1. Introduction
With the advancement of technology, Internet Gaming Disorder (IGD) has become increasingly serious among adolescents in Asia. For susceptible individuals, unrestricted online gaming can become time-consuming, energy-draining, and highly addictive. In 2021, the prevalence of gaming disorder among Japanese youth (ages 10 to 29) was 7.6% for males and 2.5% for females, with an overall prevalence of 5.1% [
1].
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) defines IGD as a condition characterized by excessive and compulsive engagement in video games, leading to significant impairment or distress over 12 months. leading to significant impairment or distress over 12 months. While excessive gaming can result in negative outcomes such as academic decline, physical health issues, and social isolation [
2,
3]. it is worth noting that moderate gaming has been associated with benefits such as improved cognitive functions and social skills [
4].
In the context of defining IGD, the World Health Organization (WHO) employs an alternative term, “Gaming Disorder” (GD), in the 11th Revision of the International Classification of Diseases (ICD-11). According to the ICD-11, GD encompasses both online and offline gaming behavior [
5].
However, the diagnostic criteria for IGD (DSM-5) and GD (ICD-11) are not entirely identical. IGD is an emerging disorder requiring further study, whereas GD signifies a formal recognition of the disorder. To diagnose IGD, the DSM-5 outlines nine criteria, including preoccupation with gaming, withdrawal symptoms, tolerance, loss of control, loss of interest in previous hobbies and entertainment, continued excessive use despite psychosocial issues, deceiving family members or therapists regarding the amount of gaming, use of gaming to escape or relieve negative moods, and significant impairment or distress. Conversely, ICD-11defines GD as a pattern of gaming behavior characterized by impaired control over gaming, increasing priority given to gaming over other activities to the extent that gaming takes precedence over other interests and daily activities, and continuation or escalation of gaming despite the occurrence of negative consequences [
6].
Some studies suggest that the measurement tools for GD and IGD exhibit factorial invariance, indicating stability across different populations and settings [
6]. Conversely, other studies report lower concordance between the two measures, indicating a lower degree of agreement [
1]. Furthermore, research has illuminated that there is a 73% overlap in the diagnostic criteria of IGD and GD [
7], yet this partial overlap does not justify the use of these terms interchangeably, as each set of criteria captures unique aspects of gaming disorders [
8].
The discrepancy in the measurement tools and their criteria has implications for the perceived prevalence of pathological gaming behaviors. A lack of consensus among researchers regarding diagnostic standards may result in false-positive diagnoses, inflating prevalence rates and potentially stigmatizing non-pathological gaming behaviors [
9].
It is imperative for the clinical and research communities to strive towards a unified diagnostic framework that can accurately identify and differentiate between pathological gaming behaviors and non-pathological engagement. Such harmonization would not only refine the diagnostic process but also enhance the quality of interventions and the interpretability of outcomes across different cultural and clinical contexts [
10].
1.1. Differences in Prevalence under Different Diagnostic Criteria
The prevalence of IGD varies significantly across studies, with recent analyses revealing rates ranging from 0.7% to 27.5% in various populations. This wide range underscores the complexity and variability of IGD, reflecting its impact across diverse demographic and geographical groups [
11]
The global prevalence of gaming disorders varies significantly across studies due to methodological differences, including the choice of screening tools and sampling criteria. A systematic review and meta-analysis reported a worldwide prevalence of 3.05%, with estimates adjusted to 1.96% when considering studies that met more stringent sampling criteria. Variability in prevalence rates is also influenced by factors such as the assessment tool used, participant age and sex, and region of the study [
12].
Considering the above, this study aimed to further organize issues related to gaming disorders and conduct a meta-analysis to avoid stigmatizing general users of games (players without dependency symptoms, e-sports athletes, and game industry employees). It seeks to clarify the impact of different gaming disorder diagnostic criteria (DSM-5 and ICD-11) and factors such as region on gaming disorder."
In the assessment of GD researchers have developed various tools. The first such tool, known as the Gaming Disorder Test (GDT), is designed to evaluate the severity and consequences of gaming behavior rather than to provide a clinical diagnosis [
9].
The second tool, the Gaming Disorder Scale for Adolescents (GADIS-A), comprises ten items that gauge the extent and impact of gaming behavior on adolescents. This scale evaluates criteria such as preoccupation with gaming, withdrawal symptoms, tolerance, and interference with personal and social functioning [
13].
The GAMES test is a screening tool consisting of nine items. It was developed in Japan for the purpose of screening gaming disorder, which is included in the WHO’s ICD-11. In the research sample, this test demonstrated a sensitivity and specificity of 98%, with a positive predictive value of 91%. The GAMES test comprises two factors and exhibits high internal consistency and test-retest reliability [
1].
While the GDT is instrumental in gauging the severity and consequences of gaming habits, its recommended threshold values have not been empirically validated, which limits its use in ascertaining the prevalence of GD. Consequently, the GADIS-A and GAMES are the scales currently available for effectively measuring the prevalence of GD, as they have been subject to more rigorous validation processes.
The assessment of IGD has several scales, notably the IGDT-10 and IGUESS. The IGDT-10 evaluates symptoms aligned with DSM-5 criteria [
14], while IGUESS measures gaming's cognitive and emotional effects [
15]. Compared to GD, the array of IGD scales reflects its established presence in research, offering diverse tools for understanding this behavioral phenomenon.
1.2. The Impact of Cultural Background
The impact of cultural background on IGD is significant, as one study suggests that individualistic and collectivistic cultural orientations can influence IGD [
16,
17]. This study identified two profiles of Internet gamers, showing that those with fewer collectivistic tendencies exhibited higher IGD behaviors. This underscores the need for culturally tailored strategies for the prevention and intervention of IGD.
A comprehensive meta-analysis highlighted that the prevalence of GD in East Asia is notably higher than in other regions of the world, with an overall pooled prevalence of 12%. This suggests significant regional differences that could be attributed to various cultural and societal factors unique to East Asian countries [
18].
Research on IGD in Japan shows that it is considered a new lifestyle-related disease among children and adolescents, indicating a high concern for game addiction owing to its psychological and social impacts. Despite Japan's prominent gaming culture, studies on IGD are less frequent than those in China and South Korea. This highlights the need for expanded research in Japan and other under-studied regions to better understand IGD's prevalence and impact of IGD and its impact across different cultural contexts [
19].
1.3. The Present Study
This study conducted a meta-analysis of the prevalence of IGD based on two diagnostic criteria: DSM-5 and ICD-11. Unlike previous meta-analyses, this study excluded research focused on tool development or scale validation to obtain more accurate data and studies that did not clearly define IGD/GD or employ related assessment tools to better distinguish between IGD and Internet addiction. The specific objectives were to (1) assess the overall prevalence of IGD in the past five years and (2) examine the differences in IGD prevalence across various characteristics (country, sample size, diagnostic criteria, quality score, and measurement tools). This will provide accurate data on IGD prevalence rates, aid in further identification and prevention of IGD, and inform policy and treatment research.
