1. Introduction
Functional and structural modifications in the microcirculation occur early in hypertension development and in aging [
1,
2,
3]. Previous studies have demonstrated that a reduction in dysfunctional vessels at rest eventually leads to anatomical micro vessel loss (structural rarefaction) as well as functional impairment of capillary perfusion and recruitment [
1,
2] are referred to as “ghost vessels” or “dysfunctional vessels.” The microcirculation in the nailfold is considered to be a predictive and noninvasive marker of generalized microvascular and endothelial function [
4]. The restoration of microvascular function can help decrease systemic blood pressure by reducing peripheral vascular resistance; this, in turn, can improve circulation in target organs and help decrease cardiovascular disease complications [
5]. However, to date, the impact of local exercise on the circulation in the non-exercising limbs remains unknown. Furthermore, details of the immediate impact of exercise on the peripheral circulation in middle-aged and elderly patients with hypertension who are at a high risk of adverse events are lacking. One of the adverse effects of exercise is the rapid activation of the sympathetic nervous system at the start of exercise, which significantly affects the peripheral circulation. Therefore, it is important to ensure the safety of exercise for high-risk individuals. For this reason, the present study aimed to investigate nailfold capillary parameters in community-dwelling individuals aged over 60 years who have hypertension and do not exercise regularly. Furthermore, the study examined the correlations between capillary function and other health-related indicators.
