1. Introduction
Adult chronic rhinosinusitis is an inflammation of the mucosal layer of the nose and paranasal sinuses, which is characterized by two or more symptoms, one of which must be either nasal congestion or nasal discharge (anterior or posterior): also presence or absence of facial pain and/or pressure, as well as the presence or absence of decreased or loss of sense of smell for 12 weeks or more and either- endoscopic signs, such as nasal polyps, and/or mucopurulent discharge predominantly from the middle nasal passage and/or swelling/obstruction of the mucosa predominantly of the middle nasal passage and/or- CT changes: mucosal changes in the osteomata complex and/or sinuses [
1]. Numerous factors are known to cause and make cases of chronic rhinosinusitis refractory to optimized treatment, including genotypic or phenotypic mucosal changes, scarring and synechiae, allergies, smoking, and gastroesophageal acid reflux [
2]. The current definition of actionable gastroesophageal reflux disease requires convincing evidence of reflux-related pathology by endoscopy and/or monitoring for abnormal reflux (using the Lyon Consensus thresholds) in the presence of compatible bothersome symptoms. Typical bothersome symptoms alone may be sufficient for antisecretory drug trials, but for all other symptom categories and in patients who do not respond to proton pump inhibitors (PPIs), preliminary esophageal testing is recommended before invasive treatment of gastroesophageal reflux disease or before long-term medical treatment [
3]. Changes in the laryngeal mucosal layer under the influence of laryngopharyngeal reflux were first described and systematized in 2001 by Belafsky
et al [
4]. In 2020, Lechien
et al. supplemented the endoscopic picture of the larynx under the influence of laryngopharyngeal reflux by describing changes on the pharyngeal side [
5]. In 2022, Zeleník
et al. identified a relationship between hypertrophy of the Inferior Turbinate and extraesophageal reflux [
6]. The aim of our study is to determine the characteristics of the endoscopic picture of the nose and nasopharynx in chronic rhinosinusitis associated with symptoms of gastroesophageal acid reflux disease. We aim to identify any abnormalities in the endoscopic picture of chronic rhinosinusitis associated with symptoms of acid gastroesophageal reflux disease. We believe this will lead to more effective management of this group of patients, which may reduce the frequency of chronic rhinosinusitis exacerbations and significantly affect the duration of chronic rhinosinusitis exacerbations.
2. Materials and Methods
2.1. Patient and Setting
A total of 521 adult patients with chronic rhinosinusitis were examined and treated at the University Medical Center Corporative Fund (UMC CF) and the multidisciplinary hospital #1 in Astana (Kazakhstan). The patients met the clinical definition of chronic rhinosinusitis, with symptoms that is caused by inflammatory process in the nose and paranasal sinuses mucosa; clinical symptoms include nasal congestion, nasal discharge and/or facial pain/pressure, ±decreased or loss of sense of smell lasting more than 12 weeks and documentation of chronic rhinosinusitis by computed tomography (CT) results, endoscopic images. All patients were examined by us and provided endoscopic diagnostic method in the remission period of chronic rhinosinusitis and before starting the anti-reflux treatment of gastroesophageal reflux disease. Confirmation of gastroesophageal reflux disease symptoms identified by endoscopic diagnostic method in all patients. Standardized questionnaires were used to question all patients with confirmed chronic rhinosinusitis and gastroesophageal reflux disease symptoms. To determine the regularity of the changes in the nasal and nasopharyngeal mucosa, we have selected patients with the highest scores on the Reflux Symptom Index (RSI) (>20) and Reflux Symptom Score-12 (RSS-12) (>130) questionnaires, as well as patients with smoking, active seasonal allergies or asthma, history of laryngeal cancer, pregnant women were excluded, which allowed us to obtain the final group of 95 patients. The study's control group comprised 41 patients with chronic rhinosinusitis but without gastroesophageal reflux disease symptoms, as well as 10 patients without any signs of chronic rhinosinusitis or gastroesophageal reflux disease symptoms.
2.2. Standardized Questionnaires.
The Reflux Symptom Index (RSI), a 9-item self-administered questionnaire developed by Belafsky
et al (2002), was used to document the presence and degree of symptoms of laryngopharyngeal reflux. The maximum score on the RSI is 45 [
7].
The Reflux Symptom Score (RSS) is a 12-item self-administered tool used to diagnose and monitor laryngopharyngeal reflux (LPR) and its impact on quality of life. The maximum score is 300 [
8].
