Submitted:
18 April 2024
Posted:
19 April 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Application of Diagnostic Radiopharmaceuticals in Oncology
3. Assessing HER2 Status in Cancer Patients by Molecular Imaging
4. Clinical Experience of HER2-Affibody Molecular Imaging in HER2-Positive Breast Cancer Patients
| Affibody ligand | HER2 status | Radioisotope (PET/SPECT) | Number of patients | Reference |
|---|---|---|---|---|
| ABY-002 | pos | 111In (SPECT); 68Ga (PET) | 3 | Baum J Nucl Med 2010 [46] |
| ABY-025 | pos/neg | 111In (SPECT) | 7 | Sörensen J Nucl Med 2014; Sandberg Eur J Nucl Med Mol Imaging 2017 [47,49] |
| ABY-025 | pos/neg | 68Ga (PET) | 16 | Sörensen Theranostics 2016; Sandberg Eur J Nucl Med Mol Imaging 2017; Sandström J Nucl Med 2016 [41,49,50] |
| NOTA-Mal-Cys-MZHer342 | pos/neg | 68Ga (PET) | 2 | Xu Br J Radiol 2019 [51] |
| HEHEHE-ZHER2-GGGC | pos | 99mTc (SPECT) | 30 | Cai Iran J Radiol 2020 [52] |
| NOTA-Mal-Cys-MZHer342 | pos/neg | 68Ga (PET) | 24 | Miao Front Oncol 2022 [53] |
| GE-226 | pos | 18F (PET) | 20 | Kenny JCO 2022 (abstract) [54] |
| RESCA-HER2-BCH / NOTA-HER2-BCH | pos/neg | 18F (PET) | 5 | Liu EJNMMI 2023 [55] |
| ABY-025 | pos | 68Ga (PET) | 40 | Alhuseinalkhudhur J Nucl Med 2023 [48] |
| ABY-025 | low | 68Ga (PET) | 10 | Altena J Nucl Med 2024 [56] |
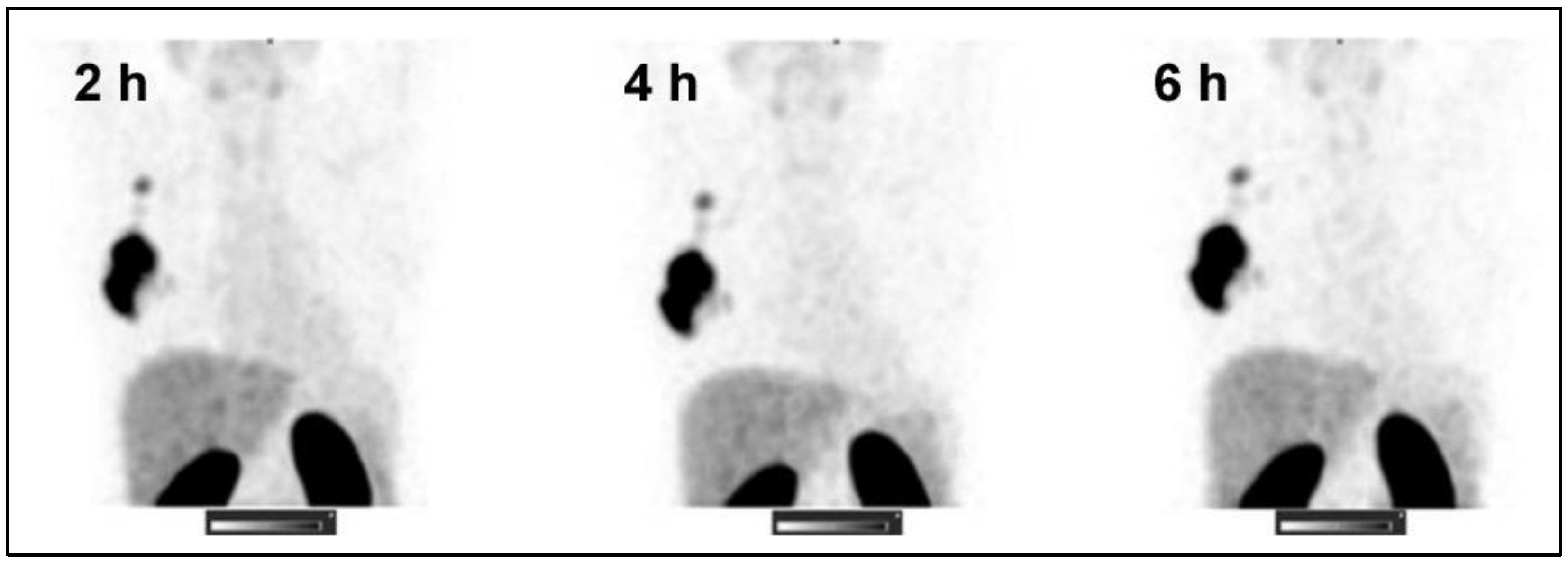
| ZHER2:41071 | pos/neg | 99mTc (SPECT) | 31 | Bragina Theranostics 2023 [57] |
5. Clinical Experience of HER2-Affibody PET Imaging in HER2-Low Breast Cancer Patients
6. SPECT Alternative for HER2-Affibody Imaging
7. Affibody-Based HER2 Imaging Outside Breast Cancer
| Affibody ligand | HER2 status | Radioisotope (PET/SPECT) | Number of patients | Reference |
|---|---|---|---|---|
| NOTA-Mal-Cys-MZHer342 | pos/ neg | 68Ga (PET) | 34 | Zhou EJNMMI 2021 [71] |
| NOTA-Mal-Cys-MZHer342 | pos | 68Ga (PET) | 1 | Zhou Clin Nucl Med 2020 [72] |
| ABY-025 | all | 68Ga (PET) | TBD | NCT05619016 (ongoing) |
8. Future Directions
9. Conclusions
Acknowledgments
References
- Schettini, F.; Chic, N.; Braso-Maristany, F.; Pare, L.; Pascual, T.; Conte, B.; Martinez-Saez, O.; Adamo, B.; Vidal, M.; Barnadas, E. Clinical, pathological, and PAM50 gene expression features of HER2-low breast cancer. NPJ Breast Cancer 2021, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Slamon, D.J.; Clark, G.M.; Wong, S.G.; Levin, W.J.; Ullrich, A.; McGuire, W.L. Human breast cancer: Correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 1987, 235, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Cronin, K.A.; Harlan, L.C.; Dodd, K.W.; Abrams, J.S.; Ballard-Barbash, R. Population-based estimate of the prevalence of HER-2 positive breast cancer tumors for early stage patients in the US. Cancer Invest 2010, 28, 963–968. [Google Scholar] [CrossRef] [PubMed]
- Yan, M.; Schwaederle, M.; Arguello, D.; Millis, S.Z.; Gatalica, Z.; Kurzrock, R. HER2 expression status in diverse cancers: Review of results from 37,992 patients. Cancer Metastasis Rev 2015, 34, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Harries, M.; Smith, I. The development and clinical use of trastuzumab (Herceptin). Endocr Relat Cancer 2002, 9, 75–85. [Google Scholar] [CrossRef]
