1. Introduction
Obstructive sleep apnea (OSA) is characterized by repeated episodes of complete or partial occlusion of the upper airways during sleep [
1,
2,
3]. Its prevalence ranges from 9 to 38% in general population [
4]. Obesity is a major risk factor for OSA, partially explaining its increased prevalence in our society. Other risk factors include age, male gender, tonsillar hypertrophy and craniofacial abnormalities that narrow the upper airway [
1,
2,
3].
Hypothyroidism has been associated with OSA, mainly due to upper airway narrowing caused by the deposition of mucopolysaccharides and protein extravasation into the tissues of the face, tongue and pharyngeal structures [
5,
6,
7]. The implication of goiter independently of thyroid function in the occurrence of OSA remains unclear [
8,
9,
10,
11,
12]. Small case series have reported improvement in OSA syndrome after thyroidectomy in patients with goiter [
5,
6,
7,
8,
13,
14,
15,
16]. However, their findings need validation, and further observations are required to determine if goiter can be considered a risk factor for OSA [
8]. Below, we present a case of a patient with large and compressive multinodular goiter who was diagnosed with OSA before thyroid surgery and whose OSA resolved after total thyroidectomy.
2. Case Description
A 66-year-old woman with a goiter and scheduled for total thyroidectomy was referred to the Pneumology Department at La Rabta University Hospital in Tunis, Tunisia, for preoperative respiratory assessment due to suspected OSA.
The patient has an eight-year history of hyperthyroidism associated with multinodular goiter. She was treated with Thyrozol 10 and Avlocardyl 40. Additionally, she has comorbidities including obesity, hypertension, dyslipidemia and diabetes with moderate chronic renal failure. The patient also has a history of lower limb trauma surgery, resulting in limited physical activity.
Total thyroidectomy has recently been indicated due to the progression of the goiter and its compressive nature. The patient achieved a euthyroid state prior to surgery with medication. However, during the preoperative anesthetic evaluation, there was suspicion of OSA, indicated by a STOP-BANG score of 6. Consequently, a specialized respiratory assessment was deemed necessary before proceeding with thyroid surgery.
During the respiratory assessment, no family history or lifestyle habits were identified as risk factors for OSA, apart from limited physical activity which can exacerbate obesity. The patient stated that she had never consulted a doctor previously for symptoms of OSA or other sleep disorders. However, upon further questioning, the patient reported experiencing snoring without choking or gasping during sleep, as well as excessive daytime sleepiness (Epworth sleepiness scale score: 21/ 24). Additionally, she complained of frequent nighttime urination (3-4 times per night), non-restorative sleep, morning fatigue, and morning headaches. The goiter was accompanied by a progressive dysphagia and discomfort in the neck.