2. Materials and Methods
2.1. Participants
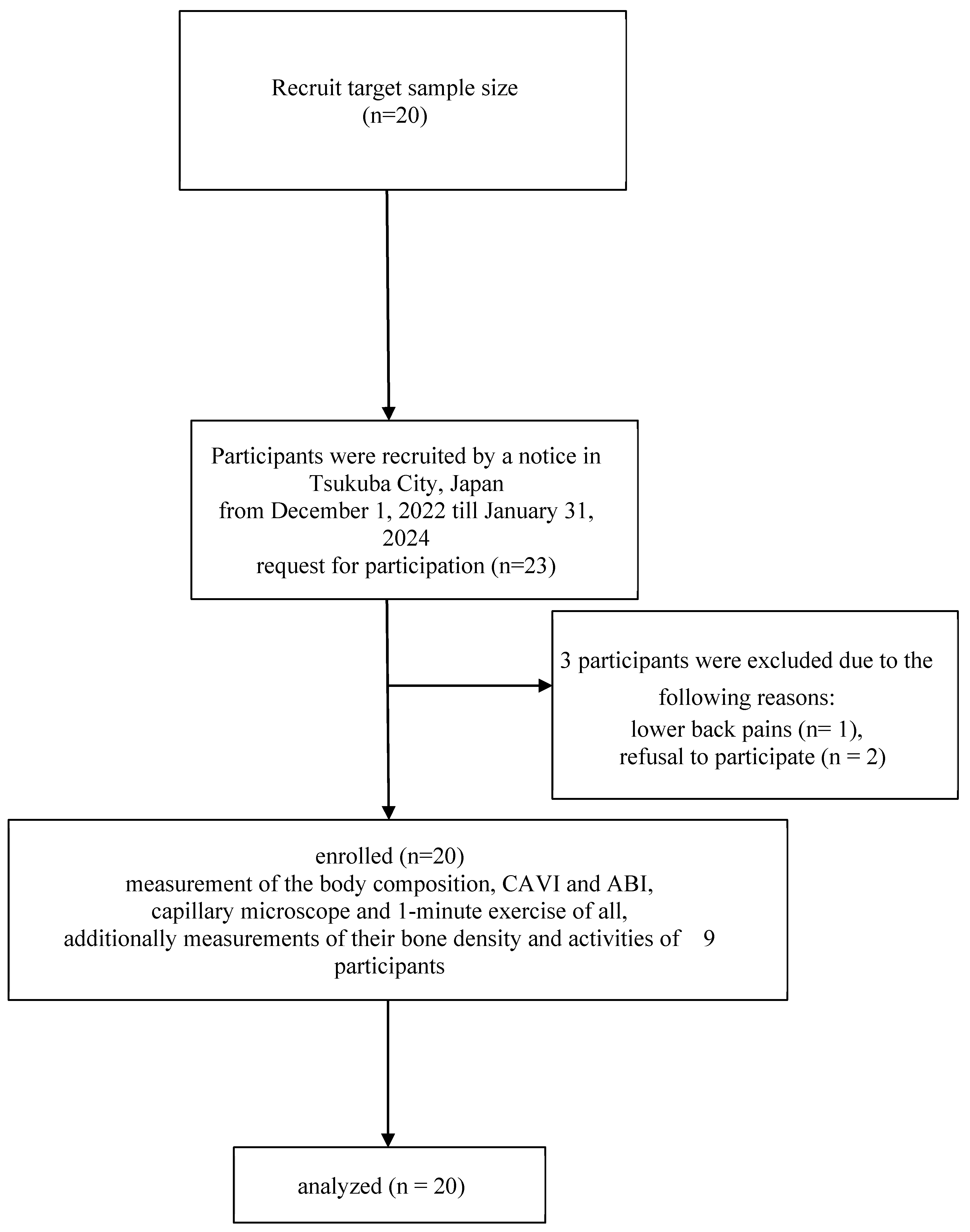
This study enrolled community-dwelling elderly individuals with hypertension who attended public facilities in Tsukuba City, Japan, between December 2022 and January 2024 (
Figure 1). Of the 23 eligible participants, 20 provided informed consent. The baseline characteristics of the participants are shown in
Table 1. Those with contraindications to these examinations, such as pacemaker use, and those with contraindications to exercise therapy as described in the American College of Sports Medicine’s Guidelines for Exercise Testing and Prescription, 9th edition [
6], were excluded from the study. The ethics committee of Tsukuba University of Technology approved the research protocol (approval number: 202204). Furthermore, the study was registered with the University Hospital Medical Network Clinical Trials Registry (Identifier UMIN000053790).
2.2. Study Design
The study followed a single- center pilot trial design.
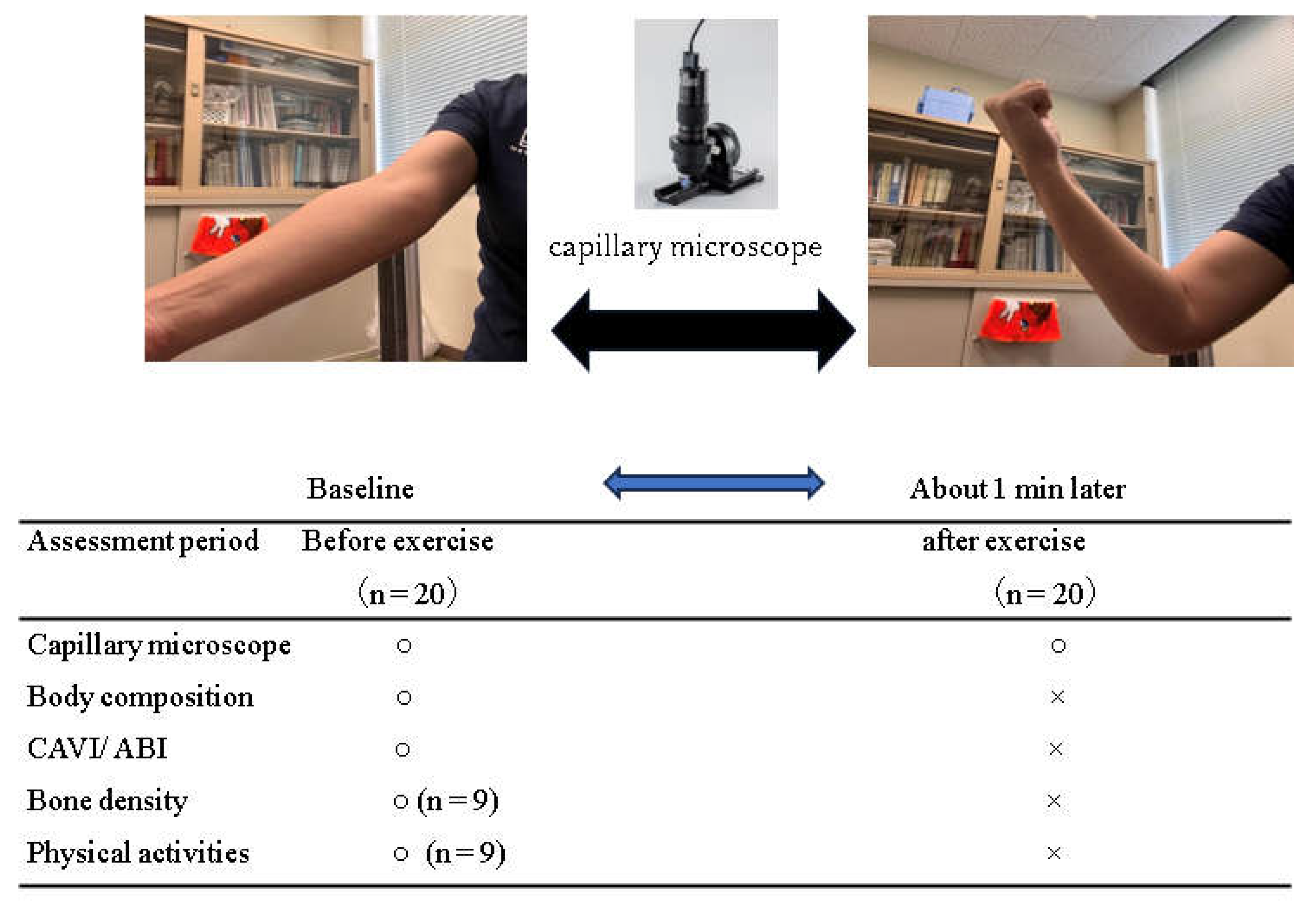
The study protocol is depicted in
Figure 2. The body composition and arterial stiffness of the participants were measured. Then, the participants were asked to perform elbow flexion and extension exercise in the sitting position at 13 RPE for 1 min. Before and after the exercise, the capillary diameter and the flow at the nailfold of the fourth finger for the non-exercising limb were measured with a microscope.
