Background
Synovial sarcomas are rare aggressive soft tissue tumors typically found in the extremities of young adults [
1]. While their occurrence in the head and neck region is uncommon, involvement in the paranasal sinuses is infrequent [
2,
3]. Among the paranasal sinuses, the ethmoid sinus stands out as the rarest site, with only five documented cases reported in the English literature to date [
4,
5,
6,
7]. Notably, these reported cases demonstrate a slight female predominance. In this context, we present an unusual case of synovial sarcoma affecting the ethmoid sinus in a young male. What makes this case particularly noteworthy is its unique presentation, characterized by an extension to the cavernous sinus. This extension introduces a distinct clinical dimension, posing challenges in both diagnosis and management. Through this case presentation, we aim to shed light on the potential pitfalls of diagnosing synovial sarcoma in the ethmoid sinus, emphasizing the rarity of such cases and their atypical clinical trajectories. Furthermore, we will compare our findings with existing literature to contribute valuable insights into the diagnostic challenges and management strategies for this malignancy.
Case Description
In this case, we detail the complex diagnostic journey of a 38-year-old Mediterranean man who presented with a 7-month history of recurrent headaches. His headache was described to be throbbing in nature, occurring twice to three times weekly, and associated with left eye pain, blurriness of vision, and increasing left-sided facial weakness. Over the last couple of months, the patient’s clinical course evolved into a cascade of alarming symptoms, including a substantial 15 kg weight loss and recurrent strokes, characterized by right-sided weakness, dysarthria, and confusion.
Upon head and neck examination, an exophthalmos of the left eye, and a mass occupying the left nasal cavity was noted on anterior rhinoscopy. Neurological examination revealed horizontal nystagmus when looking to the right, absent gag reflex, right-sided extremity weakness with hypertonia, and positive Babinski reflex.
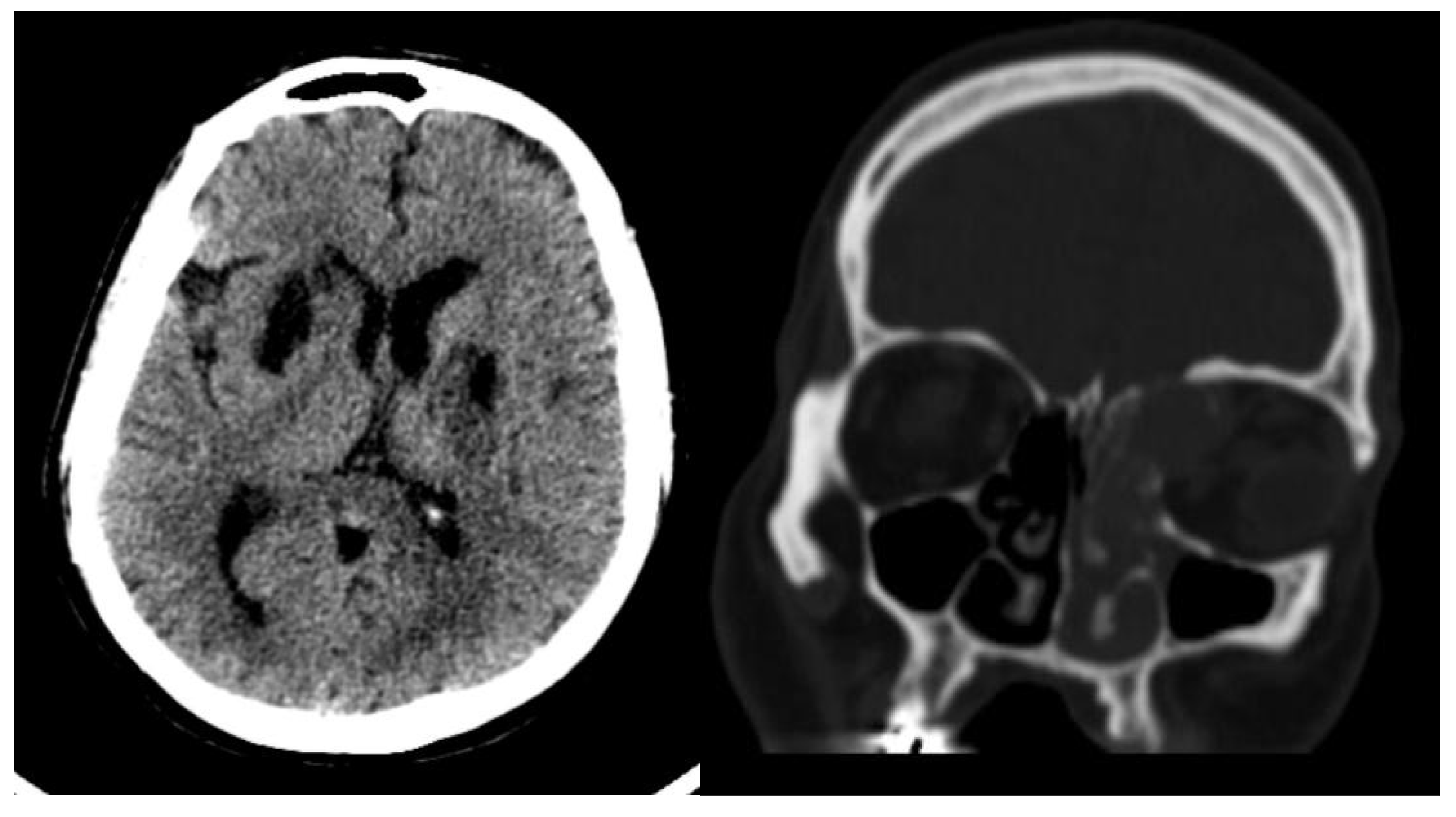
Radiological findings from high-resolution computed tomography (CT) (
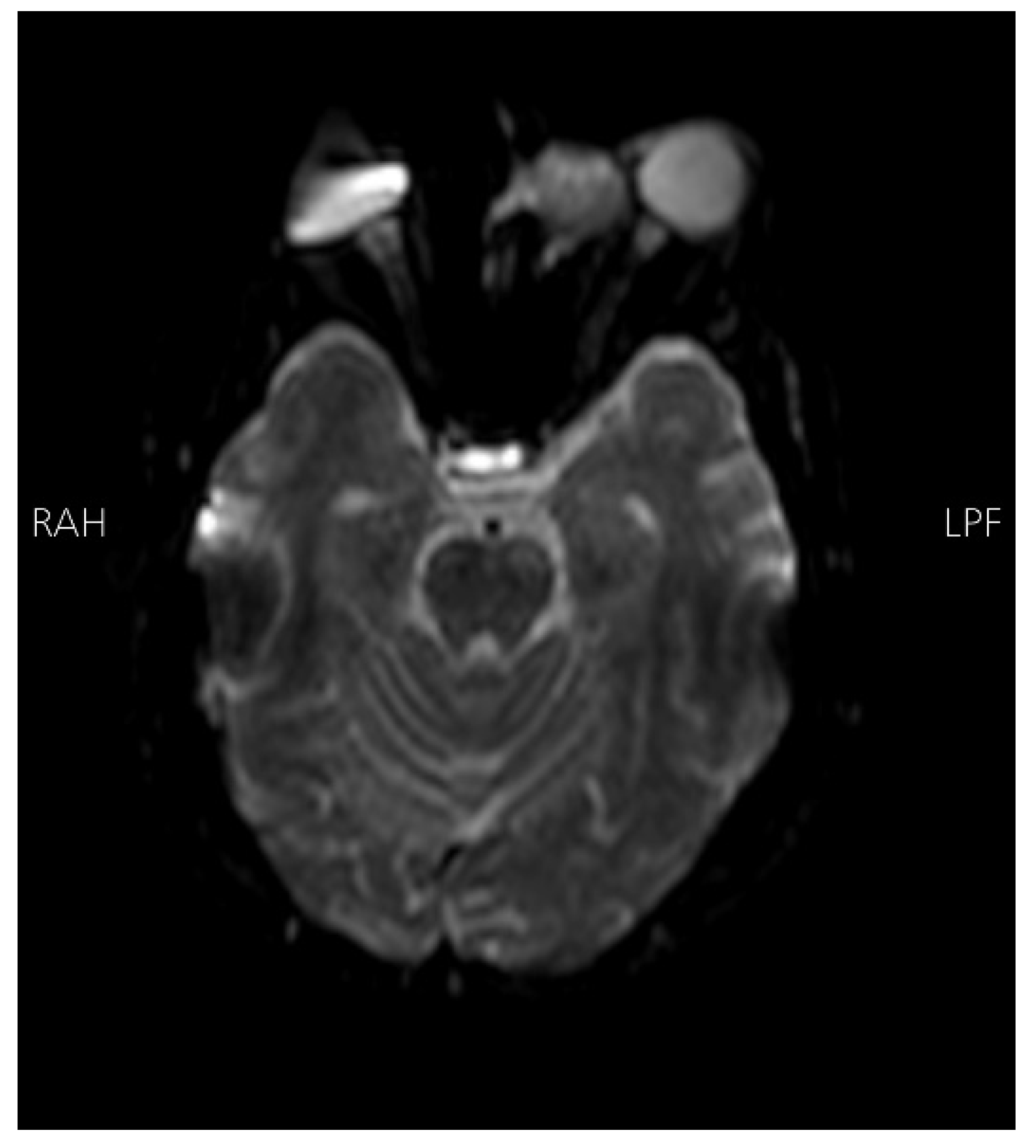
Figure 1) revealed bilateral basal ganglia hypodense areas suggestive of chronic ischemia and a more lateral hypodense area toward the left basal ganglia indicative of subacute ischemia. A coronal cut showed an iso-dense expansible soft tissue lesion with