1. Introduction
The incisional hernia represents the externalization of a viscera covered by the parietal peritoneum, under the skin, through a muscle-aponeurotic defect. It occurs post-traumatically (rarely) or postoperatively (most frequently). Incisional hernia (IH) can be detected by clinical examination and imaging methods (1). The various studies on the generation of IH have shown that there is a dynamic of the preponderance of its formation after performing abdominal surgery (2,3). The appearance of incisional hernias mainly manifests itself in the first 12 months after an operation. Over time, based on a statistical analysis of clinical data, the incidence of IH was estimated at 9.8% after 21 months, while after 10 years the incidence is 18.7%.
The surgical repair of the incisional hernia has experienced a special dynamic. This was influenced on the one hand by the appearance of prosthetic materials with controlled biocompatibility, as well as allograft fixation devices and wires. On the other hand, the advent of minimally invasive surgery (celioscopic and robotic) has expanded and refined abdominal wall repair techniques (4,5,6). The use of a certain operating technique in incisional hernia is a decision-making act of the specialist corroborated with the technical endowment at the time of the patient's presentation and with the data package resulting from the consultation and investigations. The state of the art in prosthetic materials has meant that most incisional hernia repairs include the use of surgical mesh. The positioning of the prosthesis about the anatomical elements of the abdominal wall added to the success of the long-term intervention and the reduction of complications (granulomas, suppurations, rejection of the mesh, fistulas of the cavity organs in contact with the mesh, etc.). The recurrence rate has decreased drastically by using prosthetic materials. Parietal defects are more common and larger after open versus minimally invasive surgery (7).
The objective of this study is to present the results of open surgical interventions, to resolve recurrences in incisional hernia, based on the use of well-integrated surgical mesh, with good elasticity of the musculoaponeurotic tissue, and with dimensions of the parietal defect smaller than 10 cm on the diameter of the bigger.
2. Materials and Methods
The present study is a retrospective for a period of 5 years, January 2018 - December 2022, within a single surgery department of the Ploiești County Emergency Hospital. From the total number of surgical interventions, 631 cases of incisional hernia were identified and analyzed, among which recurrences of eventrations were identified. The following inclusion (a) and exclusion (b) criteria were used in this study.
The repair of the parietal defect was done with mesh, in the past. Using the existing integrated prosthesis, with reduced parietal tension.
