Introduction
Coronary artery disease (CAD) remains one of the leading causes of morbidity and mortality worldwide [
1]. The primary treatment approach for CAD has been revascularization, aiming to restore the blood flow to the ischemic myocardium. Historically, coronary artery bypass grafting (CABG) via median sternotomy has been the gold standard for multivessel disease, offering favorable long-term outcomes [
2]. However, with advances in technology and surgical techniques, minimally invasive approaches have emerged as promising alternatives, seeking to reduce surgical trauma and enhance postoperative recovery [
3].
Minimally Invasive Direct Coronary Artery Bypass (MIDCAB) is a procedure, which provides direct access to the heart through a small thoracotomy, eliminating the need for sternotomy [
4]. It has been particularly favoured for the revascularization of the left anterior descending artery (LAD). MIDCAB procedure is also an option as a hybrid coronary revascularization (HCR) in the setting of incomplete surgical revascularization for selected patients. Furthermore, MIDCAB surgery can be applied as multivessel procedure for several coronary territories like the diagonal branch (RD) or circumflex artery (RCX) [
5]. The benefits of the MIDCAB technique have been reported which include less surgical trauma, reduced operative bleeding and fast recovery [
6,
7,
8]. However, it remains technically challenging and demands meticulous patient selection and an experienced surgical team for optimal outcomes. This study aims to analyze the short-term clinical results of our single center experience with the MIDCAB procedure and to evaluate the safety and feasibility of this technique.
Material and Methods
Study Design and Population
In this study we analysed the clinical results of 91 patients who underwent MIDCAB procedure at the Department of cardiac surgery at the University Hospital Bonn from January 2021 to December 2022, retrospectively. Patients were clinically followed up via telephone. Follow up data including coronary angiography results were retrieved from referring cardiologists. Patients´ mean age was 65 ± 10 years. The patients´ preoperative characteristics are listed in
Table 1. This study was approved by the local ethics committee (#446/21).