internal foci of calcifications centered in the anterior aspect of the left ethmoid sinus with protrusion to the left orbital conus, pushing the medial rectus muscle laterally with complete obliteration of the left frontal sinus. Brain magnetic resonance imaging with Fluid-attenuated inversion recovery sequence (MRI FLAIR) (
Figure 2) showed an abnormal hyperintense signal in the left cavernous sinus and a left ethmoidal sinus synovial tumor.
Based on these findings, there was a high initial suspicion of vasculitis. However, an exhaustive diagnostic work-up, encompassing Perinuclear Anti-Neutrophil Cytoplasmic Antibody (P-ANCA), Cytoplasmic Anti-Neutrophil Cytoplasmic Antibody (C-ANCA), Complement Component 3 (C3), Complement Component 4 (C4), Erythrocyte Sedimentation Rate (ESR), anti-Glomerular Basement Membrane Antibody (anti-GBM), Extractable Nuclear Antigen (ENA) profile
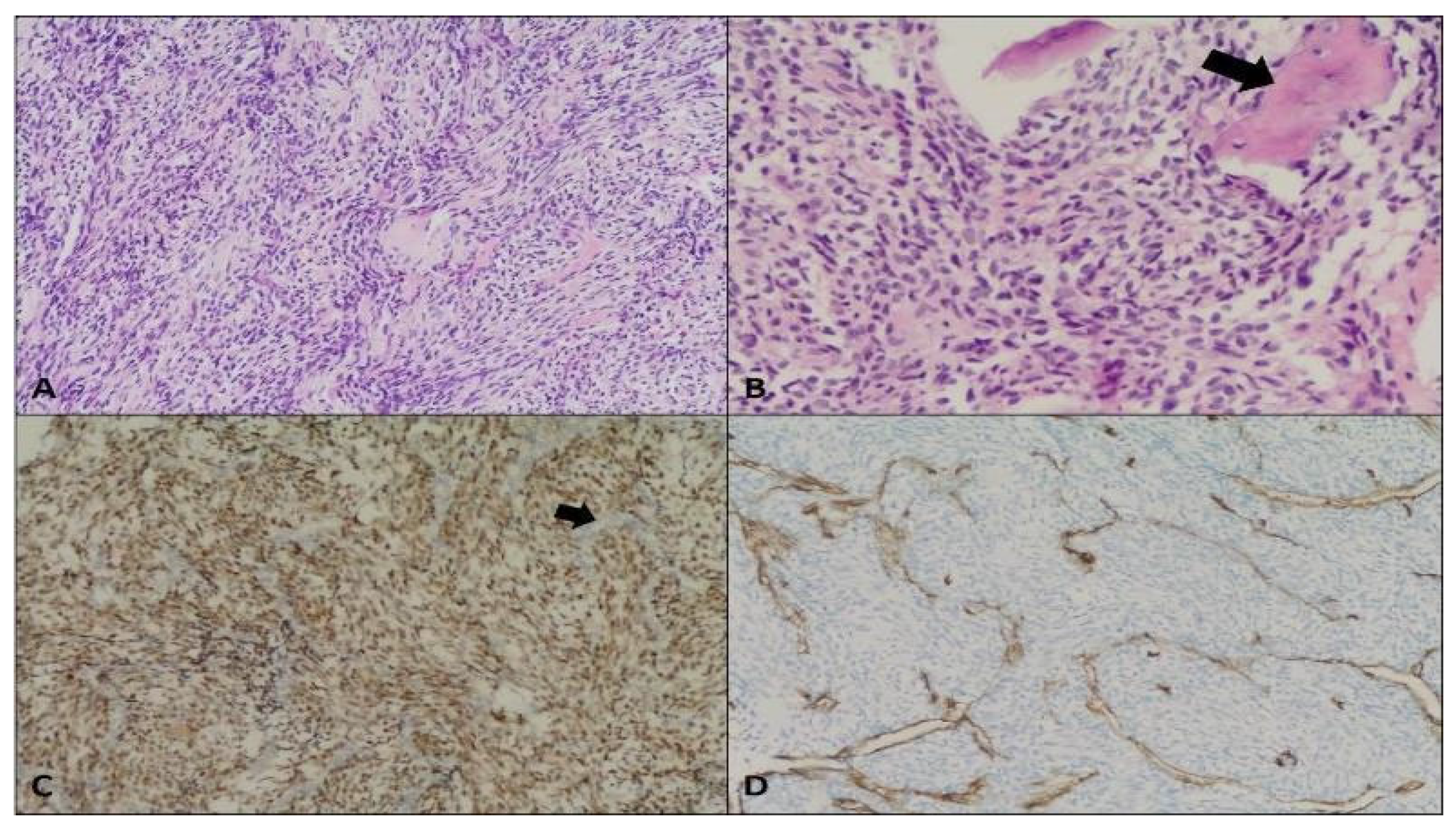
, and anti-cardiolipin antibody tests, yielded inconclusive results. Microscopic examination of an endoscopic biopsy sample (
Figure 3) depicted a monophasic synovial sarcoma composed of monotonous oval to spindle-shaped cells with minimal to moderate cytoplasm. Immunostaining for Transducin-like-Enhancer of split-1 (TLE1), B-cell lymphoma 2 BCL2, and Cluster of Differentiation 99 (CD99) confirmed the diagnosis, while negative results for CD34, signal transducer and activator of transcription 6 (STAT6), S-100, epithelial membrane antigen (EMA), and cytokeratin AE (CKAE) effectively ruled out alternative pathologies.
Owing to our knowledge that surgical resection of the tumor followed by chemo-radiation therapy is the recommended course of action, our patient was referred to a higher-qualified center for comprehensive management. This case underscores the formidable diagnostic challenges presented by synovial sarcomas, emphasizing the indispensable role of a multidisciplinary approach in achieving accurate diagnosis and tailored therapeutic strategies.
Discussion
Sarcomas are malignant tumors of connective tissue origin that usually favor the extremities, especially tendon sheaths and joint capsules, but can also arise in other locations [
8,
9]. Synovial sarcomas predominantly occur in young males in the second and third decades of life [
1]. Involvement of paranasal sinuses is rarely reported, with the ethmoid sinus being an extremely rare site for synovial sarcoma development. As per our knowledge, a sum of five cases of ethmoidal sinus synovial sarcomas have been reported to date [
4,
5,
6,
7].
