1. Introduction
Age-related macular degeneration (AMD) is one of the most common causes of central blindness in people over 50 years of age in well-developed countries [
1]. The loss of central vision is the result of geographical atrophy (GA) in a course of dry (atrophic, non-exudative) AMD or macular neovascularization (MNV) related to wet (exudative) AMD. Dry AMD accounts for 85-90% of all AMD cases [
2]. Advances form of dry AMD is geographic atrophy (GA), defined as round or oval area of atrophy outer retinal layers, retinal pigment epithelium (RPE) and choroidal vessels with a diameter of at least 175 µm. GA typically starts in the perifoveal region and gradually progress to involve the fovea with time, leading to central scotomas and permanent loss of visual acuity. According to statistical data newly recognized GA affects over 5 millions of people around the world and is significant cause of irreversible central vision loss [
3]. Median time from diagnosis to central vision loss ranges from 1.4 to 2.5 years, which is related to fovea involvement by GA [
4].
AMD appears to be complex and involve numerous processes and mechanisms involved in its development and progression. Both non-modifiable risk factors, such as age, female gender, white race, genetic background influence the development and progression of this condition [
5,
6,
7]. There are over 30 identified genes linked to the risk of AMD development, however the polymorphism of complement factor H gene (Y402H) is thought to be the strongest genetic risk variant for AMD [
8,
9,
10]. The modifiable risk factors include: cigarette smoking, cardiovascular diseases, high lipid levels, abdominal obesity, diet with low intake of antioxidants, exposure to ultraviolet radiation, as well as local factors such as cataract surgery and blue irises [
5,
6,
11,
12,
13,
14].
There is growing evidence that autoimmunity against retinal antigens and inflammatory reactions dependent on complement system activation might be involved in the pathogenesis and progression of AMD [
15,
16,
17,
18]. With aging chronic inflammation, called para-inflammation or inflammaging, is thought to be an adaptive response of the immune system due to increased oxidative stress and noxious insults to maintain local tissue homeostasis. In patients with AMD, this chronic inflammatory reaction become dysregulated and contributes to macular damage [
19]. There are publications demonstrated that various ocular diseases in a course of which autoimmune and inflammatory components play a crucial role may be associated with the presence of serum ARA [
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30]. However, the detailed role of these autoantibodies in the AMD pathogenesis remains unclear. There are speculations that their occurrence may be an epiphenomenon developing in response to macular damage or alternatively ARA may be directly involved in the development and progression of AMD [
31,
32,
33,
34,
35,
36].
Although the prevalence of serum AECA has been reported previously by us in patients with wet AMD [
37], on reviewing the literature, no publication regarding the presence of circulating AECA in a course of dry AMD is currently available. To our best knowledge this is the first research on the occurrence of circulating AECA in patients with dry AMD.
The purpose of our study was to determine the prevalence of serum AECA in patents with dry AMD in order to determine their relationship with the clinical features of the disease, notably area of GA.
2. Materials and Methods
2.1. Patients and Controls
Forty one patients with unilateral or bilateral geographic atrophy in a course of dry AMD were enrolled in the study. Exclusion criteria included the following: other retinal diseases (MNV in the contralateral eye, macular teleangiectasia, degenerative myopia), infectious or non-infectious uveitis, glaucoma, paraneoplastic retinopathies, diabetic retinopathy, systemic autoimmune comorbidities, systemic steroid and immunosuppressive therapy. Fifty sex- and age-matched healthy subjects, planned for moderate senile cataract surgery with no clinical signs of AMD or any chronic eye disease served as a control group. The determination of absence of AMD in controls was based on ophthalmological examination and supported by a classification system of AMD prepared by Ferris et al.[
2]. This system is based on fundus lesions observed within 2 disc diameters of the fovea. Individuals with no drusen or pigmentary changes or with small drusen (<63 µm) in macula were considered to have no features of AMD.
Baseline ophthalmic examination in patients and controls included best corrected visual acuity (BCVA) assessment with Snellen charts, anterior segment and fundus examination. The diagnosis of dry AMD was based on the presence of characteristic clinical features on fundoscopy and on the results of optical coherence tomography (OCT) (Topcon 3D OCT 2000, Japan) and fundus autofluorescence (FAF) (Heidelberg Engineering, Spectralis HRA-OCT, Germany) which was used to measure the area of geographic atrophy. In each patient the color fundus picture was also obtained.
2.2. Autoantibody Assays
Each subject of the study was collected 5 ml of peripheral blood from peripheral vein, next clotted and centrifuged at 3500 rpm (1970g) for 10 minutes to recover serum. Aliquoted serum samples were stored at -80° until analysis. Collected material was studied for ARA by indirect immunofluorescence (IIF) method using commercially available frozen sections of normal monkey retina. For detection of antigen bound autoantibodies a secondary goat’s anti-human IgA, G, M polyclonal antibody labelled by fluorescein isothiocyanate was used (Euroimmun AG, Lubeck, Germany). A serial dilution of patients’ or controls’ serum: 1:10, 1:20, 1:40, 1:80 etc. was used to titer positive samples against ARA, whereas starting serum 1:100 dilution was used for screening against AECA, in which human umbilical vein endothelial cells (HUVEC) and iliopsoas muscle sections were antigen substrates (Euroimmun AG, Lubeck, Germany). All details of IIF processing, including tittering, incubation and washing protocol were according to the manufacturer’s recommendations. In brief, incubation time for the serum or the secondary antibody was 30 minutes. After each incubation with diluted serum and next the secondary antibody, biochips were rinsed with phosphate buffered saline with Tween 20. Samples with positive immunological reaction to retinal vessels were screened for AECA using IIF on monkey iliopsoas muscle and HUVECs. All immunohistochemical slides were evaluated using fluorescence microscope EUROSTAR-Bluelight (Carl Zeiss, Euroimmun, Germany). Scoring of IIF results was done by two independent investigators, unaware of the diagnosis or the stage of disease. Results were recorded as the presence of fluorescence signal in the layers of the retina, iliopsoas muscle and HUVECs and the highest serum dilution. A commercial negative tissue control was included on each slide to eliminate the misinterpretation causes by autofluorescence of the tissue.
This study complied with the Declaration of Helsinki. Approval by the Jagiellonian University Bioethical Committee (approval no. 1072.6120.37.2019) was obtained. All subjects provided written informed consent to participate in the study.
2.3. Statistical Analysis
Correlation between the nominal variables and ordinal variables was determined as the association between the variables and the significance level was evaluated with chi-square test for two-way table. A nonparametric Spearman's rank correlation coefficient was used to assess the statistical dependence between discrete and continuous variables. The Student's-t distribution or non-parametric Mann-Whitney U tests were used to compare the means in two groups. Type I statistic error p-value <0.05 was taken to be significant.
3. Results
3.1. Epidemiology and Characteristics of Patients with Dry AMD and a Control Group
The study group included 41 patients (82 eyes) with dry AMD; 15 males (36.6%) and 26 females (63.4%) aged 61 - 90 years (mean: 76.3 years). The control group consisted of 20 males (40%) and 30 females (60%) aged 59 – 86 years (mean: 71.9 years). No statistical differences of age, gender distribution were noted between AMD cases and controls. There were no significant statistical differences between the study and control groups of prevalence to cardiovascular diseases and hyperlipidaemia, either.
Table 1. shows the clinical characteristics of patients with dry AMD and a control group.
The baseline BCVA ranged from counting fingers to 0.8 by Snellen charts. On fundoscopy characteristic changes for dry AMD were observed including: areas of chorioretinal atrophy in 80 eyes and large drusen with changes at the level of retinal pigment epithelium (RPE) in 2 eyes. OCT scans revealed typical findings for dry AMD; large drusen or the atrophy of the outer retinal layers involving photoreceptors, Bruch’s membrane and choriocapillaris.