2. Method
2.1. Protocol and Registration
This meta-analysis followed the preferred reporting items for systematic reviews and meta-analysis (PRISMA) standards as the framework for the methodology. Before initiating the analysis, the research protocol was formally registered with the International Prospective Register of Systematic Reviews (PROSPERO:CRD42024522606) to ensure transparency and compliance with established guidelines.
2.2. Search Strategy and Study Selection
To identify relevant studies, two authors independently conducted a comprehensive search across multiple databases, including PubMed, Web of Science covering all records up to January 2024. The following search terms with combinations of keywords were used: ("video game" OR "video gaming" OR "online game" OR "online gaming" OR "computer game" OR "computer gaming" OR "internet game" OR “internet gaming”) AND ("excessive" OR "problematic" OR "problem" OR "pathological" OR "disorder" OR "addiction" OR "addicted”) AND "prevalence”. Furthermore, the reference lists of the included studies and relevant meta-analyses or reviews were manually scrutinized for additional sources.
2.3. Inclusion and Exclusion Criteria
The inclusion criteria for this meta-analysis were as follows: (1) original research articles written in English; (2) studies published in peer-reviewed journals between March 1, 2014, and March 1, 2024; (3) research with a clear definition of IGD involving online gaming disorder/addiction, distinguishing it from general Internet addiction; (4) studies reporting IGD prevalence rates; and (5) research available in full text.
The exclusion criteria were as follows: (1) studies with incomplete data or duplicate publications; (2) studies without specified DSM-5 or ICD-11 diagnostic criteria; and (3) studies focusing on specific populations (e.g., religious figures, psychiatric patients).
2.4. Data Extraction
Data were systematically extracted using a predefined template. Two authors independently extracted data, which were then verified by a third author, including author names, publication year, study location, population type (general or gamers), sample size, assessment tools with cut-off values, and IGD prevalence rates. For longitudinal studies, only baseline data were considered. Studies covering multiple countries/regions have listed their data separately for each location.
2.5. Quality Evaluation
To assess the quality of our meta-analysis, an 11-item checklist developed by the Agency for Healthcare Research and Quality (AHRQ) was employed. This checklist covers various dimensions of study quality, such as clarity of research objectives, appropriateness of study design, representativeness of the study sample, validity and reliability of measurement tools, adequacy of statistical analysis methods, and consideration of potential sources of bias. Two reviewers independently evaluated each study based on these criteria. Any discrepancies in the assessments were resolved through discussion or consultation with a third reviewer. This systematic approach ensured a thorough evaluation of study quality and bolstered the reliability of our meta-analysis findings.
2.6. Statistical Analyses
In the statistical analyses of our meta-analysis, we initially conducted a meta-analysis using the "meta prop" package in Stata 18.0. The I2 statistic was used to assess the heterogeneity among studies. I2 describes the percentage of total variation across studies owing to heterogeneity rather than chance. Owing to the substantial heterogeneity observed among the studies (I2 = 99%), we utilized a random-effects model to estimate the overall prevalence of IGD and its 95% confidence interval (CI).
Consequently, four characteristics were considered potential influencing factors: country (based on the region where the study was conducted), sample size (categorized as less than 1000/ more than 1000), quality score (classified as high/medium/low), and assessment tool (DSM-5/ICD-11). Additionally, a meta-regression was performed based on the subgroup analysis results to further identify the sources of heterogeneity.
Publication bias was examined using Egger's test and Begg's test, with P < 0.05 indicating the presence of publication bias. A sensitivity analysis was conducted to determine the studies with the greatest impact on the summary estimates and to assess the robustness of the estimates.
3. Results
3.1. Study Characteristics
The initial literature search, conducted across two databases (PubMed: n = 344, Web of Science: n = 967), yielded a combined total of 1311 records. After excluding 273 duplicates, we screened 1038 records based on their titles and abstracts, as illustrated in
Figure 1. During this screening process, 934 records were excluded for various reasons. including those that were irrelevant to the topic, did not meet the predetermined inclusion criteria, or were not original research articles. As a result, we identified 104 records for potential inclusion. Further examination and full-text reading led to the exclusion of an additional 87 articles. However, we found six pertinent articles by adding references from the remaining studies, relevant meta-analyses, and recently published reviews. This brought the total number of relevant articles to 110.To address the imbalance between studies using the two different criteria, we performed a random selection of studies, resulting in the exclusion of 93 articles. Ultimately, 17 studies met the criteria and were incorporated into the systematic review and meta-analysis [
1,
14,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31,
32].
Table 1 summarizes the characteristics of the studies included in the meta-analysis. These studies span various regions, with concentrations in China, Japan, Korea, and other countries such as Iran, Russia, Turkey, Germany, France, and India. The publication years of these studies ranged from 2018 to 2023, and a total of 17141 participants. Most studies focused on young demographics, with only one study targeting a group of parents.
A diverse array of scales was employed to assess gaming addiction, with the ICD-11 criteria used in a subset of studies and the DSM-5 criteria adopted in other studies. The scales used included the GADIS-A, GAMES, IGDT-10, IGDS-SF9, and IGUESS, with varying cut-off points for defining addiction.
The quality scores of the included studies evaluated using the Agency for Healthcare Research and Quality scale ranged from 7 to 9, indicating that most studies were of moderate to high quality. None of the studies were deemed low quality. The prevalence of gaming disorders reported in these studies varied, reflecting the diverse methodologies and sample characteristics across the studies.
