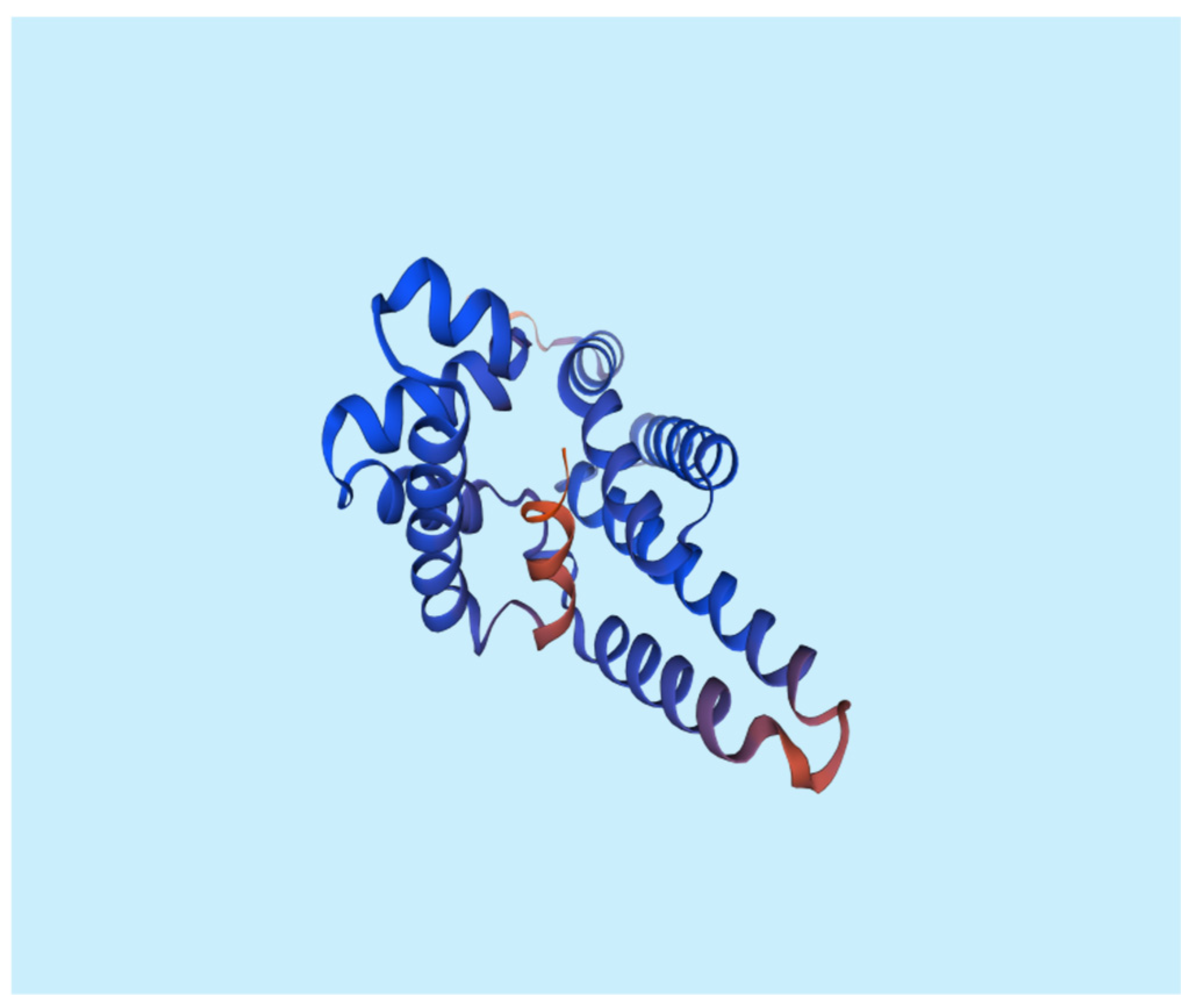
Instruments
Table 1.
List of instruments:.
Table 1.
List of instruments:.
Material:
All chemical and biochemical substances were obtained from Algomhuria Pharmaceutical Company and Alnasr Chemical Company, Egypt. All chemical reagents utilized were of expository review.
Isolation of Myxococcus SDU36 producing Myxopyronin B antibiotic:
The selective isolation of species of
Myxococcus SDU36 from different soil samples was directly performed utilizing
dilution plating. The technique included the suppression of competing bacteria exploiting antibiotics such as
10 mcg/ ml Vancomycin and/ or
10 mcg/ ml Chloramphenicol combined with wet heat treatment of soils and air drying. Fungi were eliminated via supplementing the plating medium with
2 mcg/ ml Terbinafine HCl. Swarming of
Myxococcus SDU36 colonies was controlled with
Casein Yeast Peptone(
CYP) plates incubated at
30℃ and
PH 7.2 for
5 days. The composition of
CYP plate included
0.4 % Peptone from
Casein, tryptically digested,
0.3 % CaCl2.2H2O,
0.1 % MgSO4.7H2O,
PH 7.2. The potent bacterial isolate producing
Myxopyronin was performed utilizing
16 S rRNA sequencing technique. The predominant bacterial isolate with high antibacterial activity was identified using
16S rRNA sequencing and other biochemical tests. Nucleic acid was extracted from a swab by bead-beating in a buffered solution containing Phenol, Chloroform and Isoamyl alcohol. Variable region of
16S rRNA gene was then amplified from the resulting nucleic acid using
PCR. The genomic
DNA was extracted from
120 hours cultured cells using a
DNA purification kit[
PurreLinkTM Genomic DNA Mini Kit with Catalog number: K182002 was purchased from Invitrogen, USA] according to the protocol provided by the manufacturer of
DNA purification kit.
The 16S rRNA gene was amplified by
PCR[
PCR SuperMix kit was purchased from Invitrogen,
USA] using forward[
5-AGAGTTTGATCCTGGCTCAG-3-] and reverse[
5-GGTTACCTTGTTACGACTT-3-]
primers.
PCR amplicons from up to hundreds of samples were then combined and sequenced on a single run. The resulting sequences were matched to a reference database to determine relative bacterial abundances. Polymerase Chain Reaction (
PCR) was a powerful method for amplifying particular segments of
DNA.
PCR used the enzyme
PlatinumTM Taq DNA polymerase with catalog number
10966018[ purchased from Invitrogen,
USA] that directed the synthesis of
DNA from deoxynucleotide substrates on a single-stranded
DNA template.
DNA polymerase added nucleotides to the 3` end of a custom-designed oligonucleotide when it was annealed to a longer template
DNA. Thus, if a synthetic oligonucleotide was annealed to a single-stranded template that contained a region complementary to the oligonucleotide,
DNA polymerase could use the oligonucleotide as a primer and elongate its 3` end to generate an extended region of double stranded
DNA.
Denaturation was the initial PCR cycle stage The
DNA template was heated to
94° C. This broke down the weak hydrogen bonds that held
DNA strands together in a helix, allowing the strands to separate creating single stranded
DNA.
Annealing was the second PCR cycle. The mixture was cooled to anywhere from
50-70° C. This allowed the primers to bind (anneal) to their complementary sequence in the template
DNA.
Extension was the final step of PCR cycle. The reaction was ; then heated up to
72° C, the optimal temperature for
DNA polymerase to act.
DNA polymerase extended the primers, adding nucleotides onto the primer in a sequential manner, using the target
DNA as a template.
With one cycle, a single segment of double-stranded DNA
template was amplified into two separate pieces of double-stranded DNA
. These two pieces were then available for amplification in the next cycle. As the cycles were repeated, more and more copies were generated and the number of copies of the template was increased exponentially. The amplified
PCR product was sequenced using a genetic analyzer
3130XL[ purchased from Applied biosystems,
USA].
DNA sequence homology search analysis of the predominant bacterial isolate was achieved using Blastn algorithm at
NCBI website. Fruiting bodies were examined using a
Stereomicroscope(
dissecting microscope) MSC-ST45T( purchased from Infetik, China). Wet mounts from crushed fruiting bodies were prepared. The refaractility, shape and the size of
Myxospores were determined victimizing phase contrast microscopy. On the other hand the plates were exposed to
360 nm wavelength ultraviolet light to assess the fruiting bodies fluoresced.[
16]
Identification Myxopyronin B producing bacterial isolates:
Gram stain:
It grouped bacteria into two types based on their cell wall composition.
Bacterial cells turned purple after being treated with a solution of
crystal violet and then
iodine on a microscope slide. When stained cells were treated with solvents such as alcohol or acetone,
Gram-positive bacteria retained the stain while
Gram-negative bacteria lost the stain and became colorless. With the addition of the decolorizing agent
safranin, transparent Gram-negative bacteria turned pink.[
17]
Spore shape:
This was discovered using the spore staining method. To get rid of any fingerprints, the slide was wiped with alcohol and a Kim-wipe. On the bottom of the slide, a Sharpie was used to create two circles. Each circle was filled with two tiny droplets of water using an inoculation loop. A very small amount of germs was taken out of the culture tube using an aseptic method. The water droplet on the slide had microorganisms on it. The slide was thoroughly dried by air. Bypassing the slide through the flame three to four times with the smear side up, the slide was heat-fixed. It took a while for the slide to completely cool. A piece of paper towel placed inside the slide’s border was used to hide the streaks. A beaker of heating water was situated over the slide. The slide was allowed to steam for three to five minutes; while the paper towel was covered with a malachite green liquid. Removed and thrown away was the discolored paper towel. To get rid of any stray paper towel bits, the slide was gently cleaned with water. The counter-stain was safranin for 1 minute. Before putting the slide on the microscope’s stage and seeing it via the oil immersion lens, the slide’s bottom was dried.[
18]
Spore site:
During the Gram stain test, the spore location was grooved.[
19]
Cell shape:
During the Gram stain test, the cell shape was determined.[
20]
Blood haemolysis:
On blood agar media, the test antibiotic capacity to haemolyze the blood was tried.[
21]
Motility test:
It distinguished between motile bacteria and non-motile bacteria.