- Swain, S.M.; Shastry, M.; Hamilton, E. Targeting HER2-positive breast cancer: Advances and future directions. Nat Rev Drug Discov 2023, 22, 101–126. [Google Scholar] [CrossRef]
- Kunte, S.; Abraham, J.; Montero, A.J. Novel HER2-targeted therapies for HER2-positive metastatic breast cancer. Cancer 2020, 126, 4278–4288. [Google Scholar] [CrossRef] [PubMed]
- Meric-Bernstam, F.; Johnson, A.M.; Dumbrava, E.E.I.; Raghav, K.; Balaji, K.; Bhatt, M.; Murthy, R.K.; Rodon, J.; Piha-Paul, S.A. Advances in HER2-Targeted Therapy: Novel Agents and Opportunities Beyond Breast and Gastric Cancer. Clin Cancer Res 2019, 25, 2033–2041. [Google Scholar] [CrossRef] [PubMed]
- Modi, S.; Jacot, W.; Yamashita, T.; Sohn, J.; Vidal, M.; Tokunaga, E.; Tsurutani, J.; Ueno, N.T.; Prat, A.; Chae, Y.S.; et al. Trastuzumab Deruxtecan in Previously Treated HER2-Low Advanced Breast Cancer. N Engl J Med 2022, 387, 9–20. [Google Scholar] [CrossRef]
- Indini, A.; Rijavec, E.; Grossi, F. Trastuzumab Deruxtecan: Changing the Destiny of HER2 Expressing Solid Tumors. Int J Mol Sci 2021, 22. [Google Scholar] [CrossRef]
- Gutierrez, C.; Schiff, R. HER2: Biology, detection, and clinical implications. Arch Pathol Lab Med 2011, 135, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Grassini, D.; Cascardi, E.; Sarotto, I.; Annaratone, L.; Sapino, A.; Berrino, E.; Marchio, C. Unusual Patterns of HER2 Expression in Breast Cancer: Insights and Perspectives. Pathobiology 2022, 89, 278–296. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Seo, A.N.; Kim, E.J.; Jang, M.H.; Suh, K.J.; Ryu, H.S.; Kim, Y.J.; Kim, J.H.; Im, S.A.; Gong, G.; et al. HER2 heterogeneity affects trastuzumab responses and survival in patients with HER2-positive metastatic breast cancer. Am J Clin Pathol 2014, 142, 755–766. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.; Nitta, H.; Li, Z. HER2 Intratumoral Heterogeneity in Breast Cancer, an Evolving Concept. Cancers (Basel) 2023, 15, 2664. [Google Scholar] [CrossRef] [PubMed]
- Lindstrom, L.S.; Karlsson, E.; Wilking, U.M.; Johansson, U.; Hartman, J.; Lidbrink, E.K.; Hatschek, T.; Skoog, L.; Bergh, J. Clinically used breast cancer markers such as estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 are unstable throughout tumor progression. J Clin Oncol 2012, 30, 2601–2608. [Google Scholar] [CrossRef] [PubMed]
- Giugliano, F.; Carnevale Schianca, A.; Corti, C.; Ivanova, M.; Bianco, N.; Dellapasqua, S.; Criscitiello, C.; Fusco, N.; Curigliano, G.; Munzone, E. Unlocking the Resistance to Anti-HER2 Treatments in Breast Cancer: The Issue of HER2 Spatial Distribution. Cancers (Basel) 2023, 15, 1385. [Google Scholar] [CrossRef] [PubMed]
- Filho, O.M.; Viale, G.; Stein, S.; Trippa, L.; Yardley, D.A.; Mayer, I.A.; Abramson, V.G.; Arteaga, C.L.; Spring, L.M.; Waks, A.G.; et al. Impact of HER2 Heterogeneity on Treatment Response of Early-Stage HER2-Positive Breast Cancer: Phase II Neoadjuvant Clinical Trial of T-DM1 Combined with Pertuzumab. Cancer Discov 2021, 11, 2474–2487. [Google Scholar] [CrossRef] [PubMed]