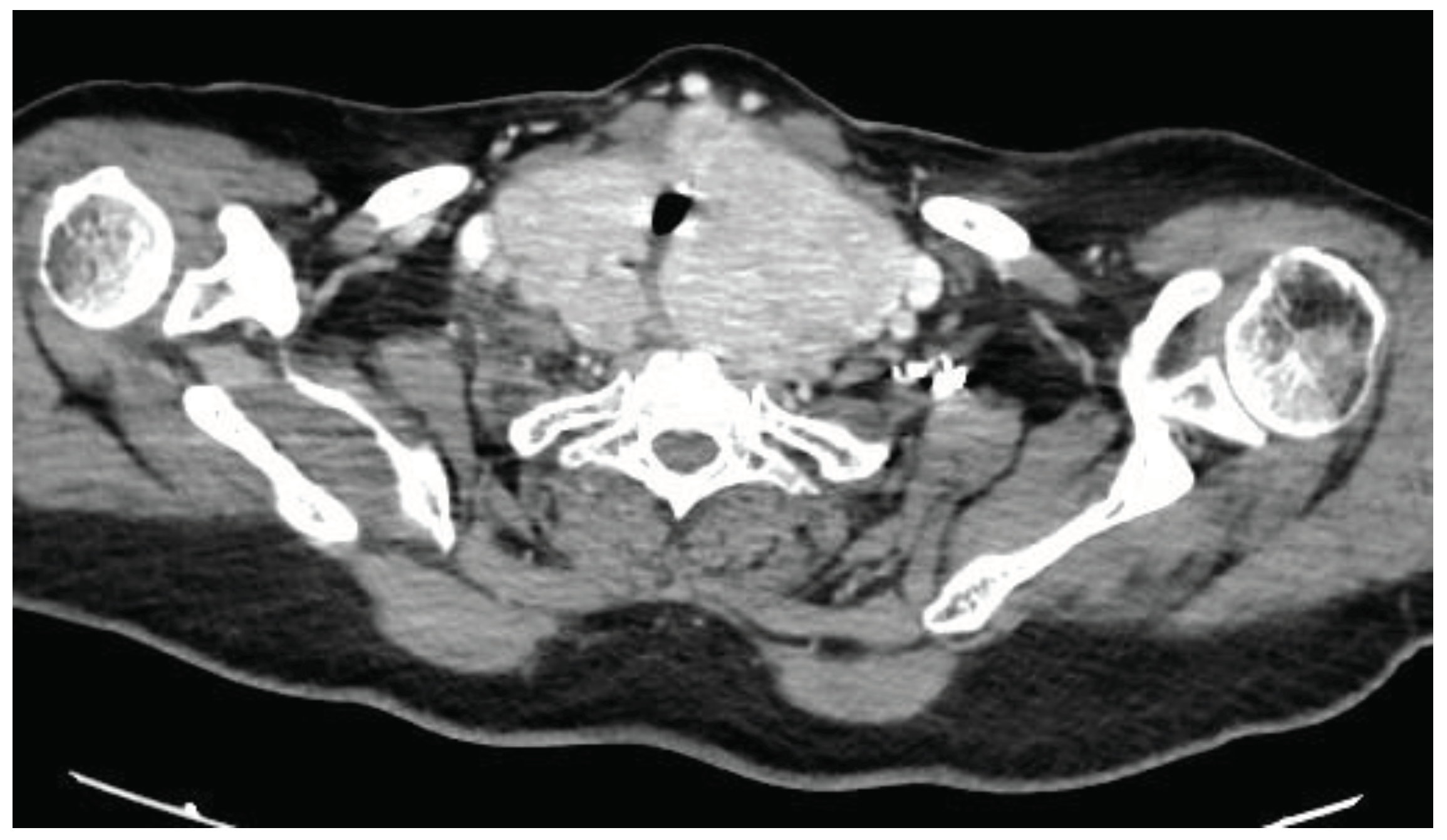
The physical examination revealed that the patient measured 149 cm in height and weighed 84 kg, resulting in a BMI of 37.8 kg/m2. Her neck circumference was measured at 49 cm. Upper airway assessment indicated a mallampati score of 4, and a large goiter was clinically evident, with no craniofacial abnormalities observed. The lower edge of the thyroid gland was not palpable during the examination. However, a computed tomography (CT) scan of the neck and thoracic inlet had previously confirmed a multinodular enlargement of the thyroid gland, with retrovascular extension and compression of the trachea (
Figure 1).
Home respiratory polygraphy showed severe OSA, with an AHI of 32 events per hour, primarily characterized by obstructive hypopneas (hypopnea index: HI= 30 events per hour). The oxygen desaturation index (ODI) correlated closely with the AHI, reaching 31 events per hour, but it did not significantly affect the mean nocturnal oxygen saturation (mean SpO2) or the cumulative time spent with SpO2 below 90% (T90) (mean SpO2= 95%; T90= 0.4%). The snoring index was high (SI= 65 events per hour) and the most preferred sleep positions were the left side (67% of sleep time) and the right side (25% of sleep time). The supine position, known to favor the occurrence of obstructive respiratory events during sleep, represented only 4% of total sleep time.
Consequently, the patient underwent CPAP titration, which showed that abnormal respiratory events were eliminated with a constant pressure of 7.6 cm H2O. CPAP therapy was continued using a nasal mask, leading to improvement in symptoms associated with OSA. Good adherence to CPAP treatment was confirmed by a CPAP compliance report, which also indicated the absence of unintentional leaks and a low residual AHI of 3 events per hour.
Following preoperative respiratory management, the patient underwent total thyroidectomy under general anesthesia at the Oto-Rhino-Laryngology Department of La Rabta University Hospital in Tunis, Tunisia. Postoperatively, the patient reported minor changes in voice quality without any other complications. Subsequently, the patient received replacement therapy with L-thyroxine.
Considering that OSA was primarily related to obesity and advanced age in this case, it was anticipated that the patient would continue to be followed up for OSA and CPAP therapy after total thyroidectomy. However, surprisingly, the patient experienced complete improvement in OSA symptoms after the thyroid surgery, in addition to resolution of dysphagia. Consequently, she chose to discontinue her CPAP therapy. Moreover, the patient’s family reported a reduction in snoring following the thyroid surgery, and an assessment of daytime sleepiness using the Epworth sleepiness scale revealed a score of 1/ 24. Notably, there were no changes observed in the patient’s weight, lifestyle habits, or medical conditions or treatments that could explain the resolution of OSA symptoms, apart from thyroidectomy.