Based on the FAF examination the mean area of the geographic atrophy ranged from 0.24 mm2 to 29.12 mm2 (mean: 9.81 mm2).
3.2. Serum Antiretinal Antibodies in Dry AMD Patients and in a Control Group
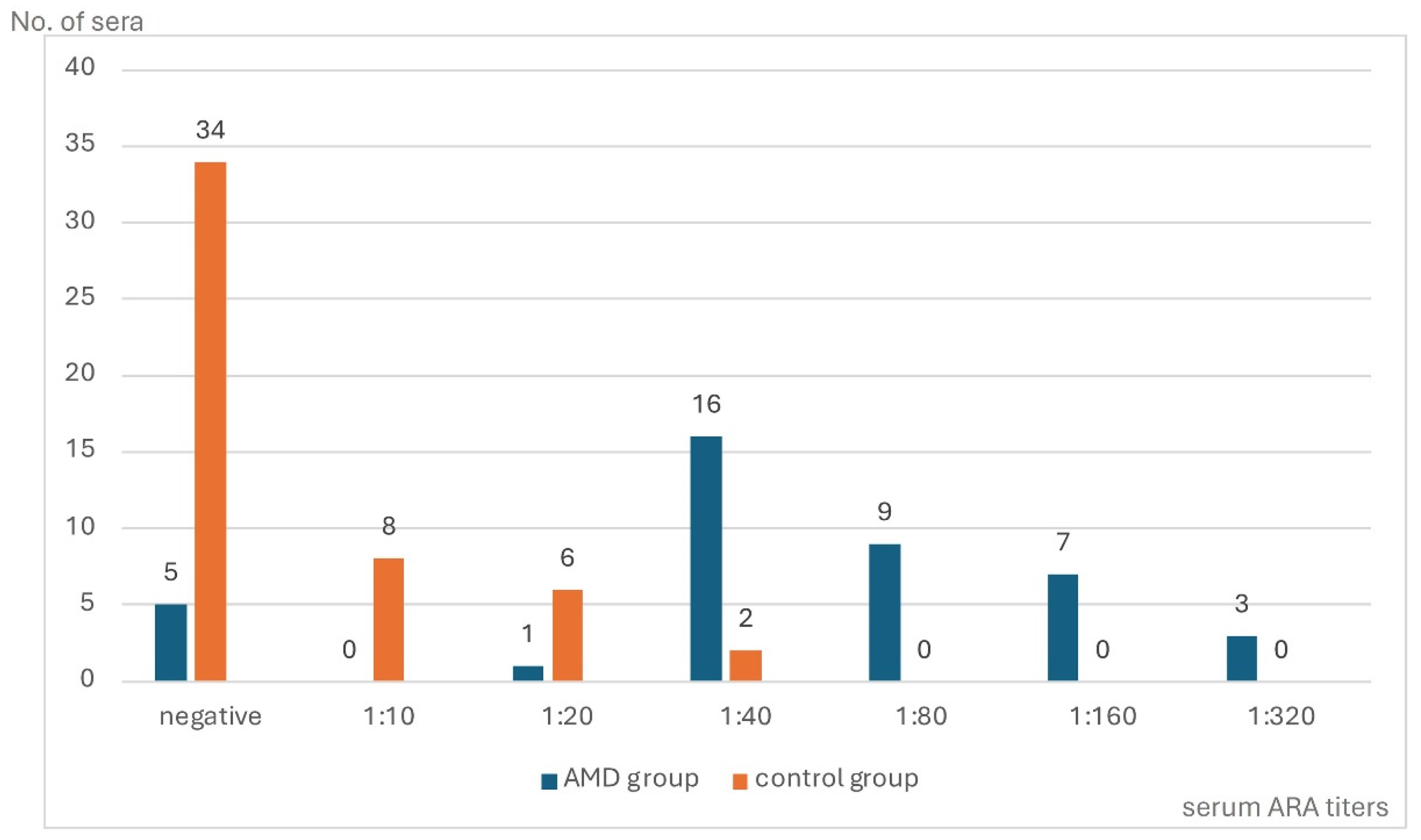
IIF test performed on monkey retina showed ARA in 36 (87.8%) of the 41 AMD patients (range from 1:20 to 1:320) and in 16 from 50 (39.0%) (range from 1:10 to 1:40) of controls (p=0.0000). The comparison of distribution and titers of serum ARA in AMD patients and in a control group are presented in
Figure 1.
Interestingly, patients with dry AMD demonstrated the presence of three types of retinal staining on monkey retina in IIF test, while control sera showed two staining patterns of reactivity with retinal tissue. Differences in ARA types in AMD and controls were statistically significant in cases with positive reaction against cones and rods, p=0.0000 and p=0.0001, respectively, while immunofluorescence within the cytoplasmic components of retinal nuclear layer cells showed no statistical differences between two analyzed groups.
Table 2 shows distribution of ARA in serum of patients with dry AMD and controls according to the staining pattern and titer.
The sera of 31 (75,6%) patients with dry AMD showed more than one immunofluorescence type, while in a control group the complexity of ARA types was observed only in 4 (8%) cases (p=0.0000).
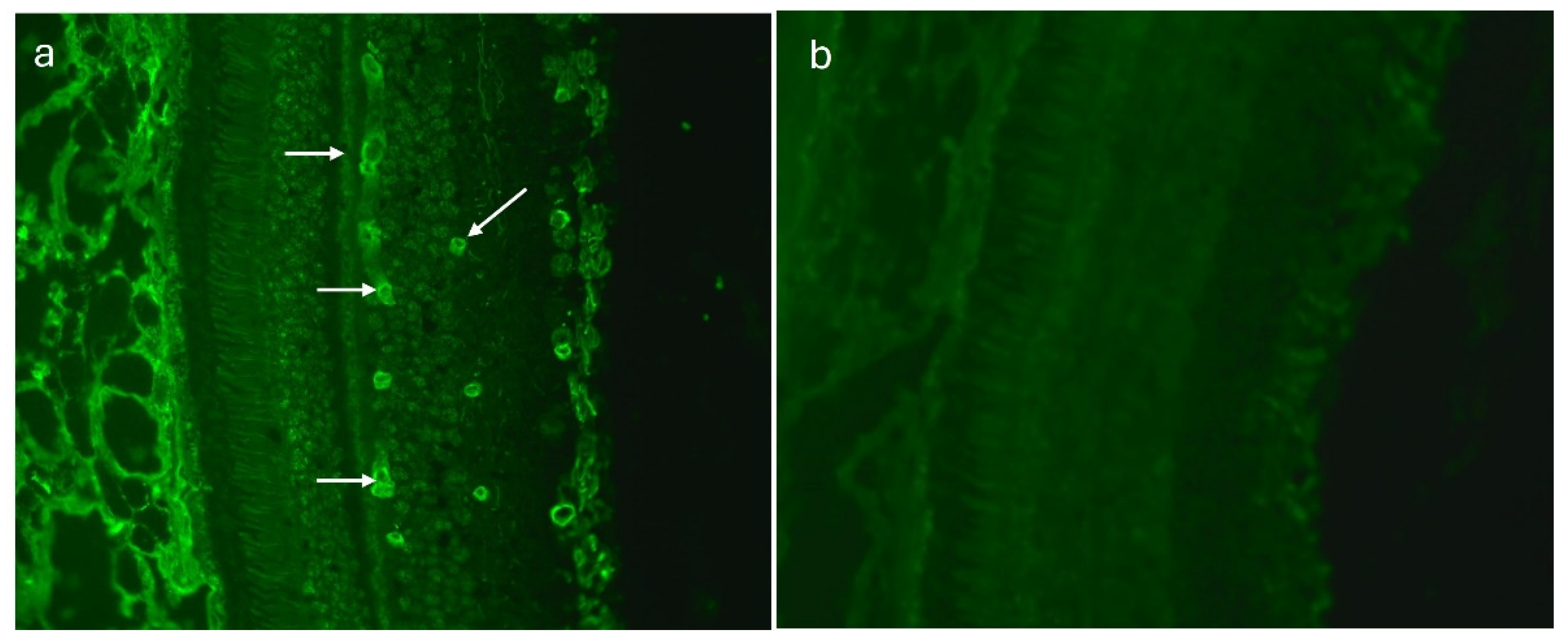
Figure 2 presents various immunofluorescence pattern reactions of AMD patients sera with monkey retina.