Like other malignancies arising from the nasal cavity, most cases of ethmoidal sinus sarcomas present with nasal obstruction, pain, and epistaxis [
10]. However, local invasiveness, and spread to the cavernous sinus may widen the clinical presentation. For example, our patient presented with recurrent episodes of headache associated with blurry vision, dysarthria, and facial nerve palsy. The constellation of such symptoms suggested that the patient was suffering from recurrent attacks of stroke. Anatomically, this is explained by the venous drainage of the ethmoidal sinus through the superior ophthalmic vein into the cavernous sinus. From there, the involvement of the internal carotid artery, one of the major contents of the cavernous sinus, becomes inevitable, leading to recurrent strokes.
Radiologically, a CT scan can indicate the malignant nature of the tumor. However, the clinical presentation and radiological features of sarcomas of the ethmoid sinus parallel that of other tumors of the paranasal sinuses. Therefore, a histopathological examination is mandatory to confirm the diagnosis. On histopathology, two different cell types are identified: epithelial and spindle cells. Based on the relative proportion of these two cellular components and degree of differentiation, sarcomas are classified into four different subtypes, including monophasic fibrous (MFSS), monophasic epithelial (MESS), biphasic, and poorly differentiated [
7,
11]. In this case, microscopic sections revealed monotonous oval to spindle-shaped cells with minimal to moderate cytoplasm. Based on these findings, the differential diagnoses considered were squamous cell carcinoma, fibrosarcoma, leiomyosarcoma, malignant peripheral nerve sheath tumor, and monophasic synovial sarcoma. The lack of significant pleomorphism, keratinization, and intercellular bridges, with no connection to the overlying epithelium, ruled out squamous cell carcinoma and malignant melanoma. Further evaluation with immunohistochemistry was conducted to confirm the diagnosis of monophasic synovial sarcoma. The tumor cells were non-reactive for S-100 and neurofilament, which excluded malignant peripheral nerve sheath tumor. Lack of immunoreactivity to SMA excluded the possibility of tumor of myogenic differentiation. Generally, sarcomas could be positive for vimentin, CK, S100, EMA, BCL-2, CD99, and others, with TLE1 being the most sensitive and specific for synovial sarcoma. In our case, immunoreactivity TLE1, BCL2, and CD99 depicted a diagnosis of monophasic synovial sarcoma.
The accepted treatment modality is wide local excision of normal tissue, if feasible, followed by chemo-radiation [
12,
13]. However, it is usually challenging to achieve negative margins with paranasal sinus surgery, especially when done endoscopically. Therefore, in advanced cases, an open surgical approach is preferred. Assurance of complete resection in either surgical approach can be done by taking a frozen section after complete resection of the tumor [
14].
Postoperative radiation therapy can improve local control and increase overall survival rates in sarcomas[
15]. In a retrospective analysis done by Andra et al, 26 patients suffering from head and neck sarcomas received postoperative radiation therapy between the years 2003, and 2012. Patients had a median age of 64 and male predominance. Tumor locations included the skull, the pharynx and larynx, and the paranasal sinuses with a median tumor size of 4.6 cm. All patients, except one, suffered from high-grade lesions, mostly angiosarcomas, malignant fibrous histiocytomas, or synovial sarcomas. 21 patients have undergone excisional surgeries. Of those, 10 patients had tumor-free margins, 6 had microscopically positive margins, and 5 had gross residual disease. All cases were treated with 66 Gy postoperative or definitive radiotherapy, with half of them receiving sequential chemotherapy [
15]. They found 5-year local control of 86%, while overall survival was 82%. In
Table 1, we summarize 6 cases of synovial sarcoma of the ethmoid sinus.
Our patient was referred for advanced management. Generally, postoperative radiotherapy is recommended to improve local control rates, although further studies are warranted in this direction. However, the prognosis remains poor even with extensive management[
16].