Patient Selection Criteria
Inclusion criteria for MIDCAB procedure were relevant stenosis or occlusion of the proximal or medial LAD. In patients with two or three vessel CAD the RD, RCX or ramus intermedius (RIM) were targets for multi-vessel (MV) MIDCAB revascularization. In patients who underwent HCR the right coronary artery and/or RCX were treated with PCI postoperatively. Following circumstances were exculsion criteria for MIDCAB procedure: chest radiation, left thoracotomy (for lung or breast surgery), redo CABG in patients´medical history, stenosis of the left subclavian artery, emergency operation and/or hemodynamically instable patients.
Surgical Technique
We already published the surgical technique for MIDCAB procedure [
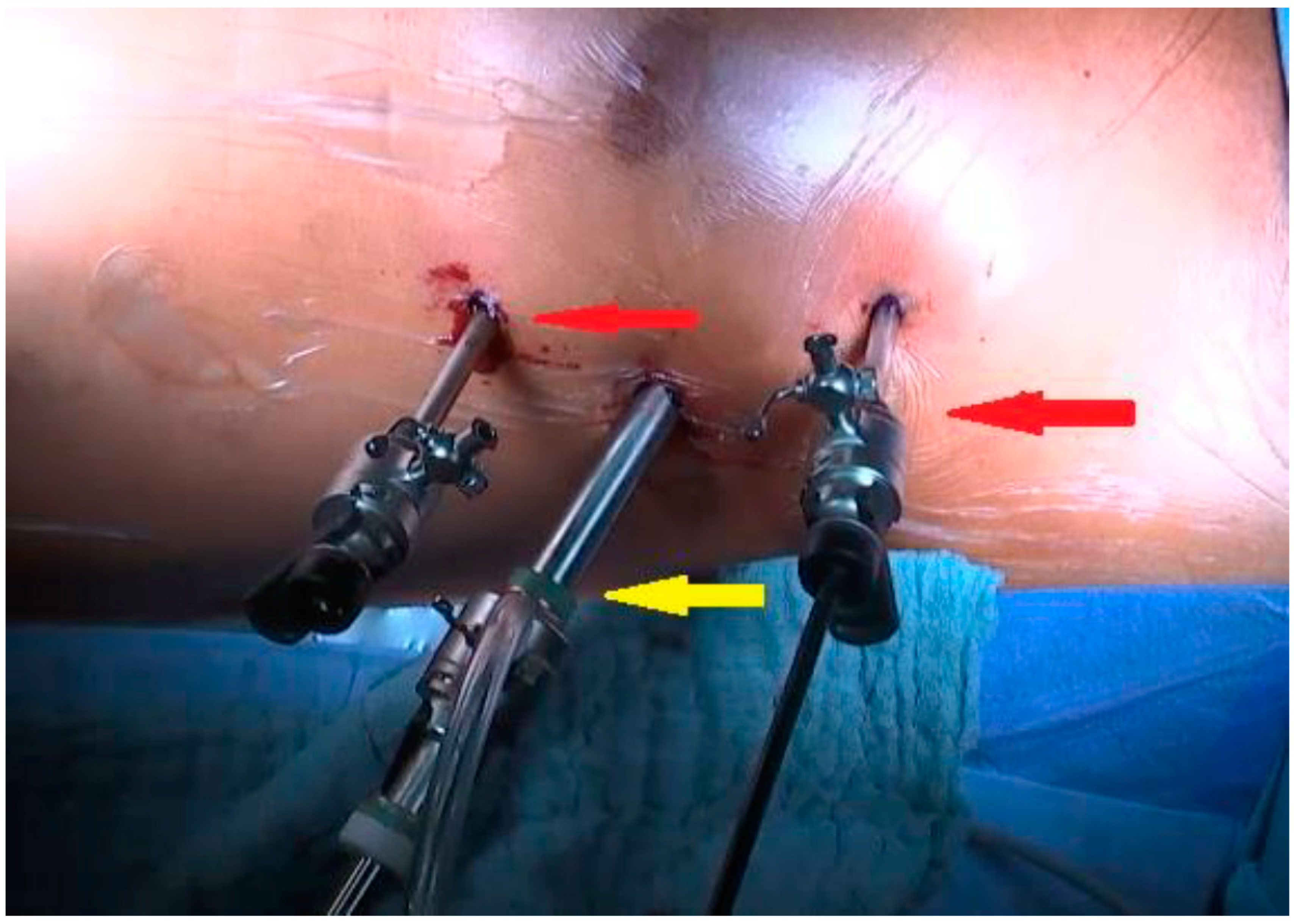
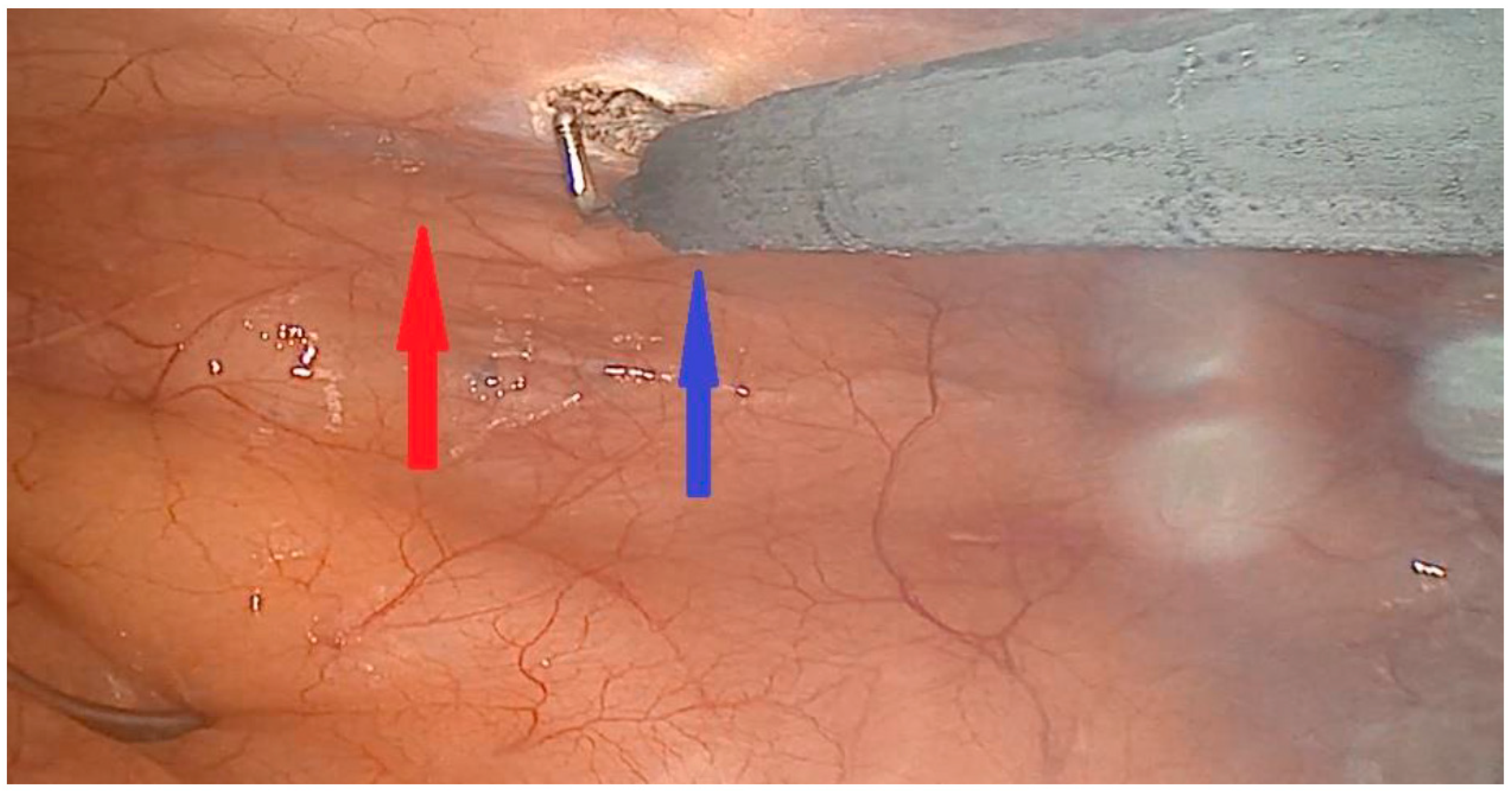
9]. In short the patients were placed in a supine position, with 30° elevation of the left thorax. They were intubated with a double-way endotracheal tube to deflate the left lung. In case of endoscopic harvesting of the left internal mammary artery (LIMA) 3 incisions for port access were done (
