Submitted:
11 April 2024
Posted:
15 April 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
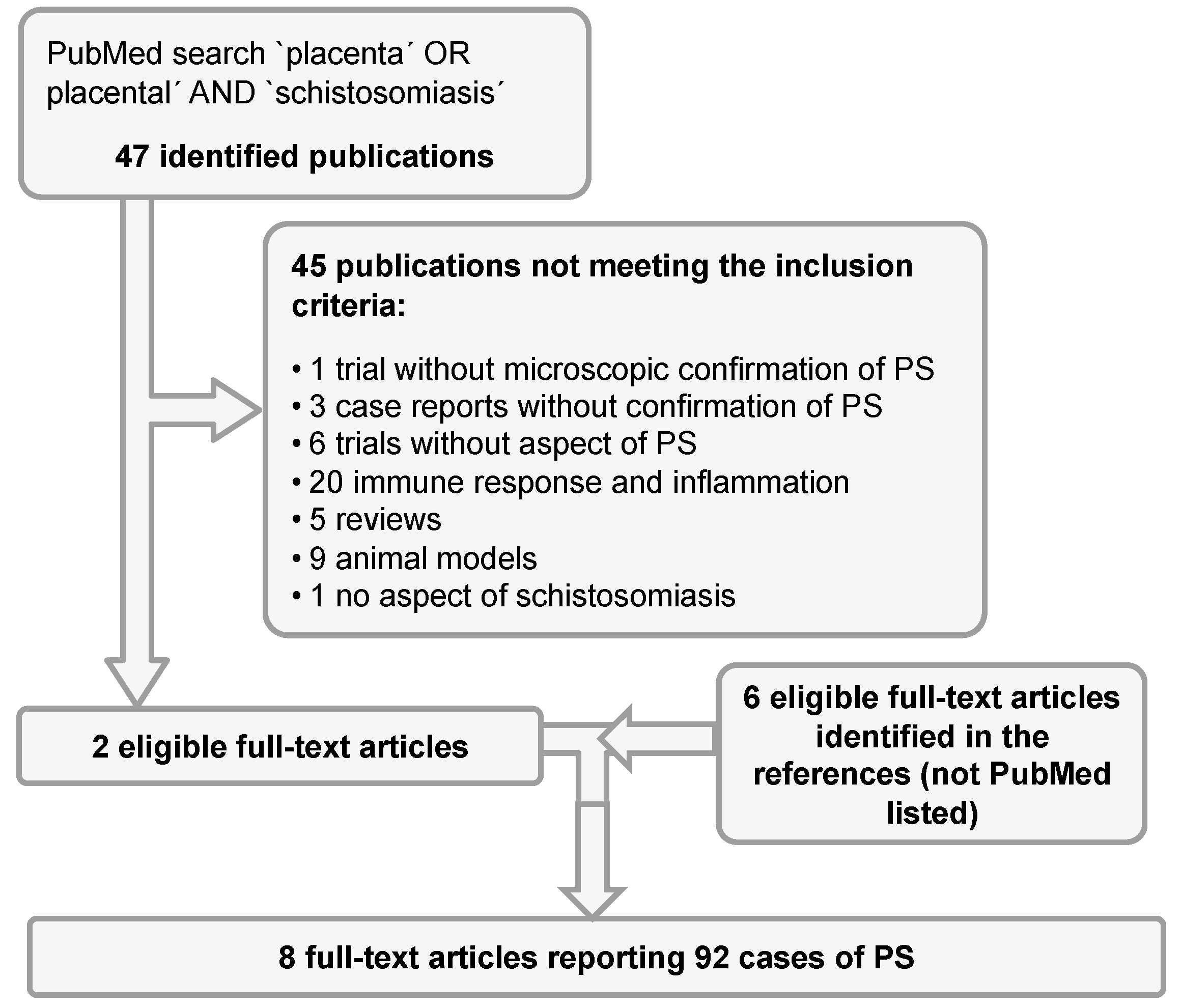
2. Materials and Methods
3. Results
4. Discussion
4.1. Underestimated Prevalence of Placental Schistosomiasis?
4.2. Contribution to Adverse Birth Outcomes (ABO)
4.3. Discussed Pathophysiologic Mechanisms
4.4. Treatment Strategies
5. Conclusion
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Hotez, P.J.; Alvarado, M.; Basáñez, M.G.; Bolliger, I.; Bourne, R.; Boussinesq, M.; Brooker, S.J.; Brown, A.S.; Buckle, G.; Budke, C.M.; u.c. The Global Burden of Disease Study 2010: Interpretation and Implications for the Neglected Tropical Diseases. PLoS Negl. Trop. Dis. 2014, 8, 17. [CrossRef]
- Friedman, J.F.; Olveda, R.M.; Mirochnick, M.H.; Bustinduy, A.L.; Elliott, A.M. Praziquantel for the Treatment of Schistosomiasis during Human Pregnancy. Bull. World Health Organ. 2018, 96, 59–65. [CrossRef]
- World Health Organization Female genital schistosomiasis: A pocket atlas for clinical health-care professionals. Who/Htm/Ntd/2015.4 2015, 2015, 49.
