1. Introduction
Acetabular fractures are complex and require accurate preoperative identification to determine an optimal treatment plan due to the difficult surgical approach and most suitable fixation technique. Acetabular fractures are identified with the aid of the worldwide recognized Judet and Letournel classification system [
1,
2].
Although it seems old, this classification remains the most used in the identification of these fractures and CT-scan nowadays represents the gold standard for emergency room radiologic wards to assess the proper planning of these fractures [
3].
Before the advent of the CT scan, standard X-rays allowed us to visualize and understand the entity of lesions, fragmentations, and dislocations only during open surgery. Understanding the dislocation of fragments, the amount of displacement, and the joint involvement is necessary for a successful treatment. CT has proven to be superior to conventional X-rays in the evaluation of articular fractures, affording optimal anatomical assessment in the axial, coronal, and sagittal planes [
4].
These two-dimensional (2D) imaging modalities are used to interpret acetabular fractures. However, the complex three-dimensional (3D) geometry and relatively low incidence of these fractures can make it difficult for residents to become adept at correctly identifying acetabular fractures [
5].
New horizons have been explored with the birth of 3D technology. 3DP models for orthopedic conditions can generate accurate reproductions of anatomical structures, with faithful representations of both normal and pathologic variations. Some current surgical applications of 3DP [
6] include preoperative templating, deformity correction planning, custom prostheses printing, use for patients, and trainee education [
7].
It has been demonstrated that the use of 3D-CT imaging significantly improved resident accuracy in acetabular fracture identification. Also, it has been observed an improvement from fair to moderate interobserver agreement when residents used 2D versus 3D CT images to identify acetabular fractures [
8]. On the other hand, the current COVID-19 pandemic has improved the use of AR technology [
9].
Different from virtual reality, AR technology provides a computer-generated overlay onto real-world surfaces, providing depth perception and stereoscopic visualization to the user [
10,
11].
