1. Introduction
Radiculopathy is a dysfunction of a spinal nerve root that can cause pain, weakness, sensory disturbances, and/or decreased myotatic reflexes in a specific anatomical territory corresponding to the level of the affected root [
1,
2,
3,
4,
5]. When the involved roots correspond to the lumbar and/or sacral spinal nerves, the term ‘lumbosacral radiculopathy’ or ‘lumbosacral radicular syndrome’ is commonly used [
6,
7]. The etiology by which a lumbosacral root can become affected is often related to mechanical and/or chemical phenomena [
2,
8,
9,
10]. Mechanical injury to the nerve root can occur due to compression, traction, or frictional forces. Chemical irritation may occur in response to ischemia of the nerve root, vascular stasis, or exposure of the root to inflammatory components released during tissue injury [
8,
11,
12]. The prevalence of this pathology ranges from 1 to 5% of the general population [
7,
13,
14].
The diagnosis of radiculopathy requires correlation of the results from different components of the evaluation process [
11,
13]. Imaging diagnosis, typically magnetic resonance imaging (MRI), and electrodiagnostic tests (EDX) are the two most commonly used reference tests to confirm nerve root damage [
10,
11,
13,
15].
The current diagnostic paradigm is overly mechanistic, focusing on structural damage that confirms disc herniation or degeneration of the structures housing the spinal cord and roots—the two major causes of radiculopathy—[
1,
5,
9,
16,
17,
18]. This perspective results in MRI carrying significant weight in the diagnostic process. However, radiculopathy is a condition that affects the physiology of the nerve root, which may not necessarily be solely of compressive etiology [
8,
19]. Therefore, EDX—which allows for the physiological assessment of the root and detects alterations in function—is another essential test [
20,
21,
22,
23,
24].
EDX exhibits high diagnostic accuracy when neurological symptoms have been present for at least three weeks, with a very low percentage of false positives. However, it can yield false negatives under circumstances of minimal demyelinating lesions, involvement of very small fibers, or selective dorsal root involvement [
21]. Although the accuracy of MRI in detecting structural abnormalities is well-established, the relationship between these detected anatomical anomalies and the signs and symptoms of patients remains controversial [
4,
10,
25,
26]. In one-third of patients diagnosed with radicular pain syndrome, no radicular compression is observed on MRI [
6,
19].
Some studies published to date coincide in reporting a low level of agreement between both reference tests [
23,
27,
28,
29]. While some of these studies analyze EDX only in patients considered positive on MRI [
23], include both cervical and lumbar radiculopathies [
27,
28] or consider back pain alone as sufficient clinical suspicion [
30]. In patients with a clear clinical presentation and imaging evidence of mechanical compression, a good level of agreement is presumable. However, in undiagnosed patients with clinical suspicion, what level of correlation could we expect between both diagnostic tests?
The aim of this study was to analyze the degree of agreement between the two most commonly used reference tests in the diagnosis of lumbosacral radiculopathy in patients with clinical suspicion of the pathology and to compare them with other clinical variables and scales.
2. Materials and Methods
A prospective epidemiological study of consecutive observational, descriptive, cross-sectional, and double-blind cases was designed. The design and execution of the study followed the guidelines of the STROBE [
31,
32] (Strengthening the Reporting of Observational Studies in Epidemiology) guide for the reporting of observational studies.
The study population focused on patients referred to the Clinical Neurophysiology Service of the University Clinical Hospital “Lozano Blesa” in Zaragoza due to suspicion of lumbosacral radiculopathy, to undergo EDX study —electromyography (EMG) and electroneurography (ENG)— for diagnostic confirmation.
The sample size calculation considered an approximate prevalence of 50% of the pathology in the study population, a 95% confidence interval, and a margin of error of 10% for similar values of sensitivity and specificity between 75% and 80%, resulting in a sample size of 142 patients [
33].
A consecutive sampling method was applied to select patients referred for an EDX (EMG-ENG) study due to clinical suspicion of lumbosacral radiculopathy over a period of two years. Patients were informed about the study and provided consent for participation before inclusion. Inclusion criteria were as follows: patients aged between 18 and 80 years [
34] presenting symptoms consistent with lumbosacral radiculopathy for more than 3 weeks at the time of the study —intermittent or constant pain in the lumbar area or radiating to a distal extremity, to the gluteal fold; or distribution of pain according to a dermatomal pattern or weakness according to a myotomal pattern of some lumbosacral nerve root— [
35,
36] and having sufficient understanding and communicative capacity to communicate their symptoms, as well as their characteristics [
37]. The main exclusion criteria for participation were: any diagnosis of type I diabetes mellitus, unregulated thyroid dysfunctions, rheumatoid arthritis, serious heart and/or lung diseases, herpes zoster infection, multiple sclerosis, hereditary neuropathy, known pregnancy, and/or serious systemic or autoimmune diseases [
35,
37,
38,
39,
40], as well as having undergone lumbar spine surgery or suffered fractures in the lumbar spine in the last year [
37].
Among the patients who met the selection criteria, data collection from the medical history was conducted. Demographic variables and information related to the pathology were recorded during the initial assessment. Additionally, patients completed the Oswestry Disability Index (ODI) scale [
41], the Neuropathic Pain Diagnostic Questionnaire (DN4) [
42], and the Visual Analog Scale (VAS) [
43,
44] to assess their current pain, with values recorded in writing. Subsequently, upon completion of the entire evaluation process and with the patient’s signed consent, the lumbar MRI report for each patient was obtained.
