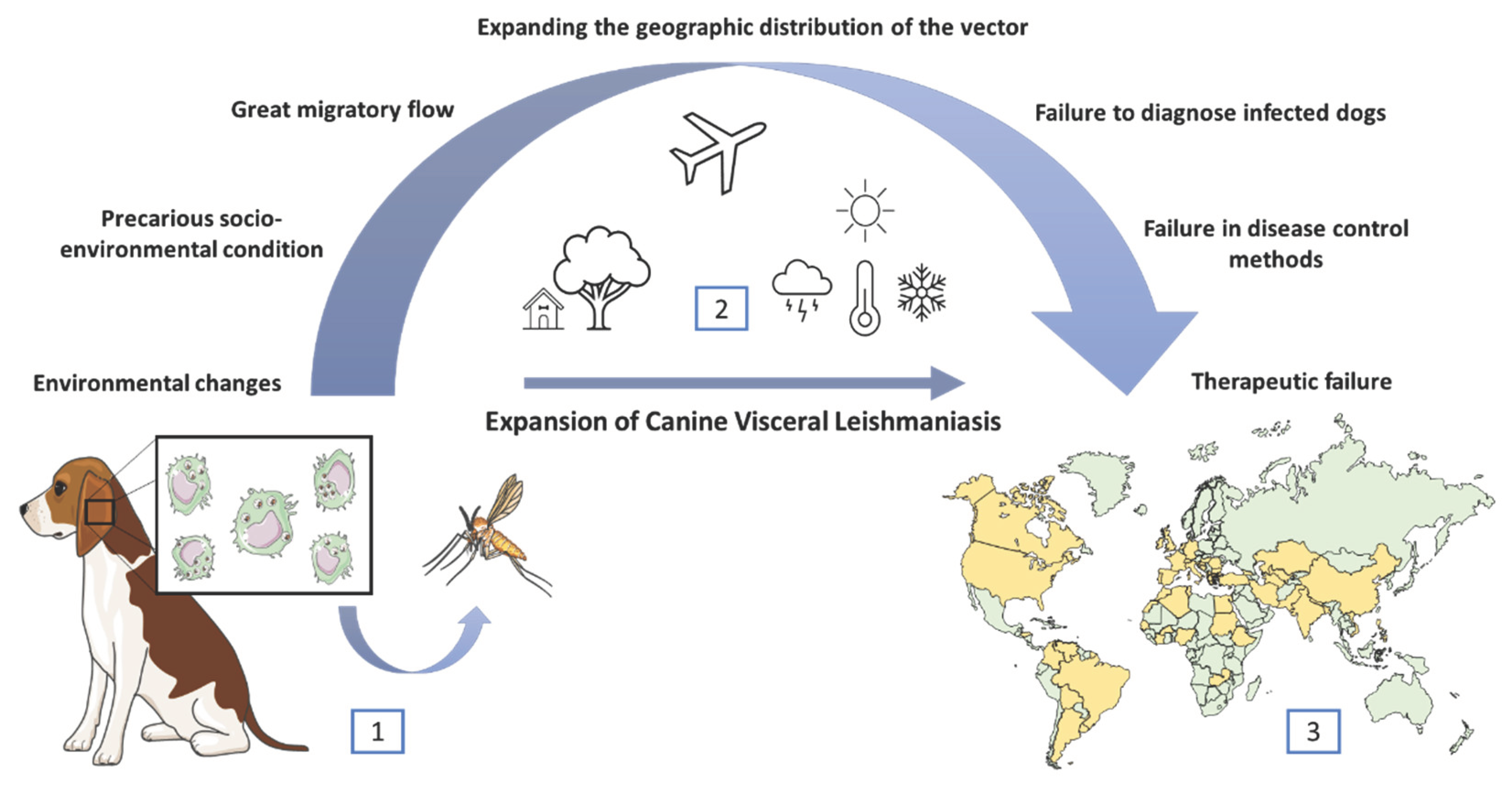
| Test | Manufacturer | Sensitivity | Specificity | References |
| IFAT 1:40 | Bio-Manguinhos, Rio de Janeiro, Brazil | 96% | 18%*; 76%** | [268] |
| IFAT 1:80 | 90% | 33%*; 93%** | ||
| ELISA | Bio-Manguinhos, Rio de Janeiro, Brazil | 91% | 79%*; 98%** | [268] |
| 84.20% | 95.6% | [269] | ||
| rK39 (Kalazar Detect) | InBios, Inc., Seattle, Washington, USA | 88% | 74%*; 98%** | [268] |
| 82.90% | 92.6% | [270] | ||
| 76.90% | 98.6% | [271] | ||
| 79.60% | 95.7% | [269] | ||
| FAST | Royal Tropical Institute, Amsterdam, The Netherlands | 93% | 68%*; 100%** | [268] |
| DAT | Royal Tropical Institute, Amsterdam, The Netherlands | 96% | 33%*; 98%** | [268] |
| TR DPP | Bio-Manguinhos, Rio de Janeiro, Brazil |
98% | 60%*; 98%** | [268] |
| 21.74% | 92.59% | [272] | ||
| 89% | 70.2% | [273] | ||
| 85.70% | 79.6% | [270] | ||
| 93.70% | 95.9% | [271] | ||
| 97.90% | 93.6% | [269] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





