1. Introduction
The neonatal period or the first 28 days of life represents the most vulnerable period in terms of survival. Every year, approximately 10% of the women who pass through the corridors of maternity hospitals to give birth, live the experience and emotions next to a new-born cared for in the neonatal intensive care unit. Changes to the newborn’s cardiovascular and respiratory system function or prematurity are unavoidable and sometimes there is a need for assistance. The incidence of resuscitative interventions and emergencies varies between different settings and countries [
1,
2].
NICU (Neonatal Intensive Care Unit) is the unit where vital support is provided for new-borns, they are treated and monitored. It is the place where can be found sophisticated technical resources for life support. The hospitalization rate in this unit increases proportionally with the exposure to different factors or agents. Technological advances in the NICU have improved the survival of neonates admitted in. On the other hand, admission to the NICU interrupts the mother-new-born bond and sometimes natural nutrition. It is a gold standard to understand the trend and the causal relationship between prenatal, general, and individual risk factors, the level of assistance at the birth, and the risk of needing admission to the NICU.
The possibility of explaining and predicting the possibility of a neonatal emergency involving admission to the NICU becomes extremely valuable for the medical unit, from the perspective of optimizing the team and resources, and from the perspective of the mother’s emotional preparation.
Mortality rate during the neonatal period is higher compared to the post-neonatal period because of complications related to preterm birth, intrapartum-related complications and infections such as neonatal sepsis or meningitis. Moreover, almost half of the deaths in children under 5 years of age occur in the neonatal period [
3,
4].
Neonatal emergencies are frequently encountered during birth, immediately postnatally or after discharge of the new-born. Many times, it tests the skills of the clinician, or the team present at the birth. An early diagnosis of respiratory depression, early sepsis or shock improves the survival of the new-born. Studies show that in the absence of risk factors, 7% of term newborns require positive pressure ventilation and/or endotracheal intubation [
5].
The most common neonatal emergency is neonatal asphyxia accounting for 20.9% of neonatal deaths and there is a need of intervention to breathe during transition from intrauterine to extrauterine life. Only 1% of newborns require extensive resuscitative measures [
6]. The purpose of neonatal resuscitation is to establish adequate spontaneous respiration and cardiac, renal functions and to prevent the morbidity and mortality associated with hypoxic-ischaemic tissues injuries.
Among the risk factors correlated with the need for resuscitation at birth, maternal, fetal factors or factors related to the moment of birth were described. Common factors associated with an increased risk of neonatal emergencies are intrauterine growth deficiency, sub 37 weeks of gestation, congenital abnormalities in fetals. Among the maternal factors, we mention age, parity, history of diabetes, hypertension, multiple pregnancies, altered amniotic fluid, detachment from the placenta, premature rupture of membranes [
7]. Intrapartum factors are meconium-stained amniotic fluid, vacuum delivery, significant bleeding, C-section before 39 weeks [
8]. A large part of these factors can be prevented, and nevertheless they are still decisive for the incidence of neonatal emergencies. In addition, the care of these newborns is more expensive [
9].
If in 1990 at the global level the incidence of neonatal deaths was 37 per thousand, in 2020 this incidence was 17 per thousand births [
10]. In Romania, the neonatal mortality was 3.5 per thousand in 2020 [
11].
This study aims to evaluate the significance of individual ante and intrapartum factors in determining the need for resuscitation of the new-born or the need for hospitalization in NICU.
2. Materials and Methods
The study is a retrospective one approved by Commission of Ethics for Scientific Research from the Bihor County Emergency Clinical Hospital from Oradea, Romania and in consent with the Declaration of Helsinki—Recommendations Guiding Medical Practice. Approval number 11 323 was assigned to the present research on 5 of April 2023.
All newborns cared for in the Maternity of Bihor County Emergency Clinical Hospital, a third level maternity between January 2012 and December 2021 were included in the study resulting in a group of 37,875 new-borns. The medical records of neonates admitted to the NICU and mothers were reviewed retrospectively to collect data about NICU admission, and outcomes. We collected data about diagnosis for admission, Apgar score, presence of complications associated with prematurity, infection status, antibiotic administration and maternal risk factors such as age, level of education, premature rupture of membranes, peripartum infections, etc.
Neonatal emergencies are considered new-borns who required resuscitation in the delivery room and were admitted to the NICU requiring intensive care.
The diagnoses were clinically confirmed by the on-call doctor, who also established the presence of the NICU admission criteria.
All these newborns were classified into two groups:
- -
The study group that includes all newborns who required resuscitation at birth and were admitted to the NICU section.
- -
The control group consisted of newborns who did not have the necessary criteria for admission to the NICU, newborns who were cared for in the rooming-in system.
We classified the risk factors most frequently encountered during childbirth. We studied the incidence of neonatal emergencies following the next types of diseases: respiratory, cardiovascular, infectious, gastrointestinal, haematological, and haemorrhagic, neurological, extreme prematurity. We established for the unit in this time frame the main factors that correlate with the need for resuscitation at birth and admission to the NICU.
IBM SPSS software version 26.0 was used for statistical analysis. Descriptive statistics were used to summarize demographic and clinical characteristics of newborns by NICU admission and multivariate logistic regression was used to estimate neonatal and maternal risk factors associated with admission to the NICU. The criterion for significance was fixed at 0.05.
3. Results
During the study period, a number of 37 875 babies were born, this number showing a downward trend, with 20.9% decrease in the number of births in 2021 compared to 2012. Around 90% of the births were on term (
Table 1).
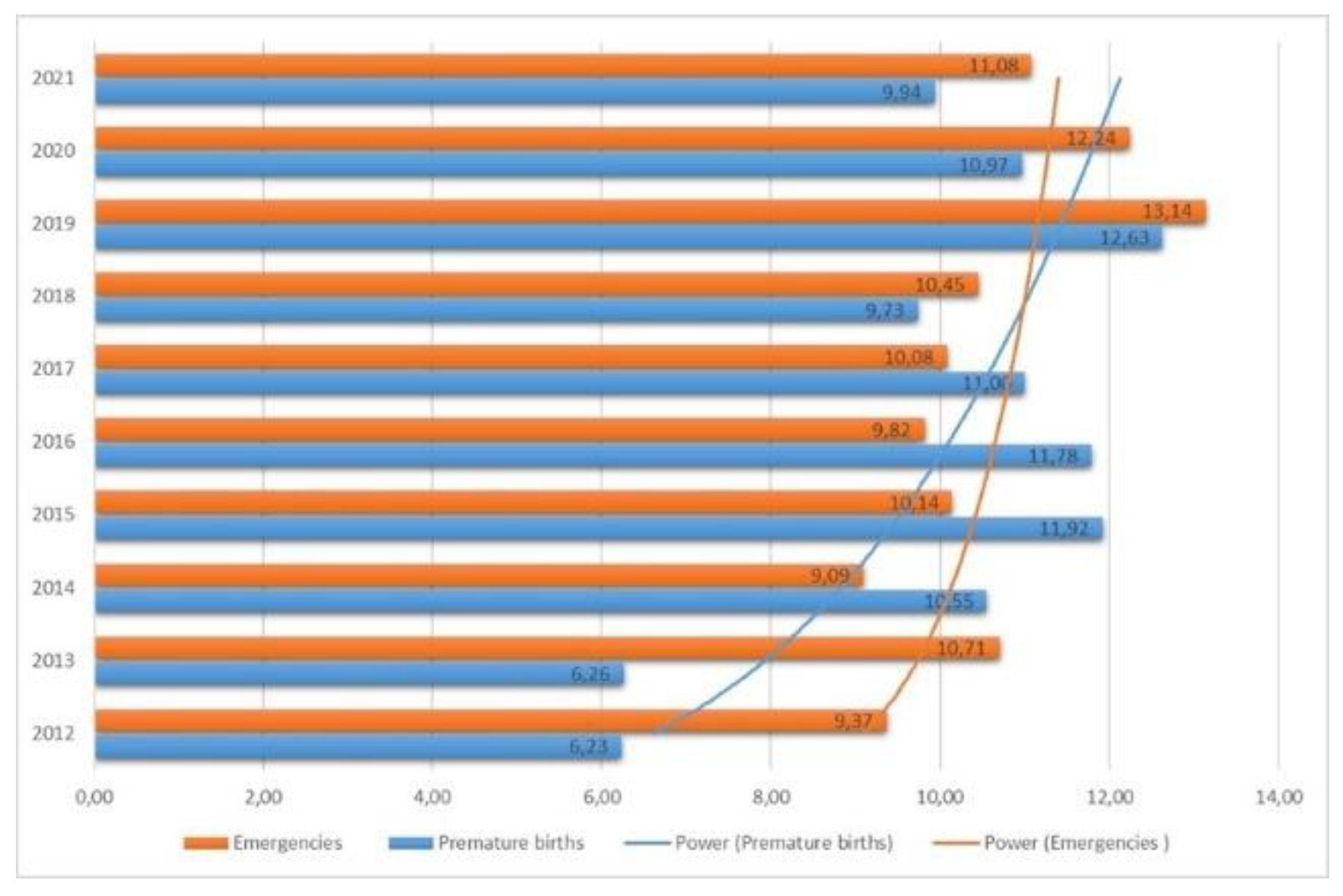
At the same time, the incidence of premature births increases from 6.23% in 2021, reaching a peak of 12.62% in 2019, after that it decreases slightly in the pandemic and post-pandemic years (10.9% and 9.93%, respectively,
Figure 1). The incidence of neonatal emergencies is also increasing in recent years, from 9.37% in 2012 to 11.08% in 2021. The incidence of neonatal emergencies was 10.52% in the studied period, and it showed an upward trend (
Figure 1).