The EDX included EMG and ENG. EMG was performed using a concentric needle electrode. The ‘H’ reflex was also recorded, and ENG was utilized to exclude other diseases and confirm the diagnosis. The algorithm established by the American Association of Electrodiagnostic & Neuromuscular Medicine (AANEM) was followed to perform the EDX as outlined in the main manuals [
21], which involves exploring the innervated muscles at the segmental level corresponding to the suspicion of radiculopathy. Muscle electrical activity was recorded at rest, during movement, and with submaximal effort. Pathological EMG findings included positive sharp waves, fibrillation potentials, complex repetitive discharges, high amplitudes, broad duration, increased polyphasic motor units, or reduced neuropathic recruitment [
21,
45]. Additional muscles with the same segmental innervation were studied to confirm the diagnosis if abnormalities were detected in one of the initially examined muscles. Additionally, the study was completed with ENG to determine if this abnormality was due to mononeuropathy. If none of the muscles exhibited abnormal findings, radiculopathy was ruled out [
46].
The diagnosis of radiculopathy was considered positive when pathological findings were observed in at least 2 muscles sharing a common nerve root but originating from different peripheral nerves, and/or when the ‘H’ reflex was positive with abolished or attenuated response for S1 root [
21,
47,
48].
Regarding the lumbar MRI reports, variables related to vertebral body degeneration, presence of osteophytes, spondylolisthesis, arthropathies, facet hypertrophy, foraminal stenosis, and different levels of disc degeneration (bulges, protrusions, extrusions) were recorded, with radiculopathy noted when the report explicitly referenced root involvement in any of these circumstances, following the main guidelines [
49,
50,
51,
52,
53].
The statistical analysis of all variables was conducted using IBM
® SPSS
® Statistics 21. A confidence level of 95% was established for the analysis of the results and statistical inference. Descriptive statistics were presented as mean and standard deviation for continuous variables and frequencies for categorical variables. Comparisons of quantitative variables with MRI and EDX were conducted using the Mann-Whitney U test as a non-parametric test and the Student’s t-test with Levene’s test for parametric analysis. The association between EDX findings, and MRI findings was examined using the Chi-Squared test, with a p-value of <0.05 considered significant [
54].
3. Results
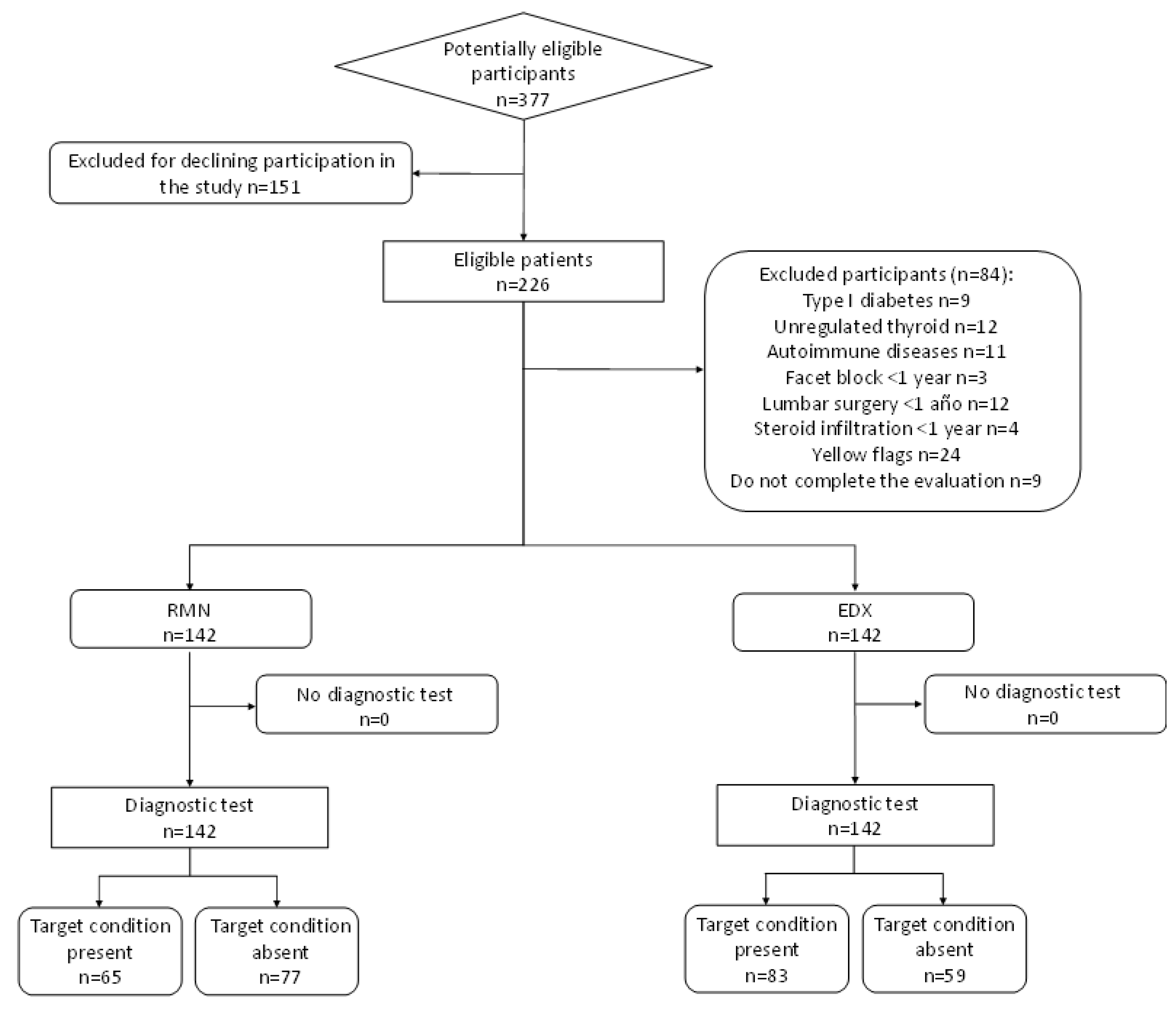
An electrodiagnostic study and magnetic resonance imaging were conducted on 142 patients suspected of lumbar radiculopathy,
Figure 1 presents the flow diagram. The sample comprised 60 (42.3%) males and 82 (57.7%) females, aged between 18 and 77 years, with a mean age of 54.82 years (SD 12.33). The mean body mass index (BMI) was 26.62 (SD 4.30), with 39.4% of the sample classified as overweight and 20.4% as pathologically obese. The mean duration of symptoms was 5.44 years (SD 6.10). Regarding the DN4 variable, the mean score was 3.44 points (SD 1.8), and considering a positive score from 4 points onwards [
42], it was positive for 47.2% of the sample and negative for 52.8%. The mean score on the ODI scale was 34.33 points (SD 18.12). Following the classification of this scale [
55], 28.9% of the sample had mild disability, 35.9% had moderate disability, 28.2% had severe disability, 6.3% had profound disability, and only 0.7% had very profound disability. Current pain, measured using the VAS scale, had a mean of 4.02 points (SD 2.47).