- Niikura, N.; Tomotaki, A.; Miyata, H.; Iwamoto, T.; Kawai, M.; Anan, K.; Hayashi, N.; Aogi, K.; Ishida, T.; Masuoka, H.; et al. Changes in tumor expression of HER2 and hormone receptors status after neoadjuvant chemotherapy in 21,755 patients from the Japanese breast cancer registry. Ann Oncol 2016, 27, 480–487. [Google Scholar] [CrossRef] [PubMed]
- Bardia, A.; Viale, G. HER2-Low Breast Cancer-Diagnostic Challenges and Opportunities for Insights from Ongoing Studies: A Podcast. Target Oncol 2023, 18, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Almuhaideb, A.; Papathanasiou, N.; Bomanji, J. 18F-FDG PET/CT imaging in oncology. Ann Saudi Med 2011, 31, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Avril, S.; Muzic, R.F., Jr.; Plecha, D.; Traughber, B.J.; Vinayak, S.; Avril, N. (1)(8)F-FDG PET/CT for Monitoring of Treatment Response in Breast Cancer. J Nucl Med 2016, 57 Suppl 1, 34S–39S. [Google Scholar] [CrossRef]
- Perez-Garcia, J.M.; Gebhart, G.; Ruiz Borrego, M.; Stradella, A.; Bermejo, B.; Schmid, P.; Marme, F.; Escriva-de-Romani, S.; Calvo, L.; Ribelles, N.; et al. Chemotherapy de-escalation using an (18)F-FDG-PET-based pathological response-adapted strategy in patients with HER2-positive early breast cancer (PHERGain): A multicentre, randomised, open-label, non-comparative, phase 2 trial. Lancet Oncol 2021, 22, 858–871. [Google Scholar] [CrossRef] [PubMed]
- Mettler, F.A.J.; Guiberteau, M.J. Essentials of Nuclear Medicine and Molecular Imaging, 7th Edition. Elsevier 2019. [Google Scholar] [CrossRef]
- Bodei, L.; Herrmann, K.; Schoder, H.; Scott, A.M.; Lewis, J.S. Radiotheranostics in oncology: Current challenges and emerging opportunities. Nat Rev Clin Oncol 2022, 19, 534–550. [Google Scholar] [CrossRef] [PubMed]
- Yoon, K.H.; Park, Y.; Kang, E.; Kim, E.K.; Kim, J.H.; Kim, S.H.; Suh, K.J.; Kim, S.M.; Jang, M.; Yun, B.; et al. Effect of Estrogen Receptor Expression Level and Hormonal Therapy on Prognosis of Early Breast Cancer. Cancer Res Treat 2022, 54, 1081–1090. [Google Scholar] [CrossRef] [PubMed]
- Dunnwald, L.K.; Rossing, M.A.; Li, C.I. Hormone receptor status, tumor characteristics, and prognosis: A prospective cohort of breast cancer patients. Breast Cancer Res 2007, 9, R6. [Google Scholar] [CrossRef] [PubMed]
- van Geel, J.J.L.; Boers, J.; Elias, S.G.; Glaudemans, A.; de Vries, E.F.J.; Hospers, G.A.P.; van Kruchten, M.; Kuip, E.J.M.; Jager, A.; Menke-van der Houven van Oordt, W.C.; et al. Clinical Validity of 16alpha-[(18)F]Fluoro-17beta-Estradiol Positron Emission Tomography/Computed Tomography to Assess Estrogen Receptor Status in Newly Diagnosed Metastatic Breast Cancer. J Clin Oncol 2022, 40, 3642–3652. [Google Scholar] [CrossRef] [PubMed]
- Mortimer, J.E.; Bading, J.R.; Frankel, P.H.; Carroll, M.I.; Yuan, Y.; Park, J.M.; Tumyan, L.; Gidwaney, N.; Poku, E.K.; Shively, J.E.; et al. Use of (64)Cu-DOTA-Trastuzumab PET to Predict Response and Outcome of Patients Receiving Trastuzumab Emtansine for Metastatic Breast Cancer: A Pilot Study. J Nucl Med 2022, 63, 1145–1148. [Google Scholar] [CrossRef] [PubMed]