The cases that were not included in this study were selected taking into account the lack of parietal prosthesis in the antecedents or the prosthesis of another defect distant from the current defect. Another exclusion criterion was the use of another prosthesis to cover the defect, alongside the existing one.
2.1. Surgical Technique
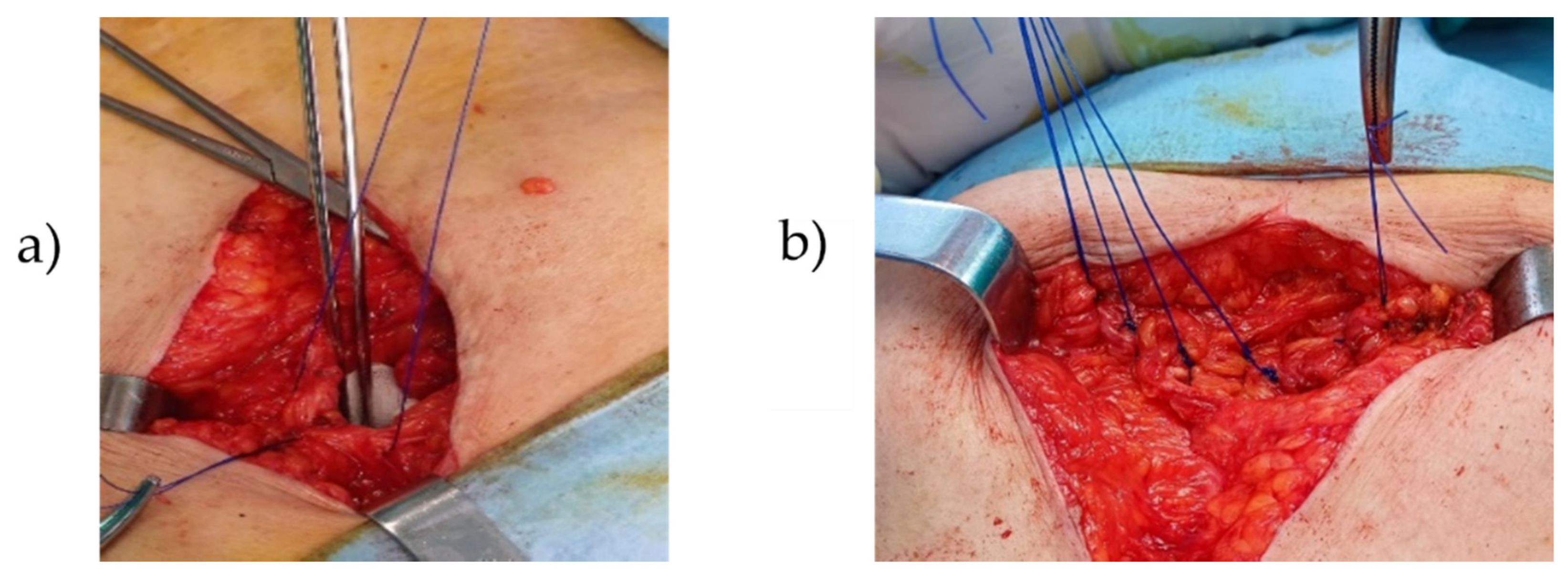
Classical open surgery with the use of the existing, well-integrated mesh was used to resolve eventration recurrences. After highlighting, opening, and dissecting the eventration sac, the parietal defect was evaluated. It was taken into account that the parietal defect was in the area of the well-integrated mesh, with a mesh width of at least 5 cm contoured to the parietal defect (8). The edges of the defect were prepared. The tension created by approaching the edges of the defect, in the direction of the smallest diameter, was verified intraoperatively. If necessary, relaxation incisions were made (9). The defect was closed using well-integrated mesh using monofilament polypropylene threads. The suture in tension is a major contraindication. The tegumentary suture was performed with an intradermal thread.
2.2. Post-Operative Monitoring
Post-operative monitoring for all cases meeting the specific criteria of this study was difficult to achieve. It was taken into account that most patients return to the same hospital and service for immediate and late complications.
2.3. Statistical Analysis
Data analysis was performed using the statistical analysis program MINITAB version 18. Continuous variables were presented as the mean value accompanied by the standard deviation while categorical variables were expressed as numbers.
3. Results
3.1. Recurrences
In this study, based on the inclusion and exclusion criteria, 13.6% of recurrent herniations after prosthetic procedures and 4.6% after tissue procedures were identified from the studied group, totaling a total of 18.22% recurrences (115 patients).
3.1.1. The Localization of Incisional Hernias
The location of the incisional hernia operations for the 631 cases analyzed is shown in
Table 1, noting both the weight of the type of area and the ratio between men and women.
Of this number of patients, 165 were men (26.15%), 466 were women (73.85%), the average age being 69 years for men and 66 years for women.
3.1.2. Duration of Operation
From the analysis of the records regarding the duration of the operations to solve the cases, the minimum time was 20 minutes while the maximum time was 130 minutes. The average value of the operating time was 63.8 minutes ± 31.16 minutes.
3.1.3. Hospitalization Period
The mean length of hospital stay was 9.22 days ± 3.95 days, with a minimum of 22 hours and a maximum of 24 days.
3.1.4. Complications Identified
Among the current acute complications, diagnosed intraoperatively, in order of frequency, the following are mentioned: incarceration, intestinal occlusion, intestinal necrosis, and perforation. The weights of these current acute complications are graphically represented in
Figure 1.
