1. Introduction
The issues of diagnosis and treatment of
Helicobacter pylori (H. pylori) infection have attracted the attention of the scientific community worldwide primarily due to its high prevalence [
1,
2,
3].
H. pylori infection in all cases leads to chronic gastritis and is the main etiological factor of gastric adenocarcinoma, including proximal gastric cancer [
4,
5,
6,
7].
Detecting and eradicating
H. pylori is a key factor in the primary prevention of gastric cancer [
8]. The efficacy of eradication regimens has decreased due to the rising resistance of
H. pylori to antibiotics, particularly clarithromycin and levofloxacin [
9].
According to the «European Registry on
Helicobacter pylori management» (Hp-EuReg), the effectiveness of classic triple therapy in Russia is only 80%, with a prescription rate of 56% [
10]. This is largely attributed to the high level of
H. pylori's resistance to clarithromycin. According to Hp-EuReg, the resistance of
H. pylori to clarithromycin in Russia is 24%, to levofloxacin – 27%, to metronidazole – 29% [
11]. A recently published meta-analysis demonstrated a decrease in the global prevalence of
H. pylori from 58% to 43% between 1980 and 2022 [
12]. In Russia in the period from 2017 to 2019 the prevalence of
H. pylori according to the 13C-urease breath test was about 40% [
13].
The increase in
H. pylori resistance to the main antibiotics used in eradication regimens has led to changes in the principles of selection of therapy. The goal of eradication therapy is to reliably cure
H. pylori infection in the majority (≥ 90%) of patients, which requires the use of antibacterial agents to which the infection is susceptible, considering regional (local) data. The strategy for selecting eradication therapy based on local data has been developed in a new consensus document [
14]. Physicians obtain information about
H. pylori resistance to antimicrobial agents through several methods. The first method involves culturing with subsequent sensitivity testing to antibiotics or molecular testing. The second method involves assessing the prevalence of resistance in other microorganisms in the community, such as respiratory pathogens to clarithromycin. The third method, accessible to all, involves conducting and organizing data from control tests after eradication and selecting the most effective empirical therapy regimens in the given population. Failure of treatment with an optimized modern regimen may clearly indicate the presence of resistance and that such therapy should no longer be recommended or used if local sensitivity is not confirmed by culture or molecular testing.
In regions with clarithromycin resistance levels of <15%, triple therapy or quadruple therapy with bismuth is still recommended as the first-line treatment. In areas with high clarithromycin resistance (>15%), bismuth quadruple therapy or non-bismuth quadruple therapy is recommended. Thus, in Maastricht VI/Florence, as in the previous consensus, emphasis is placed on the importance of local resistance with the restriction of triple therapy choices in regions with low clarithromycin resistance. A 14-day treatment duration is maintained, and in case of failure of first-line therapy, the following therapy options are proposed [
14].
When selecting triple therapy, clinicians should prefer high dose of proton pump inhibitors (PPIs). In the presented document, for the first time, a conclusion is formulated regarding the effectiveness of a new class of antisecretory agents - potassium channel blockers (P-CABs). It is noted that potassium channel blockers in combination therapy surpass traditional PPIs or are not inferior to them in first and second-line triple therapy and have an advantage in patients with antibiotic-resistant infections [
14].
Perhaps the presence of well-known antibacterial agents that are familiar to practicing specialists should be considered the most important. Rational antibacterial therapy and a focus on determining the current sensitivity of
H. pylori to antimicrobial agents are the priorities for effective eradication therapy. This allows, firstly, to avoid prescribing clearly ineffective antimicrobial drugs. Secondly, it contributes to restraining the growth of
H. pylori antibiotic resistance. Thirdly, it reduces the overall burden of antimicrobial drugs on the population [
15,
16].
The Taipen Consensus (2020) suggests considering the profile of
H. pylori antibiotic resistance, the efficacy of antibiotics, side effects, and therapy cost when choosing optimal treatment regimens for the population [
17]. Due to the increasing antibiotic resistance of
H. pylori, the Maastricht VI/Florence consensus recommends conducting sensitivity tests (molecular or bacteriological) in a planned manner, even before prescribing first-line therapy, to ensure rational antibiotic use [
14].
International guidelines highlight the relevance of developing and implementing molecular diagnostic methods for H. pylori infection and assessing its susceptibility to antibiotics, primarily clarithromycin and levofloxacin. Molecular methods, such as real-time PCR, next-generation sequencing (NGS), and digital PCR, allow for detecting mutations in genes associated with resistance to these antibiotics. Additionally, the development of technologies for detecting genes associated with resistance to metronidazole, tetracycline, and rifaximin is a promising area of research.