Respiratory polygraphy performed without CPAP following total thyroidectomy revealed a significant decrease in the AHI, which had reached a normal value (AHI<5), along with normal levels of nocturnal SpO2. These findings strongly suggested the resolution of OSA following thyroid surgery. Additionally, there was a notable decrease in the SI, and the variability in sleep positions was nearly identical to that observed prior to thyroidectomy. Parameters from respiratory polygraphy before and after thyroidectomy are summarized in
Table 1.
A medical decision influenced by clinical and polygraphic data has finally been made to approve discontinuation of CPAP therapy for the patient, alongside the implementation of hygienic and dietary measures. However, the patient will undergo follow-up and reevaluation later on. Indeed, her advanced age, obesity, and high Mallampati score place her at heightened risk for recurrence of OSA.
3. Discussion
It was concluded in this case that the large, compressive multinodular goiter was the causal factor for OSA. Indeed, resolution of OSA after thyroidectomy was complete, as indicated by clinical and polygraphic data and unrelated to other factors such as weight loss or specific changes in medical conditions or treatments.
Although goiter is not typically recognized as a cause of OSA, some case studies have reported improvement in OSA symptoms in patients with goiter after undergoing thyroidectomy [
5,
6,
7,
8,
13,
14,
15,
16]. Nevertheless, this improvement has sometimes been assessed solely based on clinical criteria, lacking objective parameters, such as the AHI to definitively prove resolution of OSA after thyroidectomy [
5,
6,
7]. Additionally, the degree of improvement in OSA after thyroidectomy has been observed to vary, potentially influenced by factors such as the severity of initial OSA and other contributing factors like advanced age or obesity [
5,
6,
7,
8,
13,
14,
15,
16]. In this case report, respiratory polygraphy was conducted alongside clinical assessment both before and after thyroidectomy. This approach allowed for the confirmation of OSA diagnosis, assessment of its severity, and objective evaluation of the patient following thyroid surgery. The reduction in AHI after thyroidectomy (
Table 1) supported the resolution of OSA that appeared complete, leading to the conclusion that goiter was indeed the causal factor for OSA in this instance. Importantly, no other factors were identified to explain resolution of OSA besides thyroidectomy.
In this case, a total thyroidectomy was indicated due to the progressive enlargement and compressive nature of the goiter, which resulted in dysphagia and neck discomfort. It also appears that the occurrence and severity of OSA are influenced by the size of the goiter and its local extension [
6,
10]. Indeed, it has been suggested that a large goiter can impede venous return from the head and neck, leading to engorgement and edema of upper airways structures, thereby reducing upper airway patency. Additionally, the displacement of the trachea and other cervical structures associated with a large goiter may interfere with the normal upper airway stiffening reflex that occurs during inspiration. A third hypothesis suggests that a large goiter itself may exert a mass loading effect on the airways, thereby facilitating the occurrence of abnormal respiratory events during sleep [
6].
The clinical and polygraphic data in this case reflect certain characteristics of OSA associated with a large and compressive multinodular goiter. Firstly, diurnal and nocturnal symptoms of OSA were identified during the preoperative anesthesia assessment, but they had not previously prompted the patient to seek medical attention. This could be attributed to the gradual progression of the goiter, resulting in the insidious development of OSA symptoms that were underestimated by the patient. Additionally, apart from diurnal symptoms, nocturia and snoring, neither the patient nor her family reported any episodes of breathing cessation. Respiratory polygraphy revealed severe OSA (AHI>30) with a predominance of hypopneas, indicating that abnormal respiratory events during sleep were primarily associated with episodic partial collapse of the upper airways. Moreover, despite the severity of OSA assessed by AHI, nocturnal SpO2 was not significantly disturbed, and there was no requirement for high pressure during CPAP therapy to eliminate abnormal respiratory events.
4. Conclusions
This case report demonstrated that a large and compressive goiter constitutes a risk factor for OSA, the resolution of which can be achieved by total thyroidectomy. We suggest that prospective studies are needed to accurately assess the effects of goiter on the occurrence of OSA and its characteristics according to the size and local extension of the enlarged thyroid.
