1. Introduction
Cervical cancer is the fourth most common type of cancer in the world after breast, colorectal, and lung cancer. According to the GLOBOCAN (Global Cancer Statistics) report in 2020, there were estimated 604,127 new cases and 341,831 deaths worldwide. In Europe, 58,169 new cases and 25,989 deaths were estimated in 2020 [
1]. All countries are affected, but incidence and mortality are higher in low- and middle-income countries, many of these countries do not have effective population-based screening programmes [
1,
2,
3].
Worldwide, Cervical cancer remains the second most prevalent cause of mortality due to cancer among women aged 20 to 39 [
4].
In 2018, it was estimated that there were approximately 569,847 new cases of cervical cancer [
5]. Studies have shown that cervical cancer can be a largely preventable disease [
6] by screening (particularly with HPV-based methods) and early detection by up to 80% [
7] and with vaccination of the population against the most oncogenic human papilloma virus (HPV) types [
8] cervical cancer can be eradicated [
9].
The prevalence of cancer has shown a decline in developed nations, primarily due to lifestyle modifications such as smoking cessation, enhanced screening methods, and improved treatment options. However, low-income and developing countries have experienced a general rise in both cancer mortality and incidence rates [
10].
The state of this disease in Romania is quite concerning.According to the International Agency for Research on Cancer, in 2020, In Romania, cervical cancer is the third most common type of cancer in women, with a mortality rate of 11,23/100,000. Romania has the highest mortality rate for cervical cancer in the EU. The average mortality rate in the EU from this type of cancer is 3.4 per 100,000 inhabitants, while in Romania, around 11 women per 100,000 die each year from this disease.[
11]. Of all cervical cancer cases diagnosed in the EU, 7.5% come from Romania, a rate three times higher than the EU average.Romania occupied the second position in Europe (EU) after Montenegro [
12].
Cervical cancer is a common condition, with the squamous variant slowly progressing over time in most patients. The long time interval to advance a CIN 1 lesion to a CIN 3 lesion, the increased frequency of cases, as well as the existence of an excision-type treatment that allows healing of the initial stages, are arguments for regular cervical cancer screening.
The introduction of the Pap test in 1940 revolutionised the detection of morphological alterations in the cervical epithelium, resulting in a notable decline in the occurrence and fatality rates of cervical cancer in developed nations. In our times the Pap test remains the fundamental diagnostic tool in the majority of contemporary screening programmes [
13].
Because cervical precancer diagnosis and screening intensity have decreased as a result of the COVID-19 pandemic, a new population of vulnerable women has emerged [
1,
14,
15].
SARS-COV-19 infection this poses a serious threat to people with underlying chronic conditions, including cancer. In the early stages of the COVID-19 pandemic there was a sharp decrease in the detection of various types of cancer [
16,
17] with an increased proportion of cancer diagnoses at advanced stages [
18]. This negative effect was due to shortcomings in health systems, lack of preparedness and resource availability, but also to the increased number of COVID-19 cases that the demand for SARS-CoV-2 testing is competing with the ability to deliver HPV testing, [
18] compounded by a shortage of staff [
19].
The aim of our study is to analyze the number of patients admitted with different types of cervical dysplasia and the treatment applied for the lesions during two years before the pandemic comparative with the period of SARS-CoV-2 pandemic .
2. Materials and Methods
The aim of this study is to compare the number of patients addressed for lesions caused by different types of cervical dysplasia during the SARS-CoV-2 pandemic to the same time for the two years before to the pandemic.
We collected data and compared the number of patients who underwent cervical cone biopsy in the Department of Obstetrics and Gynecology of Timisoara Clinical Municipal Hospital cervical cancer during pandemic and pre-pandemic periods. The inclusion criterion consisted in patients with indication for conization during the selected period. We exluded patients with previous diagnosis of cervical cancer that were hospitalized for radical surgical treatment. We performed a restrospective analysis of the volume of cervical screening tests; number of patients infected with HPV; number of patients treated with an excision method and incidence of invasive and non-invasive cervical lesions.