- Bittencourt, A.L.; Gomes Pinto Garcia, A. The Placenta in Hematogenous Infections. Pediatr. Pathol. Mol. Med. 2002, 21, 401–432. [CrossRef]
- Adam, I.; ALhabardi, N.A.; Al-Wutayd, O.; Khamis, A.H. Prevalence of schistosomiasis and its association with anemia among pregnant women: a systematic review and meta-analysis. Parasites and Vectors 2021, 14.
- Freer, J.B.; Bourke, C.D.; Durhuus, G.H.; Kjetland, E.F.; Prendergast, A.J. Schistosomiasis in the first 1000 days. Lancet Infect. Dis. 2018, 18, e193–e203. [CrossRef]
- Friedman, J.F.; Mital, P.; Kanzaria, H.K.; Olds, G.R.; Kurtis, J.D. Schistosomiasis and Pregnancy. Trends Parasitol. 2007, 23, 159–164. [CrossRef]
- Haider, B.A.; Olofin, I.; Wang, M.; Spiegelman, D.; Ezzati, M.; Fawzi, W.W. Anaemia, prenatal iron use, and risk of adverse pregnancy outcomes: Systematic review and meta-analysis. BMJ 2013, 347.
- Sutherland, J.C.; Berry, A.; Hynd, M.; Proctor, N.S.. Placental Bilharziasis. South African J. Obstet. amd Gynaecol. 1965, 76–80. [CrossRef]
- Renaud, R.; Brettes, P.; Castanier, C.; Loubiere, R. Placental Bilharziasis. Int. J. Gynecol. Obstet. 1972, 10, 24–30. [CrossRef]
- Holtfreter, M.C.; Neubauer, H.; Groten, T.; El-Adawy, H.; Pastuschek, J.; Richter, J.; Häussinger, D.; Pletz, M.W.; Schleenvoigt, B.T. Improvement of a tissue maceration technique for the determination of placental involvement in schistosomiasis. PLoS Negl. Trop. Dis. 2017, 11. [CrossRef]
- Prates, M.M.; Tropical, M.; Tropical, M. A bilharziose na Africa oriental portuguesa e sua importancia na etiología dos carcinomas primitivos do fígado dos indígenas. An. Inst. Med. Trop. (Lisb). 1948, 5, 149.
- Bittencourt, A.L.; Mott, K. Placental Schistosomiasis. Gaz. Médica da Bahia 1969, 3, 113–117.
- Viggiano, M.G.; Leite, M.S. Placentite esquistosomótica. J. Bras. Ginecol. 1978, 85, 273–278.
- Bittencourt, A.L.; De Almeida, M.A.C.; Iunes, M.A.F.; Casulari Da Motta, L.D.; Bittencourt, L.; Antonio, M.; Almeida, C.D.E.; Amelia, M.; Iunes, F. Placental Involvement in Schistosomiasis Mansoni - Report of Four Cases. Am. J. Trop. Med. Hyg. 1980, 29, 571–575. [CrossRef]
- Peres, L. Schistosoma mansoni eggs in the placenta: an unusual finding. Rev. Hosp. Säo Paulo Esc. Paul. Med 1994, 5, 788–789.
- Schleenvoigt, B.T.; Gajda, M.; Baier, M.; Groten, T.; Oppel-Heuchel, H.; Grimm, M.O.; Pfister, W.; Richter, J.; Pletz, M.W. Placental Schistosoma haematobium infection in a German returnee from Malawi. Infection 2014, 42, 1061–1064. [CrossRef]
- Fujinami, A.; Nakamura, H. On the prophylaxis of schistosomiasis and some investigations on infection with this disease. Chugi- Iji Shimpo 1911, 753.
- Narabayashi, H. Beiträge zur Frage der kongenitalen Invasion von Schistosoma japonicum. Verhandl. Jap. path. Gesellsch. 1914, 4.
- Augustine, D.L. Development in Prenatal Infestation of Belascaris. J. Parasitol. 1927, 13, 256–259. [CrossRef]
- Rodrigues, M. ari. A. Placental bilharziasis - a preliminary report. In Proceedings of the Abstracts of the 7th International Congress of International Academy of Pathology; Milano, Italy, 1968.