For molecular testing, e.g. using PCR, biopsies of the gastric mucosa are suggested to be used, including those extracted from urease tests (rapid urease test). This technology enables the assessment of antibiotic resistance in previously untreated patients and after unsuccessful eradication, forming the basis for individualized therapy selection. Moreover, the availability of resistance detection technologies allows for evaluating the prevalence of resistant strains in the region. This information is crucial for forming recommendations for knowledge-based therapy selection.
The issue of using stool samples for non-invasive molecular genetic testing of
H. pylori antibiotic resistance remains open and requires further research. Contradictory data exist in the scientific literature regarding the sensitivity of molecular tests for detecting
H. pylori and its antibiotic resistance when using stool samples [
18].
According to literature data, clarithromycin resistance is mainly caused by three-point mutations in the
23S rRNA gene: A2142G, A2142C, and A2143G, encoding peptidyl transferase in the V domain of the gene, which is the main target of macrolides. Point mutations in this region disrupt the binding of macrolides to bacterial cell ribosomes, leading to resistance formation [
18,
19,
20,
21,
22,
23,
24].
23S rRNA is found in the 50S subunit of prokaryotic ribosomes and is characterized by gene redundancy. The gene copy number of
23S rRNA can vary from 1 to 15 in different prokaryotes.
H. pylori has two copies of the
23S rRNA gene, and if a mutation is present in at least one of these copies, the bacterium is considered resistant to clarithromycin [
25].
Resistance to fluoroquinolones is caused by mutations in the
gyrA gene, which encodes the A subunit of bacterial DNA gyrase, mainly at codons 87, 88, and 91 of the
gyrA gene [
18,
19,
20,
21,
22,
23,
24]. In different regions, the frequency and nature of mutations that confer
H. pylori resistance can differ. In our recent literature review, we presented data on the molecular resistance characteristics of
H. pylori in various populations [
26].
All existing recommendations today emphasize the preference for personalized selection of antibiotic therapy based on the pre-treatment determination of H. pylori's antibiotic resistance. This determination can be based on a phenotypic method that has high accuracy but is labor-intensive, expensive, and requires specialized technical equipment. To assess resistance, it is necessary to first culture H. pylori from a gastric mucosa biopsy and then determine antibiotic sensitivity. This approach is difficult to implement in routine diagnostic laboratory practices. From an economic perspective, a PCR test for H. pylori antibiotic sensitivity is promising. However, the development of PCR diagnostic test systems for H. pylori antibiotic resistance should be based on population data about the regional characteristics of bacterial molecular resistance. Analyzing the genetic determinants responsible for clarithromycin and levofloxacin resistance in H. pylori in the Russian Federation is a necessary step for creating a valid diagnostic test system.
2. Materials and Methods
Based on the analysis of literature data regarding the genetic determinants of H. pylori antibiotic resistance, a Sanger sequencing test system for regions of the genes 23S rRNA and gyrA, containing the resistance targets to clarithromycin and levofloxacin, respectively, was developed at the A.S. Loginov Moscow Clinical Scientific Center. The study consisted of two stages. In the first stage of the study, the developed test system was validated using samples of pure cultures with known phenotypic resistance to clarithromycin and levofloxacin. The results were compared, and the sensitivity and specificity of the method were determined. In the next stage, samples of biopsies from H. pylori-positive patients were sequenced to search for mutations in the 23S rRNA and gyrA genes.
Phenotypic determination of
H. pylori strain antibiotic resistance was carried out at the Smolensk State Medical University's Research Institute of Antimicrobial Chemotherapy using the serial dilution method in Mueller-Hinton cation-adjusted agar (OXOID, UK) with the addition of sheep blood (final concentration 5%) (E&O Laboratories Ltd., Scotland) in accordance with the recommendations of the Clinical and Laboratory Standards Institute (CLSI). Criteria for assessing
H. pylori sensitivity to antimicrobial drugs, as presented in
Table 4, were used.
1These criteria are not clinical but represent epidemiological threshold values that distinguish strains with natural sensitivity from strains with reduced sensitivity.
Subsequent molecular genetic determination of resistance was performed at the A.S. Loginov Moscow Clinical Scientific Center using the Sanger sequencing method. The study was conducted blindly: after allele variants in antibiotic resistance genes were identified, the data on phenotypic resistance were revealed, and a comparative analysis of molecular genetic data with phenotypic data was conducted [
27].
To identify the genetic characteristics of H. pylori antibiotic resistance, samples of gastric mucosa were analyzed, obtained during esophagogastroduodenoscopy (EGD) in H. pylori-positive individuals in 2022-2023 as part of the "Epidemiological study of H. pylori infection prevalence in Moscow" grant funded by Moscow Center for Innovative Technologies in Healthcare of the Moscow Healthcare Department, grant No. 0903-1/22, March 21st, Prior to EGD, the patients underwent a C13-urea breath test.