3.2. Prevalence of IGD
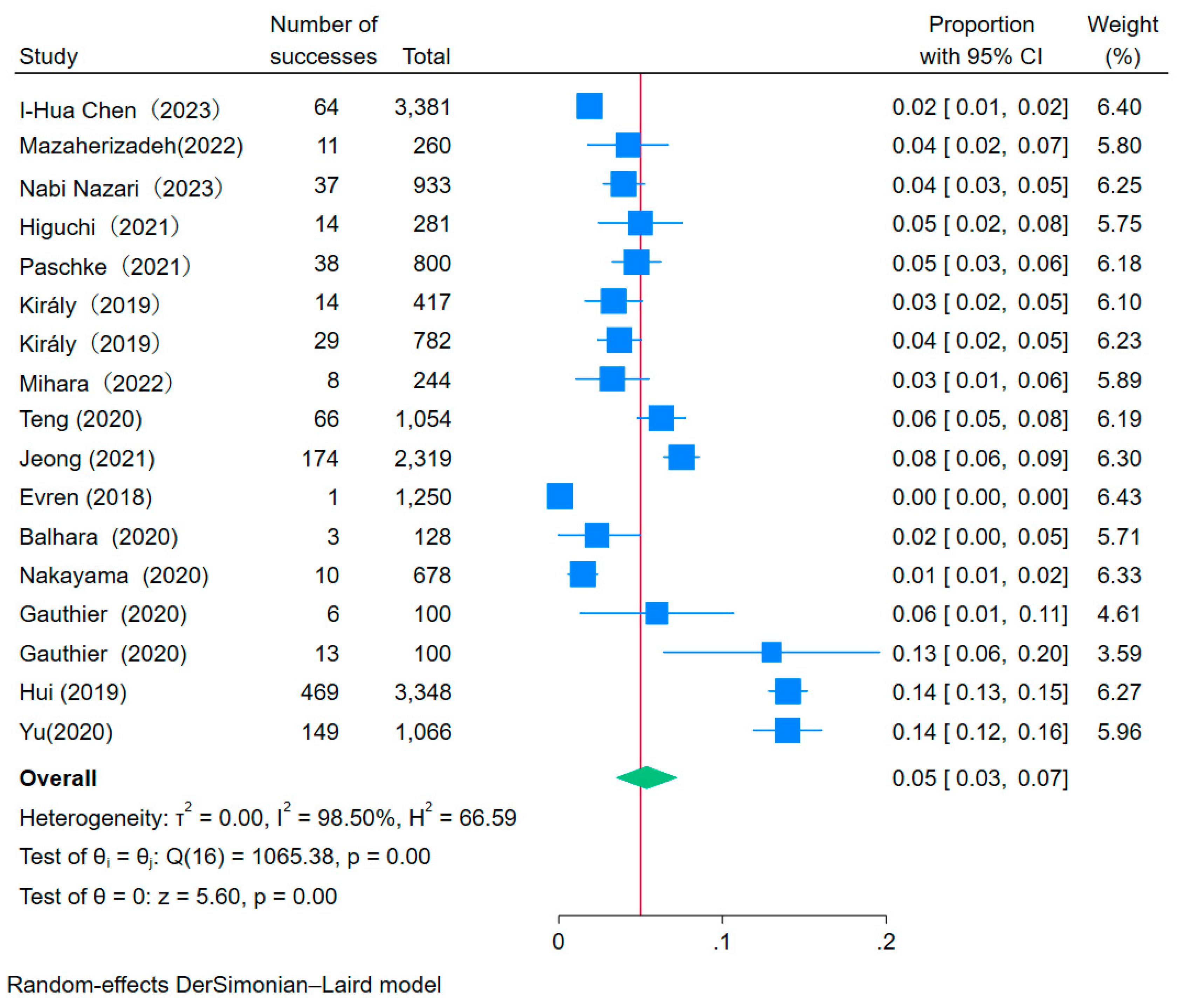
The heterogeneity test revealed a pronounced disparity across the studies included in the meta-analysis, with an I² value of 98.50% (P < 0.001), signifying a considerable level of heterogeneity. Accordingly, a random-effects model was used to compute the pooled prevalence of IGD. The forest plot, as shown in
Figure 2, illustrates the individual study prevalence ranging from 0.01% to 13.60%, indicating a considerable range across studies. The overall aggregate prevalence of IGD was 5.00%, with a 95% confidence interval (CI) extending from 3.00% to 7.00%. This estimate represents the general occurrence of IGD within the populations examined across 17 distinct studies, each characterized by varied sample sizes, measurement scales, and quality scores.
3.3. Subgroup and Meta-Regression Analyses
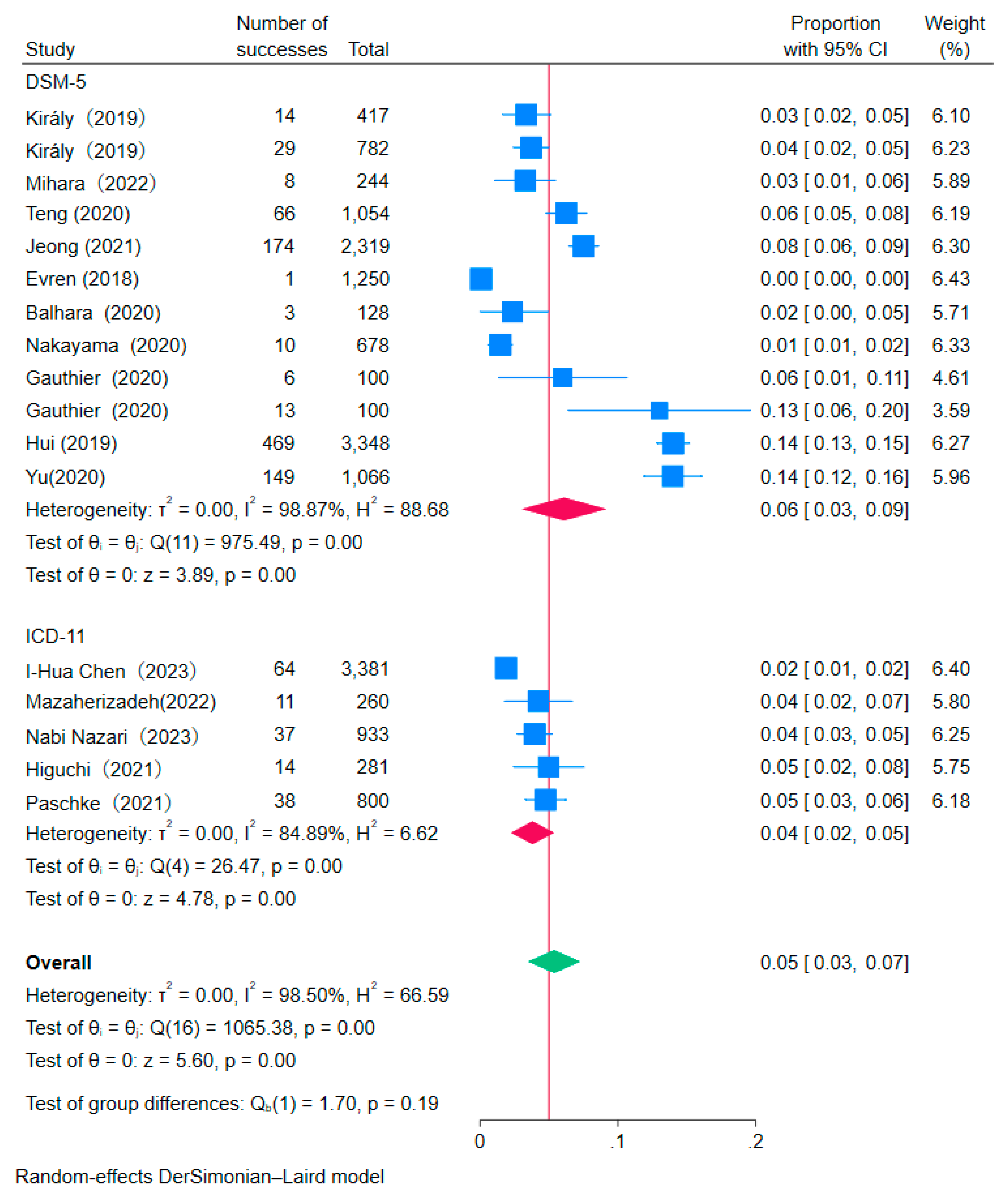
The subgroup analysis presented in the table and corresponding figure demonstrates variability in the prevalence of IGD across different variables, although not all subgroup differences reached statistical significance (
Figure 3).