Figure 1 and
Figure 2) to place the 3 D endoscope, the forceps and the hook electrocautery. For open harvesting of the LIMA a small skin incision was done, and the left pleural space was opened through the 4
th or 5
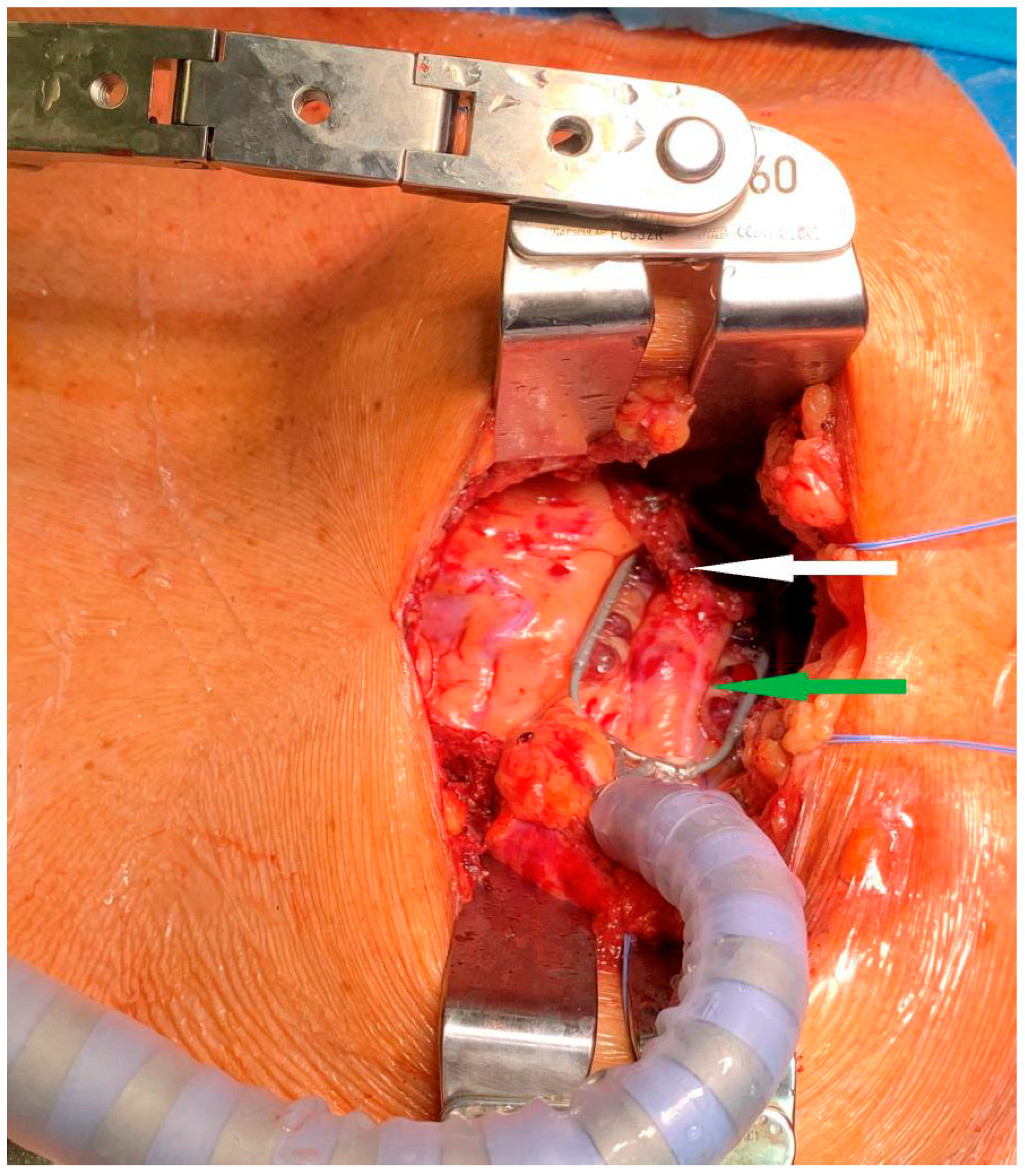
th intercostal space. With the help of a MICS retractor for LIMA (lifting retractor, Geister, Tuttlingen, Germany) a pedicled LIMA graft was harvested. Systemic heparinization was given, the pericardium was opened, and the LAD was localized. The distal anastomosis was done in Off-pump technique with the help of a vacuum tissue stabilizer (Octopus Evolution, Medtronic, Minneapolis, USA),
Figure 3, and an intracoronary shunt (Medtronic, Minneapolis, USA). Intraoperative bypass flow was measured routinely. In MV-MIDCAB (15%,
Table 2) a segment of saphenous vein was harvested from the lower leg. The venous graft was anastomosed to the target vessel in a same way. The proximal anastomosis (saphenous vein graft as T-Graft to LIMA) was performed. Protamin was given 1:1, a thorax drainage was inserted to the left pleura, and thoracotomy was closed.
