1. Introduction
Hip fractures are the most frequently treated fractures in the world [
1,
2]. Of these, intertrochanteric fractures (ITFs) account for almost 50% [
3]. After surgical fixation of ITFs, nonunion is rare, because the intertrochanteric region of the femur has an excellent blood supply and good cancellous bone [
4]. Nonunions are commonly produced from mal-reduction (in varus) and/or inadequate stability of the bone-implant construct and/or fatigue failure of the implants. Other causes of nonunion include posteromedial comminution and osteoporosis. The published incidence of ITF nonunion is 1%-2% [
5,
6].
The purpose of this article is to provide a narrative review of the literature on the treatment of intertrochanteric fractures (ITFs) to prevent nonunion. To this end, a literature search was performed in PubMed (MEDLINE) on 1 January 2024, using as keywords: intertrochanteric nonunion (317 results) and pertrochanteric nonunion (55 results). Of the 373 articles reviewed, 30 were ultimately included because we considered that they contained the most important information related to the title of this article. To avoid ITF nonunion, it is essential to have a good understanding of the concepts discussed below.
2. Mechanical Complications Can Be Averted with Stable Fixation in Osteoporotic Bone
As published by Klima in 2022, mechanical complications of ITFs include cut-out, excessive shortening of the proximal femur, delayed union, nonunion, early implant fracture, nail toggle and cut through/medial migration [
7]. That is why a fundamental goal in the treatment of ITFs is to achieve stable fixation in osteoporotic bone, allowing early weight bearing. Intraoperative determination of fracture stability is essential.
The most commonly used implant in the world for ITFs is the Gamma nail. This implant was designed for intramedullary fixation of highly volatile Orthopedic Trauma Association (OTA/AO) type 31-A2/A3 hip fractures [
8]. However, there were some defects that existed in fixation of complex femoral fractures involving the potential secondary rotation of the head-neck fragment followed by collapse at the fracture site and cut-out. That is why Gamma 3 Locking Nail (Stryker GmbH & Co. KG, Duisburg, Germany) was developed with a reduction of the diameter of the nail, a change to the valgus angle from 10 to 4 degrees, a change in the design of the femoral neck screw, and the possibility of dynamization [
9]. The Gamma Nail system provided better clinical results and a higher biomechanical stability compared with older CMNs [
10].
The InterTan Nail (Smith & Nephew GmbH, Marl, Germany), using 2 cephalocervical screws in an integrated mechanism, showed increasing stability and resistance to intra-operative and postoperative femoral head rotation compared with the traditional intramedullary nailing system. A biomechanical study showed that the InterTan Nail possessed more biomechanical benefits for internal fixation of unstable fractures compared with the traditional intramedullary nailing system [
11]. In the study of Ruecker et al. radiographic analysis at healing of 48 cases showed no nonunions (minimum 1 year follow-up, range 12-27 months) [
12].
