Submitted:
25 April 2024
Posted:
25 April 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Prevalence of Hypertension and Cardiovascular Mortality in Croatia
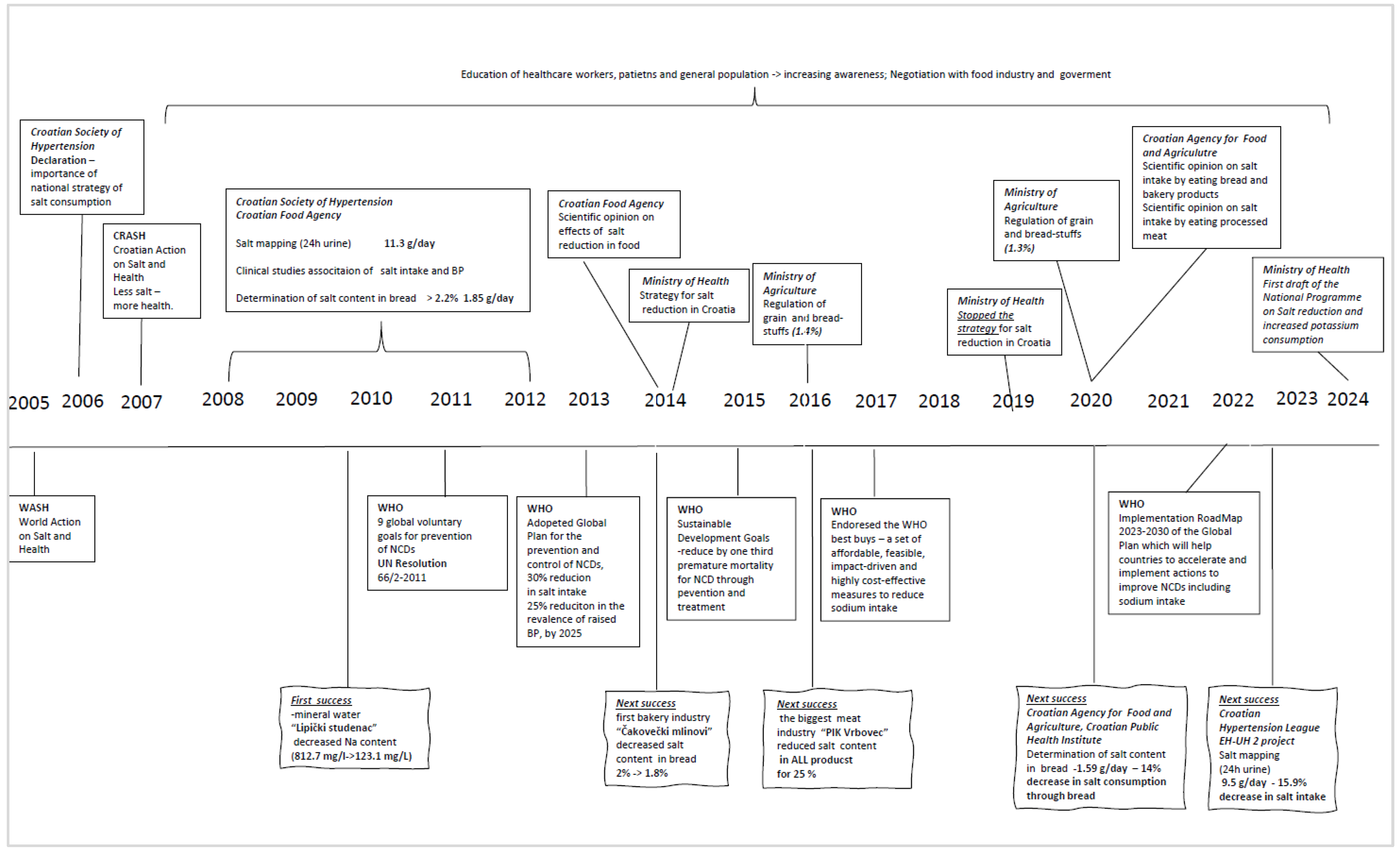
3. Brief History of Eighteen Years Old Salt War in Croatia
3.1. First Period 2005 – 2014
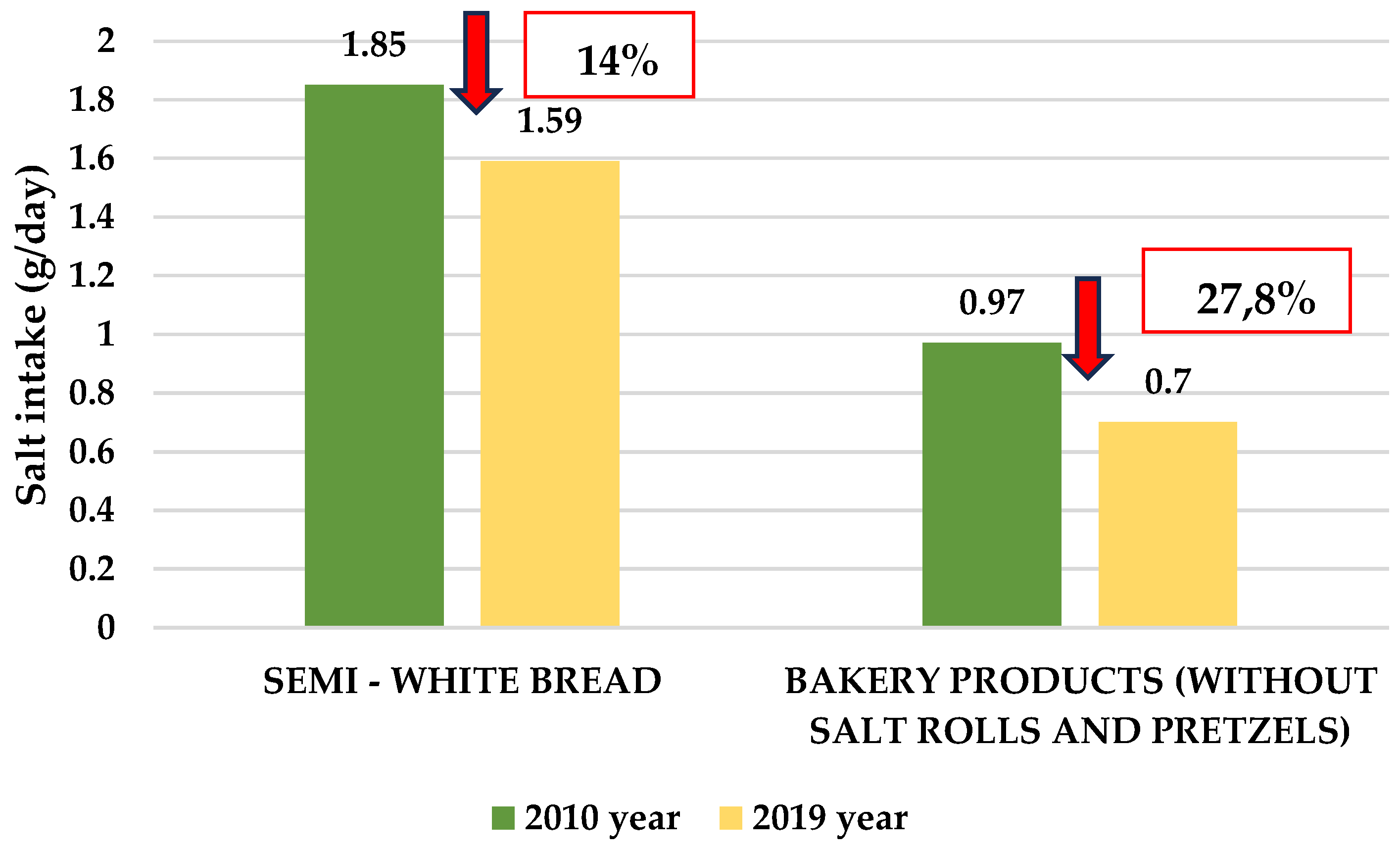
3.2. Action Plan for Salt Reduction in Croatia, Ministry of Health 2014 – 2019
3.3. Third Period 2020 – 2024
4. Future Plans and Strategies – Decrease Salt and Increase Potassium Intake
5. Conclusion
Supplementary Materials
Funding
Conflicts of Interest
References
- Huang, L.; Trieu, K.; Yoshimura, S.; Neal, B.; Woodward, M.; Campbell, N. R. C.; Li, Q.; Lackland, D. T.; Leung, A. a. C.; Anderson, C. A. M. et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ 2020, m315. [CrossRef]
- Bennett, J. L.; Stevens, G. A.; Mathers, C.; Bonita, R.; Rehm, J.; Kruk, M. E.; Riley, L.; Dain, K.; Kengne, A. P.; Chalkidou, K. et al. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet 2018, 392 (10152), 1072–1088. [CrossRef]
- Global Burden of Disease 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioral, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392 (10159), 1923–1994. [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398 (10304), 957–980. [CrossRef]
- Cook, N. R.; He, F. J.; MacGregor, G. A.; Graudal, N. Sodium and health—concordance and controversy. BMJ. (Clinical Research Ed.) 2020, m2440. [CrossRef]
- World Health Organization. Management-Screening, Diagnosis and Treatment (MND). Global report on hypertension: the race against a silent killer. Available online: https://www.who.int/publications/i/item/9789240081062 (accessed on 2 February 2024).
