1. Introduction
Early detection and diagnosis of cancer improves patient prognosis and potential for successful treatment. In the United States, the 5-year survival rate is 86% for localized head and neck cancers but decreases to 69% for regional cancers and 40% for distant metastatic cancers [
1]. Unfortunately, only 28% of head and neck cancers are detected at the localized stage [
2]. Screening methods consist primarily of incisional biopsy and histopathologic examination, which is a burden on both the patient and the healthcare system. The most common treatment for oral cancer is surgical resection; this procedure can result in devastating physiological and psychological effects [
3,
4,
5].
The multi-step progression of healthy oral mucosa through grades of dysplasia to cancer is very well understood. Dysplastic changes typically originate just above the basement membrane, a thin acellular layer separating the superficial epithelial tissue from the deeper stromal tissue [
6]. The World Health Organization (WHO) has identified architectural (presence and degree of epithelial stratification), and cytological (cellular atypia) changes as key indicators of dysplastic progression [
7]. Malignant lesions are classified by having breached the basement membrane, surpassing the barrier preventing the spread of cancerous cells into connective tissue, and allowing for potential metastasis [
8]. The most prevalent invasive tumor is oral squamous cell carcinoma (OSCC), accounting for over 90% of oral tumors [
9]. There are several structural biomarkers for invasive cancer accessible through histological staining, however ensuring that a biopsy sample contains the most pathologic tissue is difficult. Multiple biopsies are often taken to reduce false negatives as the clinical presentation of benign lesions may appear similar to occult lesions [
10].
Optical coherence tomography (OCT) is a volumetric imaging technique that generates images through reconstruction of backscattered light from a low coherence source. While the most widespread clinical application of OCT is retinal imaging [
11,
12], the utility of OCT as an adjunct screening tool for oral cancer has been previously explored [
13,
14,
15,
16]. OCT allows for non-invasive
in vivo measurement of epithelial thickness and visualization of architectural changes relating to stratification and structure within the oral cavity [
17,
18,
19]. Bridging the resolution-gap between ultrasound and microscopy, OCT has an axial resolution of ~5-10 μm, providing information at the microstructure level that was previously only available through biopsy, as morphological features imaged in OCT are strongly correlated to those observed in histology [
20]. The primary limitation of OCT is a shallow imaging depth, generally collecting data up to 2-3 mm into tissue. Yet, this depth is comparable to that of histological data collection, making it an excellent tool for examining changes to near-surface tissue [
21].
Clinical adoption of oral OCT requires data analysis tools that can provide rapid and reproducible assessment of tissue morphology, as the large volume of data collected during imaging makes manual assessment intractable. This work proposes applying deep learning methodologies for automated assessment of OCT data to extract tissue layer stratification. The intersection of deep learning and image analysis has been documented in OCT applications, with substantial evidence indicating utility in image segmentation [
22,
23,
24,
25,
26] and image classification [
27,
28,
29] tasks. We build upon previously presented classical methods for segmentation of oral OCT [
30], which were limited in clinical applicability due to poor generalizability and lengthy processing times. There is a gap in the existing literature for image analysis of oral OCT, where no pathology agnostic, site agnostic, rapid and repeatable tool exists to identify structures of interest. We posit that this tool should
not provide diagnostic suggestions, but instead empower clinical decision-making by providing additional data through easily interpreted visualization of subsurface morphology.
2. Materials and Methods
2.1 Imaging System
Images were collected using a custom-built swept-source OCT system. The system, described previously [
15], employes a 1310 ± 50 nm laser (Axsun Technologies) to achieve ~7 μm axial resolution in tissue. A helical scanning pattern is facilitated using a rotary pullback device, which collects images up to 90 mm in length, thus allowing large tissue sites to be collected in a single scan. A single-mode fiber delivers light to and collects light from the sample; during
in vivo imaging, the optical fiber is packaged into a 1.5 mm diameter catheter which is filled with water to provide refractive index matching and reduce friction during rotation. Two catheter sheath holders were developed to allow imaging of various sites in the oral cavity: a modified dental mirror and a modified saliva injector.
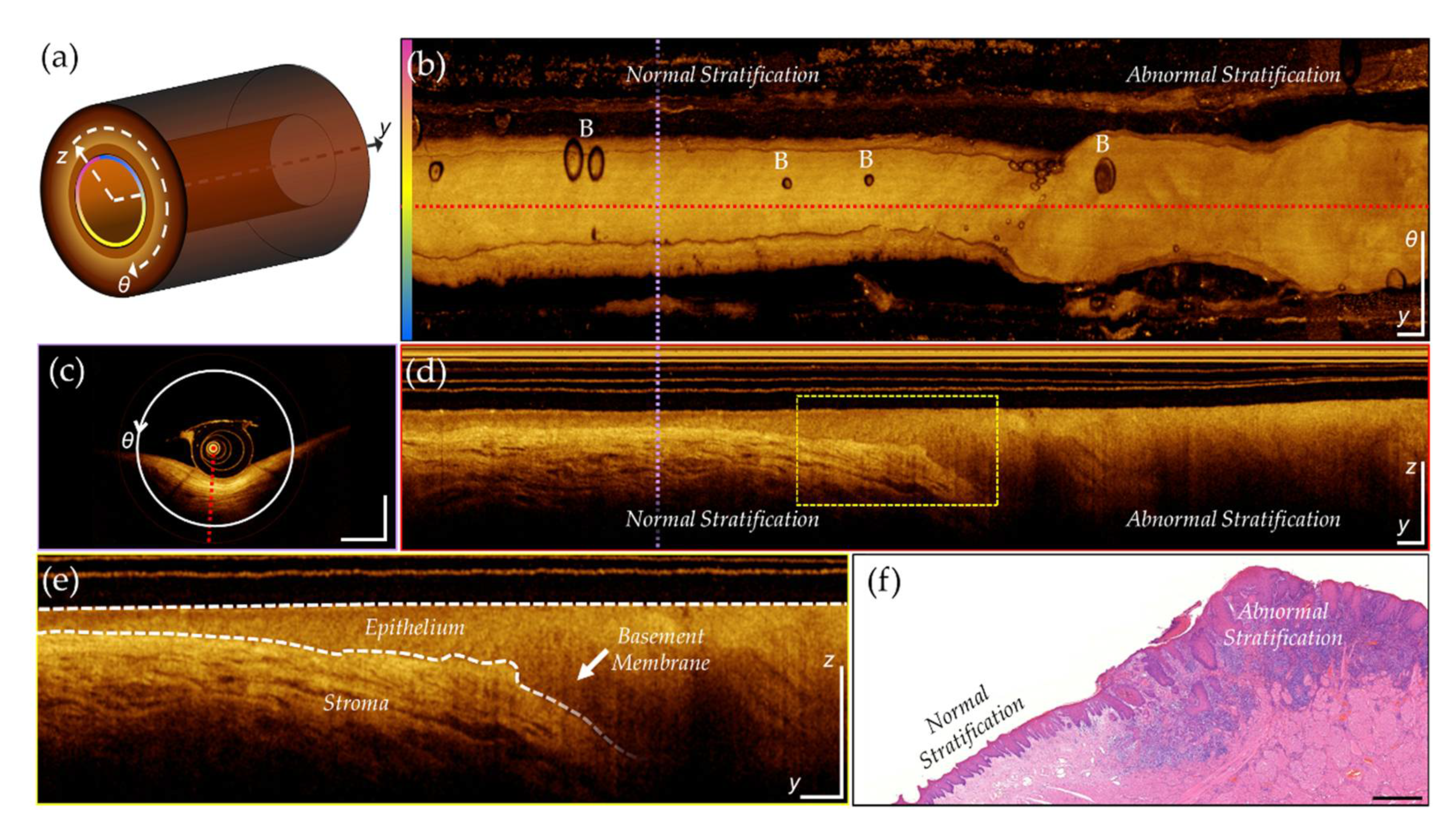
Images are acquired in a 3-dimensional cylindrical coordinate system (
Figure 1) that includes radial (
z), azimuthal (
θ), and pullback (
y) axes. Unwrapping the volume along the azimuthal axis and applying a mean intensity projection along the radial (A-line) axis creates a 2-dimensional
en face projection, shown in (b). Slicing the volume perpendicular to the pullback axis, at the purple dashed line, provides the cross-section shown in (c). Slicing perpendicular to the azimuthal axis, at the red dashed line, provides the longitudinal view, shown in (d). A magnified inset (yellow dashed box) is shown in (e). The epithelial surface and basement membrane are identified by the white dashed line, highlighting biomarkers of interest for oral cancer visualized through OCT: epithelial thickening and changes in stratification. Co-registered features can be seen in the histology slice in (f), depicting regions of normal and abnormal tissue. These features can be observed in the longitudinal image but are challenging to identify in the
en face projection. Water-filled catheters sometimes introduce air bubbles into the optical pathway. Air bubbles can be observed in the
en face (
Figure 1 (b), indicated with ‘B’), longitudinal and cross section views, and may obscure the tissue underneath.
2.2 Data Collection and Assembly
In vivo imaging of the oral mucosa was approved by the Research Ethics Board of the University of British Columbia and the British Columbia Cancer Agency (H11-02516). Images used in this study were collected from 2014-2017. The most pathologic site was identified, and one to six scans were performed over the lesion (including some tissue before and after the lesion when possible); a contralateral pullback was also taken when possible. If deemed clinically necessary, a biopsy was performed after image collection to confirm diagnosis, which could be co-registered to the OCT.
For this study, 184 volumetric scans were selected from 60 patients (34 male, 26 female). The mean age (M) was 62 years (standard deviation, SD = 14.3). Visual analysis was used to ensure good OCT quality by minimizing the presence of imaging artifacts (≤ 40% of image). Scans were required to be ≥ 30 mm in length, with pullback speeds ≤ 10 mm/s and azimuthal scan rates of 100 Hz. Each scan contained 504-512 longitudinal images. One patient was held out of the discovery sets for whole-volume evaluation. Up to three longitudinal images (minimum azimuthal separation of 15°) were selected from the remaining scans for annotation. Images included a variety of sites and pathologies to encourage robustness and generalizability, summarized in
Table 1 and
Table 2.
2.3 Rater Annotations
Supervised deep learning models were used in this study, and thus the discovery set required ground truth reference data. Annotations were generated by five raters experienced with analyzing OCT. Manual segmentation of the (1) epithelial surface, (2) basement membrane, and (3) imaging artifacts was completed using in-house annotation software. Artifacts such as air bubbles cause a decrease or complete loss of image intensity and may confound other processing steps. Each image was annotated by three randomly assigned raters. Data was anonymized prior to distribution, blinding raters to identifiers and disease status. A single rater combined these impressions to generate a single reference annotation for each image. Images with high inter-rater disagreement were discussed and a consensus annotation was created in a panel review session.
2.4 Pipeline Architecture
A three-step automated pipeline was built to pre-process the volumetric scans, generate predictions via four deep learning networks, and post-process predictions and synthesize for visual analysis. The second step of the pipeline employed the following networks:
Field-of-view (FOV) detection. A convolutional neural network (CNN) was used to predict either complete tissue contact, or partial/no tissue contact for each longitudinal image.
Artifact detection. A CNN was used to classify any regions that contained artifacts (bubbles, sheath markers) that might lead to incorrect segmentation predictions.