Depending on which layer was impacted, preneoplastic epithelial proliferative lesions were classified.
The patients included in this study were analyzed and centralized according to their histopathology. The extirpated fragments were sent to the pathological anatomy laboratory for histopathology. Lesion grades were determined by staining the fragments with hematoxylin-eosin.
The following parameters were studied to determine the study results:
- -
age and background;
- -
childbearing potential/menopausal status;
- -
-presence/absence of cervicoragia;
- -
type of cervical atypical/lesions identified by Pap test;
- -
results of HPV molecular diagnostic tests (one or more strains and strains with high oncogenic potential);
- -
number of patients that underwent colposcopies;
- -
number of dual staining tests;
- -
the dimensions of the conization specimen;
- -
patients who underwent concomitant endocervical biopsy by curetage
- -
histopathological diagnosis;
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethical Committee of the Municipal Emergency Clinical Hospital of Timisoara Nr. 81/12.12.2022. This study is a retrospective one, and all patient data has been anonymized.
3. Results
In this descriptive, retrospective study conducted in the Obstetrics-Gynecology Clinic of the Municipal Emergency Clinical Hospital of Timisoara, a number of 404 patients with indication for conization admitted in the 01.04.2018 - 31.03.2022 time interval were included. The study was split between a pre-pandemic two-year period and a pandemic two-year period. The pre-pandemic period was considered to between 01.04.2018-31.03.2020 with 194 patients, while the pandemic period included the time interval between 01.04.2020 and 31.03.2022 with 210 patients.
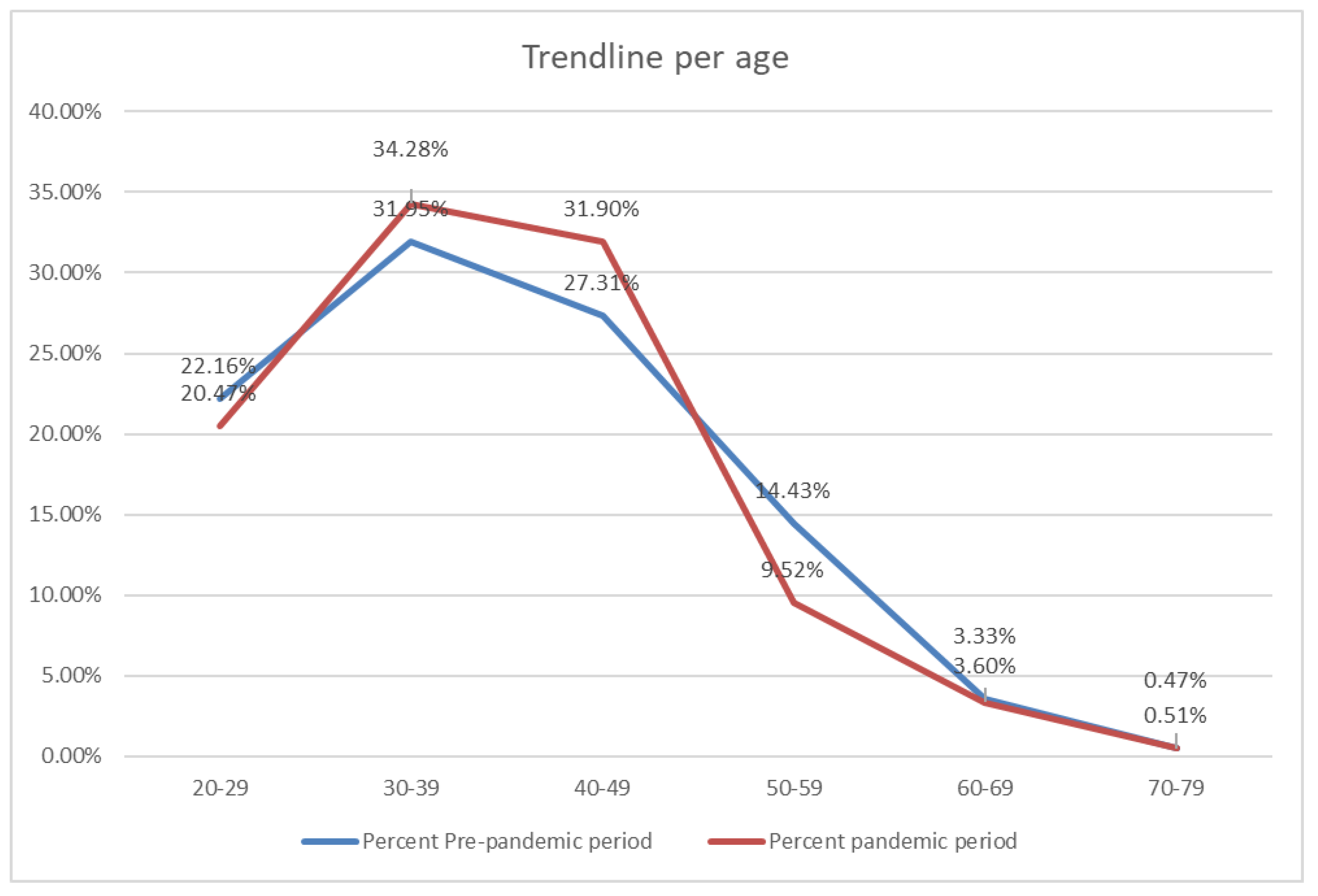
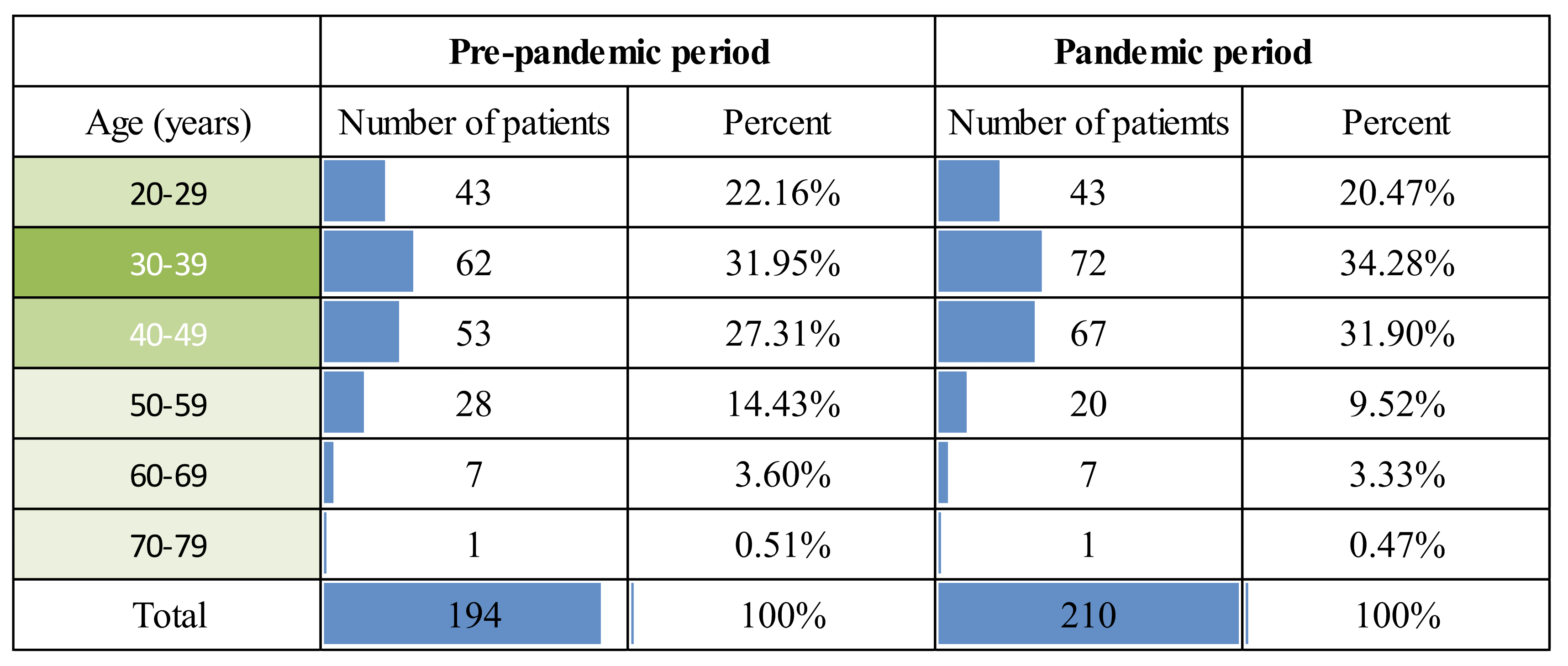
In the pre-pandemic period, according to
Table 1. the highest proportion was observed in the age group of females of reproductive potential, aged 30-39 in 31.95% (62 patients), generally causing a multi-cause infertility problem such as sexually transmitted disease and pelvic inflammatory disease sequelae. Immediately close to that are patients aged 40-49 years, in a proportion of 27.31% (53 patients) in the perimenopausal period. The next age group with a significant percentage that presented in the clinical situation ranged from 20-29 years, with a percentage of 22.16% (43 patients), the age group of acquisition of sexually transmitted infections, including HPV. From the age of 50 years, the age from which cancer pathology generally begins, a gradual decrease in the percentages is observed, in the following order: age group 50-59 years with a percentage of 14.43% (28 patients), age group 60-69 years with a percentage of 3.60% (7 patients) and age group 70-79 years with a low frequency of 0.51% (one patient).
In
Table 1 and
Figure 1, in the pandemic period, patient distribution is observed in age groups similar to the pre-pandemic period, namely: 30-39 years with a percentage of 34.28% (72 patients), 40-49 years with a percentage of 31.90% (67 patients), 20-29 years with a percentage of 20.47% (43 patients), 50-59 years with a percentage of 9.52% (20 patients), 6 0-69 years in 3.33% (7 patients) and 70-79 years with the lowest percentage, 0.47% (one patient).
There was a statistically significant age difference between the two study periods, both by average age of patients and by age group. The mean difference was 32 years before the pandemic and 35 years during the pandemic (p-value >0.05).
The majority of patients presenting for investigations before and during the pandemic was in the 30-39 years age group ( 31,95 % respectively, 34,2% p-value = 0.003). The biggest patient loss ratio identified by age group was in the 50–59 years, 14,53% prepandemic and 9,1% in pandemic period.
From
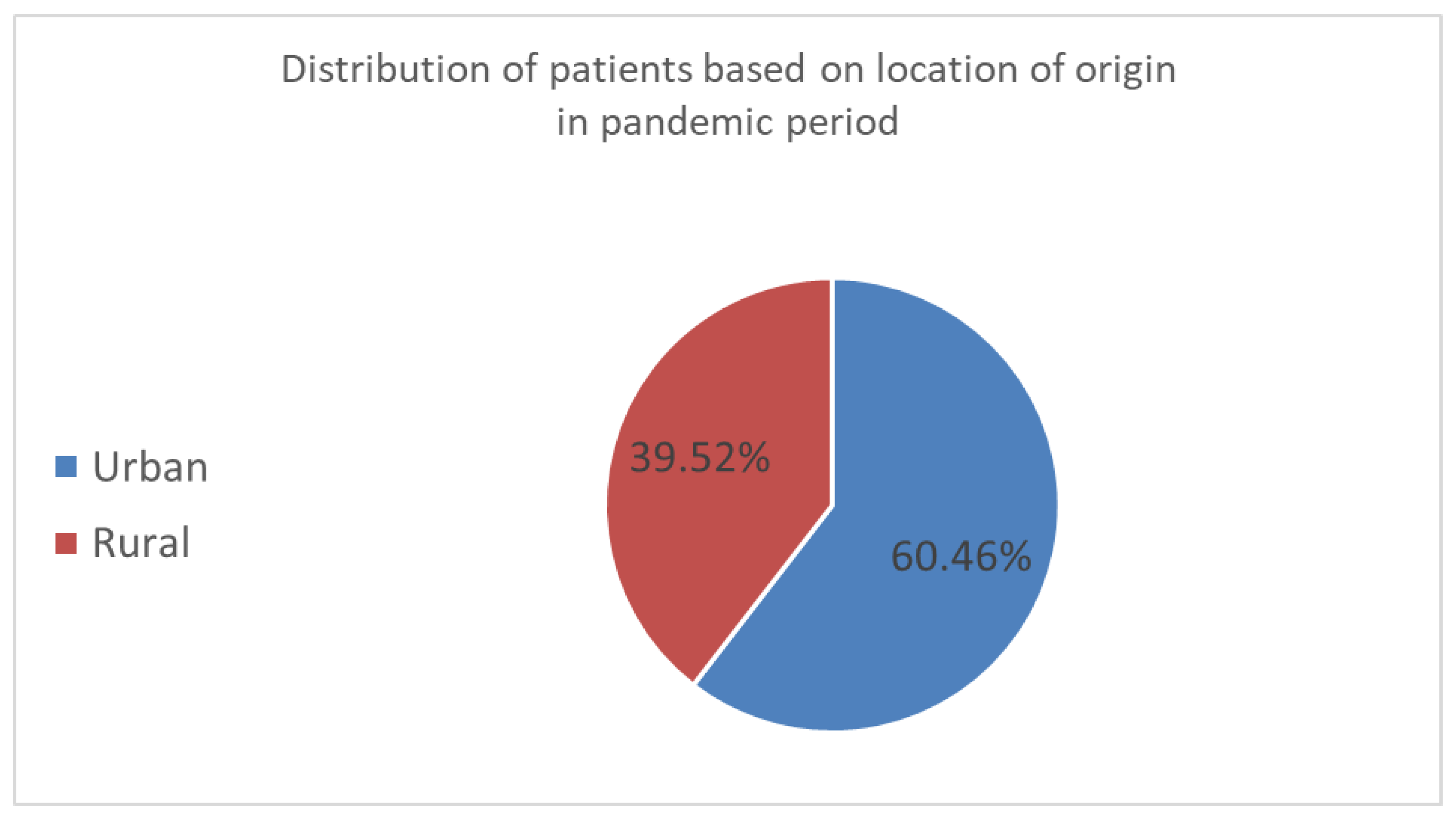
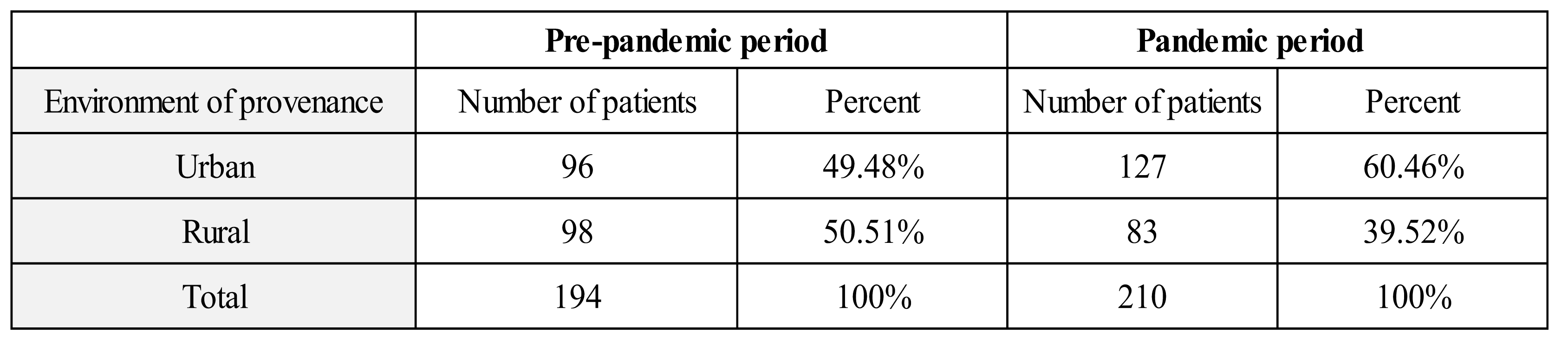
Table 2 - 50.51% (98 patients) of rural patients are observed out of all patients who presented in the clinic during the pre-pandemic period, compared with 49.48% (96 patients) in urban patients.