- Gebhart, G.; Lamberts, L.E.; Wimana, Z.; Garcia, C.; Emonts, P.; Ameye, L.; Stroobants, S.; Huizing, M.; Aftimos, P.; Tol, J.; et al. Molecular imaging as a tool to investigate heterogeneity of advanced HER2-positive breast cancer and to predict patient outcome under trastuzumab emtansine (T-DM1): The ZEPHIR trial. Ann Oncol 2016, 27, 619–624. [Google Scholar] [CrossRef] [PubMed]
- Ulaner, G.A.; Hyman, D.M.; Lyashchenko, S.K.; Lewis, J.S.; Carrasquillo, J.A. 89Zr-Trastuzumab PET/CT for Detection of Human Epidermal Growth Factor Receptor 2-Positive Metastases in Patients With Human Epidermal Growth Factor Receptor 2-Negative Primary Breast Cancer. Clin Nucl Med 2017, 42, 912–917. [Google Scholar] [CrossRef] [PubMed]
- Ulaner, G.A.; Hyman, D.M.; Ross, D.S.; Corben, A.; Chandarlapaty, S.; Goldfarb, S.; McArthur, H.; Erinjeri, J.P.; Solomon, S.B.; Kolb, H.; et al. Detection of HER2-Positive Metastases in Patients with HER2-Negative Primary Breast Cancer Using 89Zr-Trastuzumab PET/CT. J Nucl Med 2016, 57, 1523–1528. [Google Scholar] [CrossRef] [PubMed]
- Ge, S.; Li, J.; Yu, Y.; Chen, Z.; Yang, Y.; Zhu, L.; Sang, S.; Deng, S. Review: Radionuclide Molecular Imaging Targeting HER2 in Breast Cancer with a Focus on Molecular Probes into Clinical Trials and Small Peptides. Molecules 2021, 26, 6482. [Google Scholar] [CrossRef] [PubMed]
- Altena, R.; Tzortzakakis, A.; Af Buren, S.; Tran, T.A.; Frejd, F.Y.; Bergh, J.; Axelsson, R. Current status of contemporary diagnostic radiotracers in the management of breast cancer: First steps toward theranostic applications. EJNMMI Res 2023, 13, 43. [Google Scholar] [CrossRef] [PubMed]
- Tolmachev, V.; Orlova, A.; Sorensen, J. The emerging role of radionuclide molecular imaging of HER2 expression in breast cancer. Semin Cancer Biol 2021, 72, 185–197. [Google Scholar] [CrossRef] [PubMed]
- Mileva, M.; de Vries, E.G.E.; Guiot, T.; Wimana, Z.; Deleu, A.L.; Schroder, C.P.; Lefebvre, Y.; Paesmans, M.; Stroobants, S.; Huizing, M.; et al. Molecular imaging predicts lack of T-DM1 response in advanced HER2-positive breast cancer (final results of ZEPHIR trial). NPJ Breast Cancer 2024, 10, 4. [Google Scholar] [CrossRef] [PubMed]
- Tolmachev, V.; Vorobyeva, A. Radionuclides in Diagnostics and Therapy of Malignant Tumors: New Development. Cancers (Basel) 2022, 14, 297. [Google Scholar] [CrossRef]
- Keyaerts, M.; Xavier, C.; Heemskerk, J.; Devoogdt, N.; Everaert, H.; Ackaert, C.; Vanhoeij, M.; Duhoux, F.P.; Gevaert, T.; Simon, P.; et al. Phase I Study of 68Ga-HER2-Nanobody for PET/CT Assessment of HER2 Expression in Breast Carcinoma. J Nucl Med 2016, 57, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Graff, C.P.; Wittrup, K.D. Theoretical analysis of antibody targeting of tumor spheroids: Importance of dosage for penetration, and affinity for retention. Cancer Res 2003, 63, 1288–1296. [Google Scholar] [PubMed]
- Stahl, S.; Graslund, T.; Eriksson Karlstrom, A.; Frejd, F.Y.; Nygren, P.A.; Lofblom, J. Affibody Molecules in Biotechnological and Medical Applications. Trends Biotechnol 2017, 35, 691–712. [Google Scholar] [CrossRef]