The ages of the participants ranged from 18 to 80 years. All patients provided informed consent for the processing of personal data. The work was approved by the local ethics committee (approved by the Ethics Committee in A.S. Loginov Moscow Clinical Scientific Center, protocol No. 4/2022, April 21st, 2022).
DNA extraction was performed using the commercial "Probe NK" kit (DNA-Technology, Russia). Amplification was carried out using specific primers for the regions of the 23S rRNA and gyrA genes on a T100 thermocycler (Bio-Rad, USA) in a reaction mixture of 50 µL, including: 67 mM Tris-HCl (pH=8.8), 1.5-2.5 mM MgCl2, 4 ng genomic DNA, 5 pM of each primer, 10 mM of dATP, dGTP, dCTP, dTTP, and 5 units of active Taq polymerase, following this scheme: 1) denaturation at 95 °C for 5 minutes; 2) denaturation at 95 °C for 30 seconds; primer annealing at 60-66 °C for 30 seconds; elongation at 72 °C for 15 seconds; 3) final elongation at 72 °C for 7 minutes. Qualitative analysis of PCR product accumulation was performed by electrophoresis on a 2% agarose gel. Subsequent purification of the PCR product was done using columns (Eurogene, Russia). Sequencing reactions were performed with forward and reverse primers using the BigDye XTerminator v3.1 Cycle Sequencing Kit (Thermo Fisher Scientific, USA) according to the manufacturer's protocol. The sequencing products were then purified using the BigDye XTerminator Kit (Thermo Fisher Scientific). Detection of sequencing products was performed using capillary gel electrophoresis on an 8-capillary genetic analyzer 3500 (Genetic Analyzer 8ch, Thermo Fisher Scientific, Hitachi). Electropherograms were analyzed using the Chromas software and Sequencing Analysis Software 7.
3. Results
3.1. Development of a Test Platform
In the first stage of the study, sequencing data were obtained for regions of genes associated with resistance to clarithromycin and levofloxacin –
23S rRNA (2142A>G, 2142A>C, 2143A>G) and
gyrA (codons 87 and 91), respectively, from twenty-five pure cultures of
H. pylori. It was found that eleven out of the twenty-five samples had mutations in the clarithromycin resistance gene, and mutations in the levofloxacin resistance gene were detected in thirteen samples, with six samples exhibiting dual resistance. Genetic variants in the
23S rRNA and
gyrA resistance genes for the 25
H. pylori culture samples are presented in
Table 1.
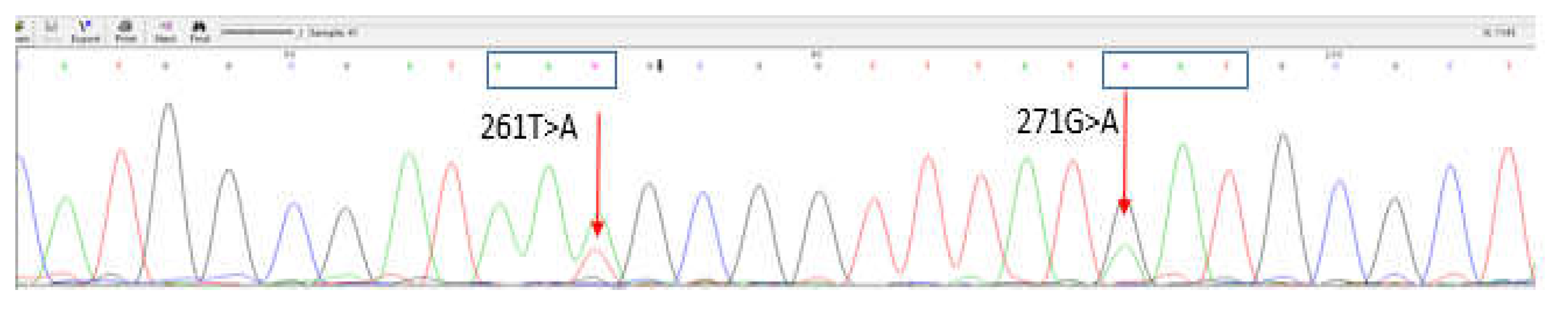
It's worth noting that in some cultures, both wild-type and mutant alleles were detected (
Figure 1). Most commonly, both alleles were found in the
gyrA gene, which is responsible for levofloxacin resistance. The presence of two allelic states may be due to the genetic heterogeneity of
H. pylori.
Comparative analysis of molecular and phenotypic resistance data for
H. pylori showed complete concurrence between molecular-genetic and phenotypic resistance to clarithromycin. All 14 cultures with phenotypic resistance to clarithromycin had mutations in the
23S rRNA gene. The analysis of levofloxacin resistance showed that 13 out of 14 cultures with phenotypic resistance to levofloxacin had mutations in the
gyrA gene. In two cultures that did not exhibit phenotypic resistance to levofloxacin, mutations in the
gyrA gene were found (
Table 2). It is possible that in addition to mutations in codons 87 and 91, levofloxacin resistance may be caused by other
gyrA gene mutations or mutations in other genes, requiring further research on levofloxacin resistance.