Postoperative Care and Clinical Follow-up
Hemodynamic parameters, wound healing, and potential post-operative complications like infections or bleeding were documented. A systematic clinical follow-up regarding health status and postoperative complications was established via phone call. Follow up data including coronary angiography results were retrieved from referring cardiologists. Mean follow-up time was 1.5 ± 0.5 years.
Statistical Analysis
Statistical analyses were calculated with the biometrically analysis of sampling software (BIAS 11.06, Frankfurt, Germany). Categorical data were presented as percentages, and continuous data were described as mean value ± standard deviation. Survival was analyzed with Kaplan-Meier method.
Results
Preoperative Data
In our cohort 87% of the patients were male (n = 79). The mean NYHA class was 3 ± 0.4. The majority of the patients (54%, n = 49), presented with three-vessel CAD (
Table 1).
In 32% of the patients myocardial infarctions was diagnosed preoperatively and 15% (n = 14) had already PCI interventions before. The mean EUROScore I log was 5 ± 11% in our cohort.
Table 1.
Preoperative patient characteristics.
Table 1.
Preoperative patient characteristics.
| Parameter |
|
| Number of patients, n |
91 |
| Age, M ± SD (years) |
65 ± 10 |
| Gender, male n (%) |
79 (87%) |
| NYHA class (M ± SD) |
3 ± 0.4 |
| CCS class (M ± SD) |
3 ± 0.3 |
| CAD 1 Vessel, n (%) |
18 (20%) |
| CAD 2 Vessels, n (%) |
24 (26%) |
| CAD 3 Vessels, n (%) |
49 (54%) |
| Ejection Fraction, M ± SD (%) |
50 ± 11 |
| Comorbidities |
|
| Diabetes mellitus, n (%) |
26 (29 %) |
| COPD, n (%) |
9 (10%) |
| Renal insufficiency, n (%) |
8 (9%) |
| Myocardial infarction, n (%) |
29 (32%) |
| Arterial hypertension, n (%) |
63 (69%) |
| EUROScore I log., (M ± SD %) |
5 ± 11 |
| Peripheral Arterial Disease (PAD), n (%) |
19 (21%) |
| Stent, n (%) |
14 (15%) |
Operative und Postoperative Results
85% of the patients (n = 77) received one coronary artery anastomosis. In 14 patients (15%) MV-MIDCAB was performed. The operative and postoperative results are listed in
Table 2. The mean operation time was 2.6 ± 0.8 hours. Conversion to sternotomy was not necessary. The 30-day mortality was 0. Mean required packed red blood cells (pRBC) was 0.4 ± 1.2 unit. The intensive care unit stay (ICU) was 1.5 ± 1.6 days mean. We observed two patients (2%) with wound infections postoperatively, who were treated with Vac-therapy. Four patients underwent rethoracotomy because of bleeding (thoracic muscle). One patient underwent re-coronary angiography due to myocardial infarction postoperatively. The LIMA-LAD anastomosis was unremarkable. This patient received PCI with stent of the diagonal branch (relevant stenosis).
Table 2.
Operative and perioperative data.
Table 2.
Operative and perioperative data.