A flexible endoscope was used to perform an endoscopy of the nasal cavity and nasopharynx. The condition of the lower nasal turbinate, were assessed according to the Camacho classification [
9,
10], Grades 1 to 4: grade 1 - 0%–25% of total airway space, grade 2 - 26%–50% of total airway space, grade 3 - 51%–75% of total airway Space, grade 4 - 76%–100% of total airway space, as well as the condition of the nasopharyngeal mucosa and the Eustachian tube junction.
3. Results
We have provided below the data structure by gender, where the total number of patients is 146. Of these, 75 are male and 71 are female. Also divided them into 3 groups: the main group of 95 patients are selected patients with the highest scores on the Reflux Symptom Index (RSI) (>20) and Reflux Symptom Score-12 (RSS-12) (>130) questionnaires with chronic rhinosinusitis in clinical remission and associated with symptoms of gastroesophageal reflux disease, control-1 with the presence of chronic rhinosinusitis in clinical remission, but with no evidence of gastroesophageal reflux disease (GERD) , control-2, a group of healthy patients with no signs of chronic rhinosinusitis and no symptoms of gastroesophageal reflux disease. (
Table 1). Additionally, age, RSS-12, and RSI data by 3 groups: primary, control-1, control-2 (
Table 2). The last table presents statistical data on gender, race, and groups (
Table 3).
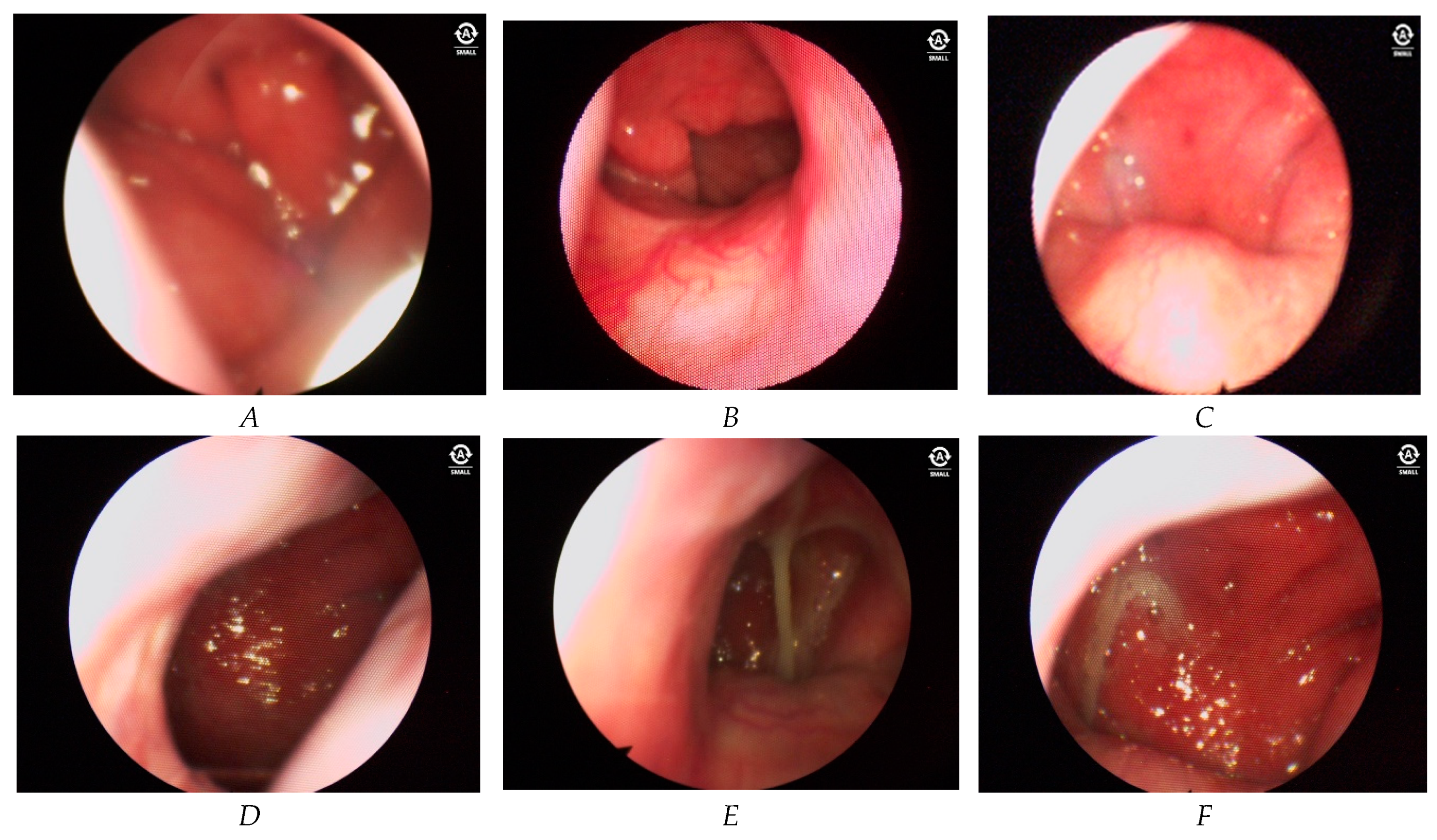
During endoscopic examination of the nose and nasopharynx, we identified changes in the mucosa of the posterior parts of the nasal cavity, particularly in the posterior end of the inferior nasal concha on one side in patients with chronic rhinosinusitis associated with GERD. Furthermore, a notable disparity in the condition of the nasal cavity mucosa was observed between the anterior and posterior parts of the nasal cavity. In the anterior parts, the mucosa may remain unchanged or show grade 1 hypertrophy according to the Camacho classification. Anterior dry rhinitis with crusts is a common occurrence. Moving to the posterior parts of the nasal cavity, severe edema, asymmetrical hypertrophy of the posterior ends of the lower nasal bones, and abundant mucus are observed. Nasal edema was found two blinded raters in 75 patients (78,9%) (Figure 1A). However, it is difficult to identify these findings as a specific feature of chronic rhinosinusitis associated with gastroesophageal disease in adults. In comparison with the control groups, this symptom was observed in the main group, such as pronounced swelling of the nasal mucosa. While no such reactive nasal oedema was observed in control group 1, hypertrophic changes without active nasal edema were observed in the remission period. In control group 2, there were no changes in the nasal mucosa because the patients in this group do not have chronic rhinosinusitis or gastroesophageal reflux disease.