A sterile needle was used to penetrate the medium to within
1 cm of the tube’s bottom to select a well-isolated colony and test for motility. The needle was certainly preserved in the same position as it was artifact-ed and removed from the medium. It took
18 hours of incubation at
35°C, or until evident growth materialized.[
22]
Nitrate reduction test:
0.5 ml of
Nitrate broth situated in a clean test tube was autoclaved for
15 minutes at
15 lbs pressure and
121°C, and was all-awed to cool to room temperature. The tube was inoculated with a heavy inoculum of unspoiled bacterial culture and was incubated at
35°C for
2 hours.
2 drops of
reagent A and
2 drops of
reagent B were added and blended well. The evolution of red color within
2 minutes was ascertained for. If no red color was formed, a small quantity of Z
inc dust was added and discovered for the alteration to the red color in
5 minutes.[
23]
Methyl red test:
In the
Methyl Red test, an pestiferous tube of MR broth was used before adding the methyl red
PH indicator. The buffers in the medium were get over by the acids when an organism utilized the blended acid fermentation pathway and brought forth stable acidic end products, consequent on an acidic environment.[
24]
Catalase test:
A little inoculum of a specific bacterial strain was enclosed to a
3% Hydrogen peroxide solution to comprehend if it might produce
Catalase. It was ascertained for the rapid emission of
Oxygen bubbles.[
25]
Oxidase test:
The
1% Kovács oxidase reagent was added to a little piece of filter paper, which was then let to air dry. A well-isolated colony was confiscated from a fresh(
18 to 24-hour culture) bacterial plate victimizing a sterile loop, and it was then hang-up onto processed filter paper. Color changes were detected.[
26]
Citrate utilization:
Five milliliters of a
Simmon Koser’s citrate medium were condemned after it had been autoclaved at
15 pounds for
15 minutes. To make up a clear slant and butt, the test tube incorporating melted citrate medium was slanted. Exploiting sterilized wire and labeled tubes, the specified samples of microbe were injected on the media’s incline. For
24 hours, the tubes were incubated at
37°C. The medium’s color alteration was observed for.[
27]
Starch hydrolysis:
For
48 hours at
37°C, the bacterium plates were injected. After incubation, a dropper was utilized to saturate the surface of the plates with an iodine solution for
30 seconds. Iodine that was in superfluous was subsequently swarmed out. The area surrounding the bacterial growth line was dictated.[
28]
Tween 80 hydrolysis:
1% Tween 80 was exploited to make up agar media. The rendered microorganism was introduced to the
Tween 80 agar plates by employing an inoculating loop to make up a single center streak in the plate. The plates were procreated for
24 hours at
37 °C.
HgCl2 solution was displaced over the plates. After a short while, the plates were discovered. Positive test outcome; well-defined halo-zone surrounding the injected area demonstrated
Tween 80 chemical reaction.[
29]
Growth at 10-45 0C:
On nutrient agar media, biological process was observed to be possible at 10-
45°C.[
30]
Indol test:
The test tube incorporating the microorganism for inoculation received
5 drops of the
Kovács reagent directly. Within seconds after inserting the reagent to the media, the reagent layer settled a pink to red colour (cherry-red ring), which was a mark of a positive
Indol test.[
31]
Tolerance salinity test:
Its capacity to evolve on nutrient agar while being responsive to
5% and
7 % NaCl was detected.[
32]
Voges-Proskauer(VP) test:
For the test,
Voges-Proskauer broth, a glucose-phosphate broth affluent-ed with microorganisms, was added to
Alpha-naphthol and
Potassium hydroxide. A successful consequence was betoken aside a
Cherry red tint; whereas an unfortunate consequence was signal via a yellow-brown color.[
33]
Casein hydrolysis test:
For testing the
Casein hydrolyzing activity of the test antibiotic, a single line streak of the given culture was performed in the center of the skim milk agar plate under aseptic conditions and plate was procreated at
37°C in an incubator for
24-48 h.[
34]
Saccharide fermentation tests:
Glucose fermentation test:
The fermentation reactions of glucose were investigated using glucose purple broth. Peptone and the
PH indicator bromcresol purple made up the purple broth. A
1% concentration of glucose was added. Isolated colonies from a 24-hour pure culture of microorganisms were added to the glucose purple broth as an inoculant. Parallel to the inoculation of the glucose-based medium, a control tube of purple broth base was used. The inoculated medium was incubated aerobically for
3 days at a temperature of
35–37 °C. The medium began to become yellow, which was a sign of a successful outcome. A poor carbohydrate fermentation response was indicated by the lack of yellow color development.[
35]
Fructose fermentation test:
A pure culture’s inoculum was aseptically transferred to a sterile tube of phenol red fructose broth. The infected tube was incubated for
18–24 hours at
35–37 °C. A color shift from red to yellow, signifying an acidic PH alteration, was a sign of a favorable response.[
36]
Maltose fermentation test:
A pure culture inoculum was aseptically transferred to a sterile tube containing phenol red maltose broth. The infected tube was incubated for
18–24 hours at
35–37 °C. A color shift from red to yellow, signifying an acidic PH alteration, was a sign of a favorable response.[
37]
Sucrose fermentation test:
A pure culture’s inoculum was aseptically transferred to a sterile tube containing phenol red sucrose broth. For
24 hours, the infected tube was incubated at
35–37 0C. A colour shift from red to yellow, signifying an acidic
PH alteration, was a sign of a favourable response.[
38]
Purification of Myxopyronin B antibiotic:
This was achieved through reversed phase chromatography technique.
The aeration rate was
0.142 V/ V. min. The stirring rate was
500 rpm.
PO2 was about
90 % of saturation; but decreased to about
20 % after
18 hours). The fermentation was stopped after
40 hours via centrifugation at
500 rpm in a gyrator shaker. The supernatants were collected; then tested for antimicrobial sensitivity using broth dilution technique to detect
MICs and agar paper diffusion discs technique. The test antibiotic was extracted from the
2 liters of culture broth with
2/ 10 volume ethyl acetate. The ethyl acetate was then removed under the reduced pressure at
40℃. Afterwards, the residue was dissolved in 398 ml of methanol-water(
90: 10) and chromatographed on reversed phase
HPLC. Methanol was the mobile phase. The eluent was
70 part
methanol:
16 part
water:
4 part
acetic acid with flow rate
300 ml/ min. Detection of the antibiotic components was achieved exploiting refractive index. The main peak with retention time
5 minutes contained the biological antibiotic activity which was determined via agar diffusion assay using paper discs and
Staphylococcus aureus as an indicator organism. On the other hand, the main peak was subjected to neutralization via
NaHCO3.
Myxopyronin B was extracted using
10 % V/ V Ethylene chloride. After the evaporation of the solvent, about
85 % of the remaining antibiotic substance was pure. It was noticed that the retention Time of
Myxopyronin B was
10 minutes. Molecular formula of the purified
Myxopyronin B was detected through mass spectrometer( Quadrupole mass spectrometer, Advion, USA).[
39]
Procedure of Broth dilution assay for determination of MICs of Myxopyronin B:
During testing, multiple
microtiter plates were filled with a certain broth, according to the needs of target bacteria. Varying concentrations of the antibiotics and the bacteria to be tested were then added to the plate. The plate was then placed into a non-
CO2 incubator and incubated at thirty-seven degrees
Celsius for sixteen to twenty hours. Following the allotted time, the plate was removed and checked for bacterial growth. When the broth became cloudy, bacterial growth occurred. The results of the broth microdilution method were reported in Minimum Inhibitory Concentration(
MIC), or the lowest concentration of antibiotics that stopped bacterial expansion.[
40]
Agar diffusion assay with paper discs procedure for the determination of Myxopyronin A antimicrobial activity:
The
disk diffusion method(
DDM) was classified as an
agar diffusion method(
ADM) because the test antibiotic extract to be tested diffused from its reservoir through the agar medium seeded with the test microorganism. Generally, the reservoir was a filter paper disk, which was placed on top of an agar surface. When tested extracts compounds were microbiologically active, an
inhibition zone developed around the filter paper disk after incubation. The diameter of the inhibition zone properly described the antimicrobial potency of test extract.[
41] The test microbes were isolated using either selective or enrich growth media or broth(
Table 2).