In terms of study location, the prevalence of IGD varies by region. Asian studies (k=12) report a prevalence of 5% with a 95% confidence interval (CI) ranging from 3% to 8%. European studies (k=5), however, show a slightly lower prevalence of 4%, with a 95% CI of 3% to 5%. The differences in prevalence rates between these geographical locations do not reach statistical significance (P= 0.46).
In terms of Sample Size, studies with more than 1000 participants show an IGD prevalence of 7% (95% CI: 0.04-0.11), in contrast to a 4% prevalence (95% CI: 0.03-0.05) in studies with 1000 or fewer participants, although this difference does not achieve statistical significance (P = 0.07).
The diverse Scales employed in these studies reflect the variance in IGD prevalence. For instance, studies utilizing the GADIS scale report a 4% prevalence (95% CI: 0.02-0.05), whereas those adopting the IGUESS scale indicate a significantly higher prevalence at 14% (95% CI: 0.13-0.15). The observed differences were statistically significant (P <0.001).
Variations are also discernible based on the diagnostic criteria,studies adhering to GD a 4% prevalence (95% CI: 0.02-0.05) compared to a 6% prevalence (95% CI: 0.03-0.09) for IGD, with no significant difference (P =0.19).
Finally, Studies with a QS of 9 show a prevalence of 6% (95% CI: 0.03-0.08) versus a 4% prevalence (95% CI: 0.03-0.06) for studies with a QS less than 9. with no significant difference (P =0.29).