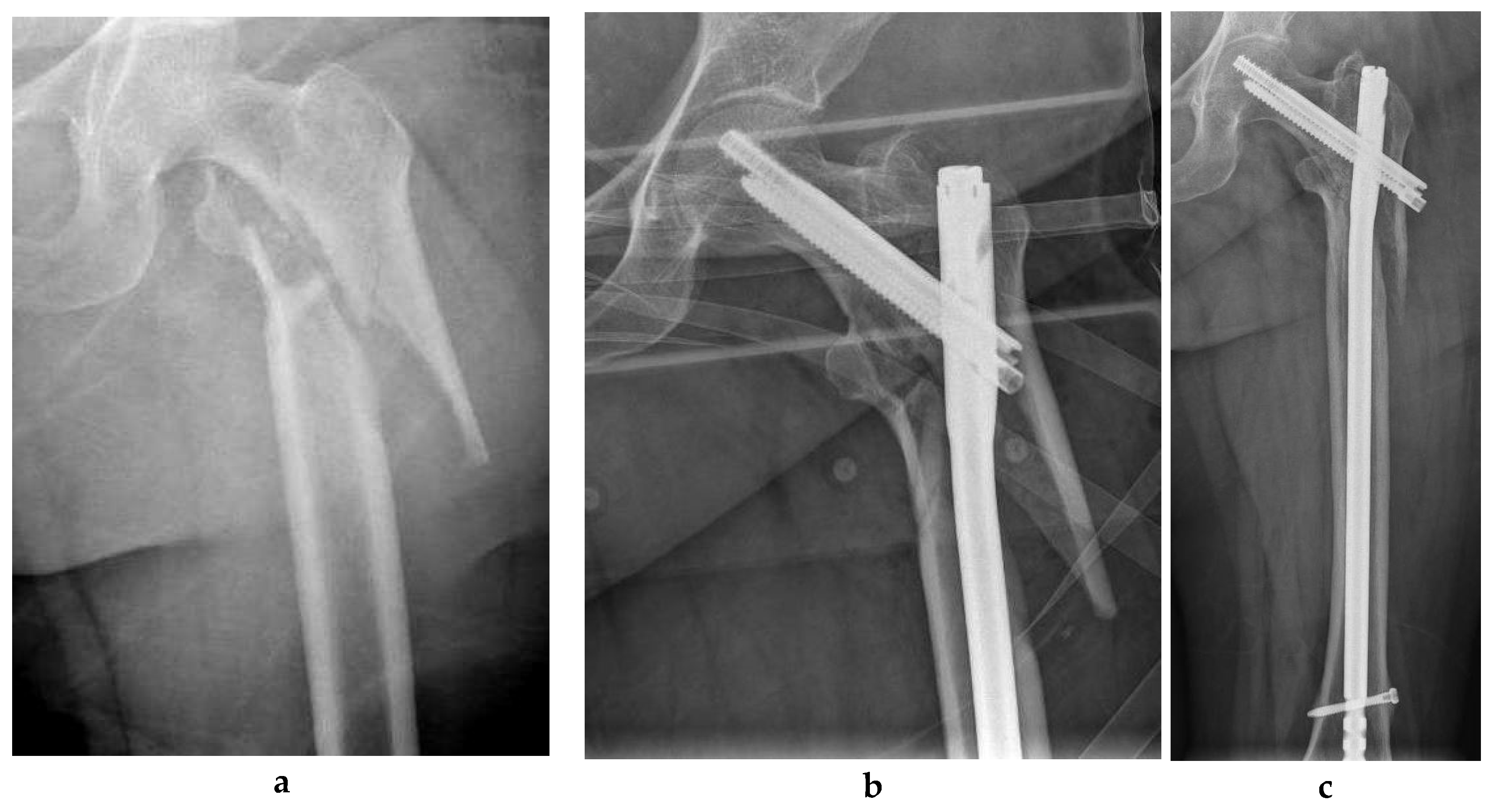
Figure 1 shows an ITF fixed with an InterTan Nail (Smith & Nephew GmbH, Marl, Germany).
In 2014 Wu et al. compared postoperative outcomes and complication rates between the InterTan nail and the Gamma 3 Locking Nail in a non-randomized trial. The incidence of cut-out and femoral shaft fracture was significantly higher in the Gamma3 nail group than the InterTan nail group. Patients treated with the InterTan nail experienced longer fluoroscopy and operative times. The InterTan nail showed a tendency to better outcomes for patients with unstable ITFs [
13].
In 2015 von Rüden et al. reported that mechanical breakage of CMN osteosynthesis was a rare complication attributed to delayed fracture union or non-union. In their study they tried to identify factors that contribute to CMN breakage. The results of this study demonstrated that revision surgery provides good clinical and radiological short-term results. Predominantly, ITF failures were related to poor execution of surgical technique by surgeons [
14].