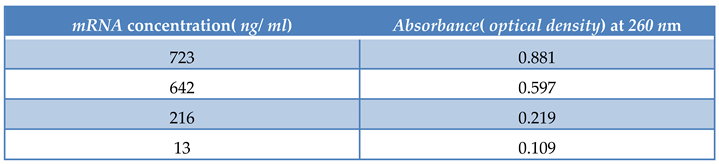
Estimation of Myxopyronin B effect on bacterial RNA synthesis:
The concentration of
RNA isolated with
RNeasy Kits( purchased from QIAGEN, USA) was determined by measuring the absorbance at
260 nm in a spectrophotometer. An absorbance of 1 unit at 260 nm corresponds to 40 µg of
RNA per ml(
A260 =
1 =
40 µg/ ml).[
42]
Estimation of Myxopyronin B effect on bacterial protein synthesis:
Absorbance was measured at
205 nm to calculate the protein concentration by comparison with a standard curve. A(
205) method could be used to quantify total protein in crude lysates and purified or partially purified protein. The
UV spectrophotometer was set to read at
205 nm allowing
15 min for the instrument to equilibrate. The absorbance reading was set to zero with a solution of the buffer and all components except the protein present. The protein solution was placed in the 1 ml cuvette and the absorbance was determined. The dilution and readings of samples were performed in duplicate.The matched cuvettes for samples and controls were utilized during the test procedure. The extinction coefficient of the protein was known, the following equation was employed.
Absorbance =
Extinction coefficient ×
concentration of protein ×
path length(
1 cm) to determine the concentration of the protein.[
43]
Estimation of pharmacodynamic and pharmacokinetic effects of Myxopyronin B during experimental animal testing in preclinical clinical trials:
In the present study, the pharmacokinetics and the pharmacodynamics of
Myxopyronin A were evaluated after dosing in male rabbit animal models weighing about
2 kg. Furthermore, compound concentrations were determined in target compartments, such as lung, kidney and thigh tissue, using
LC-MS/ MS. Based on the pharmacokinetic results, the pharmacodynamic profile of
Myxopyronin B was assessed utilizing the standard neutropenic thigh and lung infection models.[
44]
Estimation of pharmacodynamic and pharmacokinetic effects of Myxopyronin B in randomized human clinical trials phases 1/2:
This study was conducted in
150 human volunteer subjects to show the bioavailability, pharmacokinetics and the pharmacodynamics of the test antibiotic. The study was designed as randomized, single-dose,
2-treatment,
2-period crossover trial with a washout period of
1 week. Blood samples were collected at
0(
baseline),
10,
20, and
40 minutes and at
1, 1.5, 2, 3, 4, 6, 9, 12, and
24 hours postdose. Plasma concentrations of the 4 drugs were measured by using a rapid chromatography-tandem mass spectrometry method. Pharmacokinetic parameters were calculated by using noncompartmental methods. Bioequivalence was determined if the
90 % CIs of the log-transformed test/ reference ratios
AUC(
0-25),
AUC(
0-∞), and
Cmax were within the predetermined range of
80% to
125%. Tolerability was assessed by using clinical parameters and subject reports Pharmacodynamic effects were evaluated through the determination of
MICs via agar diffusion assay and broth dilution technique During randomized human clinical trials phases 1/2 all utilized infectious bacterial cell counts were estimated spectrophotometrically.[
45]
Estimation of of phototoxicity, mutagenicity and carcinogenicity of Myxopyronin B:
The phototoxicity was dictated via
3T3 neutral red uptake phototoxicity technique.[
46] On the other hand, mutagenicity and carcinogenicity of the test antibiotic were assessed using
Ames test.[
47]
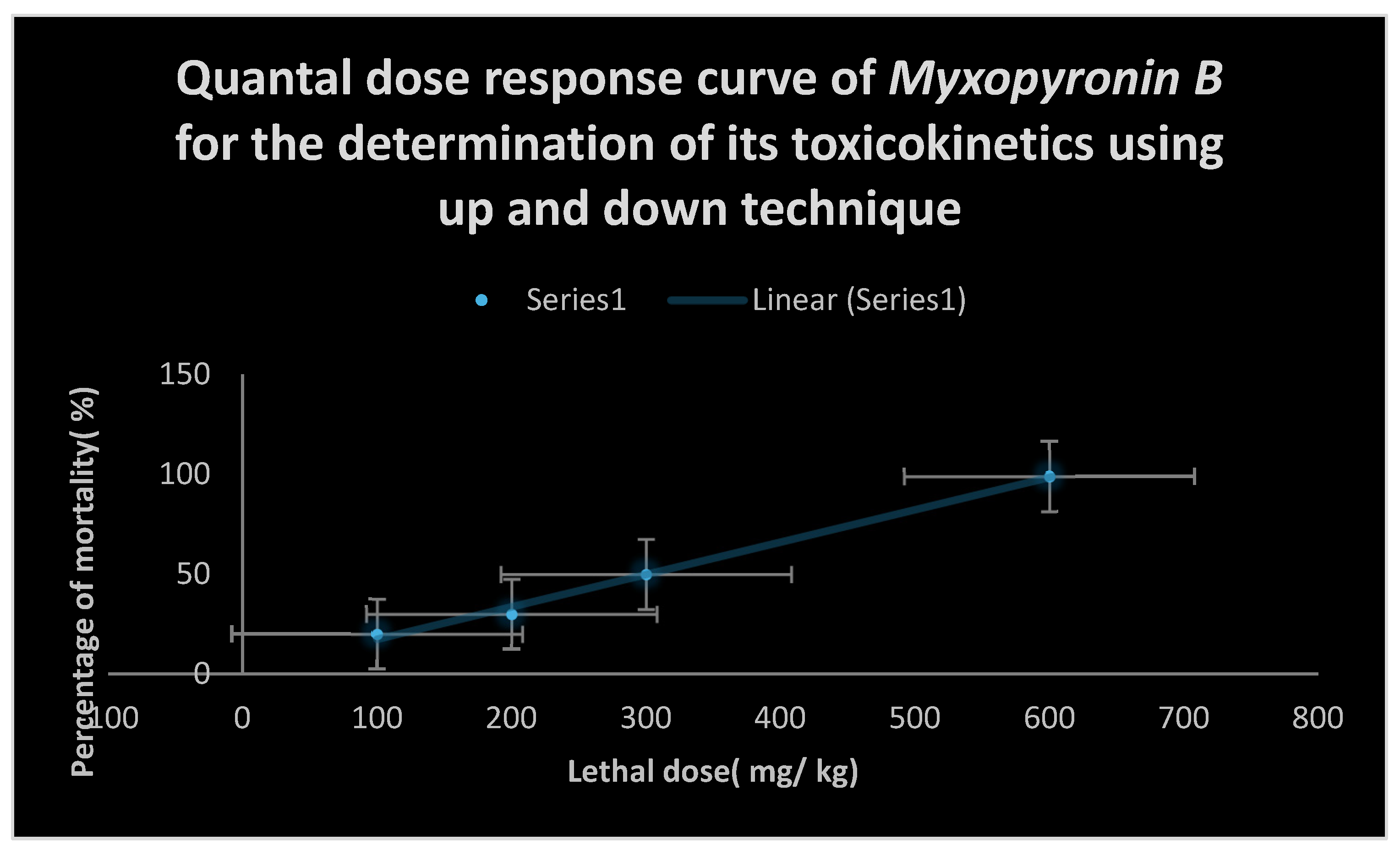
The determination of toxokinetics and toxodynamic impacts of Myxopyronin B:
Up and down method for acute toxicity detection of
Myxopyronin B was utilized for this purpose.[
48]
The determination of maximum bactericidal activity of Myxopyronin B:
A pure culture of a specified microorganism was grown overnight, then diluted in growth-supporting broth( typically
Mueller Hinton Broth) to a concentration between
1 x 10^5 and
1 x 10^6 cfu/ ml. A stock dilution of the antimicrobial test substance was made at approximately
100 times the expected
MIC. Further
1:1 dilutions were made in test tubes. All dilutions of the test antibiotic were inoculated with equal volumes of the specified microorganism. A positive and negative control tube was included for every test microorganism to demonstrate adequate microbial growth over the course of the incubation period and media sterility, respectively. An aliquot of the positive control was plated and used to establish a baseline concentration of the microorganism used.The tubes were then incubated at the appropriate temperature and duration. Turbidity indicated growth of the microorganism and the
MIC was the lowest concentration where no growth was visually observed. To determine the
MBC, the dilution representing the
MIC and at least two of the more concentrated test product dilutions were plated and enumerated to determine viable
CFU/ ml. The
MBC was the lowest concentration that demonstrated a pre-determined reduction (such as 99.9%) in
CFU/ ml when compared to the
MIC dilution.[
49]
Determination of plasma protein binding capacity of Myxopyronin B:
Using an ultrafiltration technique, the protein binding( PB) extent and changeability of the test antibiotic medicates were settled when given simultaneously to 30 patients inoculated with infectious pneumococci inside hospitals in Egypt. Clinical samples used were routinely received by microbiological laboratory inside the faculty of Pharmacy, Cairo University, Egypt. Plasma proteins were likewise plumbed. A protein-free medium was utilized to ascertain the nonspecific binding. Plasma samples from 30 patients were included, of which plasma proteins were emancipated for 24 patients.
Determination of liver, kidney and heart function tests of the test antibiotic:
These functional tests were carried out to evaluate the vitality of liver, kidney and heart during the randomized human clinical trials phases 1/2. On the other hand, Urine, stool analyses in addition to estimation of blood complete counts were performed to all experimental subjects given graded doses of Myxopyronin B.
