Submitted:
09 April 2024
Posted:
09 April 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Historical Review of Rehabilitation (Table 1)
| Year | Author | Rehabilitation method |
|---|---|---|
| 1937 | Williams [16] | Lumbar flexion exercises |
| 1955 | Kelly [17] | Hanging exercises |
| 1962 | Pheasant [18] | Posture building |
| 1968 | Calliet [19] | Lumbar lateral flexion exercises |
| 1971 | Böhler [20] | Lumbar extension exercises |
| 1979 | McKenzie [21] | Lumbar extension exercises |
3. Various Kinds of Rehabilitation
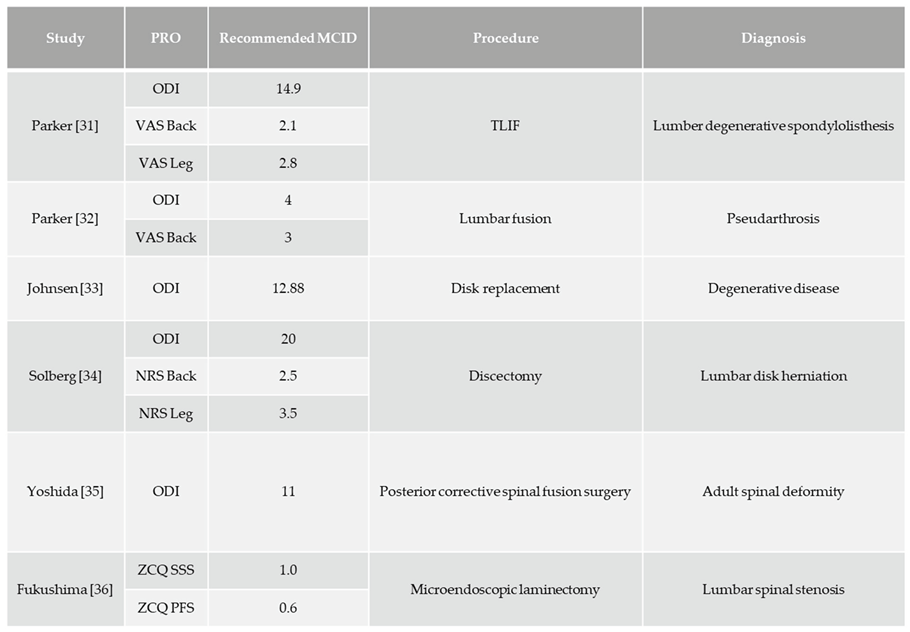
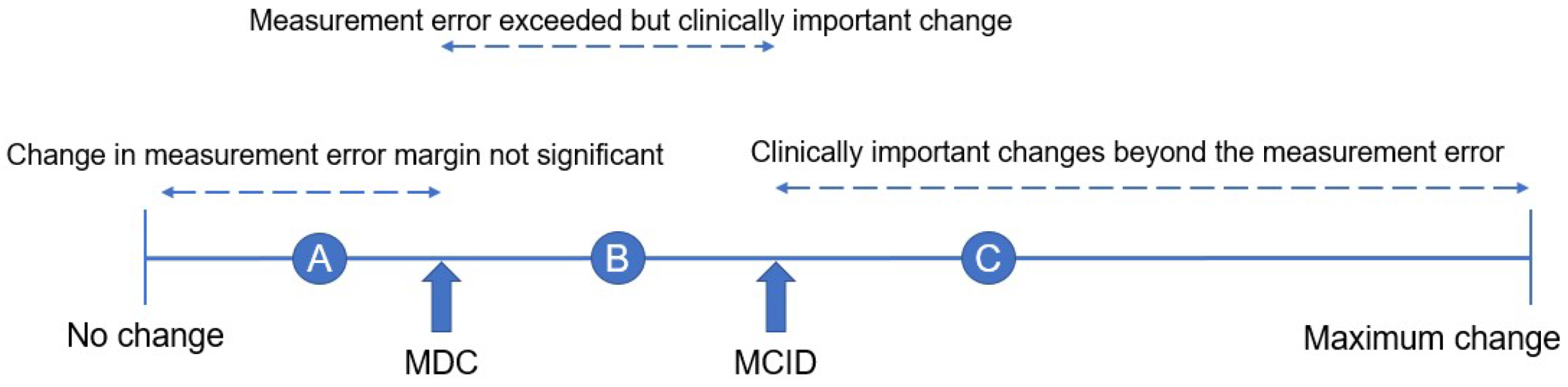
4. Patients Reported Outcome (PRO) Measures Used after Lumbar Surgery
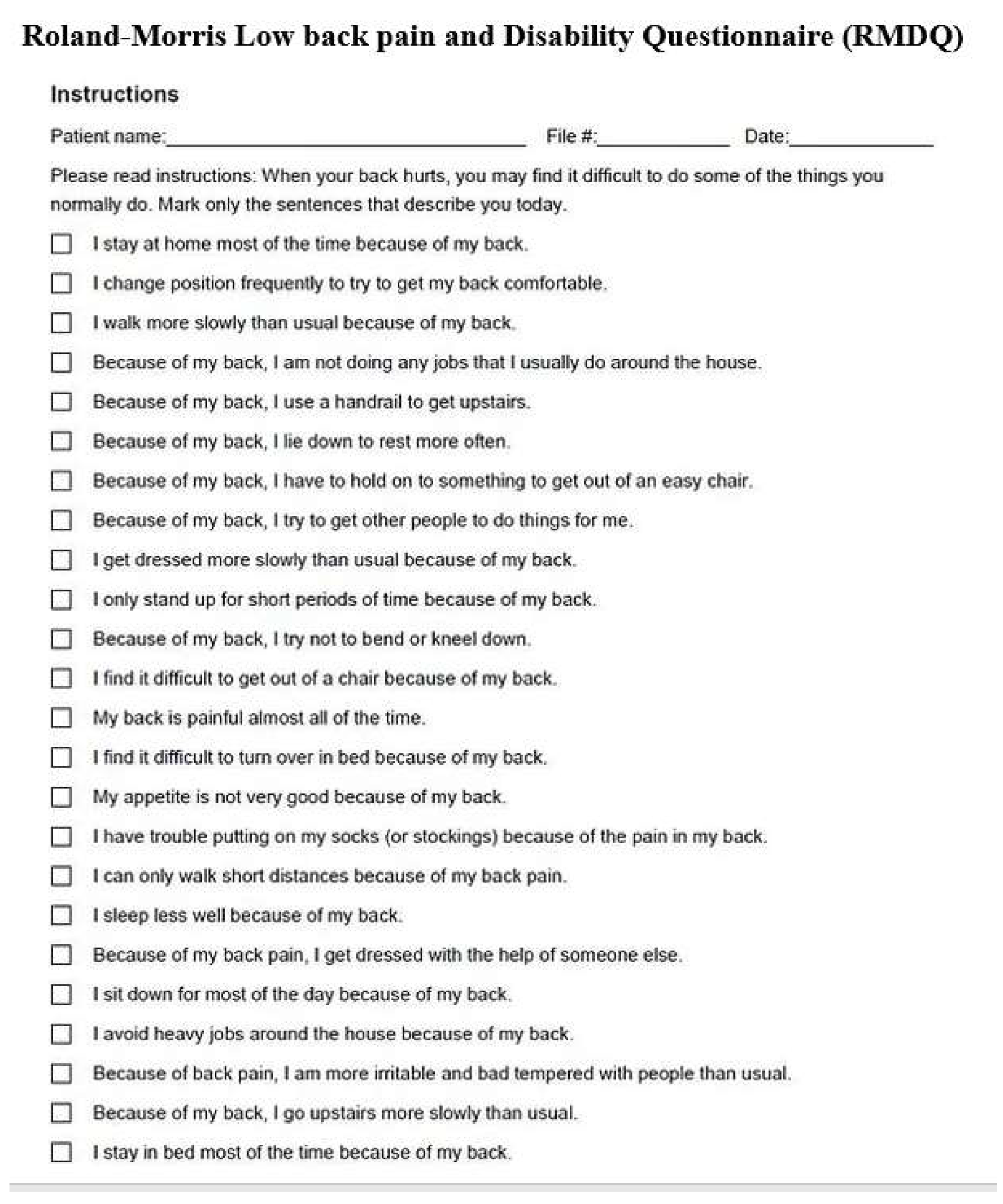
2.1. Roland-Morris Disability Questionnaire (RMDQ) (Figure 4)
2.2. Oswestry Disability Index (ODI) (Figure 5)
2.2. Zurich Claudication Questionnaire (ZCQ)
2.3. Scoliosis Research Society 22-Item Questionnaire (SRS-22)
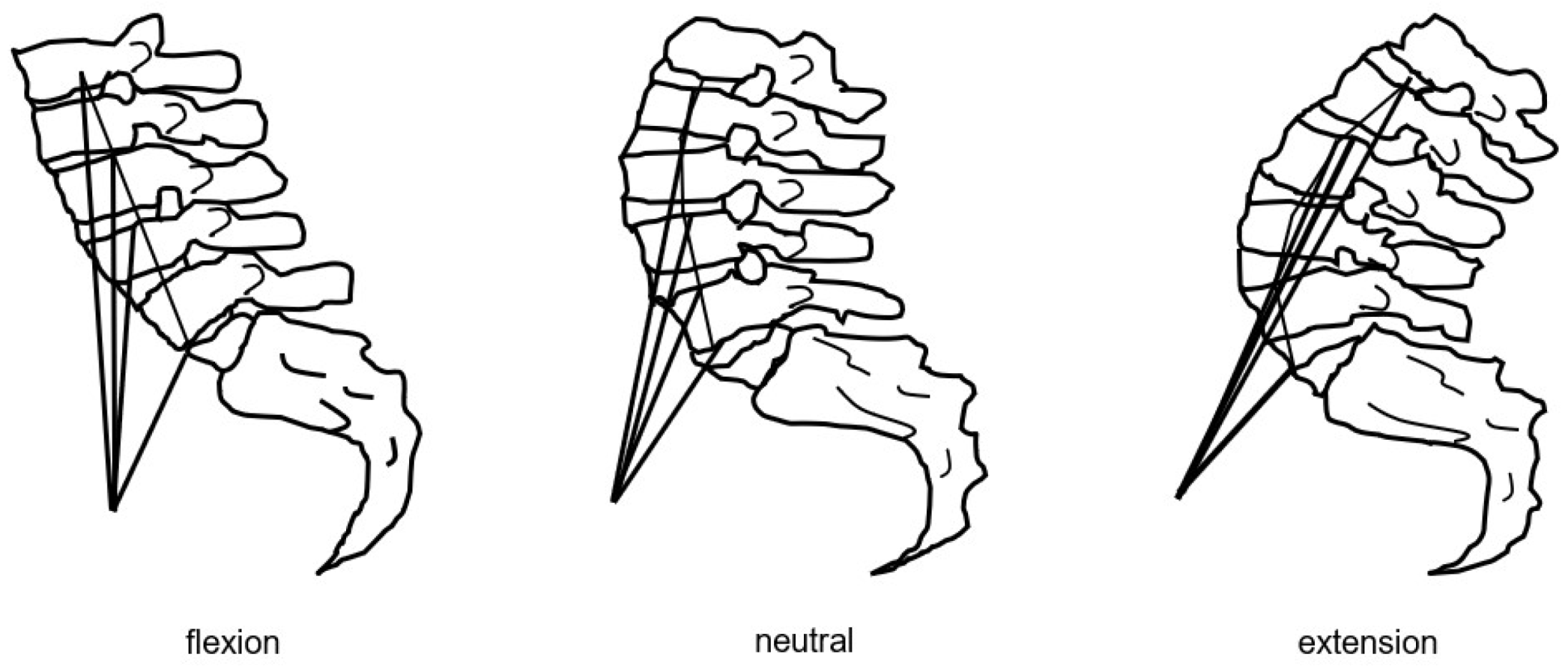
2.4. Lumbar Stiffness Disability Index (LSDI)
5. Physical Performance Tests
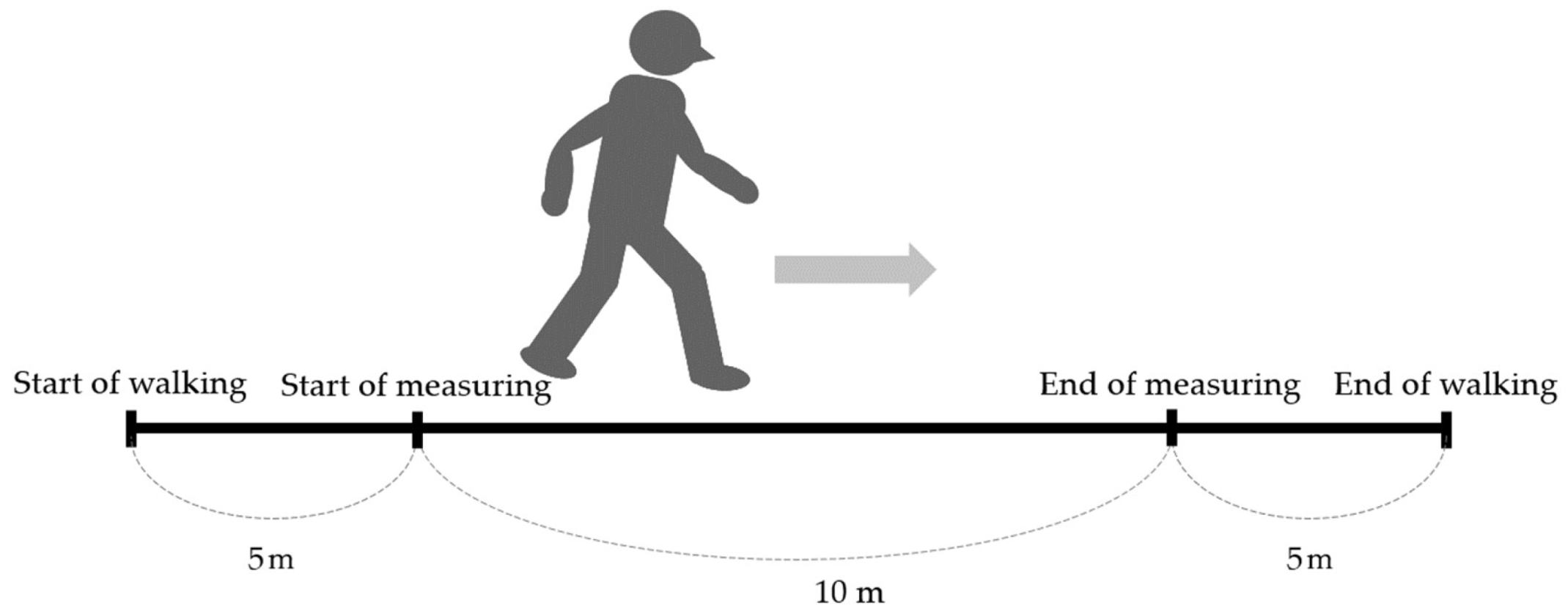
5.1. Walk Velocity (Figure 6)
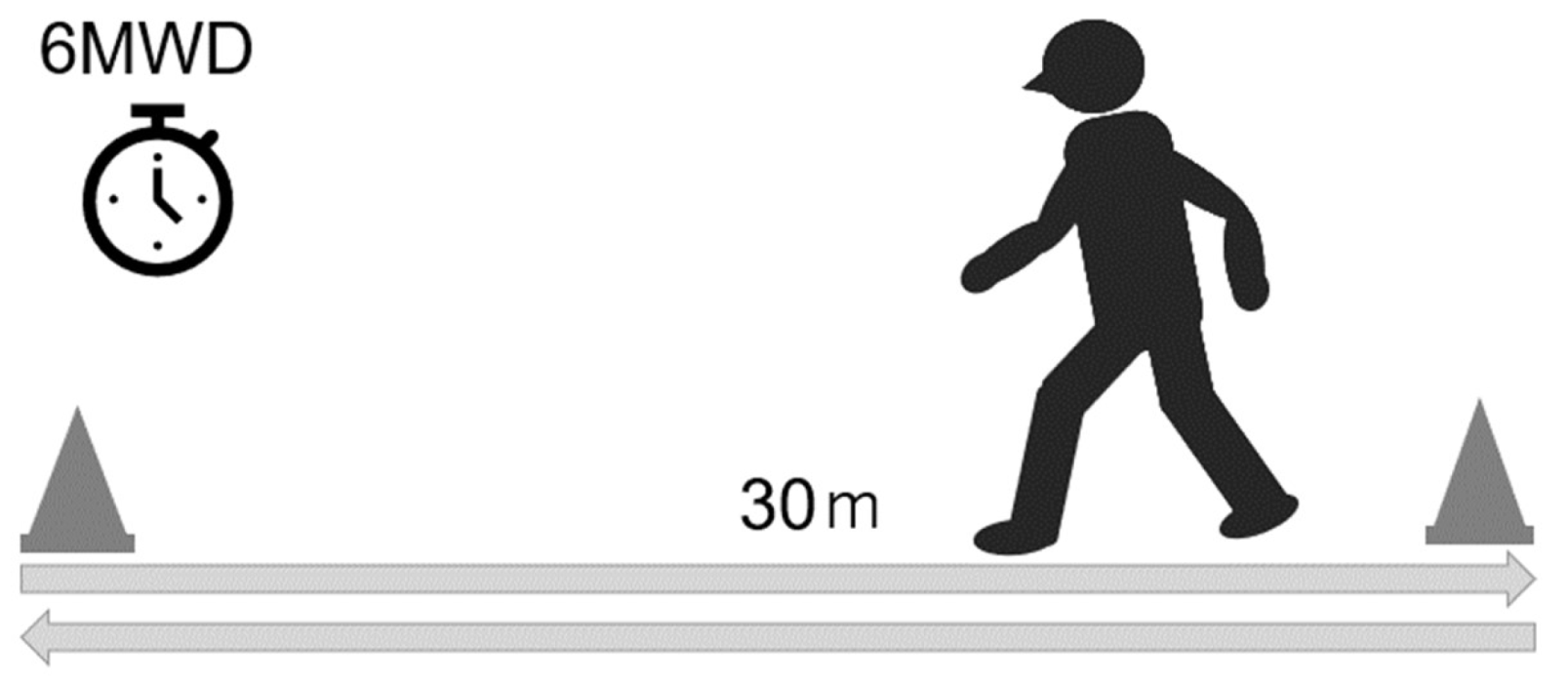
5.2 6-Minute Walk Test (Figure 6)
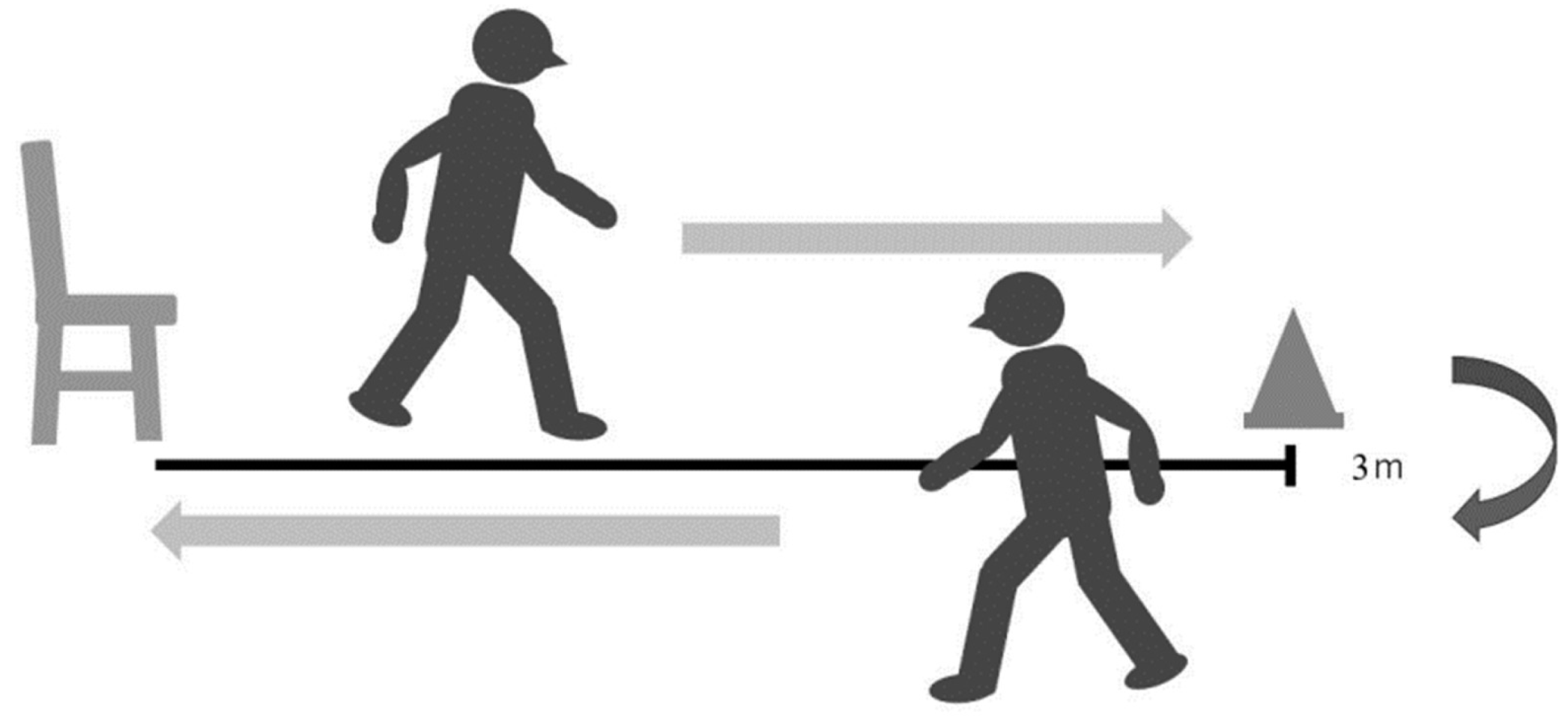
5.3. Timed Up and Go Test (TUG) (Figure 7)
5.5. Functional Reach Test (FRT) (Figure 8)
5.6. The Balance Evaluation Systems Test (BESTest) (Table 4)
5.73. D Motion Analyzers and Force Plate
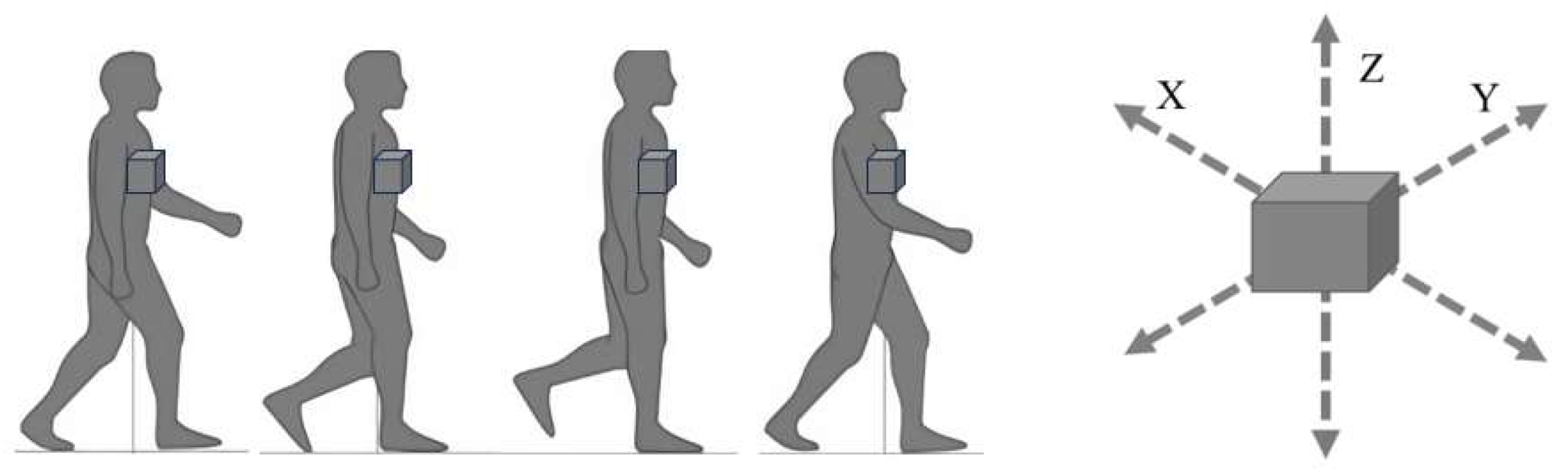
5.8. Triaxial Accelerometer (Figure 9)
6. Physical Therapy after Lumbar Spine Surgery
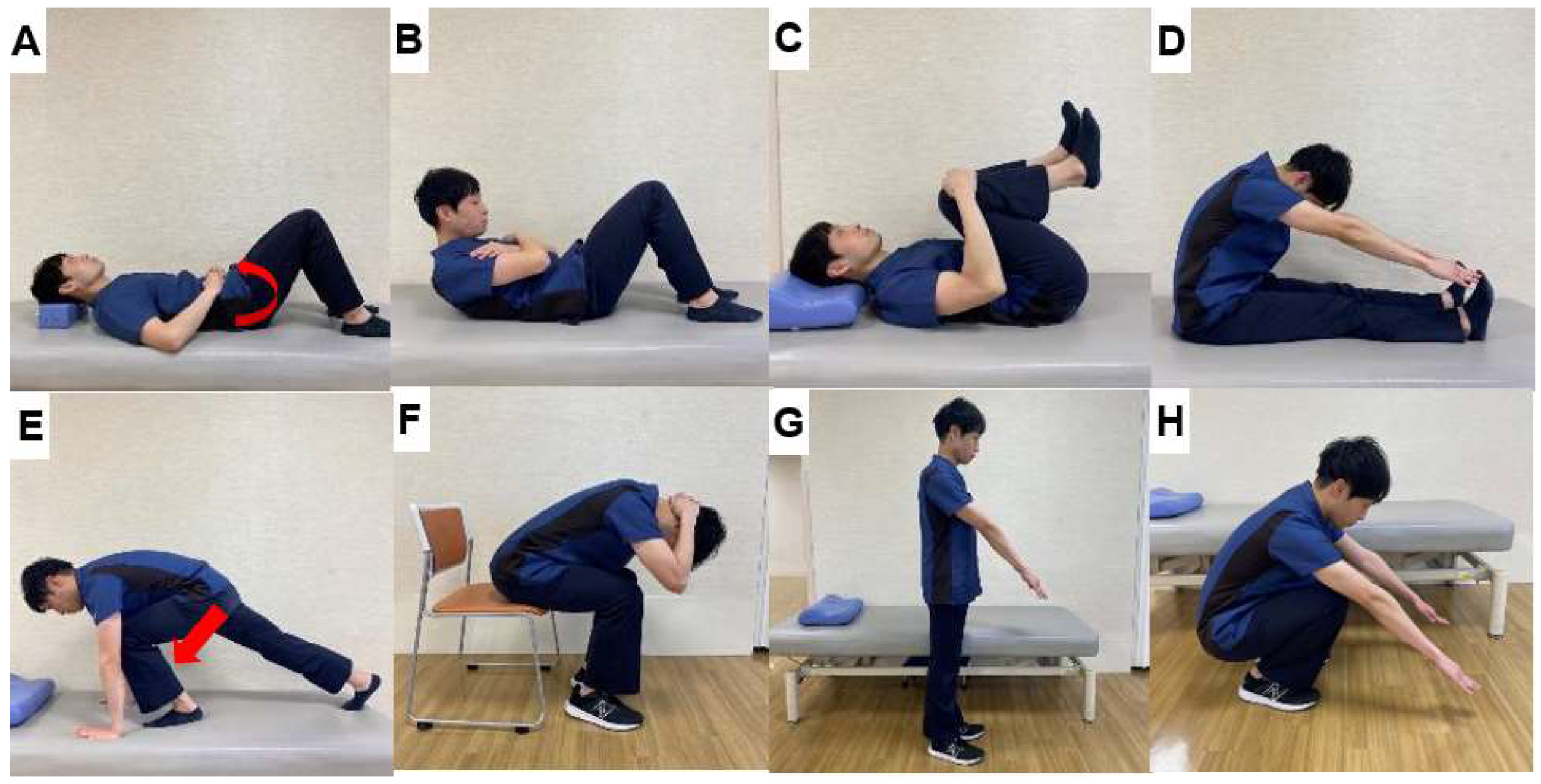
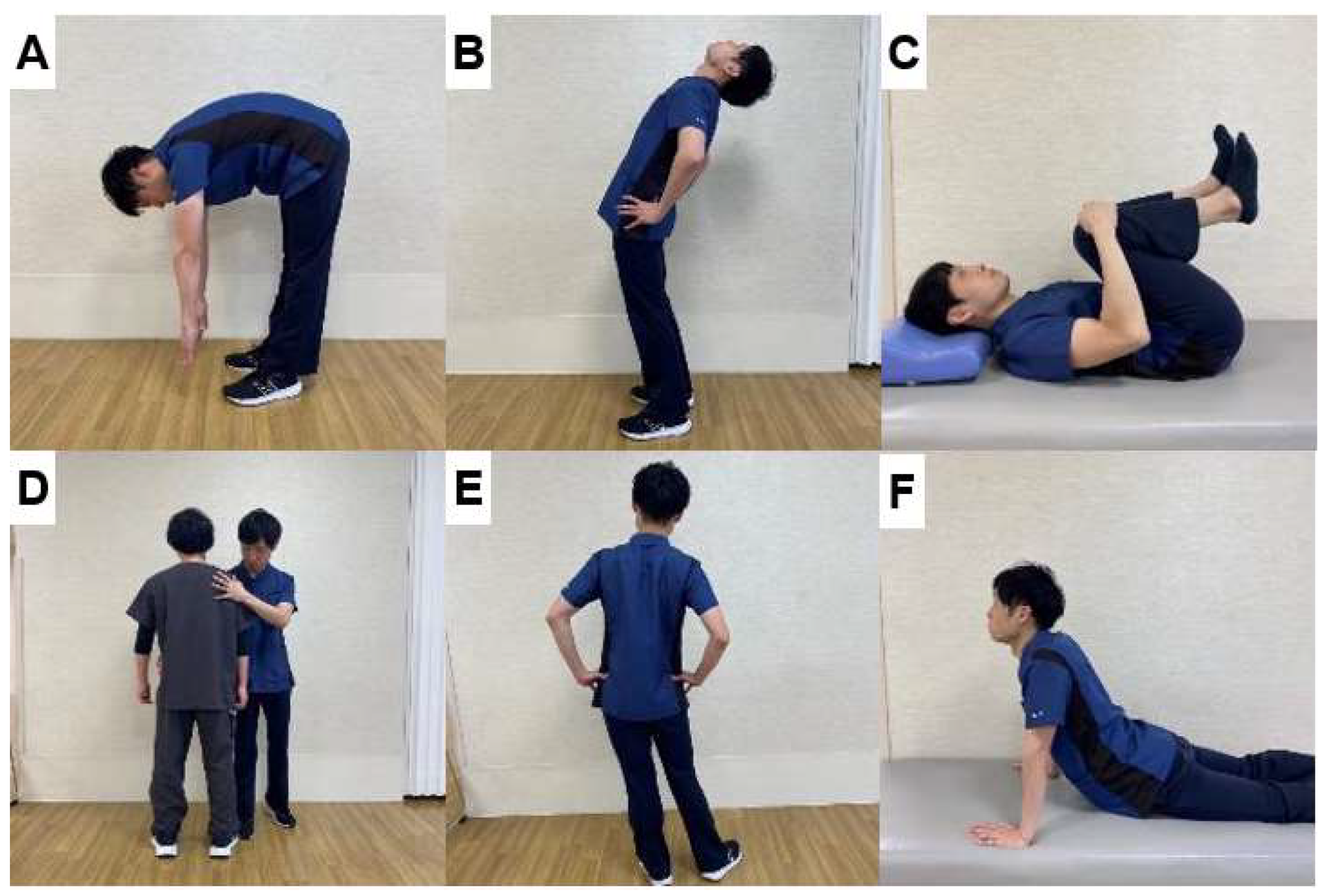
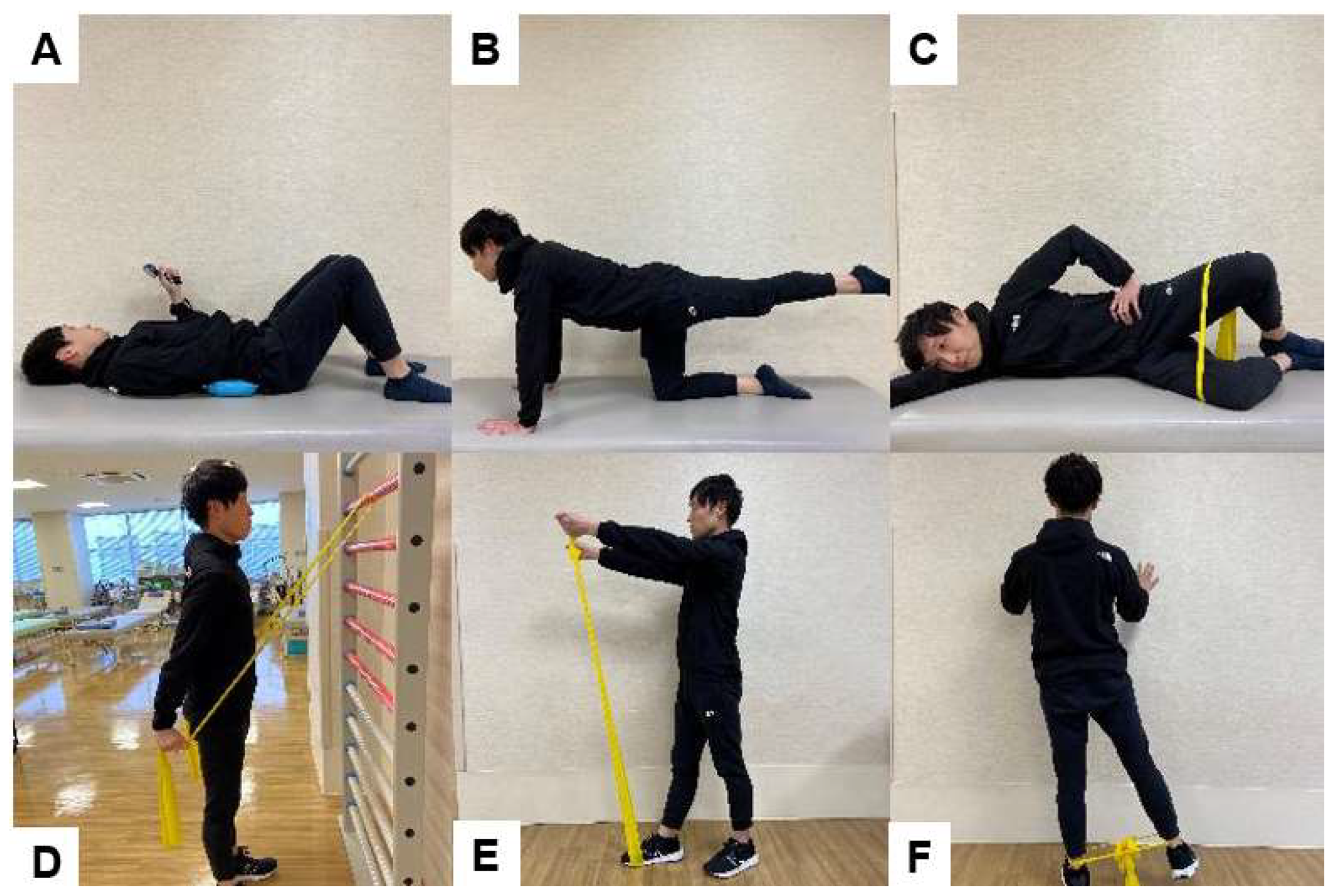
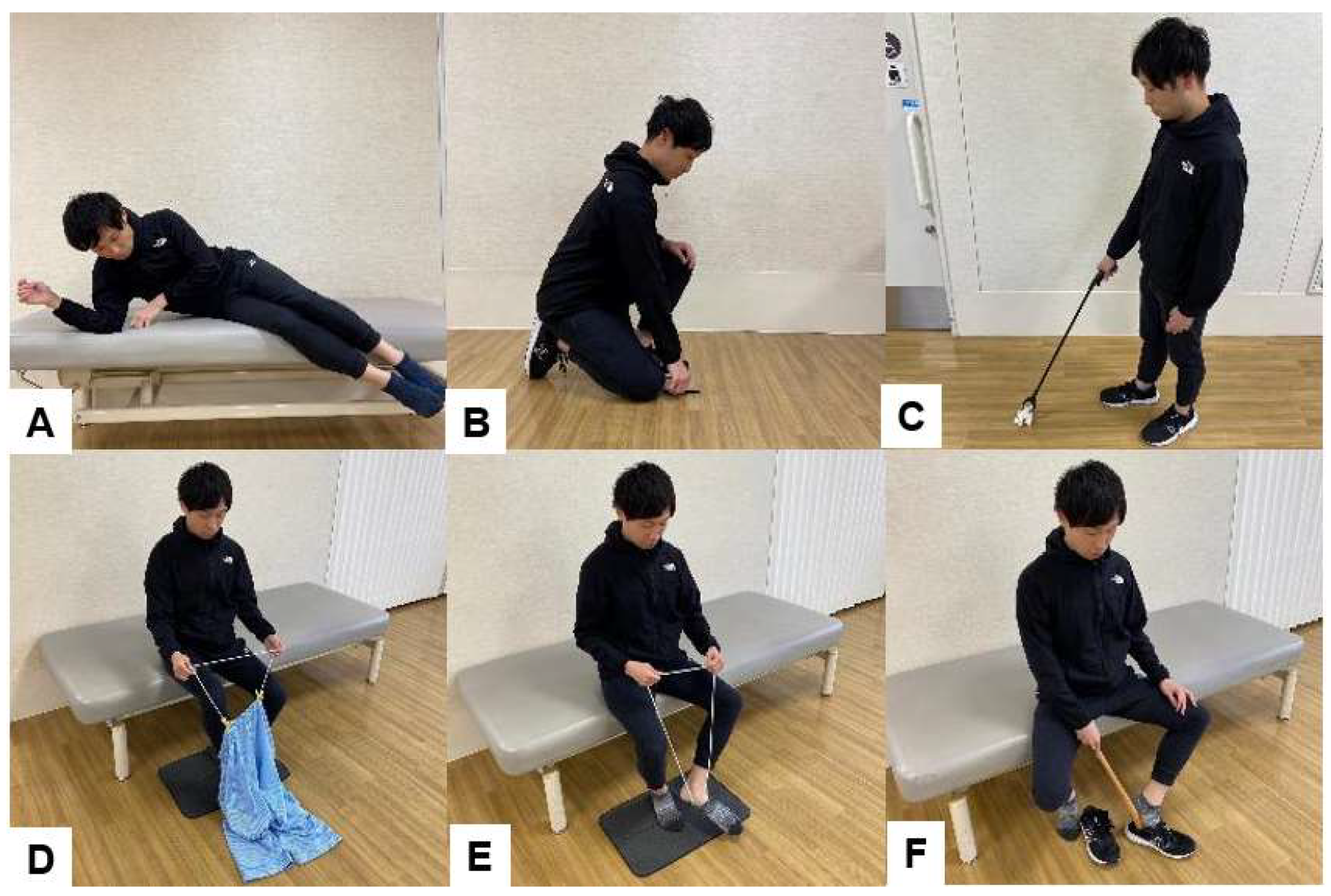
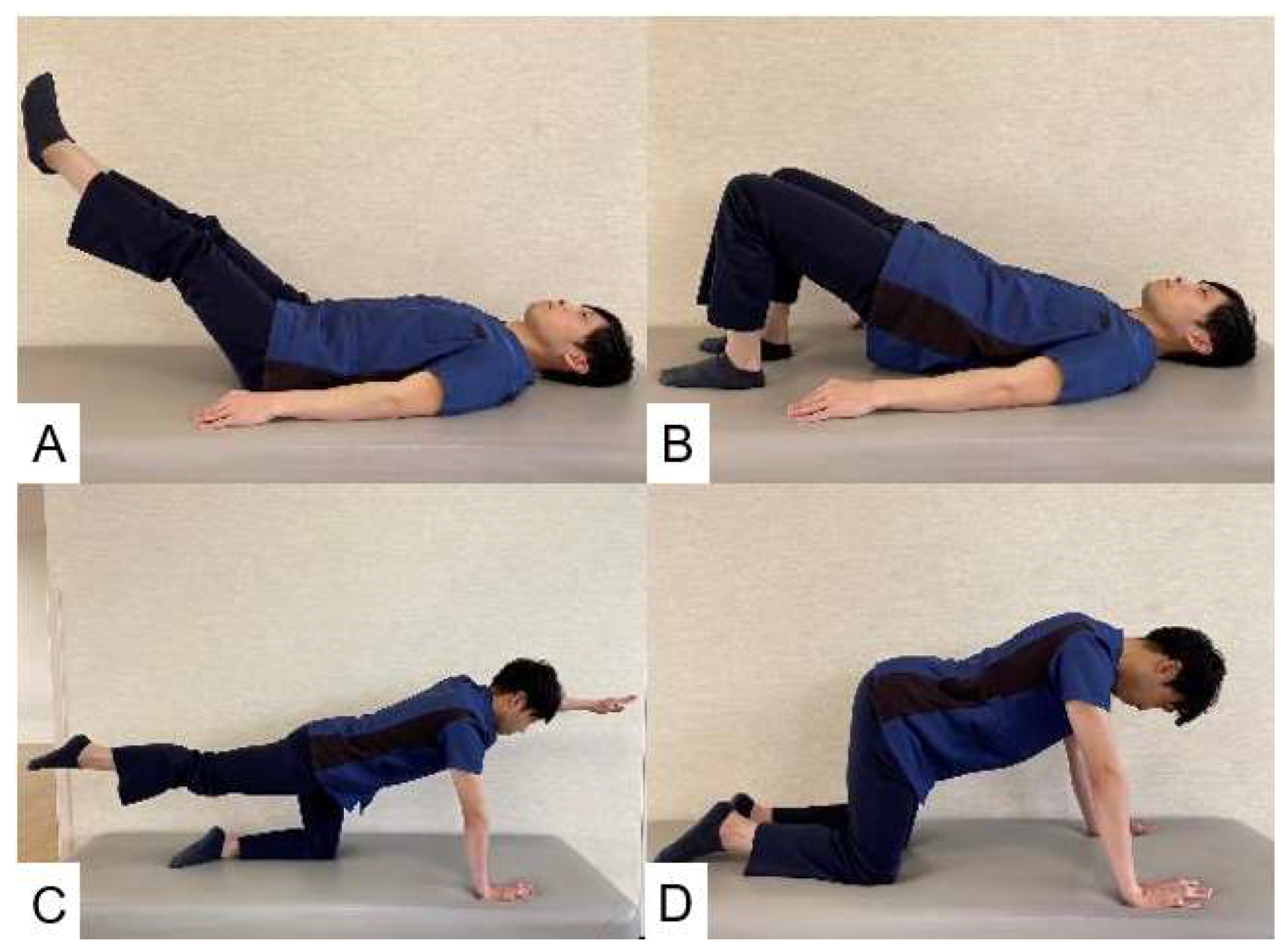
6.1. Trunk Muscle Strengthening (Figure 12)
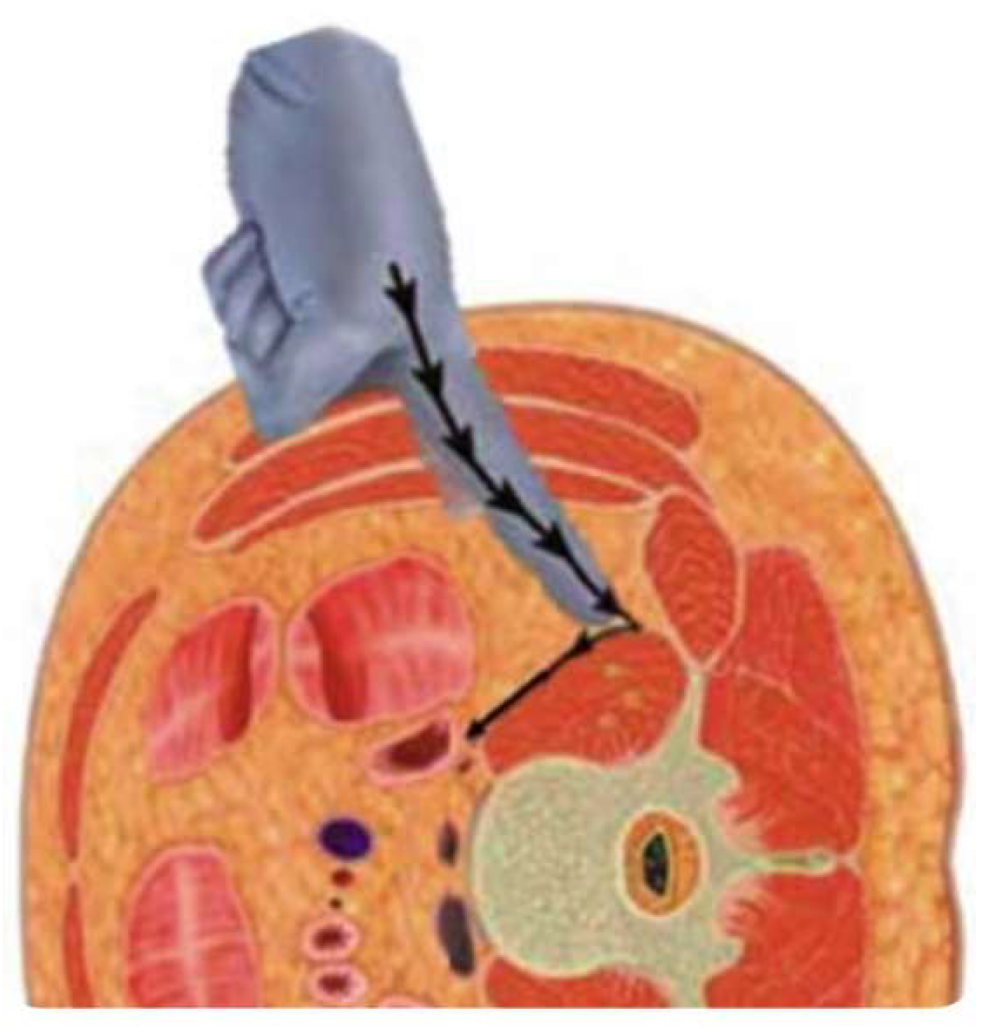
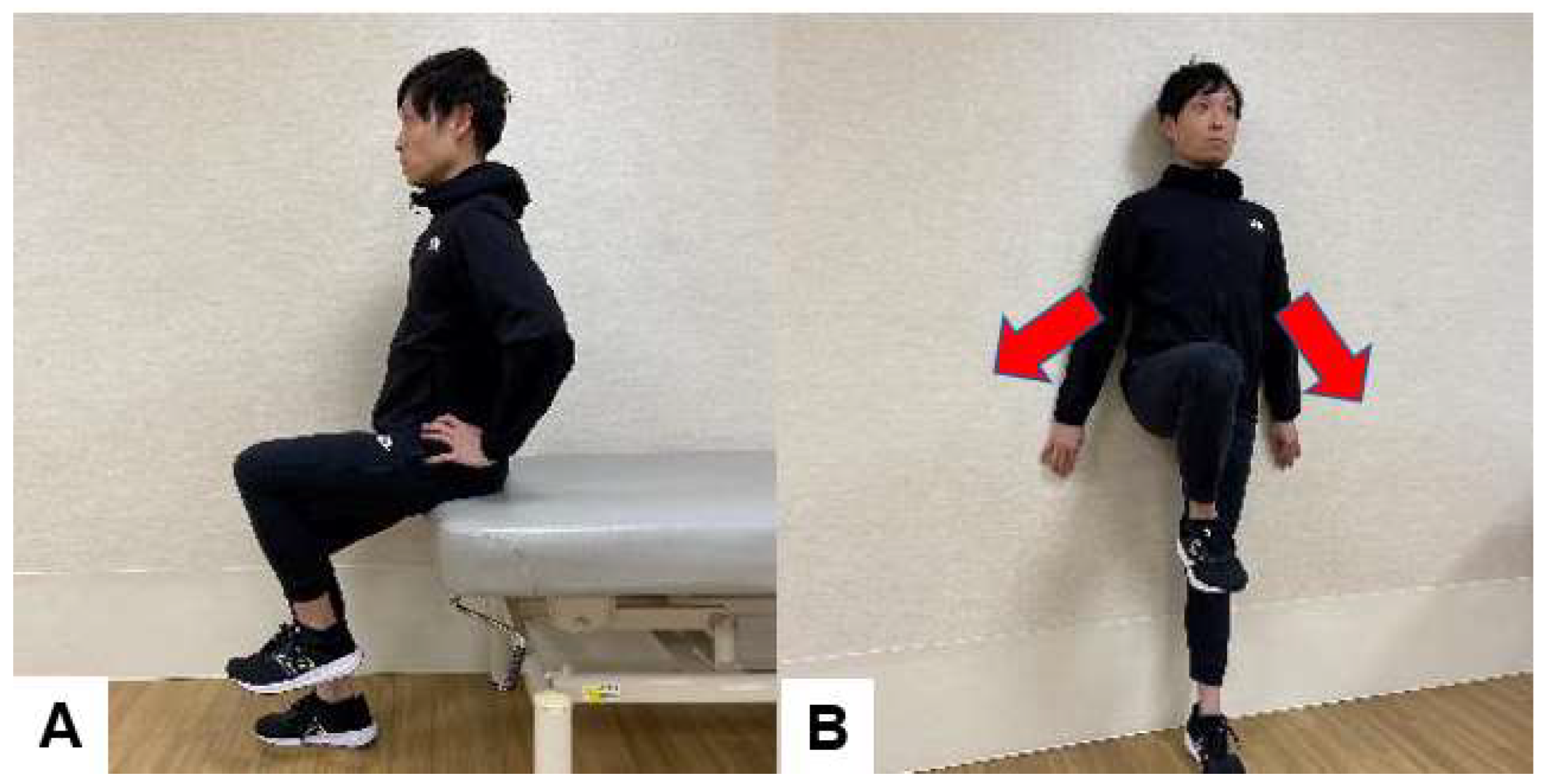
6.2. Psoas Muscle Strengthening
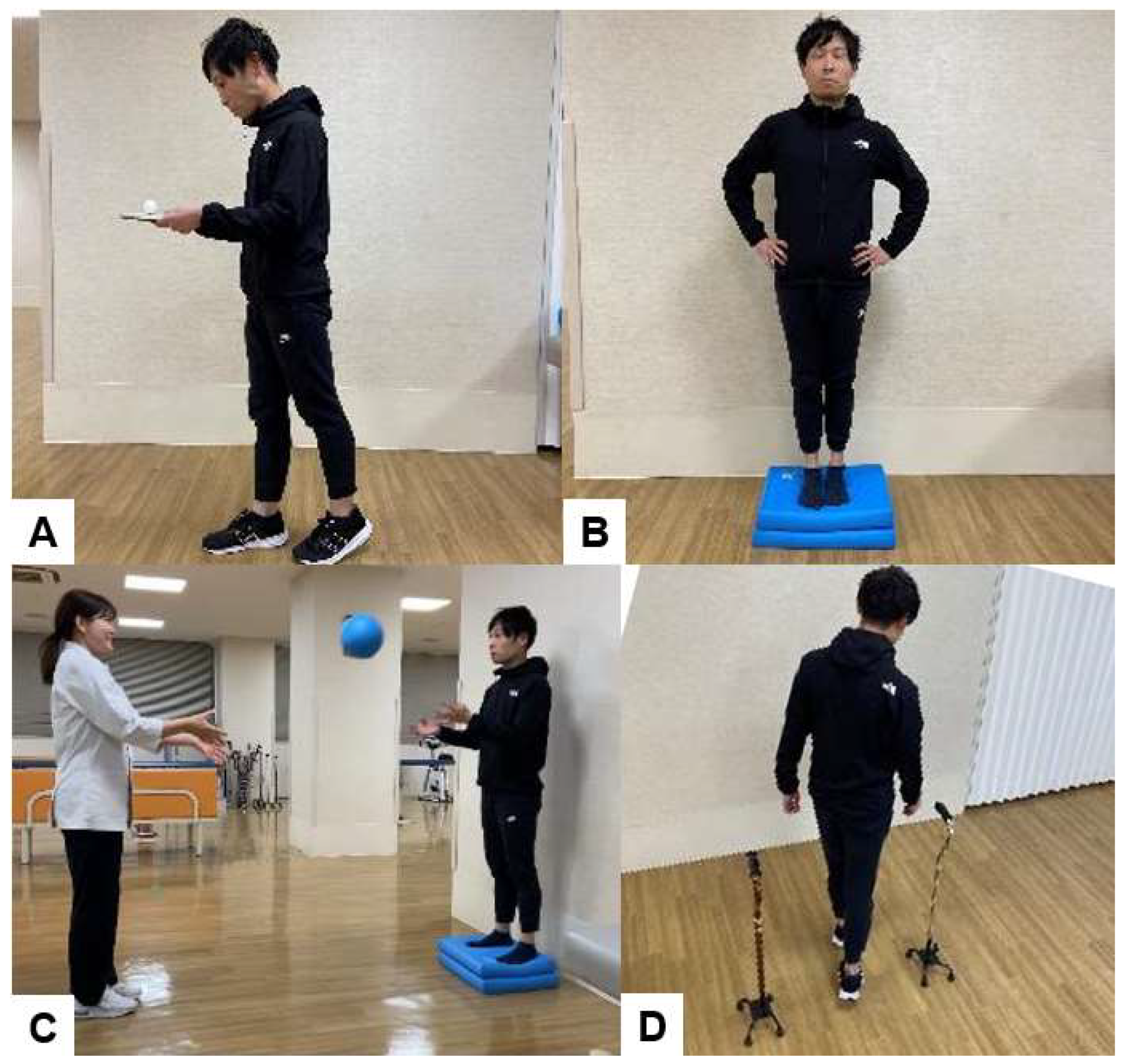
6.3. Exercises to Improve Balance after Spinal Fusion Surgery
6.4. Guidance on ADL after Spinal Fusion Surgery
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Woolf, A.D. and Pfleger, B., 2003. Burden of major musculoskeletal conditions. Bulletin of the world healthorganization, 81(9), pp.646-656.