Compared to the pre-pandemic period, a higher percentage of patients in urban settings of 60.47% (127 patients) in the pandemic period is observed in
Table 2 and
Figure 2. In the pandemic period, patients from rural areas presented in the clinical trial with a lower rate of 39.52% (83 patients).
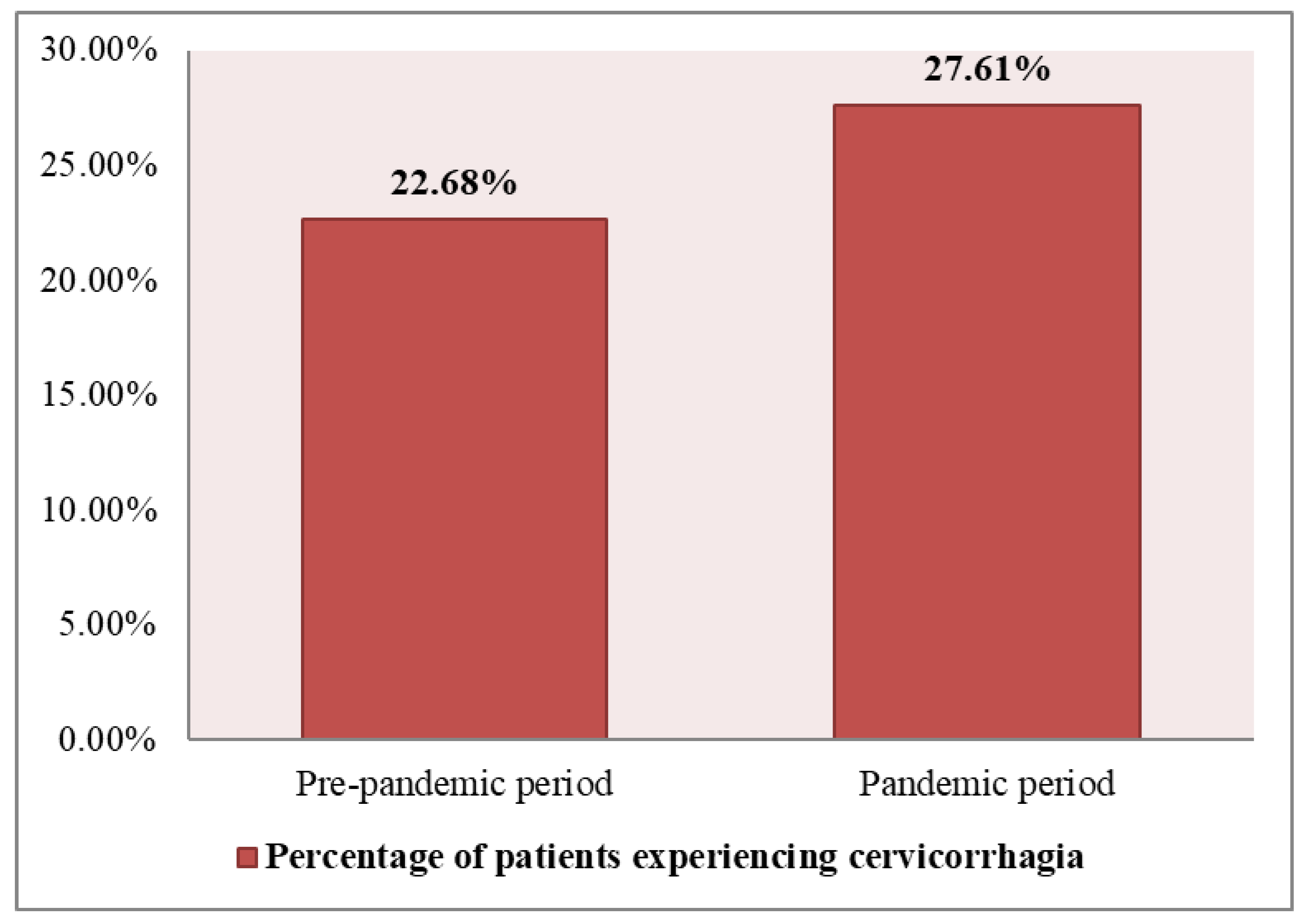
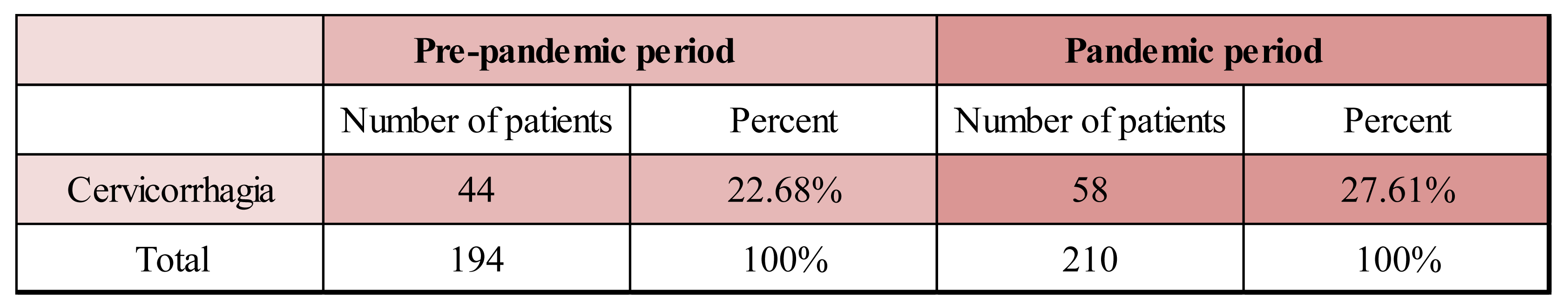
A higher percentage of patients experiencing cervicorrhagia as a clinical manifestation in the pandemic period vs. the prepandemic period is observed based on
Table 3 and
Figure 3. Cervicorrhagia was present pre-pandemic in 22.68% of patients (44 out of 194 patients) and during pandemic in 27.61% of patients (58 out of 210 patients).
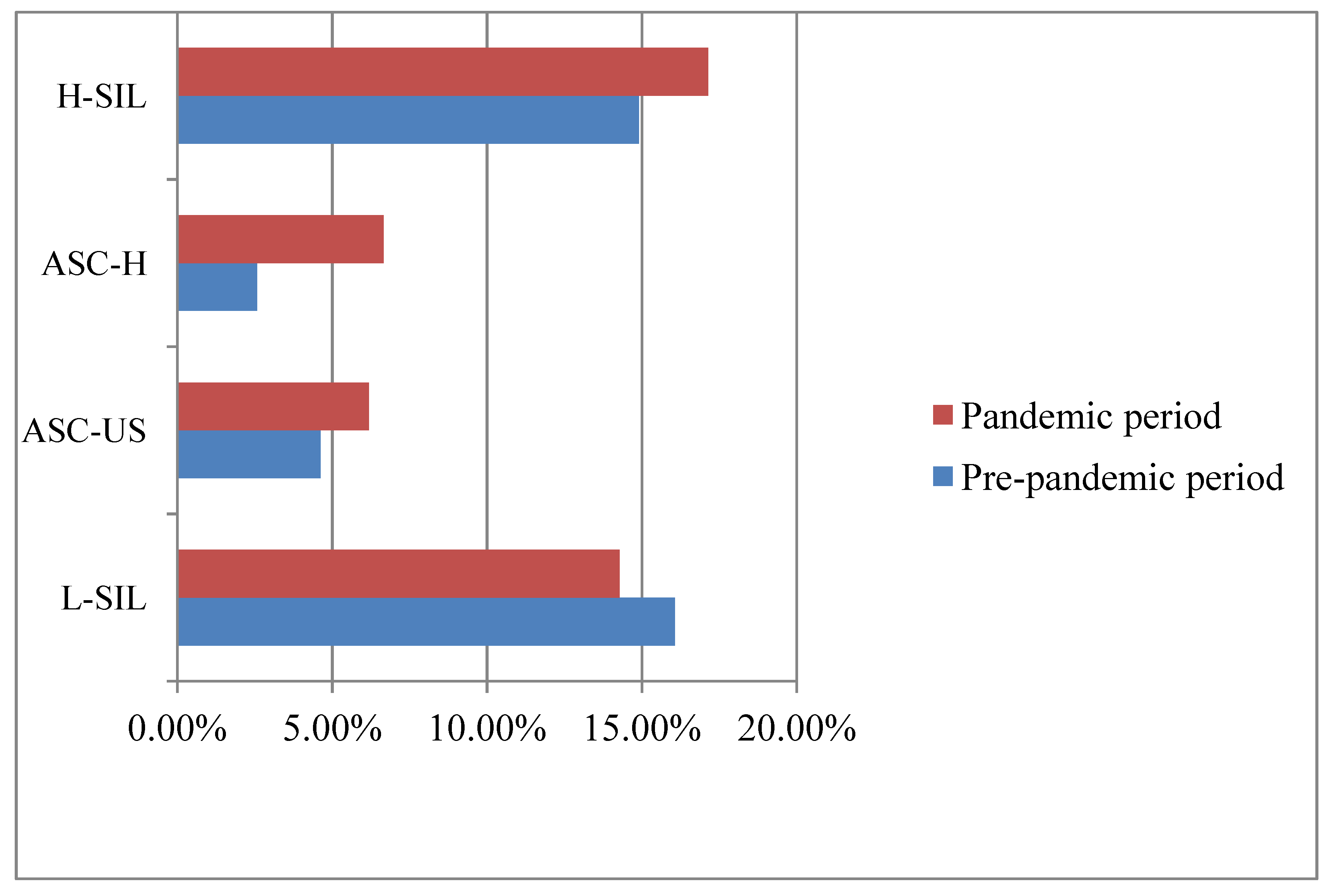
In the pre-pandemic period,
Table 4 and
Figure 4. show the high incidence of low-grade intraepithelial lesions (L-SIL), with 16.06% (31 patients) diagnosed with this dysplastic change in the cervical epithelium immediately followed by high-grade intraepithelial lesion (H-SIL) with 14.90% (29 patients). In a lower number atypical squamous cell pap cytology was found, with more frequent undetermined squamous atypia (ASC-US), which lends itself to differential diagnosis with low-grade intraepithelial lesions (L-SIL), with a percentage of 4.63% ( 9 results). A percentage of 2.57% (5 patients) had squamous types that could not exclude an H-SIL lesion (ASC-H), for which the differential diagnosis with H-SIL is made.