In 2022, three important articles have been published. Smitz et al. found that failure of fixation increased after a switch from the Gamma Trochanteric Nail (GTN3) to the TFN-Advanced Proximal Femoral Nailing System (TFNA) proximal femoral nail for the treatment of ITFs. Cut-out and mal-positioning of the calcar screw or blade appeared to be the most dominant failure mechanisms. Modifications in implant design may have played a role in this increased risk of failure of fixation [
15].
Goodnough et al. compared the revision risk between the TFNA and its prior-generation forebear, the Trochanteric Fixation Nail (TFN)
(DePuy Synthes
, Synthes, Oberdorf, Switzerland). They found that the TFNA had an overall revision rate that was similar to that of the earlier TFN, with implant breakage being a rare revision reason for both groups. These authors found that the TFNA was associated with a higher risk of revision for non-union (HR, 1.86 [95% CI, 1.11 to 3.12]; p = 0.018). TFNA had an overall revision rate that was similar to that of the earlier TFN, with implant breakage being a rare revision reason for both groups [
16]. Finally Swift et al. compared the Synthes TFN and the Zimmer Natural Nail (ZNN). No differences in rates or modes of failure were identified between the TFN and ZNN constructs [
17].
Figure 2 shows an ITF fixed with a Trochanteric Fixation Nail (TFN)
(DePuy Synthes
, Synthes, Oberdorf, Switzerland).
3. The Importance of Tip-Apex Distance (TAD)
According to Kim et al. proper reduction seems to be important in reducing the risk of cut-out. Maintaining low TAD is another important factor in accomplishing sufficient fixation of lag screw to the subchondral bone of the femoral head [
18]. Other authors have reported that the implant fixation device and the angle of fixation are the most important predictors of TAD. Smaller angle (130° or 125°) fixation devices permit better positioning of the lag screw and consequently better TAD, which leads to a smaller likelihood of implant cutout [
19].
4. Short versus Long Cephalomedullary Nailing (CMN)
In 2022, Cinque et al. compared treatment outcomes after short or long CMN in ITFs in a systematic review and meta-analysis (level 3 of evidence). Short nails were associated with statistically significantly less estimated blood loss and operative time compared to long nails. There were no substantial differences in transfusion percentages, implant failures or overall reoperation percentages between implant lengths. Similarly, there was no substantial difference in peri-implant fracture between implant lengths. Therefore, this study supported the use of short CMN nails for the majority of ITFs [
20].
5. Augmentation of Proximal Femoral Nailing with a Trochanteric Buttress Plate
In 2022, Jain et al. compared the results of lateral wall buttressing by trochanteric buttress plate (TBP) supplementary to proximal femoral nailing (PFN) in patients with broken lateral wall ITFs. The procedure provided faster union. The conclusion was that TBP can be used successfully to augment, fix or buttress the lateral trochanteric wall with good to excellent results, but at the cost of increased operative time, increased blood loss and increased radiation exposure [
21].
6. Reverse Oblique Fracture: Utilization of a Cephalomedullary Nail Diminishes the Nonunion Rate
The OTA/AO type 31 A3 ITF has a transverse or reverse oblique fracture at the level of the lesser trochanter, which increases the varus compressive stress on both the fracture site and the implant [
22]. Therefore, intramedullary fixation with various types of nails is often preferred in these fractures. Hoffmann et al. evaluated 193 ITFs treated with an intramedullary nail in relation to the surgical procedure, its complications and clinical outcomes. This study demonstrated that intramedullary nailing was a reliable surgical technique when an adequate reduction was performed. CMNs were used in 176 and reconstruction nails in 17 individuals. After the procedure, 86% healed uneventfully. Nonunion development was found in 6% and 5% had an unscheduled reoperation due to implant or fixation failure. Active smoking was reported in 16.6%. Current smokers had an increased nonunion risk compared to those who do not currently smoke (15.6% vs. 4.3%; p = 0.016). Varus reduction with a neck-shaft-angle <125° resulted in increased fixation failures. In addition, patient- and implant-related factors affected nonunion formation [
22].