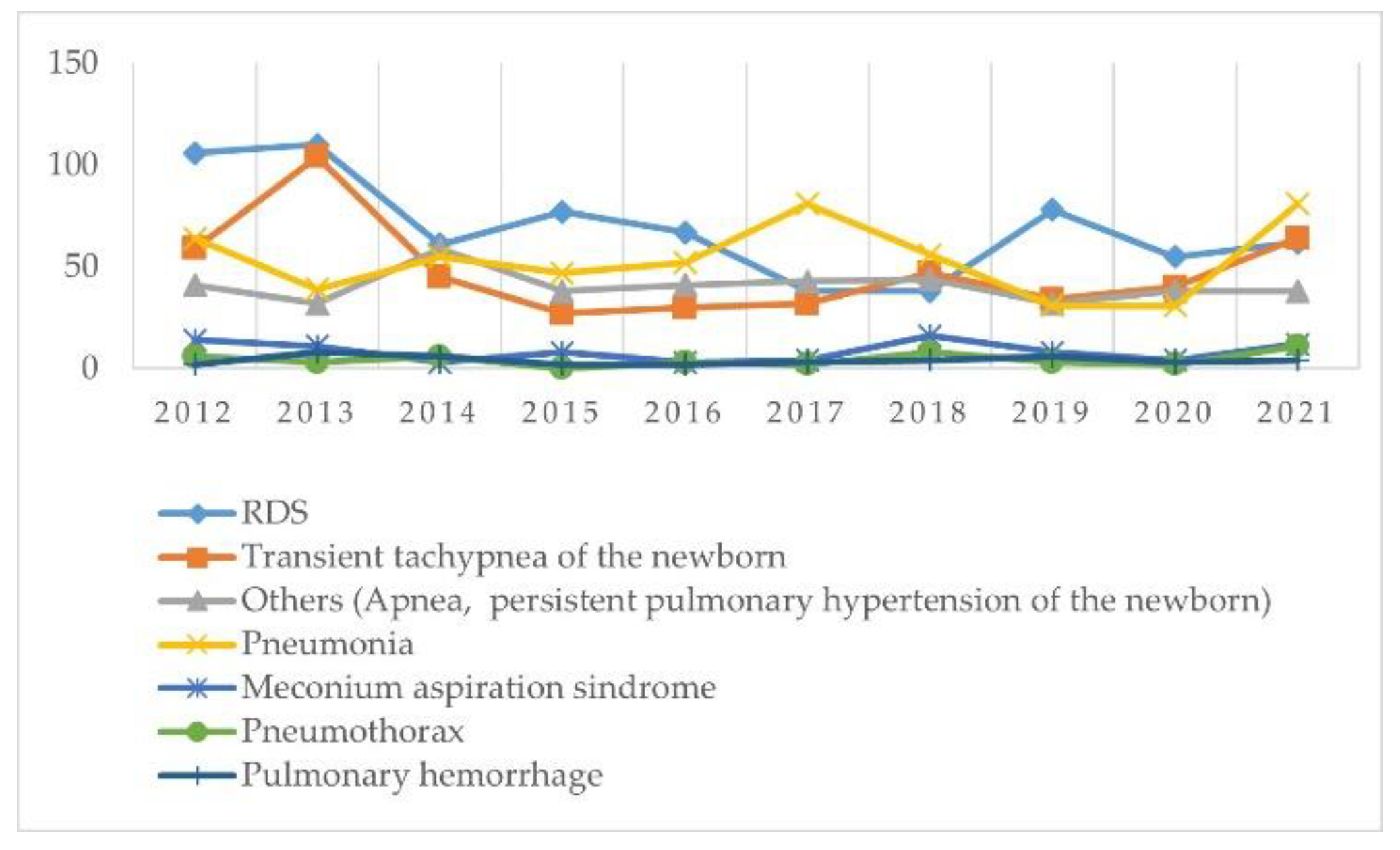
There are different aetiologies of neonatal emergencies: respiratory, cardiovascular, infections, gastrointestinal, neurological. Respiratory emergencies are found first among the aetiologies that require neonatal resuscitation (36%) and included respiratory distress syndrome (RDS), meconium aspiration syndrome (MAS), pneumothorax, pulmonary hemorrhage, pneumonia (
Table 2). Initial signs of respiratory distress are specific and include tachypnoea and increased work of breathing but if distress progresses, new-borns will develop respiratory failure and apnoea
.
There is a 41.50% decrease in new-borns with RDS due to surfactant deficiency, probably due to the effectiveness of the prophylaxis of this disease both antenatally and immediately postnatally. The trend of transient tachypnoea of the new-born remains constant. It is noticeable in the last year included in the study (2021), the marked increase in cases of meconial aspiration syndrome, pneumothorax, pulmonary haemorrhage (
Figure 2). The year 2021, the post-pandemic year, is characterized by a marked increase in the incidence of severe respiratory pathologies that occurred because of insufficient monitoring of pregnancies (due to the imposed restrictions).