During the pandemic period, the high incidence of H-SIL lesions is seen according to
Table 5 and
Figure 4, with 17.14% (36 patients) having this result. The next lesion right after is L-SIL with 14.28% (30 patients) diagnosed. The percentage of patients with squamous disease is close between the two categories in this class, namely 6.19% (13 patients) had ASC-US lesions and 6.66% (14 patients) had ASC-H results.
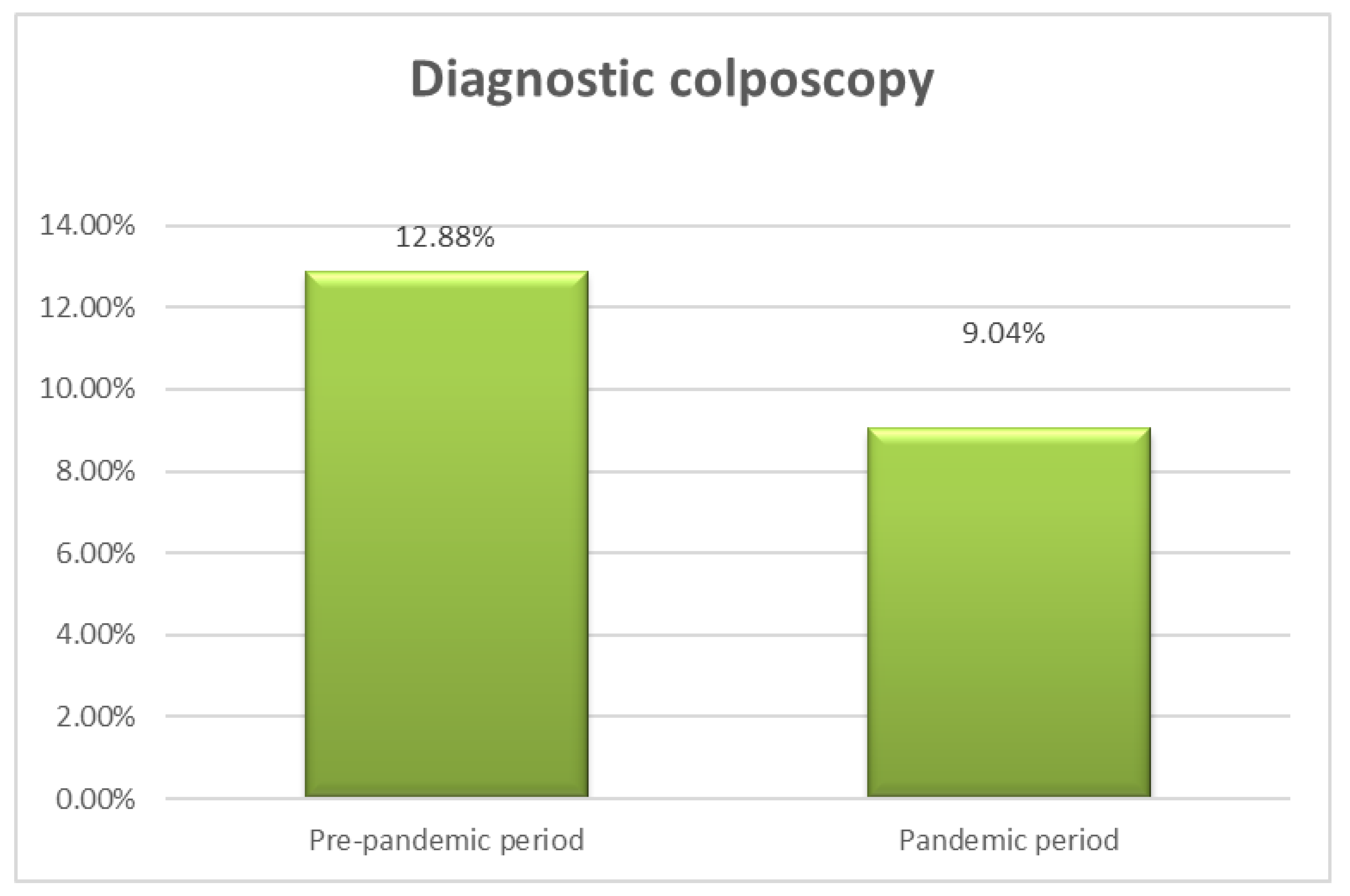
Based on the data observed analyzing the numerical and percent distribution of patients undergoing colposcopic examination, a total of 12.88% of patients underwent diagnostic colposcopy in the period prior to the pandemic, namely 25 out of 194 patients underwent diagnostic colposcopy and, in the pandemic period, 9.04% of patients (19 out of 210 patients).
Figure 5 shows a slightly increased proportion of patients with colposcopy in pre-pandemic (12.88%) versus pandemic (9.04%). Using the colposcopic examination, cervical lesions can be highlighted aceto-white and iodine-negative, with different characteristics depending on the degree of the lesion.
Dual immunocytochemical signal confirms cell cycle dysregulation caused by changes in the cell genome and signals the potential for progression to a high grade cervical lesion. According to
Table 6, a small fraction of 1.54% of patients (3 out of 194 patients) were tested prior to the pandemic for cellular markers of infection (identification of double cytology p16 and Ki67). In a higher percentage 4.28% of patients (9 out of 210 patients) are observed to undergo dual staining (double immunocytochemical staining) for detection of infection cellular markers in pandemic period.
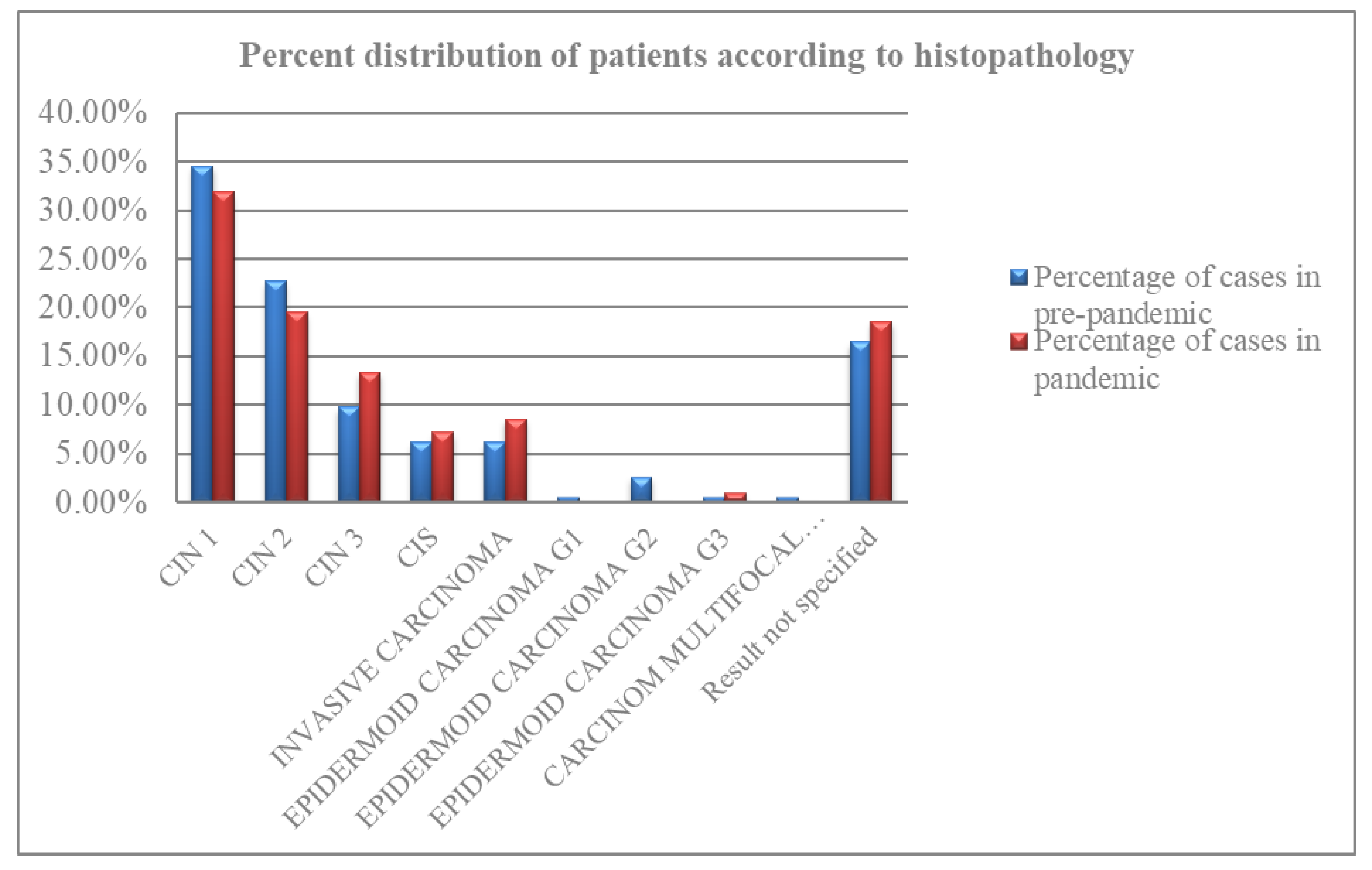
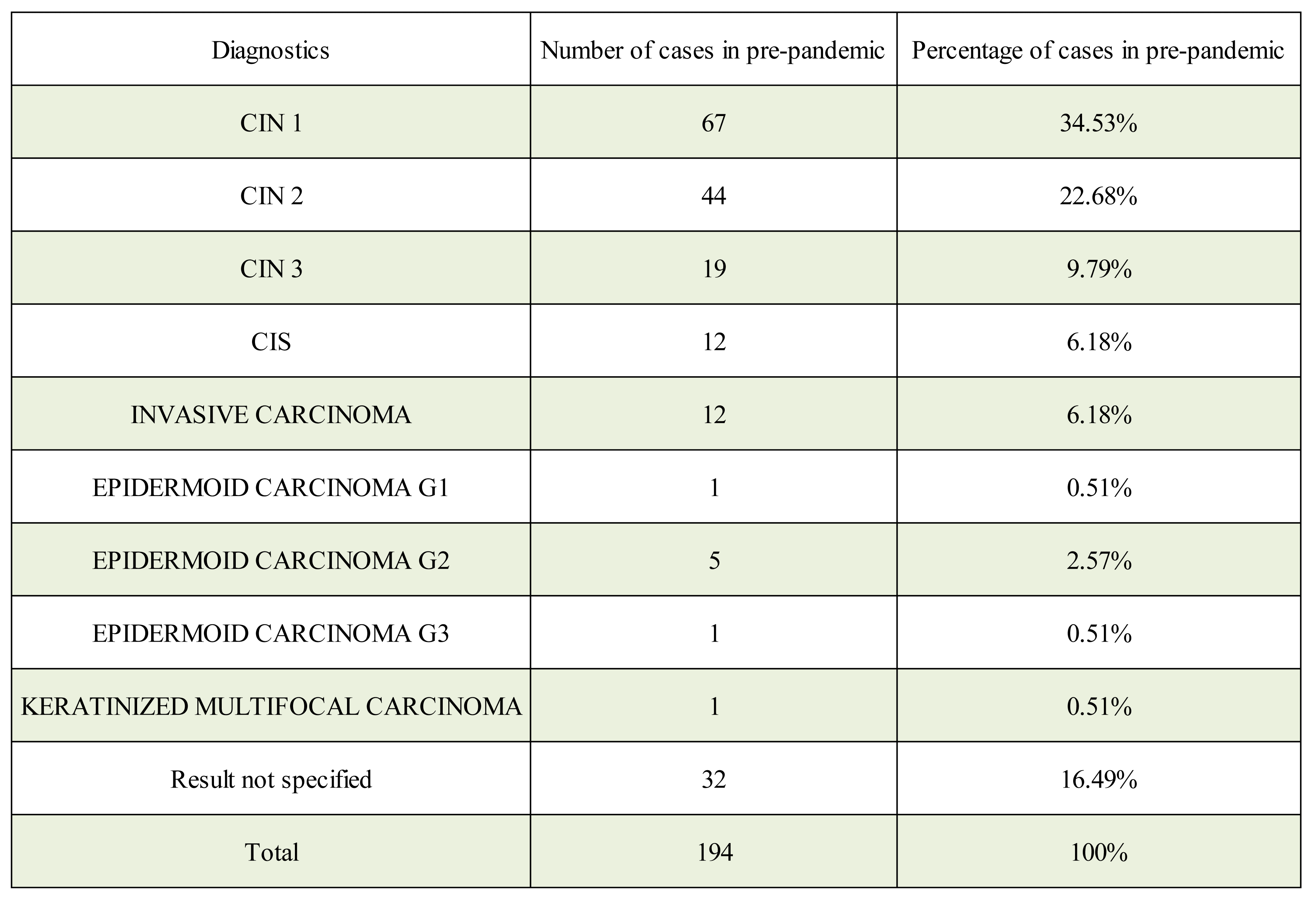