During the session, the temperature was maintained at 23°C. All experiments were conducted simultaneously between 9 and 11 AM. The participants were prohibited from engaging in vigorous exercise, drinking caffeinated beverages, and smoking within 48 h before the experiment.
2.3. Sample Size
The sample size was calculated using G*power (Heinrich-Heine-University Dusseldorf, North Rhine-Westphalia, Germany). The target number of participants was 20 (α = 0.05, 1-β = 0.95), which was based on a study in which capillary examination was conducted in elderly patients [
7,
8].
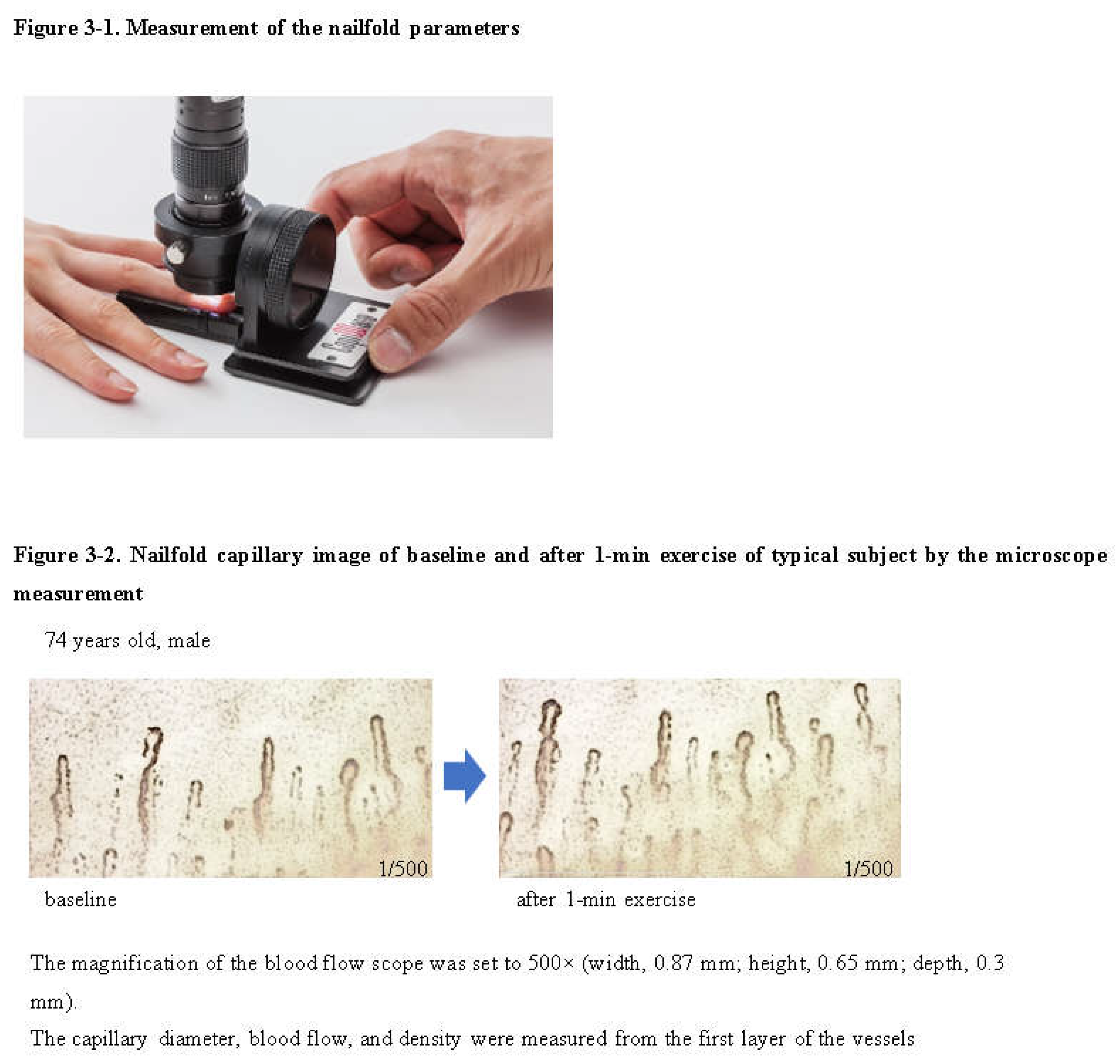
2.4. Measurement of Nailfold Capillary Parameters
Capillary flow was measured using a microscope (Bscan-Z, Tokuda Corporation, Japan) by filming the nailfold of the nondominant the fourth digits of the subjects [
8,
9]. An image analysis software (Capimetrics, KK Technology, UK) was used for the measurements. During filming, the magnification of the blood flow scope was set to 500× (width, 0.87 mm; height, 0.65 mm; depth, 0.3 mm), and 10-s videos of the nailfold of the non-exercising limb was taken [
9]; furthermore, the capillary diameter, blood flow, and density were measured from the first layer of the vessels, as shown in
Figure 3-1,2.