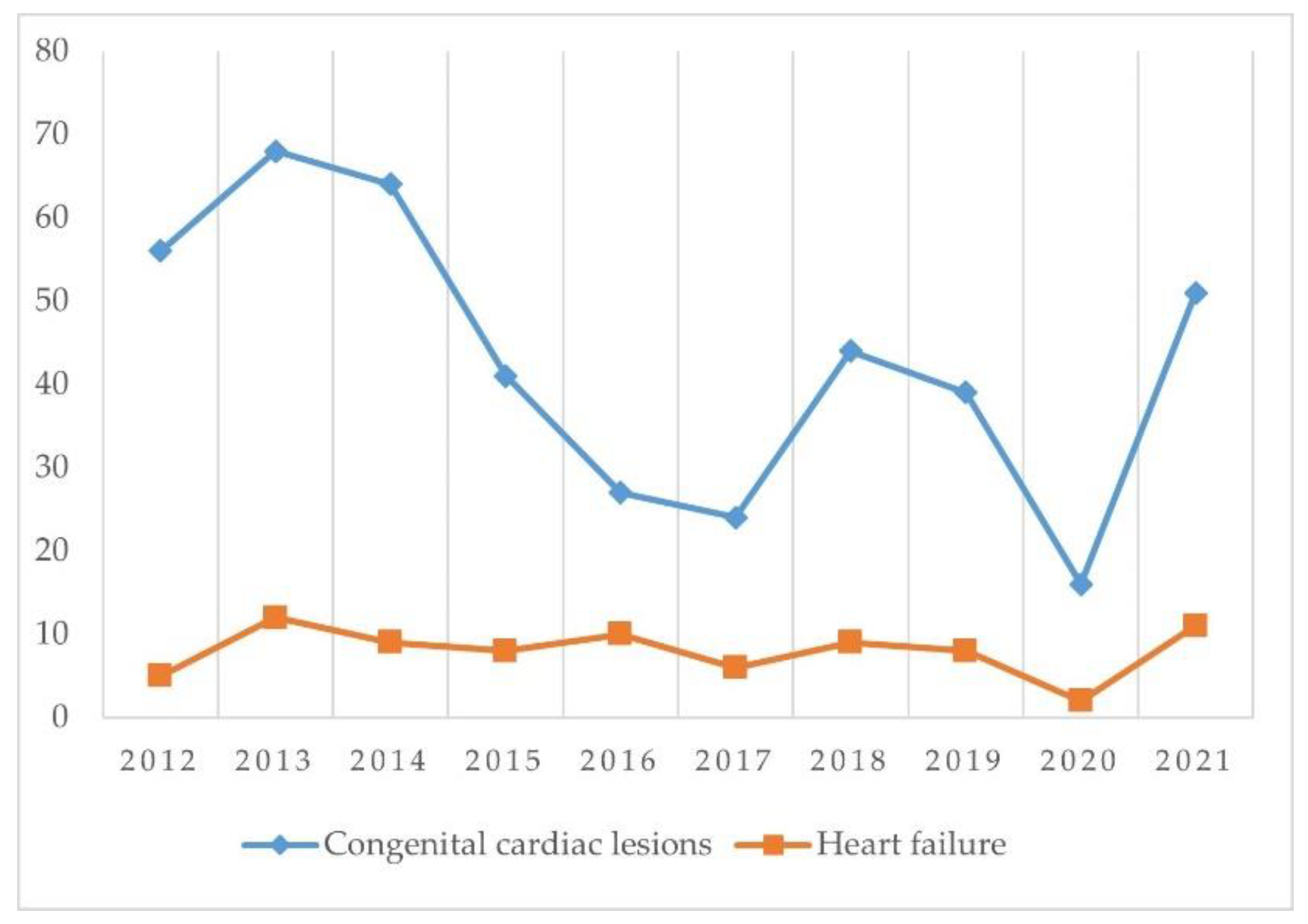
Prompt recognition of congenital cardiac deformity is imperative in the first hours or days of life. Cardiovascular emergencies represent 12.79% of all neonatal emergencies in the studied period. The trend is maintained constantly throughout the years. Except for the year 2021 when the incidence of heart malformations triples compared to previous years (
Figure 3). Probably due to poor follow-up of the pregnancy in 2020 or possibly secondary to the maternal infection with the SARS Cov 2 Virus.
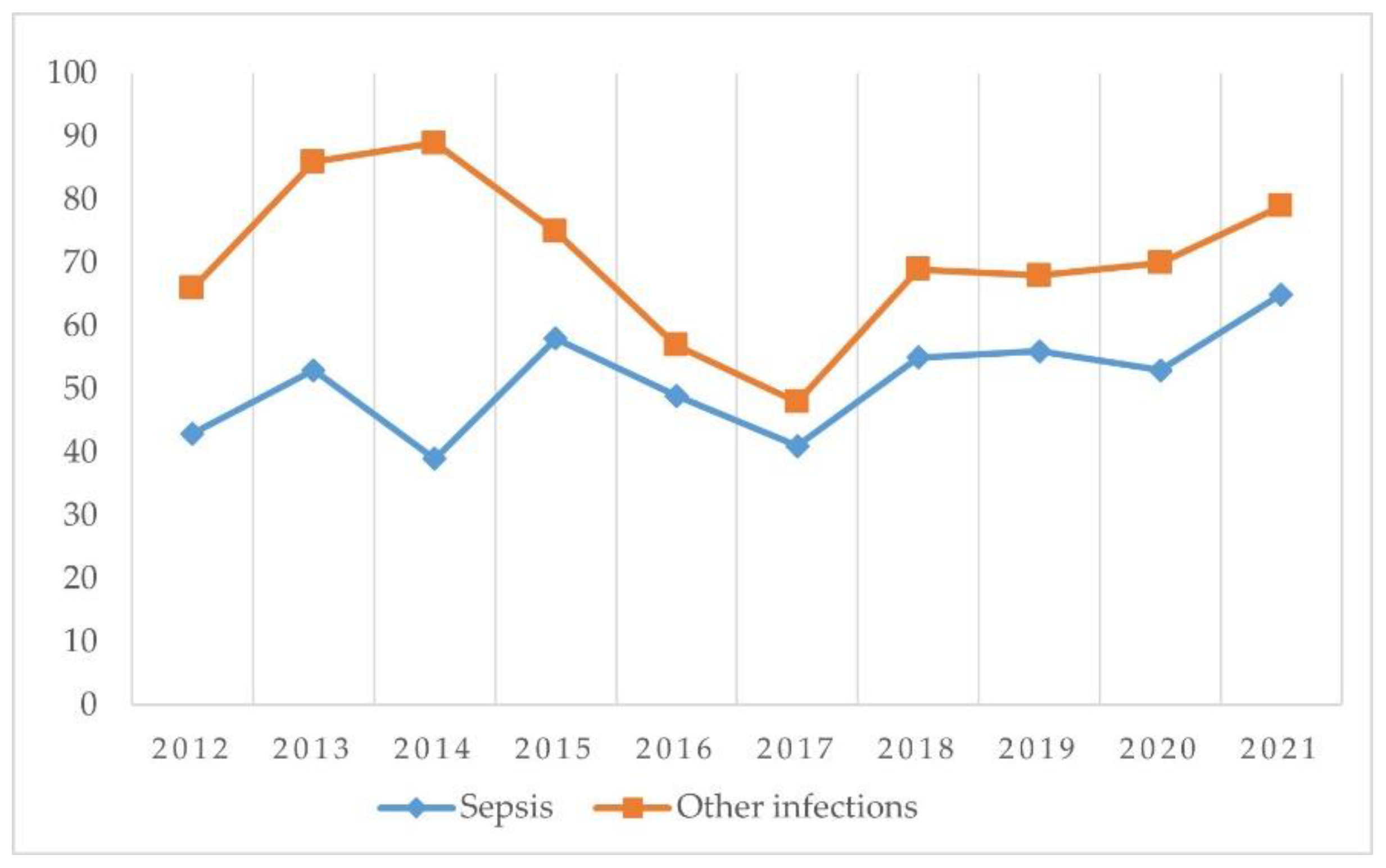
From the point of view of new-borns with neonatal sepsis, their incidence is constant during these years. The general incidence in the studied period is 17.73% and they are prevalent compared with other infections (
Figure 4).