Surface segmentation. A shallow u-net was used to segment the (epithelial) tissue surface.
Basement membrane segmentation. A shallow u-net was used to segment the basement membrane.
Post-processing steps are unique to individual tasks and described below. Predictions are presented as thickness maps which provide information about changes to epithelial thickening, stratification, and presence of imaging artifacts. Pre- and post-processing methods were completed in MATLAB. Networks were implemented with PyTorch framework using NVIDIA Cuda v11.4 and Python 3.6.9. All experiments were performed on a Windows 10 operating system, with CPU Intel Core i7-4770 3.40 GHz, GPU NVIDIA GeForce GTX 1660, and 32 GB of RAM.
2.5. Data Preparation and Augmentation
Longitudinal images were averaged in the azimuthal direction (out of plane, 5-pixel average) and resampled for isotropic pixel size (10 µm square in tissue). After resampling, images were 382 pixels (3.82 mm) high and 4000 pixels (4 cm) to 9000 pixels (9 cm) wide, depending on the pullback length. The logarithmic intensity (dB) of each image was scaled between the OCT noise floor and the maximum intensity of the image. Images were partitioned into overlapping square tiles to create uniform, memory-aware input information for model training.
The discovery sets are summarized in
Table 3. As the classification task required less contextual information, classification tiles were smaller (128 x 128) to allow faster training. Conversely, segmentation tiles were selected to be the maximum base-2 size (256 x 256) without resampling. The deepest 126 pixels contained no relevant information due signal attenuation and were discarded from each image. Tiles were overlapped (by half their width) to encourage attention at both the left and right side of the image and increase the amount of data available for training.
In the FOV detection task, longitudinal images were randomly selected from a subset of 9 volumetric scans. Images with no tissue present (no probe-tissue contact) were defined as class 0 while those with tissue present (probe-tissue contact over the entire width of the image) were defined as class 1. Images with partial tissue contact were rejected. Similarly, for the artifact detection task, images with no artifacts were defined as class 0 while those with artifacts were defined as class 1. Training, tuning, and test images for this task were selected from the pool of annotated images. Tiles with small artifacts (<30% of the tile) occurring at the edge of the tile were discarded. Segmentation tasks also used annotated images for training, with annotations being converted to ground truth masks. Prior to tiling, images were cropped to remove any regions that did not have an epithelial surface annotation.
2.6. Convolutional Neural Network Architectures
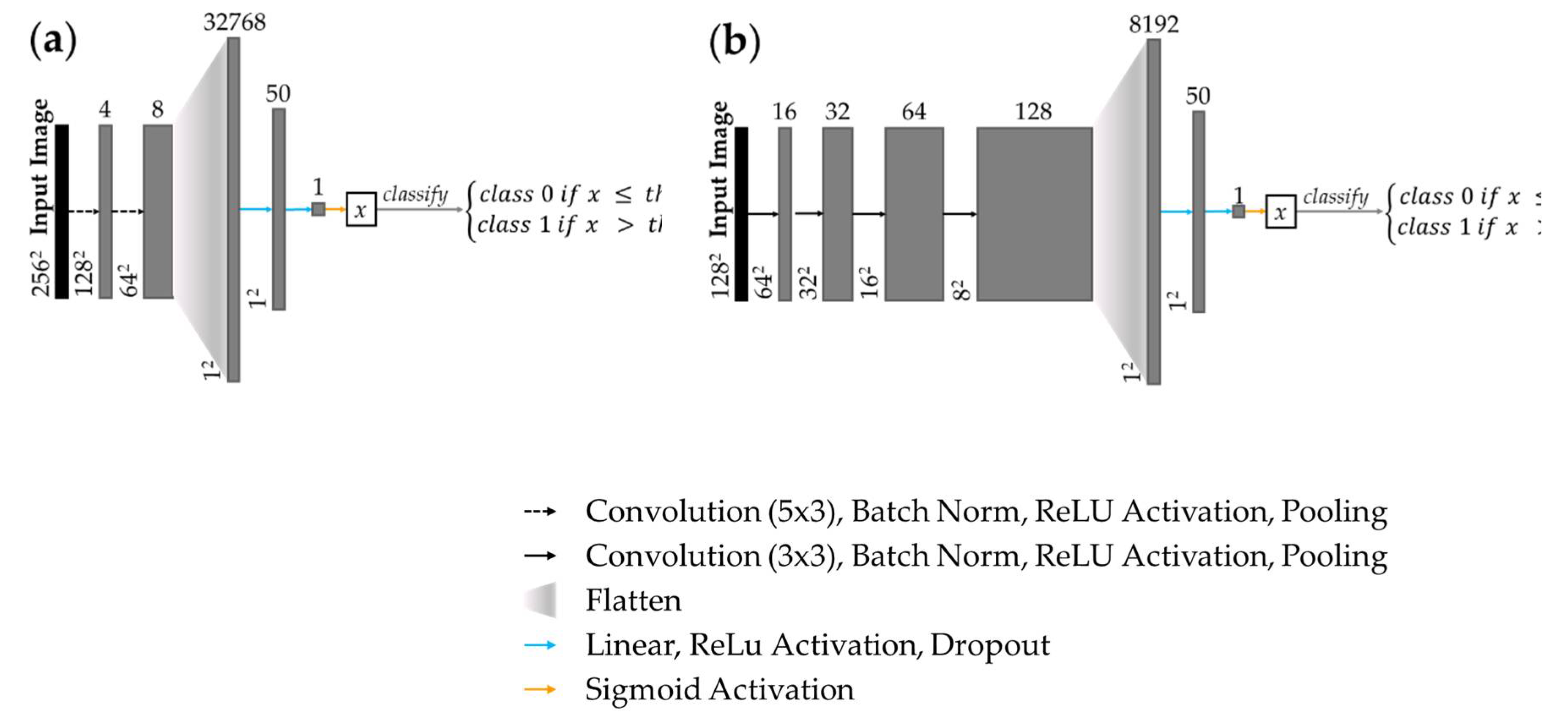
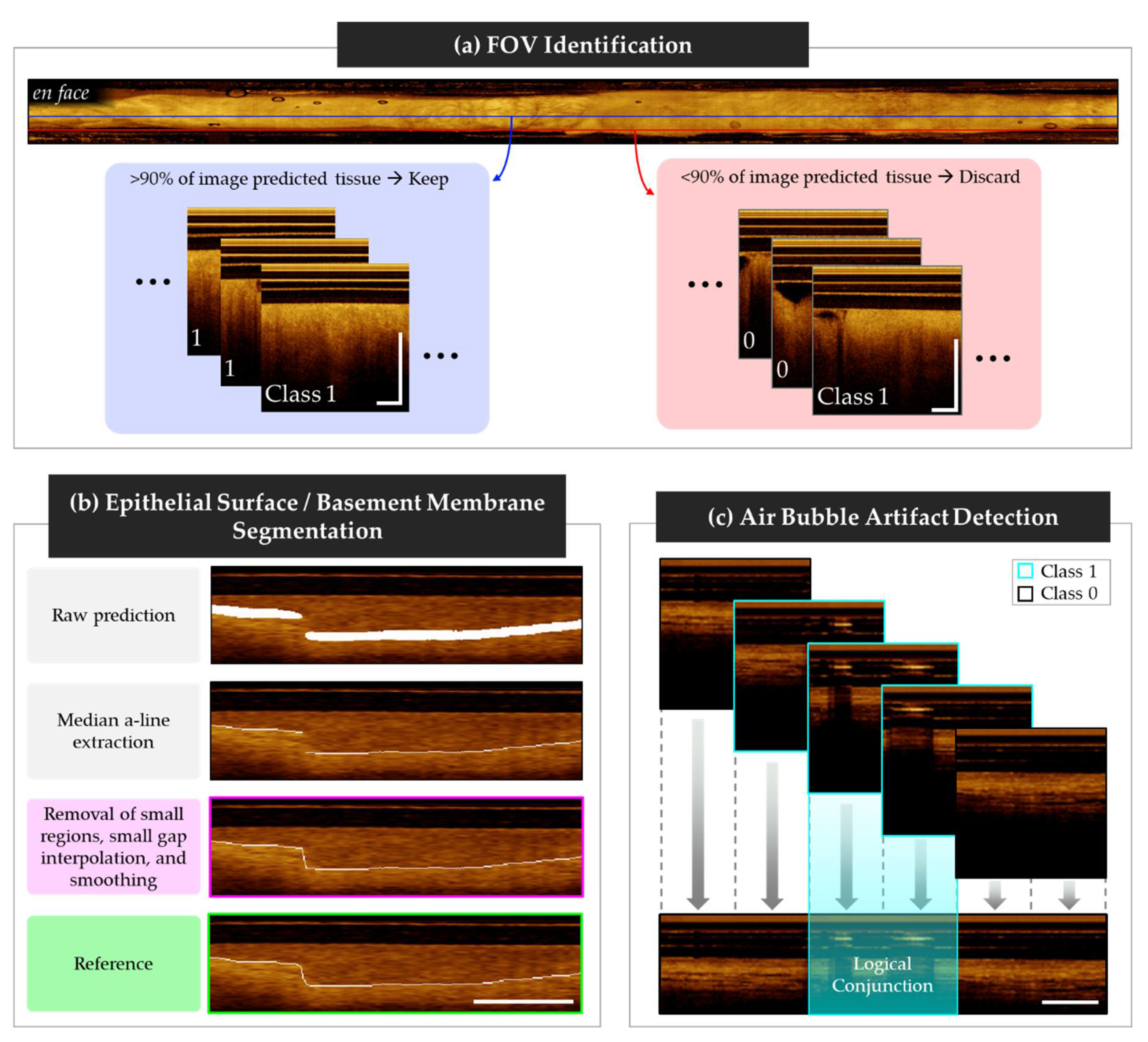
A custom CNN was trained for tile classification in the FOV and artifact detection tasks. Shown in
Figure 2 (a), the feature detection layers of the FOV detection network comprised two convolutional layers with ReLU activation and 2x2 max pooling. The network was terminated with two dense layers with ReLU activation, and a sigmoid classification layer. Shown in
Figure 2 (b), the artifact detection network followed similar topology but comprised four convolutional layers with ReLU activation and 2x2 max pooling.