Significant changes were observed in the nasopharyngeal mucosal layer. Increased vascularity of the nasopharyngeal mucosal layer was noted in 91 patients (95,7%) (Figure 1B,C). The underlying pathogenetic mechanism of this vascular pattern is not known yet. But we suggest that this was caused by thinning of mucosal layer under the effect of reflux content. Hypertrophy of the nasopharyngeal mucosal layer was found in 83 patients (87,4%) (Figure 1D). In 77 (81,1%) patients, mucus was found in the nasopharynx with different characteristics of color and consistency (Figure 1E), and no mucus or other secretions were found in the middle nasal passages in these patients. Color of mucus was verified from transparent to the pronounced green color. Consistency of the mucus was viscous, which is characterized by thick, hard to remove mucosal discharge. In 62 patients (65,3%) asymmetric hypertrophy of the mucosa of the oropharynx was noted (Figure 1F). The more pronounced lesion of one half of the nose and nasopharynx was associated with a preference for falling asleep and sleeping on the right side or left side. For this reason we can suggest that this hypertrophic changes in the nose and nasopharynx was caused under the effect of acidic reflux content.
Figure 2.
Endoscopic findings.
Figure 2.
Endoscopic findings.
By analyzing all the obtained data we came to conclusion that in chronic rhinosinusitis associated with gastroesophageal disease the mucosal layer of the posterior parts of the nose and nasopharynx are under continuous inflammatory process because of regular acidic reflux content influence.
4. Discussion
The results of our study showed that gastroesophageal reflux has an effect on the mucosal layer of the nasal cavity and nasopharynx that is similar in nature to the effect of laryngopharyngeal reflux on the larynx and pharynx: edema, presence of mucus, increased vascular pattern with hyperemia and hypertrophy. Many studies have highlighted the etiopathogenetic role of gastroesophageal reflux in the development of sinus and nasopharyngeal inflammation [
11,
12,
13,
14]. Analysis of the causal relationship between GERD and chronic rhinosinusitis at the genetic level has shown that gastroesophageal reflux disease increases the risk of developing chronic rhinosinusitis by 36% [
15]. In our study we have determined some specific abnormalities: mucosa of the posterior parts of the nose (posterior ends of the lower nasal bracts, scolex) and nasopharynx undergo significant changes. As in the pharynx [
16], we also found an increased vascular pattern and the presence of mucus in the posterior parts of the nose and nasopharynx. A study of the relationship between laryngopharyngeal reflux and otitis media with effusion in children showed that pepsin levels gradually increased as the viscosity of the fluid in the middle ear cavity increased [
12]. It is thought that exposure to gastric contents via nasopharyngeal reflux provokes hypersecretion of mucus in the nasopharynx.