- Tolmachev, V.; Orlova, A. Affibody Molecules as Targeting Vectors for PET Imaging. Cancers (Basel) 2020, 12, 651. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, J.; Velikyan, I.; Sandberg, D.; Wennborg, A.; Feldwisch, J.; Tolmachev, V.; Orlova, A.; Sandstrom, M.; Lubberink, M.; Olofsson, H.; et al. Measuring HER2-Receptor Expression In Metastatic Breast Cancer Using [68Ga]ABY-025 Affibody PET/CT. Theranostics 2016, 6, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Samkoe, K.S.; Sardar, H.S.; Gunn, J.; Feldwisch, J.; Linos, K.; Henderson, E.; Pogue, B.; Paulsen, K. Measuring microdose ABY-029 fluorescence signal in a primary human soft-tissue sarcoma resection. Proc SPIE Int Soc Opt Eng 2019, 10862. [Google Scholar] [CrossRef] [PubMed]
- Klint, S.; Feldwisch, J.; Gudmundsdotter, L.; Dillner Bergstedt, K.; Gunneriusson, E.; Hoiden Guthenberg, I.; Wennborg, A.; Nyborg, A.C.; Kamboj, A.P.; Peloso, P.M.; et al. Izokibep: Preclinical development and first-in-human study of a novel IL-17A neutralizing Affibody molecule in patients with plaque psoriasis. MAbs 2023, 15, 2209920. [Google Scholar] [CrossRef] [PubMed]
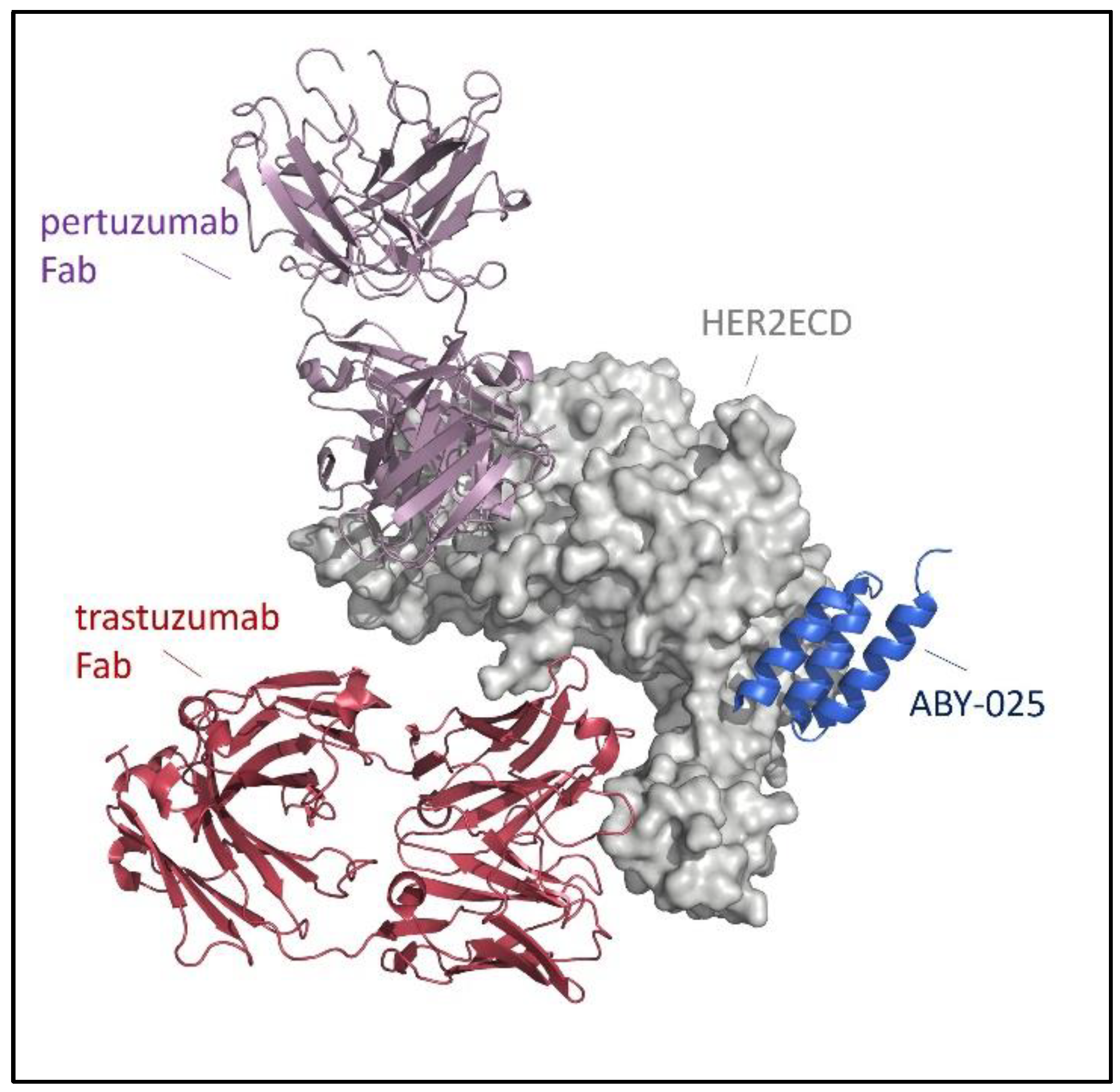
- Eigenbrot, C.; Ultsch, M.; Dubnovitsky, A.; Abrahmsen, L.; Hard, T. Structural basis for high-affinity HER2 receptor binding by an engineered protein. Proc Natl Acad Sci U S A 2010, 107, 15039–15044. [Google Scholar] [CrossRef] [PubMed]
- Feldwisch, J.; Tolmachev, V.; Lendel, C.; Herne, N.; Sjoberg, A.; Larsson, B.; Rosik, D.; Lindqvist, E.; Fant, G.; Hoiden-Guthenberg, I.; et al. Design of an optimized scaffold for affibody molecules. J Mol Biol 2010, 398, 232–247. [Google Scholar] [CrossRef] [PubMed]
- Baum, R.P.; Prasad, V.; Muller, D.; Schuchardt, C.; Orlova, A.; Wennborg, A.; Tolmachev, V.; Feldwisch, J. Molecular imaging of HER2-expressing malignant tumors in breast cancer patients using synthetic 111In- or 68Ga-labeled affibody molecules. J Nucl Med 2010, 51, 892–897. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, J.; Sandberg, D.; Sandstrom, M.; Wennborg, A.; Feldwisch, J.; Tolmachev, V.; Astrom, G.; Lubberink, M.; Garske-Roman, U.; Carlsson, J.; et al. First-in-human molecular imaging of HER2 expression in breast cancer metastases using the 111In-ABY-025 affibody molecule. J Nucl Med 2014, 55, 730–735. [Google Scholar] [CrossRef] [PubMed]
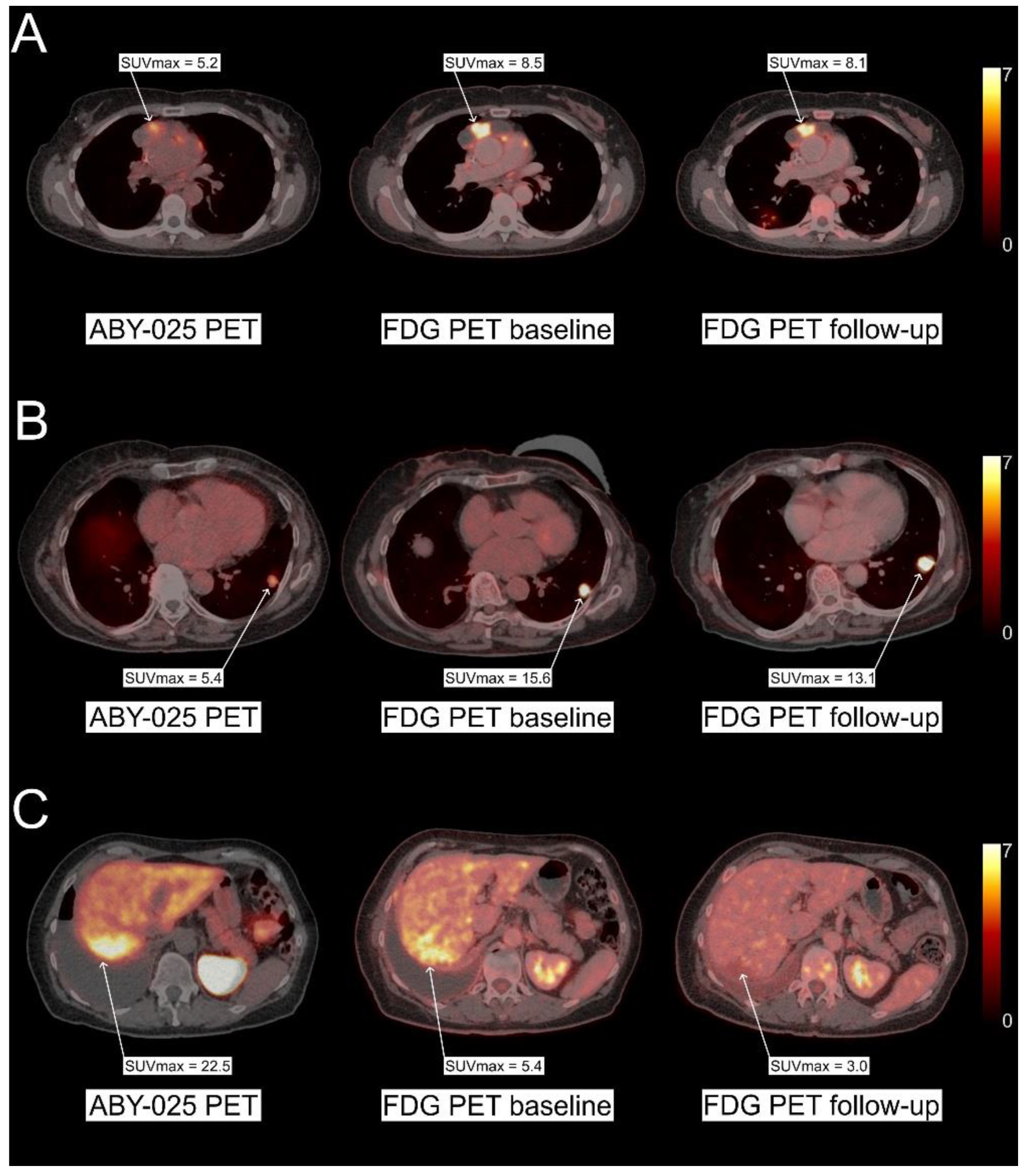
- Alhuseinalkhudhur, A.; Lindman, H.; Liss, P.; Sundin, T.; Frejd, F.Y.; Hartman, J.; Iyer, V.; Feldwisch, J.; Lubberink, M.; Ronnlund, C.; et al. Human Epidermal Growth Factor Receptor 2-Targeting [(68)Ga]Ga-ABY-025 PET/CT Predicts Early Metabolic Response in Metastatic Breast Cancer. J Nucl Med 2023, 64, 1364–1370. [Google Scholar] [CrossRef] [PubMed]
- Sandberg, D.; Tolmachev, V.; Velikyan, I.; Olofsson, H.; Wennborg, A.; Feldwisch, J.; Carlsson, J.; Lindman, H.; Sorensen, J. Intra-image referencing for simplified assessment of HER2-expression in breast cancer metastases using the Affibody molecule ABY-025 with PET and SPECT. Eur J Nucl Med Mol Imaging 2017, 44, 1337–1346. [Google Scholar] [CrossRef] [PubMed]