7. Reverse Oblique Fracture: 95º Fixed-Angle Internal Fixation Devices Perform Better than Sliding/Dynamic Hip Screws
In a study forty-seven fractures (49 patients) with a reverse obliquity pattern were followed until the fracture united or a revision operation was carried out. The mean follow-up was 18 months (range, 3 to 60 months). The failure rate was 9 of 16 for the sliding hip screws (SHSs), 2 of 15 for the blade-plates, 3 of 10 for the dynamic condylar screws (DCSs), 1 of 3 for the CMNs, and 0 of 3 for the intramedullary hip screws. Use of the fixed-angle devices (the blade-plate and the DHS) resulted in fewer failures than did use of the SHS (p = 0.023). Fifteen (32%) of the 47 failed to heal or had a failure of fixation. Of the 15 fractures that failed to heal or had a failure of fixation, 5 were treated with revision to a calcar-replacement prosthesis, 7 were treated with revision open reduction and internal fixation (ORIF) with bone-grafting, and 1 was treated with bone-grafting without revision of the fixation. Two patients refused additional surgery because they had limited functional demands [
23].
8. Lateral-Wall High-Risk Type of Intertrochanteric Fractures: Proximal Femoral Nail Anti-Rotation Is More Effective than Sliding/Dynamic Hip Screw
A study compared the efficacy of SHS and proximal femoral nail anti-rotation (PFNA) in the treatment of 98 lateral-wall high-risk types of ITF. Of these, 52 were treated with PFNA and 46 with SHS. In the PFNA group there were 1 delayed union and 1 nonunion, while in the SHS group there were 3 delayed unions and 2 nonunions. PFNA was more effective than DHS in the treatment of high-risk lateral wall fractures in the elderly (fewer delayed unions and nonunions) [
24].
9. Comparing Sliding Distance of Lag Screw and Nonunion Rate
A systematic review and meta-analysis published in 2021 by Lim et al. compared the sliding distance of the lag screw, the change in neck-shaft angle (NSA) and the nonunion rates according to the anteromedial cortical support on anteroposterior (AP) and lateral view radiographs after ITF reduction. They assessed the distance of lag screw sliding, the change in NSA and the incidence of nonunion after reduction of ITFs by extramedullary reduction (EMR), neutral reduction (NR) and intramedullary reduction (IMR). In this study, greater sliding distances, more varus in NSA and higher nonunion rates were observed in the IMR group than in the non-IMR group on both anteroposterior and lateral radiographs [
25]. In 2022, the AAOS published a set of recommendations to assist orthopedic surgeons in treating patients over 55 years of age with an ITF, based on the best available evidence at that time (
Table 1) [
26].
10. Anti-Rotation Screws/Blades in Unstable Intertrochanteric Fractures
Gavaskar et al. have stated that the InterTan may render superior functional result and less adverse events than does the PFN - Antirotation (PFNA-II) in elderly individuals with unstable trochanteric fractures. The prevalence of varus collapse and medial blade migration were greater in the PFNA-II group. The necessity for repeat surgery to address surgery-related adverse events was substantially high elevated the PFNA-II group [
27]. Yadav et al. found that both PFNA-II (N=23) and PFN (N=23) were efficacious in managing unstable trochanteric fractures in terms of functional results. However, PFNA-II was better because it needed less radiation exposure due to single guidewire employment, a brief learning curve, less blood loss, lower surgical time, and fewer adverse events. There were no cases of non-union in either group studied. Yadav et al. proposed it to be the favorite implant in ITCs in geriatric individuals and other age groups [
28].