The sensitivity and specificity of the Sanger sequencing method for determining clarithromycin resistance were 100%, while for levofloxacin resistance, they were 93% and 92%, respectively. These findings indicate the high diagnostic value of the Sanger sequencing method, allowing the determination of
H. pylori resistance to clarithromycin and levofloxacin [
27].
3.2. Testing of Patient Samples
Sequencing results using the Sanger method for 112 biopsies from H. pylori-positive patients allowed us to establish the spectrum of mutations reflecting resistance to clarithromycin and levofloxacin. Mutations in the 23S rRNA clarithromycin resistance gene were detected in 27 (24%) samples, and mutations in the levofloxacin resistance gene gyrA in 26 (23%) samples. At the same time, double resistance was detected in 16 (14%) samples, 59 (52%) of the studied samples did not have the corresponding mutations in the resistance genes to clarithromycin and levofloxacin.
3.2.1. Molecular Resistance to Clarithromycin
The frequency and spectrum of identified mutations in the 23S rRNA gene in this study are presented in Table The most prevalent nucleotide substitution is 2143G at 18%, followed by 2142G mutation at 5%, and 2142C nucleotide variant at 0.9%. The investigation of the nature and spectrum of allele variants of the 23S rRNA gene in Russia should continue. However, it is already evident that the most characteristic mutation is the nucleotide substitution A2143G.
3.2.2. Molecular Resistance to Levofloxacin
The most frequently occurring nucleotide variants of the
gyrA gene were: 261A at codon 87 and 271A at codon The frequencies and spectrum of
gyrA gene mutations characteristic for Moscow are presented in Table As shown in the
Table 3, molecular resistance to levofloxacin is characterized by the presence of mutations in both codons 87 and 91, with equal frequencies (50% each).
Figures, Tables, and Schemes
4. Discussion
H. pylori always causes gastritis.
H. pylori is one of the main etiopathogenetic factors in the development of peptic ulcer disease, primary etiological factor for gastric adenocarcinoma and is the main risk factor of mucosa-associated lymphoid tissue lymphoma [
14].
Eradication therapy of H. pylori infection eliminates the active inflammatory response in chronic active non-atrophic gastritis, leads to a reduced risk of erosive-ulcerative lesions in the gastric and duodenal mucosa, serves as a preventive measure against the development and progression of precancerous changes in the gastric mucosa (atrophic gastritis, intestinal metaplasia), and therefore acts as a primary prevention of stomach cancer. The main reason for the decreasing effectiveness of eradication therapy regimens is the formation and increasing resistance of H. pylori to antibiotics. This phenomenon is a consequence of the use of ineffective eradication therapy regimens and the widespread use of macrolides and fluoroquinolones for various indications, leading to the development of corresponding mutations in H. pylori genes. The latest international consensus, Maastricht VI/Florence, recommends individualized prescription of eradication regimens, taking antibiotic resistance into account, as well as empirical therapy considering regional variations in resistance and therapeutic efficacy. These recommendations allow for the implementation and increased accessibility of methods for determining H. pylori antibiotic resistance, both phenotypic and molecular-genetic.
When it comes to the effectiveness of H. pylori eradication, it is not solely determined by the sensitivity of H. pylori to antibiotics; this is just one of the factors influencing the effectiveness of anti-Helicobacter therapy. Overall, the effectiveness of anti-Helicobacter therapy depends on factors related to the bacterium itself, such as antibiotic resistance, strain virulence, bacterial load, and the ability to form biofilms. It also depends on patient-related factors, including compliance, hypersecretion of gastric acid, and polymorphisms in genes responsible for the metabolism of various drugs used in H. pylori eradication. An important aspect of H. pylori infection and the treatment of other gastric diseases is the treatment strategy. A well-thought-out, comprehensive, and personalized approach tailored to individual patient characteristics will contribute to treatment efficacy. Currently, the pharmacogenetic features of patients are actively being studied, which can improve treatment outcomes by allowing a targeted approach to therapy selection and reducing side effects. Exploring a patient's pharmacogenetic profile can help avoid significant costs associated with expensive drugs when they are ineffective and require prolonged treatment.
