Health services is centered around the provision of care and assistance to individuals who need medical attention. Nurses are at the forefront of patient care, providing direct assistance and support to individuals in various healthcare settings [
1]. Ethical judgments are of paramount importance in the nursing profession. They guide nurses in providing patient-centered care, resolving ethical dilemmas, upholding professional integrity, and building trust. By incorporating ethical considerations into their practice, nurses contribute to the overall well-being and safety of their patients while maintaining the highest standards of professionalism [
2,
3]. Specifically, ethical judgments can help nurses advocate for their patients' rights and well-being. Nurses must make decisions that prioritize the best interests of their patients, ensuring they receive appropriate care, respect, and dignity [
4]. Ethical judgments provide a framework for nurses to make informed decisions when faced with complex situations. They help nurses navigate moral dilemmas, such as end-of-life care, confidentiality breaches, and resource allocation, by considering the values and ethical principles involved [
5].
Therefore, understanding the relationship between nursing roles and ethical decision-making is pivotal. This research aimed to examine how the concept of nursing roles and nursing professional identification influence deontological and utilitarian inclinations in ethical decisions.
Moral Judgment and Process Dissociation Procedure
Moral judgment is defined as evaluations (good vs. bad) of the actions or character of a person that are made concerning a set of virtues held to be obligatory by culture or subculture [
6]. People often judge actions based on two principles: utilitarianism and deontology. Utilitarian judgments maximize the greatest good for the greatest number, whereas deontological judgments check whether a specific action is against existing rules, principles, and norms that must be honored [
7,
8,
9].
The present study followed Conway and Gawronski’s study [
9] using the Process dissociation procedure to discuss how nursing role affects utilitarian and deontological inclinations in moral judgments. The classical approach treats utilitarian and deontological inclinations as opposite ends of a bipolar continuum. However, Conway and Gawronski proposed that utilitarian and deontological inclinations are conceptually distinct and functionally independent processes, so moral judgement can be based on both inclinations at the same time, rather than only one of them [
9]. They think that classical moral dilemmas such as footbridge dilemma cannot analyze the specific contribution of deontological inclination or utilitarian inclination in moral judgments. Therefore, they adapted Process Dissociation (PD) procedure proposed by Jacoby [
10] to study utilitarian and deontological inclinations in moral dilemma judgments.
Moral Judgements of Nurses
A series of studies has focused on how nurses' moral judgments affect their moral behavior and clinical practice, suggesting that nurses' moral judgments play a crucial role in guiding clinical practice and ensuring patients receive quality healthcare [
1,
2,
3,
11,
12]. Therefore, studying nurses' moral judgments holds significant importance. An early study found a high correlation between moral judgments and moral behavior among practicing nurses [
2]. Similarly, recent research conducted on registered nurses has also identified the same effect. The study assessed judgments and ethical behaviors of nurses using Hospital Ethics Committee Survey Questionnaire, and found that judgments and ethical behaviors of nurses were evaluated at the moderate and good level [
1].
Furthermore, researchers have emphasized the need to enhance nurses' moral judgment abilities and moral development to better guide their professional work and provide improved healthcare services to patients [
1,
11,
13]. Thus, many studies on nurses' moral judgments have adopted Rest's Four Component Model and Kohlberg's moral development theory to understand the moral judgments of nurses at different stages of their professional careers and to explore ways to enhance nurses' moral judgment abilities [
1,
2,
13,
14].
The role of nursing education in developing ethical competence and moral judgment has been explored in various studies [
1,
2,
13,
14]. Researchers have examined the effectiveness of ethics education programs, the integration of ethics into nursing curricula, and the impact of educational interventions on nurses' moral judgment skills. Previous studies utilized different tools to measure the impact of educational interventions on improving nurses' moral judgment abilities, including Rest's Defining Issues Test [
2,
15], the Hospital Ethics Committee Survey Questionnaire [
1], Questionnaire of Moral Judgment and Ethical Decisions (QMJED) [
16], the Moral Competence Questionnaire for Public Health Nurses [
3]. These studies have found that educational interventions effectively enhance nurses' moral judgment abilities. This effect has been observed not only among registered nurses but also among practicing nurses and nursing students. Also, this findings are proved in different cultural contexts [
1,
3,
13,
15].
Nurses often encounter ethical dilemmas in their practice, such as end-of-life care, patient autonomy, informed consent, confidentiality, and resource allocation. Most moral judgments in dilemmas are based on two categories of moral theories: deontology and utilitarianism. However, previous research has paid limited attention to how nurses employ different moral theories to engage in moral reasoning when facing ethical dilemmas. The present study employs process dissociation technique to measure nurses’ deontological and utilitarian inclinations and examines how nurses make judgments based on different moral theories in moral dilemmas. Meanwhile, we further aimed to discuss what cognitive processes contributed to these moral reasoning. We used Moral Orientation Scale [
17] to assess four moral orientations (integration, deliberation, rule and sentiment inclinations) usually involved in moral reasoning, and tested if they explain the effect of nurse role identification on deontological and utilitarian thinking.