2.7 U-Net Architectures
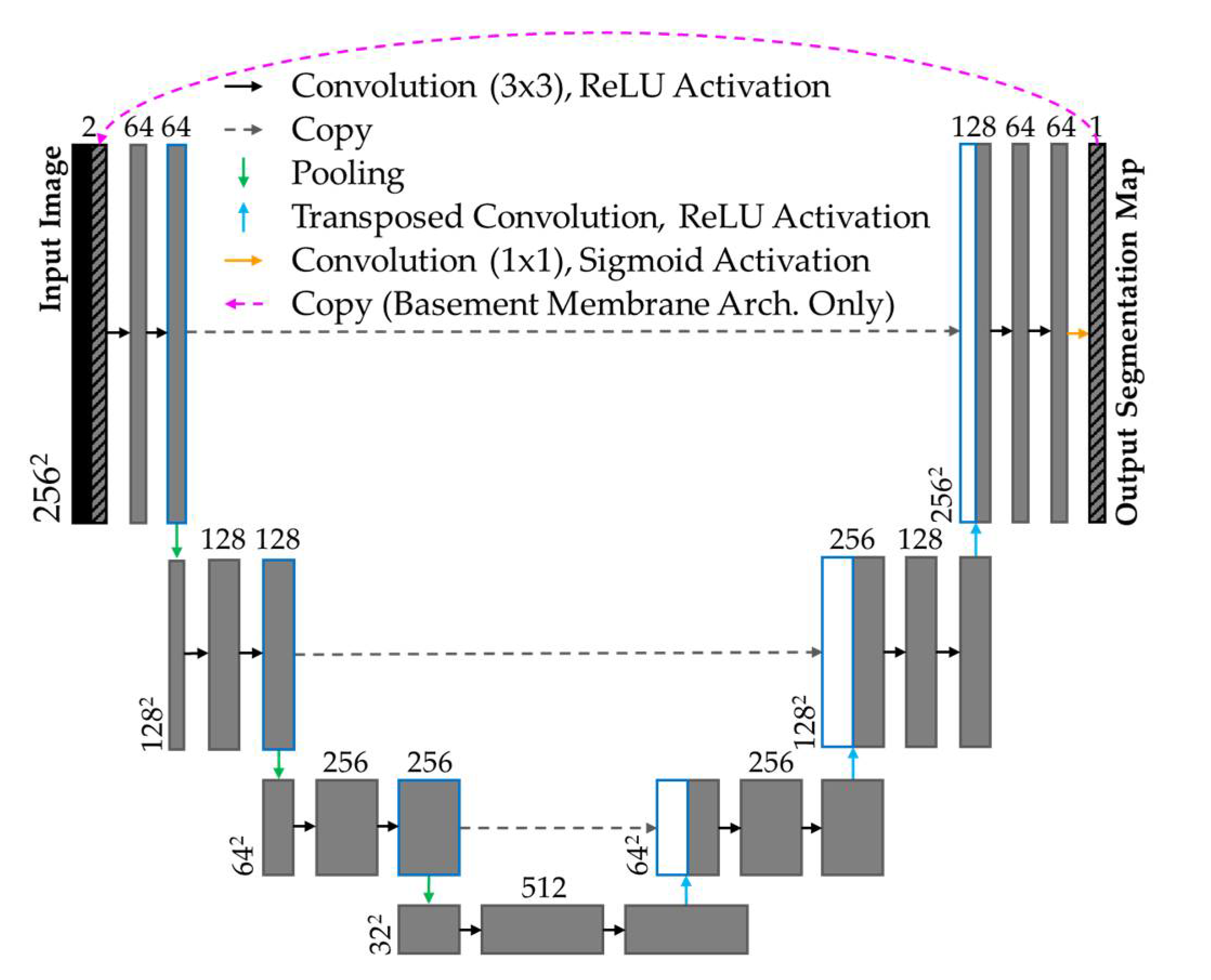
Modified u-nets [
32] were implemented to identify the epithelial surface and basement membrane. The epithelial surface task used a shallow u-net (encoder: 4 convolutional layers, 3x3 kernel, ReLU activation, 2x2 max pooling; decoder: 3 convolutional layers, 3x3 kernel, ReLU activation, 2x2 transposed convolution layers). Shown in
Figure 3, the basement membrane task used the same u-net topology with an additional connection, used during training only, concatenating the prediction of the prior epoch to the input of the subsequent epoch.
2.8. Model Training
For each task, the discovery set was divided into training, tuning and test cohorts with approximately 70%, 15%, 15% distribution, ensuring no patient overlap between intra-task cohorts. Stratified sampling was used to promote uniform representation of features of interest across the cohorts. The distribution of features by deep learning task is summarized in
Table 4. The epithelial surface task did not have a feature of interest; cohort distribution matched the basement membrane task.
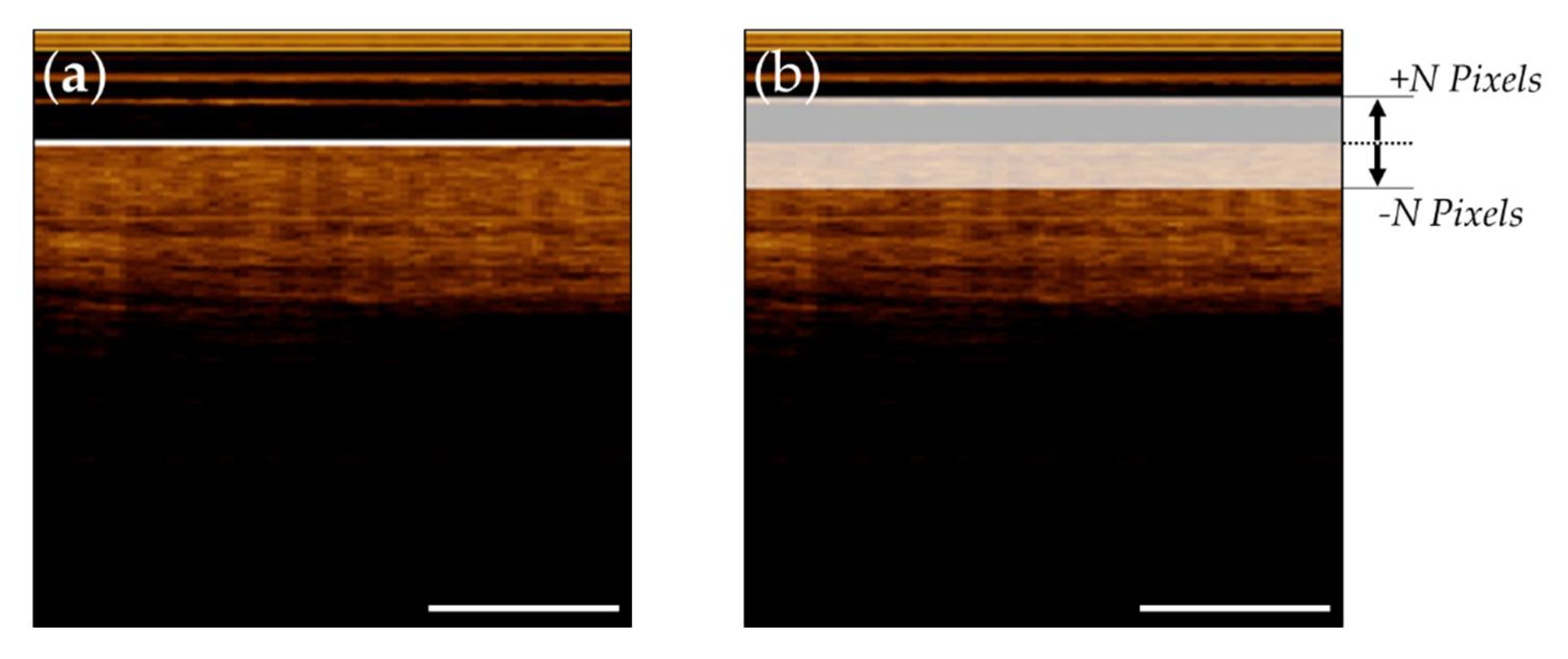
To reduce imbalanced mask content during segmentation tasks, reference annotations were thickened in the vertical (z or A-Line) direction. Various training protocols were explored, evaluating the utility of thickening the segmentation masks. For the epithelial surface task, three models were compared, trained with ± 24 pixel masks, ± 12 pixel masks and ± 4 pixel masks. The basement membrane task also explored thickened training masks, and analyzed pre-training with coarser masks, and fine-tuning with more precise masks.
Figure 4 (a) depicts a raw epithelial surface reference tile overlaid on the image tile.
Figure 4 (b) details the training reference tile after thickening (displayed with transparency to allow visualization of image tile).
2.9 Post-Processing
The FOV detection task class predictions were aggregated by original image. To reduce errors arising from incorrect prediction due to imaging artifacts, poor catheter contact, or off-target structures (e.g. gloved hand touching the catheter, mucus), >90% of the image tiles in each longitudinal image were required to be classified as containing tissue (class 1) to continue to subsequent networks. Examples of longitudinal images pulled from the center (approved, blue) and the edge (rejected, red) of the FOV is shown in
Figure 5 (a).
Post-processing steps for segmentation tasks were developed using model predictions of the test cohort. Steps from the basement membrane task are summarized graphically in
Figure 5 (b), with the final step in magenta, and the reference in green. In both tasks, the raw predictions approximately matched the thickness of the training reference masks. A single pixel thick boundary was created by extracting the median A-Line depth (z-direction) of each tile. Neighboring tiles were then stitched and overlapping regions were averaged.
For the epithelial surface task, simple morphological operations eliminated small (<10 pixels) regions and subsequently connected any gaps between predictions. Boundaries were smoothed by resampling at every 10
th pixel and reconnecting using the pchip algorithm [
33].
Figure 5
In the basement membrane task, morphological operations were used to (1) connect small gaps (< 10 pixels along the pullback (y) axis) through linear interpolation, (2) remove small predictions (< 25 pixels), (3) connect small gaps (< 30 pixels along the pullback axis) through linear interpolation, and (4) smooth predictions through resampling and interpolation with the p-chip algorithm. In steps (1) and (3), regions that were within the pullback-axis limits but were more than 10-pixels apart along the A-Line depth were not connected, to best represent biological organization of oral tissue.
The artifact detection task post-processing steps are summarized in
Figure 5 (c), with class 1 tiles outlined in cyan, and class 0 tiles outlined in black. Classified tiles were stitched into longitudinal images and overlapping tile regions were classified using logical conjunction (i.e. AND), allowing artifact localization within a 64-pixel resolution.
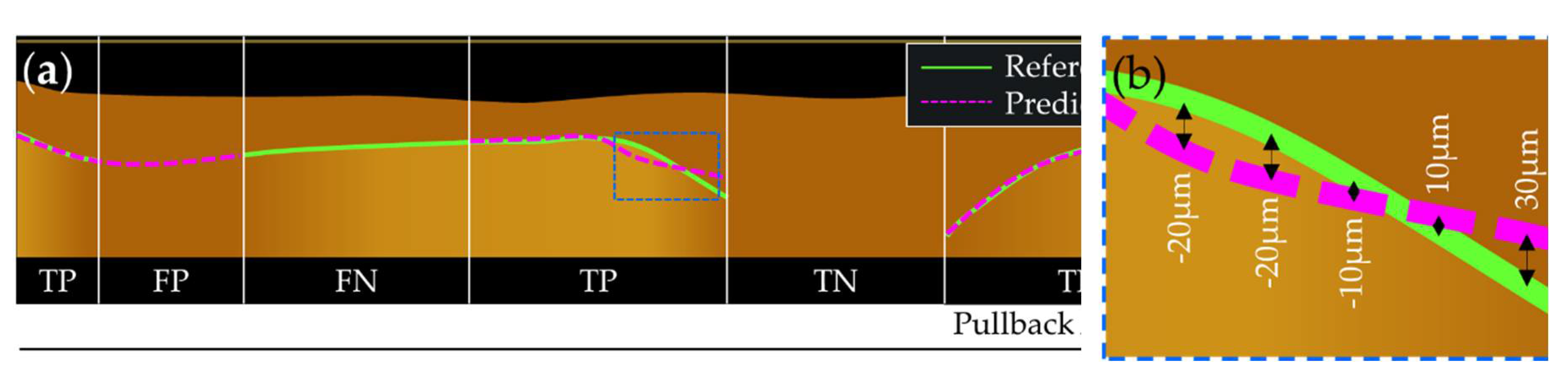
2.10 Evaluation Metrics
All metrics were calculated from the test cohort of the discovery set. Balanced accuracy, sensitivity, and specificity are reported for classification tasks, as well as the receiver operating characteristic (ROC) curve, and the precision recall (PR) curve. The area under the ROC curve (AUC) and mean average precision (mAP) are also presented.