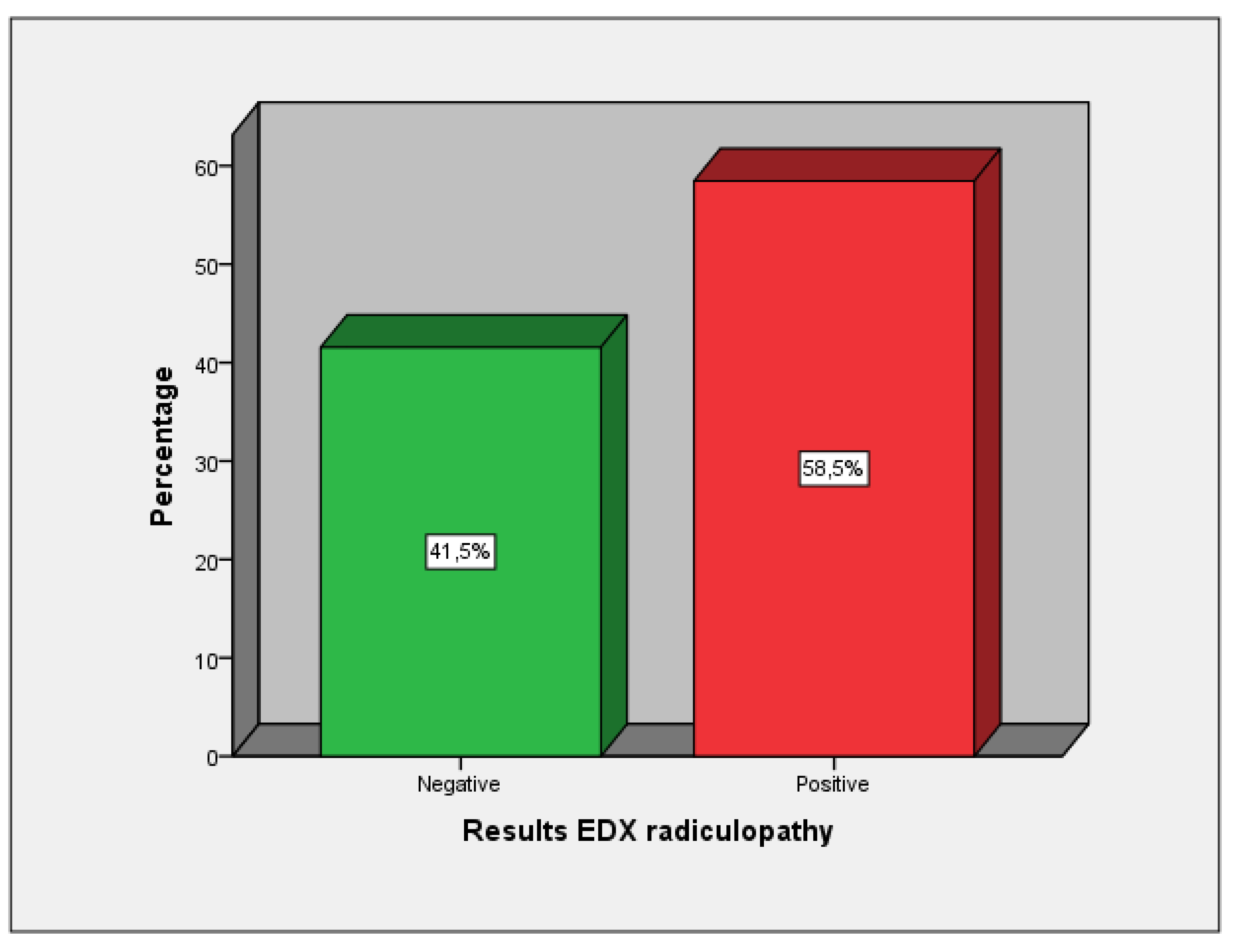
The results of the EDX were positive for radiculopathy in 58.5% and negative in 41.5% of cases (
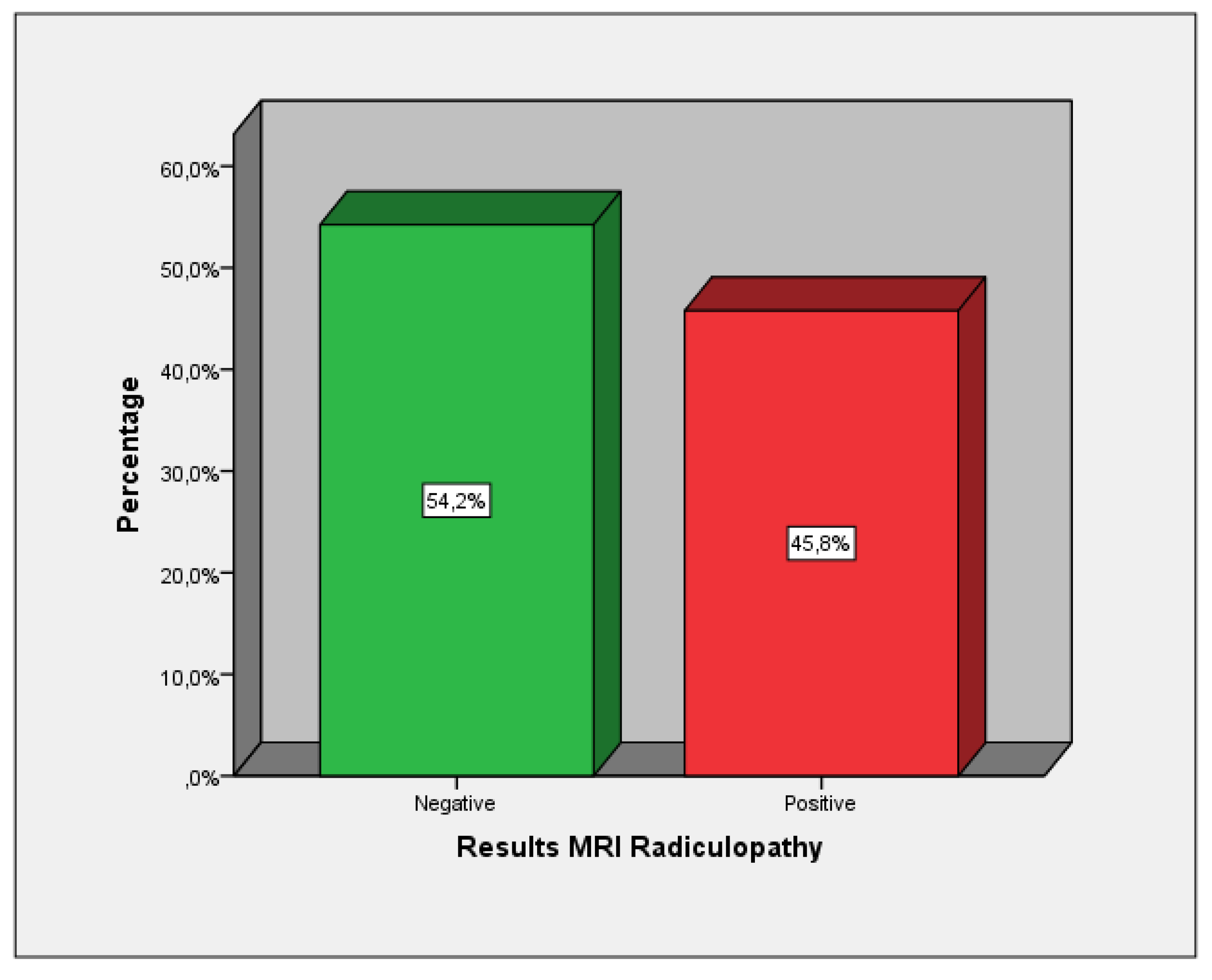
Figure 2). The L5 root was the most affected, accounting for 41.5%, followed by S1 with 26.1%. The MRI results showed that 45.8% tested positive for radiculopathy on MRI, while 54.2% tested negative (
Figure 3). 79.6% of the patients had some type of disc herniation and 66.2% presented signs of lumbosacral arthropathy, the most damaged disc was L4, affecting 63.5% of cases, followed by L5 with 61.3%.
Only the comparison of the variable ‘years with symptoms’ between the positive and negative radiculopathy groups via EDX was significant (p = 0.026) (
Table 1); however, it was not significant using MRI. The remaining clinical variables analyzed (current pain VAS, ODI scale, and DN4) did not show comparative significance using either EDX (
Table 1) or MRI (
Table 2).