The number of individual tests for cervical cancer was significantly decreased during the pandemic by the percentage of Pap smears, HPV tests, and colposcopies, but we noticed that the CINtests increased. This is due to the attempt to manage noninvasively and without hospitalization the lesions of the cervix in pandemic period , postponing the biopsy or conization of the cervix and this has led to a delay in the diagnosis of certainty. From the data presented in
Table 7 and
Figure 6 on the numerical and percentage distribution of patients by prepandemic histopathology results, the highest incidence is observed for CIN 1 lesion in 34.53% of 67 cases. The next commonly diagnosed lesion, in 22.68% (44 patients), is the CIN 2 lesion. 9.79% is observed for CIN 3, corresponding to severe dysplasia in 19 patients. In situ carcinoma (CIS) and invasive squamous cell carcinoma were diagnosed in equal numbers, 12 patients, and an equal percentage, 6.18%. In a small percentage of 0.51% (one patient), epidermoid carcinoma G1, epidermoid carcinoma G3, keratinized multifocal carcinoma were detected separately in the histopathology. G2 epidermal carcinoma was diagnosed in 2.57% in 5 patients. For 16.49% representing 32 patients, the outcome of the specified histopathologic examination was not found.
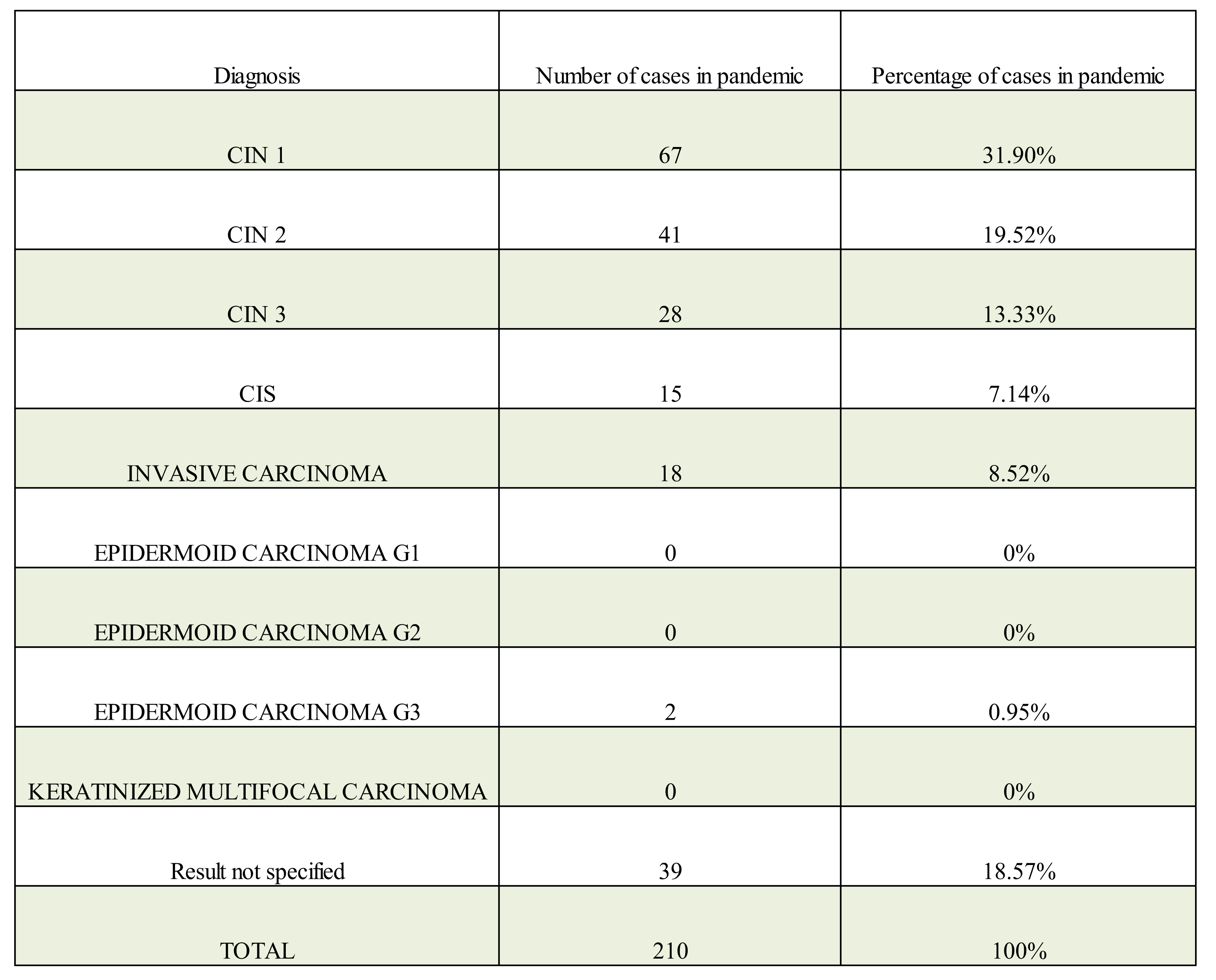
From the data observed in
Figure 6 and
Table 8 analyzing the numerical and percentage distribution of patients by histopathology results in the pandemic period, the most frequently diagnosed CIN 1 lesion is evident in 31.90% (67 patients). This is followed by CIN 2 with 19.52% (41 patients) and CIN 3 with 13.33% (28 patients). The incidence of in situ carcinoma (CIS) and invasive carcinoma is observed in close proportions, 7.14% (15 patients) and 8.52% (18 patients), respectively. G3 epidermal carcinoma was present in 0.95% in 2 patients. A total of 18.57%, 39 patients had unspecified histopathology.