The size of the parietal defect
The size of the parietal defect at IH where we used the presented method varied in the range of 4 to 10 cm, on the largest diameter, the average value being 6.53 cm ± 2.35 cm. Most defects were dimensionally located in the range of 5-7 cm, which represents a weight of 76%.
4. Discussions
Hernia as a term indicates the presence of an abnormal protrusion of an organ or part of an organ outside the visceral cavity that contains it. The occurrence of incisional hernias hurts the quality of life, and the socio-professional insertion, leading to an increase in expenses in the public health system. The solution is surgical, except for contraindications. A study shows that annually more than 20 million hernias are operated worldwide (10). Given that the incidence of incisional hernias is on average 4.3%, while the prediction of occurrence over time using the Kaplan-Meier estimate was 9.8% for 21.1 months, the size can be identified of this type of surgery and the social and economic impact it generates (11). In another study of IH recurrence (12) carried out for the period January 2012 - August 2022, the Kaplan Meier analysis indicated for the 12 months a recurrence of 8% in the presence of surgical mesh and 32.6% in the absence of surgical mesh, while for 2 years, recurrence was assessed at 19.7% for the group with surgical mesh and 52.4% for the group without surgical mesh. It is noteworthy that the use of prosthetic materials has become a standard procedure in both the repair of primary defects (hernias) and the repair of incisional hernias (13). Mesh hernia repair has thus replaced traditional defect closure techniques, contributing to an increase in the mechanical strength of the abdominal wall. The revolutionary approach of Lichtenstein et al. (14), was the introduction of the concept of tension-free repair, impacting the surgical procedures used to repair an abdominal wall defect. Incisional hernia repair has benefited from these effective approaches, where the use of a biomaterial is almost mandatory today, leading to decreased recurrence rates (15,16).
In a recent study (17), it was highlighted that the two mainly used surgical techniques, open and laparoscopic surgical repair, find their place of application in the complexity of surgical cases.
In the case of the conducted study, the evaluation of the resolution by open surgery of the cases of recurrent eventration, using the existing mesh, was aimed.
In most cases of incisional hernia, the repair was done using surgical mesh. In rare cases, with parietal or intraperitoneal suppurations, perforations, or intestinal necrosis with perforations in the sac or the peritoneal cavity, the mesh was not mounted.
In patients with recurrent herniation after a prosthetic procedure, the principle was the following: if the prosthesis is well integrated, without granulomas, suppurations, another prosthesis was mounted, in addition, or the existing prosthesis was used. Recurrence was considered when the defect appeared on the same abdominal area where the prosthesis was mounted. Thus, the following situations were considered as generative causes for relapse:
- the prosthesis put under tension from the beginning,
- the prosthesis fixed at the periphery in fixing points too far apart (x cm)
- net migration
- breaking the net.
In addition to the mentioned causes, we must also take into account the fact that some prostheses contract over time (18), the causes being the constructive nature of the net through the type of fabric, density, and size of the meshes, but they can also be caused due to the fixing technique (19). Also, comorbidities that lead to increased intra-abdominal pressure contribute to such relapses, especially from the first postoperative days (chronic obstructive pulmonary disease, dysuria, constipation, etc.).
For the percentage of 13.6% of recurrent eventrations, meaning 86 patients, a percentage of 9.3% of the cases was solved by using the existing prosthesis, according to the surgical technique described, the male: female ratio being 1:3.
The use of the existing prosthesis was done successfully, taking into account a series of criteria such as:
- absence of suppuration in the wound and the peritoneal cavity
- the tension to which the wall and the net are subjected should not be high
- the net must be well integrated.
For the situation where the puncture occurs on the periphery of the prosthesis after the edges have been sharpened, the possible suture threads have been removed, the mesh is fixed to the wall again. The distance of at least 5 cm from the edge of the defect to the periphery of the net was respected.
The location of incisional hernias for the analyzed group of patients presents a wide spectrum, mainly in the mesogastric (48.9%) and hypogastric (19.6%) areas (see
Table 1).