Table 2.
Subgroup analyses.
Table 2.
Subgroup analyses.
| Variable |
Subgroup |
k |
Prevalence |
95% CI |
P Significance test(s) |
| Study location |
Asia |
12 |
0.05 |
0.03 |
0.08 |
0.46 |
| |
European |
5 |
0.04 |
0.03 |
0.05 |
|
| |
|
|
|
|
|
|
| Sample size |
>1000 |
6 |
0.07 |
0.04 |
0.11 |
0.07 |
| |
<1000 |
11 |
0.04 |
0.03 |
0.05 |
|
| |
|
|
|
|
|
|
| |
|
|
|
|
|
|
| Scale |
GADIS |
4 |
0.04 |
0.02 |
0.05 |
0<0.001** |
| |
GAMES |
1 |
0.05 |
0.03 |
0.08 |
|
| |
IGDT |
6 |
0.04 |
0.02 |
0.05 |
|
| |
IGDS |
3 |
0.03 |
0.02 |
0.07 |
|
| |
DSM-5 |
2 |
0.08 |
0.06 |
0.09 |
|
| |
IGUESS |
1 |
0.14 |
0.13 |
0.15 |
|
| |
|
|
|
|
|
|
| criteria |
ICD-11 |
5 |
0.04 |
0.02 |
0.05 |
0.19 |
| |
DSM-5 |
12 |
0.06 |
0.03 |
0.09 |
|
| |
|
|
|
|
|
|
| QS |
9 |
4 |
0.06 |
0.03 |
0.08 |
0.29 |
| |
<9 |
13 |
0.04 |
0.03 |
0.06 |
|
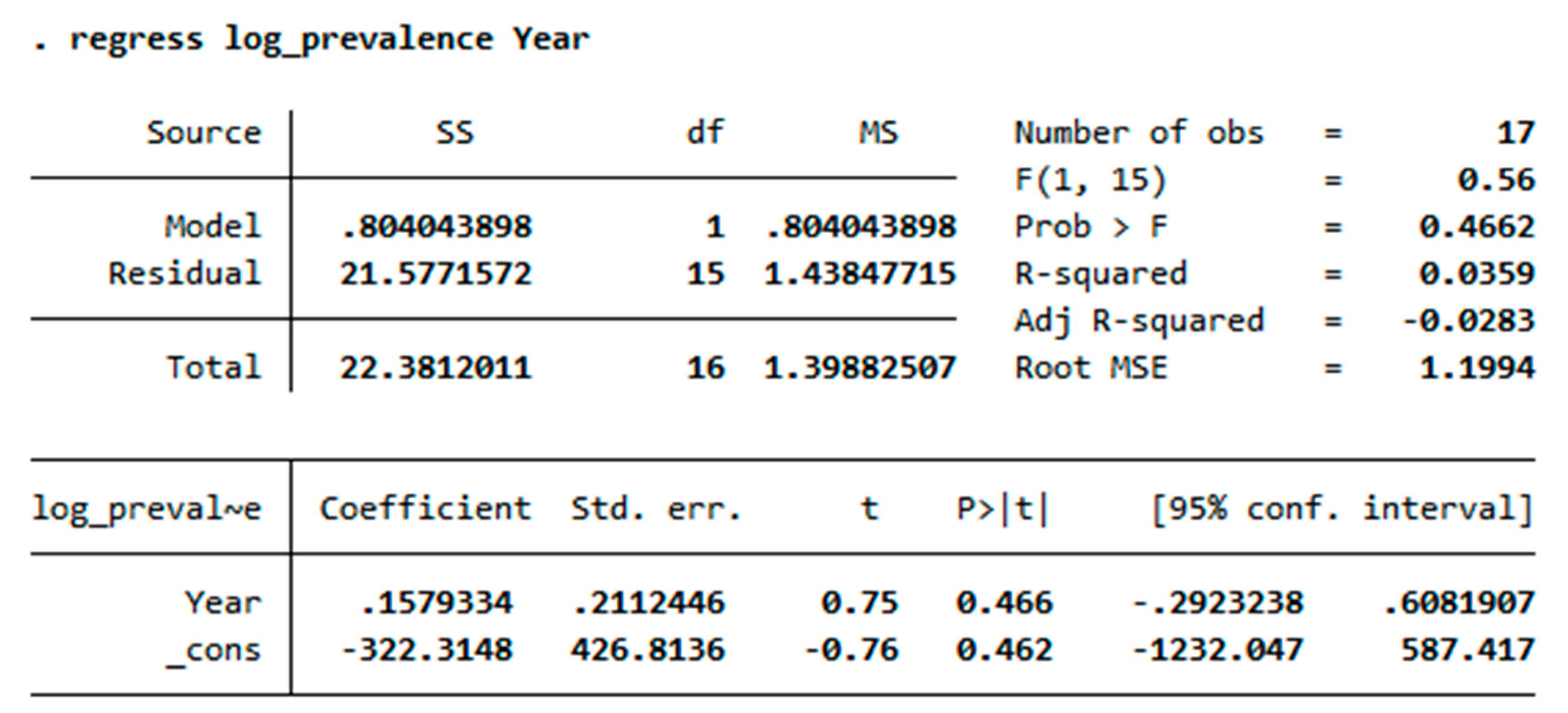
3.4. Trend Analysis between Year and Prevalence of IGD
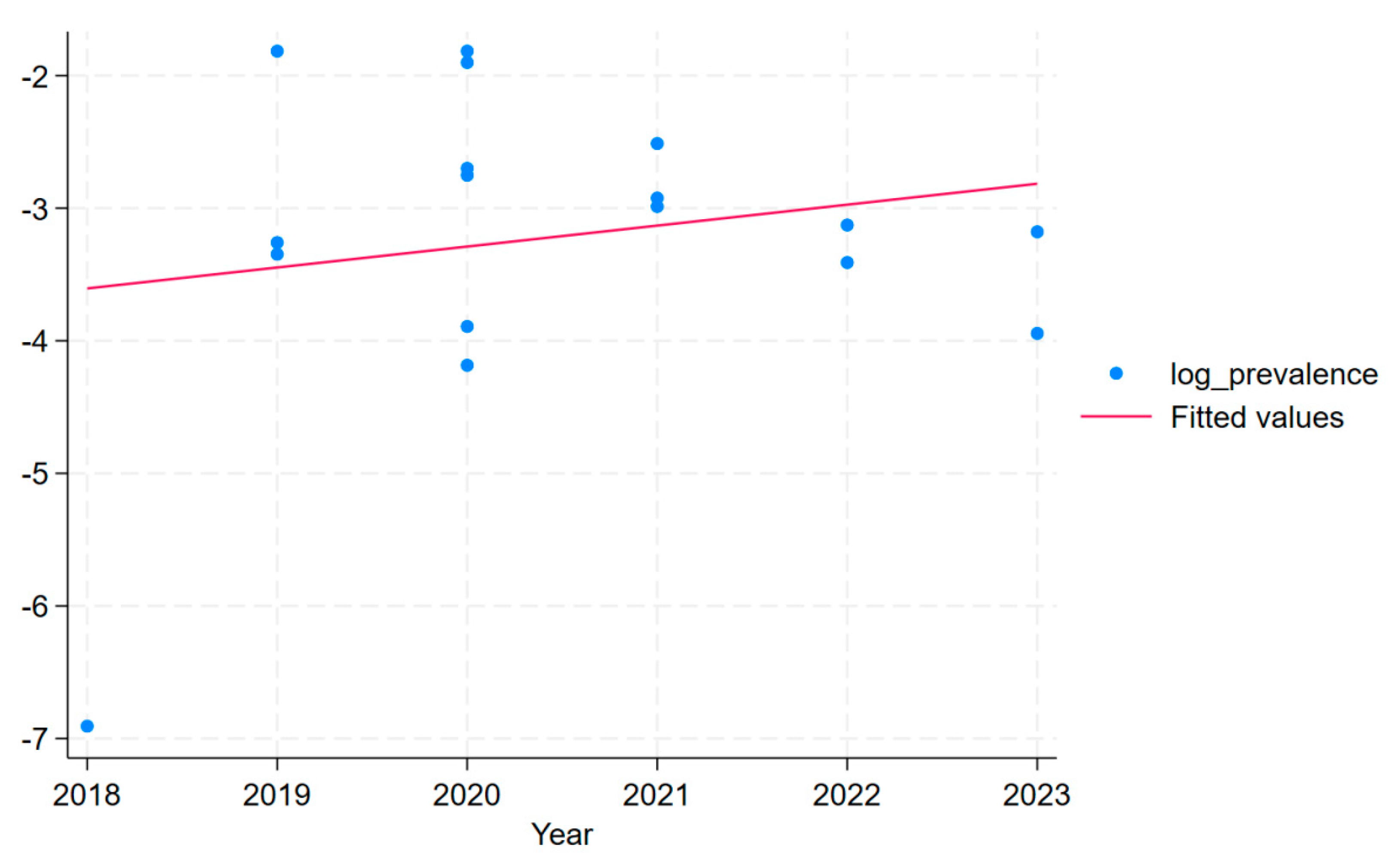
Trend analysis (
Figure 4) suggested that there was no statistically significant association between the year and prevalence of IGD. This conclusion is based on the p-value of 0.47 for the year coefficient (
Table 3), indicating that the year does not predict the prevalence of IGD significantly. The R-squared value of 0.036 indicates that the year variable explains about 3.59% of the variability in the prevalence of IGD, which is not significant.