The large amount of mucus causes a postnasal syndrome, which is the main cause of discomfort for patients with nasopharyngeal reflux and reduces their quality of life. This syndrome is characterized by flowing of nasal discharge from the nose through nasopharynx to the posterior wall of pharynx. Many patients report that they find it difficult to remove this thick mucus when they blow their nose or try to swallow.
In our study, we found significant changes in the nasopharyngeal and nasal mucosal layers. There are several theories as to how gastroesophageal reflux disease affects the nasal and nasopharyngeal cavities. One is that the acidic reflux contents may have a direct effect on the nasal and nasopharyngeal mucosal layer, as evidenced by a reaction of the nasal mucosa similar to that of the esophageal mucosa on direct contact with gastric contents: expression of pepsin A and heat shock protein 70 [
17]. Second, Helicobacter pylori may be involved in the mechanism of development of chronic rhinosinusitis, leading to the formation of nasal polyps [
18]. Thirdly, autonomic nervous system dysfunction associated with gastroesophageal reflux disease through the existing nerve reflex between the esophagus and the sinuses via the vagus nerve [
18].
The characteristics of changes in the nasal and nasopharyngeal mucosa on endoscopic examination of the nose and nasopharynx in patients with nasopharyngeal reflux are shown in
Table 4.
5. Conclusion
Our study of 95 patients with chronic rhinosinusitis associated with symptoms of gastroesophageal reflux disease and two control groups showed significant changes in the mucosa of the posterior nasal and nasopharyngeal cavities. This has allowed us to propose a convenient method for the differential diagnosis of the etiopathogenetic course of chronic rhinosinusitis. This may help general practitioners and otolaryngologists to correctly identify the triggering factor of chronic rhinosinusitis, which in turn may reduce the frequency and intensity of exacerbations of chronic rhinosinusitis. This will have a positive impact on the quality of life of the patient. We are of the opinion that this direction needs to be studied in more detail.
Author Contributions
“Conceptualization, Kalamkas T. Sagandykova, Nataliya M. Papulova, and Talapbek M. Azhenov; methodology Kalamkas T. Sagandykova; software Aliya Darbekova; validation, Nataliya M. Papulova, and Talapbek M. Azhenov; investigation, Kalamkas T. Sagandykova and Nataliya M. Papulova; writing—original draft preparation, Kalamkas T. Sagandykova; writing—review and editing, Kalamkas T. Sagandykova and Jerome R. Lechien.; visualization, Kalamkas T. Sagandykova; supervision, Jerome R. Lechien; All authors have read and agreed to the published version of the manuscript.”.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by Local Ethical Commission of the NpJSC “Astana Medical University” (protocol code LCB NpJSC AMU #13 date 11/29/2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Fokkens, W.J.; Viskens, A.-S.; Backer, V.; Conti, D.; De Corso, E.; Gevaert, P.; Scadding, G.K.; Wagemann, M.; Bernal-Sprekelsen, M.; Chaker, A.; et al. EPOS/EUFOREA update on indication and evaluation of Biologics in Chronic Rhinosinusitis with Nasal Polyps 2023. Rhinol. J. 2023, 61, 194–202. [Google Scholar] [CrossRef]
- Sella, G.C.P.; Tamashiro, E.; Anselmo-Lima, W.T.; Valera, F.C.P. Relation between chronic rhinosinusitis and gastroesophageal reflux in adults: systematic review. Braz. J. Otorhinolaryngol. 2016, 83, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Gyawali, C.P.; Yadlapati, R.; Fass, R.; Katzka, D.; Pandolfino, J.; Savarino, E.; Sifrim, D.; Spechler, S.; Zerbib, F.; Fox, M.R.; et al. Updates to the modern diagnosis of GERD: Lyon consensus 2.0. Gut 2023, 73, 361–371. [Google Scholar] [CrossRef]