The duration of the operation was calculated from the opening of the patient to the completion of the closure, the average value being 63.8 minutes. The wide spectrum of duration between the limits of 20 minutes to 130 minutes is because it is the specifics of the emergency hospital, where patients with acute and less often chronic complications are presented.
In the case of the parietal defect, the size of the largest diameter was located in the range of 4-10 cm, the average value being 6.53 cm ± 2.35 cm. From the data analysis, a concentration of the largest diameter values was observed in the 5-7 cm range, with a weight of 76%. An important role in the decision to use the existing prosthesis is the size of the defect. If the relapse occurs after a longer time, the musculoaponeurotic structures retract, not being held together, thus generating an enlargement of the defect over time.
From the perspective of age, it is found that the patients are from the old category, with the average age for men being 69 years while for women it is 66 years. In contrast, as a group dynamic by sex, the male:female ratio is 1:3.
Monitoring for the entire group of patients was difficult to achieve, as the patients came as an emergency. For the case of recurrence of the eventration solved by the mentioned surgical technique, the monitoring for 6 months to a year showed that the patients did not suffer recurrences, and the pain and swelling disappeared.
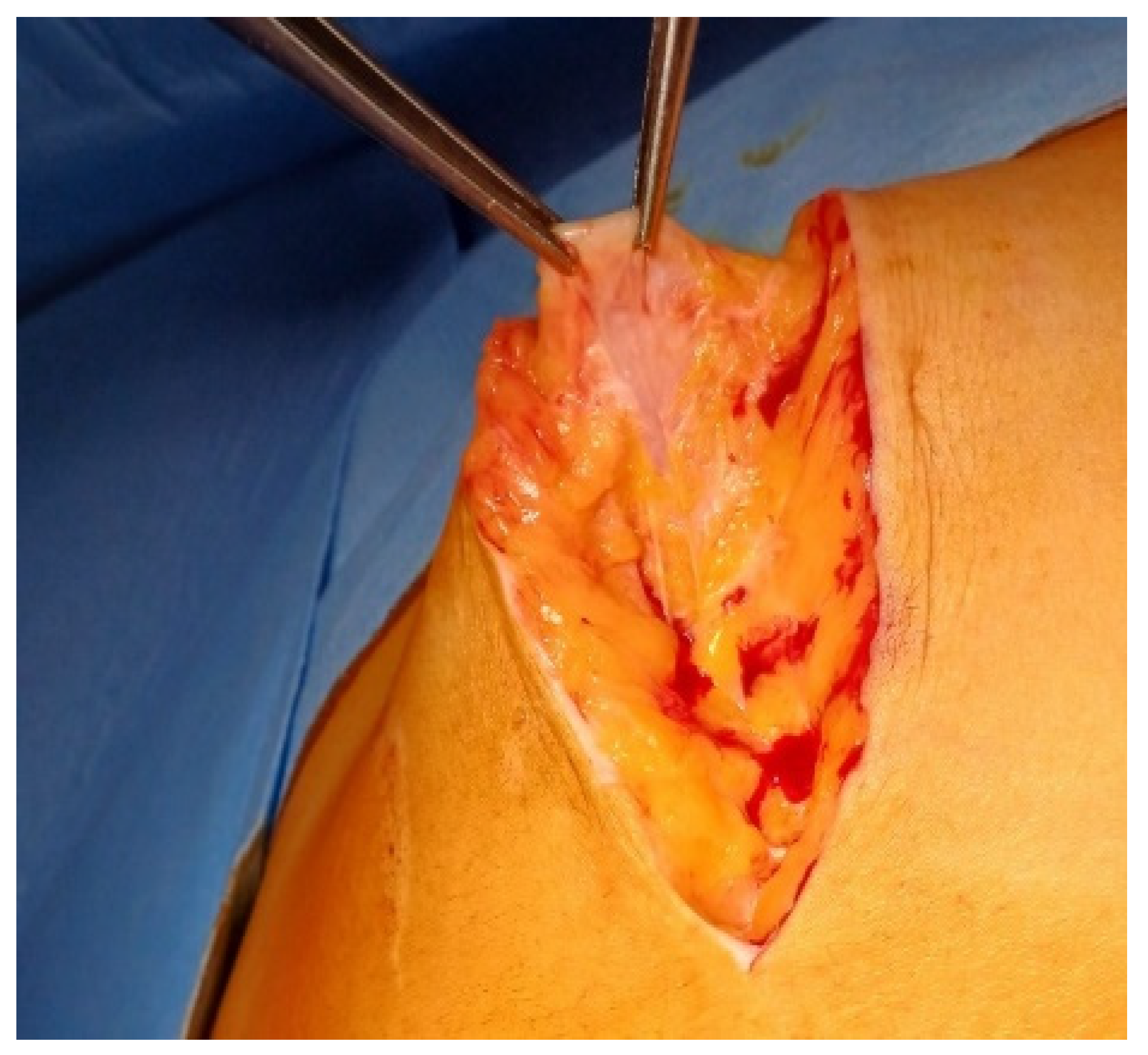
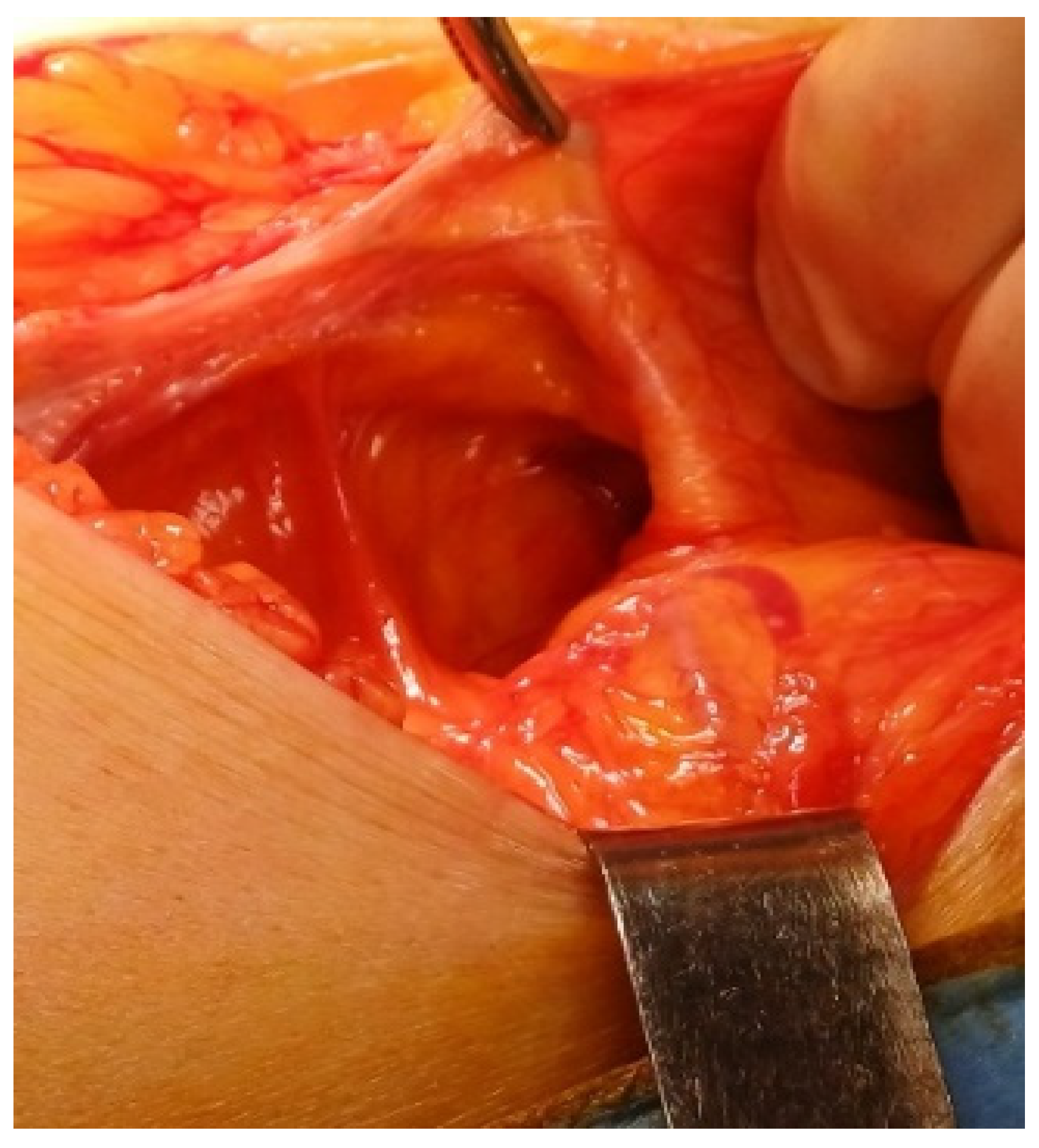
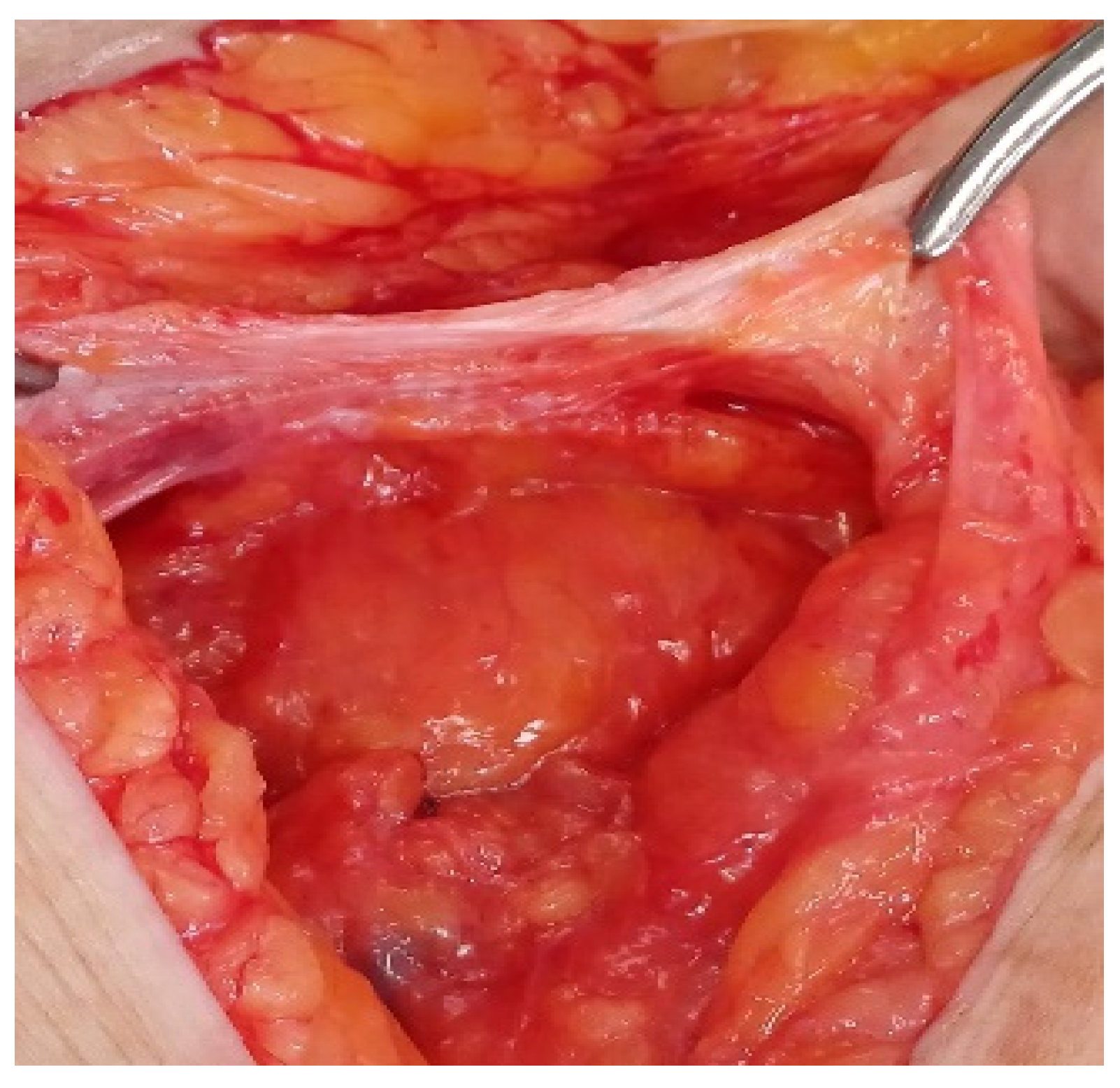
5. Case Study
In the following, it is exemplified with a case in which the recurrence occurred through the polypropylene mesh, at the level of the epigastrium. The defect most likely occurred by affecting the integrity and therefore the resistance of the net when it was mounted. This explains the 7 cm defect in the long axis, circumscribed all around by the well-integrated mesh.
The 78-year-old patient from the countryside (physical effort) presented with painful epigastric swelling, partially reducible through taxis, through which a large hole in the musculoaponeurotic plane can be partially palpated. History of post-operative eventration: 2 years ago, surgery with prosthesis (affirmative). The patient did not present the hospital discharge ticket from the previous surgical intervention.