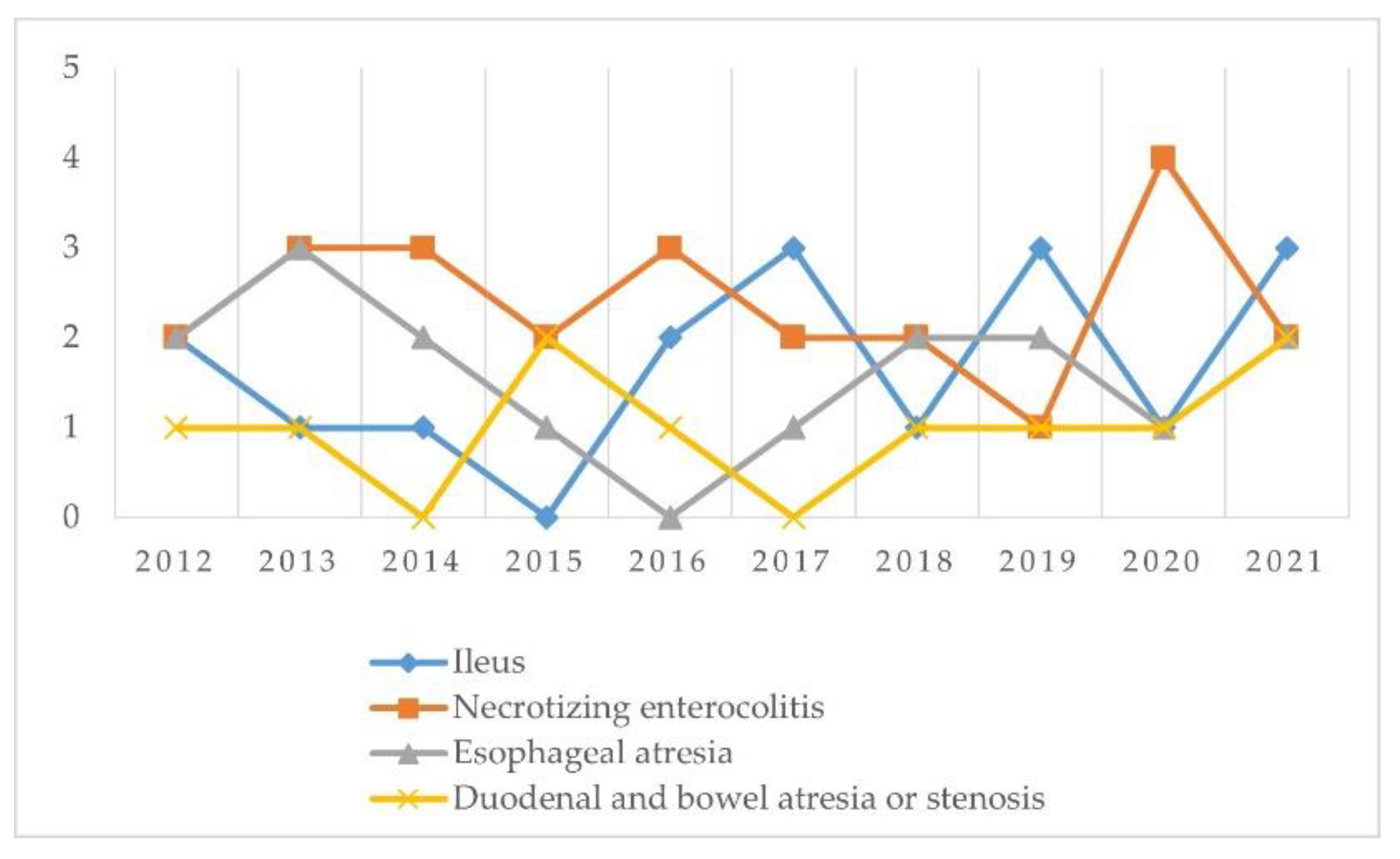
Gastrointestinal emergencies that may present in the newborn period are represented by necrotic ulcerative enterocolitis, esophageal atresia, stenosis, duodenal and intestine atresia, ileus. There is a reduced incidence of gastrointestinal emergencies in our unit, representing 1.68% of all emergencies and the most important were necrotic ulcerative enterocolitis and ileus.
Figure 5.
Types of gastrointestinal emergencies and evolution of them.
Figure 5.
Types of gastrointestinal emergencies and evolution of them.
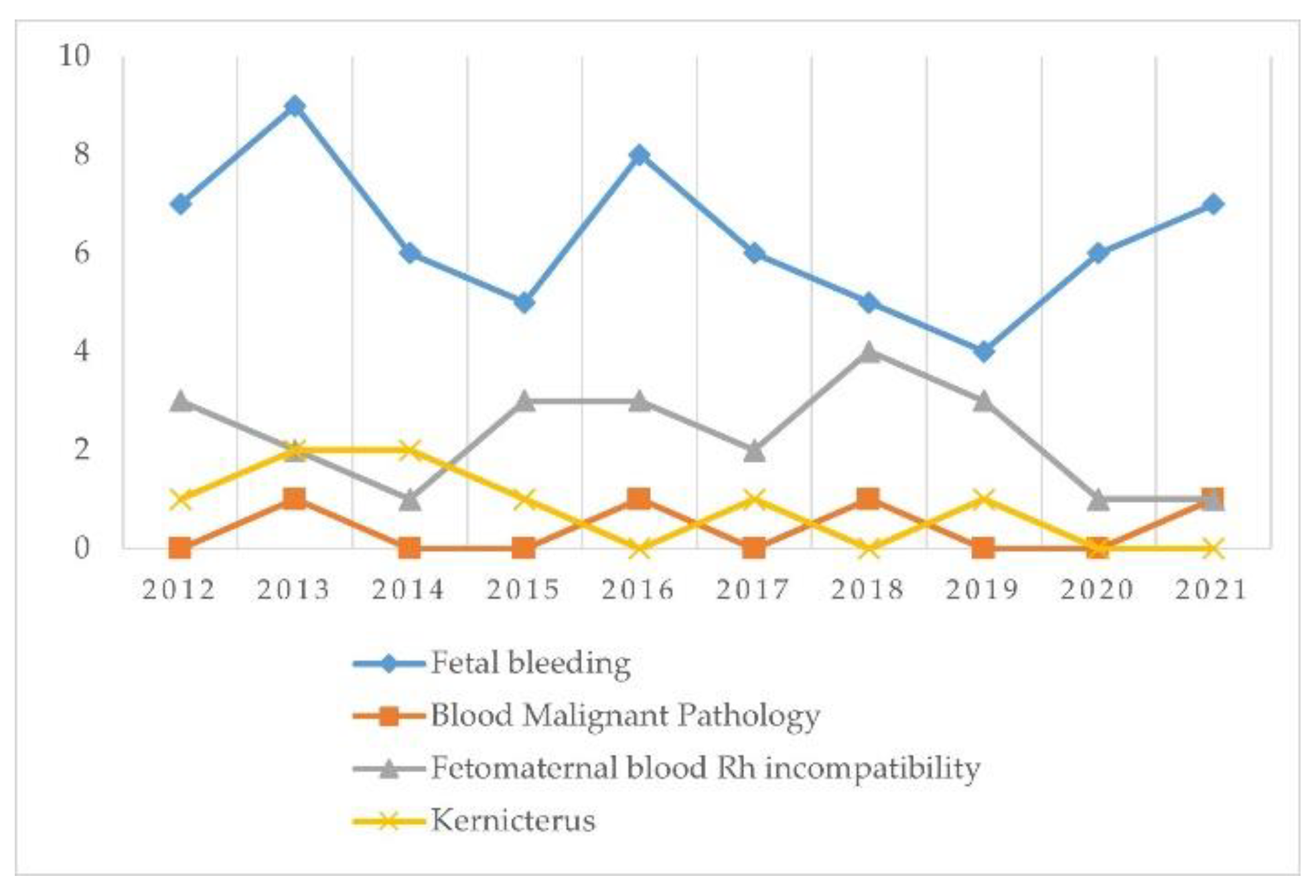
Bleeding, and petechiae are not common presenting issues in newborns, but when are present, they need to be explored and treated. Hematological emergencies represent 2.45% of all emergencies in the period studied and most of them consist in bleeding followed by isoimmunization in the Rh system (
Figure 6).