3.3. Anti-Endothelial Cells Antibodies in Patients with Dry AMD and in a Control Group
Sera of 20 (48.8%) AMD patients showed a highly distinctive pattern of tubular arrangement of the fluorescence signal on monkey retina sections within the retinal vessels (
Figure 3a,b). In a control group this type of immunofluorescence was observed only in 5 (10%) sera. This difference was significant statistically (p=0.0001).
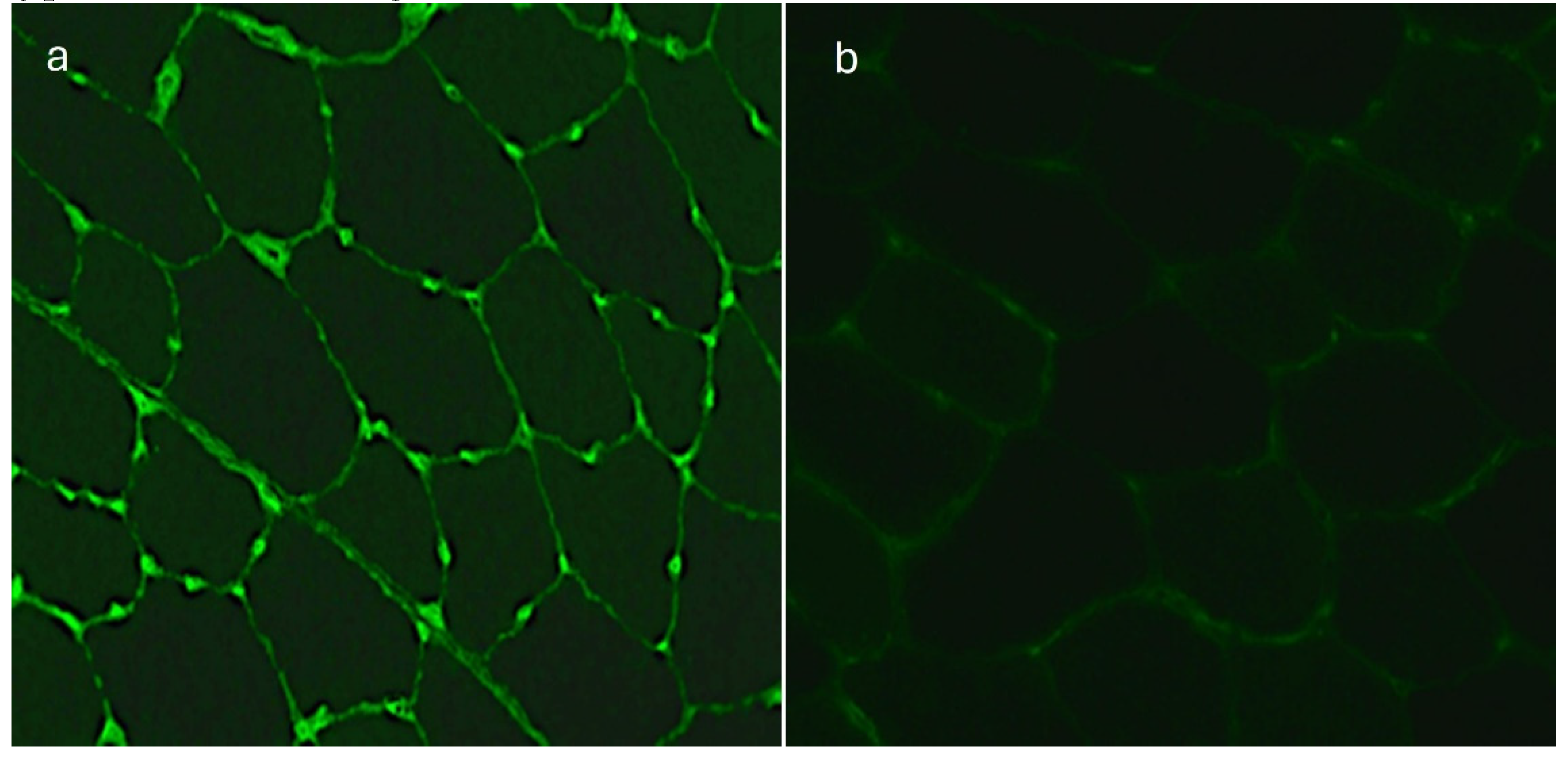
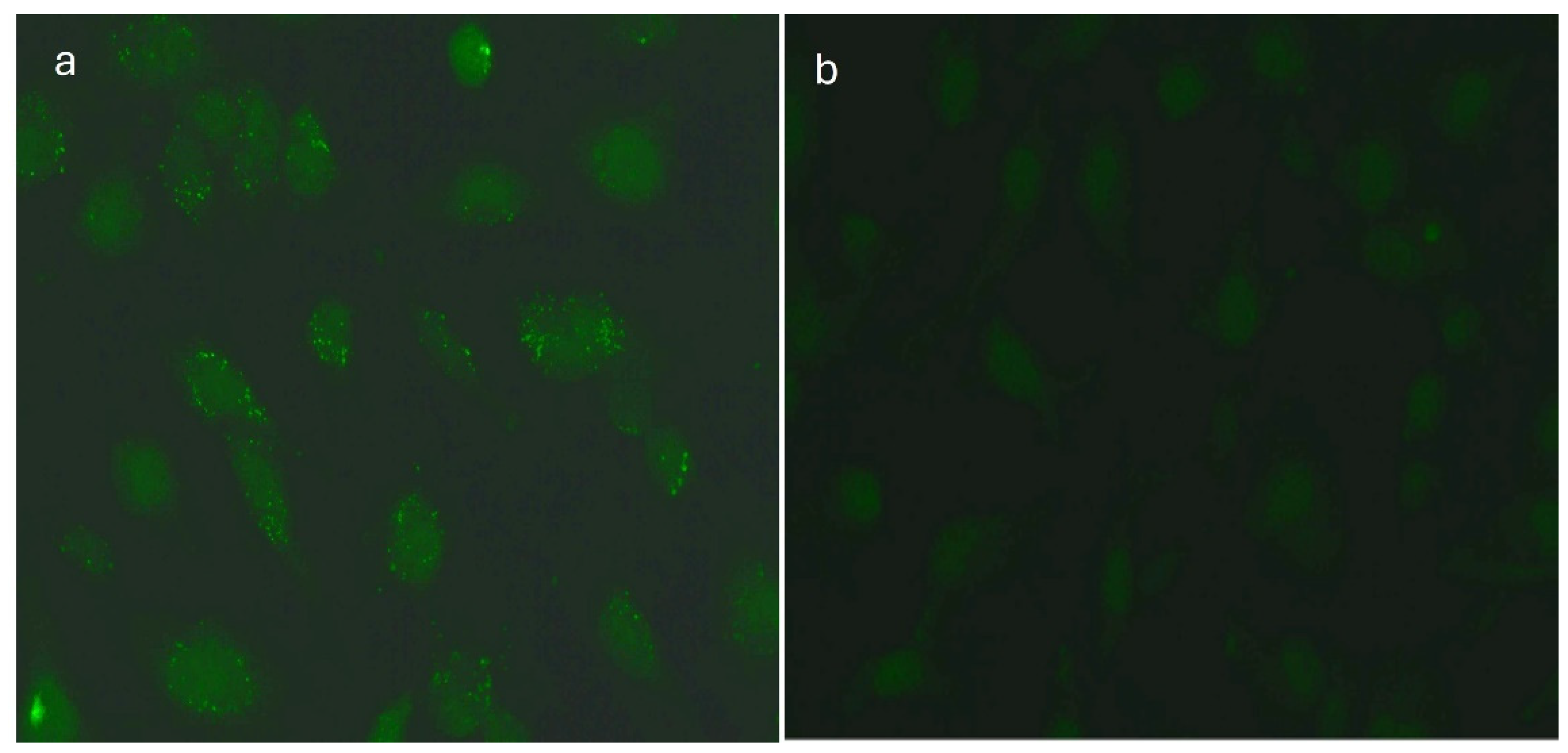
Since this type of immunofluorescence was suggesting anti-endothelial specificity of autoantibodies, we repeated the assay with a primary human cell line from umbilical vein (HUVEC) and skeletal iliopsoas muscle sections of monkey and as the substrates. The fluorescence signal located between the fibers of transversal sections of the muscle had a characteristic pattern corresponding to the striated muscle vessels. The HUVEC cellular substrate has no other epitopes than endothelial cells. Verification of auto-antibodies in IIF tests performed on monkey iliopsoas muscle and HUVEC cells confirmed the presence of AECA in 20 (48.8%) patients with dry AMD in titers ranging from 1:100 to 1:1000. All 20 (48.8%) sera of AMD patients showed the positive reaction with iliopsoas muscle and 13 (31.7%) of them with HUVEC demonstrating an immunofluorescence pattern typical for AECA (
Figure 4 and
Figure 5) .