For segmentation tasks, the dice similarity score (DSC), percent of positive agreement (PA), percent of negative agreement (NA) and mean A-line error (ME) are reported. The dice similarity score [
34],
is included for comparability to other segmentation tools; however, this metric demonstrates a bias towards larger objects. Error in comparing small shapes (such as a thin boundaries) is amplified in the DSC, as the small positive sample size is greatly outweighed by the overall sample size (pixel count). Conversely, large shapes may exhibit high DSC despite containing numerous pixels that have been inaccurately segmented [
35].
To accommodate this limitation, we also calculate percent of positive and negative agreement,
to represent agreement about boundary existence within each A-line; these metrics are only calculated for the basement membrane task as the epithelial surface post-processing methods guarantee the presence of a boundary. PA and NA are calculated by comparing the annotations for each A-line per tile. For this application, true positive (TP) is defined by boundary presence in the reference and prediction, and true negative (TN) is defined by boundary absence in the reference and prediction. False positive (FP) and false negative (FN) are counted, with the reference used as the ground truth. The ME metric is used to quantify positional (depth) disagreement in each A-line position between predicted versus reference masks; a positive value indicates the prediction is shallower than the reference, while a negative value indicates the opposite. Regions used to calculate PA and NA are shown graphically in
Figure 6 (a). The blue dashed box in
Figure 6 (b) demonstrates A-line depth errors used to calculate the ME. Per-image metrics are presented as a single value averaged from all test set predictions.
2.11 3-Dimensional Volumes
Two scans from the excluded patient in the discovery set were analyzed: a grade 2 dysplasia of the lateral tongue, and its contralateral. 504 longitudinal images were generated from each pullback. Each longitudinal image was pre-processed, passed through the four-network pipeline, and post-processed. Predictions were combined to reconstruct a 3-dimensional volume detailing the epithelial layer and imaging artifact. Epithelial thickness maps are corrected for refractive index of water (n = 1.33), which closely matches that of tissue. A small Gaussian blur was applied to the epithelial thickness maps (10x10 pixel kernel), and artifact identification map (5x5 pixel kernel) to smooth the edges. Qualitative evaluation is used in the en face view as manual annotation of complete volumes was not practical.
3. Results
3.1. Final Models
For each model, z-score normalization was applied to the discovery set calculated from the mean and standard deviation of the training cohort. Model weights were initialized per the Kaiming He method [
36]. Data augmentation of horizontal flips (50% likelihood) and y-axis shifting (± 10%) was applied to the training cohort. Binary cross entropy [
37] and Adam [
38] were used as the criterion and optimization functions. Summarized in
Table 5, hyperparameters unique to each task were determined through iterative experimentation.
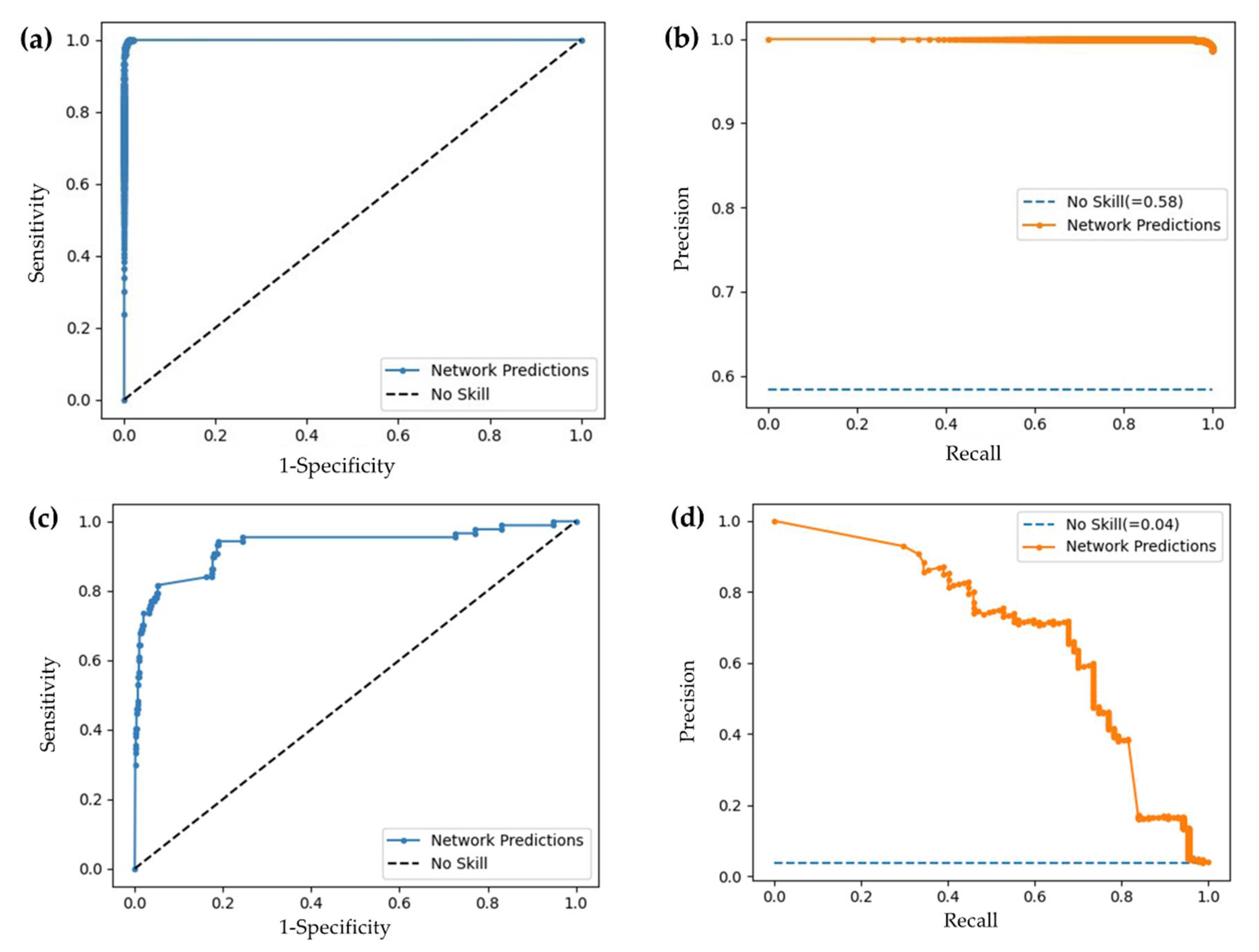
3.2 Convolutional Neural Networks Performance
Classification metrics for the FOV and artifact detection models are reported in
Table 6; ROC and PR curves are presented in
Figure 7, demonstrating improvement over an unskilled model. Evaluation metrics, ROC, and PR curves are calculated from the test set for the respective task.
3.3 U-Net Performance
Segmentation metrics are calculated on stitched, post-processed predictions from the test set. DSC values are calculated after thickening the reference and prediction masks; remaining metrics are calculated on the single pixel boundary.
Three training protocols were evaluated for the epithelial surface segmentation task, exploring the benefit of thickened training masks. Results are detailed in
Table 7. With the metrics being nearly equivalent, and acknowledging the bias of the DSC towards larger objects, selection of the smallest pixel error mean and standard deviation indicated the model trained with annotations thickened by ± 12 pixels as superior.
We also explored the effects of thickening the training masks in the basement membrane task, but also analyzed pre-training with coarser masks, and fine-tuning with more precise masks. Results are summarized in
Table 8. The affinity of the DSC towards larger objects is again observed. Yet, this protocol performed poorly in other metrics. While protocol 2 presents superior ME metrics, this simpler protocol suffered from the lowest PA and NA values, indicating poor representation of basement membrane detection. Protocol 3 yielded the highest DSC among comparable models and the highest PA and NA values, indicating the best agreement with regions both with and without an identifiable visible basement membrane. The remaining metrics are similar in protocols 3-5.
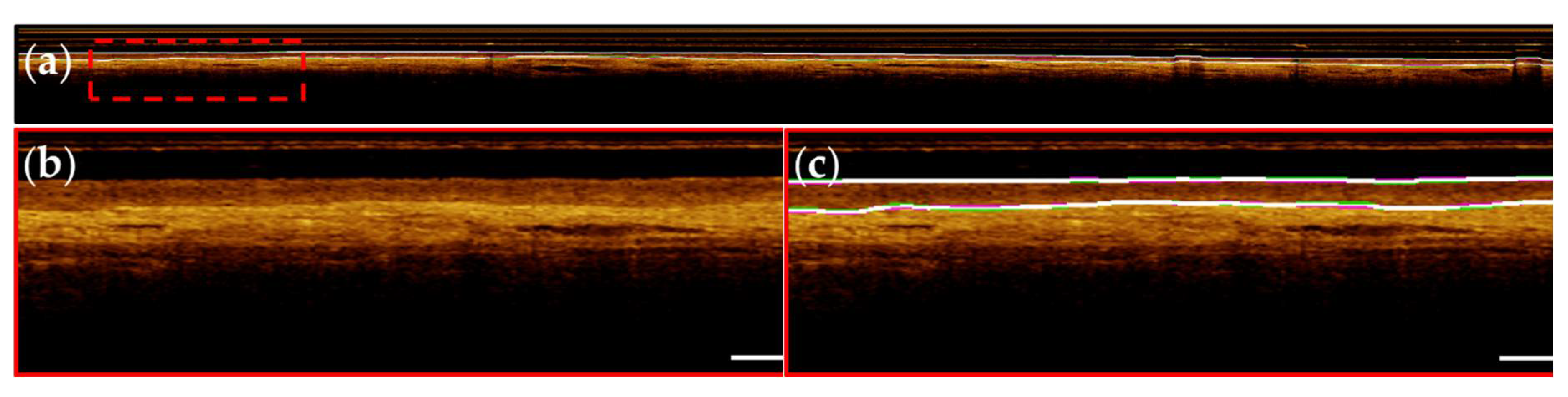
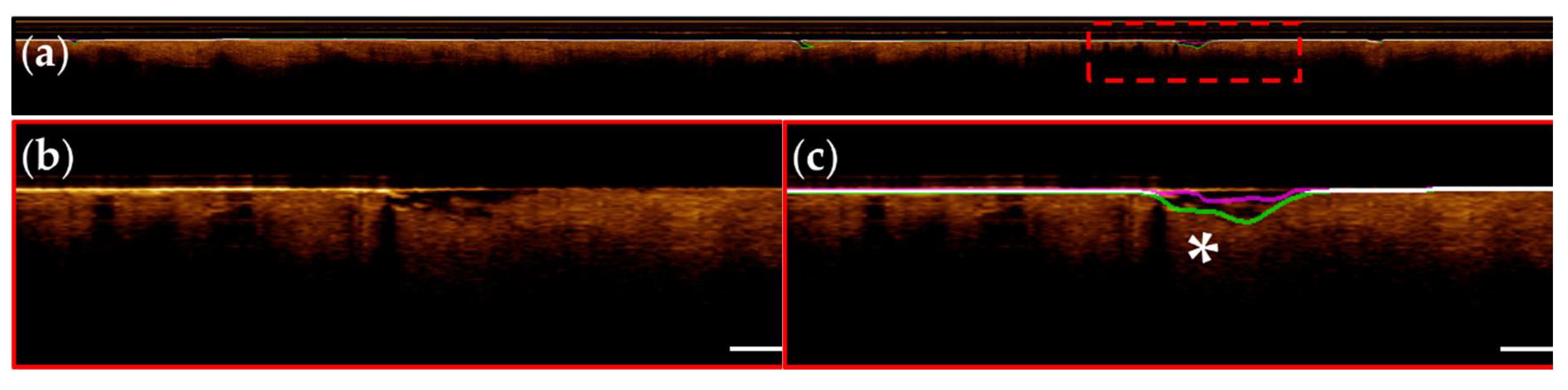
Representative images from patients within the segmentation test set are presented below; Images are taken from apparent normal (contralateral,
Figure 8) and pathologic (biopsy confirmed OSCC,
Figure 9) scans of the ventral tongue. Whole images are presented in (a) and magnified insets are presented unannotated in (b) and annotated in (c). Results from the surface segmentation u-net and basement membrane segmentation u-net are included. Reference and prediction annotations are shown in green and magenta, respectively; regions of agreement are highlighted in white. Good agreement between epithelial boundaries can be visualized in the contralateral image (
Figure 8). Folds in the tissue surface, which were infrequent in the training set, are shown to confound the surface segmentation model - marked by a white star in
Figure 9 (c). The complete loss of epithelial stratification characteristic of OSCC is captured by the basement membrane segmentation model, an example of a correctly classified true negative region.
