1. Introduction
While many people have their morning coffee or tea without giving it much thought, these daily routines have changed drastically for many in the wake of COVID-19. Olfactory loss was not only a dominant symptom during the acute phase, but is often a long-lasting or permanent burden [
1]. Even before COVID-19, losing the sense of smell was a common hidden handicap, with approximately 15% of the population suffering from a reduced sense of smell and 2-3% suffering from a complete smell loss [
2,
3].
This sudden change in awareness of the existence of smell loss among the general public was accompanied by an increase in research efforts to treat smell loss worldwide. Despite these efforts, olfactory training with essential oils remains the cornerstone for treating smell loss in most patients [
4]. While some patients regain olfactory function through olfactory training and/or spontaneous recovery, a large proportion of patients experience either partial or no recovery, which often negatively impacts their quality of life (QoL) [
5,
6].
Of all the negative aspects affecting patients with smell loss, the most common complaint is impairment of the eating experience affecting 90% of patients [
7], while 73% complain of problems with cooking [
8]. These large negative effects on the enjoyment of food and cooking are related to the dominant role of olfaction in the overall flavour experience [
9].
Eating and cooking are truly multisensory endeavours. Apart from orthonasal and retronasal aromas sensed by the olfactory system, the gustatory system contributes with information on the five basic tastants, and the trigeminal system provides information on the mouthfeel, including temperature, somatosensation and pain. Hearing provides not only information on texture such as crispiness during mastication, but also more discrete information from e.g., carbonated beverages. Additionally, vision is important for evaluating edibility and setting up expectations for the other senses. In addition to these food-related sensory inputs, numerous other internal and external factors influence our perception of food, such as hunger, mood, atmosphere, and social context [
10]. The perception of food depends on the complex interaction of both the senses and surroundings, where the overall perception can go far beyond the sum of its parts [
11]. If one single factor changes, it can have enormous effects on the hedonic yield e.g., a decarbonated soda, a warm wine, a cold steak, or a brown-spotted apple [
10]. If the olfactory input is reduced or absent, both the overall perception of food and the remaining sensory inputs are often severely altered [
12].
This results in several challenges during cooking, where enjoyment of cooking, confidence in one’s abilities, and ability to accomplish desired results are significantly reduced in patients with smell loss [
13].
No prior studies have systematically investigated methods to improve cooking and eating in patients with smell loss in settings where patient feedback and hands-on training have been key factors. In the setting of treating and consulting patients, this results in a lack of tested and tangible advice on improving cooking abilities and enjoyment of food following a smell loss.
This study aimed to evaluate the effects of a novel approach to improve the food-related quality of life and cooking abilities in patients experiencing smell loss. By describing the modification of recipes and pedagogical considerations in creating the cooking schools, a further aim is to enable other researchers and clinicians to create similar courses for patients with smell loss.
2. Materials and Methods
2.1. Participants
Adult participants with olfactory dysfunction and smell-related issues with the pleasure of eating or cooking were included primarily from our Taste and Smell Clinic at Gødstrup Regional Hospital, Denmark [
14]. Participants with all aetiologies of olfactory dysfunction were included. Participants were offered a free 5-week cooking school course with a focus on emphasizing the other senses to regain the enjoyment of food. Inclusion criteria included having an intact sense of taste, which was confirmed by taste testing before start-up by either correct recognition of sweet, salty, sour, and bitter taste sprays [
15] or in case of an incorrect taste identification of taste sprays, completion of the Taste-Drop-Test within the normal range for all four tastants [
16]. As umami generally has a low identification rate in a normative population, this basic tastant was excluded from this testing [
17]. For participants without recent olfactory and gustatory testing (within two months) from our Taste and Smell clinic, olfactory and gustatory testing were performed before starting the cooking school.
As the cooking school required a high degree of acceptance of ingredients and extended presence in a room with cooking odours, only patients with a mild severity of subjective parosmia were allowed to participate in the cooking schools.
The study was performed following the Declaration of Helsinki’s ethical principles for medical research. Approval to conduct the study was granted by the Regional Ethical Committee, Denmark Central Region (1-10-72-274-21).
2.2. Testing of Olfactory Function and Questionnaires
Olfactory testing (Sniffin’ Sticks TDI-score, Burghart Messtechnik GmbH, Germany) was carried out in all participants before start-up. This olfactory test has been validated for a Danish population [
18,
19,
20].
Participants filled in questionnaires before the first session, the day after the last session, and three months after the last session. These questionnaires included subjective sensory function, food-related quality of life, and food and cooking habits. Cooking habits were evaluated by applying the Cooking and Food Provisioning Action Scale (CAFPAS) [
21]. Food-related quality of life (‘Please rate how food impacts your quality of life’; 0=’most pronounced negative impact possible’, 100=’most pronounced positive impact possible) was evaluated using a VAS scale (0-100).
2.3. Preparation and Modification of Recipes
Initial pilot testing of concepts was initiated in 2016, where all staff at a collaborating restaurant wore nose clamps for 14 consecutive days to gain an understanding of the effects of smell loss on sensory perception of the food. This led to the first creation of meals targeted at patients with smell loss, which later aired on Danish national television in 2018 [
22]. In collaboration with a neurogastronomy Chef [
23], this initial pilot cooking and knowledge on food perception and cooking habits in patients with olfactory dysfunction [
13] was used to create initial cooking school recipes. These recipes were modified and supplemented by additional recipes during the following cooking schools through participant feedback. All participants filled in a questionnaire on each recipe, rating difficulty, usefulness of the taste- and texture kit, willingness to make the dish at home, and usefulness of the recipe for enhancing other recipes. All dishes were further evaluated during the social dining after cooking, where the taste kit was available to improve balance and consensus among participants on the relevance and edibility of the recipe was reached. For recipes with overall low ratings (<50) or occurrence of parosmic triggers among several participants, the recipe was discarded. For dishes with overall moderate ratings (50-75), recipes were modified by the chefs based on participant feedback before usage in later courses. For dishes with overall high ratings (>75), recipes were reused in a later course, where subsequent overall high ratings (>75) would result in the inclusion of the recipe in the cookbook. For further details on selected recipes, see the results section.
2.4. Cooking School Contents and Structure
The five-week course consisted of weekly sessions with theory, practical cooking guided by Chefs, social dining and evaluation of recipes, see Supplementary
Table A1 (
Appendix A).