11. The Importance of Fracture Gaps as Elements of Mal-Reduction
Karampinas et al. have reported that the amount of compression allowed by CMNs cannot always appropriately diminish large fragment gaps. They presented a technical trick of double compression of the fracture site, with the aim of accomplishing the crucial extra compression and reduction when needed, thus reducing the risk of postoperative implant cut-out. The technique was employed in 14 out of 277 peritrochanteric fractures treated with CMN for 12 months, with satisfactory results regarding both fracture site union and postoperative functional capacity. At the 1-year follow-up, a fracture union was observed in the hip X-rays of all 14 patients [
29].
12. Cement Augmentation Increases Construct Stability and Improves Outcomes in Geriatric Intertrochanteric Fractures
In a systematic review published in 2022 by Goodnough et al., it was observed that calcium phosphate or cement-augmented CMN fixation increased fracture stability and improved outcomes. Nonunion ranged from 0% to 3.6% in the group with cement augmentation and from 0% to 34% in the group without cement augmentation [
30].
13. Conclusions
Mechanical complications of ITFs include cut-out, excessive shortening of the proximal femur, delayed union, nonunion, early implant fracture, nail toggle and cut through/medial migration. That is why a fundamental goal in the treatment of ITFs is to achieve stable fixation in osteoporotic bone, allowing early weight bearing. Intraoperative determination of fracture stability is essential. A trochanteric buttress plate (TBP) can be used successfully to augment, fix or buttress the lateral trochanteric wall with good to excellent results, but at the cost of increased operative time, increased blood loss and increased radiation exposure. Calcium phosphate or cement-augmented cephalomedullary nail (CMN) fixation increases fracture stability and improves outcomes. The American Academy of Orthopedic Surgeons (AAOS) clinical practice guidelines for the management of intertrochanteric fractures (ITF) in patients older than 55 years are the following: 1) In patients with stable ITF, the use of either a sliding hip screw (SHS) or a cephalomedullary nail (CMN) is advised (strong strength of evidence). 2) In patients with reverse obliquity fractures, a CMN is recommended (strong strength of evidence). 3) Patients with unstable ITF should be treated with a CMN (strong strength of evidence). 4) In patients with ITF, a short or long CMN may be considered (limited strength of evidence).
References
- Nyholm, A.M.; Palm, H.; Malchau, H.; Troelsen, A.; Gromov, K. Lacking evidence for performance of implants used for proximal femoral fractures – A systematic review. Injury 2016, 47, 586–594. [Google Scholar] [CrossRef] [PubMed]
- Gromov, K.; Brix, M.; Kallemose, T.; Troelsen, A. Early results and future challenges of the Danish Fracture Database. Dan Med J. 2014, 61, A4851. [Google Scholar] [PubMed]
- Bhandari, M.; Schemitsch, E.; Jönsson, A.; Zlowodzki, M.; Haidukewych, G.J. Gamma Nails Revisited: Gamma Nails Versus Compression Hip Screws in the Management of Intertrochanteric Fractures of the Hip: A Meta-Analysis. J. Orthop. Trauma 2009, 23, 460–464. [Google Scholar] [CrossRef] [PubMed]