3.5. Publication Bias and Sensitivity Analysis
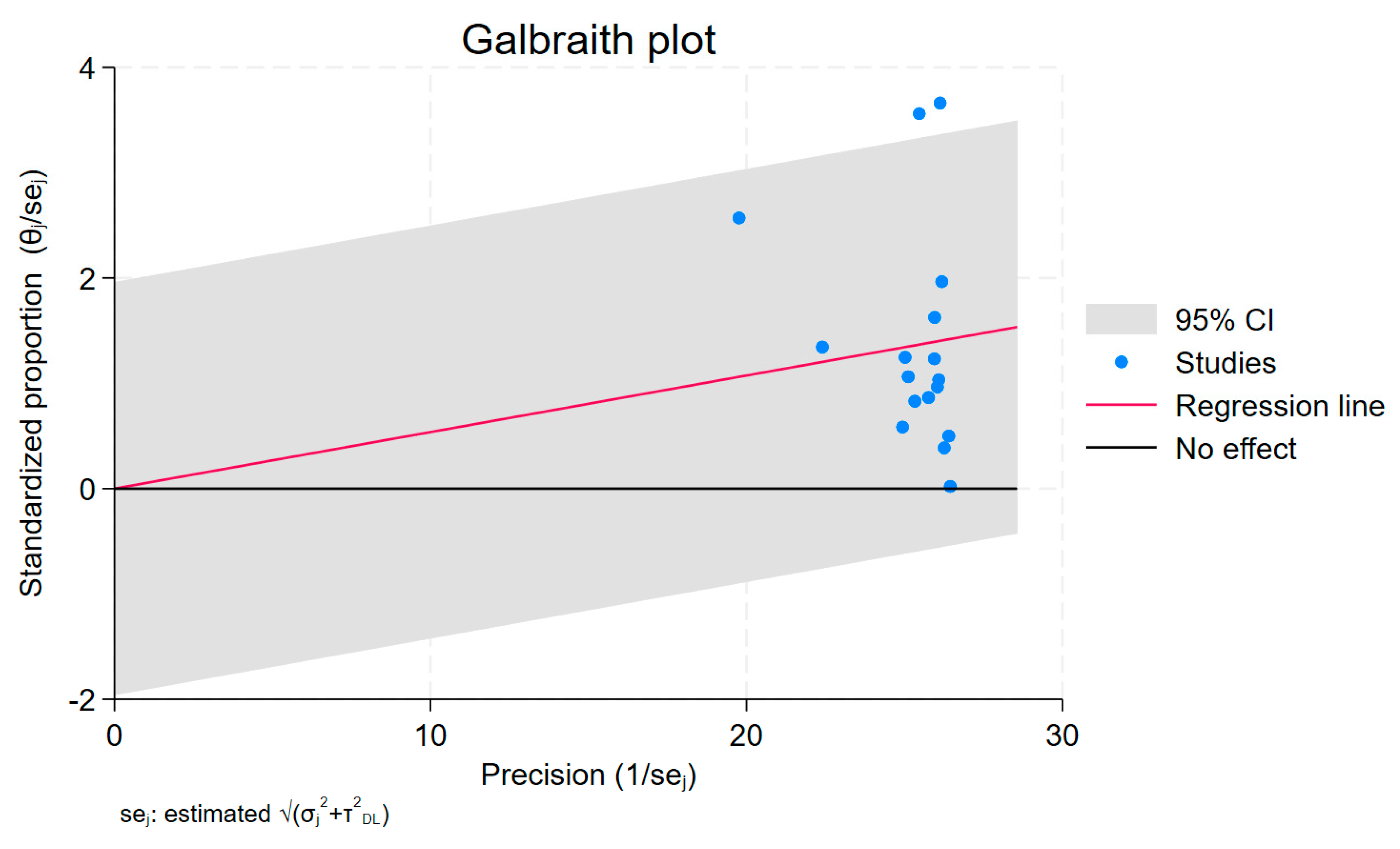
Egger’s test (z=0.30, P>0.05) and Begg’s test (z=0.16, P>0.05) revealed minimal bias in this study. Most studies in the funnel plot exhibit small bias (
Figure 5).
4. Discussion
In this meta-analysis, we found that the prevalence of IGD was 5%. This result contrasts somewhat with the findings of several other studies. For example, a meta-analysis including studies published before March 2020 reported a lower prevalence of IGD, at around 3.3% [
33], while a more recent meta-analysis published in 2022 focusing on young people showed an increased prevalence of 4.6% [
34].
These differences may reflect the influence of several key factors.Firstly, the increasing prevalence of the internet is likely a major contributing factor to the rising prevalence of IGD. As internet access becomes more widespread and convenient, a greater number of individuals are exposed to online games, thereby increasing the potential risk of IGD [
35]. Furthermore, the proliferation of smartphones and tablets may also contribute to this trend, as they provide users with increased opportunities to access and engage in online gaming [
36].Secondly, the perception of the COVID-19 pandemic may also increase the risk of IGD, as it can lead to increased symptoms of depression and anxiety, which are known to be associated with IGD [
37].
The results of this study suggest that the prevalence of IGD based on the ICD-11 cross-sectional criteria is not significantly higher than the prevalence based on the DSM-5 criteria. This indicates that the two diagnostic criteria have good consistency in identifying IGD cases.
However, there was a significant difference in the prevalence of having the disease between the different scales, For example, the GADIS showed a prevalence of 4%, whereas the IGUESS reported a substantially higher prevalence of 14% (P < 0.001). Meanwhile,this study found that the prevalence obtained using scales based on the DSM-5 diagnostic criteria had a large range, while those using scales based on the ICD-11 diagnostic criteria were more stable and had lower heterogeneity.
This discrepancy may stem from the uneven weighting of the nine symptoms in the DSM-5 criteria, with some symptoms potentially more important for diagnosing IGD. For example, loss of control over gaming behavior and preoccupation with gaming are likely to be core symptoms of IGD [
38], while other symptoms such as salience of gaming and withdrawal symptoms may be secondary manifestations of IGD. When diagnostic scales measure similar concepts, setting a more lenient cut-off point will identify more individuals. However, this may lead to increased internal heterogeneity in the diagnosed group [
39].Therefore, giving items equal weight in a scale could introduce measurement errors in IGD assessment.
A limitation of this study is the scarcity of research on IGD using ICD-11 diagnostic criteria, necessitating further investigation to ensure a comprehensive regional assessment.
Studies have concluded that culture can influence IGD [
10].To enhance the robustness of the findings, future research should adopt a more inclusive approach that encompasses all countries, utilizing both the DSM-5 and ICD-11 criteria to paint a more accurate picture of IGD prevalence. This will contribute significantly to the global understanding of IGD and its impact on public health.
Research on IGD is relatively scarce in some countries, such as Japan. The influence of the gaming industry in this region cannot be overlooked [
40], Future studies on the prevalence of IGD in different cultures should be increased to help us better understand the impact of culture on IGD. [
18].
5. Conclusions
This study provides a comprehensive assessment of the prevalence of IGD across different regions and populations, revealing a complex picture influenced by various factors. Varied methodological approaches, such as different scales and diagnostic criteria (ICD-11 and DSM-5), complicate direct comparisons across studies. This would facilitate accurate epidemiological assessments and inform targeted interventions. The observed variations in IGD prevalence underscore the need for localized research to address the nuanced cultural and regulatory landscapes that influence gaming behaviors. Overall, the findings call for a nuanced understanding of IGD, accounting for regional, cultural, and methodological factors to effectively address this growing concern.
Author Contributions
RYZ, NM, YO and TS contributed to the study’s concept and design. XYZ conducted the statistical analysis.MO and WJY reviewed the manuscript. RYZ wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This work is Support from Pioneering Research Initiated by the Next Generation, SPRING in Japan.
Institutional Review Board Statement
No ethical review is required for this article.