Only five (10.0%) of control sera showed the positive immunofluorescence pattern reaction to the retinal vessels in IIF test on normal monkey retina at titers ranging from 1:10 to 1:80. The verification carried out on monkey iliopsoas muscle and HUVEC, confirmed the presence of circulating AECA in all five (10.0%) control sera at titer 1:100.
Table 3 presents the distribution of AECA in the sera of patients with dry AMD and controls according to the immunofluorescence staining pattern and titer.
3.4. Circulating Anti-Retinal and Anti-Endothelial Cells Antibodies and Clinical Features of Dry AMD
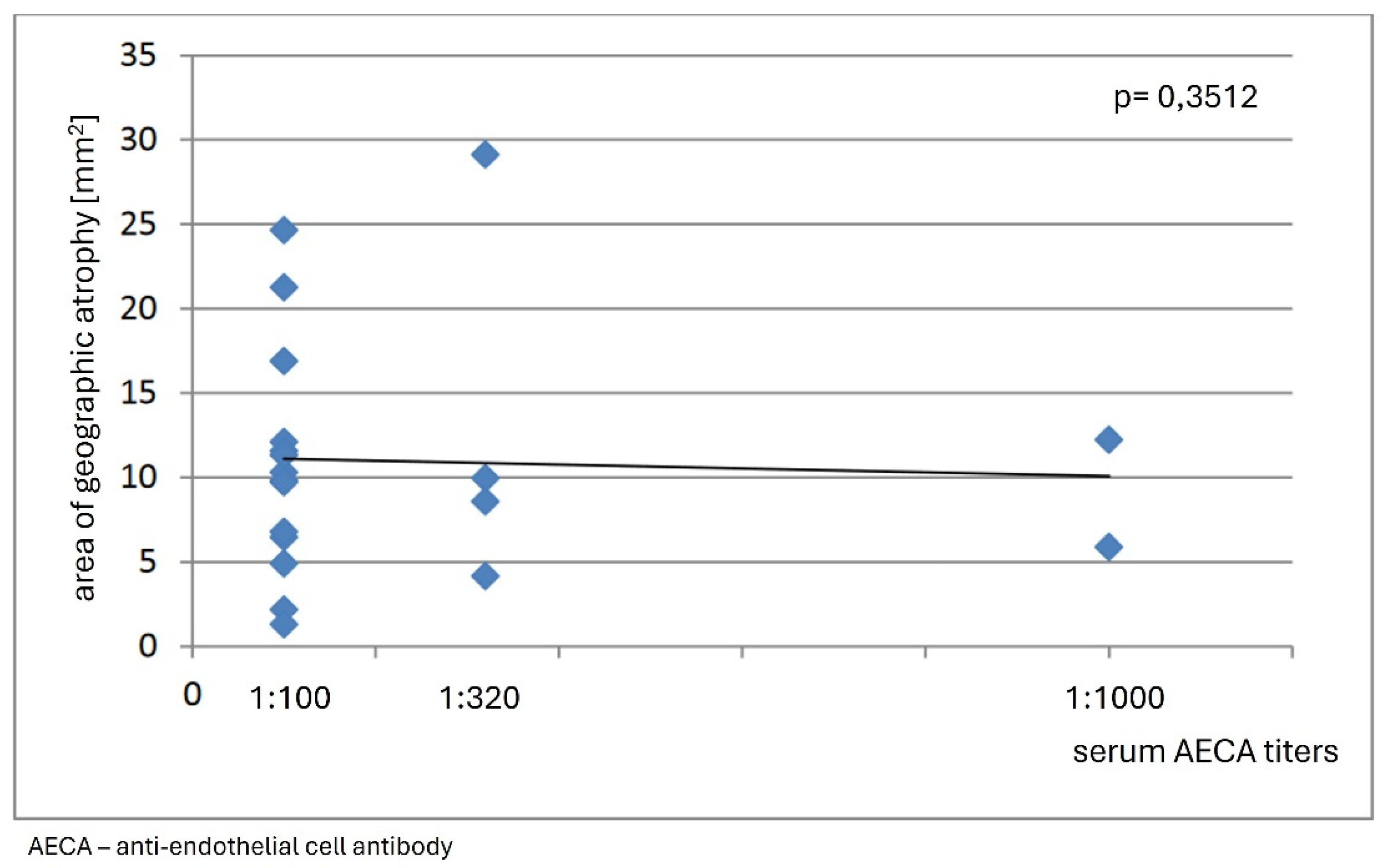
In analyzed group of patients no correlation was found between immunofluorescence staining patterns of reactivity against retinal tissue, complexity and serum levels of circulating ARA and clinical features of dry AMD. Our observations revealed no association between serum levels of circulating AECA and area of geographic atrophy, either (p = 0,3512) (
Figure 6).
The simultaneous occurrence of circulating ARA and AECA showed no differences with cases that sera showed to be positive only for ARA or AECA in terms of area of geographic atrophy.
4. Discussion
GA is a multifactorial disease in which intrinsic and extrinsic factors lead to RPE dysfunction. With age, RPE dysfunction progresses, leading to drusen and lipofuscin deposition [
10,
38]. Drusen and lipofuscin components, as well as other oxidative stress products, such as advanced glycation end products, were reported to induce inflammation through multiple pathways, including the complement cascade [
38,
39]. When regulatory components in these pathways are compromised, especially by genetic risk factors, initiation of chronic inflammation (para-inflammation) may lead to damage and ultimately retinal cell death, which constitutes a typical feature of GA [
10]. The mechanism of the late stage of dry AMD is not fully understood, but inflammation and immune dysregulation are believed to play a significant role in its pathogenesis [
40]. Pathological mechanisms initiating excessive apoptosis of photoreceptors in the course of AMD have also been implicated as one of the potential pathogenetic factors in this multifactorial condition [
41].