- Dhammi, I.K.; Jain, A.K.; Singh, A.P.; Haq, R.U.; Mishra, P.; Jain, S. Primary nonunion of intertrochanteric fractures of femur: An analysis of results of valgization and bone grafting. Indian J. Orthop. 2011, 45, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Hunter, G. The results of operative treatment of trochanteric fractures of the femur. Injury 1975, 6, 202–205. [Google Scholar] [CrossRef] [PubMed]
- Davis, T.; Sher, J.; Horsman, A.; Simpson, M.; Porter, B.; Checketts, R. Intertrochanteric femoral fractures. Mechanical failure after internal fixation. J. Bone Jt. Surg. 31. [CrossRef]
- Klima, M.L. Mechanical Complications After Intramedullary Fixation of Extracapsular Hip Fractures. J. Am. Acad. Orthop. Surg. 2022, 30, e1550–e1562. [Google Scholar] [CrossRef] [PubMed]
- Vaquero, J.; Munoz, J.; Prat, S.; Ramirez, C.; Aguado, H.; Moreno, E.; Perez, M.D. Proximal Femoral Nail Antirotation versus Gamma3 nail for intramedullary nailing of unstable trochanteric fractures. A randomised comparative study. Injury 2012, 43, S47–S54. [Google Scholar] [CrossRef] [PubMed]
- Bonnaire, F.; Lein, T.; Bula, P. Pertrochantäre Femurfrakturen. Der Unfallchirurg 2011, 114, 491–500. [Google Scholar] [CrossRef]
- Buecking, B.; Bliemel, C.; Struewer, J.; Eschbach, D.; Ruchholtz, S.; Müller, T. Use of the gamma3™ nail in a teaching hospital for trochanteric fractures: mechanical complications, functional outcomes, and quality of life. BMC Res. Notes 2012, 5, 651–651. [Google Scholar] [CrossRef]
- Rupprecht, M.; Grossterlinden, L.; Ruecker, A.H.; de Oliveira, A.N.; Sellenschloh, K.; Nüchtern, J.; Püschel, K.; Morlock, M.; Rueger, J.M.; Lehmann, W. A Comparative Biomechanical Analysis of Fixation Devices for Unstable Femoral Neck Fractures: The Intertan Versus Cannulated Screws or a Dynamic Hip Screw. J. Trauma: Inj. Infect. Crit. Care 2011, 71, 625–634. [Google Scholar] [CrossRef]
- Ruecker, A.H.; Rupprecht, M.; Gruber, M.; Gebauer, M.; Barvencik, F.; Briem, D.; Rueger, J.M. The Treatment of Intertrochanteric Fractures: Results Using an Intramedullary Nail With Integrated Cephalocervical Screws and Linear Compression. J. Orthop. Trauma 2009, 23, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Ren, G.; Peng, C.; Zheng, X.; Mao, F.; Zhang, Y. InterTan nail versus Gamma3 nail for intramedullary nailing of unstable trochanteric fractures. Diagn. Pathol. 2014, 9, 191. [Google Scholar] [CrossRef] [PubMed]
- von Rüden, C.; Hungerer, S.; Augat, P.; Trapp, O.; Bühren, V.; Hierholzer, C. Breakage of cephalomedullary nailing in operative treatment of trochanteric and subtrochanteric femoral fractures. Arch. Orthop. Trauma Surg. 2014, 135, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, P.P.; Hannink, G.; Reijmer, J.; Somford, M.P.; Van Susante, J.L.C. Increased failure rates after the introduction of the TFNA proximal femoral nail for trochanteric fractures: implant related or learning curve effect? Acta Orthop. 2022, 93, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Goodnough, L.H.; Chang, R.N.; Fasig, B.H.; Prentice, H.A.; Paxton, E.W.; Diekmann, G.R.; Jackman, J.M.; Okike, K.; Fang, A.S. Risk of Revision After Hip Fracture Fixation Using DePuy Synthes Trochanteric Fixation Nail or Trochanteric Fixation Nail Advanced. J. Bone Jt. Surg. 2022, 104, 1090–1097. [Google Scholar] [CrossRef] [PubMed]
- Swift, B.; Stewart, A.; Grammatopoulos, G.; Papp, S.; Wilkin, G.; Liew, A. Comparing the rates and modes of failure of two third generation cephalomedullary nail systems in the treatment of intertrochanteric hip fractures. Injury 2022, 53, 2846–2852. [Google Scholar] [CrossRef]