AR has also benefited from recent advancements in handheld smartphone and tablet devices, which not only improve the power of such programs but also expand their accessibility out of traditional learning spaces and into the hands of the learner [
12,
13]. AR is a rapidly developing technology. Due to its flexibility in integrating physical and virtual environments, AR-based programs are increasingly used in education, including medical education and training. The use of this technology provides various means of delivering learning content and enhancing students’ experiences, diagnosis, and surgical planning.
The purpose of this study is to evaluate the accuracy between the new diagnostic technologies: AR and 3DP and to compare these to the gold standard CT scan in the classification of acetabular fractures among orthopedic residents. The secondary outcome was to investigate the confidence levels and the differences based on years of experience.
Approval was obtained from the ethics committee of our university. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
2. Materials and Methods
2.1. Patients
20 Orthopedic residents of our department have been selected and divided by the year of the course.
First and Second Post-graduate year residents were grouped in the Junior (JUN) Group, and third, fourth, and fifth-post-graduate residents were grouped in the Senior (SEN) Group. Fractures of the acetabulum of patients admitted to our unit from 2015 to 2021 have been included in the study, the inclusion criteria were: associated fracture of acetabulum according to Letournel classification, no associated or pathological fracture ( osteoporotic bone, tumor, metabolic syndrome). Informed consent was obtained from all individual participants included in the study.
2.2. Methods
For each acetabular fracture enrolled in the study it was collected:
- -
- CT scans (1mm layer thickness, 1 mm layer interval, and a voltage of 120 kV)
- -
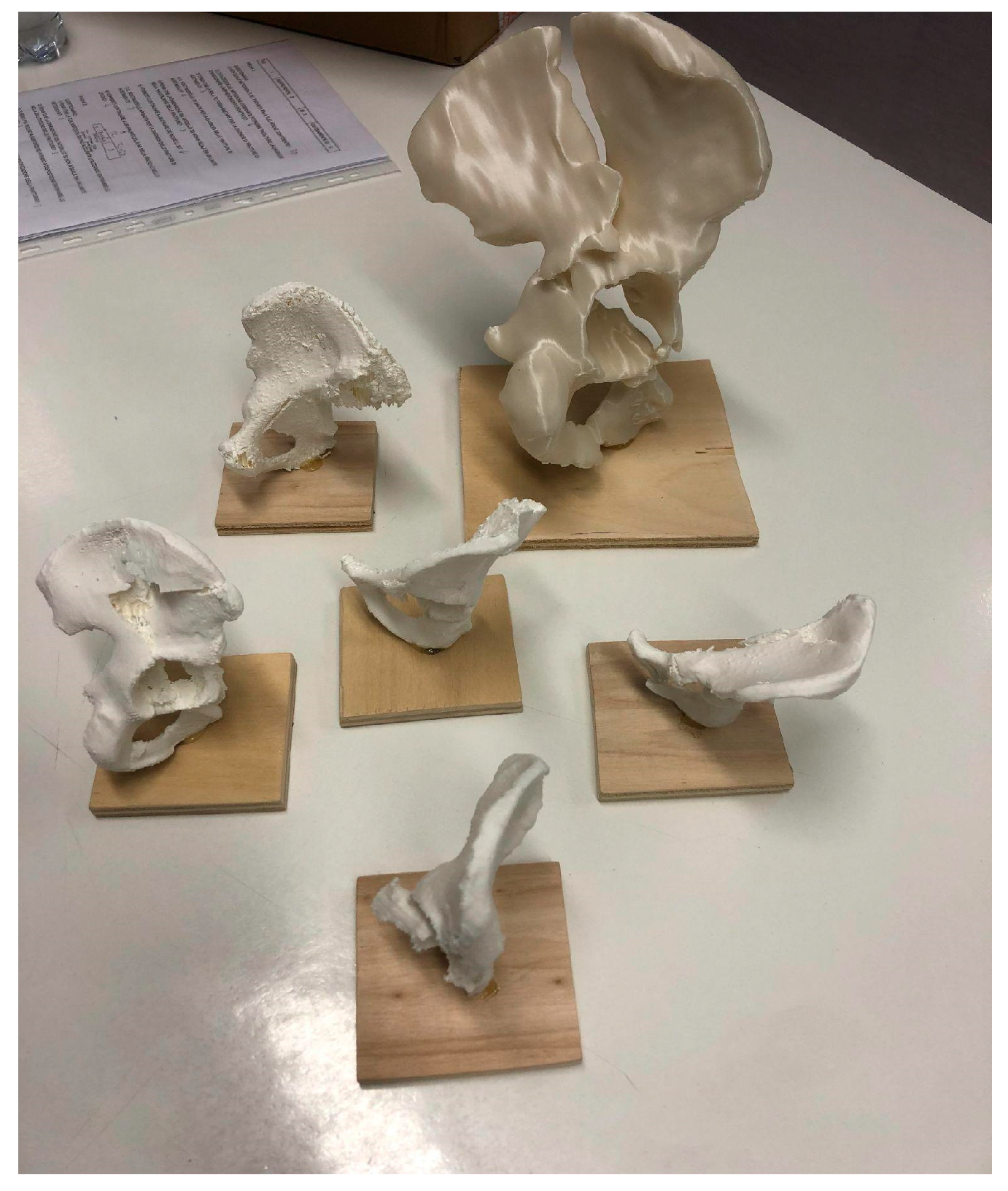
- 3DP models obtained from DICOM file using 3D planning software ( Mimics-Materialise, Meshmixer, Cura) with the use of segmentation applying the “region growing” function to separate the bones and soft tissues, define the fracture fragments and build a hemipelvis digital model for each fracture that was printed in PLA (scale 1:2) using a high precision 3D printer (Ultimaker © 2+ extended )
- -
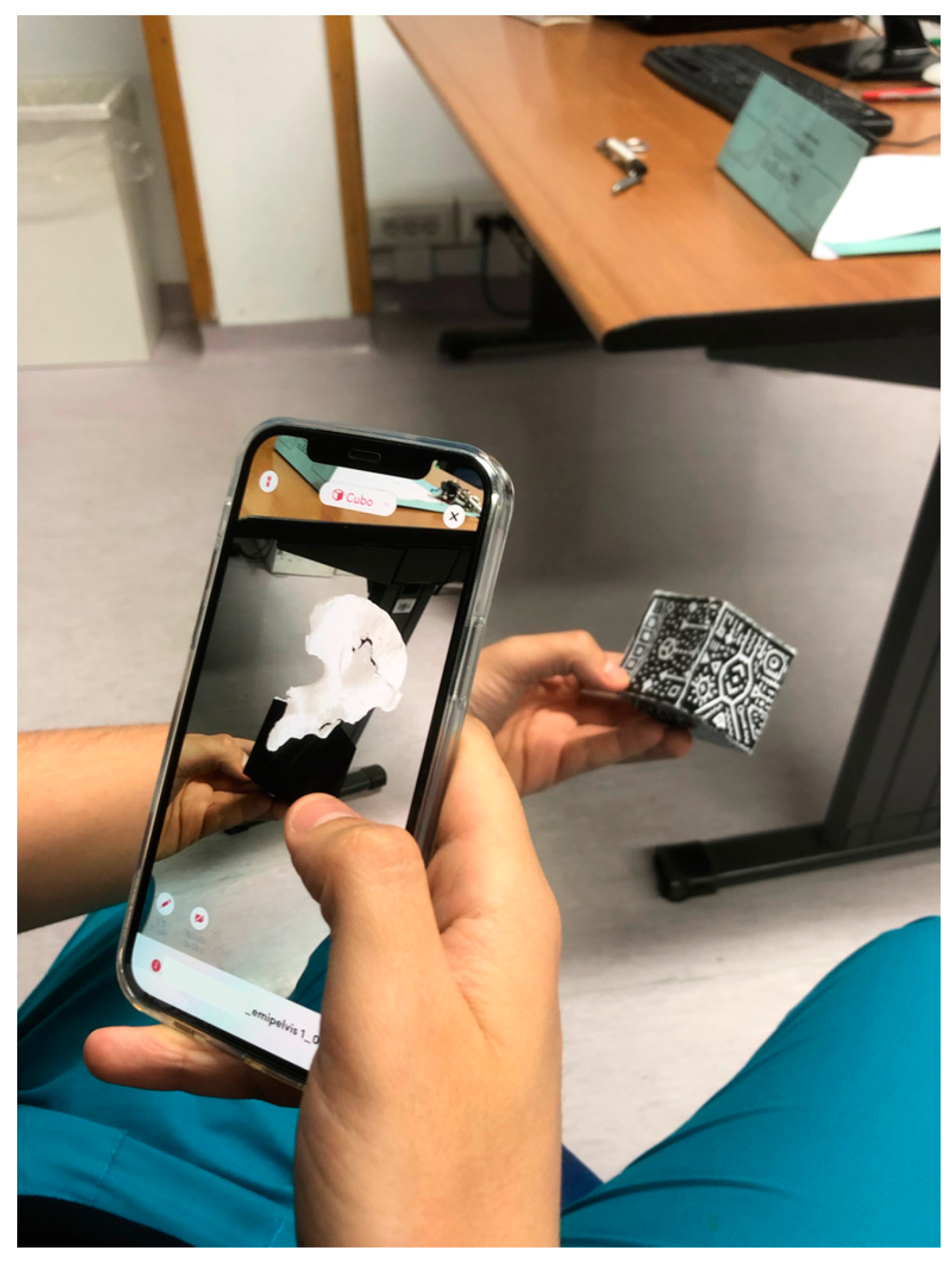
- 3D digital rendered model (format .stl) displayed in AR with a tablet screen using Object viewer App (by Merge EDU ©)
Figure 1.