- Sandstrom, M.; Lindskog, K.; Velikyan, I.; Wennborg, A.; Feldwisch, J.; Sandberg, D.; Tolmachev, V.; Orlova, A.; Sorensen, J.; Carlsson, J.; et al. Biodistribution and Radiation Dosimetry of the Anti-HER2 Affibody Molecule 68Ga-ABY-025 in Breast Cancer Patients. J Nucl Med 2016, 57, 867–871. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Wang, L.; Pan, D.; Yu, C.; Mi, B.; Huang, Q.; Sheng, J.; Yan, J.; Wang, X.; Yang, R.; et al. PET imaging of a (68)Ga labeled modified HER2 affibody in breast cancers: From xenografts to patients. Br J Radiol 2019, 92, 20190425. [Google Scholar] [CrossRef] [PubMed]
- Cai, J.; Li, X.; Mao, F.; Wang, P.; Luo, Y.; Zheng, K.; Li, F.; Zhu, Z. Non-Invasive Monitoring of HER2 Expression in Breast Cancer Patients with 99mTc-Affibody SPECT/CT. Iran J Radiol. 2020. [Google Scholar] [CrossRef]
- Miao, H.; Sun, Y.; Jin, Y.; Hu, X.; Song, S.; Zhang, J. Application of a Novel (68)Ga-HER2 Affibody PET/CT Imaging in Breast Cancer Patients. Front Oncol 2022, 12, 894767. [Google Scholar] [CrossRef]
- Kenny, L.M.; Gilbert, F.J.; Gopalakrishnan, G.; Aravind, P.; Barwick, T.; Patel, N.; Hiscock, D.R.; Boros, I.; Kealey, S.; Aigbirhio, F.I.; et al. The HERPET study: Imaging HER2 expression in breast cancer with the novel PET tracer [18F]GE-226, a first-in-patient study. American Society of Clinical Oncology 2022. [Google Scholar] [CrossRef]
- Liu, J.; Guo, X.; Wen, L.; Wang, L.; Liu, F.; Song, G.; Zhu, H.; Zhou, N.; Yang, Z. Comparison of renal clearance of [(18)F]AlF-RESCA-HER2-BCH and [(18)F]AlF-NOTA-HER2-BCH in mice and breast cancer patients. Eur J Nucl Med Mol Imaging 2023, 50, 2775–2786. [Google Scholar] [CrossRef] [PubMed]
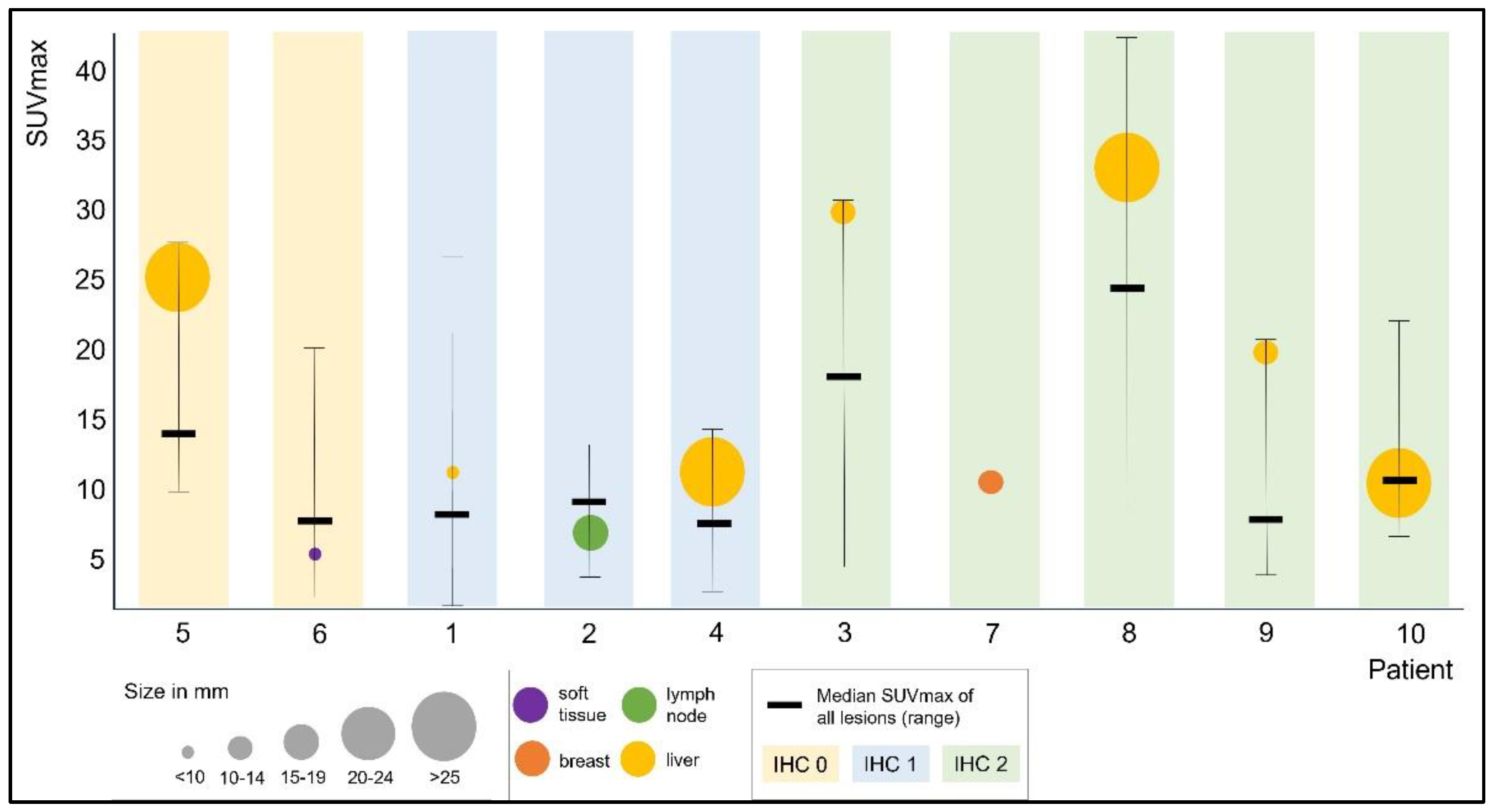
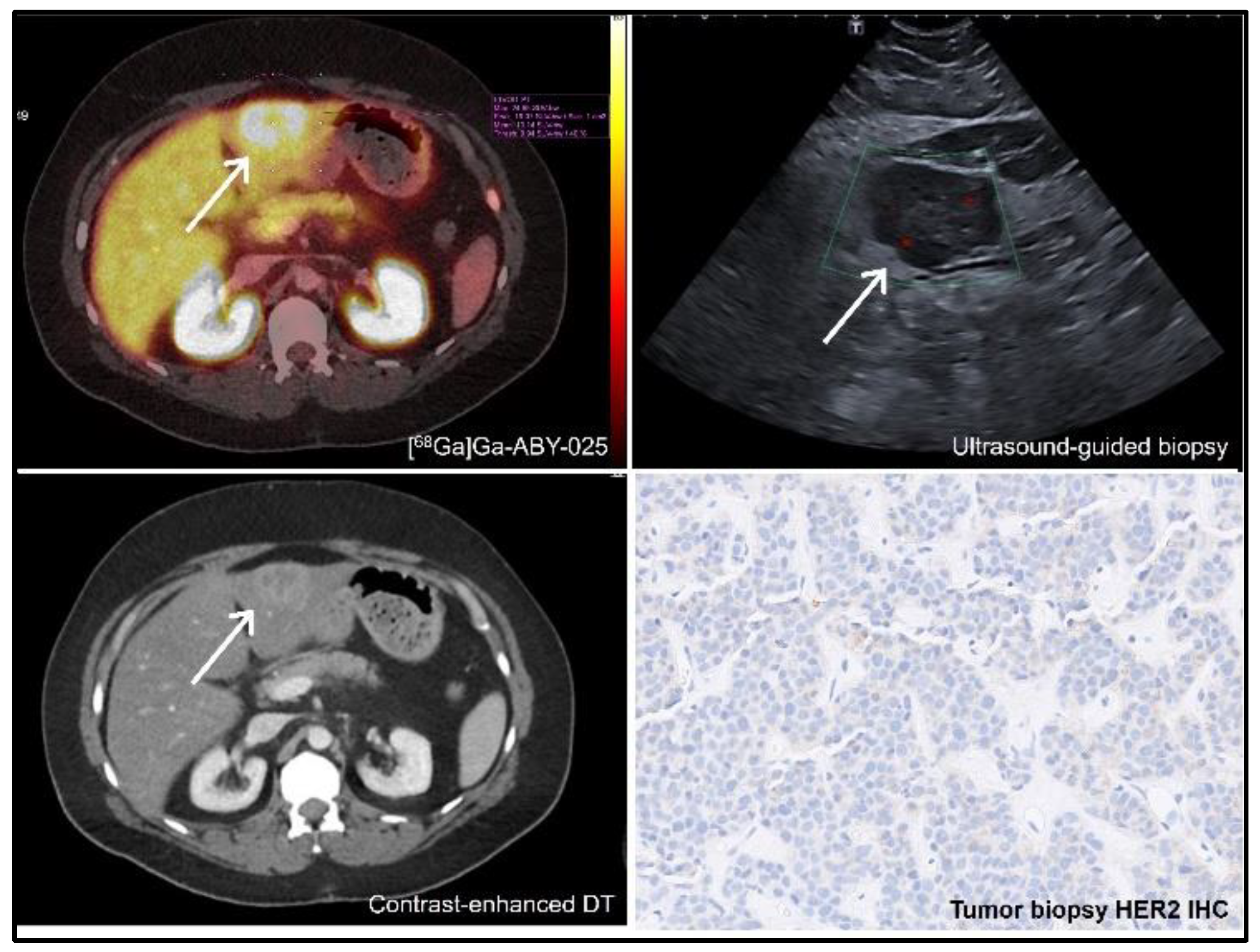
- Altena, R.; Buren, S.A.; Blomgren, A.; Karlsson, E.; Tzortzakakis, A.; Brun, N.; Moein, M.M.; Jussing, E.; Frejd, F.Y.; Bergh, J.; et al. Human Epidermal Growth Factor Receptor 2 (HER2) PET Imaging of HER2-Low Breast Cancer with [(68)Ga]Ga-ABY-025: Results from a Pilot Study. J Nucl Med 2024. [Google Scholar] [CrossRef] [PubMed]
- Chernov, V.; Rybina, A.; Zelchan, R.; Medvedeva, A.; Bragina, O.; Lushnikova, N.; Doroshenko, A.; Usynin, E.; Tashireva, L.; Vtorushin, S.; et al. Phase I Trial of [(99m)Tc]Tc-maSSS-PEG(2)-RM26, a Bombesin Analogue Antagonistic to Gastrin-Releasing Peptide Receptors (GRPRs), for SPECT Imaging of GRPR Expression in Malignant Tumors. Cancers (Basel) 2023, 15, 1631. [Google Scholar] [CrossRef] [PubMed]
- Iveson, P.B.; Glaser, M.; Indrevoll, B.; Shales, J.; Mantzilas, D.; Omtvedt, L.; Luthra, S.K.; Hiscock, D.; Grigg, J. FASTlab Radiosynthesis of the (18) F-labelled HER2-binding Affibody molecule [(18) F]GE-226. J Labelled Comp Radiopharm 2019, 62, 925–932. [Google Scholar] [CrossRef]
- Frija, G.; Blažić, I.; Frush, D.P.; Hierath, M.; Kawookya, M.; Donoso-Bach, L.; Brkljačić, B. How to improve access to medical imaging in low- and middle-income countries ? eClinicalMedicine 2021, 38. [Google Scholar] [CrossRef]
- Hricak, H.; Abdel-Wahab, M.; Atun, R.; Lette, M.M.; Paez, D.; Brink, J.A.; Donoso-Bach, L.; Frija, G.; Hierath, M.; Holmberg, O.; et al. Medical imaging and nuclear medicine: A Lancet Oncology Commission. Lancet Oncol 2021, 22, e136–e172. [Google Scholar] [CrossRef] [PubMed]