The dual-process model of moral judgment [
18,
19,
20] states that there are two key psychological processes involved: affective processes and cognitive processes. Previous studies have demonstrated that a number of factors associated affective processes lead to more deontological thinking, and cognitive evaluation of outcomes is usually associated with utilitarian moral judgments [
21,
22,
23,
24,
25,
26]. Recently researchers also focus on some other processes that might involve in moral reasoning but have not been investigated by dual-process model, such as rule orientation, deliberation orientation, integration and sentiment orientations [
17]. Previous studies found that higher rule orientation and sentiment orientation can predict higher deontological moral inclination and lower utilitarian inclination, while higher deliberation orientation is negatively associated with deontological inclination and positively associated with utilitarian inclination [
17,
19,
20,
26]. Integration orientation is characterized by the inclination to combine emotional reactions with cognitive reflection, which is considered a characteristic of advanced moral reasoning [
27]. Individuals with high scores in integration orientation engage in thorough consideration of pertinent arguments, exhibit emotional empathy towards all potential victims, and demonstrate flexibility in considering various response options. Usually, it produces a modest deontological pattern of responding on relative dilemma judgments [
17].
We predict that nursing role will lead to higher deontological inclination. Nursing is a profession deeply rooted in ethical principles [
28]. Nurses are bound by a code of ethics, which emphasizes the importance of patient advocacy, autonomy, and respect for human dignity. These ethical guidelines encourage nurses to prioritize their duty to do what is right, regardless of the consequences. Also, nurses have a strong sense of duty and responsibility towards their patients. They are trained to prioritize patient safety, provide competent care, and act in the best interest of the patient [
29]. Deontological ethics reinforces the idea that nurses have a moral obligation to fulfill their professional duties, even when faced with challenging moral dilemmas [
7].
Meanwhile, nursing practice requires nurses to engage in complex decision-making that involves integrating both affective and cognitive processes [
30]. Nurses must consider not only the clinical and medical aspects of a situation but also the emotional and psychosocial dimensions of patient care [
31]. They often encounter morally challenging situations where they need to navigate conflicting values, emotions, and ethical considerations. The integration of affective reactions with cognitive deliberation allows nurses to thoroughly consider the potential impact of their decisions on patients, families, and other stakeholders. Previous research found that integration inclination is usually associated with higher deontological thinking [
17], so we assumed that nurse role may increase deontological thinking via integration inclination.
We predict that nursing role will lead to lower utilitarian inclination. Nurses often face ethical dilemmas in which there are no clear-cut or objectively measurable outcomes. The complexity and uncertainty of healthcare situations make it challenging to accurately predict the consequences of different courses of action [
32]. In such cases, nurses may be more inclined to rely on their professional judgment, experience, and intuition rather than solely relying on utilitarian calculations [
33].
Nurses frequently work in high-pressure environments with limited time and resources [
34]. These constraints may impact their decision-making, leading them to prioritize immediate actions that address the patient's immediate needs rather than considering long-term consequences. Utilitarianism often requires a more comprehensive analysis of outcomes, which may be challenging given the practical realities nurses face [
7].
Nursing ethics emphasize principles such as autonomy, beneficence, and non-maleficence. These principles guide nurses in providing compassionate care and respecting patient autonomy [
35]. While utilitarianism also values these principles, the emphasis on the overall outcome may conflict with the individual-focused approach that nurses are trained to uphold.
Also, nurses may prioritize individual patient needs and immediate concerns, which may sometimes diverge from the utilitarian perspective. Nurses are trained to prioritize the well-being and individual needs of their patients [
36]. This focus on patient-centered care may lead nurses to consider the immediate needs and preferences of the patient, potentially influencing their moral decision-making. In some cases, this may conflict with the utilitarian perspective, which aims to maximize overall happiness or well-being for the greatest number of people.
Therefore, we assumed that deliberation, rule, integration, and sentiment thinking orientations can explain the effect of nursing role on moral judgments.
The Present Study
The present study was designed to test the effects of nurse role on moral judgments. Specifically, we manipulated the concept of nursing role (Study 1) and measured nurse-role identification (Study 2), and used PD procedure to assess participants’ deontological and utilitarian orientations. Also, in study 2, we assessed four moral orientations (integration, deliberation, rule and sentiment), and tested if they mediated the effect of nurse-role identification on deontological and utilitarian thinking. We predicted that nurse-role identification would decrease the utilitarian inclination during moral reasoning and increase the tendency to adopt a deontological approach, and that deliberation, rule, integration and sentiment orientations mediated the relationship between money and utilitarian and deontological moral thinking inclinations.
Study 1
Participants and Design
We recruited 90 nurses (77 female and 13 male, age from 18 to 50, M=26.86, SD= 7.24) from 2 hospitals in China. Participants were randomly assigned to one of two conditions: nursing role prime or neutral prime. All subjects participated voluntarily.
Procedure and Materials
Participants firstly were asked to complete a scrambled-sentences task in which they were exposed to nursing role related words or neural words. The scrambled-sentences task consists of 30 sets of five jumbled words. Participants had to create a sensible sentence using four of the five words within the time limit. In the neutral condition, the phrases primed neutral concepts (e.g., words “hometown, future, occasionally, he, recall” can be used to create a sentence “he occasionally recalls hometown”). In the nursing role prime condition, 15 of the phrases primed the concept of nursing role (e.g., words “in, observe, nurses, work, hospital” can be used to create a sentence “nurses work in hospital”), whereas the remaining 15 sets of words were neutral phrases.