2.3. Methods of Assessment
Associated acetabulum fractures were properly classified by three Senior surgeons specialized in Pelvic Trauma with an over-ten-year experience according to Letournel classification. The final assessment of the type of fracture was done in open surgery for treatment. Simple Acetabulum fractures were excluded from this study.
In double-blind, each resident was interviewed with a questionnaire to classify every fracture for each proposed method. A web-based questionnaire for each resident was done in which we collected:
- -
- numeric fracture classification according to Letournel classification ( 1: anterior wall, 2: anterior column, 3: transverse, 4: posterior wall, 5: posterior column, 6: posterior wall + posterior column, 7: anterior column + posterior hemitransverse, 8: T-shaped, 9: transverse + posterior wall, 10: both column)
- -
- time to collect a correct answer
- -
- six likert scale survey questions about confidence level perceived in a different kind of diagnostic method
From these data, we calculated the diagnostic accuracy (DA as a percentage of correct answers), the response time calculated only for the correct answer (RT), and the confidence (C) sorted by: groups, overall and diagnostic method.
Before starting the questionnaire, each resident was briefly presented with a diagram of acetabulum fractures sorted by number, and then a short course on how to read a 3D object from the augmented reality application was provided.
No one resident enrolled in the test had previously familiarity with 3D printing and Augmented reality technology.
2.4. Statistical Analysis
Data were processed statistically using mean, standard deviation, minimum, and maximum, Fisher exact test, t-student (significance p< 0.05), and Fleiss e Kappa guidelines for inter and intra-observer reliability (R) between methods and groups. All data were processed and graphs ( BoxPlot, Histograms ) were made using Microsoft Excel and SPSS software.
3. Results
20 trainees from each year of the residency program of our school were selected and enrolled in the study (5 from PGY-1, 2 from PGY-2, 3 from PGY-3, 4 from PGY-4, and 3 from PGY-5).
The mean age was 28,6 years (+-2,3), with an M:F ratio of 17:3. They were divided into JUN (n=10) and SEN ( n=10) groups. 5 associated fractures of the acetabulum (according to the Letournel classification) were included, collecting CT-scan, 3D printed (3DP) model (
Figure 2.), and augmented reality (AR) model. Results were collected using the questionnaire above.
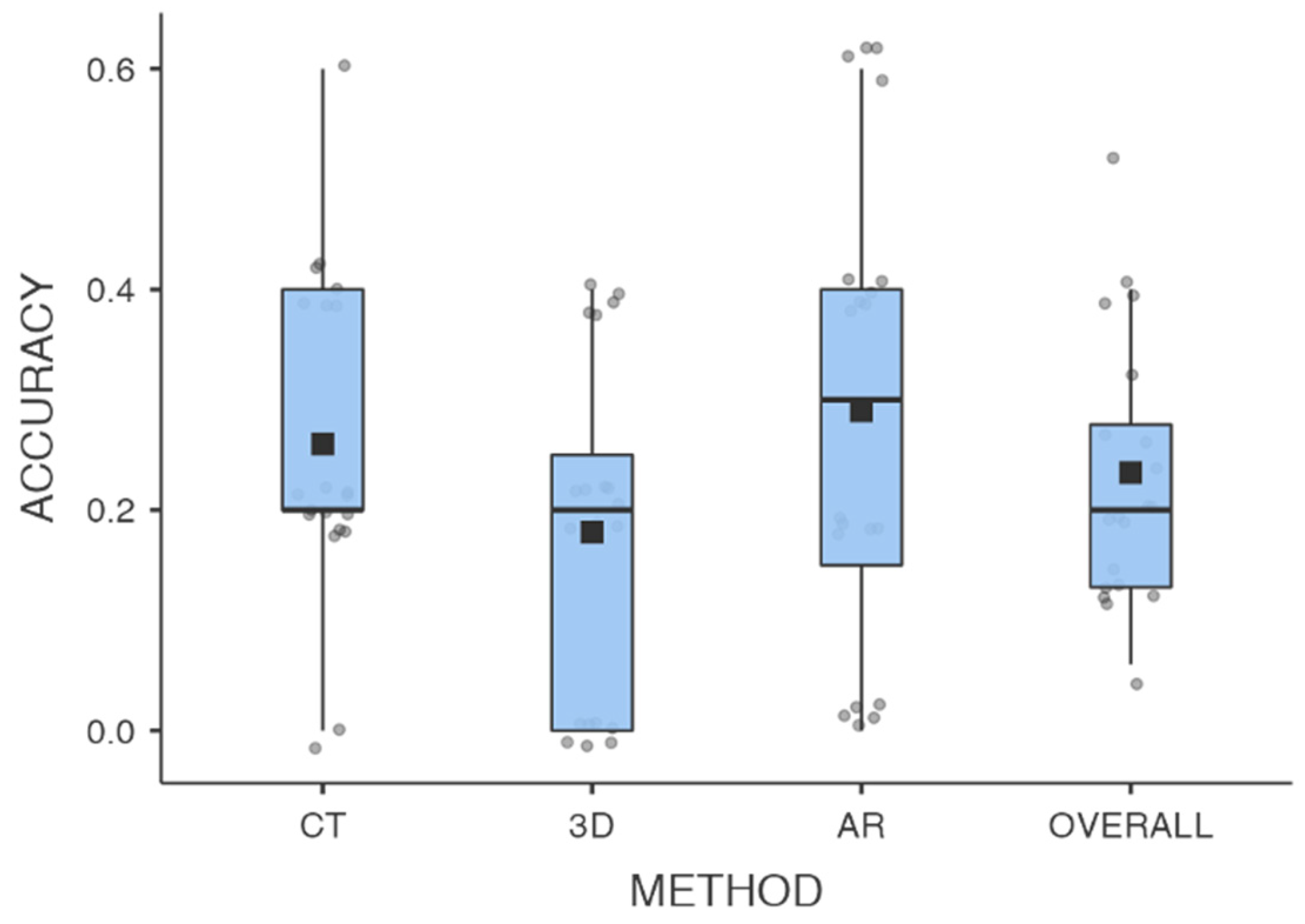
DA means between diagnostic methods resulted in 26% (+- 0.14) for CT, 18% (+-0.15) for 3DP, 29% (+- 0.30) for AR, and 23% ( +-0.20) Overall.