- Elliott, P.; Stamler, J.; Nichols, R.; Dyer, A. R.; Stamler, R.; Kesteloot, H.; Marmot, M. Intersalt revisited: further analyses of 24-hour sodium excretion and blood pressure within and across populations. BMJ. 1996, 312 (7041), 1249–1253. [CrossRef]
- Aburto, N.; Ziolkovska, A.; Hooper, L.; Elliott, P.; Cappuccio, F. P.; Meerpohl, J. J. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013, 346 (apr03 3), f1326. [CrossRef]
- He, F. J.; Li, J.; MacGregor, G. A. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013, 346 (apr03 3), f1325. [CrossRef]
- Act, A.; Mozaffarian, D.; Fahimi, S.; Singh, G.; Khatibzadeh, S.; Engell, R. E.; Lim, S. S.; Danaei, G.; Ezzati, M.; Powles, J. Global Sodium Consumption and Death from Cardiovascular Causes. N Engl J Med. 2014, 371 (7), 624–634. [CrossRef]
- Huang, L.; Trieu, K.; Yoshimura, S.; Neal, B.; Woodward, M.; Campbell, N. R. C.; Li, Q.; Lackland, D. T.; Leung, A. a. C.; Anderson, C. A. M.; MacGregor, G. A. et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ. 2020, m315. [CrossRef]
- World Health Organization. WHO global report on sodium intake reduction. Available online: https://iris.who.int/bitstream/handle/10665/366393/9789240069985-eng.pdf (accessed on 13 March 2024).
- Filippini, T.; Malavolti, M.; Whelton, P.K.; Naska, A.; Orsini, N.; Vinceti, M. Blood pressure effects of sodium reduction. Circulation. 2021, 143 (16), 1542–1567. [CrossRef]
- Wang, K.; Jin, Y.; Wang, M.; Liu, J.; Bu, X.; Mu, J.; Lu, J. Global cardiovascular diseases burden attributable to high sodium intake from 1990 to 2019. J. Clin. Hypertens. 2023, 25 (9), 868–879. [CrossRef]
- Filippini, T.; Malavolti, M.; Whelton, P. K.; Naska, A.; Orsini, N.; Vinceti, M. Blood pressure effects of sodium reduction. Circulation. 2021, 143 (16), 1542–1567. [CrossRef]
- D’Elia, L.; Galletti, F.; Strazzullo, P. Dietary Salt Intake and Risk of Gastric Cancer. In: Zappia, V., Panico, S., Russo, G., Budillon, A., Della Ragione, F. (eds) Advances in Nutrition and Cancer, Cancer Treatment and Research. 2014, vol 159. Springer, Berlin, Heidelberg. [CrossRef]
- D’Elia, L.; Rossi, G.; Ippolito, R.; Cappuccio, F. P.; Strazzullo, P. Habitual salt intake and risk of gastric cancer: A meta-analysis of prospective studies. Clin Nutr. 2012, 31 (4), 489–498. [CrossRef]
- Bolhuis, D. P.; Costanzo, A.; Newman, L. P.; Keast, R. Salt promotes passive overconsumption of dietary fat in humans. J Nutr. 2016, 146 (4), 838–845. [CrossRef]
- Moosavian, S. P.; Haghighatdoost, F.; Surkan, P. J.; Azadbakht, L. Salt and obesity: a systematic review and meta-analysis of observational studies. Int J Food Sci Nutr. 2016, 68 (3), 265–277. [CrossRef]
- Teucher, B.; Dainty, J.; Spinks, C. A.; Majsak-Newman, G.; Berry, D. J.; Hoogewerff, J.; Foxall, R. J.; Jakobsen, J.; Cashman, K. D.; Flynn, A.; Fairweather-Tait, S. Sodium and bone health: Impact of moderately high and low salt intakes on calcium metabolism in postmenopausal women. J Bone Miner Res. 2008, 23 (9), 1477–1485. [CrossRef]
- Pećin, I.; Premužić, V.; Čvorišćec, D.; Erceg, I.; Fuček, M.; Jelaković M, Jovanović A, Kaić-Rak A, Laganović M, Lederer P, Perković M, Reiner Ž, Sertić J, Špišić T, Jelaković B: Salt Intake and the metabolic syndrome. Croatian Action on Salt and Health (CRASH). Kidney and Blood Pressure Research, 2009; 32:324.