- Franz, R.; Hahn, A.; Hagen, R.M.; Rohde, H.; Eberhardt, K.A.; Ehrhardt, S.; Baum, J.; Claussen, L.; Feldt, T.; Hinz, R.; u.c. Screening for Resistant Bacteria, Antimicrobial Resistance Genes, Sexually Transmitted Infections and Schistosoma spp. in Tissue Samples from Predominantly Vaginally Delivered Placentae in Ivory Coast and Ghana. Pathogens 2023, 12. [CrossRef]
- Siegrist, D.; Siegrist-Obimpeh, P. Schistosoma Haematobium Infection in Pregnancy. Acta Trop. 1992, 50, 317–321. [CrossRef]
- Qunhua, L.; Jiawen, Z.; Bozhao, L.; Zhilan, P.; Huijie, Z.; Shaoying, W.; Deln, M.; Hsu, L.-N. Investigation of association between female genital tract diseases and Schistosomiasis japonica infection. Acta Trop. 2000, 77, 179–183.
- Mombo-Ngoma, G.; Honkpehedji, J.; Basra, A.; Mackanga, J.R.; Zoleko, R.M.; Zinsou, J.; Agobe, J.C.D.; Lell, B.; Matsiegui, P.B.; Gonzales, R.; u.c. Urogenital schistosomiasis during pregnancy is associated with low birth weight delivery: analysis of a prospective cohort of pregnant women and their offspring in Gabon. Int. J. Parasitol. 2017, 47, 69–74. [CrossRef]
- Honkpéhèdji, Y.J.; Adegbite, B.R.; Zinsou, J.F.; Dejon-Agobé, J.C.; Edoa, J.R.; Zoleko Manego, R.; McCall, M.; Mbong Ngwese, M.; Lotola Mougeni, F.; Mombo-Ngoma, G.; u.c. Association of low birth weight and polyparasitic infection during pregnancy in Lambaréné, Gabon. Trop. Med. Int. Heal. 2021, 26, 973–981. [CrossRef]
- Romia, S.A.; Handoussa, A.E.; Youseff, S.A.; el Zayat, M.M. Transplacental Transfer of Schistosomal Antigens and Antibodies. J. Egypt. Soc. Parasitol. 1992, 22, 575–582.
- Hassan, M.M.; Hassounah, O.A.; Hegab, M.; Salah, K.; El-Mahrouky, L.; Galal, N. Transmission of Circulating Schistosomal Antigens from Infected Mothers to Their Newborns. J. Egypt. Soc. Parasitol. 1997, 27, 773–780.
- Attallah, A.M.; Ghanem, G.E.; Ismail, H.; El Waseef, A.M. Placental and oral delivery of Schistosoma mansoni antigen from infected mothers to their newborns and children. Am. J. Trop. Med. Hyg. 2003, 68, 647–651. [CrossRef]
- McDonald, E.A.; Kurtis, J.D.; Acosta, L.; Gundogan, F.; Sharma, S.; Pond-Tor, S.; Wu, H.W.; Friedman, J.F. Schistosome egg antigens elicit a proinflammatory response by trophoblast cells of the human placenta. Infect. Immun. 2013, 81, 704–712. [CrossRef]
- Kurtis, J.D.; Higashi, A.; Wu, H.W.; Gundogan, F.; McDonald, E.A.; Sharma, S.; PondTor, S.; Jarilla, B.; Sagliba, M.J.; Gonzal, A.; u.c. Maternal schistosomiasis japonica is associated with maternal, placental, and fetal inflammation. Infect. Immun. 2011, 79, 1254–1261. [CrossRef]
- McDonald, E.A.; Pond-Tor, S.; Jarilla, B.; Sagliba, M.J.; Gonzal, A.; Amoylen, A.J.; Olveda, R.; Acosta, L.; Gundogan, F.; Ganley-Leal, L.M.; u.c. Schistosomiasis japonica during pregnancy is associated with elevated endotoxin levels in maternal and placental compartments. J. Infect. Dis. 2014, 209, 468–472. [CrossRef]
- Onguru, D.; Liang, Y.M.; Griffith, Q.; Nikolajczyk, B.; Mwinzi, P.; Ganley-Leal, L. Short report: Human schistosomiasis is associated with endotoxemia and toll-like receptor 2- and 4-bearing B cells. Am. J. Trop. Med. Hyg. 2011, 84, 321–324. [CrossRef]
- Hanna, N.; Hanna, I.; Hleb, M.; Wagner, E.; Dougherty, J.; Balkundi, D.; Padbury, J.; Sharma, S. Gestational Age-Dependent Expression of IL-10 and Its Receptor in Human Placental Tissues and Isolated Cytotrophoblasts. J. Immunol. 2000, 164, 5721–5728. [CrossRef]
- Ekerfelt, C.; Lidström, C.; Matthiesen, L.; Berg, G.; Sharma, S.; Ernerudh, J. Spontaneous secretion of interleukin-4, interleukin-10 and interferon-γ by first trimester decidual mononuclear cells. Am. J. Reprod. Immunol. 2002, 47, 159–166. [CrossRef]
- PrabhuDas, M.; Bonney, E.; Caron, K.; Dey, S.; Erlebacher, A.; Fazleabas, A.; Fisher, S.; Golos, T.; Matzuk, M.; McCune, J.M.; u.c. Immune mechanisms at the maternal-fetal interface: Perspectives and challenges. Nat. Immunol. 2015, 16, 328–334.