CT-DA resulted to be higher than 3DP-PA (p=0.05), AR-DA resulted to be superior to 3DP-DA (p=0,04), and no statistically significant difference was found between CT-DA and AR-DA ( p=0.645).Tab.1.
DA between group JUN and SEN resulted respectively for methods: in CT JUN-DA 20%(+- 0.09) and SEN-DA 32% (+- 0.17) (p=0.05); in 3DP, JUN-DA 12% (+-0.17) and SEN-DA 24% (+-0.13)(p=0.08); in AR JUN-DA 28% (+-0.21) and SEN-DA 30% (+- 0.23)(p=0.845); Overall JUN-DA was 17,8% (+-0.09) and SEN-DA 29% (+-0.13) (p=0.033). Tab.2.
Overall RT to obtain the correct answer was 61.2 sec (±24,6) for CT, 35.8 sec (±20,1) for 3DP, and 46,7 sec (±20,8) for AR.
RT between group JUN and SEN resulted respectively for methods: in CT JUN-RT was 48,1 sec (+- 24.5) and SEN-RT 69,5 sec (+- 21,6) (p=0.07); in 3DP, JUN-RT was 39 sec(+-0.17) and SEN-RT 34,3 sec (+21.9)(p=0.717); in AR JUN-RT was 46.5 sec (+-23.4) and SEN-RT 46.9 (+-19.2)(p=0.958).
Overall intra and inter-observer R was fairly poor between methods and group of residents ( JUN k= 0,06, SEN k=0.09).
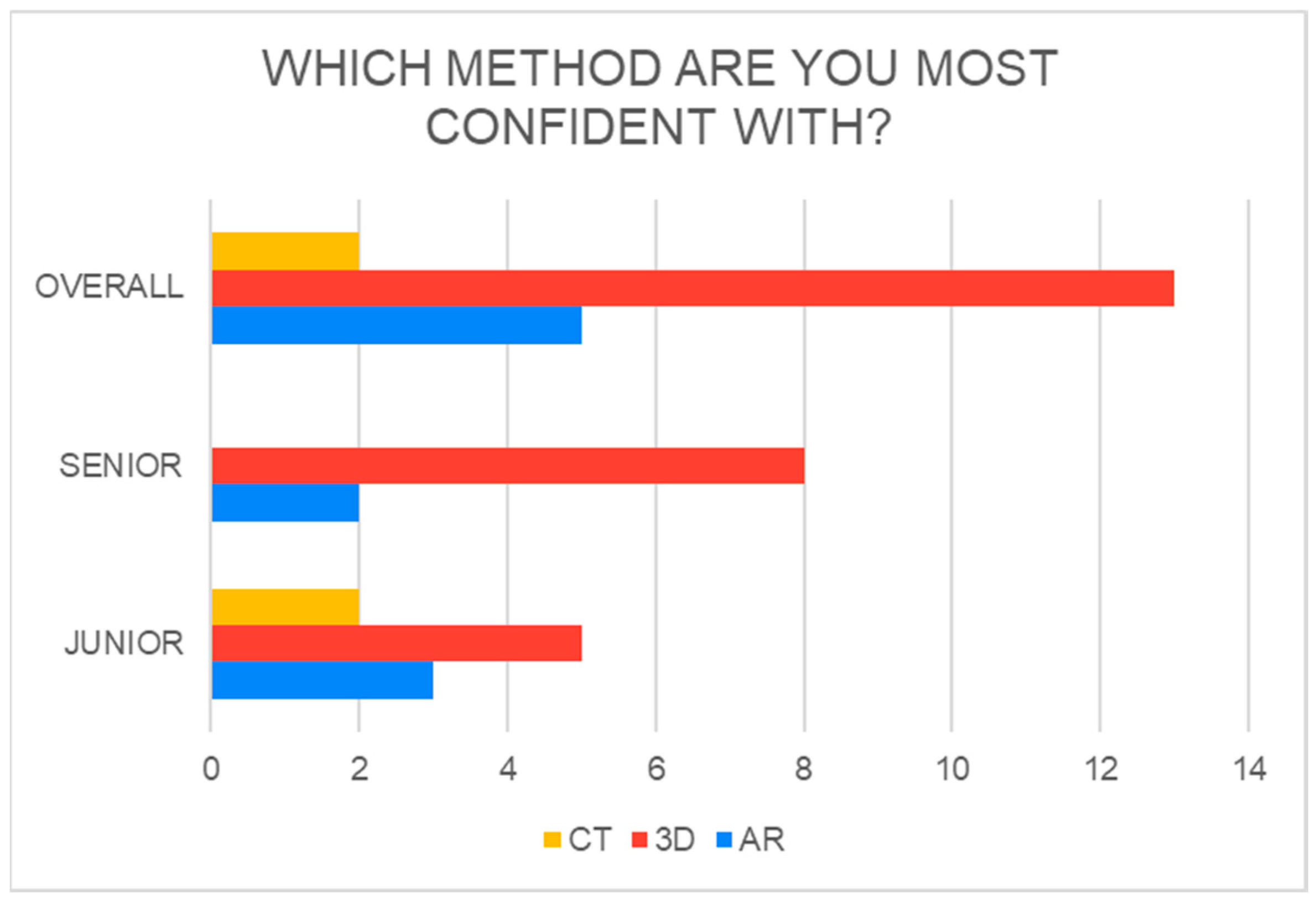
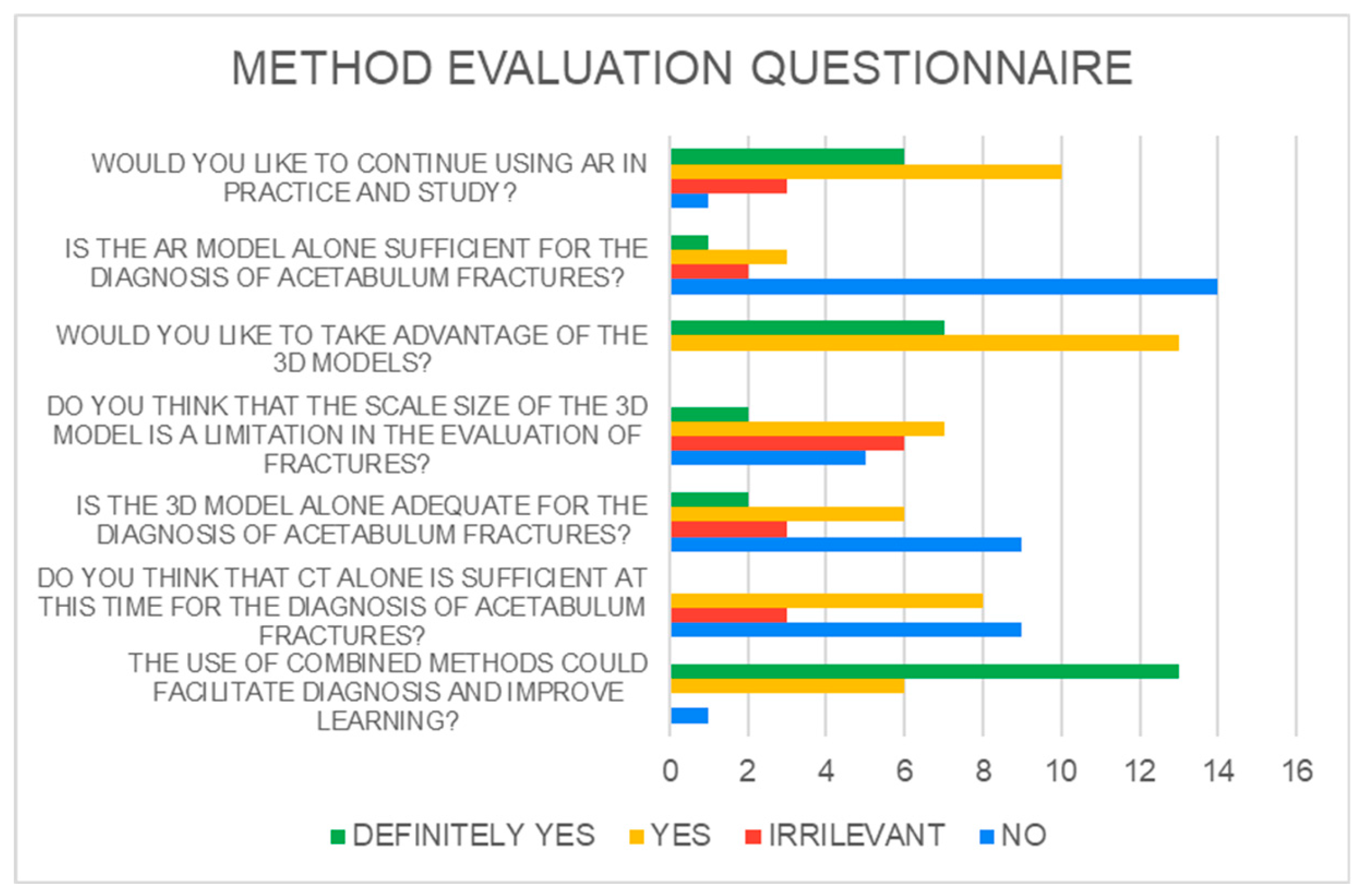
3DP models resulted to have superior overall C (65%) even if the residents answered that AR and 3DP alone are not enough to make the diagnosis ( results are shown in Histograms ,
Figure 3 and
Figure 4).