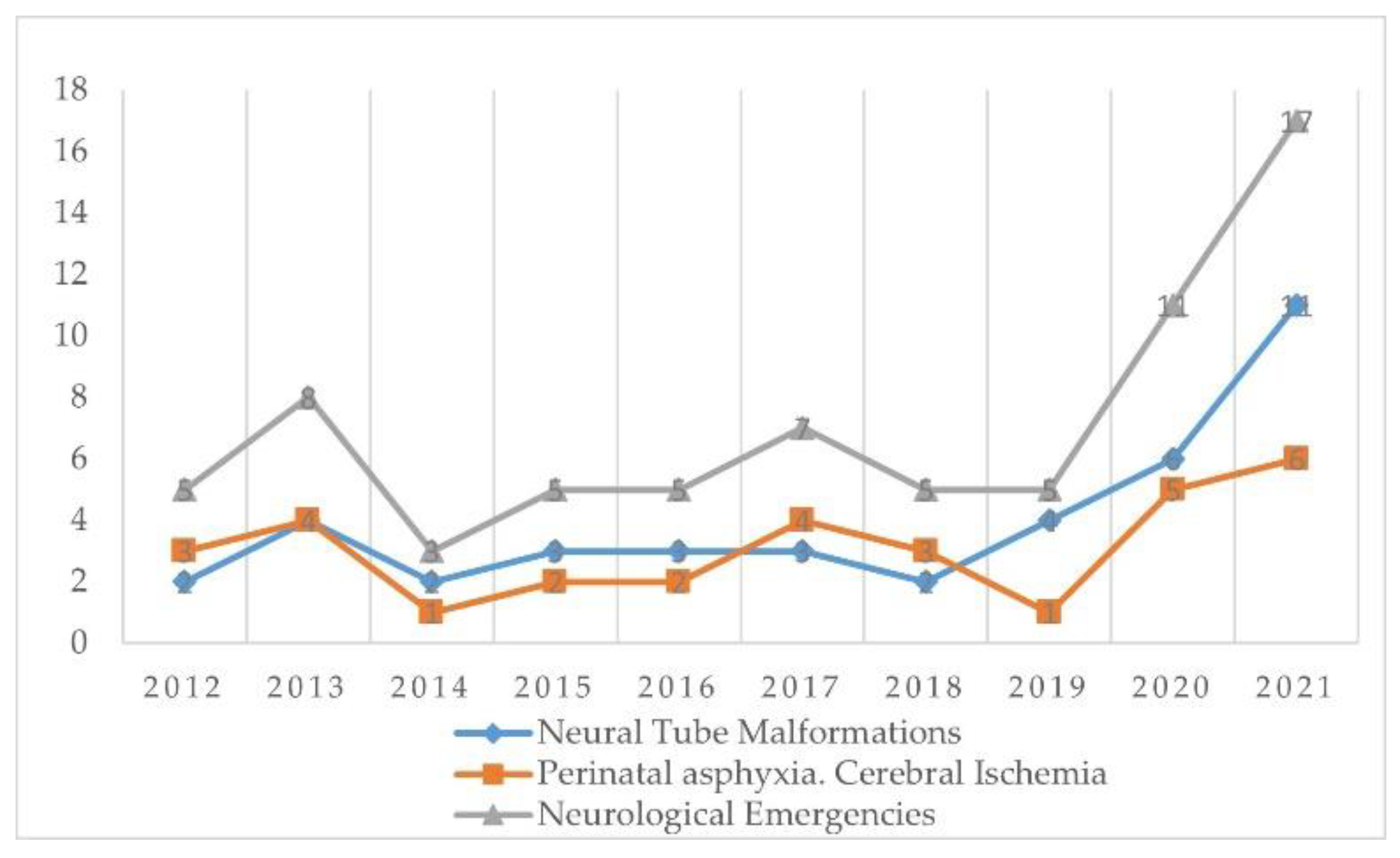
From the point of view of neurological emergencies, we evaluated perinatal asphyxia, cerebral ischemia, and neural tube malformations. It is noted that in 2021 the incidence of these neurological diseases increased by three times compared to previous years (
Figure 7). The most common neural tube anomalies were spina bifida and myelomeningocele. Ischemic neurological damage with subsequent neurological sequelae is noted
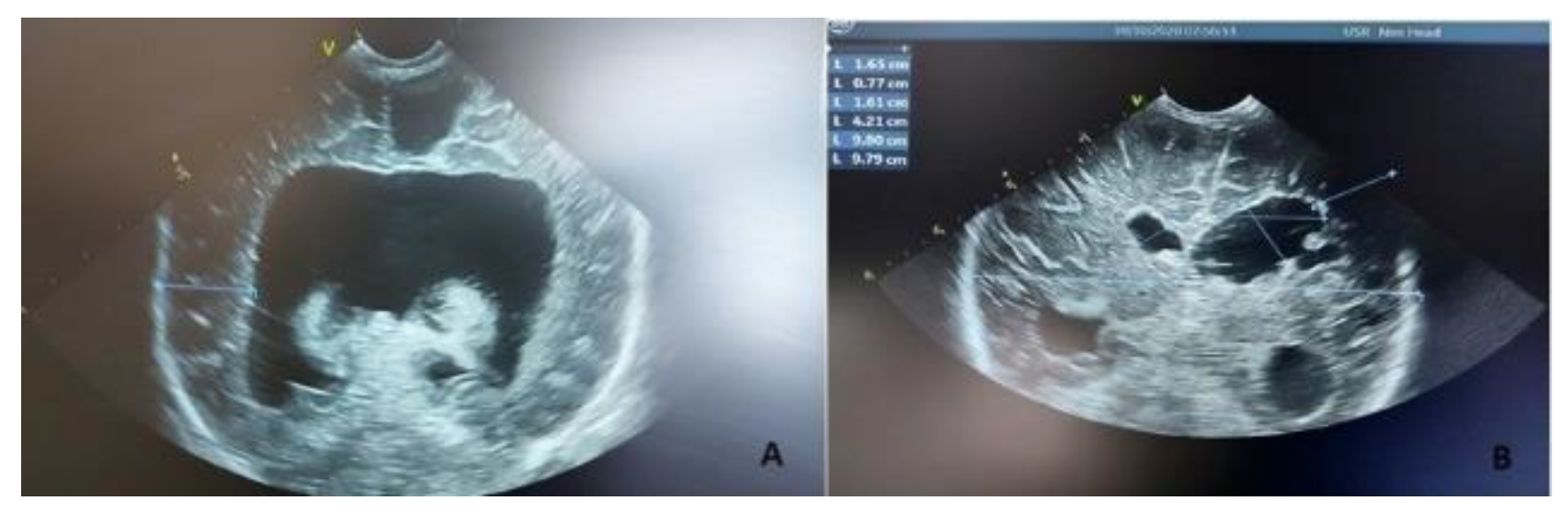
Cerebral ischemic lesions were observed during the foetal ultrasound evaluation or through trans fontanel ultrasound performed postnatal (
Figure 8). We can interpret it as secondary to severe hypoxic intrauterine injuries or ischemic accidents to the intrauterine foetus. Possibly through the increased aggressiveness of an insufficiently known virus, on the foetus, and probably through an insufficient knowledge of the treatment of the pregnant woman infected with Covid 19.