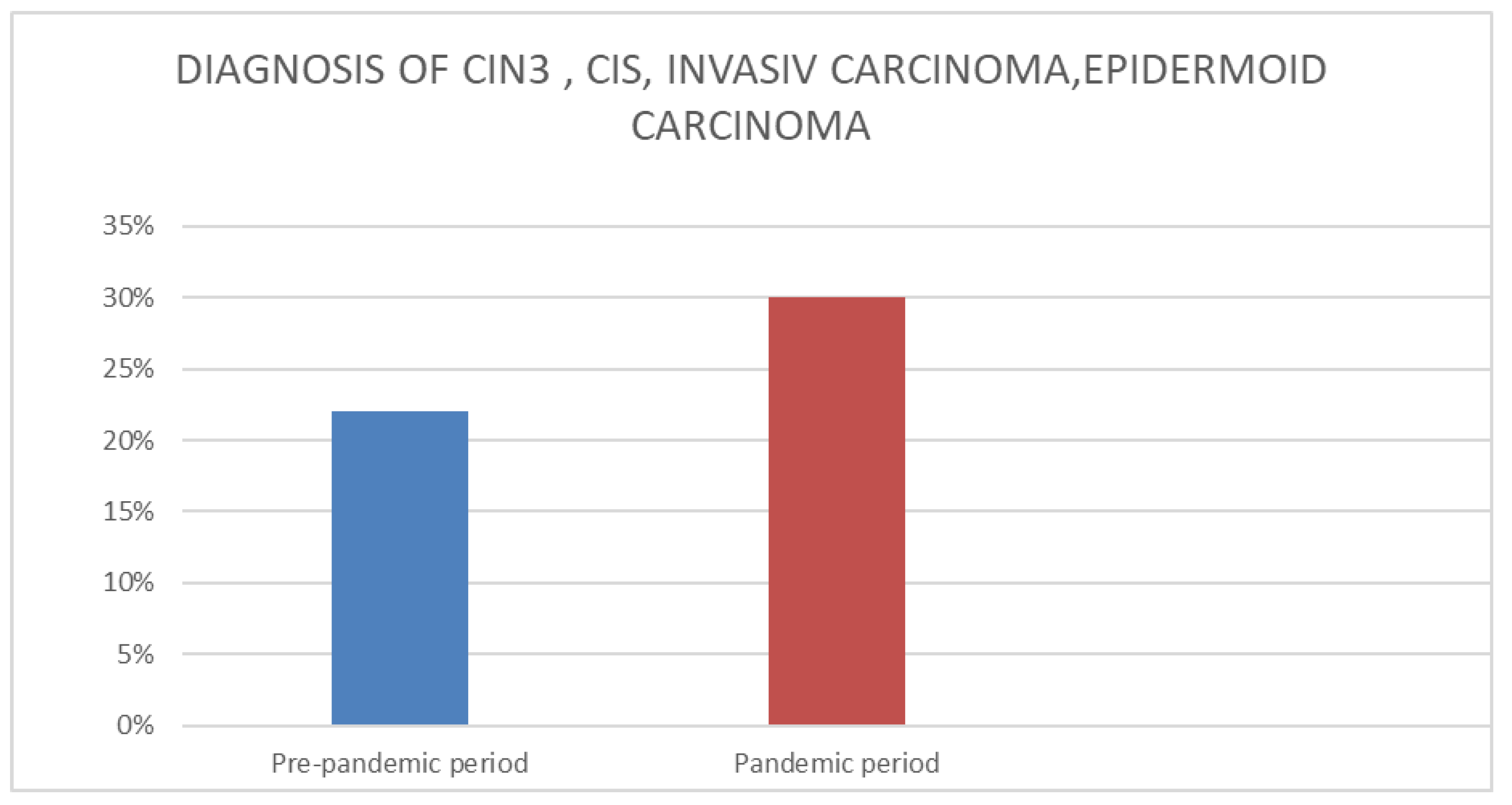
Similar concerning findings were in the stage of cancers newly diagnosed, with a significant difference in CIN 3, CIS, carcinom invaziv si G3 cancers of 8% more during the pandemic (
Figure 7).
4. Discussion
The primary impact of the COVID-19 pandemic appears to be a decrease in the number of screening appoiments and diagnostic procedures resulting in delayed diagnosis and treatment of cancer patients.
Prior studies have reported a significant decrease of 57.21% in the number of cases diagnosed with high-grade dysplasia in the pandemic period, compared to our study where we observed a 8 % increase in the diagnosis of high-grade dysplasia or CIS, invasive carcinoma in the pandemic period. In a similar way the number of colposcopies performed were observed in both studies as decreasing in the pandemic period compared to the pre-pandemic period [
20].
Also, a considerable decrease in the number of cervical cancer screening tests and the number of newly diagnosed patients with cervical cancer has been described in previous studies. Cervical cancer investigations were significantly affected by a mean percent change of 49% in reduction of test volume over the two pandemic years (p-value < 0.001) [
21].
Similar findings were confirmed by a study taking place in Brazilia, Sao Paolo indicated that the percent of cases positive for CIN-1 (p < 0.0410) and CIN-3 (p < 0.0012) increased in 2020 and 2021 as compared to 2019 levels [
22],
A significant decrease in the quantity of pap smears, conizations and mammograms performed since the start of the COVID-19 epidemic was noted in another study carried out by Mateus BO. Duarte. In addition, stage I and II breast cancer adjuvant treatment presented a reduced realization rate, whereas palliative treatment delivered for advanced cervical cancer increased [
23].
To prevent the spread of COVID-19 and shift the medical resources in emergency areas [
20,
24,
25], lead to the cancellation of elective surgeries in all the hospitals [
20,
26]. WHO has implemented new protocols to provide safety for patients and doctors, continuing to restrict surgical interventions to emergencies only [
20,
27,
28].
The last data from the nationwide Netherlands Cancer Registry showed that there was a notable decrease in overall cancer diagnosis when compared to the pre-pandemic period year of 2020 [
18,
29]. Similar data have been reported for Denmark, Germany, Austria, Poland, the United States and the United Kingdom [
18,
30,
31,
32,
33,
34,
35].
The most concerning potential adverse effect of the disruption of cancer screening programs could delay diagnosis of tumors, causing a shift to diagnosis at more advanced stages and fewer treatment options, resulting in a worse prognosis [
36,
37,
38] and an increase in future cancer morbidity and mortality [
36].
Because of a break in cervical screening service in the beginning of the pandemic four studies show that they expect an increased diagnosis rate of advanced and invasive lesions of cervical cancer and deaths in the upcoming years due the lack of hospitalizations of patients and implicitly by decreasing curative surgical maneuvers [
39,
40,
41,
42].
The incidence of cervical cancer is expected to increase if compensatory screening programs are not implemented as soon as posible to recover the diagnosis of all cases of cervical dysplasia omitted during the pandemic period by non-testingin time. On the assumption that healthcare services will not be able to increase the detection rate for cervical lesions to a level even higher that to previous years, it will become difficult to lower the cervical cancer incidence
. Therefore, there will be a delay in the diagnosis of cervical cancer for women to undergo an examination (25-64 years) according to standard international protocols [
20,
43].
A study by Smith et al. [
44] suggests the number of diagnoses of cervical cancer will increase by 1.1-3.6% due to discontinuity of cervical cancer screening in 2020. In another study, Gupta et al. [
45] noted an increase of 2.52% to 3.80% in cervical cancer-related deaths with treatment delays ranging from 9 weeks to 6 months while Kregting et al. [
46] projected a twofold increase in deaths from cervical cancer per 100 000 people in 10 years.
Davies et al. [
47] estimated that in the next 3 years there will be a considerable increase in newly diagnosed cases of cervical cancer.
The WHO had demonstrated the need to increase spendings on prevention and screening test , in particular in low financially country and this becomes even more urgent during postpandemic times, when additional financial resources are required to cover the missing tests [
36,
48].
Another solution for effectiveness could be to prioritize those who are most likely to develop cancer, such as women with a personal or family history of breast, ovarian, women with HIV immunodeficiencies or women who have not been in screening for several years [
36,
49,
50].
The systematic review of Ferrara et al. [
51] conducted on seven studies observed reductions in HPV vaccine uptake and coverage during COVID-19. Reports of cervical cancer screening and cancer diagnostic activities have shown a major impact of the pandemic on access to screening services and diagnostic procedures. All but one of the studies investigating the treatment of cervical cancer reported changes in the number of women with cervical lesions receiving treatments, and delays and discontinuations of treatment [
51].
Also, in the context of the COVID-19 pandemic, HPV vaccination and routine immunization services have presented significant disruptions with decreases in immunization coverage [
51,
52,
53].
In our study the proportion of patients with diagnostic colposcopies was higher in the pre-pandemic period, at 12.88%, but Tests for the identification of double cytological marker p16 and Ki67 increased during the pandemic period, reaching 4.28%.
Also in our study we noticed The largest percentage of the dimension of the cuts is occupied by the range 11-15 mm with a percentage of 51.02%, which is found in the pre-pandemic period, followed by a percentage of 44.28% for the pieces of the cone between 5-10 mm in the pandemic period.
Cervical cancer screening plays an important role worldwide in early diagnosis and high rates of cervical cancer cure. However, the COVID-19 pandemic required several drastic measures to halt the spread of the new coronavirus SARS-CoV-2, limiting access to non-invasive and invasive investigations essential for cervical cancer diagnosis.
Several limitations of the current study include its single-center design and the availability of data from patient records. Data collected from a single site may not be typical of the overall Romanian population, as patient background factors might vary significantly across the nation.
Careful monitoring of the downstream impacts of COVID-19-related service disruptions on cervical pre-cancer and cancer outcomes will be critical to assisting service providers in planning and mitigating negative implications. Based on these findings, we predict similar future outcomes in our area, and future priority measures for catch-up should be developed to balance potential resource constraints with clinical demands.
5. Conclusions
Cervical cancer is a malignant neoplasia with high preventive potential, with national screening programs playing an important role. The COVID-19 pandemic has imposed a number of restrictions in order to be able to mitigate the spread of SARS-CoV-2 with disruption of screening programs and medical checks. However, the addressability of the patients was not affected in a drastic way in our study.
In our study, we found an increase in cervicoragy as reason for consultation in the pandemic period. Also we encountered a decrease of appoiments in the age group 50-59 years and a decrese in patients with rural residence. A higher lesion degree, both on Pap smear and on cervical biopsy were found in the pandemic period in our study.
Therefore, the COVID pandemic has shown a negative impact in certain population subgroups, more vulnerable to cervical cancer, but no decrease in the number of cervical cone biopsies in our study. Though the data interpretation is limited by the regional variations in the population, our findings are important in highlighting the most susceptible patients that should be targeted by screening in a pandemic setting.
Given the sad probability of future pandemics caused by viral or other outbreaks, primary health care must provide appropriate coverage of people even during times of crisis by taking the essential procedures [
36].
Public health measures should concentrate on improving infrastructure and resilience, as well as including goals and objectives to assist sustain cancer prevention and treatment services during and after calamities [
54].
Author Contributions
Conceptualization, L.B., L.P., A.I., C.B and C.S; methodology, L.B and S.C.; software, A.C.; validation, A.C.; formal analysis, C.B.; investigation, C.S. and D.C.; resources, L.B , A.I. and M.P.; data curation, C.S.; writing—original draft preparation, L.B.; writing—review and editing, C.S and L .P .; visualization, C.B and M.P.; supervision, L.P.; project administration, L.P. All authors have read and agreed to the published version of the manuscript.