Table 1.
General DA differences between methods.
Table 1.
General DA differences between methods.
ACCURACY
DIFFERENCE |
Mean difference |
t-test |
p |
| TC vs AR |
-0.30 |
-0.508ᵃ |
0.614 |
| TC vs 3DP |
0.80 |
1.66 |
0.052 |
| 3DP vs AR |
0.120 |
2.04 |
0.048 |
Table 2.
DA differences between JUN and SEN groups.
Table 2.
DA differences between JUN and SEN groups.
| |
Group |
Mean |
SD |
t-test |
p |
CT ACCURACY
|
JUNIOR |
0.200 |
0.0943 |
-1.964ᵃ |
0.050 |
| SENIOR |
0.320 |
0.169 |
|
|
3D accuracy |
JUNIOR |
0.120 |
0.1687 |
-1.800 |
0.089 |
| SENIOR |
0.240 |
0.126 |
|
|
AR accuracy |
JUNIOR |
0.280 |
0.2150 |
-0.198 |
0.845 |
| SENIOR |
0.300 |
0.236 |
|
|
OVERALL accuracy
|
JUNIOR |
0.178 |
0.0909 |
-2.267 |
0.036 |
| SENIOR |
0.290 |
0.127 |
|
|
4. Discussion
CT imaging has proven to be superior to conventional X-rays in the evaluation of complex articular fractures, allowing one to understand the entity of lesions, the fragmentations, and the dislocations, affording optimal anatomical assessment in the axial, coronal, and sagittal planes [
14]. 3D volume rendering from CT led to better accuracy and it rendered the acetabular fracture diagnosis more repeatable and faster [
15]. The need to improve the “letournel accuracy” in residents with new diagnostic methods is an important topic in the literature [
16], using a different method for teaching (3D models, algorithms)[
17,
18,
19,
20,
21].
The advent of new technologies, 3DP and AR, or e-learning as well, in the last year, has increasingly gained importance in student learning and practice [
4,
22]. The incorporation of 3D models has been shown to be useful for resident education in surgical specialties such as neurological, thoracic, plastic, and general surgery [
5,
23]. Three-dimensional volume rendering reconstruction helps visualize the sense of spatial anatomy and likewise pathology.
Several orthopedics papers in the last years’ literature [
7,
24,
25,
26]demonstrated the effectiveness of using 3D printed models in the trauma field of large joint fractures such as tibial plateau and acetabulum, where the use of pre-formed plates and planned cutting masks used in the operating room makes a difference in outcomes.
Conversely to Lim et al. [
5], as well as Montgomery et al. [
27] we properly choose 5 acetabular complex fracture patterns, thinking that 2dCT could be adequate in the classification of the other types.
Lim et al. in their study demonstrate an improved resident accuracy in acetabular fracture identification with the use of 3D models compared to XR. When comparing 3D models to CTs, the participants obtained similar accuracy with each modality, and both were significantly superior to XRs. However, there was no significant difference between CT and 3D models.
In our study, we compared the use of CT, the 3DP model, and the AR model. To our knowledge, no study has evaluated the importance of AR technologies compared to 3D or CT in the diagnostic evaluation and classification of fracture patterns before.
Contrary to Lim et al. [
5] when comparing 3D models to CTs, the participants obtained different accuracy with each modality. 3DP models showed less accuracy in the classification of acetabular fracture, maybe due to the fact that staff could downgrade the severity of fracture classification. We maybe blame this problem on the difficult reproduction or interpretation of the details of the more complex fracture rhymes the 3DP model cannot reproduce every time [
28].
Despite this result, senior and junior residents agreed that they felt more confident and comfortable with 3D models. The addition of a 3Dp model had no proven benefit for residents in their final year of training.
This fact can be associated with a better approach and 3D-tactile proprioception with the object and so the tridimensional complexity of the fracture.
The overall accuracy of the surgeons in training remains different among groups, especially in this kind of fracture, Senior residents with more experience in orthopedics resulted to have higher overall DA.
Our study shows that AR seems to be successful as a CT scan method in diagnostic accuracy.
Figure 5.
Junior residents resulted to have better accuracy using AR and this method succeeds in eliminating the JUN-SEN group’s differences in accuracy in the recognition of these fractures. This is the most effective and statistically demonstrated the result of this study. However, the fastest method, albeit less accurate, seems to be 3DP.
Differently from the literature [
29,
30], Letournel’s classification in residency still has a poor interobserver agreement ( k<0.100), and our study did not find an improvement in reliability using these new technologies.
A study by Matta et al.[
30] assessed good reliability for this classification only for senior surgeons who have been taught how to interpret the images and who regularly treat acetabular fractures.