Through combined theory and practice during the cooking schools, the ability to season the food with basic tastants and highlight the flavour enhancement of the food with texture, temperature, tactility and trigeminal stimulation was trained.
Seasoning with basic tastants was trained using a ‘Taste Kit’, consisting of ingredients with different basic taste properties (e.g., honey (sweet), tamari/soy sauce (umami), vinegar (sour) salt (salty), fresh herbs/lettuce (bitter). A taste kit and the newest version (continuously updated) of our cookbook [
24] were distributed to all participants on the first day of the cooking school. Participants were encouraged to use these flavour enhancement methods at home between sessions. As most ingredients in the taste kit can be stored at room temperature, participants were recommended to place the taste kit in their kitchen next to the stove and use it daily.
The cooking school was structured to give the participants the necessary knowledge, training and feedback to empower their abilities to cook and the confidence to apply the methods of their training beyond the recipes used in the cooking school, see Supplementary
Table A2 (
Appendix A).
2.5. Statistics
Data were analysed using JMP Pro 16 (SAS Institute, NC, USA). Normal distribution was assessed using QQ-plots and the Shapiro-Wilk W test. For parametric data, mean values were compared using student’s t-test and presented as means with a 95% confidence interval (CI). For analysis of individual differences over time, the matched pair t-test was applied.
Fisher’s Exact Test was used to compare ordinal variables between groups, where contingency tables included fields of observations below five. ANOVA and Spearman’s rho were used to analyse correlations. The α level of statistical significance was set at 0.05.
3. Results
Through five classes at the cooking school, 49 participants with loss of smell have completed a cooking school course (five sessions), of which follow-up questionnaires were completed by 48 participants (see
Table 1).
3.1. Food-Related QoL
Food-related QoL increased following the cooking school and remained significantly higher at follow-up three months after the cooking school.
Table 1.
Demographics and changes in QoL assessment.
Table 1.
Demographics and changes in QoL assessment.
| |
Before cooking school |
End of cooking school |
3 months after of cooking school |
Δ |
p-value |
Age
(Mean, IQR, range) |
57
(IQR 50-67; range 20-79) |
- |
- |
Gender
(female n (%)) |
37 (75%) |
- |
- |
Duration of smell loss
(Mean, IQR, range) |
88 months
(IQR 22-69; range 9-700) |
|
|
| Food-related QoL (n=48) (range 0-100) |
58.2 |
68.7
|
66.6 |
10.5
8.4 |
0.0120
0.0269
|
3.2. Recipes
After pilot testing, the recipes had a focus on texture, temperature differences, strong aromas, and some with a relatively high content of umami and trigeminal spiciness. These three last components were represented e.g., in Asian-inspired dishes with miso soup (umami) and dishes with high contents of fresh herbs (highly aromatic). During the first two cooking schools, oral and written evaluations of the dishes with strong aromatic contents of fresh herbs were continuously low due to the bitter taste of fresh herbs. Ratings were similarly low for dishes with high umami and trigeminal contents in comparison with similar dishes with a balanced composition of the five basic tastants and less pronounced (yet present) spiciness, see
Table 2.
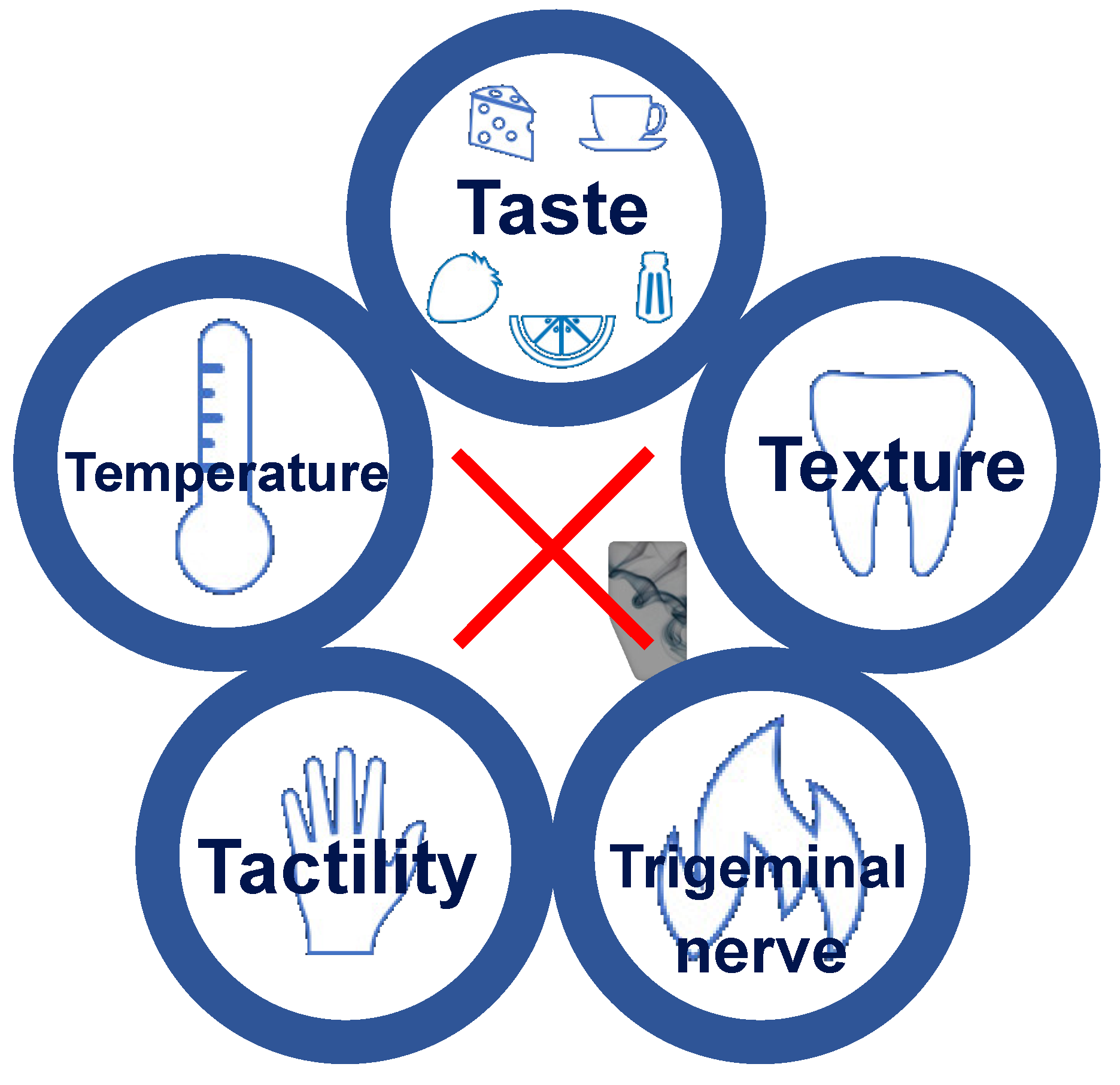
Recipes were tested and modified to include “Four T’s” consisting of Texture, Temperature, Trigeminal pain, and Tactility. As the importance of balancing basic tastants became clear in both the oral and written evaluations, this method was renamed “The 5T’s” to include ‘Taste’ after the third cooking school, see
Figure 1.