In the current study circulating ARA were detected at significantly higher frequencies and at higher titers in patients with GA as compared with controls. There are few data in the literature on the prevalence of serum ARA in patients with dry AMD; however, most of those studies reported autoantibody analysis for both wet and dry AMD [
32,
42]. Recently, there have been more studies investigating the presence of ARA in the serum of patients with exudative AMD. The results of these studies revealed the presence of ARA in 46% to 95.9% of patients with exudative AMD [
35,
43,
44,
45,
46]. This discrepancy in the occurrence of circulating ARA may result from the use of different diagnostic methods, different dilutions of the tested sera and may also be related to the heterogeneity of the studied groups, and differences in the type and the stage of the disease. The previous studies revealed the associations between the serum ARA levels and the stage of the disease and moreover treatment with intravitreal VEGF inhibitors led to decrease in the titers of these autoantibodies [
35]. Considering that exudative and dry AMD are two forms of the same condition, it seems that the effect of ARA is still insufficiently understood in patients with dry AMD. Korb et al. [
36] described ARA in patients with dry AMD and found that they occurred more frequently as compared to healthy population, however the study did not analyzed the association with the stage of the disease, thus it is difficult to compare those results with our observations. In our study serum ARA were detected more frequently in individuals with GA than in controls without AMD, suggesting their involvement in the development of the disease. Our results may support the hypothesis that circulating ARA may play some role in GA pathogenesis. Since it has been shown that circulating ARA may appear 3 to15 years prior to clinical manifestation of the disease, it seems to be reasonable for further research and to investigate their role in the pathogenesis and the progression of GA in patients with dry AMD [
47,
48].
To the best of our knowledge, the current study is the first to report the presence of circulating AECA in patients with dry AMD. We found significantly elevated serum expression of AECA in patients with GA. Studies on the association between circulating AECA with dry AMD appear to be limited. Machalinska et al. [
49] reported circulating endothelial cells (CECs) in patients with wet and dry AMD, but serum AECA levels were not assessed. Their study indicated that AMD is accompanied by endothelial dysfunction. Increased serum CECs counts in patients with AMD reflect severe vascular abnormalities and may be involved in the pathogenesis of the disease. The authors also emphasized the need to search for a common pathological mechanism for AMD and systemic vascular diseases.
AECA were first described by Lindqvist and Osterland in 1971 [
50]. These autoantibodies were reported in several autoimmune diseases associated with vasculitis, such as systemic lupus erythematosus (SLE), systemic scleroderma (SSc), rheumatoid arthritis, Kawasaki disease, granulomatosis with polyangiitis (GPA), multiple sclerosis and diabetes mellitus [
22,
51,
52]. However, the presence of AECA is not a disease-specific marker but can play an important role in monitoring disease activity, and can also be used to assess the risk of recurrence or complications [
52]. In patients with SSc there was no correlation with AECA and SSc activity, but the authors suggested that the presence of AECA might indicate vascular complications in SSc [
51]. In some reports, it has been suggested that AECA may be a good predictor of relapses in patients with small vessel vasculitis [
53].
It has been hypothesized that AECA occur in response to endothelial cell injury. However, it is also possible that they themselves have cytotoxic activity, and their presence may be inherent to the destructive inflammatory process [
47,
52,
54]. The cytotoxic activity of AECA can affect endothelial cells through complement-dependent mechanisms or as antibody-dependent cell-mediated response [
54]. Some publications suggested that AECA, by inducing the overexpression of adhesion molecules (including selectins, intercellular adhesion molecule-1, and vascular cell adhesion molecule-1) and the production of cytokines and chemokines, may lead to endothelial damage through adhesion to endothelial cells. An autoimmune basis of vasculitis is therefore suggested [
52,
55,
56]. AECA were shown to induce apoptosis of progenitors of bone marrow endothelial cells, which leads to disturbances in endothelial regeneration and healing of vascular lesions [
57]. Some studies also suggested that AECA may exert pathogenic effects by activating endothelial cells to induce a procoagulant phenotype and subsequent thrombosis [
56,
58,
59,
60].
The results of our study revealed significant differences in the occurrence of circulating AECA in patients with dry AMD and controls; these autoantibodies were detected more frequently and at higher titers in patients than in controls. Our previous study in patients with wet AMD also showed significant differences in the prevalence of AECA between the study group and healthy subjects, while there was no association between the disease advancement and average serum AECA titers [
37]. These observations are in accordance with the results revealed in a current research that showed no association between AECA titers and the clinical activity of the disease assessed as an area of GA.
The described mechanisms of initiation and progression of tissue damage related to the presence of circulating AECA cannot be excluded in the course of dry AMD. However, further studies are needed to determine whether AECA are involved in the pathogenesis of dry AMD or whether they occur secondary to endothelial cell damage in the course of the disease.
5. Conclusions
Our findings are important in light of previous research suggesting that AMD is an immune-mediated inflammatory disease. While AECA are probably involved in the pathogenesis and progression of AMD, it cannot be excluded that their presence is secondary to preexisting retinal damage. Further research is needed to clarify the clinical and pathological significance of AECA in dry AMD, which may have important implications for future treatment of this sight-threatening disease.
Author Contributions
Conceptualization, A.K.-T.; Data curation, K.Ż.-Ł., and W.P.-M.; Formal analysis, .K.Ż.-Ł., I.K.-B., B.R.-D., and A.K.-T.; Investigation, J.W., I.K.-B.,W.P-M., and M.S.; Methodology, J.W., M.S., and A.K.-T.; Project administration, K.Ż-Ł.; Resources, B.R.-D.; Software, K.Ż.-Ł.; Supervision, M.S., and A.K.-T.; Validation, W.P.-M., and B.R.-D.; Visualization, K.Ż-Ł.; Writing – original draft, K.Ż.-Ł, A.K.-T., and I.K.-B.; Writing – review & editing, A.K.-T., and B.R.-D.; Funding acquisition, K.Ż.-Ł. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by Jagiellonian University Medical College, grant number N41/DBS/000313.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Ethics Committee of Jagiellonian University (protocol code 1072.6120.37.2019, dated from 31st January 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. The patients signed an institutional informed consent for the use of medical records and the publication of this information for research purposes.
Data Availability Statement
Data supporting the findings of this study are available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Vyawahare: H.;, Shinde, P. Age-Related Macular Degeneration: Epidemiology, Pathophysiology, Diagnosis, and Treatment. Cureus 2022, Sep 26, 14(9):e29583. [CrossRef]
- Ferris, F.L.; Wilkinson, C.P.; Bird, A.; Chakravarthy, U.; Chew, E.; Csaky, K.; Sadda, S.R.; Beckman Initiative for Macular Research Classification Committee. Clinical classification of age-related macular degeneration. Ophthalmology 2013, Apr,120(4):844-51. [CrossRef]
- Friedman, D.S.; O’Colmain, B.J.; Muñoz, B.; Tomany S.C.; McCarty, C.; de Jong, P.; Nemesure, B.; Mitchell, P.; Kempen J.; Eye Diseases Prevalence Research Group. Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol 2011, Sep, 129(9):1188.
- Heier, J.S.; Pieramici, D.; Chakravarthy, U.; Patel S.S.; Gupta, S.; Lotery, A.; Lad, E.M.; Silverman, D.; Henry, E.C.; Anderesi M.; Tschosik, E.A.; Gray, S.; Ferrara, D.; Guymer, R.; Chroma and Spectri Study Investigators. Visual Function Decline Resulting from Geographic Atrophy: Results from the Chroma and Spectri Phase 3 Trials. Ophthalmol Retina 2020, Jul, 4(7):673-688. [CrossRef]
- Saunier, V.; Merle. B.M.; Delyfer, M.; Cougnard-Grégoire, A.; Rougier, M.-B.; Amouyel, P.; Lambert, J.-C.; Dartigues, J.-F.; Korobelnik, J.-F.; Delcourt, C. Incidence of and Risk Factors Associated With Age-Related Macular Degeneration: Four-Year Follow-up From the ALIENOR Study. JAMA Ophthalmol. 2018, May, 1,136(5):473–481. [CrossRef]
- Chakravarthy, U.; Wong, T.Y.; Fletcher, A.; Piault, E.; Evans, C.; Zlateva, G.; Buggage, R.; Pleil, A.; Mitchell, P. Clinical risk factors for age-related macular degeneration: a systematic review and meta-analysis. BMC Ophthalmol. 2010, Dec 13,10:31. [CrossRef]
- DeAngelis, M.M.; Owen, L.A.; Morrison, M.A.; Morgan, D.J.; Li, M.; Shakoor, A.; Vitale, A.; Iyengar, S.; Stambolian, D.; Kim, I.K.; Farrer, L.A. Genetics of age-related macular degeneration (AMD). Hum. Mol. Genet. 2017, Aug 1, 26(R1): R45–R50. [CrossRef]
- Geerlings, M.J.; de Jong, E.K.; den Hollander, A.I. The complement system in age-related macular degeneration: A review of rare genetic variants and implications for personalized treatment. Mol. Immunol. 2017, Apr, 84:65–76.