It was practiced, under general anesthesia with orotracheal intubation:
- viscerolysis
- preparation of the edges of the defect (the hole with a diameter of about 7 cm)
- suture with monofilament PP thread.
Before deciding to use the existing prosthesis, it was checked, as shown in
Figure 5, if tension is created by closing the defect on the smallest dimension. The patient evolved well, being discharged 22 hours after the intervention. She was monitored for 6 months postoperatively, recording the disappearance of pain, and swelling.
6. Conclusions
In an analysis over five years, January 2018 - December 2022, of 631 incisional hernias, recurrences were identified in a percentage of 18.22%, 13.6% being recurrences after prosthetic procedures. A percentage of 9.3% of relapses after prosthetic procedures were solved by open surgery, using the existing well-integrated prosthesis, without mechanical tension. For this type of surgery, the criteria that can lead to a successful intervention have been defined. The patients operated in this way were monitored for 6 months to a year, showing that the patients did not suffer recurrences, and the pain and swelling disappeared.
Author Contributions
Conceptualization: DIM; Software: MFD; Validation: DIM, MFD; Formal analysis: DIM, NI; Investigations: DIM; Resources: DIM, MFD; Original draft: DIM; Writing – original draft: DIM, MFD; Review writing: DIM, DMF. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Brown SR, Goodfellow PB. Transverse Verses Midline Incisions for Abdominal Surgery. Cochrane Database Syst Rev (2005) 2005(4):CD005199. [CrossRef]
- Bhaskaran A, Ambikavathy M. Incisional Hernia: A Review of Etiopathogenesis, Clinical Presentation, Complications and Management. J Clin Biomed Sci, 2013; 3(1):1-11.
- Stabilini, C., Garcia-Urena, M., Berrevoet, F. et al. An evidence map and synthesis review with meta-analysis on the risk of incisional hernia in colorectal surgery with standard closure. Hernia 26, 411–436 (2022). [CrossRef]
- Gustavo E. Muñoz Delgado*, María A. Lastra Santiago, Review of Incisional Hernias, International Surgery Journal Delgado GEM et al. Int Surg J. 2023 Apr;10(4):810-813.