Author Contributions
Conceptualization, YO.; methodology, YO.; software, YO.; validation, YO.; formal analysis, YO. and MM.; investigation, YO and AM.; resources, YO., MM., IO. and ME.; data curation, YO. and MM.; writing—original draft preparation, YO., MM., IO. and ME.; writing—review and editing, YO., MM., IO. and ME.; visualization, YO., MM., IO. and ME.; supervision, YO.; project administration, all the authors; funding acquisition, none. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
A written informed consent was obtained from the patient to publish this paper.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hirani, R.; Smiley, A. A Scoping Review of Sleep Apnea: Where Do We Stand? Life (Basel) 2023, 13, 387. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Bonitati, A. Obstructive Sleep Apnea Syndrome - A Review for Primary Care Physicians and Pulmonologists. R I Med J (2013) 2021, 104, 10–13. [Google Scholar] [PubMed]
- Chang, J.L.; Goldberg, A.N.; Alt, J.A.; Mohammed, A.; Ashbrook, L.; Auckley, D.; Ayappa, I.; Bakhtiar, H.; Barrera, J.E.; Bartley, B.L.; et al. International Consensus Statement on Obstructive Sleep Apnea. Int Forum Allergy Rhinol 2023, 13, 1061–1482. [Google Scholar] [CrossRef] [PubMed]
- Senaratna, C.V.; Perret, J.L.; Lodge, C.J.; Lowe, A.J.; Campbell, B.E.; Matheson, M.C.; Hamilton, G.S.; Dharmage, S.C. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med Rev 2017, 34, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Deegan, P.C.; McNamara, V.M.; Morgan, W.E. Goitre: a cause of obstructive sleep apnoea in euthyroid patients. Eur Respir J 1997, 10, 500–502. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, T.; Leong, A.C.; Pang, L.; Chevretton, E.; Jeannon, J.P.; Simo, R. Multinodular thyroid goitre causing obstructive sleep apnoea syndrome. J Laryngol Otol 2012, 126, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Reiher, A.E.; Mazeh, H.; Schaefer, S.; Chen, H.; Sippel, R.S. Thyroidectomy decreases snoring and sleep apnea symptoms. Thyroid 2012, 22, 1160–1164. [Google Scholar] [CrossRef] [PubMed]
- Masarwy, R.; Kampel, L.; Ungar, O.J.; Warshavsky, A.; Horowitz, G.; Rosenzweig, E.; Tauman, R.; Muhanna, N. The impact of thyroidectomy on obstructive sleep apnea: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol 2022, 279, 5801–5811. [Google Scholar] [CrossRef] [PubMed]
- Yuan, J.; Qi, S.; Zhang, X.; Lai, H.; Li, X.; Xiaoheng, C.; Li, Z.; Yao, S.; Ding, Z. Local symptoms of Hashimoto’s thyroiditis: A systematic review. Front Endocrinol (Lausanne) 2022, 13, 1076793. [Google Scholar] [CrossRef] [PubMed]
- Tunc, M.; Sazak, H.; Karlilar, B.; Ulus, F.; Tastepe, I. Coexistence of Obstructive Sleep Apnea and Superior Vena Cava Syndromes Due to Substernal Goitre in a Patient With Respiratory Failure: A Case Report. Iran Red Crescent Med J 2015, 17, e18342. [Google Scholar] [CrossRef] [PubMed]
- Haddad, L.; Haddad, F.L.; Bittencourt, L.; Gregorio, L.C.; Tufik, S.; Abrahao, M. Clinical and polysomnographic findings of patients with large goiters: polysomnographic findings of large goiters. Sleep Breath 2013, 17, 673–678. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, J.; Furtado, R.; Ramani, A.; Mitta, N.; Kudchadkar, S.; Falari, S. A rare instance of retrosternal goitre presenting with obstructive sleep apnoea in a middle-aged person. Int J Surg Case Rep 2013, 4, 1064–1066. [Google Scholar] [CrossRef] [PubMed]
- Schneider, A.; Bourahla, K.; Petiau, C.; Velten, M.; Volkmar, P.P.; Rodier, J.F. Role of thyroid surgery in the obstructive sleep apnea syndrome. World J Surg 2014, 38, 1990–1994. [Google Scholar] [CrossRef] [PubMed]
- Haddad, L.; Martinho Haddad, F.L.; Bittencourt, L.; Gregorio, L.C.; Tufik, S.; Abrahao, M. Impact of thyroidectomy on the control of obstructive sleep apnea syndrome in patients with large goiters. Sleep Breath 2014, 18, 825–828. [Google Scholar] [CrossRef] [PubMed]
- Agrama, M.T. Thyroidectomy for goiter relieves obstructive sleep apnea: results of 8 cases. Ear Nose Throat J 2011, 90, 315–317. [Google Scholar] [CrossRef] [PubMed]
- De Felice, A.; Fuschillo, S.; Martucci, M.; De Angelis, E.; Balzano, G. Euthyroid goitre and sleep apnea. Monaldi Arch Chest Dis 2006, 65, 52–55. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).