The molecular-genetic method for determining
H. pylori's resistance to antibiotics demonstrates high sensitivity and specificity. The sensitivity and specificity of the molecular-genetic method for determining clarithromycin resistance were 100%, and for levofloxacin resistance, they were 93% and 92%, respectively. According to the literature, the sensitivity and specificity of the molecular-genetic method for clarithromycin resistance determination are reported to be 93% and 98%, and for levofloxacin resistance, they are 83% and 94%, respectively [
28].
In biopsies obtained during EGD, in the period 2022-2023, molecular resistance to clarithromycin was detected in 24% of cases, to levofloxacin in 23% of cases, including double resistance in 14% of cases, 59 (52%) of the studied samples did not have the corresponding mutations in the resistance genes to clarithromycin and levofloxacin .
The nature of substitutions that lead to
H. pylori's resistance to clarithromycin, levofloxacin, and other antibiotics varies across different global populations. In our study, the most common mutations reflecting clarithromycin resistance were variants 2143G and 2142G, which is consistent with global data. However, in some regions of the world, different nucleotide variants are encountered. For example, variants 2142G and 2143G are characteristic of Iran, Tunisia, Vietnam, and Russia [
29,
30,
31]. T248C is characteristic of Myanmar, while for Sudan, in addition to 2142G and 2143G, variants T2182C and C2195T are also found [
32,
33].
The most frequent mutations responsible for H. pylori resistance to levofloxacin among Moscow residents were variants 261A and 271A, which accounted for 69% of all identified genetic determinants of levofloxacin resistance in this study. It's worth noting that the spectrum and distribution pattern of allele variants of the gyrA gene slightly differ from global data, where the most common mutations at codon 87 of the gyrA gene are reported to be 259T and 261A. For instance, the 259T mutation of the gyrA gene in H. pylori among Moscow residents was observed very rarely (0.9%), whereas the variant 260T was encountered at the same frequency (0.9%).
For example, in the population of Myanmar, almost all levofloxacin-resistant isolates had an amino acid substitution at position 91 (Asp-91 to Asn or Tyr) and had no substitutions at codon However, levofloxacin-resistant strains in neighboring countries of Southeast Asia, such as Indonesia, Malaysia, and Cambodia, had both mutations [
31]. Many studies have described single or double mutations at positions Asn87 and Asp91 as the most common mutation sites in resistant
H. pylori isolates obtained from the gastric mucosa [
34,
35,
36].
In the United States, common gene
23S rRNA substitutions include variants 2142 and 2143, while typical mutations of the
gyrA are 260T, 261A, 271A, and 271T [
27]. In northern Israel,
23S rRNA gene variants 2142G, C2173T, and G2212A were exclusively detected in phenotypically resistant
H. pylori isolates. At the same time variant 2143G was found in both resistant and susceptible
H. pylori isolates. As for the levofloxacin resistance gene, mutations at codons 87 and 91 were found in
H. pylori isolates in northern Israel at a frequency of 4.2% for both resistant and susceptible isolates, while the
gyrA T239M variant was detected in phenotypically resistant isolates [
37]. The results of conducted studies demonstrate genetic specificity regarding the molecular resistance of
H. pylori to antibiotics.
An important aspect that must be considered in the molecular diagnosis of H. pylori antibiotic resistance is the genetic heterogeneity of bacteria inhabiting the gastric mucosa, when different strains of H. pylori, both sensitive and resistant, coexist in the patient's gastric mucosa. In this regard, it is necessary to examine several fragments of the gastric mucosa from one patient, which will increase the accuracy of the diagnosis of antibiotic resistance.
5. Conclusions
A high level of detection of H. pylori resistance to clarithromycin and levofloxacin in Moscow was demonstrated, comparable to recent studies conducted in Europe. Additionally, specific features of the spectrum and nature of genetic determinants of molecular resistance of H. pylori to these antibiotics were identified.
According to current recommendations, eradication of H. pylori in adults is indicated in all cases, primarily for the primary prevention of gastric cancer. One of the strategies that enhances the effectiveness of therapy in the context of high antibiotic resistance is personalized antibiotic selection based on determining H. pylori resistance before administration. Investigating H. pylori's resistance to antibiotics also provides a rationale for choosing knowledge-based therapy based on monitoring local H. pylori resistance to clarithromycin.
Patents: Patent No. 2806581 dated 01.11.2023.