Conclusions
Synovial sarcoma is a soft tissue tumor that primarily affects the extremities. It is uncommon in the head and neck region and is extremely rare in the ethmoidal sinus. Sarcomas of the head and neck are aggressive, and most cases present as nasal obstruction and epistaxis, however, with the cavernous sinus being involved it may present with signs of recurrent strokes. The standard course of treatment is surgical resection with postoperative radiation. They do, however, have a high risk of recurrence, thus for the best outcome, intensive care and close follow-up are required. Overall, the prognosis of this rare malignancy remains poor.
References
- Ladenstein R, Treuner L, Koscielniak E, et al.: Synovial Sarcoma of Childhood and Adolescence Report of the German CWS-81 Study. [CrossRef]
- Siegel R, Naishadham D, Jemal A: Cancer statistics, 2012. CA Cancer J Clin. 2012, 62:10–29. [CrossRef]
- Kraus DH, Dubner S, Harrison LB, et al.: Prognostic Factors for Recurrence and Survival in Head and Neck Soft Tissue Sarcomas. [CrossRef]
- Wong HT, Ho CY, Nazarina AR, Prepageran N: Synovial sarcoma of the ethmoidal sinus. J Laryngol Otol. 2014, 128:1022–3. [CrossRef]
- Jain A, Saxena A, Meher R, Khurana N: ScienceDirect Synovial sarcoma of the ethmoid sinus. Eur Ann Otorhinolaryngol Head Neck Dis. 2018, 135:453–5. [CrossRef]
- Dhiman S, Negi S, Moudgil S, Thakur JS, Azad RK: Synovial Sarcoma of Ethmoidal Sinus. 2021, 7:195–8. [CrossRef]
- Kartha SS, Bumpous JM: Synovial Cell Sarcoma: Diagnosis, Treatment, and Outcomes. Laryngoscope. 2002, 112:1979–82. [CrossRef]
- Duran-Moreno J, Kampoli K, Kapetanakis EI, et al.: Pericardial Synovial Sarcoma: Case Report, Literature Review and Pooled Analysis. In Vivo. 2019, 33:1531–8. [CrossRef]
- Nuwal P, Dixit R, Shah N, Samaria A: Primary monophasic synovial sarcoma lung with brain metastasis diagnosed on transthoracic FNAC: Report of a case with literature review. Lung India. 2012, 29:384. [CrossRef]
- Salcedo-Hernández RA, Lino-Silva LS, Luna-Ortiz K: Maxillary Sinus Sarcomas: Epidemiological and Clinicopathological Experience of 25 Years in a National Reference Cancer Center. Indian J Otolaryngol Head Neck Surg. 2014, 66:359–64. [CrossRef]
- Gallia GL, Sciubba DM, Hann CL, Raman SP, Westra WH, Tufaro AP, Olivi A: Synovial sarcoma of the frontal sinus: Case report. J Neurosurg. 2005, 103:1077–80. [CrossRef]
- Nielsen TO, Poulin NM, Ladanyi M: Synovial sarcoma: recent discoveries as a roadmap to new avenues for therapy. Cancer Discov. 2015, 5:124. [CrossRef]
- Colville RJ, Charlton F, Kelly CG, Nicoll JJ, McLean NR: Multidisciplinary management of head and neck sarcomas. Head Neck. 2005, 27:814–24. [CrossRef]
- Owosho AA, Estilo CL, Rosen EB, Yom SHK, Huryn JM, Antonescu CR: A clinicopathologic study on SS18 fusion-positive head and neck synovial sarcomas. Oral Oncol. 2017, 66:46. [CrossRef]
- Andrä C, Rauch J, Li M, et al.: Excellent local control and survival after postoperative or definitive radiation therapy for sarcomas of the head and neck. Radiat Oncol. 2015, 10:. [CrossRef]
- Harb WJ, Luna MA, Patel SR, Ballo MT, Roberts DB, Sturgis EM: Survival in patients with synovial sarcoma of the head and neck: association with tumor location, size, and extension. Head Neck. 2007, 29:731–40. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).