- Manchikanti, L., Singh, V., Falco, F.J., Benyamin, R.M. and Hirsch, J.A., 2014. Epidemiology of low back pain in adults. Neuromodulation: Technology at the Neural Interface, 17, pp.3-10.
- Fehlings, M.G., Tetreault, L., Nater, A., Choma, T., Harrop, J., Mroz, T., Santaguida, C. and Smith, J.S., 2015. The aging of the global population: the changing epidemiology of disease and spinal disorders. Neurosurgery, 77, pp.S1-S5.
- Sivasubramaniam, V., Patel, H.C., Ozdemir, B.A. and Papadopoulos, M.C., 2015. Trends in hospital admissions and surgical procedures for degenerative lumbar spine disease in England: a 15-year time-series study. BMJ open, 5(12), p.e009011.
- Kobayashi, K., Sato, K., Kato, F., Kanemura, T., Yoshihara, H., Sakai, Y., Shinjo, R., Ohara, T., Yagi, H., Matsubara, Y. and Ando, K., 2022. Trends in the numbers of spine surgeries and spine surgeons over the past 15 years. Nagoya Journal of Medical Science, 84(1), p.1.
- Cancelliere C, Wong JJ, Yu H, Nordin M, Mior S, Pereira P, Brunton G, Shearer H, Connell G, Verville L, Taylor-Vaisey A, Côté P. Postsurgical rehabilitation for adults with low back pain with or without radiculopathy who were treated surgically: protocol for a mixed studies systematic review. BMJ Open. 2020 Mar 29;10(3):e036817. [CrossRef] [PubMed] [PubMed Central]
- Ebenbichler GR, Inschlag S, Pflüger V, Stemberger R, Wiesinger G, Novak K, Christoph K, Resch KL. Twelve-year follow-up of a randomized controlled trial of comprehensive physiotherapy following disc herniation operation. Clin Rehabil. 2015 Jun;29(6):548-60. Epub 2014 Oct 6. Erratum in: Clin Rehabil. 2016 Jun;30(6):623. [CrossRef] [PubMed]
- Archer KR, Devin CJ, Vanston SW, Koyama T, Phillips SE, Mathis SL, George SZ, McGirt MJ, Spengler DM, Aaronson OS, Cheng JS, Wegener ST. Cognitive-Behavioral-Based Physical Therapy for Patients With Chronic Pain Undergoing Lumbar Spine Surgery: A Randomized Controlled Trial. J Pain. 2016 Jan;17(1):76-89. Epub 2015 Oct 23. Erratum in: J Pain. 2017 Apr;18(4):477. [CrossRef] [PubMed] [PubMed Central]
- Lindgreen P, Rolving N, Nielsen CV, Lomborg K. Interdisciplinary Cognitive-Behavioral Therapy as Part of Lumbar Spinal Fusion Surgery Rehabilitation: Experience of Patients With Chronic Low Back Pain. Orthop Nurs. 2016 Jul.
- Rushton, A., Eveleigh, G., Petherick, E. J., Heneghan, N., Bennett, R., James, G., & Wright, C. (2012). Physiotherapy rehabilitation following lumbar spinal fusion: a systematic review and meta-analysis of randomised controlled trials. BMJ open, 2(4), e000829.