Acknowledgments
The datasets generated and/or analyzed in this study are not publicly available because they contain information that may compromise the privacy of study participants. Data supporting the results of this study are available upon request from the corresponding author.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Higuchi, S.; Osaki, Y.; Kinjo, A.; Mihara, S.; Maezono, M.; Kitayuguchi, T.; Matsuzaki, T.; Nakayama, H.; Rumpf, H.-J.; Saunders, J.B. Development and Validation of a Nine-Item Short Screening Test for ICD-11 Gaming Disorder (GAMES Test) and Estimation of the Prevalence in the General Young Population. JBA 2021, 10, 263–280. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Jeong, J.-E.; Cho, H.; Jung, D.-J.; Kwak, M.; Rho, M.J.; Yu, H.; Kim, D.-J.; Choi, I.Y. Personality Factors Predicting Smartphone Addiction Predisposition: Behavioral Inhibition and Activation Systems, Impulsivity, and Self-Control. PLoS ONE 2016, 11, e0159788. [Google Scholar] [CrossRef] [PubMed]
- Liao, Z.; Huang, Q.; Huang, S.; Tan, L.; Shao, T.; Fang, T.; Chen, X.; Lin, S.; Qi, J.; Cai, Y.; et al. Prevalence of Internet Gaming Disorder and Its Association With Personality Traits and Gaming Characteristics Among Chinese Adolescent Gamers. Front. Psychiatry 2020, 11, 598585. [Google Scholar] [CrossRef] [PubMed]
- Granic, I.; Lobel, A.; Engels, R.C.M.E. The Benefits of Playing Video Games. American Psychologist 2014, 69, 66–78. [Google Scholar] [CrossRef] [PubMed]
- Reed, G.M.; First, M.B.; Kogan, C.S.; Hyman, S.E.; Gureje, O.; Gaebel, W.; Maj, M.; Stein, D.J.; Maercker, A.; Tyrer, P.; et al. Innovations and Changes in the ICD-11 Classification of Mental, Behavioural and Neurodevelopmental Disorders. World Psychiatry 2019, 18, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.-Y.; Cheng, C. Psychometric Evaluation and Comparison of Two Gaming Disorder Measures Derived From the DSM-5 and ICD-11 Frameworks. Front. Psychiatry 2020, 11, 577366. [Google Scholar] [CrossRef] [PubMed]
- Tuncturk, M.; Karacetin, G.; Ermis, C.; Ciray, R.O.; Can, M.; Yesilkaya, C.; Atay, A.; Alkas, G.E.; Kasap, D.; Guney, O.; et al. Rate of Overlap between ICD-11 Gaming Disorder and DSM-5 Internet Gaming Disorder along with Turkish Reliability of the Gaming Disorder Scale for Adolescents (GADIS-A). Dubai Med J 2023, 6, 291–300. [Google Scholar] [CrossRef]
- Starcevic, V.; Choi, T.Y.; Kim, T.H.; Yoo, S.-K.; Bae, S.; Choi, B.-S.; Han, D.H. Internet Gaming Disorder and Gaming Disorder in the Context of Seeking and Not Seeking Treatment for Video-Gaming. Journal of Psychiatric Research 2020, 129, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Pontes, H.M.; Schivinski, B.; Sindermann, C.; Li, M.; Becker, B.; Zhou, M.; Montag, C. Measurement and Conceptualization of Gaming Disorder According to the World Health Organization Framework: The Development of the Gaming Disorder Test. Int J Ment Health Addiction 2021, 19, 508–528. [Google Scholar] [CrossRef]
- Stavropoulos, V.; Baynes, K.L.; O’Farrel, D.L.; Gomez, R.; Mueller, A.; Yucel, M.; Griffiths, M. Inattention and Disordered Gaming: Does Culture Matter? Psychiatr Q 2020, 91, 333–348. [Google Scholar] [CrossRef]
- Zhu, L.; Zhu, Y.; Li, S.; Jiang, Y.; Mei, X.; Wang, Y.; Yang, D.; Zhao, J.; Mu, L.; Wang, W. Association of Internet Gaming Disorder with Impulsivity: Role of Risk Preferences. BMC Psychiatry 2023, 23, 754. [Google Scholar] [CrossRef] [PubMed]
- Stevens, M.W.; Dorstyn, D.; Delfabbro, P.H.; King, D.L. Global Prevalence of Gaming Disorder: A Systematic Review and Meta-Analysis. Aust N Z J Psychiatry 2021, 55, 553–568. [Google Scholar] [CrossRef] [PubMed]
- Paschke, K.; Austermann, M.I.; Thomasius, R. Assessing ICD-11 Gaming Disorder in Adolescent Gamers: Development and Validation of the Gaming Disorder Scale for Adolescents (GADIS-A). JCM 2020, 9, 993. [Google Scholar] [CrossRef] [PubMed]
- Király, O.; Bőthe, B.; Ramos-Diaz, J.; Rahimi-Movaghar, A.; Lukavska, K.; Hrabec, O.; Miovsky, M.; Billieux, J.; Deleuze, J.; Nuyens, F.; et al. Ten-Item Internet Gaming Disorder Test (IGDT-10): Measurement Invariance and Cross-Cultural Validation across Seven Language-Based Samples. Psychology of Addictive Behaviors 2019, 33, 91–103. [Google Scholar] [CrossRef] [PubMed]
- Jo, S.; Yim, H.W.; Lee, H.; Lee, H.C.; Choi, J.; Baek, K. The Internet Game Use-Elicited Symptom Screen Proved to Be a Valid Tool for Adolescents Aged 10–19 Years. Acta Paediatrica 2018, 107, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulos, V.; Anderson, E.E.; Beard, C.; Latifi, M.Q.; Kuss, D.; Griffiths, M. A Preliminary Cross-Cultural Study of Hikikomori and Internet Gaming Disorder: The Moderating Effects of Game-Playing Time and Living with Parents. Addictive Behaviors Reports 2019, 9, 100137. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulos, V.; Frost, T.M.J.; Brown, T.; Gill, P.; Footitt, T.A.; Kannis-Dymand, L. Internet Gaming Disorder Behaviours: A Preliminary Exploration of Individualism and Collectivism Profiles. BMC Psychiatry 2021, 21, 262. [Google Scholar] [CrossRef] [PubMed]
- Liao, Z.; Chen, X.; Huang, Q.; Shen, H. Prevalence of Gaming Disorder in East Asia: A Comprehensive Meta-Analysis. JBA 2022, 11, 727–738. [Google Scholar] [CrossRef] [PubMed]
- Imataka, G.; Sakuta, R.; Maehashi, A.; Yoshihara, S. Current Status of Internet Gaming Disorder (IGD) in Japan: New Lifestyle-Related Disease in Children and Adolescents. JCM 2022, 11, 4566. [Google Scholar] [CrossRef]