| Operative |
| One coronary art anastomosis, n (%) |
77(85%) |
| Two coronary artery anastomoses, n (%) |
10 (11%) |
| Three coronary artery anastomoses, n (%) |
4 (4%) |
| Operation time, M ± SD (h) |
2.6 ± 0.8 |
| Conversion to sternotomy, n (%) |
0 |
| Number of anastomoses, n |
109 |
| postoperative |
|
| Intensive care unit (ICU) length of stay M ± SD (Days) |
1.5 ± 1.6 |
| Ventilation time, M ± SD (hours) |
4 ± 6 |
| Rethoracotomy, n (%) |
4 (4%) |
| Stroke, n (%) |
0 |
| Wound infection, n (%) |
2 (2%) |
| 30-day-mortality, n (%) |
0 |
| Myocardial infarction, n (%) |
1 (1%) |
| Stent, n (%) |
1 (1%) |
| Coronary angiography, n (%) |
1 (1%) |
| Blood transfusion (pRBCs), n (%) |
0.4 ± 1.2 |
| Complete revascularization, n (%) |
73 von 91 (80%) |
| Hybrid revascularization, n (%) |
18 von 91 (20%) |
Follow-up Results
Follow up was completed in 98%. The average NYHA class was 1.1 ± 0.4 (
Table 3). In 96% of the patients (n = 85) CCS class of 0 was observed. One patient underwent re-coronary angiography due to de novo stenosis of the RCA. Late mortality was 2%. The Kaplan-Meier survival rate was 98.8% at 1 and 2 years (
Figure 4).
Discussion
The paradigm of coronary revascularization is continuously evolving, with minimally invasive direct coronary artery bypass (MIDCAB) surgery emerging as a promising alternative to traditional CABG for selected patients [
10]. Our study, predominantly involving a male population (87%), aligns with the broader epidemiological trend of higher coronary artery disease prevalence in men [
11].
The 30-day mortality rate is 0% in our cohort and the postoperative complication rates regarding bleeding (4%), neurologic event (0%) and wound infection (2%) are low. These findings underscore the safety and favourable in-hospital clinical outcome associated with the MIDCAB procedure.
Similar results regarding the mortality rate were published before: Raja and colleagues reported a 30-day mortality rate of 2% among 668 patients undergoing the MIDCAB procedure [
12], while Holzhey noted a mortality of 0.8% in 1768 patients [
13]. Calafiore et al. observed a 30-day mortality of 0.6% in 155 patients who underwent MIDCAB procedure [
14]. We observed no cases of neurological events in our cohort that is an excellent result. Manuel and colleagues report a neurological rate of 1.8% in their MIDCAB [
15]. The rethoracotomy (for bleeding) rate in our study is 4%, that is comparable to published data which ranges between 1 and 4% [
15,
16]. Wound healing disturbances were observed in only 2% of our cohort, that is comparable to other studies as 3.4% reported by Reuthebuch and colleagues in patients undergoing MIDCAB procedures [
16], respectively 2,4 % reported by Raja [
12].
The average ICU stay in our study is 1.5 ± 1.6 days that is similar to the results reported by Reuthebuch [
16]. We observed a ventilation time of 4 ± 6 hours, that is short. There are published data regarding the ventilation time of MIDCAB patients about 24 hours [
16].
However, it is important to note that in Manuel’s study, 1.8% of patients were converted to sternotomy [
15], while our study had a 0% conversion rate. These findings underline the feasibility and procedural safety of MIDCAB procedure.
In our study, we observed one patient (1.1%) who required reintervention due to de novo stenosis of the RCA during the follow-up period. This is comparable to the reintervention rate for anastomosis stenosis of 1% reported by Reuthebuch [
16] and 0.7 % reported by Manuel [
15]. Holzhey and colleagues reported a reintervention rate of 3.3% [
13]. Our short-term survival rate of 98.8% at 1 and 2 years postoperatively is an excellent outcome. These follow-up results are comparable with published data ranging from 92% to 96% at mid-term survival [
15,
16]. At the latest follow-up, the majority of our patients (96%) were classified in the CCS class of 0, emphasizing the favourable clinical outcomes of our cohort. Our postoperative and short-term clinical results confirm that the MIDCAB procedure is safe and feasible. An optimal patient selection and the expertise of the surgical team are crucial.