- Kos, M.; Nađ, T.; Stanojević, L.; Lukić, M.; Stupin, A.; Drenjančević-Perić, I.; Pušeljić, S.; Cvetko, E. D.; Mihaljević, Z.; Dumančić, D.; Jukić, I. Estimation of salt intake in normotensive and hypertensive children: The role of body weight. Nutrients 2023, 15 (3), 736. [CrossRef]
- Cappuccio, F.P.; Kalaitzidis, R.; Duneclift, S.; Eastwood, J.B. Unravelling the links between calcium excretion, salt intake, hypertension, kidney stones and bone metabolism. J Nephrol. 2000;13(3):169–77. https://pubmed.ncbi.nlm.nih.gov/10928292/.
- Liu, W.; Zhou, L.; Yin, W.; Wang, J.; Zuo, X. Global, regional, and national burden of chronic kidney disease attributable to high sodium intake from 1990 to 2019. Front. Nutr. 2023, 10. [CrossRef]
- Premužić, V.; Miličić, B.; Krtalić, B.; Gellineo, L.; Knežević, T.; Jelaković, A.; Dapić, K.; Matašin, M.; Ivković, V.; Fuček, M.; Josipović, J.; Dika, Ž.; Kos, J.; Karanović, S.; Jelaković, B. New onset chronic kidney disease is associated with high sodium intake in population with low potassium consumption. J. Hypertens. 2019, 37, e249. [CrossRef]
- McMahon, E.; Campbell, K. L.; Bauer, J.; Mudge, D. W.; Kelly, J. Altered dietary salt intake for people with chronic kidney disease. Cochrane Library 2021, 2021 (6). [CrossRef]
- Wang, X.; Ma, H.; Kou, M.; Tang, R.; Xue, Q.; Li, X.; Harlan, T. S.; Heianza, Y.; Qi, L. Dietary sodium intake and risk of incident type 2 diabetes. Mayo Clinic Proceedings 2023, 98 (11), 1641–1652. [CrossRef]
- Hodson, E. M.; Cooper, T. E. Altered dietary salt intake for preventing diabetic kidney disease and its progression. Cochrane Library 2023, 2023 (1). [CrossRef]
- World Health Organization. Noncommunicable Diseases, Rehabilitation and Disability (NCD). Global action plan for the prevention and control of noncommunicable diseases 2013-2020. Available online: https://www.who.int/publications/i/item/9789241506236 (accessed on 15 February 2024).
- Cobiac, L.; Vos, T.; Veerman, L. Cost-effectiveness of interventions to reduce dietary salt intake. Heart 2010, 96 (23), 1920–1925. [CrossRef]
- Webb, M.; Fahimi, S.; Singh, G.; Khatibzadeh, S.; Micha, R.; Powles, J.; Mozaffarian, D. Cost effectiveness of a government supported policy strategy to decrease sodium intake: global analysis across 183 nations. BMJ. 2017, i6699. [CrossRef]
- Trieu, K.; Neal, B.; Hawkes, C.; Dunford, E.; Campbell, N. R. C.; Rodríguez-Fernández, R.; Legetić, B.; McLaren, L.; Barberio, A. M.; Webster, J. Salt Reduction Initiatives around the World – A Systematic Review of Progress towards the Global Target. PloS One 2015, 10 (7), e0130247. [CrossRef]
- Webster, J.; Dunford, E.; Hawkes, C.; Neal, B. Salt reduction initiatives around the world. J. Hypertens. 2011, 29 (6), 1043–1050. [CrossRef]
- McLaren, L.; Sumar, N.; Barberio, A. M.; Trieu, K.; Lorenzetti, D.; Tarasuk, V.; Webster, J.; Campbell, N. R. C. Population-level interventions in government jurisdictions for dietary sodium reduction. Cochrane Library 2016, 2017 (3). [CrossRef]
- Santos, J. A.; Tekle, D. Y.; Rosewarne, E.; Flexner, N.; Cobb, L. K.; Al-Jawaldeh, A.; Kim, W.; Breda, J.; Whiting, S.; Campbell, N. R. C. et al. A Systematic Review of Salt Reduction Initiatives around the world: A midterm evaluation of progress towards the 2025 Global Non-Communicable Diseases Salt Reduction Target. Adv Nutr. 2021, 12 (5), 1768–1780. [CrossRef]
- World Health Organization. Food & Nutrition Action in Health Systems (AHS). SHAKE the salt habit. Available online: https://www.who.int/publications/i/item/WHO-NMH-PND-16.4 (accessed on 19 January 2024).