Positively evaluated recipes were adjusted according to participant feedback, re-evaluated and if high ratings persisted, recipes were published in an online cookbook in Danish, English, and German [
24].
3.3. Cooking Problems and Habits
The CAFPAS questionnaire on cooking and provisioning revealed several significant changes in habits and attitudes following the cooking school. In general, there were improvements in almost all aspects of cooking, where scores of participants with smell loss after the cooking school changed towards reference scores of a normosmic population. For the most pronounced improvements, see
Table 3 (all scores are included in supplementary
Table 3).
Normative scores from Fjaeldstad et Smith, 2022 [
13]. For detailed information on the questions, see the original publication by Lahne et al. [
21]. For a complete list of changes in CAFPAS questions, see Supplementary
Table B1.
3.4. Satisfaction with the Cooking School and Parosmia
Overall ratings of satisfaction with the cooking school were comparable between participants without parosmia and participants with mild parosmia (n=16) (scale 1-5; mean scores 4.78 vs. 4.76; p=0.7111).
Overall ratings of satisfaction with the cooking school were significantly higher after modification of the methods (focus on “the 5T’s”) and recipes (after the second cooking school class) (scale 1-5; mean scores 4.53 vs. 4.93; p=0.0122).
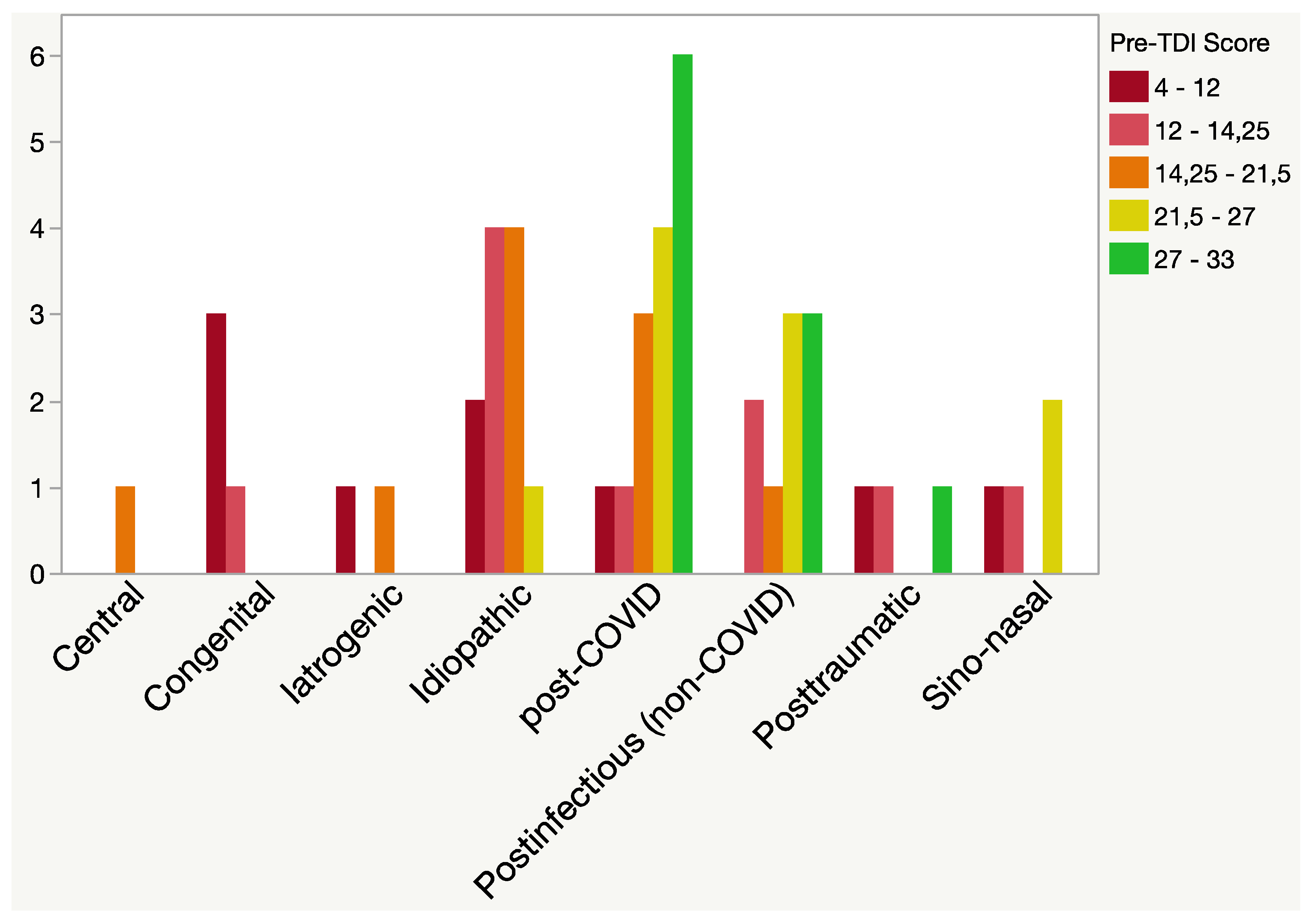
Figure 2.
Aetiology and severity of smell loss. Participants had subjective smell loss and smell-related challenges with the enjoyment of food and/or cooking. TDI: Composite Sniffin Sticks olfactory test score (threshold, discrimination, and identification).