- Armento, A.; Ueffing, M.; Clark, S.J. The complement system in age-related macular degeneration. Cell Mol Life Sci. 2021 May, 78(10):4487-4505. [CrossRef]
- Boyer, D.S.; Schmidt-Erfurth, U.; van Lookeren, C. M.; Henry, E.C.; Brittain, C. The pathophysiology of geographic atrophy secondary to age-related macular degeneration and the complement pathway as a therapeutic target. Retina 2017 May, 37(5):819-35. [CrossRef]
- Velilla, S.; García-Medina, J.J.; García-Layana, A.; Dolz-Marco, R.; Pons-Vázquez, S.; Pinazo-Durán, M.D.; Gómez-Ulla, F.; Arevalo, J.F.; Díaz-Llopis, M.; Gallego-Pinazo, R. Smoking and age-related macular degeneration: review and update. J. Ophthalmol. 2013, 2013: 895147. [CrossRef]
- Rinninella, E.; Mele, M.C.; Merendino, N.; Cintoni, M.; Anselmi, G.; Caporossi, A.; Gasbarrini, A.; Minnella, A.M. The Role of diet, micronutrients and the gut microbiota in age-related macular degeneration: New perspectives from the gut⁻retina axis. Nutrients. 2018, Nov 5, 10(11):1677. [CrossRef]
- Chiu, C.-J.; Chang, M.-L.; Zhang, F.F.; Li, T.; Gensler, G.; Schleicher, M.;Taylor, A. The relationship of major American dietary patterns to age-related macular degeneration. Am J Ophthalmol. 2014, Jul, 158(1):118–127. [CrossRef]
- Chen, Z.; Zeng, Y.; Tian, F. Effect of cataract surgery on the progression of age-related macular degeneration. Medicine (Baltimore) 2022, Nov 4, 101(44):e31566. [CrossRef]
- Chen, M.; Xu, H. Parainflammation, chronic inflammation, and age-related macular degeneration. J Leukoc Biol. 2015, Nov, 98(5):713-25. [CrossRef]
- Parmeggiani, F.; Sorrentino, F.S.; Romano, M.R.; Costagliola, C.; Semeraro, F.; Incorvaia, C.; D'Angelo, S.; Perri, P.; De Nadai, K.; Bonomo Roversi, E.; Franceschelli, P.; Sebastiani, A.; Rubini, M. Mechanism of inflammation in age-related macular degeneration: an up-to-date on genetic landmarks. Mediators Inflamm. 2013, Nov, 435607. [CrossRef]
- Tan, W.; Zou, J.; Yoshida, S.; Jiang, B.; Zhou, Y. The Role of Inflammation in Age-Related Macular Degeneration. Int. J. Biol. Sci. 2020, Sep 23, 16 (15), 2989-3001. [CrossRef]
- Ascunce, K.; Dhodapkar, R.M.; Huang, D.; Hafler, B.P. Innate immune biology in age-related macular degeneration. Front Cell Dev Biol. 2023, Feb, 28:11:1118524. [CrossRef]
- Bellezza, I. Oxidative Stress in Age-Related Macular Degeneration: Nrf2 as Therapeutic Target. Front. Pharmacol. 2018, Nov, 5:9:1280. [CrossRef]
- Adamus, G. Are Anti-Retinal Autoantibodies a Cause or a Consequence of Retinal Degeneration in Autoimmune Retinopathies? Front Immunol. 2018, Apr, 16, 9:765. [CrossRef]
- Adamus, G.; Champaigne, R.; Yang, S. Occurrence of major anti-retinal autoantibodies associated with paraneoplastic autoimmune retinopathy. Clin Immunol 2020, Jan, 210:108317. [CrossRef]
- Węglarz, M.; Karska-Basta, I.; Kubicka-Trząska, A.; Romanowska-Dixon, B. Anti-retinal antibodies as an etiopathogenetic factor and markers of retinal damage in diseases of the posterior segment of the eye. Acta Ophthalmologica Polonica 2018, 120(1):46-50. [CrossRef]
- Ten Berge, J.C; Schreurs, M.W.; Vermeer, J.; Meester-Smoor, M,A.; Rothova, A. Prevalence and clinical impact of antiretinal antibodies in uveitis. Acta Ophthalmol. 2016, May, 94(3):282-8. [CrossRef]
- Ten Berge, J.C.; van Dijk, E.H.; Schreurs, M.W.; Vermeer, J.; Boon, C.J.; Rothova, A. Antiretinal antibodies in central serous chorioretinopathy: prevalence and clinical implications. Acta Ophthalmol. 2018, Feb, 96(1):56-62. [CrossRef]
- Cursino, S.R.; Costa, T.B.; Yamamoto, J.H.; Meireles, L.R.; Silva, M.A.; de Andrade, H.F., Jr. Increased frequency of anti-retina antibodies in asymptomatic patients with chronic t. gondii infection. Clinics (Sao Paulo) 2010, Oct, 65(10): 1027–1032. [CrossRef]
- Karska-Basta, I.; Pociej-Marciak, W.; Chrzaszcz, M.; Wilanska, J.; Jager, M.J.; Markiewicz, A.; Romanowska-Dixon, B.; Sanak, M.; Kubicka-Trzaska, A. Differences in anti-endothelial and anti-retinal antibody titers: implications for the pathohysiology of acute and chronic central serous chorioretinopathy. J Physiol Pharmacol. 2020 Apr, 71(2). [CrossRef]
- Węglarz, M.; Romanowska -Dixon, B.; Wilańska, J.; Sanak, M.; Karska-Basta, I. Involvement of serum anti-retinal antibodies in the pathophysiology of diabetic retinopathy: a pilot study. J Physiol Pharmacol 2020, Oct, 71(5). [CrossRef]
- Zhu, L.; Shen, W.; Zhu, M.; Coorey, N.J.; Nguyen, A.P.; Barthelmes, D.; Gillies, M.C. Anti-retinal antibodies in patients with macular telangiectasia type 2. Invest Ophthalmol Vis Sci. 2013, Aug 21, 54(8):5675-83. [CrossRef]
- Han, X.; Zhang, L.; Tang, J.; Wang, Z.; Li, S.; Yuan, L.; Qu, J. Correlation of photoreceptor damage with anti-retina antibodies level in aqueous humor in macular edema patients. Sci Rep 2022, Dec, 8, 12(1):21212. [CrossRef]
- Sim, S.S.; Wong, C.W.; Hoang, Q.V.; Lee, S.Y.; Wong, T.Y.; Cheung, C.M. Anti-retinal autoantibodies in myopic macular degeneration: a pilot study. Eye 2020, Oct, 35, 2254–2259 (2021).