2.5. Body Composition and Physical Activities
The participants’ weight, skeletal muscle mass, and fat mass were measured by a physical therapist using a body composition analyzer (Tanita Corporation MC-780A). In addition, their height and physical activities were read from their application forms [
10].
2.6. Measurement of the CAVI and ABI
After a 15-min rest, the Ankle Brachial Index (ABI) and Cardio Ankle Vascular Index (CAVI) of the participants were measured in the supine position in an air-conditioned room using a VS-1000 instrument (Fukuda Denshi, Tokyo, Japan) [
11].
2.7. Bone Mineral Density
Bone mineral density (BMD) was measured at the right heel using Benus evo (Nihon Kohden Co., Japan) [
12,
13], which was calibrated daily according to the manufacturer’s recommendation. All measurements were performed by the same operator.
2.8. Statistical Analysis
The baseline characteristics were expressed as mean ± standard deviation. All statistical analyses were conducted using the SPSS software ver. 21(IBM Corp, Chicago, IL, USA). Student’s t-test was employed to statistically analyze the logarithmically transformed wear data, and Pearson’s product-moment correlation coefficient was used parameters of capillary and other parameters.
3. Results
All the participants completed the experiments without any difficulty or side effects. The participants’ characteristics are summarized in
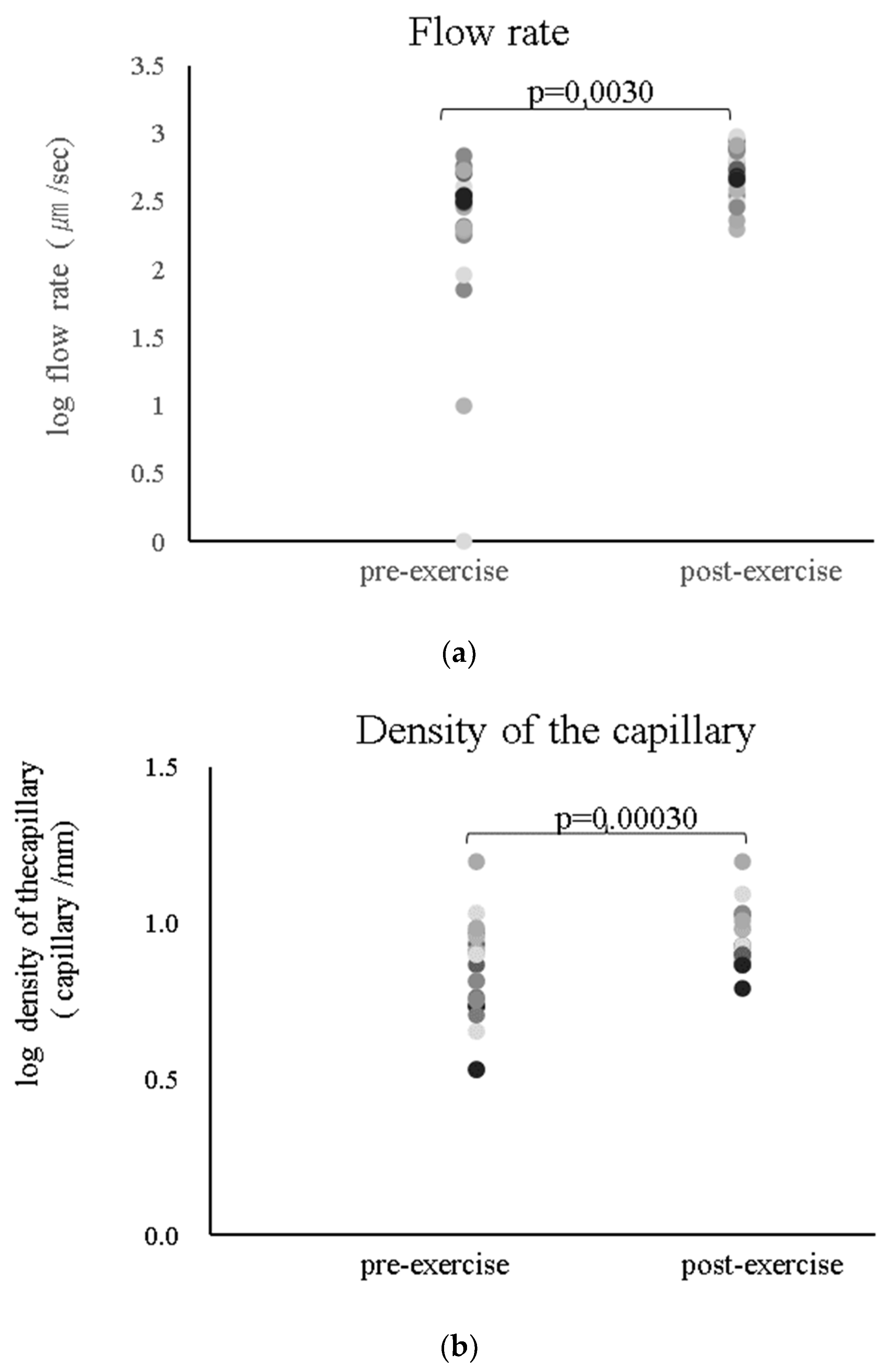
Table 1. As shown in
Figure 4-1, the capillary flow rate significantly changed from 2.3 ± 0.7 to 2.7 ± 0.2 log µm/s (
P = 0.003), and the capillary density significantly changed from 0.8 ± 0.2 to 0.9 ± 0.1 log/mm (0.0003). Nailfold capillary image of baseline and after 1-min exercise of typical subject by the microscope measurement in
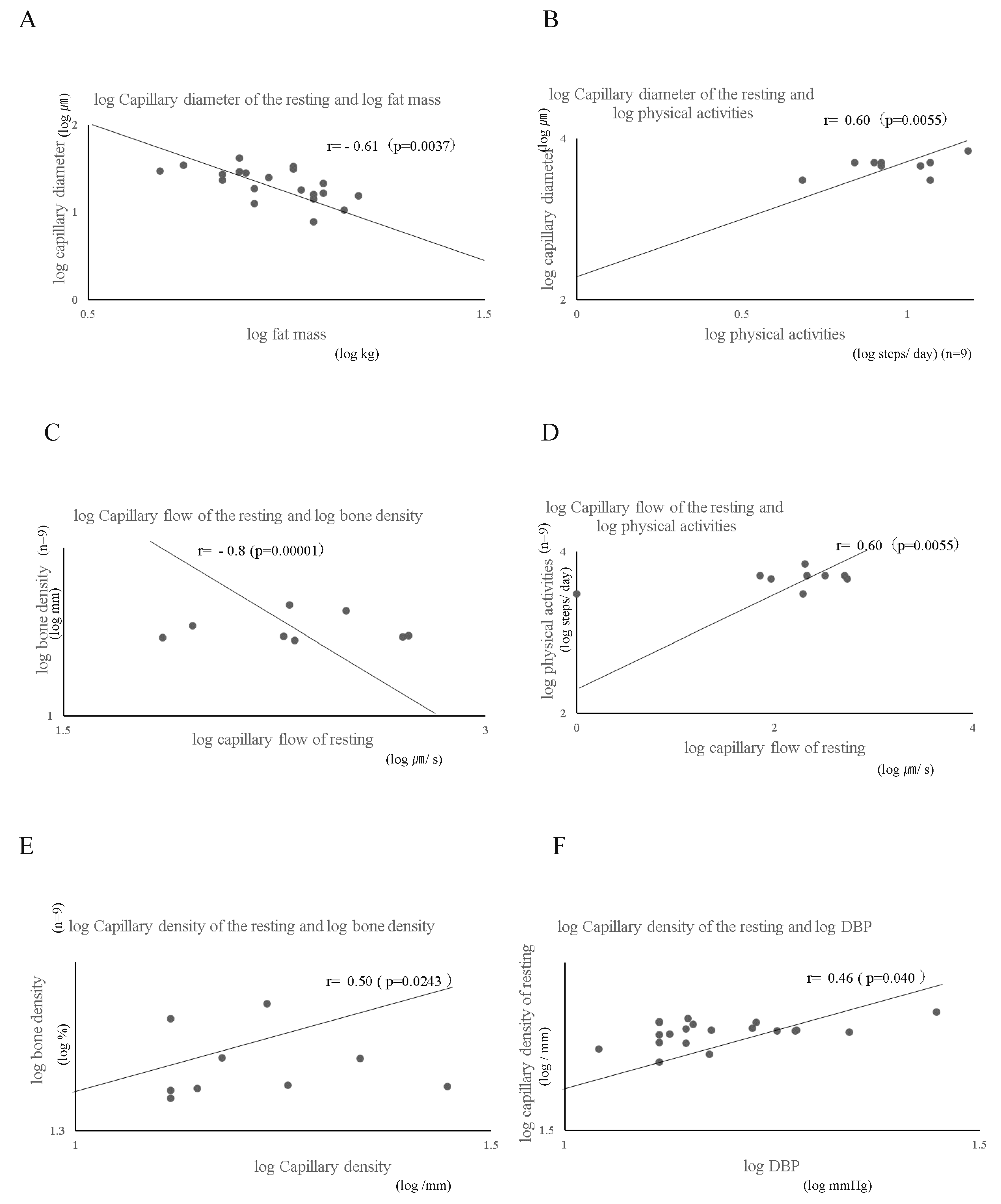
Figure 3-2. In addition, the correlation of nailfold capillary parameter at rest and other parameters is depicted in
Figure 5:
Figure 5A shows that the log capillary diameter at rest is negatively correlated with log fat mass (r = −0.61;
P = 0.0037);
Figure 5B shows that the log capillary diameter at rest is correlated with log physical activities (r = 0.60;
P = 0.0055);
Figure 5C shows that the log capillary flow at rest is negatively correlated with the log BMD (r = −0.8;
P = 0.00001);
Figure 5D shows that the log capillary flow at rest is correlated with the log physical activities (r = 0.60;
P = 0.0055);
Figure 5E shows that the log capillary density at rest is correlated with log BMD (r = 0.50;
P = 0.0243);
Figure 5F shows that the log capillary density is correlated with log DBP (r = 0.46;
P = 0.040);
Figure 5G shows that the log capillary density at rest is negatively correlated with log BMI (r = −0.49;
P = 0.0289); and
Figure 5H shows that the log capillary diameter at rest is correlated with log physical activities (r = 0.65;
P = 0.029). Furthermore, the capillary diameter at rest was significantly multiple regressed with body fat mass and DBP. Moreover, In individuals who exhibited a change in the diameter of the nailfold capillary before and after exercise, a strong correlation of 0.75 was observed between the change in nailfold diameter (Δ nailfold diameter) and body fat mass (p=0.012). Additionally, a moderate correlation of 0.64 was observed between age and systolic blood pressure (SBP) (p=0.044).
On the other hand, in individuals who did not show a change or exhibited a decrease in the diameter before and after exercise, a strong negative correlation of -0.71 was observed between age and the change in flow of the nailfold capillary (Δ flow) (p=0.021). A strong correlation of 0.95 was observed between the change in nailfold capillary flow (Δ nailfold flow) and physical activity (p=0.000020). Furthermore, a strong negative correlation of -0.76 was observed between body fat mass and physical activities (p=0.010).