Figure 2.
Aetiology and severity of smell loss. Participants had subjective smell loss and smell-related challenges with the enjoyment of food and/or cooking. TDI: Composite Sniffin Sticks olfactory test score (threshold, discrimination, and identification).
4. Discussion
A framework for a cooking school for patients with smell loss was established and evaluated. We found that cooking schools for patients with smell loss significantly improved food-related QoL and improved cooking habits.
4.1. Flavour Enhancement in Patients with Olfactory Deficits
As a result of the high occurrence of olfactory and gustatory impairments during and after the COVID-19 pandemic [
25,
26,
27,
28], new insights into the dynamics of altered eating behaviour have emerged [
29]. Profound effects of olfactory loss on appetite, sensory perception, and food behaviour have been described [
30]. Similar to our findings, increased focus on texture and trigeminal stimulation may be beneficial for maintaining food-related pleasure [
31]. However, most patients do not fully utilize other flavour-related senses in cooking or eating following their smell loss [
13]. This may contribute to the heterogeneous reports on the influence of olfactory loss on dietary behaviours [
32].
Our novel rehabilitation method for patients with smell loss focussed on using the “5T’s” to ensure adequate attention to taste, texture, temperature, tactility, and trigeminal nerve stimulation in the food. The usage of this method was the cornerstone in every session and evaluation of the food, presentations of prepared meals, and the ‘food-jam-assignment’ during the last session where no recipe was available. While the theoretical advantages of flavour enhancement have previously been mentioned in the literature [
33], no tested or complete guide to cooking is currently available for patients or clinicians. The cooking school based on the “5T’s” improved cooking habits and abilities in participants with smell loss towards ratings comparable with normosmic controls. Following the five-week course, participants increased involvement in daily meal preparations and to a higher degree preferred to cook rather than have food prepared. Cooking was rated as a more fulfilling activity after the cooking school. As food and cooking-related problems are consistently rated among the highest complaints in patients with smell loss [
7,
34], these findings indicate that targeted efforts can alleviate some of the negative consequences of smell loss.
4.2. Parosmia
A further hindrance to the enjoyment of food is the occurrence of distorted olfactory perception (parosmia). Recently, new insights have emerged indicating specific molecular patterns of odorant triggers of parosmia [
35]. These not only include groups of foods but parosmic triggers are also released during common preparations of a meal, such as frying and baking [
36]. While the setup of the current study with extensive cooking in a confined space during the cooking school constrained the inclusion of participants with severe parosmia, we found comparable high evaluations of satisfaction between participants with and without mild parosmia. Close adherence to the avoidance of common parosmic triggers described by Parker et al. [
35,
37], indicates promising prospects for applying similar methods of flavour enhancement in future cooking schools designed specifically for parosmic participants.
4.3. Gustatory Impairment in Patients with Olfactory Dysfunction
A solid understanding of the senses contributing to flavour is essential for an adequate understanding of patients’ sensory abilities and guidance of patients.
In the clinical setting, patients with olfactory loss often complain of an affected sense of taste despite taste scores within the normative range [
38]. While this well-known phenomenon of taste-smell confusion may be related to a linguistic conundrum where taste is generally used to describe the combined sensation of flavour [
39], it may also be affected by a decrease in gustatory function following an acquired olfactory impairment [
40].
In the current study, the correct identification of supra-threshold tastants was a prerequisite for participation. However, a recent study on taste rehabilitation has indicated that gustatory sensitivity can be increased through taste training [
41]. As such, some patients may benefit from focused gustatory training before engaging in cooking using “The 5T’s”. On the other hand, the continuous focus on taste seasoning with basic tastants may have similar positive effects on gustatory sensitivity as taste recall training. However, this was beyond the scope of this current study.
4.4. Cooking Schools for Other Groups with Olfactory Deficits
The current study investigated the effects on unselected participants with olfactory loss and affected enjoyment of food and cooking. However, specific patient groups with high occurrence of olfactory loss and special dietary requirements may have even more pronounced benefits from similar interventions. These groups include e.g., patients with chemosensory deficits following radio-/chemotherapy, where appetite and weight loss are key indicators for successful outcome [
42,
43,
44,
45], dietary habits and diet adherence in patients with diabetes [
46,
47,
48,
49], patients with dietary requirements associated with kidney disease [
50,
51,
52], and elderly patients in general where enjoyment of food may become severely affected due to the decline of chemosensory function [
53,
54,
55,
56].
4.5. Limitations
This study describes the initial findings from a smell loss rehabilitation initiative. Due to the aim of describing the establishment of the methods applied in this novel project, alterations of methods and recipes were made during the process, e.g., the change from “4T’s” to “5T’s”. As described in the methods section, this study included data from the first two classes of the cooking school, where the concept and methods were to a high degree still under development. As such, data on follow-up and the effects of the interventions in this manuscript may be affected by the changes made during the initial phases of this novel approach to relieving the negative consequences of olfactory dysfunction. Nonetheless, these preliminary findings have shown significant positive results for both QoL and cooking habits despite the lower level of satisfaction ratings during the first two courses. The purpose of this manuscript was not only to investigate the feasibility and possible effects of the cooking schools but also to describe the process of planning and conducting food-related rehabilitation initiatives for clinical and culinary individuals to ease the process of conducting similar initiatives. As the aim was to establish a framework for conducting cooking schools, we have not included a control group in this current study. Further studies are needed to optimise the use of cooking as smell loss rehabilitation.
As food-related cultural backgrounds and preferences may differ in other countries or cultures, confirmatory studies are needed to investigate the effects of these methods in different populations.
5. Conclusions
A focus on food and cooking in patients with olfactory loss can have a positive effect on both cooking habits and food-related quality of life. Recipes and cooking methods are available for patients with smell loss for free in online cookbooks in Danish, German, and English. Examples of tested recipes, cooking methods and setup of a cooking school for patients with smell loss are now available for both patients and clinicians as inspiration for future efforts to alleviate the negative consequences of olfactory loss.
More studies are needed to further investigate the potential of cooking as rehabilitation in patients with olfactory dysfunction.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Table S1: Setup of the five-week cooking school; Table S2: Pedagogical goals for participants and applied methods during the cooking school; Table S3: Differences in cooking and food provisioning habits between normosmics and cooking school patients.