After scrambled-sentence task, participants read 20 moral dilemmas in the study of Conway and Gawronski, in which they must choose whether to perform a harmful action to achieve a particular outcome [
9]. After reading each dilemma, participants were asked to indicate whether the described action would be
appropriate or
inappropriate according to their opinion. There were 10 basic dilemmas in total, each being presented in incongruent and congruent versions. Incongruent dilemmas depict the outcomes of harmful action as more beneficial than the harm caused by act. Responses consistent with utilitarianism (accept harm) are incongruent with responses consistent with deontology (reject harm). In congruent dilemmas, the outcome of causing harm is diminished such that causing harm no longer maximizes outcomes, so responses consistent with utilitarianism are congruent with responses consistent with deontology. Finally, participants provided demographic data.
Results and Discussion
Overall, harmful action was judged acceptable on 50.1% of the incongruent dilemmas and 37% of the congruent dilemmas. The difference between the two kinds of dilemmas was statistically significant, t(89) = 9.81, p < .001.
PD scores of deontology (D parameter) and utilitarianism (U parameter) were calculated using the algebraic formulas of Conway and Gawronski’s study [
10]. We used ANOVA analysis to test the effect of nurse roles on D and U parameters, and participants in nursing role group (
M = 0.61,
SD = 0.18) showed higher deontological inclinations compared to those in control group (
M = 0.53,
SD = 0.15),
F (1, 88) = 5.33,
p = .02,
η2p = .06, but there was no significant difference between nursing role group (
M = 0.12,
SD = 0.13) and control group (
M = 0.15,
SD = 0.13) in utilitarian inclinations,
F(1, 88) = 1.31,
p = .26,
η2p = .02.
Priming the role of nurse affects deontological inclinations, and did not influence utilitarian inclinations. Participants primed with nurse role showed higher deontological inclinations than those primed with neutral concept. This is different from our assumption. This may be due to that scrambled-sentences task cannot truly evoke the nurses' associations with real work contexts. Therefore, in Experiment 2, we directly measured the identification with the nursing role, aiming to explore the long-term influencing traits associated with the professional role on moral judgments.
Study 2
Study 2 investigated the relationship between nurse-role identification and moral judgments to further test whether long-term trait associate with nurses’ professional role has a similar effect on moral thinking as priming the role of nurse. We hypothesized that individuals with higher levels of nurse-role identification are more likely to rely on deontological thinking and less likely to rely on utilitarian thinking in moral judgments. Meanwhile, to unveil the mechanism underlying the effect of nurse role on moral thinking, we also used moral orientation scale [
17] to assess participants’ integration, deliberation, rule and sentiment orientations, and tested if these orientations mediate the effect of nurse-role identification on deontological and utilitarian approach.
Participants
We recruited 496 subjects (193 male and 303 female, age from 18-59,
M=29.58,
SD=8.10) from an online platform (
www.wenjuan.com) in China. All subjects participated voluntarily, and none of them participated in Study 1.
Procedure and Materials
In this study, nurse role identification scale (α = .736) is from the organizational identification scale originally developed by Mael and Ashforth [
37] with word firm substituted by profession in the scale items. We used five-item edition modified by Lui, Ngo and Tsang [
38]. The 5-item scale is rated on a 7-point scale ranging from 1 (strongly disagree) to 7 (strongly agree).
Next, participants were instructed to complete Moral Orientation Scale (MOS), consisting of 28 items, and each of the 7 items within each subscale [
17]. Four subscales measure integration, deliberation, rule, and sentiment. These four orientations are all important thinking processes in moral reasoning. Although we expected that only deliberation and rule acts as a mediation in the relationship between nurse-role identification and D and U inclinations, four subscales were all used in research. Participants indicated their level of agreement on a 7-point Likert scale, ranging from strongly disagree (1) to strongly agree (7). The order of the items was randomized. The internal consistencies of the subscales were found to be acceptable to good, with Cronbach's alpha coefficients ranging from .73 to .89.
After answering nurse-role identification scale, participants read moral dilemmas and made moral judgments as study 1. Finally, participants provided demographic data.
Results and Discussion
Overall, harmful action was judged acceptable on 52.8% (SD=0.19) of the incongruent dilemmas and 37.9% (SD=0.18) of the congruent dilemmas. The difference between the two kinds of dilemmas was statistically significant, t(495)=18.00, p<.001.
PD scores of deontology (D parameter) and utilitarianism (U parameter) were calculated using the algebraic formulas of Conway and Gawronski [
9]. We used regression analysis to examine the relationship between nurse-role identification and deontological inclination and utilitarian inclination, and found that nurse-role identification was positively related to individuals' deontological inclinations,
β=.20,
t(495)=4.44,
p<.001, 95%CI[.02, .04], and was negatively associated with individuals' utilitarian inclinations,
β=-.10,
t(495)=-2.21,
p=.027, 95%CI[-.03, -.002].