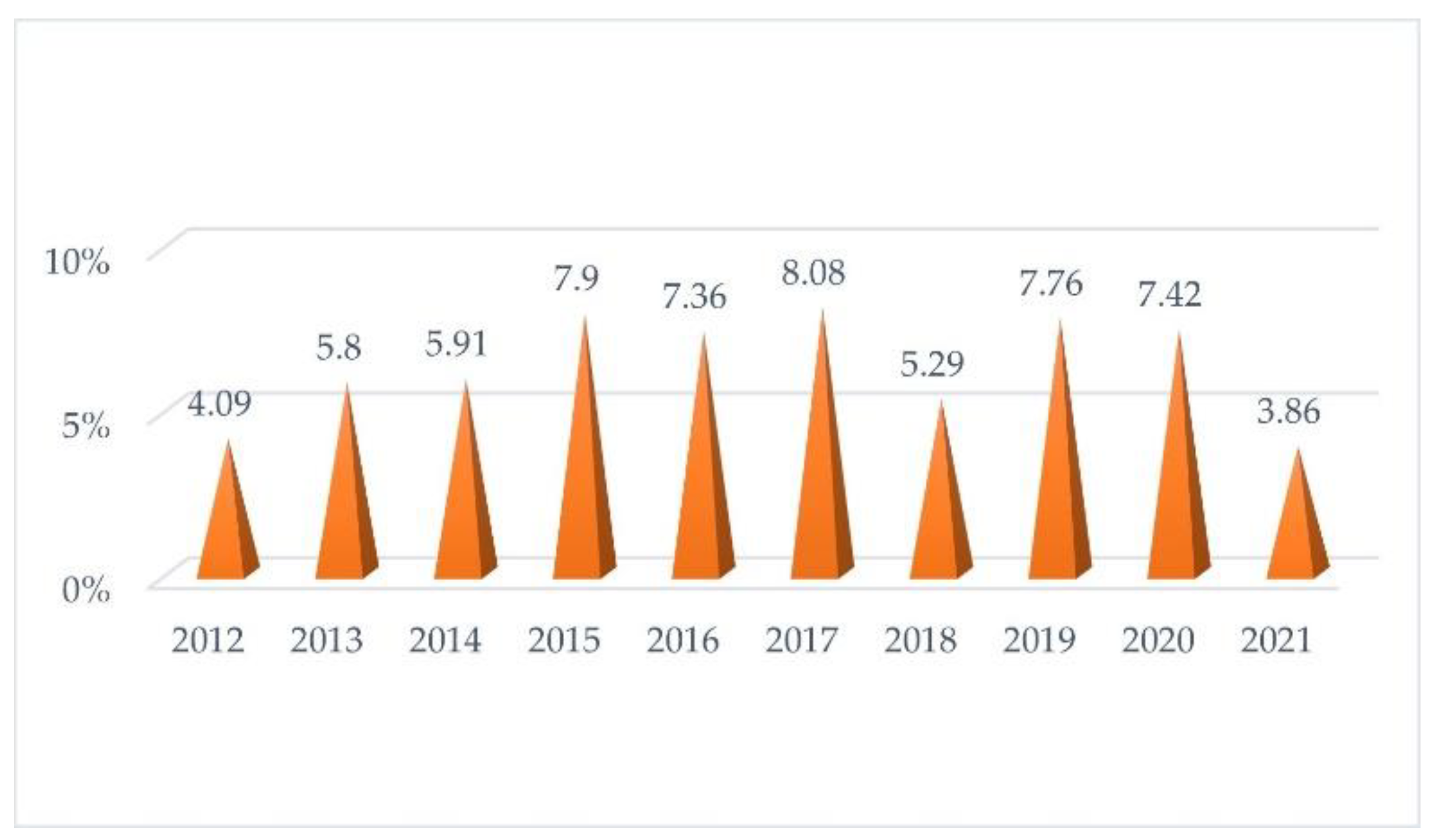
Despite increasing the quality of care for premature new-borns, extreme prematurity has an upward trend until 2020, from 4.1% of total emergencies in 2012 to 7.43% in 2020 (
Figure 9). Next is the year 2021 in which the incidence of extreme prematurity drops a lot to 3.84%. This shows the importance of physical rest in preventing premature birth (pandemic year with the imposed restrictions).
By using multivariable logistic regression, we analyzed the neonatal and maternal risk factors associated with admission to the NICU (
Table 3). Mother’s age over 35 years, low level of education, the second/more pregnancy and infectious pathology of the mother were associated with neonatal emergencies and NICU admission (p<0.001).Weight under 2500 g (OR 2.26, 95% CI: 1.21-4.21), Apgar score under 7 (OR 2,79, CI: 1.45-2.35), premature rupture of membranes (OR 2.11; CI:0.92- 4.8), macrosomia (OR 2.43, CI:0.61-6.69) had over twice the odds of neonatal emergency (respectively). Detachment from the placenta had three times the odds for neonatal emergency. No significant associations were detected between NICU admission for a neonatal emergency and maternal factors such as mother’s aged 18-34 years, medium and higher level of education, residence.
4. Discussion
According to our analysis, the number of births over the past ten years has been declining; in 2021, there were 20.9% fewer births than in 2012, and 90% of those births were at term. When compared to Europe, where there was a modest rise in births over 2020, with 4.07 million babies born, the number of children born in the EU has generally been declining, starting in 2008 (4.68 million children) and 4.09 million babies were born in 2021[
12]. In addition, the EU ‘s overall fertility rate in 2021 was 1.53 live births per woman slightly more than in 2020 (1.50) [
13]. In the United States, 3,953,590 births were registered in 2011, which is the lowest number of births since 1998 and 1% fewer than in 2010 (3,999,386). In 2011, the number of births fell for the three major racial and Hispanic origin groups: non-Hispanic white women, non-Hispanic black women, and Hispanic women. The fall was 1%, 3%, and 4%, respectively [
14].
An elevated frequency of multiple births was a contributing factor to the increase, with multiples accounting for between 17% and 27% of premature births. Over this time, there may have been an increase in the prevalence of multiple pregnancies, in vitro fertilization (IVF), older mothers, and high body mass index (BMI) [
15]. The Euro-Peristat group looked into stillbirths between gestational weeks 22 and 28 in 2004 and 2015 in a distinct study. Thirty-two percent of stillbirths were these ones. While the rates differed throughout the study ‘s participating countries, the rate of stillbirths from weeks 24+0 to 28+0 dropped from a pooled rate of 0.97 to 0.7 per 1,000 newborns [
16].
The incidence of neonatal emergencies has also increased in recent years, from 9.37% in 2012 to 11.07% in 2021. The incidence of neonatal emergencies in the studied period was 10.52% and it showed an upward trend. Similar to the previous few decades in our study, growing patient numbers, increasing complexity, and a lack of staff have led to an increase in emergency department congestion [
17].
There is a 41.50% decrease in new-borns with RDS due to surfactant deficiency, probably due to the effectiveness of the prophylaxis of this disease both antenatally and immediately postnatally. The trend of transient tachypnoea of the new-born remains constant. It is noticeable in the last year included in the study (2021), the marked increase in cases of meconial aspiration syndrome, pneumothorax, pulmonary haemorrhage. The year 2021, the post-pandemic year, is characterized by a marked increase in the incidence of severe respiratory pathologies that occurred because of insufficient monitoring of pregnancies (due to the imposed restrictions). The incidence of RDS is negatively correlated with the infant’s gestational age, according to a study by Sudeep Yadav et al., with more severe disease in smaller and preterm newborns. Even though RDS patients now have better results thanks to therapy options for such surfactants, prenatal corticosteroids, and sophisticated respiratory care for the neonate, RDS is still the primary cause of morbidity and mortality in preterm infants [
18,
19]. Similar to our investigation, during the previous 25 years, surfactant replacement therapy has transformed infant care, according to the evaluation by McCrossan et al. Research should continue to improve the timing and effectiveness of this life-saving intervention, which should lead to better long-term respiratory outcomes for preterm neonates [
20].
Prompt recognition of congenital cardiac deformity is imperative in the first hours or days of life. Cardiovascular emergencies represent 12.79% of all neonatal emergencies in the studied period. The trend is maintained constantly throughout the years. Except for the year 2021 when the incidence of heart malformations triples compared to previous years. Probably due to poor follow-up of the pregnancy in 2020 or possibly secondary to the maternal infection with the SARS Cov 2 Virus. In Europe, around one-third of babies with significant congenital malformations identified during pregnancy or early childhood have congenital cardiac disorders (CHD) [
21,
22]. In contrast to our analysis, where the incidence trend of cardiac defects triples, significant advancements in therapy over the past few decades have resulted in a decline in infant mortality and an increase in children and adults with CHD. According to registries within nations and between countries, the overall prevalence of CHD in Europe from 2000 to 2005 was 8.0 per 1000 births, whereas the prevalence of live births was 7.2 per 1000 births. A 2002 evaluation of sixty-two studies [
23] reported a median live births prevalence of 7.5 per 1000, which is comparable to the 7.5 per 1000 seen in our analysis, with an interquartile range of 6.0 to 10.6 per 1000. The most frequent cause of birth defects is congenital cardiac abnormalities. Our unit’s congenital heart disease incidence was 2.11%, which was marginally greater than the 0.3–1.2% reported in the literature [
24].
From the point of view of new-borns with neonatal sepsis, their incidence is constant during these years. The general incidence in the studied period is 17.73% and they are prevalent compared with other infections. The management of neonatal and infant care groups is challenged by the global issue of neonatal sepsis (NS). As bacterial sepsis affects 1 to 10 out of every 1000 live births globally, it has been noted that newborns are most at risk for the condition [
25,
26]. The incidence of sepsis in developing nations is significantly greater than in developed nations, in contrast to our study where the incidence of sepsis stays constant. In some of these nations, the mortality rate from sepsis-related causes has been reported to reach 50% for infants who do not receive treatment. As a result, throughout the first month of life, this was a leading cause of infant mortality. Improvements in sepsis detection and treatment can significantly reduce complications and enhance the prognosis of sepsis, particularly in premature newborns. According to available published data, sepsis accounts for roughly 10% of maternal fatalities and 26% of newborn mortality [
27].