- Kim, K.-H.; Han, K.Y.; Kim, K.W.; Lee, J.H.; Chung, M.K. Local Postoperative Complications after Surgery for Intertrochanteric Fractures Using Cephalomedullary Nails. Hip Pelvis 2018, 30, 168–174. [Google Scholar] [CrossRef]
- Ali, M.; Al-Dadah, O. A Comparison of Tip-Apex Distance at Various Angles of Fixation Devices in Hip Fractures. Cureus 2023, 15, e35576. [Google Scholar] [CrossRef] [PubMed]
- Cinque, M.E.; Goodnough, L.H.; Schultz, B.J.; Fithian, A.T.; DeBaun, M.; Lucas, J.F.; Gardner, M.J.; Bishop, J.A. Short versus long cephalomedullary nailing of intertrochanteric fractures: a meta-analysis of 3208 patients. Arch. Orthop. Trauma Surg. 2021, 142, 1367–1374. [Google Scholar] [CrossRef]
- Jain, S.; Dawar, H.; Khare, H.; Kumar, M.; Ajmera, A. Does augmentation of intramedullary nails by a buttress plate effectively restore lateral wall integrity in intertrochanteric fractures. Int. Orthop. 2022, 46, 2365–2371. [Google Scholar] [CrossRef]
- Hoffmann, M.F.; Khoriaty, J.D.; Sietsema, D.L.; Jones, C.B. Outcome of intramedullary nailing treatment for intertrochanteric femoral fractures. J. Orthop. Surg. Res. 2019, 14, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Haidukewych, G.J.; Israel, T.A.; Berry, D.J. Reverse Obliquity Fractures of the Intertrochanteric Region of the Femur. 83. [CrossRef]
- Tian, Z.; Chen, J.; Zhang, Y.; Shi, L.; Li, W. A Retrospective Study of 98 Elderly Patients with High-Risk Lateral Femoral Wall Intertrochanteric Hip Fractures to Compare Outcomes Following Surgery with Proximal Femoral Nail Antirotation (PFNA) Versus Dynamic Hip Screw (DHS). Med Sci. Monit. 2022, 28, e936923–e936923. [Google Scholar] [CrossRef] [PubMed]
- Lim, E.J.; Sakong, S.; Son, W.S.; Cho, J.-W.; Oh, J.-K.; Kim, C.-H. Comparison of sliding distance of lag screw and nonunion rate according to anteromedial cortical support in intertrochanteric fracture fixation: A systematic review and meta-analysis. Injury 2021, 52, 2787–2794. [Google Scholar] [CrossRef] [PubMed]
- O'Connor, M.I.; Switzer, J.A. AAOS Clinical Practice Guideline Summary: Management of Hip Fractures in Older Adults. J. Am. Acad. Orthop. Surg. 2022, 30, e1291–e1296. [Google Scholar] [CrossRef] [PubMed]
- Gavaskar, A.S.; Tummala, N.C.; Srinivasan, P.; Gopalan, H.; Karthik, B.; S, S. Helical Blade or the Integrated Lag Screws: A Matched Pair Analysis of 100 Patients With Unstable Trochanteric Fractures. J. Orthop. Trauma 2018, 32, 274–277. [Google Scholar] [CrossRef] [PubMed]
- Yadav, S.; Dakshinamoorthy, R. Comparison of Twin Screw Derotation Type Versus Single Helical Blade Type Cephalomedullary Nail in Trochanteric Fractures in Geriatric Population. Cureus 2022, 14, e31557. [Google Scholar] [CrossRef] [PubMed]
- Karampinas, P.; Galanis, A.; Papagrigorakis, E.; Vavourakis, M.; Krexi, A.; Pneumaticos, S.; Vlamis, J. Double lag-screw compression for optimal fixation of intertrochanteric fractures with large fragment gap: A technical note. SICOT-J 2023, 9, 9. [Google Scholar] [CrossRef]
- Goodnough, L.H.; Wadhwa, H.; Tigchelaar, S.S.; DeBaun, M.R.; Chen, M.J.; Graves, M.L.; Gardner, M.J. Indications for cement augmentation in fixation of geriatric intertrochanteric femur fractures: a systematic review of evidence. Arch. Orthop. Trauma Surg. 2021, 142, 2533–2544. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).