3.4 Evaluation of 3-Dimensional Volumes
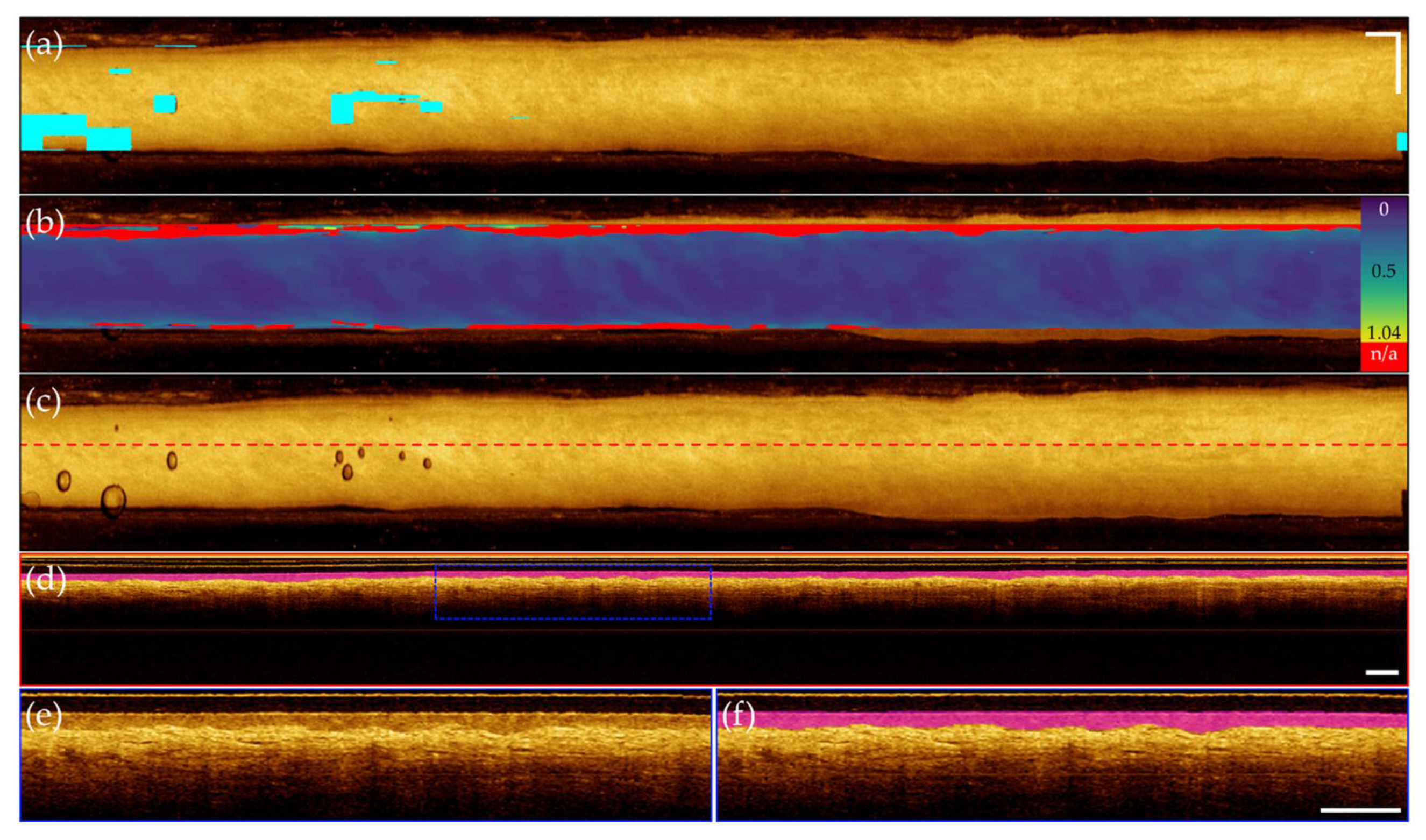
Synthesis of the 3-dimensional prediction data volumes are shown for the contralateral volume (
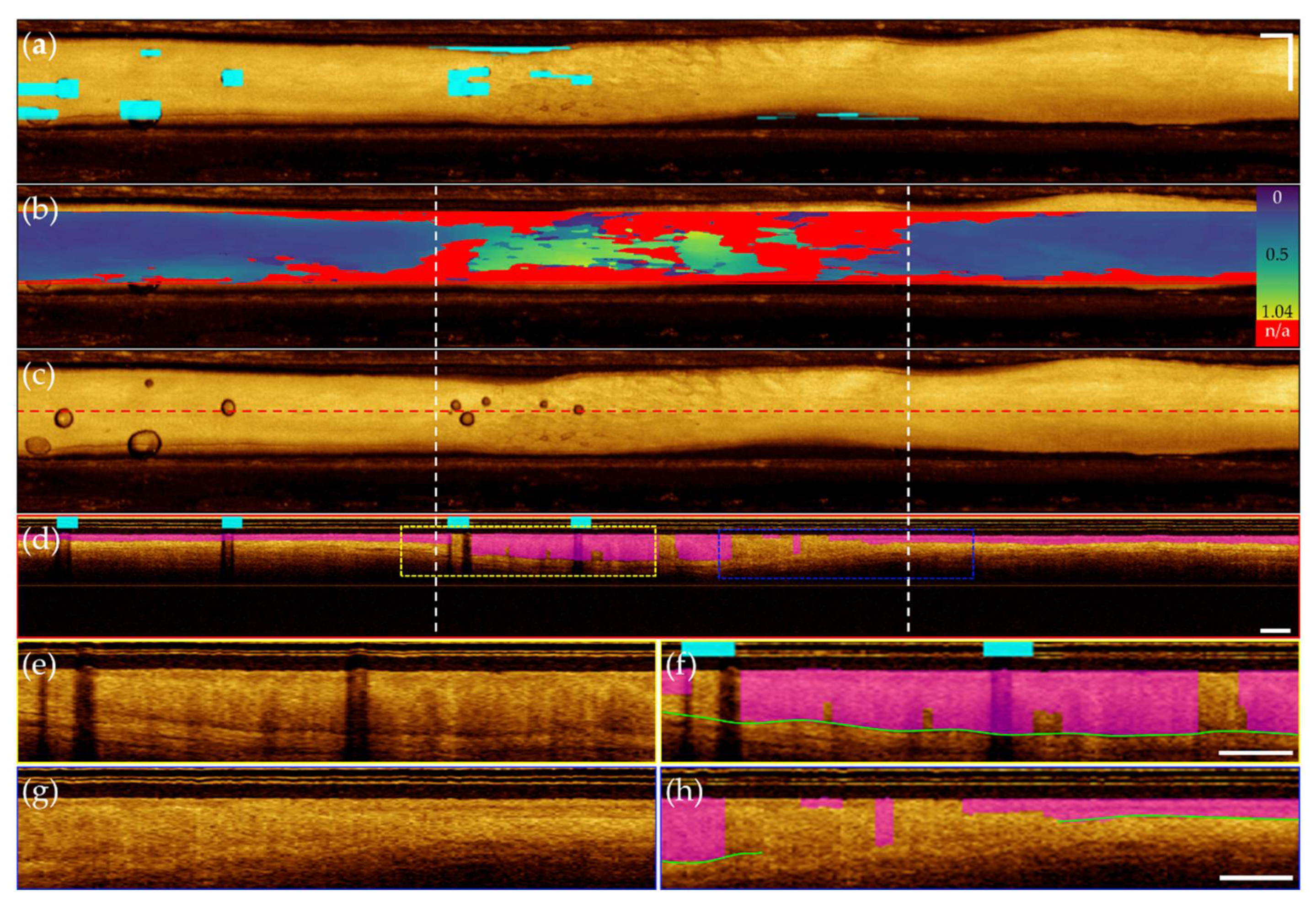
Figure 10) and the dysplastic volume (
Figure 11). For each volume, a mask highlighting imaging artifacts is included in (a) and in (b) an epithelial thickness map, identifying regions of broken or missing basement membrane. Epithelial thickening is demonstrated with the MATLB parula colormap, with darker blue regions indicating thinner epithelium, and yellow regions indicating thickened epithelium. In (c), an unannotated
en face is included for reference with a red dashed line indicating location of a sample longitudinal image. This image is shown annotated in (d) with epithelial layer prediction (magenta) and artifact locations (cyan,
Figure 10 only). Insets of
Figure 10 (d, blue dashed box) is shown in (e) and (f). Insets of
Figure 10 (d, yellow and blue dashed boxes) are included in (e)-(h). Annotated panels include green line identifying rater segmentation for dysplastic insets.
Both volumes demonstrated accurate localization of the imaging artifacts shown in (a), as well as good identification of the FOV, seen in (b). Evaluation of the contralateral volume (
Figure 10) displays near uniform epithelial thickness in (b), aligning with the expected biology of the tissue. Precise segmentation of the epithelial surface and basement membrane is observed, supported by isolating a single longitudinal image in (d), with insets in (e)-(f) demonstrating accurate epithelial layer identification. Comparatively, evaluation of the dysplastic volume (
Figure 11) demonstrates epithelial thickening and loss of the basement membrane characteristic to oral dysplasia in (b). From the left, the map indicates a slow thickening of the epithelial layer, while the right indicates a sharp transition from stratified into non-stratified tissue. Isolation of a longitudinal image shown in (d), pulled from the center of the imaging FOV allows easier visualization of this phenomena. While inconsistencies in the segmentation of the basement membrane are present, with errors highlighted by rater segmentation (green line) in (f) and (h), the general trend of abnormal tissue towards the center of the tissue, compared to the more normal stratification tissue towards the image edges is captured.