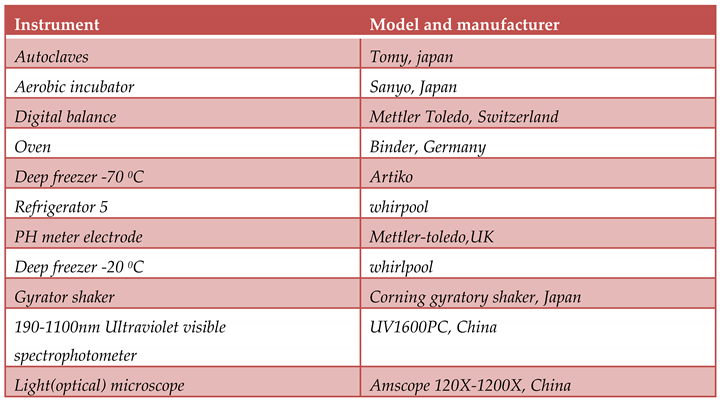
Figure 1.
It demonstrates the structure of Myxopyronin B extracted from bacterial isolates Myxococcus SDU36 collected from different soil environments in Egypt . Molecular formula of the purified test antibiotic was noticed to be C24H33NO6 determined through mass spectrometer.
Figure 1.
It demonstrates the structure of Myxopyronin B extracted from bacterial isolates Myxococcus SDU36 collected from different soil environments in Egypt . Molecular formula of the purified test antibiotic was noticed to be C24H33NO6 determined through mass spectrometer.
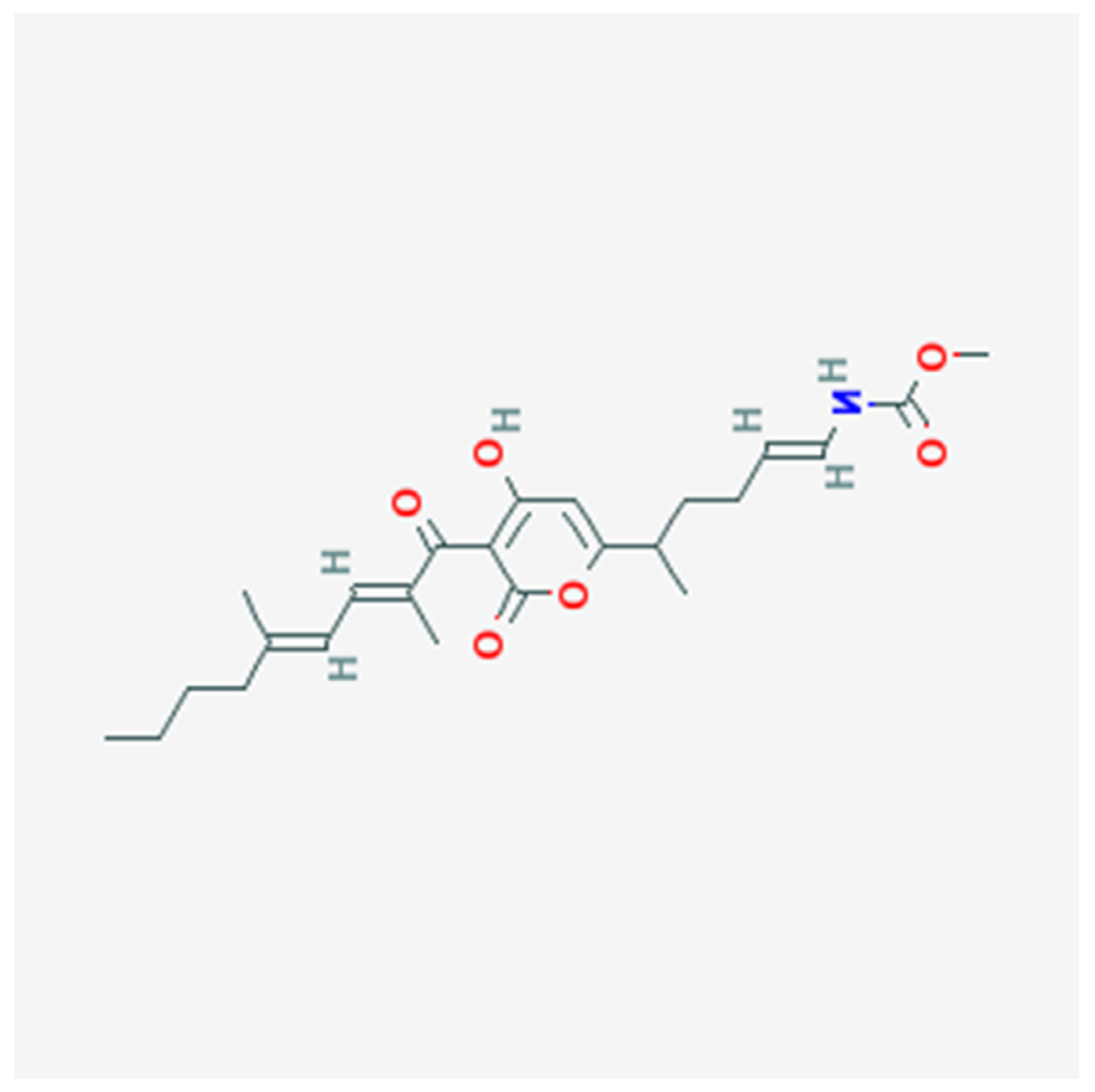
Figure 2.
It represents docking of Myxopyronin B ligand on Bacterial RNA polymerase. Myxopyronin B non-competitively showed high affinity and inhibitory effect towards the switch region. Molecular mass of Myxopyronin B was observed to be nearly 430 Da. ∆G was reached 20 joule/ mole; while Kd was observed to be nearly -290 nM.
Figure 2.
It represents docking of Myxopyronin B ligand on Bacterial RNA polymerase. Myxopyronin B non-competitively showed high affinity and inhibitory effect towards the switch region. Molecular mass of Myxopyronin B was observed to be nearly 430 Da. ∆G was reached 20 joule/ mole; while Kd was observed to be nearly -290 nM.
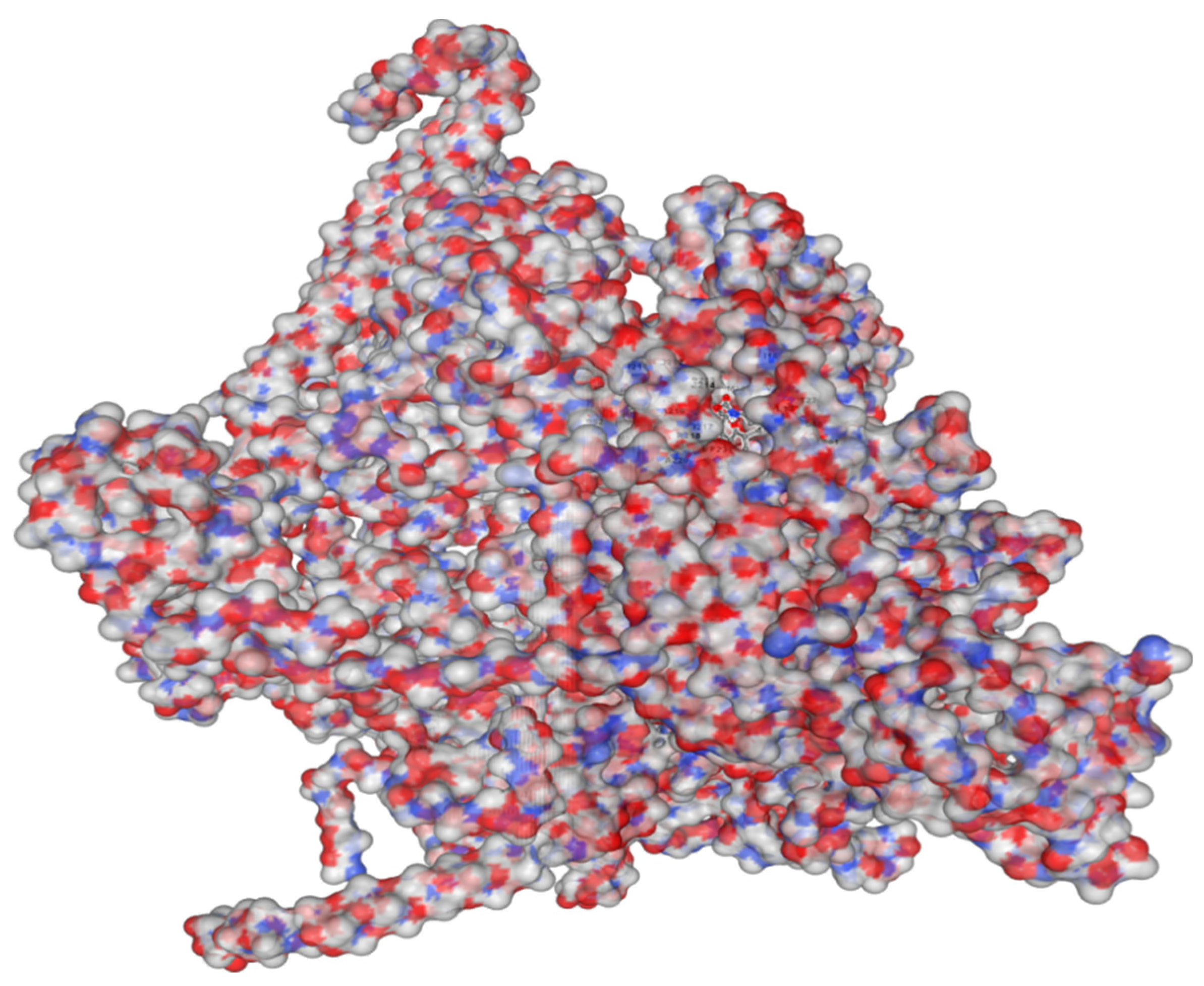
Figure 3.