- World Health Organization. Noncommunicable Diseases, Rehabilitation and Disability (NCD). Tackling NCDs: 'best buys' and other recommended interventions for the prevention and control of noncommunicable diseases. Available online: https://www.who.int/publications/i/item/WHO-NMH-NVI-17.9 (accessed 18 January 2024).
- Tang, N.; Huang, S.; Yang, Y.; Hu, A.; Wang, J.; Cheng, Z.; Liu, W. A review of the world’s salt reduction policies and strategies – preparing for the upcoming 2025. Food & Function 2023. [CrossRef]
- Eckel, R.H.; Jakicic, J.M.; Ard, J.D.; De Jesus, J.; Miller, N.H.; Hubbard, V.S.; Lee, I.-M.; Lichtenstein, A.H.; Loria, C.M.; Millen, B.E. et al. Z. 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk. Circulation 2014, 129 (25_suppl_2). [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Himmelfarb, C.D.; DePalma, S.M.; Gidding, S.S.; Jamerson, K.; Jones, D.W. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation (New York, N.Y.) 2018, 138 (17). [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clément, D.; Coca, A.; De Simone, G.; Dominiczak, A. F. bet al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. J. Hypertens. 2018, 36 (10), 1953–2041. [CrossRef]
- Board, N.; Potassium; Oria, M.; Harrison, M.; Stallings, V. A. Dietary reference intakes for sodium and potassium; 2019. [CrossRef]
- Turck, D.; Castenmiller, J.; De Henauw, S.; Hirsch-Ernst, K.; Kearney, J.; Knutsen, H. K.; Maciuk, A.; Mangelsdorf, I.; McArdle, H. J.; Peláez, C. et al. Dietary reference values for chloride. EFSA Journal 2019, 17 (9). [CrossRef]
- Croatian Institute of Public Health. Epidemiological data on cardiovascular diseases. Available online:https://www.hzjz.hr/aktualnosti/epidemioloski-podaci-o-kardiovaskularnim-bolestima/ (accessed on 10 January 2024).
- Murray, C. J. L.; Aravkin, A. Y.; Zheng, P.; Abbafati, C.; Abbas, K.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; Abdollahpour, I. et al.Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396 (10258), 1223–1249. [CrossRef]
- EH-UH | HDH. HDH. https://hdh.healthmed.hr/projekti/eh-uh (accessed on 20 February 2024).
- Jelaković, B.; Reiner, Ž.; Kusić, Z.; Ugarčić, Ž.; Drenjančević, I. Scientific opinion on the effect of reduced intake of salt in human nutrition. 2014. Zagreb. Available online: file:///C:/Users/mihaela/Downloads/HAH-Z-2014-1%20(9).pdf (accessed on 5 January 2024).
- Reiner, Ž.; Skupnjak B.; Jelaković, B. Launch of a promising national campaign to reduce salt intake in Croatia. Oral communication. Sixth Congress on Atherosclerosis, Rovinj, 2007.
- Less salt -- more health. Croatian action on salt and health (CRASH). PubMed. https://pubmed.ncbi.nlm.nih.gov/19514255/.
- Salt--hidden poison in everyday meal. PubMed. https://pubmed.ncbi.nlm.nih.gov/19642535/.
- Less salt--more health: possibilities of prevention in Croatia. PubMed. https://pubmed.ncbi.nlm.nih.gov/20649071/.
- Jelaković, B.; Vrdoljak, A.; Pećin, I.; Buzjak, V.; Karanović, S.; Ivković, V.; Dapić, K.; Domislović, V.; Reiner, Z. Less salt – more health. Croatian Action on Salt and Health (46). J Hypertens Res 2016, 2 (2), 61-68. Available online: http://hypertens.org/contents/pdfs/jhr-201606-020203.pdf (accessed on 5 February 2024).