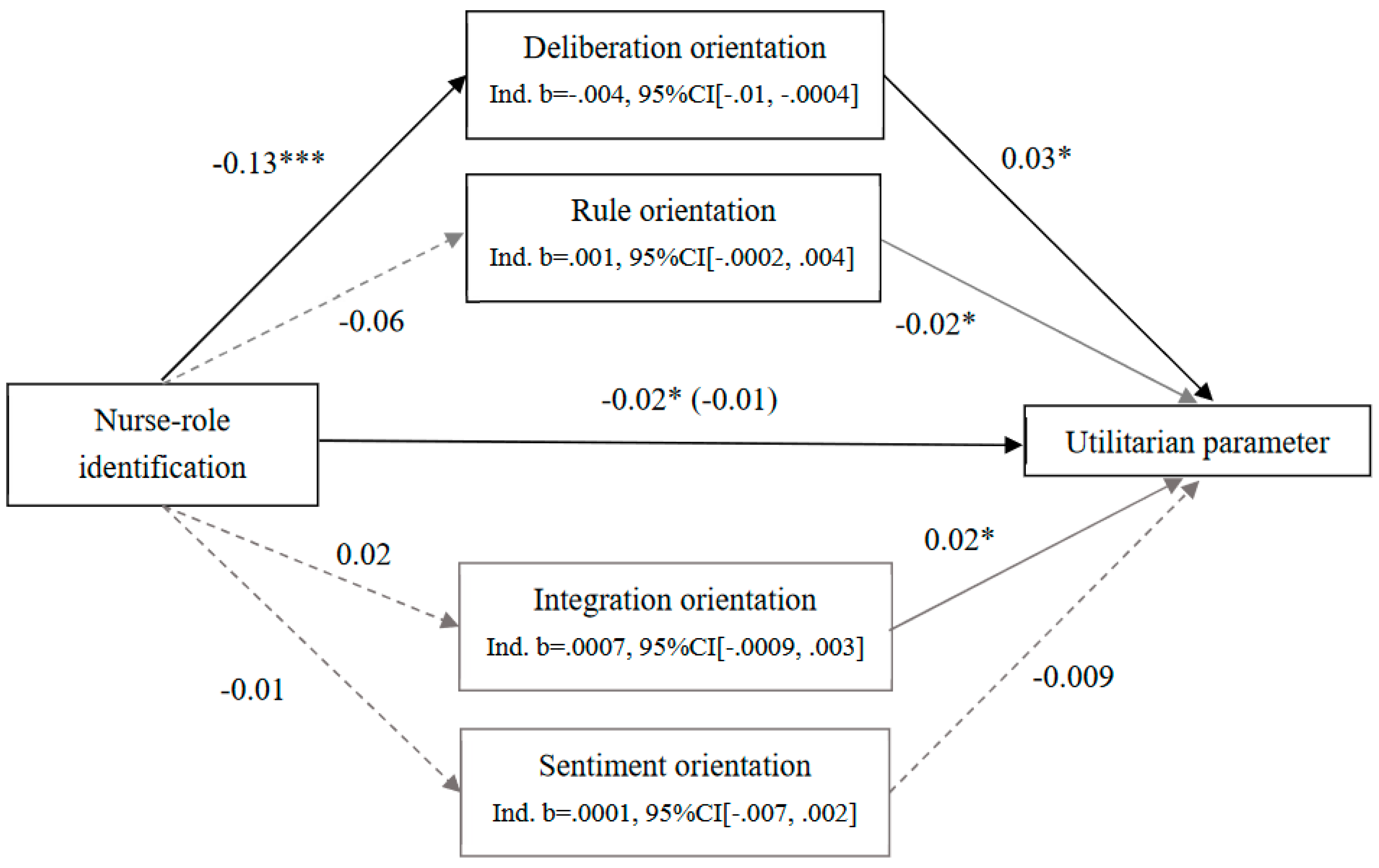
We used Process for SPSS (Model 4 [
39]) to examine whether each of the four moral orientations mediated the effect of nurse-role identification on utilitarian parameter with 5000 bootstrapped samples. Only deliberation mediated the effect of nurse-role identification on utilitarian inclination (see
Figure 1). Firstly, nurse-role identification was negatively associated with utilitarian parameter,
b=-.02, SE=.007,
t(495)=-2.21,
p=.027, 95%CI[-.03, -.002]. Meanwhile, nurse-role identification negatively predicted deliberation,
b=-.13, SE=.03,
t(495)= -5.18,
p<0.001, 95%CI[-.18, -.08], and deliberation was positively related with utilitarian parameter,
b=.03, SE=0.01,
t(495)= 1.99,
p=.047, 95%CI [.003, .06]. After including deliberation orientation, nurse-role identification had no relationship with utilitarian parameter,
b=-.01, SE=.007,
t(495)=-1.86,
p=.06, 95%CI [-.03, .0007]. Nurse-role identification was associated with decreased utilitarian parameter, because it was related to decreased deliberation orientation. However, nurse-role identification was not related with rule,
b=-.06, SE=.03,
t(495)=-1.70,
p=.09, 95%CI[-.13, .01], sentiment,
b=-.01, SE=.04,
t(495)=-.32,
p=.75, 95%CI[-.09, .06], and integration orientations,
b=.02, SE=.03,
t(495)=.76,
p=.44, 95%CI[-.04, .08]. Therefore, these three orientations did not mediate the relationship between the identification to nursing role and utilitarian parameter.