- Wibault, J., Öberg, B., Dedering, Å., Löfgren, H., Zsigmond, P., & Peolsson, A. (2017). Structured postoperative physiotherapy in patients with cervical radiculopathy: 6-month outcomes of a randomized clinical trial. Journal of Neurosurgery: Spine, 28(1), 1-9.
- Ditunno, J. F. (2017). Linking spinal cord injury rehabilitation between the World Wars: The R. Tait McKenzie legacy. The Journal of Spinal Cord Medicine, 40(6), 641–648. [CrossRef]
- Shrosbree RD. Spinal cord injuries as a result of motorcycle accidents. Paraplegia. 1978 May;16(1):102-12. [CrossRef] [PubMed]
- Bolton D. Looking forward to a decade of the biopsychosocial model. BJPsych Bulletin. 2022;46(4):228-232. [CrossRef]
- Vásquez-Ríos JR, Nava-Bringas TI. Lumbar stabilization exercises. Cir Cir. 2014;82:306–313.
- Dydyk AM, Sapra A. Williams Back Exercises. Treasure Island, FL: Stat Pearls Publishing; 2020. https://www.ncbi.nlm.nih.gov/books/NBK551558/.
- Kelly RP, Johnson JT. Acute low back pain. J Am Med Assoc. 1955 Aug 27;158(17):1520-1.
- Pheasant HC. Practical posture building. Clin Orthop. 1962;25:83-91. PMID: 13943115.
- Cailliet R: Low back pain syndrome. Philadelphia: Daves Company, 1998, pp 156–178.
- Böhler L. Ubungsbehandlung von Wirbelbrüchen [Exercise therapy in vertebral fractures]. Hefte Unfallheilkd. 1971;108:60-3.
- McKenzie R. Acute low back ache and exercises. N Z Med J. 1994 Aug 10;107(983):318. [PubMed]
- Niederer D, Mueller J. Sustainability effects of motor control stabilisation exercises on pain and function in chronic nonspecific low back pain patients: A systematic review with meta-analysis and meta-regression. PLoS One. 2020 Jan 15;15(1):e0227423. [CrossRef] [PubMed] [PubMed Central]
- WHO guideline for non-surgical management of chronic primary low back pain in adults. https://www.who.int/publications/i/item/9789240081789.
- The World Health Organization World report on disability: chapter 4 rehabilitation. Available: https://www.spine.org/Documents/ResearchClinicalCare/Guidelines/LumbarDiscHerniation.pdf [Accessed 4 Apr 2024].
- Snowdon M, Peiris CL. Physiotherapy Commenced Within the First Four Weeks Post-Spinal Surgery Is Safe and Effective: A Systematic Review and Meta-Analysis. Arch Phys Med Rehabil. 2016 Feb;97(2):292-301. Epub 2015 Sep 25. [CrossRef] [PubMed]