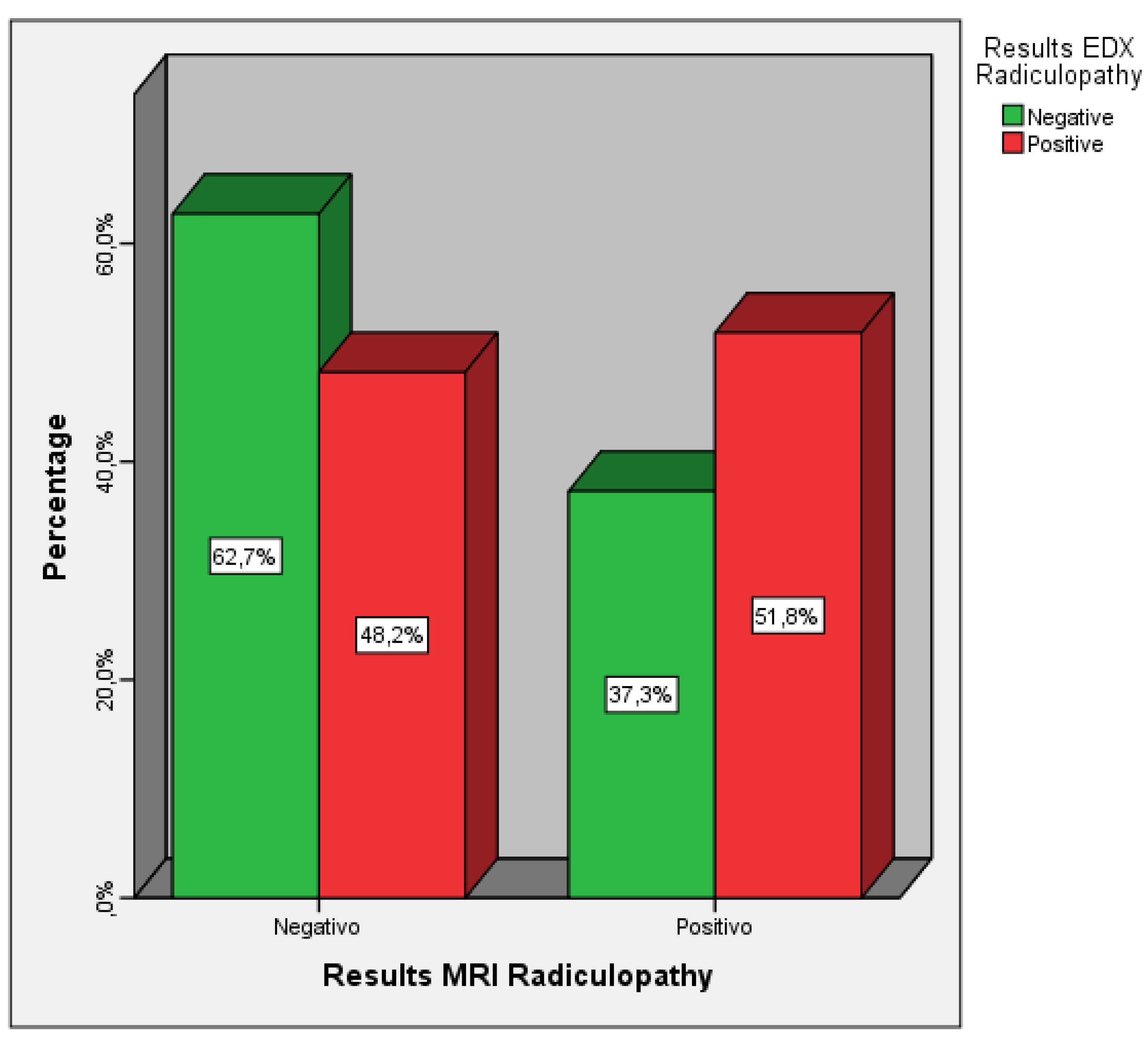
The comparison between the variable MRI Radiculopathy and EDx Radiculopathy was not statistically significant (p = 0.087), of those diagnosed as positive for radiculopathy using MRI, only 37.3% tested positive according to EDX, among those diagnosed as negative for radiculopathy using MRI, 62.7% tested negative according to EDX. The diagnostic agreement between both diagnostic tests, when seeking concordance in detecting radiculopathy on the same side and at the same lumbosacral segmental level, was 40.8% of cases (
Figure 4 and
Table 3).
4. Discussion
Our study firstly analyzes whether the comparison of different clinical variables between the positive and negative groups for radiculopathy using Electromyography (EDX) or Magnetic Resonance Imaging (MRI) as diagnostic tests was significant. Pain measured with the VAS at the time of examination resulted in the positive group showing lower levels compared to other similar studies, where significance was not observed, similar to our study using EDX as a reference [
56,
57]. The ODI scale also did not show statistical significance in the comparison using EDX; the recorded values were lower than in other studies [
36,
58]. Furthermore, the negative radiculopathy group had a higher mean than the negative group. Savage et al. [
59] in their EDX study reported similar data, where the positive group scored 37.2 compared to 43.4 in the negative group. The DN4 questionnaire also did not show significant differences when comparing the positive and negative groups for radiculopathy in our study, similar to the findings of Savage et al. [
59].
The only clinical variable that proved significant was ‘years with symptoms’ with the highest value observed in the positive group — 6.64 (SD 7.21) compared to 3.73 (SD 3.44) in the negative group. In many studies, the subject sample typically exhibits, on average, a shorter duration of symptoms, and we lack data for comparison. This finding would align with studies suggesting that a history of recurrent episodes of low back pain is a risk factor for developing radiculopathy [
4,
5,
60,
61].
The lack of significant results in any of the clinical variables — DN4, ODI scale, and current pain — when comparing positives and negatives for radiculopathy is consistent data in a sample with clinical suspicion of the pathology but without confirmation. This circumstance results in the inclusion of patients with other pathologies exhibiting concurrent symptoms, which may introduce confounding effects and complicate diagnosis [
62,
63,
64].
Regarding the agreement in the diagnosis of lumbosacral radiculopathy between MRI and EDX, various studies have presented differing results. Reza et al. [
27] compared the level of concordance between these two tests for lumbosacral radiculopathy, finding that 71% of MRIs showed findings consistent with radiculopathy, while EDX indicated 58%. Overall, the agreement level between the two tests was 59.6%. In the study by Yousif et al. [
23], among subjects with suspected radiculopathy —excluding subjects from a control group not considered for this calculation—, true negative and true positive concordance was 56.67%, which is very similar to our study and consistent with earlier studies [
28]. In a recent study by Murtaza et al. [
30], no significant relationship was found between both diagnostic tests, reinforcing the results obtained in our study.