- Penfold, P.L.; Provis, J.M.; Furby, J.H.; Gatneby, P.A.; Billson, F.A. Autoantibody to retinal astrocytes associated with age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 1990, 228(3):270-4. [CrossRef]
- Patel, N.; Ohbayashi, M.; Nugent, A.K.; Ramchand, K.; Toda, M.; Chau, K.Y.; Bunce, C.; Webster, A.; Bird, A.C.; Ono, S.J.; Chong, V. Circulating anti-retinal antibodies as immune markers in age-related macular degeneration. Immunology 2005, Jul, 115(3):422-30. [CrossRef]
- Cherepanoff, S.; Mitchell, P.; Wang, J.J.; Gillies, M.C. Retinal autoantibody profile in early age-related macular degeneration: preliminary findings from the Blue Mountains Eye Study. Clin Exp Ophthalmol 2006, Aug, 34(6):590-5. [CrossRef]
- Morohoshi, K.; Ohbayashi, M.; Patel, N.; Chong, V.; Bird, A.C.; Ono, S.J. Identification of anti-retinal antibodies in patients with age-related macular degeneration. Exp Mol Pathology 2012, Oct, 93(2):193-9. [CrossRef]
- Kubicka-Trząska, A.; Wilańska, J.; Romanowska-Dixon, B.; Sanak, M. Circulating anti-retinal antibodies changes in response to anti-angiogenic therapy in patients with exudative age-related macular degeneration. Acta Ophthalmol 2014, Dec, 92(8):e610-4. [CrossRef]
- Korb, C.A.; Lackner, K.J.; Wolters, D.; Schuster, A.K.; Nickels, S.; Beutgen, V.M.; Münzel, T.; Wild, P.S.; Beutel, M.E.; Schmidtmann, I.; Pfeiffer, N.; Grus, F.H. Association of autoantibody levels with different stages of age-related macular degeneration (AMD): Results from the population-based Gutenberg Health Study (GHS). Graefes Arch Clin Exp Ophthalmol 2023, Oct, 261(10):2763-2773. [CrossRef]
- Kubicka-Trząska, A.; Wilańska, J.; Romanowska-Dixon, B.; Sanak, M. Serum anti-endothelial cell antibodies in patients with age-related macular degeneration treated with intravitreal bevacizumab. Acta Ophthalmol 2016, Nov, 94(7):e617-e623. [CrossRef]
- Regillo, C.D.; Nijm, L.M.; Shechtman, D.L.; Kaiser, P.K.; Karpecki, P.M.; Ryan, E.H.; Ip, M.S.; Yeu, E.; Kim, T.; Rafieetary, M.R.; Donnenfeld, E.D. Considerations for the Identification and Management of Geographic Atrophy: Recommendations from an Expert Panel. Clin Ophthalmol. 2024, Feb, 2:18:325-335. [CrossRef]
- Sparrow, J.R.; Dowling, J.E.; Bok, D. Understanding RPE Lipofuscin. Invest Ophthalmol Vis Sci. 2013, Dec, 54(13): 8325–8326. [CrossRef]
- Rajanala, K.; Dotiwala, F.; Upadhyay, A. Geographic atrophy: pathophysiology and current therapeutic strategies. Front. Ophthalmol. 2023, Dec, Sec. Retina, Vol.3 – 2023.
- Dunaief, J.L.; Dentchev, T.; Ying, G.; Milam, A.H. The Role of Apoptosis in Age-Related Macular Degeneration. Arch Ophthalmol. 2002, Nov, 120(11):1435-42. [CrossRef]
- Camelo, S. Potential Sources and Roles of Adaptive Immunity in Age-Related Macular Degeneration: Shall We Rename AMD into Autoimmune Macular Disease? Autoimmune Dis. 2014, 2014: 532487. [CrossRef]
- Penfold, P.L.; Provis, J.M.; Furby, J.H.; Gatneby, P.A.; Billson, F.A. Autoantibody to retinal astrocytes associated with age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 1990, 228(3), 270-274. [CrossRef]
- Gurne, D.H.; Tso, M.O.; Edward, D.P.; Ripps, H. Antiretinal antibodies in patients with age-related macular degeneration. Ophthalmology 1991, May, 98(5):602-7. [CrossRef]
- Chen, H.; Wu, L.; Pan, S.; Wu, D.Z. An immunological study on age-related macular degeneration. Yan Ke Xue Bao 1993, Sep, 9(3):113-20.
- Patel, N.; Ohbayashi, M.; Nugent, A.K.; Ramchand, K.; Toda, M.; Chau, K.Y.; Bunce, C.; Webster, A.; Bird, A.C.; Ono, S.J.; Chong, V. Ciculating anti-retinal antibodies as immune markers in age-related macular degeneration. Immunology 2005, Jul, 115(3): 422–430. [CrossRef]
- Adamus, G. Can innate and autoimmune reactivity forecast early and advance stages of age-related macular degeneration? Autoimmune Rev. 2017, Mar, 16(3):231-236. [CrossRef]
- Deane, K.D. Preclinical Rheumatoid Arthritis (Autoantibodies): An Updated Review. Curr. Rheumatol. Rep. 2014, May, 16(5):419. [CrossRef]
- Machalińska, A.; Safranow, K.; Sylwestrzak, Z.; Szmatłoch, K.; Kuprjanowicz, L.; Karczewicz, D. Elevated level of circulating endothelial cells as an exponent of chronic vascular dysfunction in the course of AMD. Acta Ophthalmologica Polonica 2011, 113(7-9):228-32.
- Lindquist, K.J.; Osterland, C.K. Human antibodies to vascular endothelium. Clin Exp Immunol. 1971, 9:753–60.
- Michalska-Jakubus, M.; Kowal, M.; Adamczyk, M.; Krasowska, D. Anti-endothelial cell antibodies do not correlate with disease activity in systemic sclerosis. Postepy Dermatol Alergol. 2018, Apr, 35(2): 185–191. [CrossRef]
- Guilpain, P.; Mouthon, L. Antiendothelial cells autoantibodies in vasculitis-associated systemic diseases. Clin Rev Allergy Immunol. 2008, Oct, 35(1-2):59-65. [CrossRef]
- Wiik, A. Autoantibodies in vasculitis. Arthritis Res Ther. 2003, 5(3):147-52. [CrossRef]
- Lip, P.L.; Blann, A. D.; Hope-Ross, M.; Lip, G.Y. Age-related macular degeneration is associated with increased vascular endothelial growth factor, hemorheology and endothelial dysfunction. Ophthalmology 2001, Apr,108(4):705-10. [CrossRef]
- Triolo, G.; Accardo-Palumbo, A.; Carbone, M.C. IgG anti-endothelial cell antibodies (AECA) in type I diabetes mellitus; induction of adhesion molecule expression in cultured endothelial cells. Clin Exp Immunol. 1998, Mar, 111(3):491-6. [CrossRef]
- Jarius, S.; Neumayer, B.; Wandinger, K.P. Anti-endothelial serum antibodies in a patient with Susac's syndrome. J Neurol Sci. 2009, Oct 15, 285(1-2):259-61. [CrossRef]
- Del Papa, N.; Quirici, N.; Scavullo, C.; Gianelli, U.; Corti, L.; Vitali, C.; Ferri, C.; Giuggioli, D.; Manfredi, A.; Maglione, W.; Onida, F.; Colaci, M.; Bosari, S.; Deliliers, G.L. Antiendothelial cell antibodies induce apoptosis of bone marrow endothelial progenitors in systemic sclerosis. J Rheumatol 2010, Oct, 37(10):2053-63. [CrossRef]
- Alessandri, C.; Bombardieri, M.; Valesini, G. Pathogenic Mechanisms Of Anti-Endothelial Cell Antibodies (AECA): Their Prevalence And Clinical Relevance. Adv Clin Chem. 2006, 42: 297–326. [CrossRef]
- Cacciola, R.; Cacciola, E.G.; Vecchio, V.; Cacciola, E. Impact of Anti-Endothelial Cell Antibodies (AECAs) in Patients with Polycythemia Vera and Thrombosis. Diagnostics (Basel) 2022, May, 12(5): 1077. [CrossRef]
- Boos, C.J.; Lip, G.Y.; Blann, A.D. Circulating endothelial cells in cardiovascular disease. J Am Coll Cardiol 2006, Oct 17;48(8):1538-47. [CrossRef]
Figure 1.