- Bragina, O.; Chernov, V.; Larkina, M.; Rybina, A.; Zelchan, R.; Garbukov, E.; Oroujeni, M.; Loftenius, A.; Orlova, A.; Sorensen, J.; et al. Phase I clinical evaluation of (99m)Tc-labeled Affibody molecule for imaging HER2 expression in breast cancer. Theranostics 2023, 13, 4858–4871. [Google Scholar] [CrossRef] [PubMed]
- Gravalos, C.; Jimeno, A. HER2 in gastric cancer: A new prognostic factor and a novel therapeutic target. Ann Oncol 2008, 19, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.L.; He, Y.; Xu, R.H. Gastric cancer treatment: Recent progress and future perspectives. J Hematol Oncol 2023, 16, 57. [Google Scholar] [CrossRef] [PubMed]
- Cabel, L.; Fuerea, A.; Lacroix, L.; Baldini, C.; Martin, P.; Hollebecque, A.; Postel-Vinay, S.; Varga, A.; Balheda, R.; Gazzah, A.; et al. Efficacy of histology-agnostic and molecularly-driven HER2 inhibitors for refractory cancers. Oncotarget 2018, 9, 9741–9750. [Google Scholar] [CrossRef] [PubMed]
- Oh, D.Y.; Bang, Y.J. HER2-targeted therapies - a role beyond breast cancer. Nat Rev Clin Oncol 2020, 17, 33–48. [Google Scholar] [CrossRef] [PubMed]
- Tsurutani, J.; Iwata, H.; Krop, I.; Janne, P.A.; Doi, T.; Takahashi, S.; Park, H.; Redfern, C.; Tamura, K.; Wise-Draper, T.M.; et al. Targeting HER2 with Trastuzumab Deruxtecan: A Dose-Expansion, Phase I Study in Multiple Advanced Solid Tumors. Cancer Discov 2020, 10, 688–701. [Google Scholar] [CrossRef]
- Meric-Bernstam, F.; Makker, V.; Oaknin, A.; Oh, D.Y.; Banerjee, S.N.; Gonzalez Martin, A.; Jung, K.H.; Lugowska, I.A.; Manso, L.; Manzano, A.; et al. Efficacy and safety of trastuzumab deruxtecan (T-DXd) in patients (pts) with HER2-expressing solid tumors: DESTINY-PanTumor02 (DP-02) interim results. American Society of Clinical Oncology 2023. [Google Scholar] [CrossRef]
- Meric-Bernstam, F.; Makker, V.; Oaknin, A.; Oh, D.Y.; Banerjee, S.; Gonzalez-Martin, A.; Jung, K.H.; Lugowska, I.; Manso, L.; Manzano, A.; et al. Efficacy and Safety of Trastuzumab Deruxtecan in Patients With HER2-Expressing Solid Tumors: Primary Results From the DESTINY-PanTumor02 Phase II Trial. J Clin Oncol 2024, 42, 47–58. [Google Scholar] [CrossRef] [PubMed]
- Grillo, F.; Fassan, M.; Sarocchi, F.; Fiocca, R.; Mastracci, L. HER2 heterogeneity in gastric/gastroesophageal cancers: From benchside to practice. World J Gastroenterol 2016, 22, 5879–5887. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Yu, T.; Zhao, Z.; Zhang, S.; Huang, Q.; Liu, G. Temporal heterogeneity of HER2 expression in metastatic gastric cancer: A case report. World J Surg Oncol 2022, 20, 157. [Google Scholar] [CrossRef] [PubMed]
- Zhou, N.; Liu, C.; Guo, X.; Xu, Y.; Gong, J.; Qi, C.; Zhang, X.; Yang, M.; Zhu, H.; Shen, L.; et al. Impact of (68)Ga-NOTA-MAL-MZHER2 PET imaging in advanced gastric cancer patients and therapeutic response monitoring. Eur J Nucl Med Mol Imaging 2021, 48, 161–175. [Google Scholar] [CrossRef] [PubMed]