- Elsayyad MM, Abdel-Aal NM, Helal ME. Effect of Adding Neural Mobilization Versus Myofascial Release to Stabilization Exercises after Lumbar Spine Fusion: A Randomized Controlled Trial. Arch Phys Med Rehabil. 2021 Feb;102(2):251-260. Epub 2020 Aug 19. [CrossRef] [PubMed]
- Daniels CJ, Cupler ZA, Gliedt JA, Walters S, Schielke AL, Hinkeldey NA, Golley DJ, Hawk C. Manipulative and manual therapies in the management of patients with prior lumbar surgery: A systematic review. Complement Ther Clin Pract. 2021 Feb;42:101261. Epub 2020 Nov 17. [CrossRef] [PubMed]
- Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989 Dec;10(4):407-15. [CrossRef] [PubMed]
- van Hooff ML, Mannion AF, Staub LP, Ostelo RW, Fairbank JC. Determination of the Oswestry Disability Index score equivalent to a "satisfactory symptom state" in patients undergoing surgery for degenerative disorders of the lumbar spine-a Spine Tango registry-based study. Spine J. 2016 Oct;16(10):1221-1230. Epub 2016 Jun 22. [CrossRef] [PubMed]
- Issa TZ, Lee Y, Henry TW, Trenchfield D, Schroeder GD, Vaccaro AR, Kepler CK. Values derived from patient reported outcomes in spine surgery: a systematic review of the minimal clinically important difference, substantial clinical benefit, and patient acceptable symptom state. Eur Spine J. 2023 Oct;32(10):3333-3351. Epub 2023 Aug 29. [CrossRef] [PubMed]
- Parker SL, Adogwa O, Paul AR, Anderson WN, Aaronson O, Cheng JS, McGirt MJ. Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine. 2011 May;14(5):598-604. Epub 2011 Feb 18. [CrossRef] [PubMed]
- Parker SL, Adogwa O, Mendenhall SK, Shau DN, Anderson WN, Cheng JS, Devin CJ, McGirt MJ. Determination of minimum clinically important difference (MCID) in pain, disability, and quality of life after revision fusion for symptomatic pseudoarthrosis. Spine J. 2012 Dec;12(12):1122-8. Epub 2012 Nov 14. [CrossRef] [PubMed]
- Johnsen LG, Hellum C, Nygaard OP, Storheim K, Brox JI, Rossvoll I, Leivseth G, Grotle M. Comparison of the SF6D, the EQ5D, and the oswestry disability index in patients with chronic low back pain and degenerative disc disease. BMC Musculoskelet Disord. 2013 Apr 26;14:148. [CrossRef] [PubMed] [PubMed Central]