4. Discussion
We present a novel pipeline for automated segmentation of oral OCT, using deep learning and image processing methods to provide repeatable, time-sensitive information about epithelial status. Our approach is unique as it employs segmentation strategies to characterize the epithelial layer, rather than classify disease status. This contrasts prior
in vivo oral OCT studies, which were used to triage healthy, pre-cancerous and cancerous samples [
16,
39,
40] or classify states of dysplasia [
39]. While these methods achieved high agreement they are constrained by rigid classification labels, and either have limited transparency in the diagnostic process or employ explainability methods to foster physician trust. Instead, we propose a tool to retrieve oral cancer biomarkers and empower clinicians with morphological information upon which to make treatment plan recommendations.
The processing pipeline employed four independent deep learning networks, preventing the propagation of errors through the analysis pipeline, while simplifying the adaptation (domain-transfer) of these networks to other datasets (lung or cervical OCT, for example). Further investigation into generalizability across oral cavity sites is warranted, where changes in imaging site and pathology may influence network predictions. The networks presented in this research are unavoidably biased towards the more prevalent presentation of oral cancer of the tongue, comprising 71.7% of our data. Whereas the presentation of the epithelial surface (tissue surface) is consistent across imaging site and pathology, the site imbalance in training data may influence network predictions of the basement membrane in sites other than the tongue.
4.1. Convolutional Neural Networks
Training data for the FOV classification task excluded images near the tissue-air transition, as inconsistent contact required manual labelling of tiles. However, this step of the pipeline is designed to discard entire longitudinal images and misclassification of individual tiles is mostly managed through averaging during post-processing. Current methods may be too lenient at the edges of tissue contact, for example at the upper border of
Figure 10 (b). While these images contain oral tissue, the lack of visible basement membrane is likely not attributed to epithelial thickening, but rather a result of the incident angle of the scanning beam approaching perpendicular to the tissue surface. Consequentially, these images proceed to segmentation steps and are either predicted with thickened epithelium, or marked as N/A. Another potential limitation of this approach includes an intolerance for scans experiencing non-uniform rotational distortion, an occasional artifact due to the helical scanning endoscopic OCT system [
41]. However, this effect occurs primarily when the imaging catheter movement is restricted during collection, which is rare when collecting oral OCT due to the accessibility of the site of interest.
Training data for the artifact classification task excluded image tiles that featured small, borderline artifacts. Potential errors arising from under-representing this type of image are accommodated through overlapping tiles. Stitching tiles using logical conjunction allows for more focal identification of the regions of artifact. However, as observed in
Figure 10 (a) and
Figure 11 (a), applying classification labels to whole tiles results in over-identification of artifact regions; a better suited method may be segmentation of the
en face projection. If the artifacts of most concern are air bubbles,
en face projections could be examined over a reduced A-Line depth to readily identify the sheath and holder region. This would reduce pre-processing time.
4.2. U-Nets
U-net models were trained on thickened masks to reduce class imbalance. Size bias is apparent in the DSC metrics of the thicker training masks, yet limitations of these training protocols can be observed in the other metrics. Selection of the ± 12 pixel thick mask for the epithelial surface task allowed the necessary precision to avoid basing predictions on the imaging core artifacts, but provided sufficient spatial information that remained useable at the lowest levels of the network. For the more complex basement membrane segmentation task, fine-tuning with thinner masks generated improvements in protocols 3 and 5. This difference may be attributed to the more challenging task, or the adaptation of the network topology, where the input layer contained both the input image tile, and the prediction of the previous epoch. Training protocol 3 exhibited the best response to post-processing methods, despite the algorithm being developed using the predictions of protocol 5.
The uniqueness of this approach limits its comparability with prior studies as, to our knowledge, no other deep learning segmentation applications have been applied to oral OCT. To validate the success of our models, we present our evaluation metrics calculated against the reference annotations, shown in
Table 9. Segmentation is a laborious and subjective task, resulting in human raters being prone to error or differences of opinion regarding boundary location. Model success may be indicated if the reference-prediction metrics are within the distribution of inter-rater metrics.
Comparison of these results to reference prediction metrics for the epithelial surface task and the basement membrane task demonstrates that deep learning methods offer an improvement over manual annotation metric. The A-Line resolution of these images is 10 µm, thus errors beyond this resolution indicate high agreement. Some poor inter-rater agreement may be attributed to labelling errors rather than misidentification of the surface of interest: this type of error supports the motivation for automated methods.
Challenges identified in the epithelial surface segmentation task include a limited selection of images containing unique features: longitudinal images where unknown materials occlude the image (n = 3) and tissue folds occurring in softer mucosal membranes (n = 2). An example of this can be seen in
Figure 9 (c), denoted by a white star. Generally, models struggled to decipher irregular substances (e.g. mucous, keratinization) or structures (e.g. tissue folds and gaps) resulting in incorrect predictions. This error may be addressable with increased sample size including more cases in the training data.
It is evident that segmentation of the basement membrane is a more complex task for both manual and automated methods, in comparison to the epithelial surface task. The loss of stratification characteristic of cancerous and pre-cancerous oral lesions is difficult to quantify using manual annotations, and some cases required the raters to use contextual information present in the entire longitudinal slice. Accordingly, the image tiling step introduces a network limitation as this context is lost.
4.x Comparison of Predictions for Contralateral and Dysplastic OCT Volumes
The distinction between epithelial and stromal layers in the contralateral volume is well captured by model predictions, particularly clear in the longitudinal image shown in
Figure 10 (d), with inset comparisons in (e) and (f). The basement membrane was segmented for 91.5% of the in-FOV tissue, with the missing 8.5% occurring at the tissue edges. The average predicted epithelial thickness is 208µm, in agreement with prior research measuring the epithelial thickness of the lateral tongue using OCT (216±59µm) [
42].
Conversely, the delineation between the epithelial and stromal layers becomes more nuanced in the dysplastic case, shown in
Figure 11, particularly in the region of epithelial thickening indicated by white dashed lines in (b) – (d). The transition across the layers becomes less sharp and while normal tissue morphology dictates the basement membrane is visible across the entire image, the network delivers a discontinuous prediction. We hypothesize a few scenarios that result in incorrect model predictions. As discussed above, the loss of contextual information restricts available data upon which to make segmentation predictions. Moreover, as the epithelial layer thickens, the transitionary zone moves lower in the longitudinal image and approaches the maximum imaging depth of our system. At this depth, the signal to noise ratio decreases as the light attenuates towards the level of the noise floor, and the transition between the two layers is more difficult to delineate. In cases with extreme epithelial thickening, the basement membrane cannot be visualized at all. Finally, as oral tissue transitions through pre- and potentially-malignant lesions towards cancer, changes in cell size, content and organization alters the scattering properties [
43] of the tissue and OCT images become more homogeneous in appearance, further complicating the basement membrane segmentation task. Continued development of complex architectures may improve such errors. Currently, the basement membrane was segmented for 68.7% of the in-FOV tissue and the average predicted epithelial thickness is 319µm. Both the loss of visible stratification and increased epithelial thickness agree with the expected changes arising in dysplastic tissue.
This work highlights the opportunity for automated depth analysis of OCT data, wherein differences in tissue content are non-obvious in the en face view, and the quantity of longitudinal images renders manual assessment unmanageable. Additionally, presenting depth information in the en face view allows for qualitative image interpretation.
5. Conclusions
A novel deep learning pipeline is presented as a tool to detect and quantify the presence and depth of the epithelial layer in OCT images, potentially decreasing barriers towards clinical applications of oral OCT. Defining the tissue analysis task to be completed through segmentation allows for a more generalized approach, not restricted by specific oral sites and diseases. Built with two CNNs, for FOV and artifact detection, and two modified u-nets, for epithelial layer isolation, this pipeline provides fast and reproducible results. Comparison of inter-rater agreement to network predictions demonstrate as-good-as or better agreement, and evaluation of whole OCT volumes of exemplifies ability to identify pathological progression.
Potential impacts for this work include monitoring of pre- and potentially malignant oral lesions, guiding biopsy site selection to reduce false negative biopsies and intra-operative margin assessment during tumor resection procedures.
Author Contributions
Conceptualization, CH and PL; methodology, CH, JM and CM; image collection, CP, SN and KL; software, CH; validation, CH; formal analysis, CH; investigation, CH; resources, CP, CM and PL; data curation, CH, JM and CP; writing—original draft preparation, CH; writing—review and editing, CH, JM, CP, CM and PL; visualization, CH and JM; supervision, CM and PL; project administration, PL; funding acquisition, CM, CP and PL. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by a Collaborative Health Research Project (CHRP) grant co-sponsored by the Canadian Institutes of Health Research (CIHR, FRN 134740) and the Natural Sciences and Engineering Research Council of Canada (NSERC, Appl ID 462490-2014). CH acknowledges scholarship support from NSERC and Simon Fraser University. JM acknowledges fellowship support from the University of British Columbia, the Mitacs Accelerate program, and the British Columbia Cancer Foundation. KL acknowledges fellowship support from CIHR.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Board of the University of British Columbia and the British Columbia Cancer Agency (H11-02516, amended for this study August 19, 2014).
Informed Consent Statement
Informed written consent was obtained from all subjects involved in the study.
Data Availability Statement
The raw data supporting the conclusions of this article and the code used to process it will be made available by the authors on request.
Acknowledgments
We thank our collaborators in Integrative Oncology, our clinical partners in Oral Medicine & Oral Pathology, the patients who participated in this study, and the members of the Optical Cancer Imaging Lab (OCIL).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyzes, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Oral Cavity and Pharynx Cancer — Cancer Stat Facts. Available online: https://seer.cancer.gov/statfacts/html/oralcav.html (accessed on 12 December 2023).
- Oral and Oropharyngeal Cancer: Statistics. Available online: https://www.cancer.net/cancer-types/oral-and-oropharyngeal-cancer/statistics (accessed on 26 January 2023).
- Canadian Cancer Society Supportive Care for Leukemia | Canadian Cancer Society. Available online: https://cancer.ca/en/cancer-information/cancer-types/oral/supportive-care (accessed on 28 May 2023).
- Osazuwa-Peters, N.; Simpson, M.C.; Zhao, L.; Boakye, E.A.; Olomukoro, S.I.; Deshields, T.; Loux, T.M.; Varvares, M.A.; Schootman, M. Suicide Risk among Cancer Survivors: Head and Neck versus Other Cancers. Cancer 2018, 124, 4072–4079. [Google Scholar] [CrossRef] [PubMed]
- Kar, A.; M R, A.; Bhaumik, U.; Rao, V.U.S. Psychological Issues in Head and Neck Cancer Survivors: Need for Addressal in Rehabilitation. Oral Oncol. 2020, 110, 104859. [Google Scholar] [CrossRef] [PubMed]
- Brizuela, M.; Winters, R. Histology, Oral Mucosa. StatPearls 2023. [Google Scholar]
- Ranganathan, K.; Kavitha, L. Oral Epithelial Dysplasia: Classifications and Clinical Relevance in Risk Assessment of Oral Potentially Malignant Disorders. J. Oral Maxillofac. Pathol. 2019, 23, 19. [Google Scholar] [CrossRef]
- Poh, C.F.; Ng, S.; Berean, K.W.; Williams, P.M.; Rosin, M.P.; Zhang, L. Biopsy and Histopathologic Diagnosis of Oral Premalignant and Malignant Lesions. J. Can. Dent. Assoc. 2008, 74, 283–288. [Google Scholar] [PubMed]
- Neville, B.W.; Day, T.A. Oral Cancer and Precancerous Lesions. CA. Cancer J. Clin. 2002, 52, 195–215. [Google Scholar] [CrossRef] [PubMed]
- Pindborg, J.J.; Reichart, P.A.; Smith, C.J.C.; van der Waal, I.; Waal, I. Van der Histological Typing of Cancer and Precancer of the Oral Mucosa; 2nd ed.; Springer Berlin Heidelberg, 1997.