Author Contributions
Conceptualization, Natalia Bodunova, Irina Voynovan and Dmitry Bordin; Data curation, Natalia Bodunova and Dmitry Bordin; Formal analysis, Vera Polyakova and Dmitry Bordin; Investigation, Larisa Tsapkova, Irina Baratova, Konstantin Rumyantsev, Natalia Dekhnich, Karina Nikolskaya, Margarita Chebotareva, Irina Voynovan, Elena Parfenchikova, Galina Pronina, Ekaterina Chernikova and Dmitry Bordin; Methodology, Larisa Tsapkova, Irina Baratova, Natalia Dekhnich, Elena Parfenchikova, Galina Pronina and Ekaterina Chernikova; Project administration, Natalia Bodunova and Dmitry Bordin; Supervision, Natalia Bodunova and Dmitry Bordin; Validation, Natalia Bodunova, Natalia Dekhnich and Dmitry Bordin; Visualization, Natalia Dekhnich and Dmitry Bordin; Writing – original draft, Larisa Tsapkova, Vera Polyakova, Konstantin Rumyantsev, Margarita Chebotareva and Irina Voynovan; Writing – review & editing, Natalia Bodunova, Natalia Dekhnich, Karina Nikolskaya and Dmitry Bordin.
Funding
research was conducted within the research project “Epidemiological study of H. pylori infection prevalence in Moscow” funded by the autonomous non-profit organization "Moscow Center for Innovative Technologies in Healthcare" of the Moscow Healthcare Department, grant No. 0903-1/22, March 21st, 2022.
Institutional Review Board Statement
study was conducted per the Declaration of Helsinki and approved by the Ethics Committee of Loginov Moscow Clinical Scientific Center, protocol N 4/2022, April 21st, 2022.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data are available upon request to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hooi, J.K.Y.; Lai, W.Y.; Ng, W.K.; Suen, M.M.Y.; Underwood, F.E.; Tanyingoh, D.; Malfertheiner, P.; Graham, D.Y.; Wong, V.W.S.; Wu, J.C.Y. Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology 2019, 8, 420–429. [Google Scholar] [CrossRef] [PubMed]
- Mezmale, L.; Coelho, L.G.; Bordin, D.; Leja, M. Epidemiology of Helicobacter pylori. Helicobacter 2020, 9, 25. [Google Scholar] [CrossRef] [PubMed]
- Mladenova, I. Review – Epidemiology of Helicobacter pylori infection. Microb Health Dis 2023; 5: e913. [CrossRef]
- Sugano K, Tack J, Kuipers EJ, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut 2015;64:1353–67.
- Tran, V.; Saad, T.; Tesfaye, M.; Walelign, S.; Wordofa, M.; Abera, D.; Desta, K.; Tsegaye, A.; Ay, A.; Taye, B. Analysis of risk factors of (H. pylori) and prediction of prevalence: Machine learning approach: Infectious diseases. Gut 2022, 22, 655. [Google Scholar]
- Noto, J.M.; Rose, K.L.; Hachey, A.J.; Delgado, A.G.; Romero-Gallo, J.; Wroblewski, L.E.; Schneider, B.G.; Shah, S.C.; Cover, T.L.; Wilson, K.T.; et al. Carcinogenic strains of Helicobacter pylori selectively dysregulate the stomach proteome In Vivo, which may be associated with the progression of gastric cancer. Mol. Cell Proteom. 2019, 18, 352–371. [Google Scholar] [CrossRef] [PubMed]
- Elbehiry, A.; Marzouk, E.; Aldubaib, M.; Abalkhail, F.; Anagreyyah, S.; Anajirih, N.; Almuzaini, A.M.; Rawway, M.; Alfadhel, A.; Draz, A.; et al. Helicobacter pylori Infection: Current Status and Future Prospects on Diagnostic, Therapeutic and Control Challenges. Antibiotics 2023, 12, 191. [Google Scholar] [CrossRef] [PubMed]
- Huang RJ, Epplein M, Hamashima C, Choi IJ, Lee E, Deapen D, Woo Y, Tran T, Shah SC, Inadomi JM, Greenwald DA, Hwang JH. An Approach to the Primary and Secondary Prevention of Gastric Cancer in the United States. Clin Gastroenterol Hepatol. 2022 Oct;20(10):2218-2228.e2.