Funding
We would like to acknowledge VICTOR BABES UNIVERSITY OF MEDICINE AND PHARMACY TIMISOARA for their support in covering the costs of publication for this research paper.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethical Committee of the Municipal Emergency Clinical Hospital of Timisoara No. 81/12.12.2022. This study is a retrospective one, and all patient data has been anonymized.
Data Availability Statement
The data presented in this study are available on request from the principal author. Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Singh, D.; Vignat, J.; Lorenzoni, V.; Eslahi, M.; Ginsburg, O.; Lauby-Secretan, B.; Arbyn, M.; Basu, P.; Bray, F.; Vaccarella, S. Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO Global Cervical Cancer Elimination Initiative. Lancet Glob Health. 2023, 11, e197–e206. [Google Scholar] [CrossRef]
- Poljak, M.; Rogovskaya, S.I.; Kesić, V.; Bray, F.; Berkhof, J.; Seme, K.; Brotons, M.; Castellsagué, X.; Syrjänen, S.; Arbyn, M.; Bosch, F.X. Recommendations for cervical cancer prevention in central and eastern Europe and central Asia. Vaccine. 2013, 31 (suppl 7), H80–H82. [Google Scholar] [CrossRef] [PubMed]
- Arbyn, M.; Antoine, J.; Mägi, M.; Smailyte, G.; Stengrevics, A.; Suteu, O.; Valerianova, Z.; Bray, F.; Weiderpass, E. Trends in cervical cancer incidence and mortality in the Baltic countries, Bulgaria and Romania. Int J Cancer. 2011, 128, 1899–1907. [Google Scholar] [CrossRef]
- Buskwofie, A.; David-West, G.; Clare, C.A. A Review of Cervical Cancer: Incidence and Disparities. 2020, 112, 229–232. [Google Scholar] [CrossRef]
- Rees, M.; Angioli, R.; Coleman, R.L.; Glasspool, R.; Plotti, F.; Simoncini, T.; Terranova, C. European Menopause and Andropause Society (EMAS) and International Gynecologic Cancer Society (IGCS) Position Statement on Managing the Menopause after Gynecological Cancer: Focus on Menopausal Symptoms and Osteoporosis. Maturitas 2020, 134, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Bouvard, V.; Wentzensen, N.; Mackie, A.; Berkhof, J.; Brotherton, J.; Giorgi-Rossi, P.; Kupets, R.; Smith, R.; Arrossi, S.; Bendahhou, K.; Canfell, K.; Chirenje, Z.M.; Chung, M.H.; Del Pino, M.; de Sanjosé, S. Elfström, M.; Franco, E.L.; Hamashima, C.; Hamers, F.F.; Herrington, C.S.; Murillo, R.; Sangrajrang, S.; Sankaranarayanan, R.; Saraiya, M.; Schiffman, M.; Zhao, F.; Arbyn, M.; Prendiville, W.; Indave Ruiz, B.I.; Mosquera-Metcalfe, I.; Lauby-Secretan, B. The IARC perspective on cervical cancer screening. N Engl J Med. 2021, 385, 1908–1918. [Google Scholar] [CrossRef]
- Kalliala, I.; Athanasiou, A.; Veroniki, A.A.; Salanti, G.; Efthimiou, O.; Raftis, N.; Bowden, S.; Paraskevaidi, M.; Aro, K.; Arbyn, M.; Bennett, P.; Nieminen, P.; Paraskevaidis, E.; Kyrgiou, M. Incidence and Mortality from Cervical Cancer and Other Malignancies after Treatment of Cervical Intraepithelial Neoplasia: A Systematic Review and Meta-Analysis of the Literature. Ann. Oncol. 2020, 31, 213–227. [Google Scholar] [CrossRef]
- Arbyn, M.; Xu, L. Efficacy and safety of prophylactic HPV vaccines. A Cochrane review of randomized trials. Expert Rev Vaccines 2018, 17, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Simms, K.T.; Steinberg, J.; Caruana, M.; Smith, M.A.; Lew, J.B.; Soerjomataram, I.; Castle, P.E.; Bray, F.; Canfell, K. Impact of scaled up human papillomavirus vaccination and cervical screening and the potential for global elimination of cervical cancer in 181 countries, 2020-99: a modelling study. Lancet Oncol. 2019; 20, 394–407. [Google Scholar] [CrossRef]
- Akinyemiju, T.F. F. Socio-economic and health access determinants of breast and cervical cancer screening in lowincome countries: analysis of the World health Survey. PLoS ONE 2012, 7. [Google Scholar] [CrossRef]
- Arbyn, M.; Raifu, A.O.; Weiderpass, E.; Bray, F.; Anttila, A. Trends of Cervical Cancer Mortality in the Member States of the European Union. Eur. J. Cancer 2009, 45, 2640–2648. [Google Scholar] [CrossRef]
- Cancer Today. Available online: http://gco.iarc.fr/today/home (accessed on 20 March 2024).
- Chrysostomou, A.C.; Stylianou, D.C.; Constantinidou, A.; Kostrikis, L.G. A Review Cervical Cancer Screening Programs in Europe: The Transition. Viruses 2018, 10, 729. [Google Scholar] [CrossRef] [PubMed]
- Bonadio, R.C.; Messias, A.P.; Moreira, O.A.; Leis, L.V.; Orsi, B.Z.; Testa, L.; Estevez-Diz, M.D.P. Impact of the COVID-19 pandemic on breast and cervical cancer stage at diagnosis in Brazil. Ecancermedicalscience. 2021, 15. [Google Scholar] [CrossRef] [PubMed]
- Ivanuš, U. ; Jerman, T; Gašper Oblak, U.; Meglič, L.; Florjančič, M.; Strojan Fležar, M.; Premru Sršen, T.; Smrkolj, Š.; Pakiž, M.; Primic Žakelj, M.; Kloboves Prevodnik, V.; Pogačnik, A.; Josipović, I.; Mate, T.; Gobec, M. The impact of the COVID-19 pandemic on organised cervical cancer screening: the first results of the Slovenian cervical screening programme and registry. Lancet Reg Health Eur 2021, 5. [Google Scholar]
- Center for Systems Science and Engineering at Johns Hopkins University. COVID-19 Dashboard [Internet]. 2021. Available from: https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6. 24 March.
- World Health Organization. Rapid assessment of service delivery for noncommunicable diseases (NCDs) during the COVID-19 pandemic. Geneva; 2020.
- Poljak, M.; Cuschieri, K.; Waheed, D.E.; Baay, M.; Vorsters, A. Impact of the COVID-19 pandemic on human papillomavirus-based testing services to support cervical cancer screening. Acta Dermatovenerol Alp Pannonica Adriat 2021, 30, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Vahabi, M.; Shahil-Feroz, A.; Lofters, A.; Wong, J.P.; Prakash, V.; Pimple, S.; Anand, K.; Mishra, G. Surviving the Storm: The Impact of COVID-19 on Cervical Cancer Screening in Low- and Middle-Income Countries. Healthcare 2023, 11, 3079. [Google Scholar] [CrossRef] [PubMed]
- Istrate-Ofițeru, A.M.; Berbecaru, E.I.; Ruican, D.; Nagy, R.D.; Rămescu, C.; Roșu, G.C.; Iovan, L.; Dîră, L.M.; Zorilă, G.L.; Țieranu, M.L.; Iliescu, D.G. The Influence of SARS-CoV-2 Pandemic in the Diagnosis and Treatment of Cervical Dysplasia. Medicina 2021, 57, 1101. [Google Scholar] [CrossRef] [PubMed]
- Popescu, A.; Craina, M. ; Pantea, S; Pirvu, C.; Chiriac, V.D.; Marincu, I.; Bratosin, F.; Bogdan, I.; Hosin, S.; Citu, C.; Bernad, E.; Neamtu, R.; Dumitru, C.; Mocanu, A.G.; Avram, C.; Gluhovschi, A. COVID-19 Pandemic Effects on Cervical Cancer Diagnosis and Management: A Population-Based Study in Romania. Diagnostics, 2022; 12, 907. [Google Scholar] [CrossRef]
- Martins, T.R.; Witkin, S.S.; Mendes-Corrêa, M.C.; Godoy, A.S.; Cury, L.; Balancin, M.L.; Ab'Saber, A.M.; Peres, S.V.; Messias, S.; Tozetto Mendoza, T.R.; Longatto-Filho, A. Impact of the COVID-19 Pandemic on Cervical Cancer Screening in São Paulo State. Brazil Acta Cytol 2023, 67, 388–394. [Google Scholar] [CrossRef] [PubMed]
- Duarte, M.B.O.; Argenton, J.L.P.; Carvalheira, J.B.C. Impact of COVID-19 in Cervical and Breast Cancer Screening and Systemic Treatment in São Paulo, Brazil: An Interrupted Time Series Analysis, O JCO Glob Oncol, 2022; 8, e2100371. [Google Scholar] [CrossRef]
- AHA Letter to Surgeon General Re: Elective Surgeries and COVID-19. Available online: https://www.aha.org/lettercomment/2020-03-15-aha-letter-surgeon-general-re-elective-surgeries-and-covid-19 (accessed on 03 March 2024).
- COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures. Available online: http://www.facs.org/covid-19/clinical-guidance/triage (accessed on 03 March 2024).
- HealthLeaders Surgeon General Urges Providers to “Consider Stopping Elective Surgeries.” Hospitals Push Back. Available online: https://www.healthleadersmedia.com/clinical-care/surgeon-general-urges-providers-consider-stopping-elective-surgeries-hospitals-push (accessed on 14 March 2024).