Author Contributions
Conceptualization, methodology, formal analysis, investigation, data curation, writing—original draft preparation, writing—review and editing, visualization, project administration, and funding acquisition; AWF.
Funding
This research was funded by VELUX FONDEN, grant number 00035282. The sponsors had no say, roles or responsibilities concerning the study, including (but not limited to) the study design, data collection, management, analysis, or decision to publish.
Data Availability Statement
Data is unavailable due to privacy and legal restrictions.
Acknowledgments
The two chefs in the project, Christian Bøjlund and Rasmus Bredahl, have been imperative for all phases of the project, including the development of the cooking school concept, the creation of recipes and content, the execution of cooking schools, and creation of a welcoming and open atmosphere for participants. Associate Professor Per Bøjlund assisted in optimizing the pedagogical principles of the cooking school. Clinical dietitian Kirstine Guld Frederiksen introduced participants to the nutritional aspects of cooking with smell loss. All participants have been enthusiastic and generous in sharing thoughts, ideas and feedback. The staff at the Flavour Clinic, Gødstrup Regional Hospital, have made an excellent effort to support the awareness of the cooking school among relevant patients, especially Dovile Stankevice and Therese Ovesen. Our Lab Technician, Dorthe Rasmussen, has been irreplaceable due to her efforts with olfactory testing.
Conflicts of Interest
The author has no conflict of interest. Cookbooks created during this project are available for free online.
Appendix A
Supplemental information on the design and contents of the cooking school. This additional information is included to enable other clinics to design similar rehabilitation efforts for patients with smell loss. For additional questions, contact the corresponding author.
Table A1.
Setup of the five-week cooking school.
Table A1.
Setup of the five-week cooking school.
| Session |
Contents |
Session 1
(-1 day)
|
- -
Olfactory and gustatory testing (TDI and taste spray/taste drop test) - -
Questionnaires on taste/smell, QoL, and food/cooking habits |
| Session 1 |
- Introduction to the cooking school, smell loss and current knowledge on cooking with smell loss (researcher and ENT physician)- Introduction to the concept of the cooking school, including 5T’s, taste kit and texture bank (chef)- ‘Sensory Circus’ with tasting samples and description of all senses involved in the perception of food (chef)- Meal prepared by chefs and social dining- Availability of ENT physician if participants have questions regarding smell loss and treatment- Box with printed cookbook 24, taste kit, and texture bank to take home |
| Session 2-3 |
- -
Short description of the 5T’s, seasoning with the taste kit, texture and guidance on how to use the kitchen - -
Cooking (recipes) in small teams based on TDI-scores - -
Guidance by chefs during cooking and seasoning - -
Presentation of food samples using three levels of seasoning (1: salt and pepper; 2: added balanced seasoning of all five basic tastes; 3: added different textures and visual presentation 24
- -
Presentation of dishes and usage of the 5T’s in plenum - -
Social dining and evaluation of dishes and recipes |
| Session 4 |
- -
Presentation of nutritional aspects and challenges in smell loss (clinical dietitian) - -
Identical contents as session 2-3 |
| Session 5 |
- -
Participants were encouraged to bring a relative to join the cooking school on the final day. - -
Short description of the 5T’s, seasoning with the taste kit, texture and guidance on how to use the kitchen - -
“Food Jam”, where participants create a dish using limited available ingredients and learned methods without being handed a recipe. Continuous feedback from chef during the preparation process - -
Presentation of created dishes before social dining to the class with emphasis on applied methods and used ingredients. - -
Social dining and evaluation |
Session 5
(+0 days)
|
- -
Online individual evaluation of the cooking school - -
Questionnaires on taste/smell, QoL, and food/cooking habits |
Session 5
(+90 days)
|
- -
Questionnaires on taste/smell, QoL, and food/cooking habits |
Table A2.
Pedagogical goals for participants and applied methods during the cooking school [
59].
Table A2.
Pedagogical goals for participants and applied methods during the cooking school [
59].
| Pedagogical goals |
Applied methods |
-
1.
Acquire an understanding of own sensory abilities |
- -
Pre-test of measured taste (taste spray/taste drop test) and smell scores (Sniffin’ Sticks TDI score) - -
Sensory challenge (day one) using food samples to illustrate how other senses still give sensory stimulation in food. |
-
2.
Acquire a basic knowledge on all senses involved in the multisensory experience of eating |
- -
Sensory challenge (day 1), where oral and visual information was combined with food samples to illustrate the perception of basic tastes, smell, texture, colours, mouthfeel, spiciness, and multisensory integration. - -
Introductory lecture on all senses relevant for flavour perception (day 1) - -
A printed version of the cooking school cook book was given to all participants (day one) 24
- -
Presentation of food samples using three levels of seasoning (1: salt and pepper; 2: added balanced seasoning of all five basic tastes; 3: added different textures and visual presentation 24
|
-
3.
Improve cooking and seasoning abilities |
- -
Practicing seasoning with “The 5T’s” (see Figure 1) - -
Practicing achieving a balance of basic tastants 56,57
- -
Introduction to the sensory qualities of new foods and seasoning products to increase knowledge and repertoire of food items in their cooking. |
-
4.
Build confidence in cooking abilities |
- -
Cooking preparation in teams (n=2-3) with continuous feedback from chef during the preparation process - -
Presentation of created dishes before social dining (day 2-5) to the class with emphasis on applied methods and used ingredients. - -
“Food Jam” (day 5), where participants create a dish using limited available ingredients and learned methods without being handed a recipe. |
-
5.
Transfer of cooking school contents to own kitchen |
- -
Encouragement to use ‘taste kit’ and methods at home between sessions. - -
Participants were encouraged to bring a relative to join the cooking school on the final day. |
-
6.
Social belonging |
- -
Social dining (day 1-5) where all participants and staff share the produced dishes at the same table. - -
Meeting others with similar olfactory deficits and discussing experiences and coping mechanisms during cooking - -
Presence of physician and researcher experienced in working with smell loss to demystify any general questions on smell loss in a relaxed setting (day 1 and 5) |
Appendix B
Table B1.
Differences in cooking and food provisioning habits between normosmics and cooking school patients.
Table B1.