- Megraud F, Bruyndonckx R, Coenen S, Wittkop L, Huang TD, Hoebeke M, Bénéjat L, Lehours P, Goossens H, Glupczynski Y; European Helicobacter pylori Antimicrobial Susceptibility Testing Working Group. Helicobacter pylori resistance to antibiotics in Europe in 2018 and its relationship to antibiotic consumption in the community. Gut. 2021 Oct;70(10):1815-1822. [PubMed]
- Nyssen, O.P.; Vaira, D.; Tepes, B.; Kupcinskas, L.; Bordin, D.; Pérez-Aisa, A.; Gasbarrini, A.; Castro-Fernández, M.; Bujanda, L.; Garre, A. Hp-EuReg Investigators. Room for Improvement in the Treatment of Helicobacter pylori Infection: Lessons from the European Registry on H. pylori Management (Hp-EuReg). J. Clin. Gastroenterol. 2022, 2, 98–108. [Google Scholar]
- Bujanda, L.; Nyssen, O.P.; Vaira, D.; Saracino, L.M.; Fiorini, G.; Lerang, F.; Georgopoulos, S.; Tepes, B.; Heluwaert, F.; Antonio Gasbarrini, A. The Hp-EuReg Investigators. Antibiotic Resistance Prevalence and Trends in Patients Infected with Helicobacter pylori in the Period 2013-2020: Results of the European Registry on H. pylori Management (Hp-EuReg). Antibiotics 2021, 9, 1058. [Google Scholar]
- Li, Y.; Choi, H.; Leung, K.; Jiang, F.; Graham, D.Y.; Leung, W.K. Global prevalence of Helicobacter pylori infection between 1980 and 2022: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2023. doi.org/10.1016/ S2468-1253(23)00070-5.
- Bordin D, Morozov S, Plavnik R, Bakulina N, Voynovan I, Skibo I, Isakov V, Bakulin I, Andreev D, Maev I. Helicobacter pylori infection prevalence in ambulatory settings in 2017-2019 in RUSSIA: The data of real-world national multicenter trial. Helicobacter. 2022 Oct;27(5):e12924. [PubMed]
- Malfertheiner P, Megraud F, Rokkas T, Gisbert JP, Liou JM, Schulz C, Gasbarrini A, Hunt RH, Leja M, O'Morain C, Rugge M, Suerbaum S, Tilg H, Sugano K, El-Omar EM; European Helicobacter and Microbiota Study group. Management of Helicobacter pylori infection: the Maastricht VI/Florence consensus report. Gut 2022;71:1724–1762. [CrossRef]
- De Brito, B.B.; Da Silva, F.A.F.; Soares, A.S.; Pereira, V.A.; Santos, M.L.C.; Sampaio, M.M.; Neves, P.H.M.; De Melo, F.F. Pathogenesis and clinical management of Helicobacter pylori gastric infection. World J. Gastroenterol. 2019, 25, 5578–5589. [Google Scholar] [CrossRef] [PubMed]
- Kotilea, K.; Bontems, P.; Touati, E. Epidemiology, diagnosis and risk factors of Helicobacter pylori infection. Adv. Exp. Med. Biol. 2019, 11, 17–33. [Google Scholar]
- Liou J.M., Malfertheiner P., Lee Y.C., et al. Screening and eradication of Helicobacter pylori for gastric cancer
prevention: the Taipei global consensus. Gut. 2020; 69 (12): 2093.
- Ng, H.-Y.; Leung, W.K.; Cheung, K.-S. Antibiotic Resistance, Susceptibility Testing and Stewardship in Helicobacter pylori Infection. Int. J. Mol. Sci. 2023, 24, 11708. [Google Scholar] [CrossRef]
- Puah, S.M.; Goh, K.L.; Ng, H.K.; Chua, K.H. The current state of resistance of Helicobacter pylori to clarithromycin and levofloxacin in Malaysia–Results of a molecular study. PeerJ 2021, 1, 12. [Google Scholar]
- Li, Y.; Lv, T.; He, C.; Wang, H.; Cram, D.S.; Zhou, L.; Zhang, J.; Jiang, W. Evaluation of multiplex ARMS-PCR for detection of Helicobacter pylori mutations conferring resistance to clarithromycin and levofloxacin. Gut Pathog. 2020, 7, 10–12. [Google Scholar] [CrossRef] [PubMed]
- Ziver-Sarp, T.; Yuksel-Mayda, P.; Saribas, S.; Demiryas, S.; Gareayaghi, N.; Ergin, S.; Tasci, I.; Ozbey, D.; Bal, K.; Erzin, Y. Point mutations at gyrA and gyrB genes of levofloxacin resistant Helicobacter pylori strains and dual resistance with clarithromycin. Clin. Lab. 2021, 67, 10. [Google Scholar] [CrossRef] [PubMed]
- Srisuphanunt, M.; Wilairatana, P.; Kooltheat, N.; Duangchan, T.; Katzenmeier, G.; Rose, J.B. Molecular Mechanisms of Antibiotic Resistance and Novel Treatment Strategies for Helicobacter pylori Infections. Trop. Med. Infect. Dis. 2023, 8, 163. [Google Scholar] [CrossRef] [PubMed]
- Ishibashi, F.; Suzuki, S.; Nagai, n.; Mochida, K.; Morishita, T. Optimizing Helicobacter pylori Treatment: An Updated Review of Empirical and Susceptibility Test-Based Treatments. Gut Liver. 2023. [CrossRef] [PubMed]
- Maev, I.V. Helicobacter pylori Infection: Monograph; GEOTAR-Media: Moscow, Russia, 2016; p. 256. [Google Scholar]
- Pei A, Nossa CW, Chokshi P, Blaser MJ, Yang L, et al. (2009) Diversity of 23S rRNA Genes within Individual Prokaryotic Genomes. PLoS ONE 4(5): e5437. [CrossRef]
- Medakina, I.; Tsapkova, L.; Polyakova, V.; Nikolaev, S.; Yanova, T.; Dekhnich, N.; Khatkov, I.; Bordin, D.; Bodunova, N. Helicobacter pylori Antibiotic Resistance: Molecular Basis and Diagnostic Methods. Int. J. Mol. Sci. 2023, 24, 9433. [Google Scholar] [CrossRef] [PubMed]
- Tsapkova, L.; Polyakova, V.; Bodunova, N. and others. The possibilities of a molecular genetic method for detecting resistance to clarithromycin and levofloxacin in Helicobacter pylori. Effective pharmacotherapy. 2022; 18 (42): 16–DOI 10.33978/2307-3586-2022-18-42-16-21.