It demonstrates 3D structure of bacterial prokaryotic RNA polymerase comprising the switch binding site to which Myxopyronin B Ligand strongly bound inhibiting bacterial RNA polymerase activity selectively leading to the inhibition of mRNA transcription and subsequently the mortality of the microbe. The secondary structure of RNA polymerase enzyme consisted of spiral alpha and beta sheets. Its molecular mass was approximately 198 amino-acids.
Figure 3.
It demonstrates 3D structure of bacterial prokaryotic RNA polymerase comprising the switch binding site to which Myxopyronin B Ligand strongly bound inhibiting bacterial RNA polymerase activity selectively leading to the inhibition of mRNA transcription and subsequently the mortality of the microbe. The secondary structure of RNA polymerase enzyme consisted of spiral alpha and beta sheets. Its molecular mass was approximately 198 amino-acids.
Figure 4.
It shows the impact of various concentrations of Soluble Starch on the production of Myxopyronin B.
Figure 4.
It shows the impact of various concentrations of Soluble Starch on the production of Myxopyronin B.
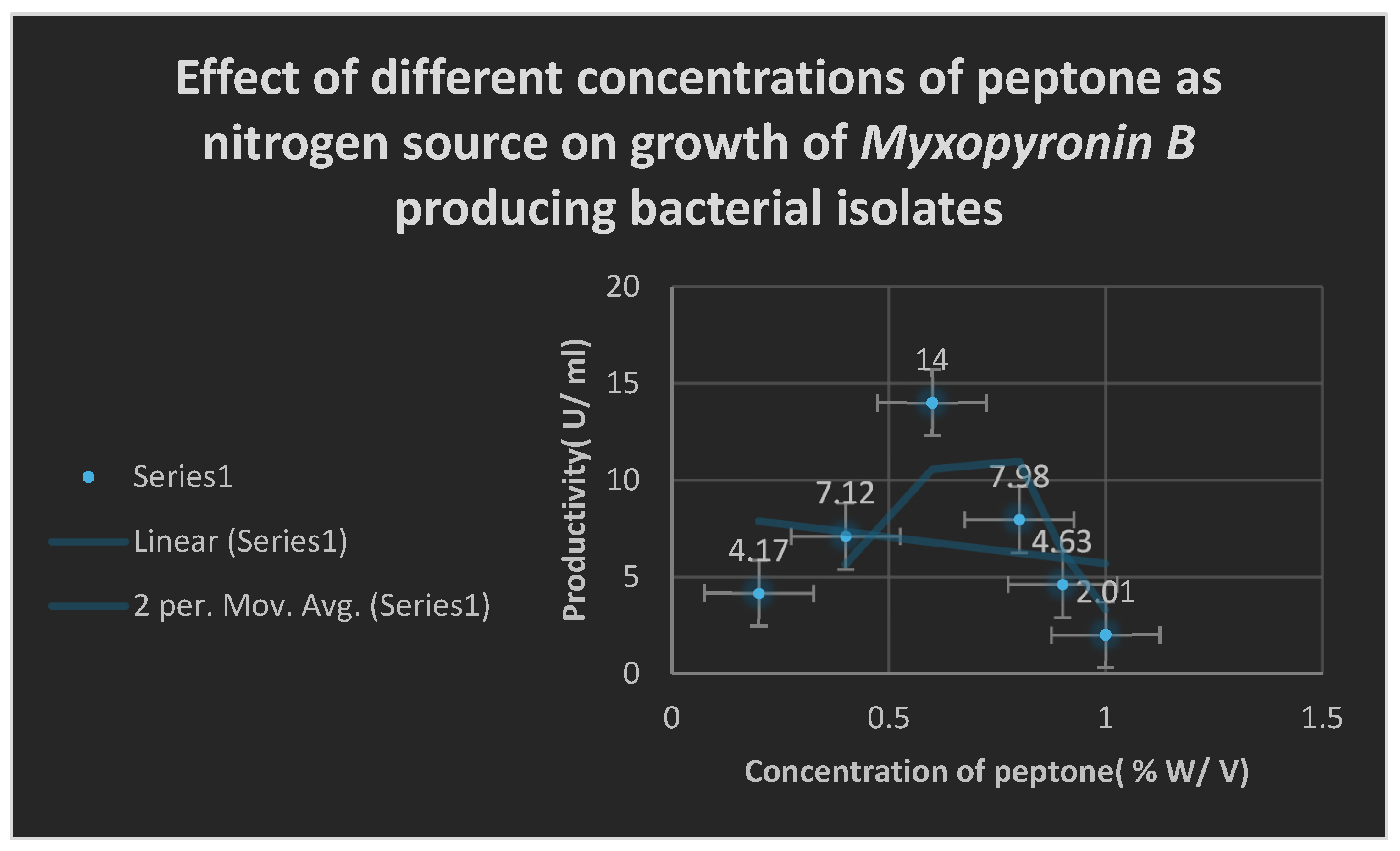
Figure 5.
It shows the effects of different Peptone concentrations as nitrogen growth factor on the productivity of Myxopyronin B.
Figure 5.
It shows the effects of different Peptone concentrations as nitrogen growth factor on the productivity of Myxopyronin B.
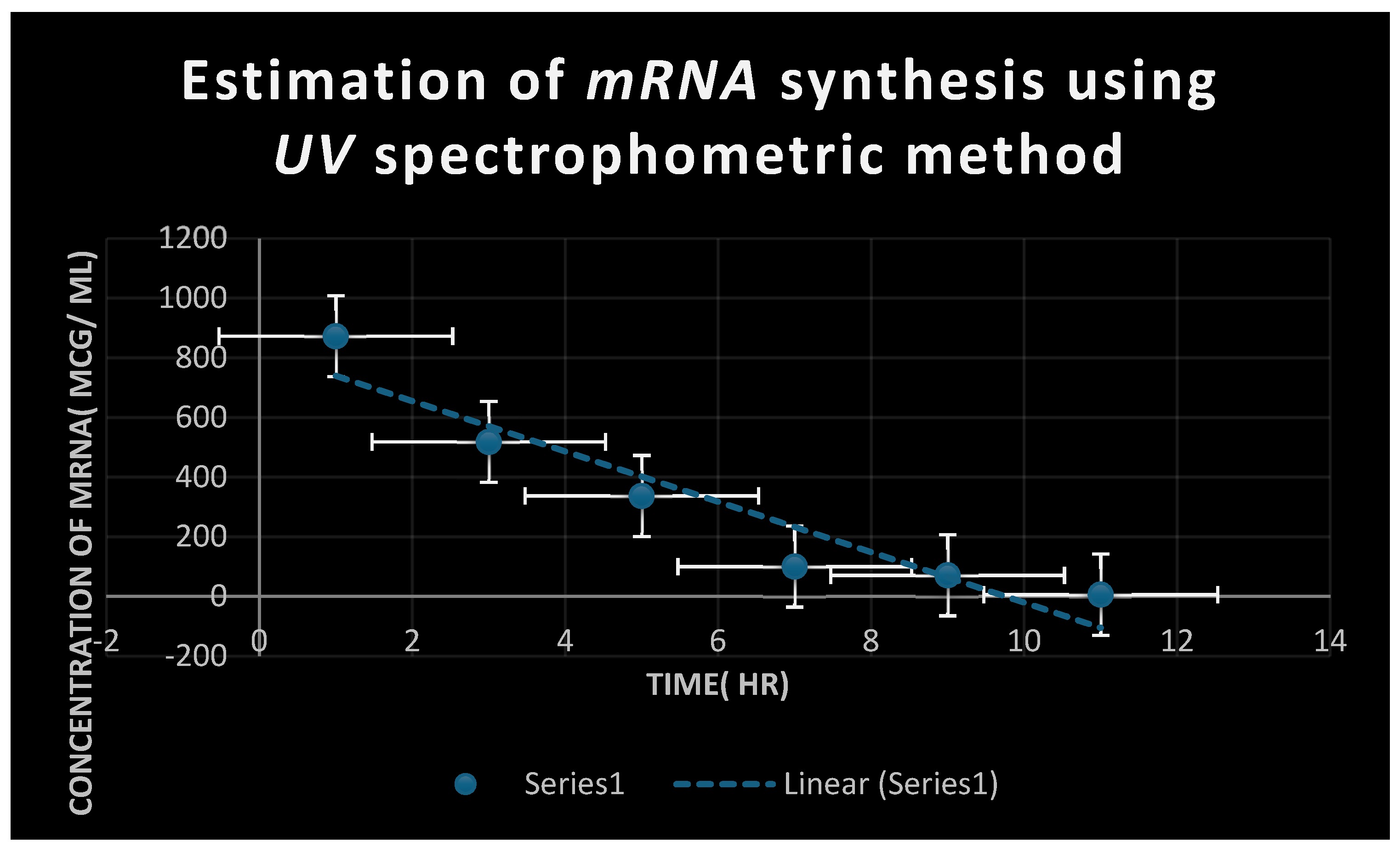
Figure 6.
It refers to the estimation of effect of Myxopyronin B on microbial mRNA productivity. mRNA synthesis was detected to be diminished proportionately up on employment of exploding doses of Myxopyronin B antibiotic.
Figure 6.
It refers to the estimation of effect of Myxopyronin B on microbial mRNA productivity. mRNA synthesis was detected to be diminished proportionately up on employment of exploding doses of Myxopyronin B antibiotic.