- Chen, R.; Zhang, Y.; Huang, L.; Cheng, B.-H.; Xia, Z.-Y.; Meng, Q.-T. Safety and Efficacy of Different Anesthetic Regimens for Parturients with COVID-19 Undergoing Cesarean Delivery: A Case Series of 17 Patients. Can. J. Anaesth. 2020, 67, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Lie, S.A.; Wong, S.W.; Wong, L.T.; Wong, T.G.L.; Chong, S.Y. Practical Considerations for Performing Regional Anesthesia: Lessons Learned from the COVID-19 Pandemic. Can. J. Anaesth. 2020, 67, 885–892. [Google Scholar] [CrossRef]
- Dinmohamed, A.G.; Visser, O.; Verhoeven, R.H.A.; Louwman, M.W.J.; van Nederveen, F.H.; Willems, S.M.; Merkx, M.A.W.; Lemmens, V.E.P.P.; Nagtegaal, I.D.; Siesling, S. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol. 2020, 21, 750–1. [Google Scholar] [CrossRef]
- Skovlund, C.W.; Friis, S.; Dehlendorff, C.; Nilbert, M.C.; Mørch, L.S. Hidden morbidities: drop in cancer diagnoses during the COVID-19 pandemic in Denmark. Acta Oncol. 2021, 60, 20–3. [Google Scholar] [CrossRef] [PubMed]
- Jacob, L.; Loosen, S.H.; Kalder, M.; Luedde, T.; Roderburg, C.; Kostev, K. Impact of the COVID-19 pandemic on cancer diagnoses in general and specialized practices in Germany. Cancers 2021, 13, 408. [Google Scholar] [CrossRef] [PubMed]
- Tsibulak, I.; Reiser, E.; Bogner, G.; Petru, E.; Hell-Teutsch, J.; Reinthaller, A.; Weirather, C.; Weiss, T.; Bozsa, S.; Puschacher, B.; Hall, M.; Hittler, D.; Hrauda, K.; Thell, E.; Clauss, S.; Pozniak, J.; Alicke, S.; Gangl, D.; Gamperl, G.; Ebner, C.; Knoll, K.; Leitner, K.; Schilcher, A.; Schinnerl, M.; Sigl, V.; Singer, C.; Aigmüller, T.; Hofstätter, B.; Marth, C. Decrease in gynecological cancer diagnoses during the COVID-19 pandemic: an Austrian perspective. Int J Gynecol Cancer. 2020, 30, 1667–71. [Google Scholar] [CrossRef] [PubMed]
- Maluchnik, M.; Podwójcic, K.; Więckowska, B. Decreasing access to cancer diagnosis and treatment during the COVID-19 pandemic in Poland. Acta Oncol. 2021, 60, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.J.; Xu, L.; Qin, J.; Hahn, E.E.; Ngo-Metzger, Q.; Mittman, B.; Tewari, D.; Hodeib, M.; Wride, P.; Saraiya, M.; Chao, C.R. Impact of COVID-19 on cervical cancer screening rates among women aged 21–65 years in a large integrated health care system—southern California, January 1 – September 30, 2019, and January 1 – September 30, 2020. MMWR Morb Mortal Wkly Rep. 2021, 70, 109–13. [Google Scholar] [CrossRef] [PubMed]
- Castanon, A.; Rebolj, M.; Pesola, F.; Sasieni, P. Recovery strategies following COVID-19 disruption to cervical cancer screening and their impact on excess diagnoses. Brit J Cancer, Epub ahead of print. 2021. [Google Scholar]
- Elemes, S.; Stachteas, P.; Haidich, A.B.; Mamopoulos, A.; Smyrnakis, E. The Impact of the COVID-19 Pandemic on Breast and Cervical Cancer Screening: A Systematic Review. In Vivo 2023, 37, 1455–1476. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Haynes, K.; Du, S.; Barron, J.; Katz, A. Association of cancer screening deficit in the United States with the COVID-19 pandemic. JAMA Oncology 2021, 7, 878. [Google Scholar] [CrossRef] [PubMed]
- Patt, D.; Gordan, L.; Diaz, M.; Okon, T.; Grady, L.; Harmison, M.; Markward, N.; Sullivan, M.; Peng, J.; Zhou, A. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clinical Cancer Informatics 2022, 1059–1071. [Google Scholar] [CrossRef]
- Yong, J.H.; Mainprize, J.G.; Yaffe, M.J.; Ruan, Y.; Poirier, A.E.; Coldman, A.; Nadeau, C.; Iragorri, N.; Hilsden, R.J.; Brenner, D.R. The impact of episodic screening interruption: COVID-19 and population-based cancer screening in Canada. J Med Screen. 2021, 28, 100–107. [Google Scholar] [CrossRef]
- Dinmohamed, A.G.; Cellamare, M.; Visser, O.; de Munck, L.; Elferink, M.A.G.; Westenend, P.J.; Wesseling, J.; Broeders, M.J.M.; Kuipers, E.J.; Merkx, M.A.W.; Nagtegaal, I.D.; Siesling, S. The Impact of the Temporary Suspension of National Cancer Screening Programmes Due to the COVID-19 Epidemic on the Diagnosis of Breast and Colorectal Cancer in the Netherlands. J. Hematol. Oncol. 2020, 13, 147. [Google Scholar] [CrossRef]
- Maringe, C.; Spicer, J.; Morris, M.; Purushotham, A.; Nolte, E.; Sullivan, R.; Rachet, B.; Aggarwal, A. The Impact of the COVID-19 Pandemic on Cancer Deaths Due to Delays in Diagnosis in England, UK: A National, Population-Based, Modelling Study. Lancet Oncol. 2020, 21, 1023–1034. [Google Scholar] [CrossRef] [PubMed]
- de Jonge, L.; Worthington, J.; van Wifferen, F.; Iragorri, N.; Peterse, E.F.P.; Lew, J.-B.; Greuter, M.J.E.; Smith, H.A.; Feletto, E.; Yong, J.H.E.; Canfell, K.; Coupé, V.M.H.; Lansdorp-Vogelaar, I. Impact of the COVID-19 Pandemic on Faecal Immunochemical Test-Based Colorectal Cancer Screening Programmes in Australia, Canada, and the Netherlands: A Comparative Modelling Study. Lancet Gastroenterol. Hepatol. 2021, 6, 304–314. [Google Scholar] [CrossRef]
- De Pelsemaeker, M.-C.; Guiot, Y.; Vanderveken, J.; Galant, C.; Van Bockstal, M.R. The Impact of the COVID-19 Pandemic and the Associated Belgian Governmental Measures on Cancer Screening, Surgical Pathology and Cytopathology. Pathobiology. 2021, 88, 46–55. [Google Scholar] [CrossRef]
- Modelled Analysis of Hypothetical Impacts of COVID-19 Related Disruptions on the National Cervical Screening Program. Report to the Department of Health (May 2020). New South Wales: Cancer Research Division, Cancer Council NSW. 2020. Available online: https://www.health.gov.au/resources/publications/modelled-analysis-of-hypothetical-impacts-of-covid-19-related-disruptions-to-the-national-cervical-screening-program (accessed on 21 March 2024).
- Gupta, N.; Chauhan, A.S.; Prinja, S.; Pandey, A.K. Impact of COVID-19 on Outcomes for Patients with Cervical Cancer in India. JCO Glob. Oncol. 2021, 7, 716–725. [Google Scholar] [CrossRef]
- Kregting, L.M.; Kaljouw, S.; de Jonge, L.; Jansen, E.E.L.; Peterse, E.F.P.; Heijnsdijk, E.A.M.; van Ravesteyn, N.T.; Lansdorp-Vogelaar, I.; de Kok, I.M.C.M. Effects of cancer screening restart strategies after COVID-19 disruption. Br J Cancer 2021, 124, 1516–1523. [Google Scholar] [CrossRef] [PubMed]
- Davies, J.M.; Spencer, A.; Macdonald, S.; Dobson, L.; Haydock, E.; Burton, H.; Angelopoulos, G.; Martin-Hirsch, P.; Wood, N.J.; Thangavelu, A.; Hutson, R.; Munot, S.; Flynn, M.; Smith, M.; DeCruze, B.; Myriokefalitaki, E.; Sap, K.; Winter-Roach, B.; Macdonald, R.; Edmondson, R.J. Cervical cancer and COVID-an assessment of the initial effect of the pandemic and subsequent projection of impact for women in England: A cohort study. BJOG 2022, 11, 17098. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation Primary health care on the road to universal health coverage: 2019 monitoring report, 2019. Available online: https://www.who.int/publications/i/item/9789240029040 (accessed on 25 May 2023).
- Ajenifuja, K.; Belinson, J.; Goldstein, A.; Desai, K.; de Sanjose, S.; Schiffman, M. Designing low-cost, accurate cervical screening strategies that take into account COVID-19: a role for self-sampled HPV typing. Infectious Agents and Cancer 2021, 15, 61. [Google Scholar] [CrossRef]
- Croswell, J.; Corley, D.; Lafata, J.; Haas, J.; Inadomi, J.; Kamineni, A.; Ritzwoller, D.; Vachani, A.; Zheng, Y. Cancer screening in the U.S. through the COVID-19 pandemic, recovery, and beyond. Preventive Medicine 2021, 151, 106595. [Google Scholar] [CrossRef]
- Ferrara, P.; Dallagiacoma, G.; Alberti, F.; Gentile, L.; Bertuccio, P.; Odone, A. Prevention, diagnosis and treatment of cervical cancer: A systematic review of the impact of COVID-19 on patient care. Preventive Medicine 2022, 164, 107264. [Google Scholar] [CrossRef]
- Ramírez, M.; Fuente, J.; Andía, D.; José Hernández, J.; Fiol, G.; Torné, A. HPV vaccination coverage in women between 15 and 55 years old in Spain: temporal trend during the period 2007–2020. Int. J. Gynecol. Obstet. 2022. [CrossRef]
- Sabbatucci, M.; Odone, A.; Signorelli, C. ; Siddu A, Silenzi, A.; Maraglino, F.P.; Rezza, G. Childhood immunisation coverage during the COVID-19 epidemic in Italy. Vaccines. 2022, 10, 120. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, A.P.; Calo, W.A.; Mendez-Lazaro, P.; García-Camacho, S.; Mercado-Casillas, A.; Cabrera-Marquez, J.; Tortolero-Luna, G. Strengthening resilience and adaptive capacity to disasters in cancer control plans: lessons learned from Puerto Rico. Cancer Epidemiol Biomarkers Prev. 2020, 29, 1290–1293. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).