- Solberg T, Johnsen LG, Nygaard ØP, Grotle M. Can we define success criteria for lumbar disc surgery? : estimates for a substantial amount of improvement in core outcome measures. Acta Orthop. 2013 Apr;84(2):196-201. Epub 2013 Mar 19. [CrossRef] [PubMed] [PubMed Central]
- Yoshida G, Hasegawa T, Yamato Y, Kobayashi S, Shin O, Banno T, Mihara Y, Arima H, Ushirozako H, Yasuda T, Togawa D, Matsuyama Y. Minimum Clinically Important Differences in Oswestry Disability Index Domains and Their Impact on Adult Spinal Deformity Surgery. Asian Spine J. 2019 Feb;13(1):35-44. Epub 2018 Oct 18. [CrossRef] [PubMed] [PubMed Central]
- Fukushima M, Oka H, Oshima Y, Yuzawa Y, Matsudaira K, Tanaka S, Inanami H. Evaluation of the Minimum Clinically Important Differences of the Zurich Claudication Questionnaire in Patients With Lumbar Spinal Stenosis. Clin Spine Surg. 2020 Dec;33(10):E499-E503. [CrossRef] [PubMed]
- Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976). 1983 Mar;8(2):141-4. [CrossRef] [PubMed]
- Fujiwara A, Kobayashi N, Saiki K, Kitagawa T, Tamai K, Saotome K. Association of the Japanese Orthopaedic Association score with the Oswestry Disability Index, Roland-Morris Disability Questionnaire, and short-form 36. Spine (Phila Pa 1976). 2003 Jul 15;28(14):1601-7. [PubMed]
- Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000 Nov 15;25(22):2940-52; discussion 2952. [CrossRef] [PubMed]
- Vianin M. Psychometric properties and clinical usefulness of the Oswestry Disability Index. J Chiropr Med. 2008 Dec;7(4):161-3. [CrossRef] [PubMed] [PubMed Central]
- Haro H, Maekawa S, Hamada Y. Prospective analysis of clinical evaluation and self-assessment by patients after decompression surgery for degenerative lumbar canal stenosis. Spine J. 2008 Mar-Apr;8(2):380-4. Epub 2007 Mar 13. [CrossRef] [PubMed]
- Carreon LY, Berven SH, Djurasovic M, Bratcher KR, Glassman SD. The discriminative properties of the SF-6D compared with the SF-36 and ODI. Spine (Phila Pa 1976). 2013 Jan 1;38(1):60-4. [CrossRef] [PubMed]
- Stucki G, Daltroy L, Liang MH, Lipson SJ, Fossel AH, Katz JN. Measurement properties of a self-administered outcome measure in lumbar spinal stenosis. Spine (Phila Pa 1976). 1996 Apr 1;21(7):796-803. [CrossRef] [PubMed]
- North American Spine Society (NASS). Clinical Guidelines for Multidisciplinary Spine Care Diagnosis and Treatment of Degenerative Lumbar Spinal Stenosis. Burr Ridge (IL): North American Spine Society (NASS); 2007.