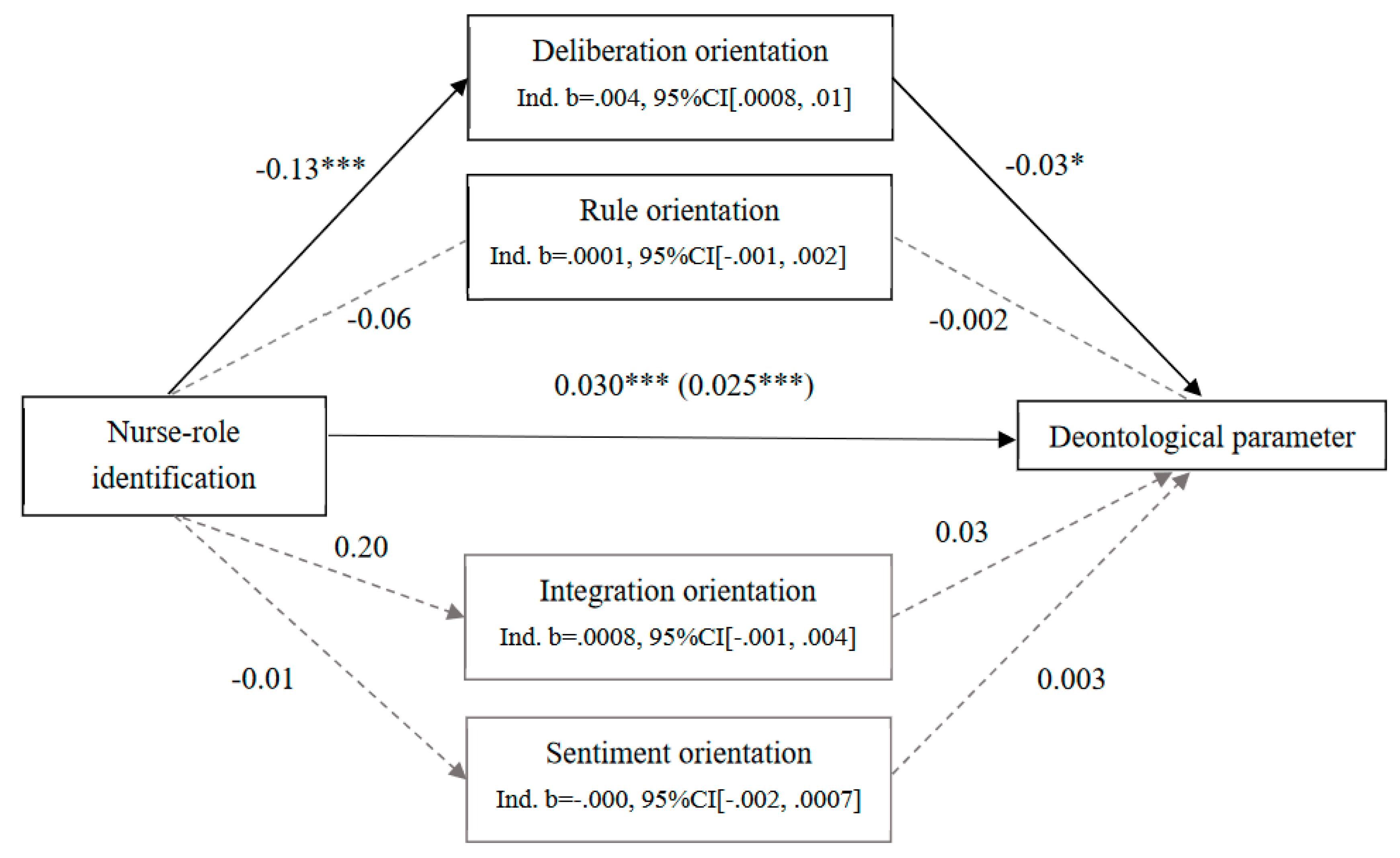
Also, we examined whether each of the four moral orientations mediated the effect of nurse-role identification on deontological parameter with 5000 bootstrapped samples. Only deliberation orientations partly mediated the effect of nurse-role identification on deontological inclination (see
Figure 2). Firstly, nurse-role identification was positively associated with deontological parameter,
b=.030, SE=.007,
t(495)=4.44,
p<.001, 95%CI[.017, .044]. Meanwhile, nurse-role identification negatively predicted deliberation orientation,
b=-.13, SE=.03,
t(495)=-5.18,
p<.001, 95% CI [-.18, .08], and deliberation was negatively related with deontological parameter,
b=-.03, SE=0.02,
t(495)=-2.17,
p=.03, 95%CI [-.06, -.003]. After including deliberation orientation, the effect of nurse-role identification on deontological parameter decreased,
b=.025, SE=.007,
t(495)=3.53,
p=.0004, 95%CI[.011, .039]. This prove that deliberation partly mediated the effect of nurse-role identification on deontological inclination. As nurse-role identification was not related with rule, sentiment, and integration orientations, these three orientations did not mediate the relationship between the identification with nursing role and deontological parameter.
Study 1 used scrambled-sentence task to prime nursing role, while study 2 selected nurse-role identification, a trait variable, to investigate the effect of nursing role on moral judgments. Consistent with study 1, study 2 found that nursing role was positively associated with individuals' deontological inclination. Nursing role identification was negatively related to utilitarian inclinations, which is different from the effect of priming nursing role on moral judgments. Also, study 2 explored the mechanism underlying the effect of nursing role on deontological and utilitarian thinking. Nursing role can decrease utilitarian moral thinking and increase deontological thinking, because the identification with nursing role grant individuals lower deliberation orientation.