- Jelaković, B.; Premužić, V.; Čvorišćec, D.; Erceg, I.; Fuček, M.; Jelaković, M.; Jovanović, A.; Kaić-Rak, A.; Laganović, M.; Lederer, P. et al. Salt Mapping in Croatia. Croatian Action on Salt and Health (CRASH). Kidney and Blood Press Research, 2009; 32:323, 2009.
- Sović, S.;Vitale, K.;Keranović, A;Dražić;Džakula, A.; Jelaković, B. Prevalence, awareness, treatment and control of hypertension and salt intake in some rural area of Sisak – Moslavina county, Croatia. Period. Biol. 2011. Vol. 113, No 3, 321 – 326.
- Pezo-Nikolić, B. Clinical benefit of continuous arterial pressure measurement in the early phase of essential hypertension. Master's thesis (mentor B. Jelaković). School of Medicine, University of Zagreb, Zagreb, Croatia. 2009.
- Salt and hypertension--silent killers. Inform yourself and live longer. World day of hypertension 2009 in Croatia]. PubMed. https://pubmed.ncbi.nlm.nih.gov/19642537/ .
- Ugarčić-Hardi, Ž.; Dumančić, G.; Pitlik, N.; Koceva Komlenić, D.; Jukić, M.; Kuleš, A.; Sabo, M. The salt content in bakery products in Osječko-baranjska County. At Proceedings of 5th International Congress „Flour-Bread ̀09“ and 7th Croatian Congress of Cereal Technologists, 551-556. Faculty of Food Technology, Osijek, 2010.
- Ugarčić-Hardi, Ž. Importance of salt content reduction in bakery products. U Annual 2010/2011 of the Croatian Academy of Engineering, 213-219. Croatian Academy of Engineering, Zagreb, 2012.
- Jurković, M.; Marijanović-Vincetić, D.; Jurković, Z.; Mandić, M.L.; Sokolić-Mihalak D. Salt intake through bakery products in Slavonia region. 7th International Congress "Flour-Bread '13" and 9th Croatian Congress of Cereal Technologists "Brašno-Kruh '13", 42-49, Faculty of Food Technology, Osijek, 2013.
- Pleadin, J.; Koprivnjak, O.; Krešić, G.; Gross-Bošković, A.; Buzjak Služek, V.; Tomljanović, A.; Kovačević, D. Daily salt intake through traditional meat products in Croatia. 2015; 17(6): 566-571.
- Hrvatska agencija za poljoprivredu i hranu, HAPIH (Croatian Agency for Agriculture and Food, CAAF), 2020. Scientific report on the intake of salt through the consumption of bread and bakery products. Ad hoc. Task force of the Center for Food Safety. Available online: https://www.hapih.hr/wp-content/uploads/2021/01/Znanstveno-izvjesce-o-unosu-kuhinjske-soli-konzumacijom-kruha-i-pekarskih-proizvoda_compressed.pdf (accessed on 15 January 2024).
- Hrvatska agencija za hranu, HAH (Croatian Food agency). Less salt – more health. 2014. ISBN: 978-953-55680-3-2. Available online: https://www.hah.hr/pdf/brosura-manje-soli-2014.pdf (accessed on 11 January 2024).
- Ordinance on cereals and cereal products (NN 101/2022.) Available online: https://narodne-novine.nn.hr/clanci/sluzbeni/2016_09_81_1823.html (accessed on 5 February 2024).
- Domislović, V.; Dapić, K.; Miličić, B.; Matašin, M.; Bukal, N.; Capak, K.; Drenjančević, I.; Gulin, M.; Herceg-Cavrak; Jelaković, A. et al. Positive trends in awareness of harmful effects of high salt intake - 10 years Croatian action on salt and health (CRASH). Data from 2008 and 2017 World hypertension days. J. Hypertens. 2018, 36 (Supplement 1), e130. [CrossRef]
- Croatian national programme for reduction of excessive salt intake. PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/25632778/ (accessed on 10 February 2024).