- Zhou, N.; Guo, X.; Yang, M.; Zhu, H.; Yang, Z. 68Ga-ZHER2 PET/CT Reveals HER2-Positive Metastatic Gastric Cancer With Better Image Quality Than 18F-FDG. Clin Nucl Med 2020, 45, e101–e102. [Google Scholar] [CrossRef] [PubMed]
- Godoy-Ortiz, A.; Alba-Bernal, A.; Pascual, J.; Comino-Mendez, I.; Alba, E. Unveiling the Potential of Liquid Biopsy in HER2-Positive Breast Cancer Management. Cancers (Basel) 2022, 14, 587. [Google Scholar] [CrossRef] [PubMed]
- Taniguchi, H.; Yagisawa, M.; Satoh, T.; Kadowaki, S.; Sunakawa, Y.; Nishina, T.; Komatsu, Y.; Esaki, T.; Sakai, D.; Doi, A.; et al. Tissue-agnostic efficacy of trastuzumab deruxtecan (T-DXd) in advanced solid tumors with HER2 amplification identified by plasma cell-free DNA (cfDNA) testing: Results from a phase 2 basket trial (HERALD/EPOC1806). Journal of Clinical Oncology 2023. [Google Scholar] [CrossRef]
- Massicano, A.V.F.; Marquez-Nostra, B.V.; Lapi, S.E. Targeting HER2 in Nuclear Medicine for Imaging and Therapy. Mol Imaging 2018, 17, 1536012117745386. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Xu, T.; Vorobyeva, A.; Loftenius, A.; Bodenko, V.; Orlova, A.; Frejd, F.Y.; Tolmachev, V. Radionuclide Therapy of HER2-Expressing Xenografts Using [(177)Lu]Lu-ABY-027 Affibody Molecule Alone and in Combination with Trastuzumab. Cancers (Basel) 2023, 15, 2409. [Google Scholar] [CrossRef] [PubMed]
| Name | Drug type | Indication |
|---|---|---|
| trastuzumab (Herceptin®) | mAB | HER2+ BC (adjuvant, metastatic); HER2+ GC (metastatic) |
| pertuzumab (Perjeta®) | mAB | HER2+ BC (metastatic, locally advanced, inflammatory, or early stage) |
| ado-trastuzumab emtansine (Kadcyla®) | ADC | HER2+ BC (metastatic or early stage) |
| trastuzumab deruxtecan (Enhertu®) | ADC | HER2+ BC (unresectable or metastatic); HER2-mutant NSCLC; HER2+ GC and GEJ carcinoma (locally advanced or metastatic); HER2-low BC (metastatic) |
| margetuximab (Margenza®) | mAB | metastatic HER2+ BC |
| tucatinib (TUKYSA®) | TKI | HER2+ BC (locally advanced or metastatic) |
| lapatinib (Tykerb®) | TKI | HER2+ BC (advanced or metastatic; HR+ metastatic) |
| neratinib (NERLYNX®) | TKI | HER2+ BC (early stage or metastatic) |
| Name | approval | Active ingredient(s) | Indication |
|---|---|---|---|
| DetectNETTM | FDA | 64Cu dotatate | SSTR+ neuroendocrine tumors |
| NETSPOT® | FDA | 68Ga dotatate | SSTR+ neuroendocrine tumors |
| SomaKit TOC® | EMA | edotreotide (kit for radiolabeling with gallium-68) | SSTR+ neuroendocrine tumors |
| OctreoscanTM | FDA and EU national approvals | pentetreotide (kit for radiolabeling with indium-111) | SSTR+ neuroendocrine tumors |
| LYMPHOSEEK® | FDA and EMA | tilmanocept (kit for radiolabeling with technetium-99m) | Guiding sentinel lymph node biopsy in cancer patients; locate tumor draining lymph nodes in adults and children. |
| LOCAMETZ® | FDA and EMA | gozetotide (kit for radiolabeling with gallium-68) | PSMA+ prostate cancer |
| Illuccix® | FDA | gozetotide (kit for radiolabeling with gallium-68) | PSMA+ prostate cancer |
| PYLARIFY® / PYLCLARY® | FDA and EMA | piflufolastat F-18 | PSMA+ prostate cancer |
| CeriannaTM * | FDA | fluoroestradiol F-18 | ER+ breast cancer |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