- Drexler, W.; Fujimoto, J.G. Special Section Guest Editors Optical Coherence Tomography in Ophthalmology. J. Biomed. Opt. 2007, 12, 041201. [Google Scholar] [CrossRef]
- Chen, S.; Abu-Qamar, O.; Kar, D.; Messinger, J.D.; Hwang, Y.; Moult, E.M.; Lin, J.; Baumal, C.R.; Witkin, A.; Liang, M.C.; et al. Ultrahigh Resolution OCT Markers of Normal Aging and Early Age-Related Macular Degeneration. Ophthalmol. Sci. 2023, 3, 100277. [Google Scholar] [CrossRef] [PubMed]
- Ridgway, J.M.; Armstrong, W.B.; Guo, S.; Mahmood, U.; Su, J.; Jackson, R.P.; Shibuya, T.; Crumley, R.L.; Gu, M.; Chen, Z.; et al. In Vivo Optical Coherence Tomography of the Human Oral Cavity and Oropharynx. Arch. Otolaryngol. Neck Surg. 2006, 132, 1074–1081. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-K.; Chi, T.-T.; Wu, C.-T.; Tsai, M.-T.; Chiang, C.-P.; Yang, C.-C. Diagnosis of Oral Precancer with Optical Coherence Tomography. Biomed. Opt. Express 2012, 3, 1632. [Google Scholar] [CrossRef]
- Lee, A.M.D.; Cahill, L.; Liu, K.; MacAulay, C.; Poh, C.; Lane, P. Wide-Field in Vivo Oral OCT Imaging. Biomed. Opt. Express 2015, 6, 2664. [Google Scholar] [CrossRef] [PubMed]
- Heidari, A.E.; Sunny, S.P.; James, B.L.; Lam, T.M.; Tran, A. V.; Yu, J.; Ramanjinappa, R.D.; Uma, K.; Birur, P.; Suresh, A.; et al. Optical Coherence Tomography as an Oral Cancer Screening Adjunct in a Low Resource Settings. IEEE J. Sel. Top. Quantum Electron. 2018, 25. [Google Scholar] [CrossRef]
- Wilder-Smith, P.; Jung, W.G.; Brenner, M.; Osann, K.; Beydoun, H.; Messadi, D.; Chen, Z. In Vivo Optical Coherence Tomography for the Diagnosis of Oral Malignancy. Lasers Surg. Med. 2004, 35, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, M.; Schnabel, C.; Mueller, J.; Golde, J.; Koch, E.; Walther, J. In Vivo Endoscopic Optical Coherence Tomography of the Healthy Human Oral Mucosa: Qualitative and Quantitative Image Analysis. Diagnostics 2020, 10, 827. [Google Scholar] [CrossRef] [PubMed]
- Stasio; Lauritano; Iquebal; Romano; Gentile; Lucchese Measurement of Oral Epithelial Thickness by Optical Coherence Tomography. Diagnostics 2019, 9, 90. [CrossRef] [PubMed]
- Fujimoto J.and Drexler, W. Introduction to Optical Coherence Tomography. In Optical Coherence Tomography: Technology and Applications; Drexler Wolfgangand Fujimoto, J.G., Ed.; Springer Berlin Heidelberg: Berlin, Heidelberg, 2008; pp. 1–45 ISBN 978-3-540-77550-8.
- Jung, W.; Boppart, S.A. Optical Coherence Tomography for Rapid Tissue Screening and Directed Histological Sectioning. Anal. Cell. Pathol. 2012, 35, 129–143. [Google Scholar] [CrossRef]
- Kugelman, J.; Alonso-Caneiro, D.; Read, S.A.; Hamwood, J.; Vincent, S.J.; Chen, F.K.; Collins, M.J. Automatic Choroidal Segmentation in OCT Images Using Supervised Deep Learning Methods. Sci. Rep. 2019. [Google Scholar] [CrossRef]
- Pekala, M.; Joshi, N.; Liu, T.Y.A.; Bressler, N.M.; DeBuc, D.C.; Burlina, P. Deep Learning Based Retinal OCT Segmentation. Comput. Biol. Med. 2019, 114, 103445. [Google Scholar] [CrossRef]
- Fang, L.; Cunefare, D.; Wang, C.; Guymer, R.H.; Farsiu, S.; Huang, D.; Swanson, E.A.; Lin, C.P.; Schuman, J.S.; Stinson, W.G.; et al. Automatic Segmentation of Nine Retinal Layer Boundaries in OCT Images of Non-Exudative AMD Patients Using Deep Learning and Graph Search. Biomed. Opt. Express, Vol. 8, Issue 5, pp. 2732-2744 2017, 8, 2732–2744. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Soltanian-Zadeh, S.; Chu, K.K.; Zhang, H.; Moussa, L.; Watts, A.E.; Shaheen, N.J.; Wax, A.; Farsiu, S.; Farsiu, S. Connectivity-Based Deep Learning Approach for Segmentation of the Epithelium in in Vivo Human Esophageal OCT Images. Biomed. Opt. Express, Vol. 12, Issue 10, pp. 6326-6340 2021, 12, 6326–6340. [Google Scholar] [CrossRef] [PubMed]
- Gharaibeh, Y.; Prabhu, D.S.; Kolluru, C.; Lee, J.; Zimin, V.; Bezerra, H.G.; Wilson, D.L. Coronary Calcification Segmentation in Intravascular OCT Images Using Deep Learning: Application to Calcification Scoring. https://doi.org/10.1117/1.JMI.6.4.045002 2019, 6, 045002, doi:10.1117/1.JMI.6.4.045002.
- Lee, C.S.; Baughman, D.M.; Lee, A.Y. Deep Learning Is Effective for Classifying Normal versus Age-Related Macular Degeneration OCT Images. Kidney Int. Reports 2017, 1, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.; Wang, C.; Li, S.; Rabbani, H.; Chen, X.; Liu, Z. Attention to Lesion: Lesion-Aware Convolutional Neural Network for Retinal Optical Coherence Tomography Image Classification. IEEE Trans. Med. Imaging 2019, 38, 1959–1970. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Tong, Y.; Yu, Y.; Xing, Y.; Chen, C.; Shen, Y. Deep Learning-Based Automated Classification of Multi-Categorical Abnormalities From Optical Coherence Tomography Images. Transl. Vis. Sci. Technol. 2018, 7, 41. [Google Scholar] [CrossRef] [PubMed]
- Goldan, R.N.; Lee, A.M.D.; Cahill, L.; Liu, K.; MacAulay, C.; D.D.S., C.F.P.; Lane, P. Automated Segmentation of Oral Mucosa from Wide-Field OCT Images (Conference Presentation). In Proceedings of the Proc.SPIE; April 27 2016; Vol. 9698, p. 96980R.
- Adjust Image Intensity Values or Colormap - MATLAB Imadjust. Available online: https://www.mathworks.com/help/images/ref/imadjust.html (accessed on 20 March 2023).
- Ronneberger, O.; Fischer, P.; Brox, T. U-Net: Convolutional Networks for Biomedical Image Segmentation. In Proceedings of the Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics); 2015.
- Piecewise Cubic Hermite Interpolating Polynomial (PCHIP) - MATLAB Pchip. Available online: https://www.mathworks.com/help/matlab/ref/pchip.html (accessed on 11 April 2023).
- Dice, L.R. Measures of the Amount of Ecologic Association Between Species. Ecology 1945, 26, 297–302. [Google Scholar] [CrossRef]
- Reinke, A.; Tizabi, M.D.; Sudre, C.H.; Eisenmann, M.; Rädsch, T.; Baumgartner, M.; Acion, L.; Antonelli, M.; Arbel, T.; Bakas, S.; et al. Common Limitations of Image Processing Metrics: A Picture Story. 2021, doi:10.48550/arxiv.2104.05642.
- He, K.; Zhang, X.; Ren, S.; Sun, J. Delving Deep into Rectifiers: Surpassing Human-Level Performance on ImageNet Classification. In Proceedings of the 2015 IEEE International Conference on Computer Vision (ICCV); 2015; pp. 1026–1034.
- BCEWithLogitsLoss — PyTorch 2.0 Documentation. Available online: https://pytorch.org/docs/stable/generated/torch.nn.BCEWithLogitsLoss.html (accessed on 20 April 2023).
- Kingma, D.P.; Ba, J.L. Adam: A Method for Stochastic Optimization. In Proceedings of the 3rd International Conference on Learning Representations, ICLR 2015 - Conference Track Proceedings; San Diego, 2015.
- James, B.L.; Sunny, S.P.; Heidari, A.E.; Ramanjinappa, R.D.; Lam, T.; Tran, A. V.; Kankanala, S.; Sil, S.; Tiwari, V.; Patrick, S.; et al. Validation of a Point-of-Care Optical Coherence Tomography Device with Machine Learning Algorithm for Detection of Oral Potentially Malignant and Malignant Lesions. Cancers (Basel). 2021, 13. [Google Scholar] [CrossRef]
- Yang, Z.; Pan, H.; Shang, J.; Zhang, J.; Liang, Y. Deep-Learning-Based Automated Identification and Visualization of Oral Cancer in Optical Coherence Tomography Images. Biomedicines 2023, 11, 802. [Google Scholar] [CrossRef] [PubMed]
- Kang, W.; Wang, H.; Wang, Z.; Jenkins, M.W.; Isenberg, G.A.; Chak, A.; Rollins, A.M. Motion Artifacts Associated with in Vivo Endoscopic OCT Images of the Esophagus. Opt. Express 2011, 19, 20722. [Google Scholar] [CrossRef]
- Prestin, S.; Rothschild, S.I.; Betz, C.S.; Kraft, M. Measurement of Epithelial Thickness within the Oral Cavity Using Optical Coherence Tomography. Head Neck 2012, 34, 1777–1781. [Google Scholar] [CrossRef] [PubMed]
- Backman, V.; Wallace, M.B.; Perelman, L.T.; Arendt, J.T.; Gurjar, R.; Müller, M.G.; Zhang, Q.; Zonios, G.; Kline, E.; McGillican, T.; et al. Detection of Preinvasive Cancer Cells. Nat. 2000 4066791 2000, 406, 35–36. [Google Scholar] [CrossRef] [PubMed]
Figure 1.