Differences in cooking and food provisioning habits between normosmics and cooking school patients.
| |
Normosmic reference (n=166) |
Start of cooking school (n=48) |
End of Cooking school (n=47) |
Δ |
p-value* |
| Want to get through cooking asap. (FSE14 (neg)) |
2.58 (2.28;2.88) |
3.33 (2.82;3.85) |
3.17 (2.67;3.67) |
-0.16 |
0.3305 |
| Cooking is a fulfilling activity (FSE11) |
5.70 (5.42;5.98) |
5.02 (4.48;5.56) |
5.48 (5.06;5.89) |
0.46 |
0.0245 |
| Comfortable preparing food (ISCO1) |
6.21 (5.95;6.47) |
5.58 (5.12;6.05) |
5.69 (5.34;6.04) |
0.11 |
0.5924 |
| Inspired to cook for other people (STR2) |
5.67 (5.39;5.96) |
5.34 (4.84;5.84) |
5.53 (5.11;5.96) |
0.19 |
0.1725 |
| Easy to accomplish desired results during cooking (FSE7) |
5.67 (5.42;5.93) |
4.75 (4.29;5.21) |
4.85 (4.48;5.22) |
0.10 |
0.4784 |
| Cooking is a waste of effort (ISCU4 (neg)) |
1.89 (1.64;2.15) |
2.15 (2.54;3.05) |
1.77 (1.46;2.01) |
-0.38 |
0.0626 |
| Will not make a new dish again after unsuccessful first attempt (FSE16 (neg)) |
3.43 (3.16;3.71) |
4.08 (3.58;4.59) |
3.83 (3.25;4.41) |
-0.25 |
0.2784 |
| Cooking brings little enjoyment (FSE15 (neg)) |
3.31 (3.02;3.61) |
4.60 (4.14;5.07) |
4.53 (4.10;4.96) |
-0.07 |
0.7644 |
| Confidence in ability to deal with unexpected results during cooking (FSE6) |
5.38 (5.11;5.64) |
4.73 (4.18;5.28) |
5.13 (4.73;5.52) |
0.40 |
0.1896 |
| Ability to decide what to eat (FSE3) |
4.99 (4.70;5.28) |
4.85 (4.35;5.36) |
4.63 (4.16;5.09) |
-0.22 |
0.5771 |
| Cooking for others is a burden (STR3 (neg)) |
2.57 (2.28;2.85) |
2.71 (2.17;3.24) |
2.52 (2.08;2.96) |
-0.19 |
0.2713 |
| Coping with problems during cooking (FSE8) |
5.67 (5.43;5.92) |
5.06 (4.58;5.55) |
5.15 (4.76;5.54) |
0.09 |
0.6248 |
| Prefer to spend time om more important things than food (HO5 (neg)) |
3.20 (2.92;3.47) |
3.60 (3.11;4.09) |
3.15 (2.71;3.58) |
-0.55 |
0.0371 |
| Limited by lack of cooking knowledge (FSE2 (neg)) |
2.36 (2.07;2.65) |
2.73 (2.22;3.24) |
3.13 (2.62;3.63) |
0.40 |
0.1714 |
| Involvement in daily meal preparations (ISMP2) |
6.15 (5.88;6.42) |
5.94 (5.45;6.42) |
6.27 (5.90;6.64) |
0.33 |
0.0250 |
| Prefer to cook rather than having food prepared (ISCO3) |
4.31 (4.01;4.61) |
3.49 (2.96;4.02) |
4.23 (3.76;4.70) |
0.74 |
0.0074 |
| Confidence in creating meals from ingredients on hand (ISMP5) |
6.04 (5.81;6.28) |
5.64 (5.18;6.10) |
6.02 (5.75;6.29) |
0.38 |
0.0867 |
| Confidence in choosing between similar products (ISSH4) |
5.93 (5.71;6.16) |
5.50 (5.09;5.91) |
5.96 (5.73;6.18) |
0.46 |
0.0166 |
| Reflection on what to cook and eat (HO4) |
5.14 (4.88;5.41) |
4.60 (4.19;5.00) |
4.96 (4.60;5.32) |
0.36 |
0.0711 |
| Knowledge of usage of ingredients during purchasing (ISMP3) |
6.17 (5.97;6.38) |
5.89 (5.50;6.29) |
5.98 (5.71;6.24) |
0.11 |
0.5062 |
| Difficult finding time to prepare preferred food (STR4 (neg)) |
3.63 (3.35;3.90) |
2.94 (2.39;3.48) |
3.09 (2.56;3.61) |
0.15 |
0.2196 |
| Knowledge on where to find needed ingredients (ISSH5) |
6.34 (6.15;6.53) |
6.10 (5.75;6.46) |
6.23 (5.95;6.51) |
0.13 |
0.2424 |
| No time to prepare meals due to family responsibilities (STR8 (neg)) |
2.62 (2.36;2.88) |
2.40 (1.92;2.87) |
2.33 (1.86;2.75) |
-0.07 |
0.8165 |
| No time to prepare meals due to job responsibilities (STR10 (neg)) |
3.31 (3.00;3.62) |
2.35 (1.82;2.89) |
2.23 (1.78;2.68) |
-0.12 |
0.5418 |
| Knowledge of kitchen equipment usage (ISCO5) |
6.37 (6.19;6.56) |
6.15 (5.76;6.54) |
6.31 (6.06;6.56) |
0.16 |
0.3375 |
| Mental plan of steps before cooking (ISMP7) |
5.82 (5.59;6.05) |
5.71 (5.31;6.11) |
5.92 (5.58;6.25) |
0.21 |
0.3021 |
| No time to prepare meals due to social responsibilities (STR9 (neg)) |
2.43 (2.19;2.66) |
2.17 (1.71;2.63) |
2.11 (1.73;2.48) |
-0.06 |
0.8167 |
| Wish for more time to plan meals (ISMP1 (neg)) |
3.98 (3.73;4.24) |
3.48 (2.94;4.01) |
3.48 (2.94;4.01 |
0.00 |
0.9070 |
References
- Gerkin RC, Ohla K, Veldhuizen MG, et al. Recent smell loss is the best predictor of COVID-19 among individuals with recent respiratory symptoms. Chemical Senses. 2020;46. [CrossRef]
- Brämerson A, Johansson L, Ek L, Nordin S, Bende M. Prevalence of olfactory dysfunction: The Skövde population-based study. The Laryngoscope. 2004;114(4):733-737. [CrossRef]
- Vennemann MM, Berger K. The association between smoking and smell and taste impairment in the general population. Journal of Neurology. 2008;255(8):1121-1126. [CrossRef]
- Addison AB, Wong B, Ahmed T, et al. Clinical Olfactory Working Group consensus statement on the treatment of postinfectious olfactory dysfunction. J Allergy Clin Immun. 2021;147(5):1704-1719. [CrossRef]
- Croy I, Nordin S. Olfactory Disorders and Quality of Life--An Updated Review. Chemical Senses. 2014;39(3):185-194. [CrossRef]
- Fjaeldstad AW, Ovesen T, Stankevice D, Ovesen T. Olfactory training in long COVID-19 patients with lasting symptoms including olfactory dysfunction. Dan Méd J. 2023;70(3).