- Bae J, Theologis AA, Strom R, Tay B, Burch S, Berven S, Mummaneni PV, Chou D, Ames CP, Deviren V. Comparative analysis of 3 surgical strategies for adult spinal deformity with mild to moderate sagittal imbalance. J Neurosurg Spine. 2018 Jan;28(1):40-49. Epub 2017 Nov 3. [CrossRef] [PubMed]
- Lonner B, Yoo A, Terran JS, Sponseller P, Samdani A, Betz R, Shuffelbarger H, Shah SA, Newton P. Effect of spinal deformity on adolescent quality of life: comparison of operative scheuermann kyphosis, adolescent idiopathic scoliosis, and normal controls. Spine (Phila Pa 1976). 2013 May 20;38(12):1049-55. [CrossRef] [PubMed]
- Haher TR, Gorup JM, Shin TM, Homel P, Merola AA, Grogan DP, Pugh L, Lowe TG, Murray M. Results of the Scoliosis Research Society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis. A multicenter study of 244 patients. Spine (Phila Pa 1976). 1999 Jul 15;24(14):1435-40. [CrossRef] [PubMed]
- Berven S, Deviren V, Demir-Deviren S, Hu SS, Bradford DS. Studies in the modified Scoliosis Research Society Outcomes Instrument in adults: validation, reliability, and discriminatory capacity. Spine (Phila Pa 1976). 2003 Sep 15;28(18):2164-9; discussion 2169. [CrossRef] [PubMed]
- Yoshihara H, Hasegawa K, Okamoto M, Hatsushikano S, Watanabe K. Relationship between sagittal radiographic parameters and disability in patients with spinal disease using 3D standing analysis. Orthop Traumatol Surg Res. 2018 Nov;104(7):1017-1023. Epub 2018 Aug 11. [CrossRef] [PubMed]
- Smith JS, Klineberg E, Schwab F, Shaffrey CI, Moal B, Ames CP, Hostin R, Fu KM, Burton D, Akbarnia B, Gupta M, Hart R, Bess S, Lafage V; International Spine Study Group. Change in classification grade by the SRS-Schwab Adult Spinal Deformity Classification predicts impact on health-related quality of life measures: prospective analysis of operative and nonoperative treatment. Spine (Phila Pa 1976). 2013 Sep 1;38(19):1663-71. [CrossRef] [PubMed]
- Hart RA, Pro SL, Gundle KR, Marshall LM. Lumbar stiffness as a collateral outcome of spinal arthrodesis: a preliminary clinical study. Spine J. 2013 Feb;13(2):150-6. Epub 2012 Dec 6. [CrossRef] [PubMed]
- Hart RA, Gundle KR, Pro SL, Marshall LM. Lumbar Stiffness Disability Index: pilot testing of consistency, reliability, and validity. Spine J. 2013 Feb;13(2):157-61. Epub 2013 Jan 19. [CrossRef] [PubMed]
- Furuya H, Ito T, Hirohata K, Mitomo S, Yamasaki K, Igarashi H, Omori K, Hoshino M, Hart RA. Construct Validity and Reliability of the Japanese Version of the Lumbar Stiffness Disability Index. Spine (Phila Pa 1976). 2021 Mar 1;46(5):E333-E337. [CrossRef] [PubMed]
- Durand WM, Daniels AH, Hamilton DK, Passias PG, Kim HJ, Protopsaltis T, Lafage V, Smith JS, Shaffrey C, Gupta M, Kelly MP, Klineberg E, Schwab F, Burton D, Bess S, Ames C, Hart R; International Spine Study Group. Younger Patients Are Differentially Affected by Stiffness-Related Disability Following Adult Spinal Deformity Surgery. World Neurosurg. 2019 Dec;132:e297-e304. Epub 2019 Aug 31. [CrossRef] [PubMed]
- Daniels AH, Reid D, Durand W, Disilvestro K, Hamilton DK, Passias P, Kim HJ, Protopsaltis T, LaFage V, Smith JS, Shaffrey C, Gupta M, Klineberg E, Schwab F, Burton D, Bess S, Ames C, Hart R; International Spine Study Group. Sexual Dysfunction Secondary to Lumbar Stiffness in Adult Spinal Deformity Patients Before and After Long-Segment Spinal Fusion. World Neurosurg. 2020 Jul;139:e474-e479. Epub 2020 Apr 18. [CrossRef] [PubMed]
- Watters WC 3rd, Baisden J, Gilbert TJ, Kreiner S, Resnick DK, Bono CM, Ghiselli G, Heggeness MH, Mazanec DJ, O'Neill C, Reitman CA, Shaffer WO, Summers JT, Toton JF; North American Spine Society. Degenerative lumbar spinal stenosis: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis. Spine J. 2008 Mar-Apr;8(2):305-10. Epub 2007 Dec 21. [CrossRef] [PubMed]
- Ishimoto Y, Yoshimura N, Muraki S, Yamada H, Nagata K, Hashizume H, Takiguchi N, Minamide A, Oka H, Kawaguchi H, Nakamura K, Akune T, Yoshida M. Prevalence of symptomatic lumbar spinal stenosis and its association with physical performance in a population-based cohort in Japan: the Wakayama Spine Study. Osteoarthritis Cartilage. 2012 Oct;20(10):1103-8. Epub 2012 Jul 10. [CrossRef] [PubMed]
- Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010 Apr 7;303(13):1259-65. [CrossRef] [PubMed] [PubMed Central]
- Nagai S, Kawabata S, Michikawa T, Ito K, Takeda H, Ikeda D, Kaneko S, Fujita N. Association between frailty and locomotive syndrome in elderly patients with lumbar spinal stenosis: A retrospective longitudinal analysis. Geriatr Gerontol Int. 2024 Jan;24(1):116-122. Epub 2023 Dec 23. [CrossRef] [PubMed]
- Kato S, Demura S, Kabata T, Matsubara H, Kurokawa Y, Okamoto Y, Kuroda K, Kajino Y, Yokogawa N, Inoue D, Tsuchiya H. Risk factors that hinder locomotive syndrome improvement following surgery for musculoskeletal diseases in older patients: A multicentre prospective study. Mod Rheumatol. 2023 Jul 4;33(4):836-842. [CrossRef] [PubMed]
- Kobayashi T, Morimoto T, Otani K, Mawatari M. Locomotive Syndrome and Lumbar Spine Disease: A Systematic Review. J Clin Med. 2022 Feb 27;11(5):1304. [CrossRef] [PubMed] [PubMed Central]
- Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, Brach J, Chandler J, Cawthon P, Connor EB, Nevitt M, Visser M, Kritchevsky S, Badinelli S, Harris T, Newman AB, Cauley J, Ferrucci L, Guralnik J. Gait speed and survival in older adults. JAMA. 2011 Jan 5;305(1):50-8. [CrossRef] [PubMed] [PubMed Central]
- Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, Schneider SM, Sieber CC, Topinkova E, Vandewoude M, Visser M, Zamboni M; Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019 Jan 1;48(1):16-31. Erratum in: Age Ageing. 2019 Jul 1;48(4):601. [CrossRef] [PubMed] [PubMed Central]
- Wada T, Tanishima S, Kitsuda Y, Osaki M, Nagashima H, Noma H, Hagino H. Walking speed is associated with postoperative pain catastrophizing in patients with lumbar spinal stenosis: a prospective observational study. BMC Musculoskelet Disord. 2022 Dec 20;23(1):1108. [CrossRef] [PubMed] [PubMed Central]
- Sakaguchi T, Meena U, Tanaka M, Xiang H, Fujiwara Y, Arataki S, Taoka T, Takamatsu K, Yasuda Y, Nakagawa M, Utsunomiya K. Minimal Clinically Important Differences in Gait and Balance Ability in Patients Who Underwent Corrective Long Spinal Fusion for Adult Spinal Deformity. J Clin Med. 2023 Oct 12;12(20):6500. [CrossRef] [PubMed] [PubMed Central]
- Singh SJ, Puhan MA, Andrianopoulos V, Hernandes NA, Mitchell KE, Hill CJ, Lee AL, Camillo CA, Troosters T, Spruit MA, Carlin BW, Wanger J, Pepin V, Saey D, Pitta F, Kaminsky DA, McCormack MC, MacIntyre N, Culver BH, Sciurba FC, Revill SM, Delafosse V, Holland AE. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. Eur Respir J. 2014 Dec;44(6):1447-78. Epub 2014 Oct 30. [CrossRef] [PubMed]
- Takenaka H, Kamiya M, Sugiura H, Nishihama K, Ito A, Suzuki J, Hanamura S. Responsiveness and Minimal Clinically Important Difference of the 6-minute Walk Distance in Patients Undergoing Lumbar Spinal Canal Stenosis Surgery. Clin Spine Surg. 2022 Apr 1;35(3):E345-E350. [CrossRef] [PubMed]
- Kondo R, Yamato Y, Nagafusa T, Mizushima T, Hasegawa T, Kobayashi S, Togawa D, Oe S, Kurosu K, Matsuyama Y. Effect of corrective long spinal fusion to the ilium on physical function in patients with adult spinal deformity. Eur Spine J. 2017 Aug;26(8):2138-2145. Epub 2017 Feb 11. [CrossRef] [PubMed]
- Tomkins-Lane CC, Battié MC. Validity and reproducibility of self-report measures of walking capacity in lumbar spinal stenosis. Spine (Phila Pa 1976). 2010 Nov 1;35(23):2097-102. [CrossRef] [PubMed]
- Takenaka H, Kamiya M, Sugiura H, Nishihama K, Suzuki J, Hanamura S. Minimal Clinically Important Difference of the 6-Minute Walk Distance in Patients Undergoing Lumbar Spinal Canal Stenosis Surgery: 12 Months Follow-Up. Spine (Phila Pa 1976). 2023 Apr 15;48(8):559-566. Epub 2022 Dec 28. [CrossRef] [PubMed]
- Gautschi OP, Smoll NR, Corniola MV, Joswig H, Chau I, Hildebrandt G, Schaller K, Stienen MN. Validity and Reliability of a Measurement of Objective Functional Impairment in Lumbar Degenerative Disc Disease: The Timed Up and Go (TUG) Test. Neurosurgery. 2016 Aug;79(2):270-8. [CrossRef] [PubMed]
- Lin SI, Lin RM. Disability and walking capacity in patients with lumbar spinal stenosis: association with sensorimotor function, balance, and functional performance. J Orthop Sports Phys Ther. 2005 Apr;35(4):220-6. [CrossRef] [PubMed]
- Joswig H, Stienen MN, Smoll NR, Corniola MV, Chau I, Schaller K, Hildebrandt G, Gautschi OP. Effects of Smoking on Subjective and Objective Measures of Pain Intensity, Functional Impairment, and Health-Related Quality of Life in Lumbar Degenerative Disk Disease. World Neurosurg. 2017 Mar;99:6-13. Epub 2016 Nov 22. [CrossRef] [PubMed]