Gastrointestinal emergencies that may present in the newborn period are represented by necrotic ulcerative enterocolitis, esophageal atresia, stenosis, duodenal and intestine atresia, ileus. There is a reduced incidence of gastrointestinal emergencies in our unit, representing 1.68% of all emergencies. Emergencies related to the gastrointestinal system (GI) may arise at any point along the GI tract in newborns and babies. While fetal imaging may be useful in identifying the root reasons, postnatal radiologic evaluation, along with a thorough physical examination and detailed history collection, is necessary to restrict the differential diagnosis, choose the best course of action, and reduce the risk of death and morbidity [
28]. Of all surgical GI conditions in neonates, necrotizing enterocolitis (NEC) is the most prevalent surgical emergency with the highest morbidity and fatality rate [
29,
30]. Our analysis confirms that the incidence is inversely linked to gestational age and birth weight, with most patients being premature newborns with low birth weights (particularly 500–750 g) and only 7%–13% being full-term infants [
31].
Bleeding and petechiae are not common presenting issues in newborns, but when are present, they need to be explored and treated. Hematological emergencies represent 2.45% of all emergencies in the time studied and most of them consist in bleeding followed by isoimmunization in the Rh system. In the neonatal phase, hemorrhagic diseases are especially common. The causes of bleeding in neonates are complex and include trauma, hepatic illness, disseminated intravascular coagulation, vitamin K insufficiency, inherited bleeding disorders, thrombocytopenia, and platelet function deficiencies [
32]. A rare condition with a significant death and morbidity rate is hemorrhagic disease of the newborn (HDN) [
33]. In the first year of life, it is among the most common causes of cerebral hemorrhage. Only 20–50% of an adult’s coagulation activity is present in newborns. They are more vulnerable to vitamin K deficient bleeding if they are not given vitamin K from birth, are exclusively breastfed, have chronic diarrhea, or use antibiotics for an extended period [
34]. Our analysis confirms the prevalence of newborn hemorrhagic syndromes, which account for 2.17% of neonatal hospitalizations in Salem et al. [
35] and 5.9% in Jabnoun et al. [
36] studies.
From the point of view of neurological emergencies, we evaluated perinatal asphyxia, cerebral ischemia, and neural tube malformations. It is noted that in 2021 the incidence of these neurological diseases increased by three times compared to previous years. Ischemic neurological damage with subsequent neurological sequelae is noted. Cerebral ischemic lesions were observed during the foetal ultrasound evaluation or through trans fontanel ultrasound performed postnatal. Perinatal asphyxia counts among the top three causes of under-five child mortality (11%) in the World Health Organization, along with preterm delivery (17%) and pneumonia (15%) [
37]. In developed nations, the rate of perinatal asphyxia is 2 per 1000 live births; however, in developing nations, where access to maternal and neonatal care is inadequate, the rate is 10 times higher. This finding is further supported by our research, which shows a three-fold increase in the incidence of these diseases. Of those newborns who are asphyxiated, 15–25% will pass away during the neonatal stage, and about 25% of those who survive will always have neurological impairments [
38]. The high prevalence of perinatal asphyxia in the study by Gebrehiwot et al. is also supported by our research. Perinatal hypoxia has a startlingly high case fatality rate. Perinatal asphyxia was predicted by prolonged labor, preeclampsia, and the presence of amniotic fluid stained with meconium. Health care professionals should identify and treat high-risk moms early on, and they should use partographs to monitor these mothers during birth [
39,
40].
Mother’s age over 35 years, low level of education, second or more pregnancy, infectious pathology of the mother, detachment from the placenta emerged as risk maternal factors for neonatal emergency demonstrated also in other studies while weight under 2500 g, Apgar score under 7, macrosomia are the neonatal risk factors similar with other studies [
41,
42,
43].
5. Conclusions
Even though most neonatal complications are preventable with the proper explorations and treatments, there are a few severe risk factors predisposing newborns to severe complications and death. Depending on the predisposing factors for the need for neonatal resuscitation, it would be ideal to identify the cases at risk early for an adequate preparation and our study identified the mother and neonate profile, including the aspects at birth. Obviously, preventive strategies, such as prenatal care, monitoring, and careful anamnesis, are crucial for obtaining better outcomes.
Author Contributions
Conceptualization, F.R.D. and N.O.P.; methodology, C.D.D. and C.P.; software, D.C.Z.; validation, F.R.D., C.D.C. and N.O.P.; formal analysis, D.C.Z., P.P. and C.P.; investigation, D.G.D. and P.P.; resources, I.C.C. and P.P.; writing—original draft preparation, F.R.D. and C.D.D.; writing—review and editing, D.G.D.; visualization, I.C.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Bihor County Emergency Clinical Hospital for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Bjorland, P.A.; Øymar, K.; Ersdal, H.L.; Rettedal, S.I. Incidence of newborn resuscitative interventions at birth and short-term outcomes: A regional population-based study. BMJ Paediatr Open 2019, 3, e000592. [Google Scholar] [CrossRef]
- Skåre, C.; Kramer-Johansen, J.; Steen, T.; Ødegaard, S.; Niles, D.E.; Nakstad, B.; Solevåg, A.L.; Nadkarni, V.M.; Olasveengen, T.M. Incidence of Newborn Stabilization and Resuscitation Measures and Guideline Compliance during the First Minutes of Life in Norway. Neonatology 2015, 108, 100–107. [Google Scholar] [CrossRef]
- Quinn, C.E.; Sivasubramaniam, P.; Blevins, M.; Al Hajajra, A.; Znait, A.T.; Khuri-Bulos, N.; Faouri, S.; Halasa, N. Risk factors for neonatal intensive care unit admission in Amman, Jordan. East Mediterr Health J. 2016, 22, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Bizzego, A.; Gabrieli, G. Predictors of Contemporary under-5 Child Mortality in Low- and Middle-Income Countries: A Machine Learning Approach. Int J Environ Res Public Health. 2021, 18, 1315. [Google Scholar] [CrossRef]
- Aziz, K.; Chadwick, M.; Baker, M.; Andrews, W. Ante- and intra-partum factors that predict increased need for neonatal resuscitation. Resuscitation 2008, 79, 444–452. [Google Scholar] [CrossRef]
- Chadha, I.A. Neonatal resuscitation: Current issues. Indian J Anaesth. 2010, 54, 428–438. [Google Scholar] [CrossRef] [PubMed]
- Yangthara, B.; Horrasith, S.; Paes, B.; Kitsommart, R. Predictive factors for intensive birth resuscitation in a developing-country: A 5-year, single-center study. J Matern Fetal Neonatal Med. 2020, 33, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Weiner, G.M. Textbook of neonatal resuscitation. 7th Edn. American Academy of Pediatrics; Elk Grove Village, I: 2016.
- Dorobanțu, F.R.; Hodoșan, V.; Tîrb, A.M.; Zaha, D.C.; Galușca, D.; Pop, N.O.; Dorobanțu, C.D. Pattern of Newborn Antibiotic Use in a Tertiary Level Maternity for Five Years. Pharmacophore, 2020, 13, 57–63. [Google Scholar] [CrossRef]
- WHO. Levels and trends in child mortality: Report 2021. https://www.who.int/publications/m/item/levels-and-trends-in-child-mortality-report-2021.
- https://ec.europa.eu/eurostat/web/products-eurostat-news/w/ddn-20230309-1.
- Woodd, S.L.; Montoya, A.; Barreix, M.; Pi, L.; Calvert, C.; Rehman, A.M.; Chou, D.; Campbell, O.M.R. Incidence of maternal peripartum infection: A systematic review and meta-analysis. PLoS Med. 2019, 16, e1002984. [Google Scholar] [CrossRef]
- https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Fertility_statistics.
- https://stacks.cdc.gov/view/cdc/23435.