- Heller L, Chike-Obi C, Xue AS. Abdominal wall reconstruction with mesh and components separation. Semin Plast Surg. 2012 Feb;26(1):29-35. PMID: 23372456; PMCID: PMC3348745. [CrossRef]
- Dietz UA, Menzel S, Lock J, Wiegering A: The treatment of incisional hernia. Dtsch Arztebl Int 2018; 115: 31–7. [CrossRef]
- Gábor Martis , Máté Rózsahegyi, János Deák, László Damjanovich, Incarcerated and eventrated abdominal wall hernia reconstruction with autologous double-layer dermal graft in the field of purulent peritonitis—A case report International Journal of Surgery Case Reports 30 (2017) 126–12. [CrossRef]
- Howard R, Ehlers A, O'Neill S, Shao J, Englesbe M, Dimick JB, Telem D, Huynh D. Mesh overlap for ventral hernia repair in current practice. Surg Endosc. 2023 Dec;37(12):9476-9482. Epub 2023 Sep 11. PMID: 37697114. [CrossRef]
- López-Cano M, García-Alamino JM, Antoniou SA, Bennet D, Dietz UA, Ferreira F, Fortelny RH, Hernandez-Granados P, Miserez M, Montgomery A, Morales-Conde S, Muysoms F, Pereira JA, Schwab R, Slater N, Vanlander A, Van Ramshorst GH, Berrevoet F. EHS clinical guidelines on the management of the abdominal wall in the context of the open or burst abdomen. Hernia. 2018 Dec;22(6):921-939. Epub 2018 Sep 3. PMID: 30178226. [CrossRef]
- Kingsnorth, A.; LeBlanc, K. Hernias: Inguinal and incisional. Lancet 2003, 362, 1561–1571. [CrossRef]
- Höer J, Lawong G, Klinge U, Schumpelick V. Einflussfaktoren der Narbenhernienentstehung. Retrospektive Untersuchung an 2.983 laparotomierten Patienten über einen Zeitraum von 10 Jahren [Factors influencing the development of incisional hernia. A retrospective study of 2,983 laparotomy patients over a period of 10 years]. Chirurg. 2002 May;73(5):474-80. German. PMID: 12089832. [CrossRef]
- Bhardwaj P, Huayllani MT, Olson MA, Janis JE. Year-Over-Year Ventral Hernia Recurrence Rates and Risk Factors. JAMA Surg. 2024 Mar 27:e240233. Epub ahead of print. PMID: 38536183; PMCID: PMC10974689. [CrossRef]
- The HerniaSurge Group. International guidelines for groin hernia management. Hernia 2018, 22, 1–165.
- Lichtenstein, I.L.; Shulman, A.G. Ambulatory outpatient hernia surgery. Including a new concept, introducing tension-free repair. Int. Surg. 1986, 71, 1–4.
- Lior Heller, Chuma Chike-Obi, Amy Shengnan Xue, Abdominal Wall Reconstruction with Mesh and Components Separation, Seminars in Plastic Surgery Vol. 26 No. 1/2012.
- Sanders, D.L.; Kingsnorth, A.N. From ancient to contemporary times: A concise history of incisional hernia repair. Hernia 2011, 16, 1–7. [CrossRef]
- Nadine van Veenendaal et al., The INCH-trial: a multicenter randomized controlled trial comparing short- and long-term outcomes of open and laparoscopic surgery for incisional hernia repair, Surgical Endoscopy (2023) 37:9147–9158 . [CrossRef]
- Lee D, Zimmern PE. Management of complications of mesh surgery. Curr Opin Urol. 2015 Jul;25(4):284-91. PMID: 26049869. [CrossRef]
- Sekmen U, Gurleyik G, Kayadibi H, Saglam A. The role of suture fixation on mesh contraction after abdominal hernia repair. J Invest Surg. 2009 Mar-Apr;22(2):117-21. PMID: 19283614. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).