General Discussion
Although a large number of previous studies have explored the moral judgment of nurses, most of the research has focused on the developmental stages of nurses' moral levels and the association between moral judgment and their professional behavior [
1,
2,
4]. These studies aimed to improve nurses' moral development through educational interventions in order to enhance their ability to provide better healthcare services. However, there is limited research on how nurses engage in moral reasoning based on different moral principles when facing moral dilemmas. Deontology and utilitarianism are two moral frameworks that have received significant attention in the study of moral dilemmas. However, previous researchers have paid little attention to these aspects in the study of nurses' moral judgment.
The current research examined how nursing role (the concept of nursing role and nurse-role identification) affects deontological and utilitarian moral thinking inclinations in moral judgments using process dissociation technique. We predicted that both priming the concept of nurse role and nursing role identification would decrease utilitarian inclinations and increase deontological moral inclinations in moral judgments. Also, we tested whether the effect of nursing role on deontological and utilitarian inclinations is mediated by moral orientations.
Our predictions are partly supported by two studies, while activating the concept of nursing role and assessing nurse-role identification show different effects on moral judgments. Study 1 examined the effect of nursing role on moral judgments by activating the concept of nursing role, demonstrating that participants primed with nursing role showed higher deontological inclinations in moral judgments than those primed with neutral concept. No difference was found in utilitarian moral thinking inclination between two conditions. To test whether long-term attitudes towards nursing profession have similar influences on moral judgments, Study 2 further tested the effect of nurse-role identification, and revealed that the nursing role identification was positively related to deontological inclinations, and was negatively related to utilitarian inclinations, which was different from Study 1. We also found the mediating effect of deliberation underlying the relationship between nursing role identification and deontological and utilitarian inclinations in study 2.
As all the participants recruited for our study were adult nurses who were already working, we believe that their moral development levels have already reached a relatively high stage in Kohlberg's theory [
40] of moral development. Therefore, unlike previous research, our focus is not on how high individuals' moral development levels are, but rather on how the nursing profession influences individuals' moral reasoning and judgment after nurses have reached a relatively mature level of moral development. The nursing profession has its own uniqueness compared to other professions. Nurses are generally perceived to possess higher morality level. Due to the connection between nursing work and human life and health, nurses bear significant responsibilities and are required to have a stronger sense of duty, as well as greater compassion and empathy compared to other professions [
28,
35]. Additionally, the demanding and high-pressure work environment may lead nurses to exhibit different moral judgment patterns compared to ordinary individuals or other professions in moral dilemmas [
34]. Therefore, we believe that the nursing profession and the identification with nursing role can influence individuals' moral judgments.
Nursing, as a profession, is characterized by a strong emphasis on ethical principles and codes of conduct [
28]. Nurses are guided by professional ethics, such as beneficence, non-maleficence, autonomy, and justice [
35], which align closely with deontological ethics. Furthermore, professional identification fosters a sense of responsibility and identification towards the nursing profession's values and standards [
29]. Nurses who deeply identify with their profession are more likely to perceive their role as one of moral stewardship and advocate for ethical practices [
32]. They may prioritize upholding professional norms and obligations, even when faced with conflicting considerations or potential negative consequences. Deontological ethics prioritize adherence to moral rules and duties, regardless of the consequences or outcomes [
7,
8]. Nurses who strongly identify with their profession are more likely to internalize and embrace these ethical principles, leading to a higher inclination towards deontological reasoning.
In recent years, nurses face increasing workload and time constraints [
41]. Due to staffing shortages and an ever-increasing demand for healthcare services, nurses often find themselves working in a fast-paced and high-pressure environment [
42]. As a result, they may not have enough time to engage in extensive deliberation when making decisions. The decrease in deliberation orientation can have implications for ethical decision-making as it can lead to higher deontological thinking. Deontological ethics emphasizes following moral rules and duties regardless of the consequences [
7,
8,
9]. In the context of nursing, this means that nurses may rely more on established protocols and guidelines rather than considering the specific needs and values of individual patients.
Nevertheless, deliberation orientation only partially mediates the effect of nursing role identification on deontological thinking. This means that there is still other mechanism that can explain the relationship between nursing role identification and deontological thinking. Further study can discuss this question.
Nursing role identification reduces individuals' utilitarian inclination, primarily due to nurses facing limited time and heavy workloads [
34,
41], which leaves them with insufficient time for deep reflection, while utilitarian moral tendencies often result from thoughtful deliberation. Nurses are not given ample time or opportunity to deliberate or think deeply about their actions and decisions. This decrease in deliberation orientation can lead to lower utilitarian thinking among nurses.
The nursing role guides people to not rely on utilitarian thinking to make judgments. However, this effect only exists in nursing role identification, but was not found in people primed with nursing role. Priming the nursing role and professional identification have different influences on moral reasoning. This suggests that the effects of word scramble tasks on moral judgments are different from long-term professional identification.
This research contributes to the understanding of moral thinking of nurses. Both temporary thinking about nursing role and long-term identification with nursing role lead to decreasing the willingness to harm others to achieve greater good. As a profession, nursing work and the role of nurses encourage people to think more about caring for others and following rules, when faced with moral dilemmas.