- Moormann, A.M.; Sullivan, A.D.; Rochford, R.A.; Chensue, S.W.; Bock, P.J.; Nyirenda, T.; Meshnick, S.R. Malaria and pregnancy: Placental cytokine expression and its relationship to intrauterine growth retardation. J. Infect. Dis. 1999, 180, 1987–1993. [CrossRef]
- Abioye, A.I.; McDonald, E.A.; Park, S.; Joshi, A.; Kurtis, J.D.; Wu, H.; Pond-Tor, S.; Sharma, S.; Ernerudh, J.; Baltazar, P.; u.c. Maternal, placental and cord blood cytokines and the risk of adverse birth outcomes among pregnant women infected with schistosoma japonicum in the Philippines. PLoS Negl. Trop. Dis. 2019, 13. [CrossRef]
- 2002; 39. World Health Organization Report of the WHO Informal Consultation on the use of Praziquantel during Pregnancy/Lactation and Albendazole/Mebendazole in Children under 24 months; 2002;
- World Health Organization WHO Guideline on control and elimination of human Schistosomiasis; 2022; ISBN 978 92 4 004160 8.
- Ndibazza, J.; Muhangi, L.; Akishule, D.; Kiggundu, M.; Ameke, C.; Oweka, J.; Kizindo, R.; Duong, T.; Kleinschmidt, I.; Muwanga, M.; u.c. Effects of deworming during pregnancy on maternal and perinatal outcomes in entebbe, Uganda: A randomized controlled Trial. Clin. Infect. Dis. 2010, 50, 531–540. [CrossRef]
- Olveda, R.M.; Acosta, L.P.; Tallo, V.; Baltazar, P.I. A randomized double blind placebo controlled trial assessing the efficacy and safety of praziquantel for the treatment of human schistosomiasis during pregnancy. Lancet Infect. Dis. 2016, 16, 199–208. [CrossRef]
- Honkpehedji, Y.J.; Adegnika, A.A.; Dejon-Agobe, J.C.; Zinsou, J.F.; Mba, R.B.; Gerstenberg, J.; Rakotozandrindrainy, R.; Rakotoarivelo, R.A.; Rasamoelina, T.; Sicuri, E.; u.c. Prospective, observational study to assess the performance of CAA measurement as a diagnostic tool for the detection of Schistosoma haematobium infections in pregnant women and their child in Lambaréné, Gabon: Study protocol of the freeBILy clinical trial. BMC Infect. Dis. 2020, 20. [CrossRef]
- Holtfreter, M.C.; Mischlinger, J.; Davi, S.D.; Schleenvoigt, B.T. Investigation on birth weight outcomes in schistosomiasis and praziquantel research: a correspondence. Eur. J. Med. Res. 2023, 28, 231. [CrossRef]
| Year | Author | Genre | No. of cases | Country of origin | Age | Schistosoma spp. | Adult helminth |
Pregnancy complications |
Applied technique |
|---|---|---|---|---|---|---|---|---|---|
| 1948 | Prates [12] | Case series |
5 | Mozambique | - | S. haematobium | no | NA | Histology |
| 1965 | Sutherland [9] | Case series |
8 | South Africa |
19, NA |
S. haematobium (6) S. mansoni (1) both species (1) |
no | Seizures (1) Preeclampsia (1) | Histology (1), Maceration (7) |
| 1969 | Bittencourt [13] | Case report |
1 | Brazil | 34 | S. mansoni | yes | No | Histology |
| 1971 | Renaud [10] | Clinical study | 72 | Ivory coast |
- | S. haematobium | no | LBW (21) Fetal death (10) Prematurity (21) |
Histology and Maceration |
| 1978 | Viggiano [14] | Case report |
1 | Brazil | 19 | S. mansoni | yes | Fetal death | Histology |
| 1980 | Bittencourt [15] | Case series |
4 (3)Ψ | Brazil | 34, 23, 18, NA | S. mansoni | yes (2) | Fetal death (2) EUG (1) | Histology |
| 1994 | Peres [16] | Case report |
1 | Brazil | 31 | S. mansoni | no | Prematurity, LBW | Histology |
| 2014 | Schleenvoigt [17] | Case report |
1 | Malawi | 28 | S. haematobium | no | no | Histology |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