Figure 7.
It demonstrates the influence of Myxopyronin B on protein synthesis using UV spectrophotometer absorption at 205 nm. Protein synthesis was noticed to be decreased dramatically up on utilization of increasing doses of Myxopyronin B antibiotic.
Figure 7.
It demonstrates the influence of Myxopyronin B on protein synthesis using UV spectrophotometer absorption at 205 nm. Protein synthesis was noticed to be decreased dramatically up on utilization of increasing doses of Myxopyronin B antibiotic.
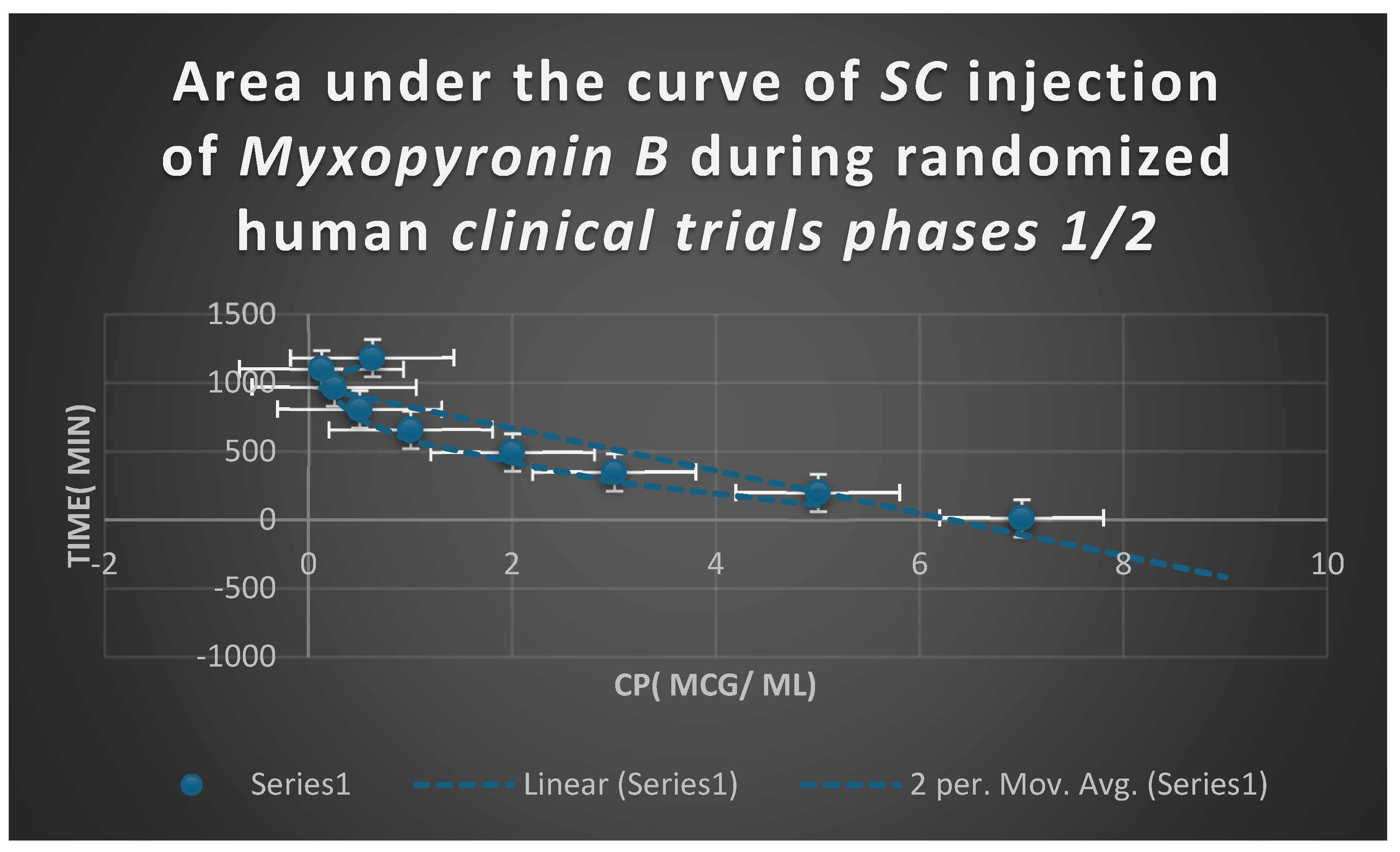
Figure 8.
It shows AUC of Myxopyronin B following SC administration in clinical trials stages 1/2. Efficacious dose ranged from 7-8 mg/ kg of body weight. Onset of action was observed following closely 15 minutes. It followed first order of elimination kinetics. Bioavailability reached nearly 92%.
Figure 8.
It shows AUC of Myxopyronin B following SC administration in clinical trials stages 1/2. Efficacious dose ranged from 7-8 mg/ kg of body weight. Onset of action was observed following closely 15 minutes. It followed first order of elimination kinetics. Bioavailability reached nearly 92%.
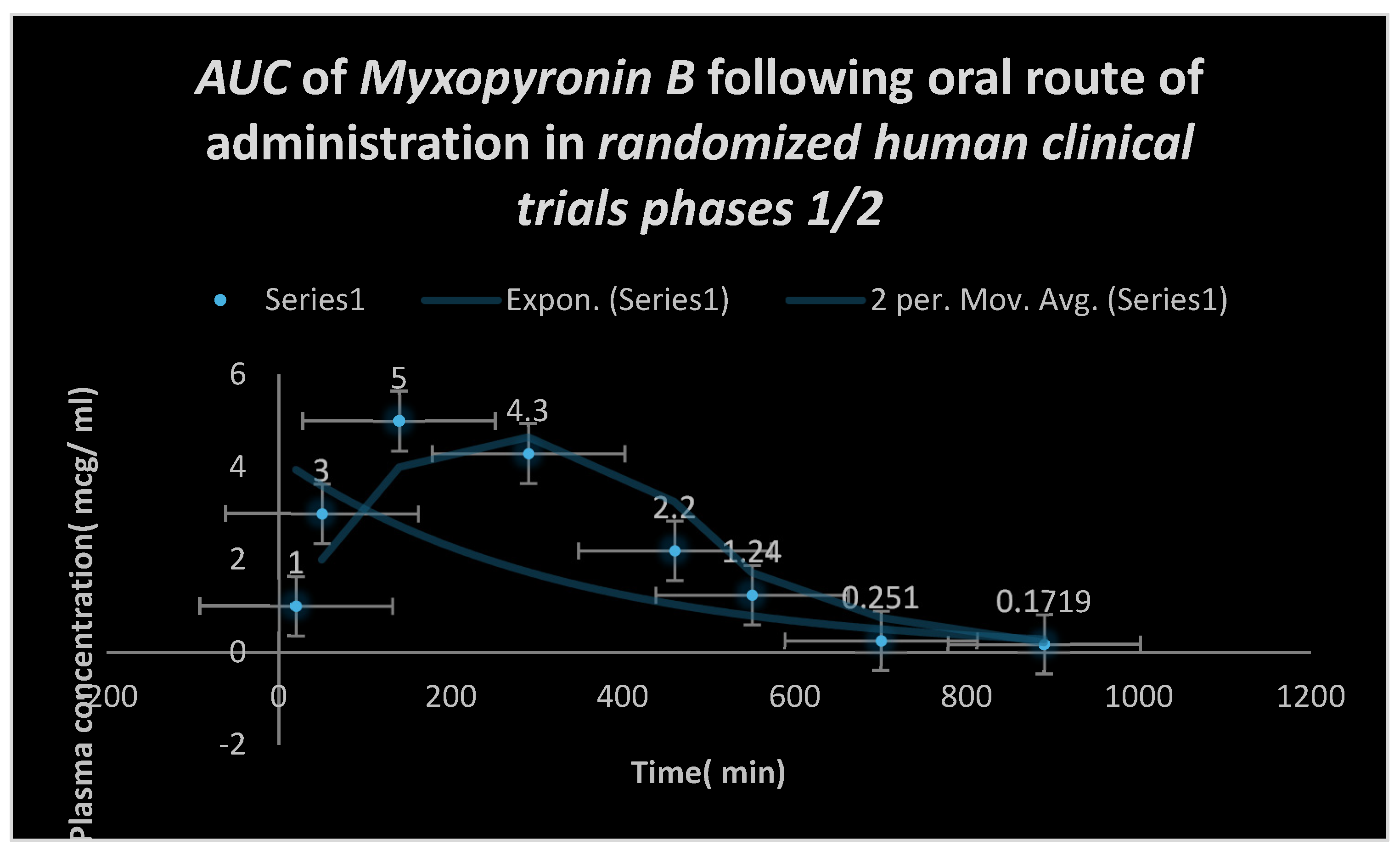
Figure 9.
Area under the curve( AUC) following oral administration of Myxopyronin B during clinical trials phases 1/2. Effective dose ranged from 9-10 mg/ kg of body weight. Onset of action was observed following nearly 28 minutes. It followed first order of elimination kinetics. Bioavailability reached about 90%.
Figure 9.
Area under the curve( AUC) following oral administration of Myxopyronin B during clinical trials phases 1/2. Effective dose ranged from 9-10 mg/ kg of body weight. Onset of action was observed following nearly 28 minutes. It followed first order of elimination kinetics. Bioavailability reached about 90%.