Subjectively, 65% of the residents agreed or strongly agreed that they felt confident identifying acetabular fractures before interacting with the 3DP models. However, over 95% agreed or strongly agreed that exposure to the 3D models combined with the AR improved their confidence in fracture identification. This result is due to their absence of experience or exposure to the new method. Participants also indicated that the visual appearance of the models was an accurate representation of the fractures, but the size was the real limit. Furthermore, 80% of respondents stated that they either agreed or strongly agreed that they would like to continue using 3D models in other areas of their education. Overall, the subjective data supports the notion that 3D models are perceived as a positive addition to orthopedic resident training. AR seems to be the most intuitive method. Some works argue for the use of both technologies AR and VR in orthopedic trauma surgery, highlighting specifically the combination of AR with 3Dp direct empirical comparison of the technologies is already done [
31]. More studies should be done, making augmented reality, both with 3DP technology, an increasingly used tool in learning, diagnostics, and pre-operative planning.
Talking about limits, the cohort of Fractures included in the study will be improved in future research, although the measures obtained between methods were statistically valid to assess results.1:2 Scale model may have affected the correct visualization in the observers from a real-size model perception but the declared detail of the fracture rhymes remains the same for the accuracy of the printer used for the study models.Certainly more investigations and studies need to be carried out on a large scale to introduce augmented reality technology to difficult everyday joint trauma, considering the demonstrated benefit in faster and more accurate identification of the most complex fracture patterns.
5. Conclusions
This study demonstrated that AR diagnostic accuracy in acetabulum fractures resulted to be similar to CT and superior to 3DP models. It represents a novel technology that evens out the differences based on experienced surgeons. AR and 3DP technology must not be the alternative solution to the CT gold standard for the diagnosis of complex joint fractures but can be a better tool for learning and managing fractures in the future of Orthopedics.
Author Contributions
Conceptualization, M.M.; methodology, G. Pu.; software, E.M.; validation, G.T.; formal analysis, F.M.C.P..; investigation, G. Pa.; resources, M.M.; data curation, M.M.; writing—original draft preparation, M.M.; writing—review and editing, G.T.; visualization, V.P.; supervision, V.P.; project administration, V.P.; funding acquisition, V.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available in the tables of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- JUDET R, JUDET J, LETOURNEL E. LES FRACTURES DU COTYLE [FRACTURES OF THE ACETABULUM]. Acta Orthop Belg. 1964;30:285-293. In.
- Cimerman, M.; Kristan, A.; Jug, M.; Tomaževič, M. Fractures of the Acetabulum: From Yesterday to Tomorrow. International Orthopaedics (SICOT) 2021, 45, 1057–1064. [CrossRef]
- Tile, M. Fractures of the Acetabulum. Orthop Clin North Am 1980, 11, 481–506.
- Bizzotto, N.; Sandri, A.; Regis, D.; Romani, D.; Tami, I.; Magnan, B. Three-Dimensional Printing of Bone Fractures: A New Tangible Realistic Way for Preoperative Planning and Education. Surg Innov 2015, 22, 548–551. [CrossRef]
- Lim, P.K.; Stephenson, G.S.; Keown, T.W.; Byrne, C.; Lin, C.C.; Marecek, G.S.; Scolaro, J.A. Use of 3D Printed Models in Resident Education for the Classification of Acetabulum Fractures. Journal of Surgical Education 2018, 75, 1679–1684. [CrossRef]
- Baskaran, V.; Štrkalj, G.; Štrkalj, M.; Di Ieva, A. Current Applications and Future Perspectives of the Use of 3D Printing in Anatomical Training and Neurosurgery. Front. Neuroanat. 2016, 10. [CrossRef]
- Meyer-Szary, J.; Luis, M.S.; Mikulski, S.; Patel, A.; Schulz, F.; Tretiakow, D.; Fercho, J.; Jaguszewska, K.; Frankiewicz, M.; Pawłowska, E.; et al. The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals—Cross-Sectional Multispecialty Review. IJERPH 2022, 19, 3331. [CrossRef]
- Garrett, J.; Halvorson, J.; Carroll, E.; Webb, L.X. Value of 3-D CT in Classifying Acetabular Fractures During Orthopedic Residency Training. Orthopedics 2012, 35. [CrossRef]
- Salta, K.; Paschalidou, K.; Tsetseri, M.; Koulougliotis, D. Shift From a Traditional to a Distance Learning Environment during the COVID-19 Pandemic: University Students’ Engagement and Interactions. Sci & Educ 2022, 31, 93–122. [CrossRef]
- Jud, L.; Fotouhi, J.; Andronic, O.; Aichmair, A.; Osgood, G.; Navab, N.; Farshad, M. Applicability of Augmented Reality in Orthopedic Surgery – A Systematic Review. BMC Musculoskelet Disord 2020, 21, 103. [CrossRef]