- Zeitlin, J.; Szamotulska, K.; Drewniak, N.; Mohangoo, A.D.; Chalmers, J.; Sakkeus, L.; Irgens, L.; Gatt, M.; Gissler, M.; Blondel, B. Euro-Peristat Preterm Study Group. Preterm birth time trends in Europe: A study of 19 countries. BJOG. 2013, 120, 1356–1365. [Google Scholar] [CrossRef]
- Smith, L.K.; Hindori-Mohangoo, A.D.; Delnord, M.; Durox, M.; Szamotulska, K.; Macfarlane, A. Quantifying the burden of stillbirths before 28 weeks of completed gestational age in high-income countries: A population-based study of 19 European countries. Lancet 2018, 392, 1639–1646. [Google Scholar] [CrossRef]
- Kappy, B.; Berkowitz, D.; Isbey, S.; Breslin, K.; McKinley, K. Characteristics and patient impact of boarding in the pediatric emergency department, 2018-2022. Am J Emerg Med. 2024, 77, 139–146. [Google Scholar] [CrossRef]
- Yadav, S.; Lee, B.; Kamity, R. Neonatal Respiratory Distress Syndrome. 2023. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- McPherson, C.; Wambach, J.A. Prevention and Treatment of Respiratory Distress Syndrome in Preterm Neonates. Neonatal Netw. 2018, 37, 169–177. [Google Scholar] [CrossRef]
- McCrossan, P.M.; Sweet, D.G. Surfactant therapy–past, present and future. Infant 2018, 14, 218–222. [Google Scholar]
- Suard, C.; Flori, A.; Paoli, F.; Loundou, A.; Fouilloux, V.; Sigaudy, S.; Michel, F.; Antomarchi, J.; Moceri, P.; Paquis-Flucklinger, V.; D’Ercole, C.; Bretelle, F. Accuracy of prenatal screening for congenital heart disease in population: A retrospective study in Southern France. PLoS ONE. 2020, 15, e0239476. [Google Scholar] [CrossRef]
- Daalderop, L.A.; Been, J.V.; Steegers, E.A.P.; Bertens, L.C.M. Impact of the EURO-PERISTAT Reports on obstetric management: A difference-in-regression-discontinuity analysis. Eur J Public Health. 2023, 33, 342–348. [Google Scholar] [CrossRef]
- Wu, W.; Shao, X. Incidence and mortality trend of congenital heart disease at the global, regional, and national level, 1990–2017. Medicine 2020, 99, e20593. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, S.; Zühlke, L.; Black, G.C.; Choy, M.K.; Li, N.; Keavney, B.D. Global birth prevalence of congenital heart defects 1970–2017: Updated systematic review and meta-analysis of 260 studies. Int J Epidemiol 2019, 48, 455–463. [Google Scholar] [CrossRef]
- Schlapbach, L.J.; Kissoon, N. Defining Pediatric Sepsis. JAMA Pediatr. 2018, 172, 313–314. [Google Scholar] [CrossRef]
- Menon, K.; Schlapbach, L.J.; Akech, S.; Argent, A.; Biban, P.; Carrol, E.D.; Chiotos, K.; Jobayer Chisti, M.; Evans, I.V.R.; Inwald, D.P.; et al. Pediatric Sepsis Definition Taskforce of the Society of Critical Care Medicine. Criteria for Pediatric Sepsis-A Systematic Review and Meta-Analysis by the Pediatric Sepsis Definition Taskforce. Crit Care Med. 2022, 50, 21–36. [Google Scholar] [CrossRef]
- Carcillo, J.A.; Berg, R.A.; Wessel, D.; Pollack, M.; Meert, K.; Hall, M.; Newth, C.; Lin, J.C.; Doctor, A.; Shanley, T.; et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network. A Multicenter Network Assessment of Three Inflammation Phenotypes in Pediatric Sepsis-Induced Multiple Organ Failure. Pediatr Crit Care Med. 2019, 20, 1137–1146. [Google Scholar] [CrossRef]
- Shah, B.A.; Padbury, J.F. Neonatal sepsis: An old problem with new insights. Virulence. 2014, 5, 170–178. [Google Scholar] [CrossRef]
- Stanescu, A.L.; Liszewski, M.C.; Lee, E.Y.; Phillips, G.S. Neonatal Gastrointestinal Emergencies: Step-by-Step Approach. Radiol Clin North Am. 2017, 55, 717–739. [Google Scholar] [CrossRef]
- Suciu, L.M.; Puscasiu, L.; Szabo, B.; Cucerea, M.; Ognean, M.L.; Oprea, I.; Bell, E.F. Mortality and morbidity of very preterm infants in Romania: How are we doing? Pediatr. Int. 2014, 56, 200–206. [Google Scholar] [CrossRef]
- Coran, A.G.; Adzick, N.S.; Krummel, T.M.; Laberge, J.M.; Shamberger, R.; Caldamone, A. Pediatric Surgery E-Book: Expert Consult-Online and Print (Vol. 2). Elsevier Health Sciences, 2012.
- Xu, C.; Li, Y.; Zhang, W.; Wang, Q. Analysis of perinatal coagulation function in preeclampsia. Medicine 2021, 100, e26482. [Google Scholar] [CrossRef]
- Kher, P.; Verma, R.P. Hemorrhagic Disease of Newborn. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558994/.
- Murariu, M.G.; Dorobanțu, F.R.; Tărniceriu, D. A Novel Automated Empirical Mode Decomposition (EMD) Based Method and Spectral Feature Extraction for Epilepsy EEG Signals Classification. Electronics. 2023, 12, 1958. [Google Scholar] [CrossRef]
- Araki, S.; Shirahata, A. Vitamin K Deficiency Bleeding in Infancy. Nutrients. 2020, 12, 780. [Google Scholar] [CrossRef]
- Ng, E.; Loewy, A.D. Document de principes: Lignes directrices sur la prophylaxie à la vitamine K chez les nouveau-nés: Une déclaration conjointe de la Société canadienne de pédiatrie et du Collège des médecins de famille du Canada. Can Fam Physician. 2018, 64, e431–e434. [Google Scholar]
- El Hasbaoui, B.; Karboubi, L.; Benjelloun, B.S. Newborn haemorrhagic disorders: About 30 cases. Pan African Medical Journal 2017, 28, 123–123. [Google Scholar] [CrossRef]
- WHO. Global health observatory data repository world health organization. 2015. August 2019. https://apps.who.int/ghodata/.
- Odd, D.; Heep, A.; Luyt, K.; Draycott, T. Hypoxic-ischemic brain injury: Planned delivery before intrapartum events. J Neonatal Perinatal Med. 2017, 10, 347–353. [Google Scholar] [CrossRef]
- Gebregziabher, G.T.; Hadgu, F.B.; Abebe, H.T. Prevalence and Associated Factors of Perinatal Asphyxia in Neonates Admitted to Ayder Comprehensive Specialized Hospital, Northern Ethiopia: A Cross-Sectional Study. Int J Pediatr. 2020, 2020, 4367248. [Google Scholar] [CrossRef] [PubMed]
- Phaloprakarn, C.; Manusirivithaya, S.; Boonyarittipong, P. Risk score comprising maternal and obstetric factors to identify late preterm infants at risk for neonatal intensive care unit admission. J Obstet Gynaecol Res. 2015, 41, 680–688. [Google Scholar] [CrossRef] [PubMed]
- Bouvier, D.; Forest, J.C.; Blanchon, L.; Bujold, E.; Pereira, B.; Bernard, N.; Gallot, D.; Sapin, V.; Giguère, Y. Risk Factors and Outcomes of Preterm Premature Rupture of Membranes in a Cohort of 6968 Pregnant Women Prospectively Recruited. J. Clin. Med. 2019, 8, 1987. [Google Scholar] [CrossRef] [PubMed]
- Ilyes, S.-G.; Chiriac, V.D.; Gluhovschi, A.; Valcovici, M.; Dahma, G.; Mocanu, A.G.; Neamtu, R.; Silaghi, C.; Radu, D.; Bernad, E.; Craina, M. The Influence of Maternal Factors on Neonatal Intensive Care Unit Admission and In-Hospital Mortality in Premature Newborns from Western Romania: A Population-Based Study. Medicina. 2022, 58, 709. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).