Results
The primary soil bacterial isolate cultivated on Casein yeast peptone plate, Myxococcus SDU36 produced the culture supernatant from which Myxopyronin B was produced. The test antibiotic reduced the growth of a few Gram-ve bacteria, including Escherichia coli, at MICs more than 100 mcg/ml, but it did not prevent the development of numerous Gram+ve bacteria at MICs lower than 100 mcg/ml. Eukaryotic cells, on the other hand, including those in humans and fungi, were unharmed. The test antibiotic’s bactericidal effect was shown by its inhibition of bacterial DNA-dependent RNA polymerase( RNLP). In phase 1/2 of randomized human clinical trials, the mean Cmax was 9–10 mcg/ml, and the mean Tmax was 1 hour when the 600 mg dosage was taken orally. T1/2 also reached 2.25 hours after first-order kinetics of elimination. It took over eight hours for it to start working after oral administration. In fewer than 7% of experimental candidates, rare toxicity in the form of mild diarrhea and GI discomfort was found during preclinical and randomized human clinical trial stages 1/2. It demonstrated around 90% affinity to plasma proteins, particularly Albumin, which led to a lasting therapeutic effect. It demonstrated an antibiotic’s concentration-dependent killing action.
The pace and amount of antimicrobial activity in the concentration-dependent killing pattern increase with drug concentration in relation to the pathogen minimum inhibitory concentration(
MIC). After the test antibiotics were refined and purified using
the reverse phase HPLC technology,
Myxopyronin B was the predominant component(
Table 4).
The 3T3 neutral red uptake phototoxicity test was used to determine the phototoxicity, and it revealed no phototoxicity. Conversely,
the Ames test was used to evaluate the mutagenicity and carcinogenicity of the test antibiotic, and the results showed no genotoxicity or carcinogenicity at all.
The quantal dosage response curve for
Myxopyronin B’s toxicokinetics is shown in
Figure 10. It was discovered that
LD50% was
300 mg/kg and
LD99% was over
600 mg/kg. Using a stereomicroscope,
Figure 11 depicts
Myxococcus SDU36 bacterial isolates on
CYP isolation plates secreting the antibiotic
Myxopyronin B.
Table 3.
It shows the distribution of Myxopyronin B producing bacterial isolates:.
Table 3.
It shows the distribution of Myxopyronin B producing bacterial isolates:.
| No of +ve bacterial isolates producing Myxopyronin B |
No of -ve bacterial isolates producing Myxopyronin B
|
| 42 |
58 |
Table 4.
It demonstrates the degree of purity of test antibiotics following the purification via reversed phase HPLC technique:.
Table 4.
It demonstrates the degree of purity of test antibiotics following the purification via reversed phase HPLC technique:.
| Test antibiotic |
Degree of purity( %) |
| Myxopyronin A |
15 |
| Myxopyronin B |
85 |
Table 5.
It demonstrates 16 S rRNA detection of Myxopyronin B producing isolates using BLASTn software:.
Table 5.
It demonstrates 16 S rRNA detection of Myxopyronin B producing isolates using BLASTn software:.
| Description |
Scientific Name |
Max Score |
Total Score |
Query Cover |
E value |
Per. ident |
| Myxococcus sp. MH1 DNA, complete genome |
Myxococcus sp. MH1 |
525 |
1051 |
99% |
3.00E-144 |
94.94 |
| Myxococcus sp. SDU36 chromosome, complete genome |
Myxococcus sp. SDU36 |
436 |
870 |
99% |
1.00E-117 |
90.15 |
| Myxococcus hansupus strain mixupus chromosome, complete genome |
Myxococcus hansupus |
126 |
126 |
65% |
3.00E-24 |
77.23 |
| Cystobacter fuscus strain DSM 52655 chromosome, complete genome |
Cystobacter fuscus |
124 |
124 |
54% |
1.00E-23 |
78.92 |
| Cystobacter fuscus strain Cbf 8 chromosome, complete genome |
Cystobacter fuscus |
124 |
124 |
54% |
1.00E-23 |
78.92 |
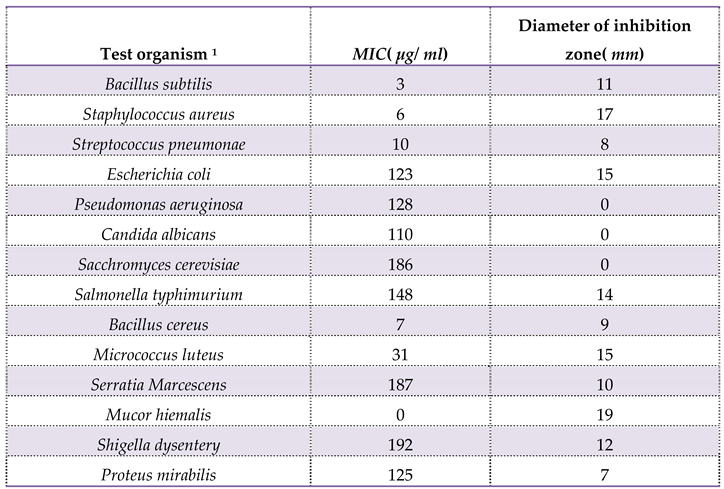
Table 6.
It shows the estimation of zones of inhibition and minimum inhibitory concentrations of Myxopyronin B via Agar diffusion assay using paper discs:.
Table 6.
It shows the estimation of zones of inhibition and minimum inhibitory concentrations of Myxopyronin B via Agar diffusion assay using paper discs:.
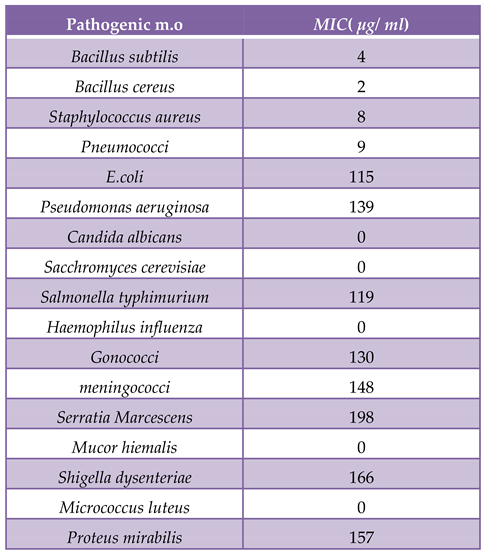
Table 7.
It demonstrates MICs of Myxopyronin B on different microorganisms using broth microdilution technique:.
Table 7.
It demonstrates MICs of Myxopyronin B on different microorganisms using broth microdilution technique:.
Table 8.
It demonstrates Minimum bactericidal concentrations( MBCs) of Myxopyronin B on different microorganisms using broth microdilution technique:.
Table 8.
It demonstrates Minimum bactericidal concentrations( MBCs) of Myxopyronin B on different microorganisms using broth microdilution technique:.
Table 9.
It shows the estimation of mRNA quantity via UV spectrophotometer at 260 nm after addition of Myxopyronin B:.
Table 9.
It shows the estimation of mRNA quantity via UV spectrophotometer at 260 nm after addition of Myxopyronin B:.
Table 10.
It shows the effect of Myxopyronin B on the microbial protein synthesis using UV spectrophotometer at 205 nm:.
Table 10.
It shows the effect of Myxopyronin B on the microbial protein synthesis using UV spectrophotometer at 205 nm:.
| Bacterial protein concentration( mcg/ ml) |
Time( min) |
| 80.2 |
60 |
| 31.56 |
180 |
| 21.08 |
300 |
| 2.85 |
450 |
| 0.03 |
720 |
Table 11.
The resolution of biochemical reactions:.
Table 11.
The resolution of biochemical reactions:.
Table 9 and
Table 10, respectively, show that there was a substantial reduction in protein synthesis and
mRNA synthesis as the dosage of
Myxopyronin B was increased. Docking experiments with the
MCULE and
SWISS DOCK software showed that the test antibiotic’s mode of action was most likely caused by inhibiting
RNA polymerase by binding to its switch region. The test antibiotic’s high
∆G was found to be around
20 J/mol using the
SWISS model software. However, utilizing
SWISS MODEL software, it was discovered that the test antibiotic’s low
Kd near the switch area was around
-290 nM.
Table 11 provides a summary of the biochemical profile and morphology of the strong bacterial isolates used in this investigation to produce the test antibiotic.
Myxococcus SDU36 was the most common bacterial isolate found to be secreting the extracellular test antibiotic, according to its morphology and biochemical responses. The study had
150 human volunteers in total, with a mean age of
28.1[
8.7] years(
SD). The
90% confidence intervals(
CIs) for the long transformed ratios of
Cmax,
AUC(
0-25), and
AUC(
0-∞) for the test antibiotic were, respectively,
89.2 to
95.3,
88.2 to
96.1, and
90.8 to
93.4. For
Myxopyronin B, the mean protein binding(
PB) was found to be around
90%. It was shown that albumin exhibited the predominant protein binding for both
Rifampicin and
Myxopyronin B. The therapeutic activity was discovered to be attributed to the unbound fraction. The structure of
Myxopyronin B, which was isolated from bacterial isolates of
Myxococcus SDU36 collected from various soil habitats in Egypt, is depicted in
Figure 1. Using a mass spectrometer, the molecular formula of the purified test antibiotic was found to be
C24H33NO6. The area under the curve(
AUC) after oral
Myxopyronin B dosing throughout
phases 1/2 of
clinical trials is displayed in
Figure 9. The range of the effective dosage was
9–10 mg/kg of body weight. The first signs of activity( onset of action) were noted after about
28 minutes. It adhered to
the kinetics of first order elimination. The location of bacterial isolates that produce
Myxopyronin B is displayed in
Table 3. The resolution of biological reactions is shown in
Table 11.