While deontological thinking has its merits, it may overlook the unique circumstances and preferences of patients. It can result in a one-size-fits-all approach to care, potentially compromising patient-centeredness and autonomy. Utilitarian thinking is a moral framework that focuses on maximizing overall happiness or utility for the greatest number of people [
7,
8]. In the context of nursing, utilitarian thinking involves making decisions and taking actions that prioritize the well-being and best interests of patients. When nurses have less time for deliberation or thoughtful consideration, they may be more likely to rely on quick, instinctive judgments or follow established protocols without fully considering the unique needs and circumstances of individual patients. Furthermore, decreased deliberation orientation may limit nurses' ability to critically analyze complex situations, weigh potential risks and benefits, and consider alternative courses of action. This can lead to suboptimal decision-making and potentially compromise patient outcomes. Therefore, it is important for nurses and healthcare organizations to strike a balance between adhering to guidelines and incorporating ethical deliberation to ensure the best possible care for patients.
Conclusions
The present study investigated the relationship between nursing role and moral judgments. Priming nursing role affects individuals' deontological inclinations in moral judgments, but do not influence individuals’ utilitarian inclinations. Individuals primed with the concept of nursing role show higher deontological inclinations compared with those priming with neutral concept. Nursing role identification is positively associated with deontological inclinations in moral judgments, and is negatively associated with utilitarian inclinations, because nursing role identification decreased deliberation orientation.
Data availability statements
The raw data supporting the conclusions of this article will be made available by the authors on request.
Ethics Approval
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Department of Psychology, Wuhan University (No: 202002, date of approval: 15th April, 2020).
Author Contributions
Mufan Zheng and Junhua Zhao conceived the original ideas, designed the experiments. Mufan Zheng carried out the experiments, collected the data, and analysed the data. Mufan Zheng and Junhua Zhao wrote, reviewed and edited the manuscript.
Acknowledgments
This research was supported by a grant from National Social Science Foundation of China (Grant No. 20CSH071) to Mufan Zheng.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Borhani, F., Abbaszadeh, A., Bahrampour, A., Ameri, G. F., & Aryaeenezhad, A. Role of judgment in promoting nurses’ decisions and ethical behavior. Journal of Education and Health Promotion, 2021, 10, 1–5.
- Ketefian, S. (1981) Moral reasoning and moral behavior among selected groups of practicing nurses. Nursing Research, 1981, 30, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Asahara, K. , Kobayashi, M., & Ono, W. (2015) Moral competence questionnaire for public health nurses in Japan: S cale development and psychometric validation. Japan Journal of Nursing Science, 2015, 12, 18–26. [Google Scholar] [PubMed]
- Pavlish, C., Brown-Saltzman, K., Hersh, M., Shirk, M., & Rounkle, A. M. (2011) Nursing priorities, actions, and regrets for ethical situations in clinical practice. Journal of Nursing Scholarship, 2011, 43, 385–395.
- Hayes, C. (2004) Ethics in end-of-life care. Journal of Hospice & Palliative Nursing, 2004, 6, 36–43. [Google Scholar]
- Haidt, J. (2001) The emotional dog and its rational tail: A social intuitionist approach to moral judgment. Psychological Review, 2001, 108, 814–834. [Google Scholar] [CrossRef] [PubMed]
- Gawronski, B., Armstrong, J., Conway, P., Friesdorf, R., & Hütter, M. (2017) Consequences, norms, and generalized inaction in moral dilemmas: The CNI model of moral decision-making. Journal of Personality and Social Psychology, 2017, 113, 343–376.
- Gawronski, B., & Beer, J. S. (2017) What makes moral dilemma judgments “utilitarian” or “deontological”? Social Neuroscience, 2017, 12, 626–632.
- Conway, P., & Gawronski, B. (2012) Deontological and utilitarian inclinations in moral decision making: A process dissociation approach. Journal of Personality and Social Psychology, 2012, 104, 216–235.
- Jacoby, L. L. (1991) A process dissociation framework: Separating automatic from intentional uses of memory. Journal of Memory and Language, 1991, 30, 513–541. [Google Scholar] [CrossRef]
- Ketefian, S. (1981). Critical thinking, educational preparation, and development of moral judgment among selected groups of practicing nurses. Nursing research, 1981, 30, 98–103. [Google Scholar] [CrossRef]
- Khoobi, M., & Ahmadi, F. (2023) Maintaining Moral Sensitivity as an Inevitable Necessity in the Nursing Profession. Journal of Caring Science, 2023, 12, 1–2.
- Lee, M. A. (2013) Changes in nursing students' moral judgment and ways to evaluate the effect of ethics education. Journal of Korean Academy of Nursing Administration, 2013, 19, 351–360. [Google Scholar] [CrossRef]
- McLeod-Sordjan, R. (2014). Evaluating moral reasoning in nursing education. Nursing ethics, 2014, 21, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Iz, F. B., & Ozsoy, S. A. (2013) Determination of nursing students’ moral judgment: A city in west regıon of Turkey. HealthMED, 2013, 7, 142–149.
- Abou Hashish, E. A., & Ali Awad, N. H. (2019) Relationship between ethical ideology and moral judgment: Academic nurse educators’ perception. Nursing Ethics, 2019, 26, 845–858.