In summary, it can be emphasized that both reference tests have their pros and cons, as MRI seeks structural damage while EDX detects alterations in the function of the neural system. As we can observe, the current mechanistic paradigm of seeking structural damage to confirm disc herniation or degeneration of structures housing the spinal cord and roots [
1,
5,
9,
16,
17,
18] through MRI does not align with the physiological study of the root using EDX. Currently, these are two diagnostic tests that assess different aspects of the pathology. Therefore, EDX —which allows for the physiological assessment of the root and detects when there is a functional alteration— will be a crucial test to confirm functional root impairment when there is clinical suspicion and a positive MRI [
20,
21,
22,
23,
24].
5. Conclusions
The number of years with pain symptoms is a significantly related factor to the diagnosis of lumbosacral radiculopathy via EDX in patients with clinical suspicion of the pathology, but not via MRI. Neither the ODI scale, DN4, nor current pain are significantly related factors to the diagnosis of lumbosacral radiculopathy in patients with clinical suspicion of the pathology using MRI or EDX as reference tests.
The comparison between the diagnosis of lumbosacral radiculopathy in patients with clinical suspicion of the pathology using MRI and EDX as diagnostic tests did not yield statistically significant results. MRI and EDX are complementary tests assessing different aspects in patients with suspected radiculopathy; degeneration of the structures supporting the spinal cord does not necessarily imply root dysfunction
Author Contributions
Conceptualization and methodology, A.M.-C., and E.B.-G; formal analysis, G.C. and P.P.-A.; resources, D.R.-M. and S.C.-P.; data curation, A.M.-C., D.R.-M. and G.C.; writing—original draft, A.M.-C., E.B.-G. and I.A.-C.; writing—review and editing, G.C., J.P.-R.-and S.C.-P.; supervision, E.B.-G. and A.M.-C..; project administration, E.B.-G. and S.C.-P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
The study was conducted in accordance with the ethical principles of the Declaration of Helsinki on human research. The local ethics committee (CEICA) approved the protocol of this study (PI21/073).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Adams AC. Mayo Clinic Essential Neurology. 1a edición. CRC Press; 2008. [CrossRef]
- Pardo-Fernández J, García-Sobrino T, Costa-Arpín E. Neuropatías, radiculopatías y plexopatías. Med - Programa Form Médica Contin Acreditado. 2015;11(78):4698-4710. [CrossRef]
- Vaduva RC, Orts Castro E, García Gálvez P, Yusta Izquierdo A. Diagnóstico y tratamiento de las neuropatías y radiculopatías. Med - Programa Form Médica Contin Acreditado. 2011;10(77):5227-5235. [CrossRef]
- Van Boxem K, Cheng J, Patijn J, et al. 11. Lumbosacral Radicular Pain. Pain Pract. 2010;10(4):339-358. [CrossRef]
- Casey E. Natural History of Radiculopathy. Phys Med Rehabil Clin N Am. 2011;22(1):1-5. [CrossRef]
- Swart NM, Apeldoorn AT, Conijn D, Meerhoff GA, Ostelo RWJG. KNGF Guideline on Low Back Pain and Lumbosacral Radicular Syndrome. Royal Dutch Society for Physical Therapy; 2021. https://www.kngf.nl/binaries/content/assets/kennisplatform/onbeveiligd/guidelines/low-back-pain-2021/kngf_guide_on_low_back_pain_justification.pdf.
- Tarulli AW, Raynor EM. Lumbosacral Radiculopathy. Neurol Clin. 2007;25(2):387-405. [CrossRef]
- Durrant DH, True JM. Chapter 7. Pathomechanisms of Radiculopathy. In: Myelopathy, Radiculopathy, and Peripheral Entrapment Syndromes. CRC Press LLC; 2002:161-199.
- Patel E, Perloff M. Radicular Pain Syndromes: Cervical, Lumbar, and Spinal Stenosis. Semin Neurol. 2018;38(06):634-639. [CrossRef]
- Tawa N, Rhoda A, Diener I. Accuracy of clinical neurological examination in diagnosing lumbo-sacral radiculopathy: a systematic literature review. BMC Musculoskelet Disord. 2017;18(1):93. [CrossRef]
- Durrant DH, True JM. Chapter 8. Classic Signs and Symptoms of Radiculopathy. In: Myelopathy, Radiculopathy, and Peripheral Entrapment Syndromes. CRC Press LLC; 2002:201-249.
- Vanhoestenberghe A. Chronic nerve root entrapment: compression and degeneration. J Neural Eng. 2013;10(1):011001. [CrossRef]
- Berry JA, Elia C, Saini HS, Miulli DE. A Review of Lumbar Radiculopathy, Diagnosis, and Treatment. Cureus. 2019;11(10):e5934. [CrossRef]
- Schoenfeld AJ, Laughlin M, Bader JO, Bono CM. Characterization of the Incidence and Risk Factors for the Development of Lumbar Radiculopathy. J Spinal Disord Tech. 2012;25(3):163-167. [CrossRef]
- Boyero Durán S. Protocolo diagnóstico de las radiculopatías. Medicine (Baltimore). 2007;9(78):5039-5041. [CrossRef]
- Barbero Jiménez DE, Hernández Ramírez MR, Celi Celi J, Villamor Rodríguez J. Neuropatías y radiculopatías. Med. 2023;13(77):4547-4560. [CrossRef]
- Scholz J, Finnerup NB, Attal N, et al. The IASP classification of chronic pain for ICD-11: chronic neuropathic pain. Pain. 2019;160(1):53-59. [CrossRef]
- van der Windt DA, Simons E, Riphagen I, et al. Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain. In: van der Windt DA, ed. Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd.; 2008. [CrossRef]
- Brinjikji W, Luetmer PH, Comstock B, et al. Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations. Am J Neuroradiol. 2015;36(4):811-816. [CrossRef]
- Ibarra Lúzar JI, Pérez Zorrilla E, Fernández García C. Electromiografía clínica. Rehabilitación. 2005;39(6):265-276. [CrossRef]
- Gutiérrez-Rivas E, Jiménez Hernández MD, Pardo Fernández J, Romero-Acebal M. Manual de Electromiografía Clínica. Ergon; 2007.