- Belafsky, P.C.; Postma, G.N.; Koufman, J.A. The Validity and Reliability of the Reflux Finding Score (RFS). Laryngoscope 2001, 111, 1313–1317. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Bobin, F.; Muls, V.; Mouawad, F.; Dapri, G.; Dequanter, D.; Horoi, M.; Thill, M.-P.; Ruiz, A.R.; Saussez, S. Changes of Laryngeal and Extralaryngeal Symptoms and Findings in Laryngopharyngeal Reflux Patients. Laryngoscope 2021, 131, 1332–1342. [Google Scholar] [CrossRef] [PubMed]
- Zeleník, K.; Javorská, Z.; Taimrová, R.; Vrtková, A.; Hránková, V.; Tedla, M.; Lukáčová, K.; Lubojacký, J.; Formánek, M.; Komínek, P. Association Between Inferior Turbinate Hypertrophy and Extraesophageal Reflux. JAMA Otolaryngol. Neck Surg. 2022, 148, 773–778. [Google Scholar] [CrossRef]
- Belafsky, P.C.; Postma, G.N.; A Koufman, J. Validity and Reliability of the Reflux Symptom Index (RSI). J. Voice 2002, 16, 274–277. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Bobin, F.; Rodriguez, A.; Dequanter, D.; Muls, V.; Huet, K.; Harmegnies, B.; Crevier-Buchman, L.; Hans, S.; Saussez, S.; et al. Development and Validation of the Short Version of the Reflux Symptom Score: Reflux Symptom Score–12. Otolaryngol. Neck Surg. 2020, 164, 166–174. [Google Scholar] [CrossRef]
- Camacho, M.; Zaghi, S.; Certal, V.; Abdullatif, J.; Means, C.; Acevedo, J.; Liu, S.; Brietzke, S.E.; Kushida, C.A.; Capasso, R. Inferior Turbinate classification system, grades 1 to 4: Development and validation study. Laryngoscope 2014, 125, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Camacho, M.; Zaghi, S.; Certal, V.; Abdullatif, J.; Modi, R.; Sridhara, S.; Tolisano, A.M.; Chang, E.T.; Cable, B.B.; Capasso, R. Predictors of Nasal Obstruction: Quantification and Assessment Using Multiple Grading Scales. Plast. Surg. Int. 2016, 2016, 1–9. [Google Scholar] [CrossRef]
- Anzić, S.A.; Turkalj, M.; Župan, A.; Labor, M.; Plavec, D.; Baudoin, T. Eight weeks of omeprazole 20 mg significantly reduces both laryngopharyngeal reflux and comorbid chronic rhinosinusitis signs and symptoms: Randomised, double-blind, placebo-controlled trial. Clin. Otolaryngol. 2017, 43, 496–501. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Yang, Q.; Sheng, Y.; Wang, Z.; Zhang, Q.; Yan, J.; Hou, J.; Zhu, K.; Cheng, Y.; Wang, B.; et al. Role of pepsin and pepsinogen: Linking laryngopharyngeal reflux with otitis media with effusion in children. Laryngoscope 2013, 124, E294–E300. [Google Scholar] [CrossRef]
- Brunworth, J.D.; Mahboubi, H.; Garg, R.; Johnson, B.; Brandon, B.; Djalilian, H.R. Nasopharyngeal Acid Reflux and Eustachian Tube Dysfunction in Adults. Ann. Otol. Rhinol. Laryngol. 2014, 123, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Brar, S.; Watters, C.; Watson, N.; Birchall, M.; Karagama, Y. Ear, nose and throat (ENT) manifestations and complications of reflux. Front. Gastroenterol. 2022, 13, e57–e64. [Google Scholar] [CrossRef]
- Chen, G.; Guo, W.; Liu, S.; Wang, Y.; Zhang, X. Causal analysis between gastroesophageal reflux disease and chronic rhinosinusitis. Eur. Arch. Oto-Rhino-Laryngology, 7. [CrossRef]
- Lechien, J.R.; Ruiz, A.R.; Dequanter, D.; Bobin, F.; Mouawad, F.; Muls, V.; Huet, K.; Harmegnies, B.; Remacle, S.; Finck, C.; et al. Validity and Reliability of the Reflux Sign Assessment. Ann. Otol. Rhinol. Laryngol. 2019, 129, 313–325. [Google Scholar] [CrossRef] [PubMed]
- Ren, J.; Zhao, Y.; Wang, J.; Ren, X.; Xu, Y.; Tang, W.; He, Z. PepsinA as a Marker of Laryngopharyngeal Reflux Detected in Chronic Rhinosinusitis Patients. Otolaryngol. Neck Surg. 2017, 156, 893–900. [Google Scholar] [CrossRef]
- Chen, W.C.; Chang, Y.T.; Chen, S.F.; Lin, W.C.; Su, Y.Y.; Luo, S.D. The symptom burden of autonomic dysfunction is positively associated with chronic rhinosinusitis status. Rhinol. J. 2018, 56, 227–233. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).