- Fleischmann, A., Lammers, J., Conway, P., & Galinsky, A. D. (2019) Paradoxical effects of power on moral thinking: Why power both increases and decreases deontological and utilitarian moral decisions. Social Psychological and Personality Science, 2019, 10, 110–120.
- Greene, J. D. (2009) Dual-process morality and the personal/impersonal distinction: A reply to McGuire, Langdon, Coltheart, and Mackenzie. Journal of Experimental Social Psychology, 2009, 45, 581–584. [Google Scholar] [CrossRef]
- Greene, J. D., Nystrom, L. E., Engell, A. D., Darley, J. M., Cohen, J. D. (2004) The neural bases of cognitive conflict and control in moral judgment. Neuron, 2004, 44, 389–400. [CrossRef]
- Greene, J. D., Sommerville, R. B., Nystrom, L. E., Darley, J. M., & Cohen, J. D. (2001) An fMRI investigation of emotional engagement in moral judgment. Science, 2001, 293, 2105–2108.
- Bartels, D. M. (2008) Principled moral sentiment and the flexibility of moral judgment and decision making. Cognition, 2008, 108, 381–417. [Google Scholar] [CrossRef]
- Greene, J. D., Morelli, S. A., Lowenberg, K., Nystrom, L. E., & Cohen, J. D. (2008) Cognitive load selectively interferes with utilitarian moral judgment. Cognition, 2008, 107, 1144–1154.
- Kroneisen, M., & Steghaus, S. (2021) The influence of decision time on sensitivity for consequences, moral norms, and preferences for inaction: time, moral judgments, and the CNI model. Journal of Behavioral Decision Making, 2021, 34, 140–153.
- Li, Z., Xia, S., Wu, X., & Chen, Z. (2018) Analytical thinking style leads to more utilitarian moral judgments: An exploration with a process-dissociation approach. Personality and Individual Differences, 2018, 131.
- Moore, A. B., Clark, B. A., & Kane, M. J. (2008) Who shalt not kill? Individual differences in working memory capacity, executive control, and moral judgment. Psychological Science, 2008, 19, 549–557.
- Patil, I., Zucchelli, M. M., Kool, W., Campbell, S., Fornasier, F., Calo, M., Silani, G., Cikara, M., & Cushman, F. (2020) Reasoning supports utilitarian resolutions to moral dilemmas across diverse measures. Journal of Personality and Social Psychology, 2020, 120, 443–460.
- Frimer, J. A., & Walker, L. J. (2009) Reconciling the self and morality: An empirical model of moral centrality development. Developmental Psychology, 2009, 45, 1669–1681.
- Thompson, I. E., Melia, K. M., Boyd, K. M., & Horsburgh, D. Nursing Ethics; Elsevier Health Sciences: London, UK, 2006. [Google Scholar]
- Rosli, N. A., Sofian, H. N. H. M., Saiful, F. H. M., & Zolkefli, Y. Nurses’ perceptions of the responsibility of patients with diabetes mellitus: A vignetter study. The Malaysian Journal of Nursing (MJN), 2022, 13, 19–25.
- Kozlowski, D., Hutchinson, M., Hurley, J., Rowley, J., & Sutherland, J. The role of emotion in clinical decision making: an integrative literature review. BMC medical education, 2017, 17, 1–13.
- Melin-Johansson, C., Palmqvist, R., & Rönnberg, L. (2017) Clinical intuition in the nursing process and decision-making—A mixed-studies review. Journal of clinical nursing, 26, 3949.
- Edwards, S. Nursing ethics: a principle-based approach. Bloomsbury Publishing: London, UK, 2009.
- Pretz, J. E., & Folse, V. N. Nursing experience and preference for intuition in decision making. Journal of clinical nursing, 2011, 20(, 2889.
- Li, B., Li, Z., & Wan, Q. Effects of work practice environment, work engagement and work pressure on turnover intention among community health nurses: Mediated moderation model. Journal of advanced nursing, 2019, 75, 3485–3494.
- Cheraghi, R., Valizadeh, L., Zamanzadeh, V., Hassankhani, H., & Jafarzadeh, A. Clarification of ethical principle of the beneficence in nursing care: an integrative review. BMC nursing, 2023, 22, 1–9.
- Søvold, L. E., Naslund, J. A., Kousoulis, A. A., Saxena, S., Qoronfleh, M. W., Grobler, C., & Münter, L. Prioritizing the mental health and well-being of healthcare workers: an urgent global public health priority. Frontiers in public health, 2021, 9, 679397.
- Mael, F., & Ashforth, B. E. Alumni and their alma maters: A partial test of the reformulated model of organizational identification. Journal of Organizational Behavior, 1992, 13, 103–123.
- Lui, S. S., Ngo, H. Y., & Tsang, A. W. N. Inter-role conflict as a predictor of job satisfaction and propensity to leave: A study of professional accountant. Journal of Managerial Psychology, 2001, 16, 469–484.
- Hayes, A. F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Publications: New York, USA, 2013.
- Kohlberg, L. Stages of moral development. Moral education, 1971, 1, 23–92. [Google Scholar]
- DeCola, P. R., & Riggins, P. Nurses in the workplace: expectations and needs. International Nursing Review, 2010, 57, 335–342.
- Lloyd-Rees, J. How emergency nurse practitioners view their role within the emergency department: a qualitative study. International Emergency Nursing, 2016, 24, 46–53. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).