The distribution of circulating antiretinal antibodies (ARA) titers in patients with dry age-related macular degeneration (AMD) and in a control group.
Figure 1.
The distribution of circulating antiretinal antibodies (ARA) titers in patients with dry age-related macular degeneration (AMD) and in a control group.
Figure 2.
Monkey retina – indirect immunofluorescence test (IIF): (a) a positive staining of cones (yellow arrows), magnification 400x; (b) a positive staining of rods (yellow arrows), magnification 200x; (c) a positive staining of cytoplasmic components of both retinal nuclear layers (yellow arrows), magnification 400x; (d) a combined positive reaction within cones (red arrows), rods (white arrows) and cytoplasmic components of both retinal nuclear layers (yellow arrows), magnification 200x; (e) a positive reaction within photoreceptors: cones (red arrows) and rods (white arrows), magnification 200x; (f) a negative control, magnification 200x.
Figure 2.
Monkey retina – indirect immunofluorescence test (IIF): (a) a positive staining of cones (yellow arrows), magnification 400x; (b) a positive staining of rods (yellow arrows), magnification 200x; (c) a positive staining of cytoplasmic components of both retinal nuclear layers (yellow arrows), magnification 400x; (d) a combined positive reaction within cones (red arrows), rods (white arrows) and cytoplasmic components of both retinal nuclear layers (yellow arrows), magnification 200x; (e) a positive reaction within photoreceptors: cones (red arrows) and rods (white arrows), magnification 200x; (f) a negative control, magnification 200x.
Figure 3.
(a) Indirect immunofluorescence test (IIF) performed on monkey retina revealed a positive retinal vessels pattern staining (white arrows), magnification 200x; (b) Monkey retina - a negative control, magnification 200x.
Figure 3.
(a) Indirect immunofluorescence test (IIF) performed on monkey retina revealed a positive retinal vessels pattern staining (white arrows), magnification 200x; (b) Monkey retina - a negative control, magnification 200x.
Figure 4.
(a) Iliopsoas muscle - indirect immunofluorescence (IIF) test demonstrates a positive reaction with serum of AMD patient, immunofluorescence of endothelial cells of muscle vessels is observed, magnification 400x; (b) Iliopsoas muscle - a negative reaction with a control serum, magnification 400x.
Figure 4.
(a) Iliopsoas muscle - indirect immunofluorescence (IIF) test demonstrates a positive reaction with serum of AMD patient, immunofluorescence of endothelial cells of muscle vessels is observed, magnification 400x; (b) Iliopsoas muscle - a negative reaction with a control serum, magnification 400x.
Figure 5.
(a) Human umbilical vein endothelial cells (HUVEC) – indirect immunofluorescence (IIF) test shows a positive reaction with AMD patient serum, immunofluorescence of endothelial cells is present, magnification 400x; (b) Human umbilical vein endothelial cells (HUVEC) - a negative reaction with a control serum, magnification 400x.
Figure 5.
(a) Human umbilical vein endothelial cells (HUVEC) – indirect immunofluorescence (IIF) test shows a positive reaction with AMD patient serum, immunofluorescence of endothelial cells is present, magnification 400x; (b) Human umbilical vein endothelial cells (HUVEC) - a negative reaction with a control serum, magnification 400x.
Figure 6.
The graph shows no association between the area of geographic atrophy and serum anti-endothelial cell antibodies (AECA) titers in patients with dry age-relate macular degeneration.
Figure 6.
The graph shows no association between the area of geographic atrophy and serum anti-endothelial cell antibodies (AECA) titers in patients with dry age-relate macular degeneration.
Table 1.
Epidemiologic and clinical characteristic of patients with dry age-related macular degeneration (AMD) and a control group.
Table 1.
Epidemiologic and clinical characteristic of patients with dry age-related macular degeneration (AMD) and a control group.
| Characteristics |
AMD group
n = 41 |
Control group
n = 50 |
P value |
Sex
Females
Males
Age
Arterial hypertension
Ischaemic heart disease
Artherosclerosis
Hyperlipidaemia |
26 (63.4%)
15 (36.6%)
61-90 yrs (mean: 76.3 yrs)
20 (48.8%)
6 (14.6%)
5 (12.2%)
4 (9.8%) |
31 (62.0%)
19 (38.0%)
59-86 yrs (mean: 71.9 yrs)
11 (22.4%)
3 (6.1%)
1 (2.0%)
3 (6.1%) |
0.7390
0.0770
0.5324
0.1931
0.0678
0.6109 |
Table 2.
Distribution of seruum anti-retinal antibodies in patients with dry age-related macular degeneration (AMD) and controls according to the titer and immunofluorescence staining pattern on retinal tissue.
Table 2.
Distribution of seruum anti-retinal antibodies in patients with dry age-related macular degeneration (AMD) and controls according to the titer and immunofluorescence staining pattern on retinal tissue.
| Type of immunofluorescence staining pattern |
Study group |
|
Titre |
P value |
| Negative |
1:10 |
1:20 |
1:40 |
1:80 |
1:160 |
1:320 |
| Cones, n (%) |
AMD
n=41 |
17
(41.5) |
0
(0) |
1
(2.4) |
13
(31.7) |
5
(12.2) |
3
(7.3) |
2
(4.9) |
0.0000
|
Control
n=50 |
50
(100) |
0
(0) |
0
(0) |
0
(0) |
0
(0) |
0
(0) |
0
(0) |
Rodes,
n (%) |
AMD
n=41 |
20
(48.8) |
0
(0) |
0
(0) |
2
(4.8) |
10
(24.4) |
7
(17.1) |
2
(4.8) |
0.0005
|
Control
n=50 |
34
(68.0) |
7
(14.0) |
7
(14.0) |
2
(4.0) |
0
(0) |
0
(0) |
0
(0) |
Cytoplasmic components of retinal nuclear layer cells,
n (%) |
AMD
n=41 |
34
(82.9) |
0
(0) |
0
(0) |
5
(12.2) |
1
(2.4) |
1
(2.4) |
0
(0)
|
0.3230
|
Control
n=50 |
34
(96) |
0
(0) |
1
(2) |
1
(2) |
0
(0) |
0
(0) |
0
(0) |
| Retinal vessels, n (%) |
AMD n=41 |
21
(51.2) |
0
(0) |
0
(0) |
9
(22) |
5
(12.2) |
4
(9.8) |
2
(4.9) |
0.0001 |
| Control n=50 |
45
(90) |
3
(6) |
2
(4) |
0
(0) |
0
(0) |
0
(0) |
0
(0) |
Table 3.
Distribution of anti-endothelial cell antibodies (AECA) in the sera of patients with dry age-related macular degeneration (AMD) and controls according to the titer and immunofluorescence staining pattern on retinal tissue.
Table 3.
Distribution of anti-endothelial cell antibodies (AECA) in the sera of patients with dry age-related macular degeneration (AMD) and controls according to the titer and immunofluorescence staining pattern on retinal tissue.
| Type of immunofluorescence staining pattern |
Study group |
Titer |
P value |
| Negative |
1:100 |
1:320 |
1:000 |
|
| Iliopsoas muscle, n (%) |
AMD
n=41 |
21
(51.2) |
14
(34.1) |
4
(9.8) |
2
(4.9) |
0.0000
|
Control
n=50 |
45
(90) |
5
(10) |
0
(0) |
0
(0) |
| HUVEC, n (%) |
AMD
n=41 |
28
(68.3) |
8
(19.5) |
3
(7.3) |
2
(4.9) |
0.0001
|
Control
n=50 |
45
(90) |
5
(10) |
0
(0) |
0
(0) |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).