- Hulten, K.G. , Genta R.M., Kalfus I.N., Zhou Y., Zhang H., Graham D.Y. Comparison of Culture With Antibiogram to Next-Generation Sequencing Using Bacterial Isolates and Formalin-Fixed, Paraffin-Embedded Gastric Biopsies. Gastroenterology. 2021 Nov;161(5):1433-1442.e2.
- Ziver-Sart, T. Point mutations at gyrA and gyrB genes of levofloxacin resistant Helicobacter pylori strains and dual resistance with clarithromycin. Clin. Lab. 2021; 67 (10).
- Alavifard, H.; Mirzaei, N.; Yadegar, A.; Baghaei, K.; Smith, S.M.; Sadeghi, A.; Zali, M.R. Investigation of mutations associated with clarithromycin resistance and Helicobacter pylori virulence genotypes isolated from the Iranian population: A cross-sectional study. Curr. Microbiol. 2021, 78, 244–254. [Google Scholar] [CrossRef] [PubMed]
- Chtourou, L.; Moalla, M.; Mnif, B.; Smaoui, H.; Gdoura, H.; Boudabous, M.; Mnif, L.; Amouri, A.; Hammami, A.; Tahri, N. Prevalence of Helicobacter pylori resistance to clarithromycin in Tunisia. J. Med. Microbiol. 2022, 8, 71. [Google Scholar] [CrossRef] [PubMed]
- Tran, V.H.; Ha, T.M.T.; Le, P.T.Q.; Phan, T.N.; Tran, T.N.H. Characterisation of point mutations in domain V of the 23S rRNA gene of clinical Helicobacter pylori strains and clarithromycin-resistant phenotype in central Vietnam. J. Glob. Antimicrob. Resist. 2019, 3, 87–91. [Google Scholar] [CrossRef]
- Subsomwong, P.; Doohan, D.; Fauzia, K.A.; Akada, J.; Matsumoto, T.; Yee, T.T.; Htet, K.; Waskito, L.A.; Tuan, V.; Uchida, T. Next-Generation Sequencing-Based Study of Helicobacter pylori Isolates from Myanmar and Their Susceptibility to Antibiotics. Microorganisms 2022, 10, 196. [Google Scholar] [CrossRef]
- Zerbetto De Palma, G. , Mendiondo N., Wonaga A., et al. Occurrence of mutations in the antimicrobial target genes related to levofloxacin, clarithromycin, and amoxicillin resistance in Helicobacter pylori isolates from Buenos Aires city. Microb. Drug. Resist. 2016; 23: 351–358.
- Garcia, M. , Raymond J., Garnier M., et al. Distribution of spontaneous gyrA mutations in 97 fluoroquinolone-resistant Helicobacter pylori isolates collected in France. Antimicrob. Agents. Chemother. 2012; 56: 550–551.
- Albasha, A.M.; Elnosh, M.M.; Osman, E.H.; Zeinalabdin, D.M.; Fadl, A.A.M.; Ali, M.A.; Altayb, H.N. Helicobacter pylori 23S rRNA gene A2142G, A2143G, T2182C, and C2195T mutations associated with clarithromycin resistance detected in Sudanese patients. BMC Microbiol. 2021, 2, 21–38. [Google Scholar] [CrossRef] [PubMed]
- Domanovich-Asor, T.; Motro, Y.; Khalfin, B.; Craddock, H.A.; Peretz, A.; Moran-Gilad, J. Genomic Analysis of Antimicrobial Resistance Genotypeto-Phenotype Agreement in Helicobacter pylori. Microorganisms 2021, 9, 2. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).