- Philpott CM, Boak D. The Impact of Olfactory Disorders in the United Kingdom. Chemical Senses. 2014;39(8):711-718. [CrossRef]
- Temmel AFP, Quint C, Schickinger-Fischer B, Klimek L, Stoller E, Hummel T. Characteristics of Olfactory Disorders in Relation to Major Causes of Olfactory Loss. Arch OtolaryngolHead Neck Surg. 2002;128(6):635-641. [CrossRef]
- Spence C. Just how much of what we taste derives from the sense of smell? Flavour. 2015;4(1):30. [CrossRef]
- Piqueras-Fiszman B, Fjaeldstad A, Spence C, Hartevelt TJV, Kringelbach ML. Pleasure of food in the brain. In: Multisensory Flavor Perception. ; 2016:211-234. [CrossRef]
- Spence C. Multisensory Flavor Perception. Cell. 2015;161(1):24-35. [CrossRef]
- Migneault-Bouchard C, Hsieh JW, Hugentobler M, Frasnelli J, Landis BN. Chemosensory decrease in different forms of olfactory dysfunction. Journal of Neurology. 2019;267(1):138-143. [CrossRef]
- Fjaeldstad AW, Smith B. The Effects of Olfactory Loss and Parosmia on Food and Cooking Habits, Sensory Awareness, and Quality of Life—A Possible Avenue for Regaining Enjoyment of Food. Foods. 2022;11(12):1686. [CrossRef]
- Fjaeldstad AW, Stankovic J, Onat M, Stankevice D, Ovesen T. Patients and experiences from the first Danish flavour clinic. Danish medical journal. 2020;67(4):1-5.
- Walliczek U, Negoias S, Hähner A, Hummel T. Assessment of Chemosensory Function Using “Sniffin’ Sticks”, Taste Strips, Taste Sprays, and Retronasal Olfactory Tests. Curr Pharm Design. 2016;22(15):2245-2252. [CrossRef]
- Fjaeldstad A, Niklassen AS, Fernandes HM. Re-Test Reliability of Gustatory Testing and Introduction of the Sensitive Taste-Drop-Test. Chemical Senses. 2018;43(5):341-346. [CrossRef]
- Satoh-Kuriwada S, Blachier F, Kawai M, et al. Development of an Umami Taste Sensitivity Test and Its Clinical Use. PLoS ONE. 2014;9(4):e95177-8. [CrossRef]
- Hummel T, Sekinger B, Wolf SR, Pauli E, Kobal G. ‘Sniffin’ Sticks’: Olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chemical Senses. 1997;22(1):39-52. [CrossRef]
- Fjaeldstad A, Kjærgaard T, Hartevelt TJV, Moeller A, Kringelbach ML, Ovesen T. Olfactory screening: validation of Sniffin’ Sticks in Denmark. Clin Otolaryngol. 2015;40(6):545-550. [CrossRef]
- Niklassen AS, Ovesen T, Fernandes H, Fjaeldstad AW. Danish validation of sniffin’ sticks olfactory test for threshold, discrimination, and identification. The Laryngoscope. 2018;128(8):1759-1766. [CrossRef]
- Lahne J, Wolfson JA, Trubek A. Development of the Cooking and Food Provisioning Action Scale (CAFPAS): A new measurement tool for individual cooking practice. Food Quality and Preference. Published online 2017:1-38. [CrossRef]
- DR.dk. Michelin-kok laver middag til Rune, der næsten ikke kan smage. Published online September 8, 2018. https://www.dr.dk/nyheder/viden/kroppen/video-michelin-kok-laver-middag-til-rune-der-naesten-ikke-kan-smage.
- Bredahl R, Buchardt N. Neurogastronomi. FADL; 2016. www.neurogastronomi.com.
- Fjaeldstad A, Bredahl R, Bøjlund C. Cooking With a Smell Loss. Apple Books; 2023. http://books.apple.com/us/book/id6450322002.
- Parma V, Ohla K, Veldhuizen MG, et al. More than smell - COVID-19 is associated with severe impairment of smell, taste, and chemesthesis. Chemical Senses. 2020;45(7):609-622. [CrossRef]
- Stankevice D, Fjaeldstad AW, Agergaard J, Ovesen T. Long-Term COVID-19 Smell and Taste Disorders Differ Significantly from Other Post-Infectious Cases. Laryngoscope. 2023;133(1):169-174. [CrossRef]
- Schwab J, Fjaeldstad AW. Recovery rates and parosmia in olfactory loss during the COVID-19 era. Dan Med J. 2022;9(69).
- Haldrup M, Johansen MI, Fjaeldstad AW. [Anosmia and ageusia as primary symptoms of COVI D-19]. Ugeskr Laeger. 2020;182:1-3.