- Paschke, K.; Austermann, M.I.; Thomasius, R. Assessing ICD-11 Gaming Disorder in Adolescent Gamers by Parental Ratings: Development and Validation of the Gaming Disorder Scale for Parents (GADIS-P). JBA 2021, 10, 159–168. [Google Scholar] [CrossRef]
- Chen, I.-H.; Chang, Y.-L.; Yang, Y.-N.; Yeh, Y.-C.; Ahorsu, D.K.; Adjorlolo, S.; Strong, C.; Hsieh, Y.-P.; Huang, P.-C.; Pontes, H.M.; et al. Psychometric Properties and Development of the Chinese Versions of Gaming Disorder Test (GDT) and Gaming Disorder Scale for Adolescents (GADIS-A). Asian Journal of Psychiatry 2023, 86, 103638. [Google Scholar] [CrossRef] [PubMed]
- Mazaherizadeh, A.; Taherifar, Z.; Farahani, H. Psychometric Properties of the Farsi Version of the Gaming Disorder Scale for Adolescents (GADIS-A). BMC Psychol 2022, 10, 195. [Google Scholar] [CrossRef] [PubMed]
- Nazari, N.; Shabbir, M.S.; Sevbitov, A.V.; Sadeghi, M.; Griffiths, M.D. Psychometric Evaluation of the Russian Version of the Gaming Disorder Scale for Adolescents. Curr Psychol 2023, 42, 13754–13768. [Google Scholar] [CrossRef] [PubMed]
- Mihara, S.; Osaki, Y.; Kinjo, A.; Matsuzaki, T.; Nakayama, H.; Kitayuguchi, T.; Harada, T.; Higuchi, S. Validation of the Ten-Item Internet Gaming Disorder Test (IGDT-10) Based on the Clinical Diagnosis of IGD in Japan. JBA 2022, 11, 1024–1034. [Google Scholar] [CrossRef]
- Nakayama, H.; Matsuzaki, T.; Mihara, S.; Kitayuguchi, T.; Higuchi, S. Relationship between Problematic Gaming and Age at the Onset of Habitual Gaming. Pediatrics International 2020, 62, 1275–1281. [Google Scholar] [CrossRef] [PubMed]
- Teng, Z.; Griffiths, M.D.; Nie, Q.; Xiang, G.; Guo, C. Parent–Adolescent Attachment and Peer Attachment Associated with Internet Gaming Disorder: A Longitudinal Study of First-Year Undergraduate Students. J Behav Addict 2020, 9, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.; Yim, H.W.; Lee, S.; Lee, H.K.; Potenza, M.N.; Lee, H. Factors Associated with Severity, Incidence or Persistence of Internet Gaming Disorder in Children and Adolescents: A 2-year Longitudinal Study. Addiction 2021, 116, 1828–1838. [Google Scholar] [CrossRef] [PubMed]
- Evren, C.; Dalbudak, E.; Topcu, M.; Kutlu, N.; Evren, B.; Pontes, H.M. Psychometric Validation of the Turkish Nine-Item Internet Gaming Disorder Scale–Short Form (IGDS9-SF). Psychiatry Research 2018, 265, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Balhara, Y.S.; Kattula, D.; Singh, S.; Chukkali, S.; Bhargava, R. Impact of Lockdown Following COVID-19 on the Gaming Behavior of College Students. Indian J Public Health 2020, 64, 172. [Google Scholar] [CrossRef]
- Gauthier, B.; Rolland, B.; Berthiller, J.; Tatou, M.; Charvet, D.; Gansel, Y.; Fleury, R.; Saoud, M.; Laconi, S. Need for Systematic Screening for IGD in Adolescent Psychiatric Inpatients. L’Encéphale 2020, 46, 420–426. [Google Scholar] [CrossRef]
- Hui, B.P.H.; Wu, A.M.S.; Pun, N. Disentangling the Effects of Empathy Components on Internet Gaming Disorder: A Study of Vulnerable Youth in China. J Behav Addict 2019, 8, 181–189. [Google Scholar] [CrossRef]
- Yu, Y.; Yang, X.; Wang, S.; Wang, H.; Chang, R.; Tsamlag, L.; Zhang, S.; Xu, C.; Yu, X.; Cai, Y.; et al. Serial Multiple Mediation of the Association between Internet Gaming Disorder and Suicidal Ideation by Insomnia and Depression in Adolescents in Shanghai, China. BMC Psychiatry 2020, 20, 460. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Son, G.; Roh, E.-B.; Ahn, W.-Y.; Kim, J.; Shin, S.-H.; Chey, J.; Choi, K.-H. Prevalence of Gaming Disorder: A Meta-Analysis. Addictive Behaviors 2022, 126, 107183. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.-X.; Wang, J.-Y.; Dong, G.-H. The Prevalence and Possible Risk Factors of Internet Gaming Disorder among Adolescents and Young Adults: Systematic Reviews and Meta-Analyses. Journal of Psychiatric Research 2022, 154, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Kuss, D.J.; Van Rooij, A.J.; Shorter, G.W.; Griffiths, M.D.; Van De Mheen, D. Internet Addiction in Adolescents: Prevalence and Risk Factors. Computers in Human Behavior 2013, 29, 1987–1996. [Google Scholar] [CrossRef]
- Yuan, G.; Elhai, J.D.; Hall, B.J. The Influence of Depressive Symptoms and Fear of Missing out on Severity of Problematic Smartphone Use and Internet Gaming Disorder among Chinese Young Adults: A Three-Wave Mediation Model. Addictive Behaviors 2021, 112, 106648. [Google Scholar] [CrossRef] [PubMed]
- Teng, Z.; Pontes, H.M.; Nie, Q.; Griffiths, M.D.; Guo, C. Depression and Anxiety Symptoms Associated with Internet Gaming Disorder before and during the COVID-19 Pandemic: A Longitudinal Study. JBA 2021, 10, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Pontes, H.M.; Schivinski, B.; Brzozowska-Woś, M.; Stavropoulos, V. Stavropoulos Laxer Clinical Criteria for Gaming Disorder May Hinder Future Efforts to Devise an Efficient Diagnostic Approach: A Tree-Based Model Study. JCM 2019, 8, 1730. [Google Scholar] [CrossRef]
- Dahl, D.; Bergmark, K.H. Persistence in Problematic Internet Use—A Systematic Review and Meta-Analysis. Front. Sociol. 2020, 5, 30. [Google Scholar] [CrossRef]
- Newzoo Newzoo’s Global Games Market Report 2023; 2024; https://newzoo.com/resources/trend-reports/newzoo-global-games-market-report-2023-free-version.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).