- Stienen MN, Joswig H, Smoll NR, Corniola MV, Schaller K, Hildebrandt G, Gautschi OP. Influence of Body Mass Index on Subjective and Objective Measures of Pain, Functional Impairment, and Health-Related Quality of Life in Lumbar Degenerative Disc Disease. World Neurosurg. 2016 Dec;96:570-577.e1. Epub 2016 Sep 28. [CrossRef] [PubMed]
- Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991 Feb;39(2):142-8. [CrossRef] [PubMed]
- Maldaner N, Sosnova M, Ziga M, Zeitlberger AM, Bozinov O, Gautschi OP, Weyerbrock A, Regli L, Stienen MN. External Validation of the Minimum Clinically Important Difference in the Timed-up-and-go Test After Surgery for Lumbar Degenerative Disc Disease. Spine (Phila Pa 1976). 2022 Feb 15;47(4):337-342. [CrossRef] [PubMed]
- Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol. 1990 Nov;45(6):M192-7. [CrossRef] [PubMed]
- Schenkman M, Morey M, Kuchibhatla M. Spinal flexibility and balance control among community-dwelling adults with and without Parkinson's disease. J Gerontol A Biol Sci Med Sci. 2000 Aug;55(8):M441-5. [CrossRef] [PubMed]
- de Waroquier-Leroy L, Bleuse S, Serafi R, Watelain E, Pardessus V, Tiffreau AV, Thevenon A. The Functional Reach Test: strategies, performance and the influence of age. Ann Phys Rehabil Med. 2014 Aug-Sep;57(6-7):452-64. Epub 2014 May 29. [CrossRef] [PubMed]
- Biering-Sørensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine (Phila Pa 1976). 1984 Mar;9(2):106-19. [CrossRef] [PubMed]
- Song J, Araghi K, Dupont MM, Shahi P, Bovonratwet P, Shinn D, Dalal SS, Melissaridou D, Virk SS, Iyer S, Dowdell JE, Sheha ED, Qureshi SA. Association between muscle health and patient-reported outcomes after lumbar microdiscectomy: early results. Spine J. 2022 Oct;22(10):1677-1686. Epub 2022 Jun 6. [CrossRef] [PubMed]
- Horak FB, Wrisley DM, Frank J. The Balance Evaluation Systems Test (BESTest) to differentiate balance deficits. Phys Ther. 2009 May;89(5):484-98. Epub 2009 Mar 27. [CrossRef] [PubMed] [PubMed Central]
- Moke L, Severijns P, Schelfaut S, Van de Loock K, Hermans L, Molenaers G, Jonkers I, Scheys L. Performance on Balance Evaluation Systems Test (BESTest) Impacts Health-Related Quality of Life in Adult Spinal Deformity Patients. Spine (Phila Pa 1976). 2018 May 1;43(9):637-646. [CrossRef] [PubMed]
- Severijns P, Overbergh T, Scheys L, Moke L, Desloovere K. Reliability of the balance evaluation systems test and trunk control measurement scale in adult spinal deformity. PLoS One. 2019 Aug 26;14(8):e0221489. [CrossRef] [PubMed] [PubMed Central]
- Franchignoni F, Horak F, Godi M, Nardone A, Giordano A. Using psychometric techniques to improve the Balance Evaluation Systems Test: the mini-BESTest. J Rehabil Med. 2010 Apr;42(4):323-31. [CrossRef] [PubMed] [PubMed Central]
- Miura K, Kadone H, Koda M, Abe T, Funayama T, Noguchi H, Mataki K, Nagashima K, Kumagai H, Shibao Y, Suzuki K, Yamazaki M. Thoracic kyphosis and pelvic anteversion in patients with adult spinal deformity increase while walking: analyses of dynamic alignment change using a three-dimensional gait motion analysis system. Eur Spine J. 2020 Apr;29(4):840-848. Epub 2020 Jan 31. [CrossRef] [PubMed]
- Asada T, Miura K, Koda M, Kadone H, Funayama T, Takahashi H, Noguchi H, Shibao Y, Sato K, Eto F, Mataki K, Yamazaki M. Can Proximal Junctional Kyphosis after Surgery for Adult Spinal Deformity Be Predicted by Preoperative Dynamic Sagittal Alignment Change with 3D Gait Analysis? A Case-Control Study. J Clin Med. 2022 Oct 4;11(19):5871. [CrossRef] [PubMed] [PubMed Central]
- Haddas R, Wood A, Lieberman I, Derman PB. Assessing the cone of economy in patients with spinal disease using only a force plate: an observational retrospective cohort study. Eur Spine J. 2021 Sep;30(9):2504-2513. Epub 2021 Apr 20. [CrossRef] [PubMed]
- Godzik J, Frames CW, Smith Hussain V, Olson MC, Kakarla UK, Uribe JS, Lockhart TE, Turner JD. Postural Stability and Dynamic Balance in Adult Spinal Deformity: Prospective Pilot Study. World Neurosurg. 2020 Sep;141:e783-e791. Epub 2020 Jun 12. [CrossRef]
- Yagi M, Ohne H, Konomi T, Fujiyoshi K, Kaneko S, Takemitsu M, Machida M, Yato Y, Asazuma T. Walking balance and compensatory gait mechanisms in surgically treated patients with adult spinal deformity. Spine J. 2017 Mar;17(3):409-417. Epub 2016 Oct 17. [CrossRef] [PubMed]
- Huysmans SMD, Senden R, Jacobs E, Willems PJB, Marcellis RGJ, Boogaart MVD, Meijer K, Willems PC. Gait alterations in patients with adult spinal deformity. N Am Spine Soc J. 2023 Dec 30;17:100306. [CrossRef] [PubMed] [PubMed Central]
- Zhong R, Rau PP. Are cost-effective technologies feasible to measure gait in older adults? A systematic review of evidence-based literature. Arch Gerontol Geriatr. 2020 Mar-Apr;87:103970. Epub 2019 Nov 2. [CrossRef] [PubMed]
- Sekine M, Tamura T, Yoshida M, Suda Y, Kimura Y, Miyoshi H, Kijima Y, Higashi Y, Fujimoto T. A gait abnormality measure based on root mean square of trunk acceleration. J Neuroeng Rehabil. 2013 Dec 26;10:118. [CrossRef] [PubMed] [PubMed Central]
- Sakaguchi, T.; Sake, N.; Tanaka, M.; Fujiwara, Y.; Arataki, S.; Taoka, T.; Kodama, Y.; Takamatsu, K.; Yasuda, Y.; Nakagawa, M.; et al. Use of a Triaxial Accelerometer to Measure Changes in Gait Sway and Related Motor Function after Corrective Spinal Fusion Surgery for Adult Spinal Deformity. J. Clin. Med. 2024, 13, 1923. [CrossRef]
- Hulleck AA, Menoth Mohan D, Abdallah N, El Rich M, Khalaf K. Present and future of gait assessment in clinical practice: Towards the application of novel trends and technologies. Front Med Technol. 2022 Dec 16;4:901331. [CrossRef] [PubMed] [PubMed Central]
- Menz HB, Lord SR, Fitzpatrick RC. Acceleration patterns of the head and pelvis when walking on level and irregular surfaces. Gait Posture. 2003 Aug;18(1):35-46. [CrossRef] [PubMed]
- Amundsen T, Weber H, Nordal HJ, Magnaes B, Abdelnoor M, Lilleâs F. Lumbar spinal stenosis: conservative or surgical management?: A prospective 10-year study. Spine (Phila Pa 1976). 2000 Jun 1;25(11):1424-35; discussion 1435-6. [CrossRef] [PubMed]
- Liang HF, Liu SH, Chen ZX, Fei QM. Decompression plus fusion versus decompression alone for degenerative lumbar spondylolisthesis: a systematic review and meta-analysis. Eur Spine J. 2017 Dec;26(12):3084-3095. Epub 2017 Jun 24. [CrossRef] [PubMed]
- Chen Z, Xie P, Feng F, Chhantyal K, Yang Y, Rong L. Decompression Alone Versus Decompression and Fusion for Lumbar Degenerative Spondylolisthesis: A Meta-Analysis. World Neurosurg. 2018 Mar;111:e165-e177. Epub 2017 Dec 14. [CrossRef] [PubMed]
- Briggs H, Milligan PR: Chip fusion of the low back following exploration of the spinal canal. J Bone Joint Surg 26:125- 130,1944.
- Hammad A, Wirries A, Ardeshiri A, Nikiforov O, Geiger F. Open versus minimally invasive TLIF: literature review and meta-analysis. J Orthop Surg Res. 2019 Jul 22;14(1):229. [CrossRef] [PubMed] [PubMed Central]
- Tan MWP, Sayampanathan AA, Jiang L, Guo CM. Comparison of Outcomes Between Single-level Lateral Lumbar Interbody Fusion and Transforaminal Lumbar Interbody Fusion: A Meta-analysis and Systematic Review. Clin Spine Surg. 2021 Dec 1;34(10):395-405. [CrossRef] [PubMed]
- Hsieh PC, Koski TR, O'Shaughnessy BA, Sugrue P, Salehi S, Ondra S, Liu JC. Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine. 2007 Oct;7(4):379-86. [CrossRef] [PubMed]
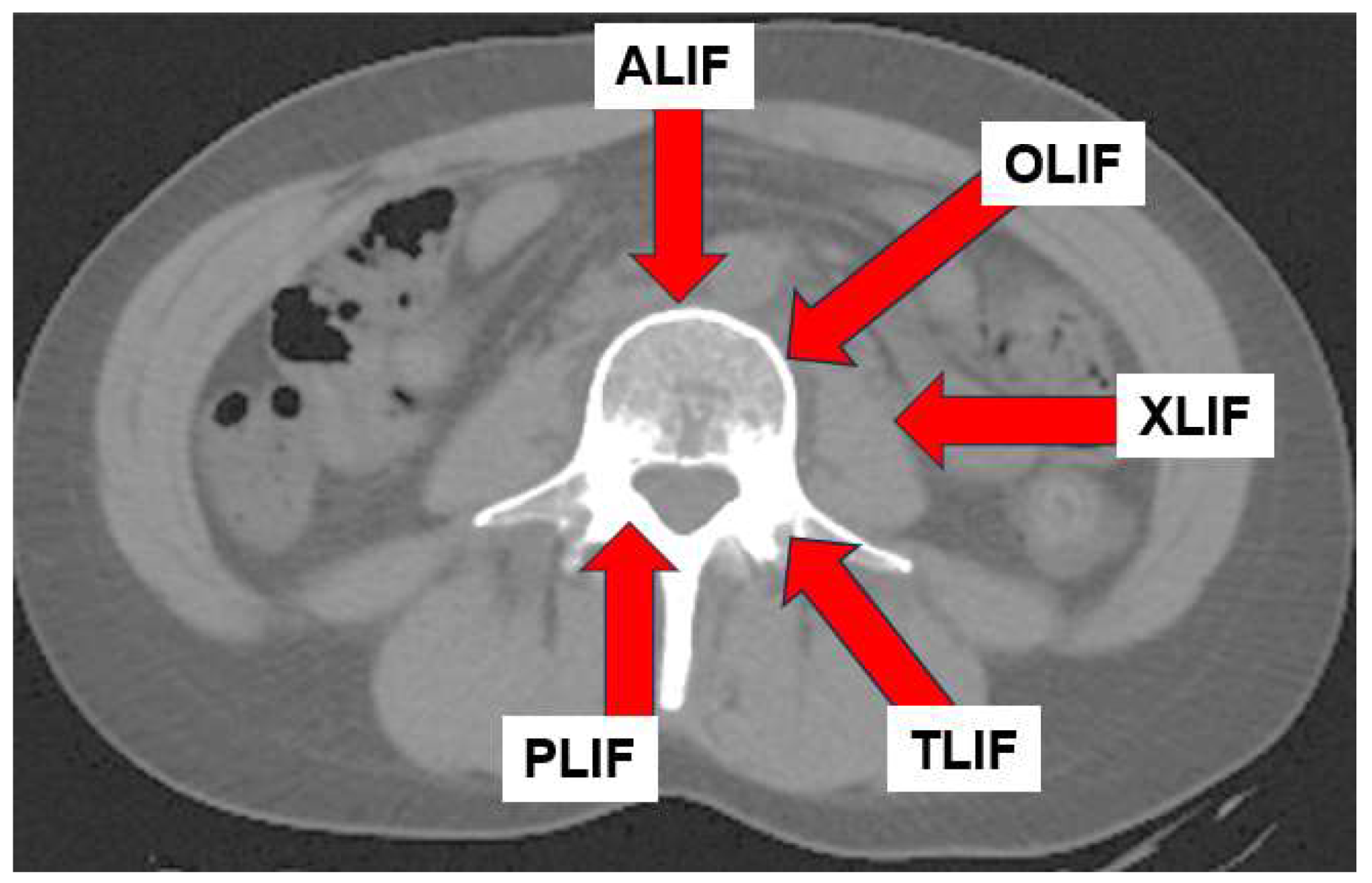
- Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015 Dec;1(1):2-18. [CrossRef] [PubMed] [PubMed Central]
- Waschke A, Hartmann C, Walter J, Dünisch P, Wahnschaff F, Kalff R, Ewald C. Denervation and atrophy of paraspinal muscles after open lumbar interbody fusion is associated with clinical outcome--electromyographic and CT-volumetric investigation of 30 patients. Acta Neurochir (Wien). 2014 Feb;156(2):235-44. Epub 2014 Jan 3. [CrossRef] [PubMed]
- Cho SM, Kim SH, Ha SK, Kim SD, Lim DJ, Cha J, Kim BJ. Paraspinal muscle changes after single-level posterior lumbar fusion: volumetric analyses and literature review. BMC Musculoskelet Disord. 2020 Feb 5;21(1):73. [CrossRef] [PubMed] [PubMed Central]
- Tarnanen S, Neva MH, Kautiainen H, Ylinen J, Pekkanen L, Kaistila T, Vuorenmaa M, Häkkinen A. The early changes in trunk muscle strength and disability following lumbar spine fusion. Disabil Rehabil. 2013 Jan;35(2):134-9. Epub 2012 Jun 7. [CrossRef] [PubMed]
- Tarnanen SP, Neva MH, Häkkinen K, Kankaanpää M, Ylinen J, Kraemer WJ, Newton RU, Häkkinen A. Neutral spine control exercises in rehabilitation after lumbar spine fusion. J Strength Cond Res. 2014 Jul;28(7):2018-25. [CrossRef] [PubMed]
- Hagins M, Adler K, Cash M, Daugherty J, Mitrani G. Effects of practice on the ability to perform lumbar stabilization exercises. J Orthop Sports Phys Ther. 1999 Sep;29(9):546-55. [CrossRef] [PubMed]