- Pellegrino R, Fjaeldstad AW. The Effect of Olfactory Disorder (and Other Chemosensory Disorders) on Perception, Acceptance, and Consumption of Food. In: Stafford LD, ed. Smell, Taste, Eat: The Role of the Chemical Senses in Eating Behaviour. Vol 1. Palgrave Macmillan Cham; 2024:119-137. [CrossRef]
- Chaaban N, Høier ATZB, Andersen BV. A Detailed Characterisation of Appetite, Sensory Perceptional, and Eating-Behavioural Effects of COVID-19: Self-Reports from the Acute and Post-Acute Phase of Disease. Foods. 2021;10(4):892. [CrossRef]
- Høier ATZB, Chaaban N, Andersen BV. Possibilities for Maintaining Appetite in Recovering COVID-19 Patients. Foods. 2021;10(2):464. [CrossRef]
- Aschenbrenner K, Hummel C, Teszmer K, et al. The influence of olfactory loss on dietary behaviors. The Laryngoscope. 2008;118(1):135-144. [CrossRef]
- Seo HS, Pramudya RC, Singh A, Hummel T. Recent evidence for the impacts of olfactory disorders on food enjoyment and ingestive behavior. Curr Opin Food Sci. 2021;42:187-194. [CrossRef]
- Keller A, Malaspina D. Hidden consequences of olfactory dysfunction: a patient report series. BMC Ear, Nose and Throat Disorders. 2013;13(1):1-1. [CrossRef]
- Parker JK, Kelly CE, Gane SB. Molecular Mechanism of Parosmia. Medrxiv. Published online 2021:2021.02.05.21251085. [CrossRef]
- Parker JK, Methven L, Pellegrino R, Smith BC, Gane S, Kelly CE. Emerging Pattern of Post-COVID-19 Parosmia and Its Effect on Food Perception. Foods. 2022;11(7):967. [CrossRef]
- Parker J, Methven L, Pellegrino R, Smith B, Gane S, Kelly C. Emerging Pattern of Post-COVID-19 Parosmia and Its Effect on Food Perception. Foods. Published online March 27, 2022. [CrossRef]
- Nørgaard HJ, Fjaeldstad AW. Differences in Correlation between Subjective and Measured Olfactory and Gustatory Dysfunctions after Initial Ear, Nose and Throat Evaluation. International Archives of Otorhinolaryngology. 2021;(EFirst). [CrossRef]
- Rozin P. “Taste-smell confusions” and the duality of the olfactory sense. Perception & psychophysics. 1982;31(4):397-401. [CrossRef]
- Landis BN, Scheibe M, Weber C, et al. Chemosensory interaction: acquired olfactory impairment is associated with decreased taste function. J Neurol. 2010;257(8):1303-1308. [CrossRef]
- Otsubo Y, Miyagi M, Sekiya H, Kano O, Ebihara S. Improving taste sensitivity in healthy adults using taste recall training: a randomized controlled trial. Sci Rep. 2022;12(1):13849. [CrossRef]
- Vries YC de, Winkels RM, Berg MMGA van den, et al. Altered food preferences and chemosensory perception during chemotherapy in breast cancer patients_ A longitudinal comparison with healthy controls. Food Quality and Preference. 2017;63:135-143. [CrossRef]
- Nolden AA, Hwang LD, Boltong A, Reed DR. Chemosensory Changes from Cancer Treatment and Their Effects on Patients’ Food Behavior: A Scoping Review. Nutrients. 2019;11(10):2285. [CrossRef]
- Johnston CA, Keane TJ, Prudo SM. Weight loss in patients receiving radical radiation therapy for head and neck cancer: a prospective study. JPEN Journal of parenteral and enteral nutrition. 1982;6(5):399-402. [CrossRef]
- Spotten LE, Corish CA, Lorton CM, et al. Subjective and objective taste and smell changes in cancer. Annals of Oncology. 2017;28(5):969-984. [CrossRef]
- Zaghloul H, Pallayova M, Al-Nuaimi O, Hovis KR, Taheri S. Association between diabetes mellitus and olfactory dysfunction: current perspectives and future directions. Diabetic Medicine. 2017;35(1):41-52. [CrossRef]
- Papamichou D, Panagiotakos DB, Itsiopoulos C. Dietary patterns and management of type 2 diabetes: A systematic review of randomised clinical trials. Nutrition Metabolism Cardiovasc Dis. 2019;29(6):531-543. [CrossRef]
- Falkowski B, Duda-Sobczak A, Araszkiewicz A, et al. Insulin Resistance is Associated with Impaired Olfactory Function in Adult Patients with Type 1 Diabetes - a Cross-sectional Study. Diabetes/Metabolism Research and Reviews. Published online 2020:dmrr.3307-8. [CrossRef]
- Kim J, Hur MH. The Effects of Dietary Education Interventions on Individuals with Type 2 Diabetes: A Systematic Review and Meta-Analysis. Int J Environ Res Pu. 2021;18(16):8439. [CrossRef]
- Kim TH, Kim YH, Bae NY, Kang SS, Lee JB, Kim SB. Salty taste thresholds and preference in patients with chronic kidney disease according to disease stage: A cross-sectional study. Nutrition & Dietetics. 2017;75(1):59-64. [CrossRef]
- McMahon EJ, Campbell KL, Bauer JD. Taste perception in kidney disease and relationship to dietary sodium intake. Appetite. 2014;83(C):236-241. [CrossRef]
- Madsen A, Danielsen LMA, Niklassen AS, et al. Chemosensory function and food preferences among haemodialysis patients. Dan Med J. 2022;69(11).
- Spence C, Youssef J. Aging and the (Chemical) Senses: Implications for Food Behaviour Amongst Elderly Consumers. Foods. 2021;10(1):168-16. [CrossRef]
- Sulmont-Rossé C, Maitre I, Amand M, et al. Evidence for Different Patterns of Chemosensory Alterations in the Elderly Population: Impact of Age Versus Dependency. Chemical Senses. 2015;40(3):153-164. [CrossRef]
- Sergi G, Bano G, Pizzato S, Veronese N, Manzato E. Taste loss in the elderly: Possible implications for dietary habits. Critical Reviews in Food Science and Nutrition. 2017;57(17):3684-3689. [CrossRef]
- Manesse C, Ferdenzi C, Mantel M, et al. The prevalence of olfactory deficits and their effects on eating behavior from childhood to old age: A large-scale study in the French population. Food Qual Prefer. 2021;93:104273. [CrossRef]
- Keast R, preference PBF quality and, 2003. An overview of binary taste–taste interactions. Elsevier. 2003;14(2):111-124. [CrossRef]
- Fjaeldstad AW, Fernandes HM. Chemosensory Sensitivity after Coffee Consumption Is Not Static: Short-Term Effects on Gustatory and Olfactory Sensitivity. Foods. 2020;9(4):493-499. [CrossRef]
- Kolb DA. Experiential Learning: Experience as the Source of Learning and Development. Vol 8. FT press; 2014. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).