Correlation between the capillary parameters at rest and other health-related parameters
Graph A shows that the log capillary diameter at rest is significantly correlated with log fat mass (r = −0.61; P = 0.0037). Graph B shows that the log capillary diameter at rest is significantly correlated with log physical activities (r = 0.60; P = 0.0055). Graph C shows that the log capillary flow at rest is significantly correlated with log bone density (r = −0.80; P = 0.00001). Graph D shows that the log capillary flow at rest is significantly correlated with log bone density (r = 0.60; P = 0.0055). Graph E shows that the log capillary density at rest is significantly correlated with log bone density (r = 0.50; P = 0.024). Graph F shows that the log capillary density at rest is significantly correlated with log DBP (r = 0.46; P = 0.040). Graph G shows that the log capillary diameter at rest is significantly correlated with log BMI (r = −0.49; P = 0.029). Graph H shows that log age is significantly correlated with log bone density (r = 0.50; P = 0.024)
4. Discussion
Exercise and drug therapy have been reported to be effective for dysfunctional vessels during recanalization. However, excessive response of the sympathetic nervous system to exercise may increase the risk of cardiovascular events [
13]. Furthermore, whether local and acute exercises affect the capillaries remain unclear. It is crucial to explore the acute effects of exercise on high-risk elderly individuals. Therefore, this study included elderly individuals aged over 60 years who do not exercise regularly. The function of the capillaries on the non-exercising limb before and after a 1-min moderate-intensity exercise was measured. To the best of our knowledge, this is the first study to examine the immediate effects of exercise on peripheral circulation and the safety of exercise for elderly individuals with hypertension. Furthermore, it investigated the correlation between capillary function and other health-related indicators. As a result of this study, all protocols could be safely implemented. It was suggested that even a 1-min exercise could safely and effectively improve peripheral circulation, even on the non-exercising limb. The capillary examination parameters were adopted in the medical guidelines [
14] and can be improved by medication and lifestyle habits. It has been demonstrated that the capillary parameters were related to other health-related indicators. In this study, a significant change was observed in the dysfunctional vessels of the non-exercising limb before and after a 1-min exercise, which could be attributed to two reasons: First, the arm-curl exercise induced systemic circulation. Although it was against the principle of specificity in the principles of exercise therapy, which was because it was not skeletal muscle but the whole body’s microcirculation. Second, the capillary diameter did not significantly change. This is because the subjects were elderly individuals with hypertension, and their capillary function had declined due to aging. That was because no change was observed in the capillary diameter. Capillaries exist throughout the body and are involved in the transport of nutrients to cells, which is why a correlation with health-related indicators was observed. In recent years, it has been reported that ectopic fat decline functions in various organs of the body [
15]. A recent study has demonstrated an inverse correlation between body fat mass and capillary diameter. Therefore, it is essential to reduce body fat through continuous exercise therapy. However, exercise therapy can trigger cardiovascular events in high-risk elderly individuals; thus, this therapy is difficult to implement continuously. In addition, the rapid activation of the sympathetic nervous system at the start of exercise increases the risk of cardiovascular events in this population, but results from this study, safely and effectively even for the high-risk elderly. The main reason in this study was moderate intensity. This study demonstrated not only the acute effects of exercise but also its long-term effects, such as improved capillary function, formation, and density [
16]. Consequently, it is considered essential to establish regular exercise habits. The results of this study indicated that for patients with hemiplegia or plaster fixation, which causes them to be inactive, exercising healthy local limbs can positively affect the non-exercising limbs. This study has some limitations. First, the sample size was small because the study focused on a single center. Second, the participants did not exhibit long-term effects of exercise. Consequently, it is necessary to increase the sample size and extend the intervention period in future studies.
5. Conclusions
In this study, community-dwelling elderly individuals with hypertension safely performed a 1-min exercise without experiencing serious adverse events and the capillary impact whole body function. Therefore, it may be a useful diagnostic tool to assess nailfold capillary.
Author Contributions
Conceptualization, MISA Miura; Data curation, Chie Saito and Osamu Ito; Investigation, Hisashi Sugaya, Shingo Koyama and Yasushi Matsui; Methodology, Chie Saito, Satoshi Sakai and Tohru Sakuma; Supervision, Masahiro Kohzuki, Osamu Ito and Kunihiro Yamagata; Writing – original draft, MISA Miura; Writing – review & editing, Masahiro Kohzuki, Chie Saito, Satoshi Sakai, Hisashi Sugaya and Kunihiro Yamagata.
Funding
Misa Miura is currently receiving grants (21K11189, 23H03249) from JSPS KAKENHI.
Institutional Review Board Statement
The trial was registered at Japan registry of clinical trials under 2204 and was the ethics committee (Review Board of Tsukuba University of Technology). It was conducted in accordance with the Declaration of Helsinki.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
The authors thank all participants who volunteered for this study. The authors thank Keiji Kawagoe for his technical assistance.
Declaration of Conflicting Interests
All authors declare that there are no conflicts of interest.
Research Ethics and Patient Consent
Informed consent was obtained from all subjects involved in the study.