Table 10 uses a
UV spectrophotometer set at
205 nm to illustrate how
Myxopyronin B affects the synthesis of microbial proteins.
Table 8 uses the broth microdilution technique to show the minimum bactericidal concentrations(
MBCs) of
Myxopyronin B on various bacteria. The estimation of
Myxopyronin B’s impact on microbial
mRNA productivity is shown in
Figure 6. An increase in the dosage of the antibiotic
Myxopyronin B was found to cause a commensurate decrease in
mRNA production. Following the administration of
Myxopyronin B,
Table 9 displays the estimation of
mRNA quantity using a
UV spectrophotometer at
260 nm.
Table 7 shows
the broth microdilution technique’s minimum inhibitory concentrations(
MICs) for several bacteria.
Table 6 illustrates how
the Agar diffusion assay, which uses
paper discs, was used to estimate the zones of inhibition and lowest inhibitory doses of
Myxopyronin B.
Table 5 shows how to use
BLASTn software to detect isolates that produce
Myxopyronin B using
16S rRNA. The range of bacterial isolates that produce
Myxopyronin B is displayed in
Table 3. Using a stereomicroscope,
Figure 11 depicts
Myxococcus SDU36 bacterial isolates on
CYP isolation plates secreting the antibiotic
Myxopyronin B. The quantal dosage response curve for
Myxopyronin B’s toxicokinetics is shown in
Figure 10. It was discovered that
LD50% was
300 mg/kg and
LD99% was over
600 mg/kg. The structure of
Myxopyronin B, which was isolated from bacterial isolates of
Myxococcus SDU36 collected from various soil conditions in Egypt, is depicted in
Figure 1.
Using a mass spectrometer, the molecular formula of the purified test antibiotic was found to be
C24H33NO6. The area under the curve(
AUC) after oral
Myxopyronin B dosing during
phases 1/2 of clinical trials is shown in
Figure 9. The range of the effective dose was
9–10 mg/kg of body weight. The onset of actions were noted after almost
28 minutes. It adhered to the kinetics of first order elimination.
The AUC of
Myxopyronin B after
SC injection in
phases 1/2 of clinical trials is displayed in
Figure 8. The range of effective doses was
7-8 mg/kg of body weight. The beginning of the action was noted after a close
15 minutes. It adhered to the kinetics of first order elimination.
Figure 4 illustrates how different soluble starch concentrations affect the synthesis of
Myxopyronin B.
Figure 7 uses the
UV spectrophotometer absorption at
205 nm to illustrate how
Myxopyronin B affects protein production. A significant reduction in protein synthesis was seen upon administration of escalating dosages of the antibiotic
Myxopyronin B.
The 3D structure of bacterial prokaryotic
RNA polymerase is shown in
Figure 3. It includes the switch binding site, to which
Myxopyronin B Ligand binds strongly and inhibits bacterial
RNA polymerase activity selectively, thereby inhibiting
mRNA transcription and ultimately causing the microbe to die.
Alpha and
Beta spiral sheets made up the
RNA polymerase enzyme’s secondary structure. It had a molecular mass of about
198 amino acids. The docking of the
Myxopyronin B ligand on Bacterial
RNA polymerase is shown in
Figure 2. High affinity and an inhibitory action were demonstrated by
Myxopyronin B towards the switch region.
Discuss
The in vitro and in vivo antimicrobial activity of
Myxopyronin B, a novel antibiotic was evaluated in the present study. It demonstrated excellent bactericidal activity against a broad spectrum of
G +ve bacteria with
MICs did not exceed
20 mcg/ ml. On the other hand It showed few bactericidal activities against
G -ve bacteria.with minimal inhibitory concentrations were greater than
100 mcg/ ml. Its mechanism of action was realized during the investigation of
RNA synthesis to be via the inhibition of prokaryotic
DNA-dependant-RNA polymerase; whereas no inhibitory impact was observed for Eukaryotic one. Docking studies through
SWISS DOCK software confirmed this as well. The antibiotic activities
Myxopyronin A and
B were isolated from the culture supernatant of
29 bacterial isolates of Myxobacterium
Myxococcus SDU36 detected molecularly using
16 S rRNA technique(
Table 3).
The antibiotic activity did not inhibit the growth or kill eukaryotic cells such as human and fungal cells reflecting selectivity towards the inhibition of the growth of prokaryotic bacterial cells. This selectivity effect minimized the adverse effects noticed during the present study. Docking studies via
SWISS DOCK software revealed that desmethylation of either
Myxopyronin A or
B enhanced its biological activity. Purification was performed through reversed phase
HPLC.
Myxopyronin B was the main refined antibiotic. Its purity degree reached approximately
85 %; while, the remaining purified antibiotic was detected to be
Myxopyronin A. The antibacterial activity was assessed via the determination of
MICs of the test antibiotics using the agar diffusion technique utilizing paper discs
5 mm in diameter and the broth dilution assay. The initial density of each test microorganism was about
105/ ml of the culture suspension. The mean
MICs of test antibiotic against
G +ve bacteria ranged from
5 to
20 mcg/ ml; Whereas
MICs reached above
100 mcg/ ml against some selected
G -ve bacteria. On the other hand no effect was detected against the growth of fungi and yeasts. (
Irschik H et al., 1983) stated that
myxovalargin A was a novel peptide antibiotic isolated from the culture supernatant of the
myxobacterium Myxococcus fulvus strain Mx f65. It was active against
Gram-positive bacteria(
MIC 0.3 approximately
5 micrograms/ ml), at higher concentrations also against Gram-negative ones(
MIC 6 approximately 100 micrograms/ ml), and not at all against yeasts and molds. Its mechanism of action involved the inhibition of the bacterial protein synthesis.[
50] According to( Glaus F et al., 2018)
Ripostatin, a novel antibiotic, isolated from the culture supernatant of
Myxobacterium,
Sorangium cellulosum strain So ce377. On the other hand it interfered of the bacterial
RNA synthesis.[
51] On the other hand,
Myxopyronin A was found to be structurally related to α-pyrone antibiotics from
myxobacteria. Its ability to inhibit
RNA polymerase was through interaction with the switch region of
RNA polymerase; while
Rifampicin inhibited the same enzyme through different region.[
52] Myxopyronin showed no phototoxicity and mutagenicity in rabbit animal models during
the preclinical trials stage, in the present study. Rare adverse effects including mild diarrhea and cholestatic jaundice were reported in less than
5 % of the experimental subjects received the test antibiotics during
randomized human clinical trials phases 1/2. The biological half life of
Myxopyronin A reached approximately
2.5 hours.
0.6 % peptone and 8
% soluble starch were detected to be the optimal nitrogen and carbon growth factors for bacterial isolates producing the test antibiotics, respectively(
Figure 4 and
Figure 5). High
∆G of the test antibiotic was observed to be approximately
20 J/ mole as determined via
SWISS MODEL software reflecting high catalytic activity of the test antibiotic towards the switch region. On the other hand, low
Kd of the test antibiotic towards the switch region was found to be approximately -
290 nM using
SWISS MODEL software indicating high affinity and binding capacity. Bioavailability studies were performed using
HPLC during
randomized human clinical trials phases 1/2 revealed that
Myxopyronin B reached nearly
90% oral bioavailability,
92% IM bioavailability and
100% IV bioavailability. Metabolic studies using
HPLC revealed that the test antibiotic showed no in vivo induction of hepatic metabolizing C
ytochrome P450 enzymatic system; while rifampicin induced
CYP3A4 hepatic metabolizing enzyme potently. Up and down procedure intended for the evaluation of acute toxicity profile of the test antibiotic showed that
LD50% was about
200 mg/ kg body weight; while
LD99% reached
300 mg/ kg. On the other hand, therapeutic margin of the test antibiotic ranged from
7 mcg/ ml to
100 mcg/ ml.
Myxopyronin A producing bacterial isolates were gram negative, spore forming
obligate aerobes and
chemoorganotrophic. They were
elongated rods with
tapered ends. No
flagella were present; but the cells moved via
gliding. They fermented
Tween 80,
starch and
casein. On the other hand they were positive for
catalase while negative for
oxidase tests. They reduced
nitrates
And were able to grow at
10-37 ℃. A total of
150 human subjects( mean
SD age,
27.3[
9.8] years were enrolled and completed the study. The
90% confidence intervals(
CIs) for the long transformed ratios of
Cmax,
AUC(
0-25), and
AUC(
0-∞) for the test antibiotic were, respectively,
89.2 to
95.3,
88.2 to
96.1, and
90.8 to
93.4. The point estimates for
Cmax in the present study were outside the limit for bio-equivalence for rifampicin standard drug.
The mean PB was observed for Myxopyronin B which approximated
90% while that of
Rifampicin reached
88%.[
53] It was noticed that plasma protein binding was proportionally increased with increasing the doses of the test antibiotic. The plasma protein binding participated in extending the
Myxopyronin B duration of action. The major protein binding for
Myxopyronin B and
Rifampicin was noticed to be albumin. The unbound fraction was detected to be responsible for the therapeutic activity.