References
- Smith, S.C.; Benjamin, E.J.; Bonow, R.O.; et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll of Cardiol 2011, 58, 2432–2446. [Google Scholar] [CrossRef]
- Chang, M.; Lee, C.W.; Ahn, J.M.; et al. Coronary artery bypass graft surgery versus drug-eluting stent implantation for high-surgical-risk patients with left main or multivessel coronary artery disease. Eur J Cardiothorac Surg 2017, 51, 943–949. [Google Scholar] [CrossRef] [PubMed]
- Van Praet, K.M.; Kofler, M.; Nazari Shafti, T.Z.; et al. Minimally invasive coronary revascularisation surgery: a focused review of the available literature. Interv Cardiol 2021, 16, e08. [Google Scholar] [CrossRef] [PubMed]
- Varrone, M.; Sarmiento, I.C.; Pirelli, L.; et al. Minimally invasive direct coronary artery bypass: an evolving paradigm over the past 25 years. Innovations 2022, 17, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, K.K.; Wadhawa, V.; Jawarkar, M.; et al. Total arterial multivessels minimally invasive direct coronary artery bypass grafting via left minithoracotomy. Gen Thorac Cardiovasc Surg 2021, 69, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Al-Ruzzeh, S.; Mazrani, W.; Wray, J.; et al. The clinical outcome and quality of life following minimally invasive direct coronary artery bypass surgery. J Card Surg 2004, 19, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Tekin, A.I.; Arslan, Ü. Perioperative outcomes in minimally invasive direct coronary artery bypass versus off-pump coronary artery bypass with sternotomy. Wideochir Inne Tech Maloinwazyjne 2017, 12, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Xiao, L.B.; Gao, Z.S.; et al. Clinical effect and prognosis of off-pump minimally invasive direct coronary artery bypass. Med Sci Monit 2017, 23, 1123–1128. [Google Scholar] [CrossRef] [PubMed]
- Monsefi, N.; Alaj, E.; Sirat, S.; Bakhtiary, F. Postoperative results in minimally invasive direct coronary artery bypass procedure in 234 patients. Front in Cardiovasc Med 2023, 9, 1051105. [Google Scholar] [CrossRef] [PubMed]
- Kettering, K.; Dapunt, O.; Baer, F.M. Minimally invasive direct coronary artery bypass grafting: a systematic review. J Cardiovasc Surg (Torino) 2004, 45, 255–264. [Google Scholar] [PubMed]
- Blum, A. Gender differences in vascular aging and in coronary artery disease pathophysiology. QJM. 2023, 116, 745–749. [Google Scholar] [CrossRef] [PubMed]
- Raja, S.G.; Garg, S.; Rochon, M.; et al. Short-term clinical outcomes and long-term survival of minimally invasive direct coronary artery bypass grafting. Ann Cardiothorac Surg 2018, 7, 521–627. [Google Scholar] [CrossRef] [PubMed]
- Holzhey, D.M.; Cornely, J.P.; Rastan, A.J.; et al. Review of a 13-year single-center experience with minimally invasive direct coronary artery bypass as the primary surgical treatment of coronary artery disease. Heart Surg Forum 2012, 15, E61–E68. [Google Scholar] [CrossRef] [PubMed]
- Calafiore, A.M.; Angelini, G.D.; Bergsland, J.; Salerno, T.A. Minimally invasive coronary artery bypass grafting. Ann Thorac Surg 1996, 62, 1445–1448. [Google Scholar] [CrossRef] [PubMed]
- Manuel, L.; Fong, L.S.; Betts, K.; et al. LIMA to LAD grafting returns patient survival to age-matched population: 20-year outcomes of MIDCAB surgery. Interact Cardiovasc Thorac Surg 2022, 35, ivac243. [Google Scholar] [CrossRef] [PubMed]
- Reuthebuch, O.; Stein, A.; Koechlin, L. Five-Year Survival of Patients Treated with Minimally Invasive Direct Coronary Artery Bypass (MIDCAB) Compared with the General Swiss Population. Thorac Cardiovasc Surg online ahead of print. 2023. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).