References
- Feihl, F.; Liaudet, L.; Waeber, B. The macrocirculation and microcirculation of hypertension. Curr. Hypertens. Rep. 2009, 11, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Serné, E.H.; Gans, R.O.; ter Maaten, J.C.; ter Wee, P.M.; Donker, A.J.; Stehouwer, C.D. Capillary recruitment is impaired in essential hypertension and relates to insulin's metabolic and vascular actions. Cardiovasc. Res. 2001, 49, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Jorneskog, G.; Brismar, K.; Fagrell, B. Skin capillary circulation severely impaired in toes of patients with IDDM, with and without late diabetic complications. Diabetologia 1995, 38, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Holowatz, L.A.; Thompson-Torgerson, C.S.; Kenney, W.L. The human cutaneous circulation as a model of generalized microvascular function. Journal of applied physiology (Bethesda, Md: 1985) 2008, 105, 370–372. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; Marciniak, M.; Markandu, N.D.; Antonios, T.F.; MacGregor, G.A. Effect of Modest Salt Reduction on Skin Capillary Rarefaction in White, Black, and Asian Individuals With Mild Hypertension. Hypertension 2010, 56, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Pescatello LS and Medicine ACoS. ACSM’s Guidelines for Exercise Testing and Prescription. Wolters Kluwer Health, 2014.
- McGuigan, M.R.M.; Bronks, R.; Newton, R.U.; Sharman, M.J.; Graham, J.C.; Cody, D.V.; Kraemer, W.J. Resistance Training in Patients With Peripheral Arterial Disease: Effects on Myosin Isoforms, Fiber Type Distribution, and Capillary Supply to Skeletal Muscle. Journals Gerontol. Ser. A 2001, 56, B302–B310. [Google Scholar] [CrossRef]
- Simms, A.-G.; Parrino, R.; Gameiro, G.R.; Cipolla, J.; Wang, J.; Jiang, H.; Signorile, J.F. Decreased retinal capillary density as a beneficial response to 24-week high-speed circuit resistant training in healthy older adults. Microvasc. Res. 2024, 153, 104668. [Google Scholar] [CrossRef] [PubMed]
- Yin, H.; Wu, Z.; Huang, A.; Luo, J.; Liang, J.; Lin, J.; Ye, Q.; Xie, M.; Ye, C.; Li, X.; et al. Automated nailfold capillary density measurement method based on improved YOLOv5. Microvasc. Res. 2023, 150, 104593. [Google Scholar] [CrossRef] [PubMed]
- Homma, M.; Miura, M.; Hirayama, Y.; Takahashi, T.; Miura, T.; Yoshida, N.; Miyata, S.; Kohzuki, M.; Ebihara, S. Belt Electrode-Skeletal Muscle Electrical Stimulation in Older Hemodialysis Patients with Reduced Physical Activity: A Randomized Controlled Pilot Study. J. Clin. Med. 2022, 11, 6170. [Google Scholar] [CrossRef] [PubMed]
- Boyaci, F.; Akcay, M.; Hatem, E.; Yanik, A.; Gokdeniz, T.; Cardiology, M.C.H.C.O. Assessment of Arterial Stiffness with Cardio-Ankle Vascular Index in Patients with Mitral Annular Calcification. Eurasian J. Med. 2021, 53, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Métrailler, A.; Hans, D.; Lamy, O.; Gonzalez Rodriguez, E.; Shevroja, E. Heel quantitative ultrasound (QUS) predicts incident fractures independently of trabecular bone score (TBS), bone mineral density (BMD), and FRAX: the OsteoLaus Study. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 2023, 34, 1401–1409. [Google Scholar] [CrossRef] [PubMed]
- Shoji, M.K.; Cousins, C.C.; Saini, C.; e Silva, R.N.; Wang, M.; Brauner, S.C.; Greenstein, S.H.; Pasquale, L.R.; Shen, L.Q. Paired Optic Nerve Microvasculature and Nailfold Capillary Measurements in Primary Open-Angle Glaucoma. Transl. Vis. Sci. Technol. 2021, 10, 13–13. [Google Scholar] [CrossRef] [PubMed]
- Abularrage, C.J.; Sidawy, A.N.; Aidinian, G.; Singh, N.; Weiswasser, J.M.; Arora, S. Evaluation of the microcirculation in vascular disease. J. Vasc. Surg. 2005, 42, 574–581. [Google Scholar] [CrossRef]
- Aldahhan, R.A.; Motawei, K.H.; Al-Hariri, M.T. Lipotoxicity-related sarcopenia: a review. J. Med. Life 2023, 15, 1334–1339. [Google Scholar] [CrossRef]
- Hoier, B.; Hellsten, Y. Exercise-Induced Capillary Growth in Human Skeletal Muscle and the Dynamics of VEGF. Microcirculation 2014, 21, 301–314. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).