- Verhey, J.T.; Haglin, J.M.; Verhey, E.M.; Hartigan, D.E. Virtual, Augmented, and Mixed Reality Applications in Orthopedic Surgery. Int J Med Robot 2020, 16. [CrossRef]
- Moro, C.; Štromberga, Z.; Raikos, A.; Stirling, A. The Effectiveness of Virtual and Augmented Reality in Health Sciences and Medical Anatomy: VR and AR in Health Sciences and Medical Anatomy. American Association of Anatomists 2017, 10, 549–559. [CrossRef]
- Dhar, P.; Rocks, T.; Samarasinghe, R.M.; Stephenson, G.; Smith, C. Augmented Reality in Medical Education: Students’ Experiences and Learning Outcomes. Medical Education Online 2021, 26, 1953953. [CrossRef]
- Puglisi, G.; Montemagno, M.; Denaro, R.; Condorelli, G.; Caruso, V.F.; Vescio, A.; Testa, G.; Pavone, V. 3D-Printed Models versus CT Scan and X-Rays Imaging in the Diagnostic Evaluation of Proximal Humerus Fractures: A Triple-Blind Interobserver Reliability Comparison Study. Advances in Orthopedics 2022, 2022, 1–7. [CrossRef]
- Sebaaly, A.; Riouallon, G.; Zaraa, M.; Upex, P.; Marteau, V.; Jouffroy, P. Standardized Three Dimensional Computerised Tomography Scanner Reconstructions Increase the Accuracy of Acetabular Fracture Classification. International Orthopaedics (SICOT) 2018, 42, 1957–1965. [CrossRef]
- Butler, B.A.; Lawton, C.D.; Hashmi, S.Z.; Stover, M.D. The Relevance of the Judet and Letournel Acetabular Fracture Classification System in the Modern Era: A Review. Journal of Orthopaedic Trauma 2019, 33, S3–S7. [CrossRef]
- Goyal, S.; Chua, C.; Chen, Y.; Murphy, D.; O.’Neill, G. Utility of 3D Printed Models as Adjunct in Acetabular Fracture Teaching for Orthopaedic Trainees. BMC Med Educ 2022, 22, 595. [CrossRef]
- Hurson, C.; Tansey, A.; O’Donnchadha, B.; Nicholson, P.; Rice, J.; McElwain, J. Rapid Prototyping in the Assessment, Classification and Preoperative Planning of Acetabular Fractures. Injury 2007, 38, 1158–1162. [CrossRef]
- Prevezas, N.; Antypas, G.; Louverdis, D.; Konstas, A.; Papasotiriou, A.; Sbonias, G. Proposed Guidelines for Increasing the Reliability and Validity of Letournel Classification System. Injury 2009, 40, 1098–1103. [CrossRef]
- Brandser, E.; Marsh, J.L. Acetabular Fractures: Easier Classification with a Systematic Approach. American Journal of Roentgenology 1998, 171, 1217–1228. [CrossRef]
- Hansen, E.; Marmor, M.; Matityahu, A. Impact of a Three-Dimensional “Hands-On” Anatomic Teaching Module on Acetabular Fracture Pattern Recognition by Orthopaedic Residents. Journal of Bone and Joint Surgery 2012, 94, e177. [CrossRef]
- Boboc, R.G.; Băutu, E.; Gîrbacia, F.; Popovici, N.; Popovici, D.-M. Augmented Reality in Cultural Heritage: An Overview of the Last Decade of Applications. Applied Sciences 2022, 12, 9859. [CrossRef]
- Kong, X.; Nie, L.; Zhang, H.; Wang, Z.; Ye, Q.; Tang, L.; Li, J.; Huang, W. Do Three-Dimensional Visualization and Three-Dimensional Printing Improve Hepatic Segment Anatomy Teaching? A Randomized Controlled Study. Journal of Surgical Education 2016, 73, 264–269. [CrossRef]
- Assink, N.; Reininga, I.H.F.; ten Duis, K.; Doornberg, J.N.; Hoekstra, H.; Kraeima, J.; Witjes, M.J.H.; de Vries, J.-P.P.M.; IJpma, F.F.A. Does 3D-Assisted Surgery of Tibial Plateau Fractures Improve Surgical and Patient Outcome? A Systematic Review of 1074 Patients. Eur J Trauma Emerg Surg 2022, 48, 1737–1749. [CrossRef]
- Alemayehu, D.G.; Zhang, Z.; Tahir, E.; Gateau, D.; Zhang, D.-F.; Ma, X. Preoperative Planning Using 3D Printing Technology in Orthopedic Surgery. BioMed Research International 2021, 2021, 1–9. [CrossRef]
- Ejnisman, L.; Gobbato, B.; de França Camargo, A.F.; Zancul, E. Three-Dimensional Printing in Orthopedics: From the Basics to Surgical Applications. Curr Rev Musculoskelet Med 2021, 14, 1–8. [CrossRef]
- Montgomery, S.J.; Kooner, S.S.; Ludwig, T.E.; Schneider, P.S. Impact of 3D Printed Calcaneal Models on Fracture Understanding and Confidence in Orthopedic Surgery Residents. Journal of Surgical Education 2020, 77, 472–478. [CrossRef]
- Samaila, E.M.; Negri, S.; Zardini, A.; Bizzotto, N.; Maluta, T.; Rossignoli, C.; Magnan, B. Value of Three-Dimensional Printing of Fractures in Orthopaedic Trauma Surgery. J Int Med Res 2020, 48, 300060519887299. [CrossRef]
- Keltz, E.; Keshet, D.; Peled, E.; Zvi, Y.; Norman, D.; Keren, Y. Interobserver and Intraobserver Agreement for Letournel Acetabular Fracture Classification System Using 3-Dimensional Printed Solid Models. WJO 2021, 12, 82–93. [CrossRef]
- Beaulé, P.E.; Dorey, F.J.; Matta, J.M. Letournel Classification for Acetabular Fractures. Assessment of Interobserver and Intraobserver Reliability. J Bone Joint Surg Am 2003, 85, 1704–1709.
- Negrillo-Cárdenas, J.; Jiménez-Pérez, J.-R.; Feito, F.R. The Role of Virtual and Augmented Reality in Orthopedic Trauma Surgery: From Diagnosis to Rehabilitation. Computer Methods and Programs in Biomedicine 2020, 191, 105407. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).