- FitzGerald MJT, Gruener G, Mtui E. Neuroanatomía Clínica y Neurociencia. 6a edicion. Elsevier España S.L.; 2012.
- Yousif S, Musa A, Ahmed A, Abdelhai A. Correlation between Findings in Physical Examination, Magnetic Resonance Imaging, and Nerve Conduction Studies in Lumbosacral Radiculopathy Caused by Lumbar Intervertebral Disc Herniation. Adv Orthop. 2020;2020:1-6. [CrossRef]
- Plastaras CT, Joshi AB. The Electrodiagnostic Evaluation of Radiculopathy. Phys Med Rehabil Clin N Am. 2011;22(1):59-74. [CrossRef]
- Sánchez Sendín D, Calderón Moreno M, García Leoni ME, Palazuelos Molinero V. Dolores musculoesqueléticos. Radiculopatías. Afectación de partes blandas. Artritis aguda. Med Programa Form Médica Contin Acreditado. 2011;10(89):6023-6040. [CrossRef]
- Kaito T, Yamato Y. The Essence of Clinical Practice Guidelines for Lumbar Disc Herniation, 2021: 3. Diagnosis. Spine Surg Relat Res. 2022;6(4):2022-0044. [CrossRef]
- Reza Soltani Z, Sajadi S, Tavana B. A comparison of magnetic resonance imaging with electrodiagnostic findings in the evaluation of clinical radiculopathy: a cross-sectional study. Eur Spine J. 2014;23(4):916-921. [CrossRef]
- Levin KH. Electromyography and magnetic resonance imaging in the evaluation of radiculopathy. Muscle Nerve. 1999;22(8):1158-1159. [CrossRef]
- Coster S, Bruijn SFTM, Tavy DLJ. Diagnostic value of history, physical examination and needle electromyography in diagnosing lumbosacral radiculopathy. J Neurol. 2010;257(3):332-337. [CrossRef]
- Murtaza F, Haider S, Amin A, Zahid A, Rehman AU. Correlation between Electrodiagnostic Study and Magnetic Resonance Imaging in Lumbar Radiculopathy Patients in a Tertiary Care Hospital. Case Reports Clin Med. 2023;12(10):363-370. [CrossRef]
- Vandenbroucke JP, Von Elm E, Altman DG, et al. Mejorar la comunicación de estudios observacionales en epidemiología (STROBE): explicación y elaboración. Gac Sanit. 2009;23(2):1-28. [CrossRef]
- Elm E von, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Declaración de la Iniciativa STROBE (Strengthening the Reporting of Observational studies in Epidemiology): directrices para la comunicación de estudios observacionales. Gac Sanit. 2008;22(5):144-150.
- Hajian-Tilaki K. Sample size estimation in diagnostic test studies of biomedical informatics. J Biomed Inform. 2014;48:193-204. [CrossRef]
- Rabin A, Gerszten PC, Karausky P, Bunker CH, Potter DM, Welch WC. The Sensitivity of the Seated Straight-Leg Raise Test Compared With the Supine Straight-Leg Raise Test in Patients Presenting With Magnetic Resonance Imaging Evidence of Lumbar Nerve Root Compression. Arch Phys Med Rehabil. 2007;88(7):840-843. [CrossRef]
- Urban LM, MacNeil BJ. Diagnostic Accuracy of the Slump Test for Identifying Neuropathic Pain in the Lower Limb. J Orthop Sport Phys Ther. 2015;45(8):596-603. [CrossRef]
- Ekedahl H, Jönsson B, Annertz M, Frobell RB. Accuracy of Clinical Tests in Detecting Disk Herniation and Nerve Root Compression in Subjects With Lumbar Radicular Symptoms. Arch Phys Med Rehabil. 2018;99(4):726-735. [CrossRef]
- Grondin F, Cook C, Hall T, Maillard O, Perdrix Y, Freppel S. Diagnostic accuracy of upper limb neurodynamic tests in the diagnosis of cervical radiculopathy. Musculoskelet Sci Pract. 2021;55(June):102427. [CrossRef]
- Pesonen J, Shacklock M, Suomalainen JS, et al. Extending the straight leg raise test for improved clinical evaluation of sciatica: validity and diagnostic performance with reference to the magnetic resonance imaging. BMC Musculoskelet Disord. 2021;22(1):808. [CrossRef]
- González Espinosa de los Monteros FJ, Gonzalez-Medina G, Ardila EMG, Mansilla JR, Expósito JP, Ruiz PO. Use of Neurodynamic or Orthopedic Tension Tests for the Diagnosis of Lumbar and Lumbosacral Radiculopathies: Study of the Diagnostic Validity. Int J Environ Res Public Health. 2020;17(19):7046. [CrossRef]
- Majlesi J, Togay H, Ünalan H, Toprak S. The Sensitivity and Specificity of the Slump and the Straight Leg Raising Tests in Patients With Lumbar Disc Herniation. JCR J Clin Rheumatol. 2008;14(2):87-91. [CrossRef]
- Alcántara-Bumbiedro S, Flórez-García MT, Echávarri-Pérez C, García-Pérez F. Escala de incapacidad por dolor lumbar de Oswestry. Rehabilitación. 2006;40(3):150-158. [CrossRef]
- Perez C, Galvez R, Huelbes S, et al. Validity and reliability of the Spanish version of the DN4 (Douleur Neuropathique 4 questions) questionnaire for differential diagnosis of pain syndromes associated to a neuropathic or somatic component. Health Qual Life Outcomes. 2007;5(1):66. [CrossRef]
- Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17(1):45-56. [CrossRef]
- Hjermstad MJ, Fayers PM, Haugen DF, et al. Studies Comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for Assessment of Pain Intensity in Adults: A Systematic Literature Review. J Pain Symptom Manage. 2011;41(6):1073-1093. [CrossRef]
- American-Association-of-Electrodiagnostic-&-Neuromuscular-Medicine. AANEM’s top five choosing wisely recommendations. Muscle Nerve. 2015;51(4):617-619. [CrossRef]
- Dillingham TR, Annaswamy TM, Plastaras CT. Evaluation of persons with suspected lumbosacral and cervical radiculopathy: Electrodiagnostic assessment and implications for treatment and outcomes (Part 1). Muscle Nerve. 2020;62(4):462-473. [CrossRef]
- Michael J, Tavee J. Electrodiagnosis of radiculopathy. In: K.H. Levin and P. Chauvel E, ed. Handbook of Clinical Neurology Clinical Neurophysiology: Diseases and Disorders. Vol 161. 3rd ed. Elsevier B.V.; 2019:305-316. [CrossRef]
- Dillingham TR, Annaswamy TM, Plastaras CT. Evaluation of persons with suspected lumbosacral and cervical radiculopathy: Electrodiagnostic assessment and implications for treatment and outcomes (Part II). Muscle Nerve. 2020;62(4):474-484. [CrossRef]
- Fardon DF. Nomenclature and Classification of Lumbar Disc Pathology. Spine (Phila Pa 1976). 2001;26(5):461-462. [CrossRef]
- Fardon DF, Williams AL, Dohring EJ, Murtagh FR, Gabriel Rothman SL, Sze GK. Lumbar disc nomenclature: version 2.0. Spine J. 2014;14(11):2525-2545. [CrossRef]
- Canga Villegas A. RM de la columna vertebral. In: Cerezal Pesquera L, García-Valtuille R AAF y CSJ, ed. Resonancia Magnética Del Sistema Músculoesquelético. SERME; 2005:231. chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://www.serme.es/wp-content/uploads/2016/05/capitulo8p.pdf.
- Burbano-Burbano H, Belalcázar-Bolaños E, Fernández-Tapia S. Resonancia magnética de la columna lumbar: lo que el radiólogo debe conocer antes de elaborar un reporte. An Radiol México. 2014;13:292-305. https://www.medigraphic.com/pdfs/anaradmex/arm-2014/arm143l.pdf.
- Li Y, Fredrickson V, Resnick DK. How Should We Grade Lumbar Disc Herniation and Nerve Root Compression? A Systematic Review. Clin Orthop Relat Res. 2015;473(6):1896-1902. [CrossRef]
- Montanero Fernández J, Minuesa Abril C. Estadistica Basica Para Ciencias de La Salud. (Universidad de Extremadura. Servicio de Publicaciones, ed.).; 2018. http://matematicas.unex.es/~jmf/Archivos/Manual de Bioestadística.pdf.
- Fairbank JCT, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25(22):2940-2953. [CrossRef]
- Stankovic R, Johnell O, Maly P, Wilmer S. Use of lumbar extension, slump test, physical and neurological examination inthe evaluation of patients with suspected herniated nucleurs pulposus. A prospective clinical study. Man Ther. 1999;4(1):25-32. [CrossRef]
- Skorupska E, Bednarek A, Urna M, Lisiński P, Sobieska M, Samborski W. Usefulness of clinical tests for assessing radicular and pseudoradicular components of pain in diagnosing sciatica – a pilot study. Rheumatology. 2013;51(4):265-270. [CrossRef]
- Suri P, Rainville J, Katz JN, et al. The Accuracy of the Physical Examination for the Diagnosis of Midlumbar and Low Lumbar Nerve Root Impingement. Spine (Phila Pa 1976). 2011;36(1):63-73. [CrossRef]
- Savage NJ, Fritz JM, Thackeray A. The Relationship Between History and Physical Examination Findings and the Outcome of Electrodiagnostic Testing in Patients With Sciatica Referred to Physical Therapy. J Orthop Sport Phys Ther. 2014;44(7):508-517. [CrossRef]
- Schroeder GD, Guyre CA, Vaccaro AR. The epidemiology and pathophysiology of lumbar disc herniations. Semin Spine Surg. 2016;28(1):2-7. [CrossRef]
- López-Zuazo Aroca I, Colato López A, Vaduva RC. Neuropatías y radiculopatías. Med - Programa Form Médica Contin Acreditado. 2011;10(77):5220-5226. [CrossRef]
- Grimm BD, Blessinger BJ, Darden BV, Brigham CD, Kneisl JS, Laxer EB. Mimickers of Lumbar Radiculopathy. J Am Acad Orthop Surg. 2015;23(1):7-17. [CrossRef]
- DeFroda SF, Daniels AH, Deren ME. Differentiating Radiculopathy from Lower Extremity Arthropathy. Am J Med. 2016;129(10):1124.e1-1124.e7. [CrossRef]
- Conger A, Smuck M, Truumees E, Lotz JC, DePalma MJ, McCormick ZL. Vertebrogenic Pain: A Paradigm Shift in Diagnosis and Treatment of Axial Low Back Pain. Pain Med. 2022;23(Supplement_2):S63-S71. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).