- Aždajić, M.D.; Delaš, I.; Aždajić, S.; Grbić, D. Š.; Vahčić, N. A cross sectional study of salt content in bakery bread in Zagreb, Croatia. Archives for Occupational Hygiene and Toxicology. 2019, 70 (3), 219–223. [CrossRef]
- Karanović, S.; Vrdoljak, A.; Ivković, V.; Dika, Ž.; Domislović, V.; Dapic, K.; Gallineo, L.; Ivandić, E.; Josipović, J.; Vuković, I.; Kos, J.; Laganović, M.; Vrkić, T. Ž.; Fodor, Lj.; Matijević, V.; Fuček, M.; Čulig, J.; Stevanović, R.; Jelaković, B. [PP.30.14] salt consumption in Croatian continental rural population. Journal of Hypertension 2016, 34 (Supplement 2), e311. [CrossRef]
- Croatian Agency for Agriculture and Food, Ad hoc Working Group, Jelaković, B.; Pollak, L.;, Medić, H.; Čačić Kenjerić, D.; Šimundić, T.; Stražanac, D.; Gross - Bošković, A.: Scientific report on the intake of table salt through the consumption of meat products. in 2020.
- Ordinance on salt (NN 89/11), 2011. Available online: https://www.zakon.hr/cms.htm?id=12012 (accessed on 2 March 2024).
- Ma, Y.; He, F. J.; Sun, Q.; Yuan, C.; Kieneker, L. M.; Curhan, G. C.; MacGregor, G. A.; Bakker, S. J. L.; Campbell, N. R. C.; Wang, M. et al. 24-Hour urinary sodium and potassium excretion and cardiovascular risk. N Engl J Med. 2022, 386 (3), 252–263. [CrossRef]
- World Health Organization. Effect of increased potassium intake on blood pressure, renal function, blood lipids and other potential adverse effects. Available online: https://www.who.int/publications/i/item/9789241504881 (accessed on 10 January 2024).
- D’Elia, L.; Barba, G.; Cappuccio, F. P.; Strazzullo, P. Potassium intake, stroke, and cardiovascular disease. J Am Coll Cardiol. 2011, 57 (10), 1210–1219. [CrossRef]
- World Health Organization. Guidelines Review Committee. Guideline: potassium intake for adults and children. Available online: https://www.who.int/publications/i/item/9789241504829 (accessed on 21 February 2024).
- Vulin, M.; Magušić, L.; Metzger, A.-M.; Muller, A.; Drenjančević-Perić, I.; Jukić, I.; Šijanović, S.; Lukić, M.; Stanojević, L.; Cvetko, E. D. et al. Sodium-to-Potassium ratio as an indicator of diet quality in healthy pregnant women. Nutrients 2022, 14 (23), 5052. [CrossRef]
- Miličić, B.; Krtalić, B.; Gellineo, L.; Knežević, T.; Jelaković, A.; Premužić, V.; Dapić, K.; Ivković, V.; Matašin, M.; Fuček, M. et al. Sodium and potassium intake in rural population. J. Hypertens. 2019, 37, e315–e316. [CrossRef]
- Jelaković, A.; Miličić, B.; Krtalić, B.; Gellineo, L.; Knežević, T.; Premužić, V.; Abramović, M.; Domislović, V.; Ivković, V.; Fuček, M. et al. Sodium-to-potassium ratio and new onset hypertension. J. Hypertens. 2019, 37, e121. [CrossRef]
- Chairperson, G.M.; Co-Chair, R.K.; Brunström, M.; Burnier, M.; Grassı, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, C.; Agabiti-Rosei, E.; Algharably, E. et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension. Journal of Hypertension 2023, 41 (12), 1874–2071. [CrossRef]
| 2008 | 2020 | Difference in the salt intake | % of change |
|
|---|---|---|---|---|
| Whole group | 11.3 (4.5) | 9.5 (4.1) | -1.8 | 15.9 % |
| Men | 13.3 (4.3) | 10.3 (4.4) | -3.0 | 22.8 % |
| Women | 10.2 (4.2) | 9.0 (3.3) | -1.2 | 11.7 % |
| World Hypertension Day, 2008 (%) |
World Hypertension Day, 2017 (%) | May Measurement Month, 2023 (%) | ||
|---|---|---|---|---|
| N | 1076 | 2175 | 10 480 | |
| Questions | Do you know that high salt intake is harmful for your health ? Yes. | 65.3 | 95.8 | 96.9 |
| Have you got this information from physician ? Yes. | 48.9 | 89.1 | 33.8 | |
| Are you eating to salty? Yes | 27 | 36.1 | 36.2 | |
| If advised, would you be able to reduce salt intake ? Yes. | 69.4 | 77.8 | 87.9 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