- Grooms DR, Grindstaff TL, Croy T, Hart JM, Saliba SA. Clinimetric analysis of pressure biofeedback and transversus abdominis function in individuals with stabilization classification low back pain. J Orthop Sports Phys Ther. 2013 Mar;43(3):184-93. Epub 2012 Nov 16. [CrossRef] [PubMed]
- McGill SM, Karpowicz A, Fenwick CM, Brown SH. Exercises for the torso performed in a standing posture: spine and hip motion and motor patterns and spine load. J Strength Cond Res. 2009 Mar;23(2):455-64. [CrossRef] [PubMed]
- Voight ML, Hoogenboom BJ, Cook G. The chop and lift reconsidered: integrating neuromuscular principles into orthopedic and sports rehabilitation. N Am J Sports Phys Ther. 2008 Aug;3(3):151-9. [PubMed] [PubMed Central]
- Tarnanen S, Neva MH, Dekker J, Häkkinen K, Vihtonen K, Pekkanen L, Häkkinen A. Randomized controlled trial of postoperative exercise rehabilitation program after lumbar spine fusion: study protocol. BMC Musculoskelet Disord. 2012 Jul 20;13:123. [CrossRef] [PubMed] [PubMed Central]
- Epstein NE. Review of Risks and Complications of Extreme Lateral Interbody Fusion (XLIF). Surg Neurol Int. 2019 Dec 6;10:237. [CrossRef] [PubMed] [PubMed Central]
- Li JX, Phan K, Mobbs R. Oblique Lumbar Interbody Fusion: Technical Aspects, Operative Outcomes, and Complications. World Neurosurg. 2017 Feb;98:113-123. Epub 2016 Oct 21. [CrossRef] [PubMed]
- Yagi M, Fujita N, Hasegawa T, Inoue G, Kotani Y, Ohtori S, Orita S, Oshima Y, Sakai D, Sakai T, Taneichi H, Togawa D, Nakanishi K, Nakashima H, Yoshii T, Nakamura M, Iwasaki M, Watanabe M, Haro H, Kanemura T, Hosogane N; New Technology Assessment Committee of The Japanese Society for Spine Surgery and Related Research. Nationwide Survey of the Surgical Complications Associated with Lateral Lumbar Interbody Fusion in 2015-2020. Spine Surg Relat Res. 2022 Dec 12;7(3):249-256. [CrossRef] [PubMed] [PubMed Central]
- Choi MK, Kim SB, Park CK, Malla HP, Kim SM. Cross-Sectional Area of the Lumbar Spine Trunk Muscle and Posterior Lumbar Interbody Fusion Rate: A Retrospective Study. Clin Spine Surg. 2017 Jul;30(6):E798-E803. [CrossRef] [PubMed]
- Santaguida PL, McGill SM. The psoas major muscle: a three-dimensional geometric study. J Biomech. 1995 Mar;28(3):339-45. [CrossRef] [PubMed]
- Blondel B, Schwab F, Ungar B, Smith J, Bridwell K, Glassman S, Shaffrey C, Farcy JP, Lafage V. Impact of magnitude and percentage of global sagittal plane correction on health-related quality of life at 2-years follow-up. Neurosurgery. 2012 Aug;71(2):341-8; discussion 348. [CrossRef] [PubMed]
- Phan K, Nazareth A, Hussain AK, Dmytriw AA, Nambiar M, Nguyen D, Kerferd J, Phan S, Sutterlin C 3rd, Cho SK, Mobbs RJ. Relationship between sagittal balance and adjacent segment disease in surgical treatment of degenerative lumbar spine disease: meta-analysis and implications for choice of fusion technique. Eur Spine J. 2018 Aug;27(8):1981-1991. Epub 2018 May 28. Erratum in: Eur Spine J. 2021 Dec;30(12):3774. [CrossRef] [PubMed]
- Li CY, Chang CL, Tai TW. Incidence and risk factors for hip fracture in elderly patients undergoing lumbar spine surgery: a nationwide database study with 11-year follow-up. Osteoporos Int. 2018 Dec;29(12):2717-2723. Epub 2018 Oct 15. [CrossRef] [PubMed]
- Yagi M, Ohne H, Kaneko S, Machida M, Yato Y, Asazuma T. Does corrective spine surgery improve the standing balance in patients with adult spinal deformity? Spine J. 2018 Jan;18(1):36-43. Epub 2017 May 23. [CrossRef] [PubMed]
- Sakaguchi, T.; Tanaka, M.; Suthar, H.; Fujiwara, Y.; Uotani, K.; Arataki, S.; Yamauchi, T.; Sugyo, A.; Takamatsu, K.; Yasuda, Y.; et al. Chronological Evaluation of Gait Ability and Posture Balance after Adult Spinal Deformity Surgery. Appl. Sci. 2022, 12, 4285. [CrossRef]
- Sakaguchi T, Tanaka M, Sake N, Latka K, Fujiwara Y, Arataki S, Yamauchi T, Takamatsu K, Yasuda Y, Nakagawa M, Takahashi N, Kishimoto T. The Most Significant Factor Affecting Gait and Postural Balance in Patients' Activities of Daily Living Following Corrective Surgery for Deformity of the Adult Spine. Medicina (Kaunas). 2022 Aug 18;58(8):1118. [CrossRef] [PubMed] [PubMed Central]
- Halvarsson A, Dohrn IM, Ståhle A. Taking balance training for older adults one step further: the rationale for and a description of a proven balance training programme. Clin Rehabil. 2015 May;29(5):417-25. Epub 2014 Sep 8. [CrossRef] [PubMed] [PubMed Central]
- Agmon M, Belza B, Nguyen HQ, Logsdon RG, Kelly VE. A systematic review of interventions conducted in clinical or community settings to improve dual-task postural control in older adults. Clin Interv Aging. 2014 Mar 25;9:477-92. [CrossRef] [PubMed] [PubMed Central]
- Kimura H, Fujibayashi S, Otsuki B, Takahashi Y, Nakayama T, Matsuda S. Effects of Lumbar Stiffness After Lumbar Fusion Surgery on Activities of Daily Living. Spine (Phila Pa 1976). 2016 Apr;41(8):719-27. [CrossRef] [PubMed]
- Togawa D, Hasegawa T, Yamato Y, Yoshida G, Kobayashi S, Yasuda T, Oe S, Banno T, Arima H, Mihara Y, Ushirozako H, Matsuyama Y. Postoperative Disability After Long Corrective Fusion to the Pelvis in Elderly Patients With Spinal Deformity. Spine (Phila Pa 1976). 2018 Jul 15;43(14):E804-E812. [CrossRef] [PubMed]
- Rohlmann A, Pohl D, Bender A, Graichen F, Dymke J, Schmidt H, Bergmann G. Activities of everyday life with high spinal loads. PLoS One. 2014 May 27;9(5):e98510. [CrossRef] [PubMed] [PubMed Central]
- Rohlmann A, Schwachmeyer V, Graichen F, Bergmann G. Spinal loads during post-operative physiotherapeutic exercises. PLoS One. 2014 Jul 7;9(7):e102005. [CrossRef] [PubMed] [PubMed Central]


| Intervention | Definition | Example |
| Patient education and self-management [9] | Teaching patient’s skills that they can use to manage their health condition | How to deal with pain The importance of physical activity in pain reduction Restrictions and working posture postoperatively (ergonomics) Coping with pain flare-ups How to return to work and cope with physical, social, and other barriers |
| Early Exercise [25] | A subcategory of physical activity that is planned, structured, repetitive, and purposeful; can be supervised (eg, by a healthcare professional) or unsupervised | Stretching, Muscle strengthening Endurance exercises Neuromuscular closed chain exercises Range of motion exercise |
| Manual therapies [26,27] | Myofascial release: Technique that applies low-impact, prolonged stretching to the fascial complex to restore optimal length of fascial tissue, decrease pain, and improve functionality. Neural mobilization: A technique that stretches damaged nerves and improves their glide and extensibility. Manipulation: techniques incorporating a high-velocity low-amplitude impulse or thrust applied at or near the end of a joint’s passive range of motion Mobilization: techniques incorporating a low-velocity and small or large amplitude oscillatory movement, within a joint’s passive range of motion |
Myofascial release Neural mobilization Massage Lumbar manipulation, mobilization |
| Assistive technologies | Any item, piece of equipment or product system, used to increase, maintain, or improve the functional capabilities of people with disabilities | Walking aids Socks aids Pants aids Shoehorn Reacher |
| Ⅰ. Biomechanical constraints | Ⅱ. Stability limits | Ⅲ. Anticipatory Postural Adjustments | Ⅳ. Postural Responses | Ⅴ. Sensory orientation | Ⅵ. Stability in gait |
|---|---|---|---|---|---|
| 1. Base of support | 6. Sitting verticality (left and right) and lateral lean | 9. Sit to stand | 14.In-place response, forward | 19. Sensory integration for balance, Stance on firm surface, | 21. Gait level surface |
| 2. CoM alignment | 7. Functional reach forward | 10.Rise to toes | 15. In-place response, backward | 20. Incline, EC | 22. Change in gait speed |
| 3. Ankle strength and ROM | 8. Functional reach lateral | 11. Stand on one leg | 16. Compensatory stepping correction, forward | 23. Walk with head turns, horizontal | |
| 4. Hip/trunk lateral strength | 12. Alternate stair touching | 17. Compensatory stepping correction, backward | 24. Walk with pivot turns | ||
| 5. Sit on floor and stand up | 13. Standing arm raise | 18. Compensatory stepping correction, lateral | 25. Step over obstacles | ||
| 26. Timed “Get Up & Go” Test | |||||
| 27. Timed “Get Up & Go” Test with dual task |
| Anticipatory Postural Adjustments | Postural Responses | Sensory Orientation | Dynamic Gait |
|---|---|---|---|
| 1. Sit to stand | 4. Compensatory stepping correction, forward | 7. Stance on firm surface, EO | 11. Change in gait speed |
| 2.Rise to toes | 5. Compensatory stepping correction, backward | 9. Stance on foam, EC | 12. Walk with head turns, horizontal |
| 3. Stand on one leg (left and right) | 6. Compensatory stepping correction, lateral (left and right) | 10. Incline, EC | 13. Walk with pivot turns |
| 12. Step over obstacles | |||
| 14. Cognitive Get up and Go |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