OCT of lateral tongue with biopsy confirmed OSCC. (a) Helical scanning coordinate system illustrating (A-line), (azimuthal, pink to blue color gradient), and (pullback) axes; (b) en face mean intensity projection, unwrapped along pink to blue gradient of (a), with air bubbles marked by B; (c) cross-sectional view at purple dashed line in (b) and (d); (d) longitudinal view at dashed red line in (b); (e) Inset magnified from yellow dashed box in (c), highlighting appearance of epithelial and stromal layers in OCT. Epithelial surface and basement membrane marked by white dashed lines; (f) Histology section with regions of normal and abnormal stratification, with corresponding regions marked in (b) and (d). Scale bars 1 mm.
Figure 1.
OCT of lateral tongue with biopsy confirmed OSCC. (a) Helical scanning coordinate system illustrating (A-line), (azimuthal, pink to blue color gradient), and (pullback) axes; (b) en face mean intensity projection, unwrapped along pink to blue gradient of (a), with air bubbles marked by B; (c) cross-sectional view at purple dashed line in (b) and (d); (d) longitudinal view at dashed red line in (b); (e) Inset magnified from yellow dashed box in (c), highlighting appearance of epithelial and stromal layers in OCT. Epithelial surface and basement membrane marked by white dashed lines; (f) Histology section with regions of normal and abnormal stratification, with corresponding regions marked in (b) and (d). Scale bars 1 mm.
Figure 2.
CNN architecture network topology for (a) FOV detection task; (b) artifact detection task. Arrows represent layer operations (defined bottom right), grey boxes represent feature maps, labelled with number of feature maps (above) and image dimension (left).
Figure 2.
CNN architecture network topology for (a) FOV detection task; (b) artifact detection task. Arrows represent layer operations (defined bottom right), grey boxes represent feature maps, labelled with number of feature maps (above) and image dimension (left).
Figure 3.
Segmentation u-net topology shown for segmentation tasks. Arrows denote layer operations and grey boxes denote feature maps. Number of feature maps (top) and image dimension (left) are labelled. White boxes are copied feature maps of corresponding blue-outline boxes. Magenta arrow (top) is included in basement membrane architecture only.
Figure 3.
Segmentation u-net topology shown for segmentation tasks. Arrows denote layer operations and grey boxes denote feature maps. Number of feature maps (top) and image dimension (left) are labelled. White boxes are copied feature maps of corresponding blue-outline boxes. Magenta arrow (top) is included in basement membrane architecture only.
Figure 4.
Epithelial surface tile with reference annotation overlaid. (a) Raw annotation; (b) thickened annotation. Scale bars 1 mm.
Figure 4.
Epithelial surface tile with reference annotation overlaid. (a) Raw annotation; (b) thickened annotation. Scale bars 1 mm.
Figure 5.
Network post-processing steps. (a) Tile aggregation for FOV classification task. Includes example of accepted longitudinal image (left, blue) pulled from center of the en face projection (blue line), and a rejected longitudinal image (right, red) pulled from the tissue-air transition of the en face projection (red line); (b) Prediction cleaning for surface segmentation tasks, listed top to bottom: stitched raw prediction; single pixel boundary taken at median A-Line; remove small objects, connect gaps, and smooth prediction (end of process – magenta); reference data (green); (c) Tile aggregation for air bubble detection, with overlapping regions classified using logical conjunction. Scale bars 1 mm.
Figure 5.
Network post-processing steps. (a) Tile aggregation for FOV classification task. Includes example of accepted longitudinal image (left, blue) pulled from center of the en face projection (blue line), and a rejected longitudinal image (right, red) pulled from the tissue-air transition of the en face projection (red line); (b) Prediction cleaning for surface segmentation tasks, listed top to bottom: stitched raw prediction; single pixel boundary taken at median A-Line; remove small objects, connect gaps, and smooth prediction (end of process – magenta); reference data (green); (c) Tile aggregation for air bubble detection, with overlapping regions classified using logical conjunction. Scale bars 1 mm.
Figure 6.
Segmentation metrics. (a) Regions of TP, TN, FP and FN used to calculate PA and NA; (b) regions of depth disagreement used to calculate ME, enhance from blue dashed box in (a).
Figure 6.
Segmentation metrics. (a) Regions of TP, TN, FP and FN used to calculate PA and NA; (b) regions of depth disagreement used to calculate ME, enhance from blue dashed box in (a).
Figure 7.
(a) ROC and (b) PRC curves for FOV classification task; (c) ROC and (d) PR curves for artifact classification task.
Figure 7.
(a) ROC and (b) PRC curves for FOV classification task; (c) ROC and (d) PR curves for artifact classification task.
Figure 8.
Contralateral ventral tongue. (a) Image with reference (green) and prediction (magenta) annotations; white annotations indicate overlap; (b) Magnified region of red dashed box in (a); (c) With annotation overlay (bolded for visualization). Scale bars 1mm.
Figure 8.
Contralateral ventral tongue. (a) Image with reference (green) and prediction (magenta) annotations; white annotations indicate overlap; (b) Magnified region of red dashed box in (a); (c) With annotation overlay (bolded for visualization). Scale bars 1mm.
Figure 9.
OSCC of the ventral tongue. (a) Image with reference (green) and prediction (magenta) annotations; white annotations indicate overlap; (b) Magnified region of red dashed box in (a); (c) With annotation overlay (bolded for visualization), white star indicates region of tissue fold confounding the network. Scale bars 1mm.
Figure 9.
OSCC of the ventral tongue. (a) Image with reference (green) and prediction (magenta) annotations; white annotations indicate overlap; (b) Magnified region of red dashed box in (a); (c) With annotation overlay (bolded for visualization), white star indicates region of tissue fold confounding the network. Scale bars 1mm.
Figure 10.
Contralateral pullback of the lateral tongue. (a) En face projection with artifact overlay; (b) En face projection with epithelial thickness map. Color bar indicates 0 to 1.04mm thickness, with bright red indicating no visible basement membrane; (c) unannotated en face projection with red dashed line indicating location of longitudinal image in (d); (d) longitudinal image with predicted epithelial layer overlay (magenta); (e) inset of blue dashed box in (d), unannotated; (f) inset of blue dashed box in (d), mirroring inset of (e) with annotation. Scale bars 1mm.
Figure 10.
Contralateral pullback of the lateral tongue. (a) En face projection with artifact overlay; (b) En face projection with epithelial thickness map. Color bar indicates 0 to 1.04mm thickness, with bright red indicating no visible basement membrane; (c) unannotated en face projection with red dashed line indicating location of longitudinal image in (d); (d) longitudinal image with predicted epithelial layer overlay (magenta); (e) inset of blue dashed box in (d), unannotated; (f) inset of blue dashed box in (d), mirroring inset of (e) with annotation. Scale bars 1mm.
Figure 11.
Grade 2 dysplasia of the lateral tongue. (a) En face projection with artifact overlay (cyan); (b) En face projection with epithelial thickness map. Blue to yellow color bar indicates 0 to 1.04mm thickness, with red indicating no visible basement membrane. White dashed lines flank predicted region of epithelial thickening and loss, also seen in (c) and (d); (c) unannotated en face projection with red dashed line indicating location of longitudinal image in (d); (d) longitudinal image with predicted epithelial layer overlay (magenta) and identified artifact overlay (cyan); (e) inset of yellow dashed box in (d), unannotated; (f) inset of yellow dashed box in (d) mirroring inset of (e) with annotation, green line indicating rater segmentation; (g) inset of blue dashed box in (d), unannotated; (h) inset of blue dashed box in (d), mirroring inset of (h) with annotation, green line indicating rater segmentation. Scale bars 1 mm.
Figure 11.
Grade 2 dysplasia of the lateral tongue. (a) En face projection with artifact overlay (cyan); (b) En face projection with epithelial thickness map. Blue to yellow color bar indicates 0 to 1.04mm thickness, with red indicating no visible basement membrane. White dashed lines flank predicted region of epithelial thickening and loss, also seen in (c) and (d); (c) unannotated en face projection with red dashed line indicating location of longitudinal image in (d); (d) longitudinal image with predicted epithelial layer overlay (magenta) and identified artifact overlay (cyan); (e) inset of yellow dashed box in (d), unannotated; (f) inset of yellow dashed box in (d) mirroring inset of (e) with annotation, green line indicating rater segmentation; (g) inset of blue dashed box in (d), unannotated; (h) inset of blue dashed box in (d), mirroring inset of (h) with annotation, green line indicating rater segmentation. Scale bars 1 mm.
Table 1.
Summary of dataset pathology.
Table 1.
Summary of dataset pathology.
| Diagnosis |
No. Scans |
% of Dataset |
No. Longitudinal Images |
% of Dataset |
| Contralateral (assumed normal) |
59 |
31.6 |
133 |
45.2 |
| Benign (pathology confirmed) |
14 |
7.5 |
19 |
6.5 |
| Scar |
3 |
1.6 |
4 |
1.4 |
| Trauma |
1 |
0.5 |
1 |
0.3 |
| Reactive Fibroma |
1 |
0.5 |
1 |
0.3 |
| Actinic Cheilitis |
2 |
1.1 |
3 |
1.0 |
| Hyperplasia |
2 |
1.1 |
2 |
0.7 |
| Verrucous Hyperplasia |
3 |
1.6 |
4 |
1.4 |
| Dysplasia Grade 1 |
24 |
12.8 |
31 |
10.5 |
| Dysplasia Grade 2 |
21 |
11.2 |
25 |
8.5 |
| Dysplasia Grade 3 |
12 |
6.4 |
18 |
6.1 |
| Carcinoma In Situ |
5 |
2.7 |
7 |
2.4 |
| Lentigo Maligna |
4 |
2.1 |
5 |
1.7 |
| OSCC |
27 |
14.4 |
32 |
10.9 |
| Verrucous Carcinoma |
9 |
4.8 |
9 |
3.1 |
| Total |
187 |
100.0 |
294 |
100.0 |
Table 2.
Summary of dataset imaging site.
Table 2.
Summary of dataset imaging site.
| Site |
No. Scans |
% of Dataset |
No. Longitudinal Images |
% of Dataset |
| Buccal Mucosa |
23 |
12.3 |
38 |
12.9 |
| Floor Of Mouth |
8 |
4.3 |
13 |
4.4 |
| Gingiva |
10 |
5.3 |
11 |
3.7 |
| Labial Mucosa |
4 |
2.1 |
8 |
2.7 |
| Lip |
1 |
0.5 |
1 |
0.3 |
| Tongue - Dorsal |
4 |
2.1 |
6 |
2.0 |
| Tongue - Lateral |
55 |
29.4 |
86 |
29.3 |
| Tongue - Ventral |
76 |
40.6 |
124 |
42.2 |
| Vestibule |
6 |
3.2 |
7 |
2.4 |
| Total |
187 |
100.0 |
294 |
100.0 |
Table 3.
Summary of discovery sets for deep learning tasks.
Table 3.
Summary of discovery sets for deep learning tasks.
| Task |
Model |
No. Patients |
No. Scans |
No. Images |
No. Tiles |
Tile Size (overlap) [pixels] |
FOV
Detection |
Classification |
9 |
9 |
2427 |
Class 0: 64,250
Class 1: 87,376 |
256x256 (128) |
Artifact
Detection |
Classification |
59 |
864 |
288 |
Class 0: 20,467
Class 1: 1,459 |
128x128 (64) |
Epithelial
Surface |
Segmentation |
59 |
864 |
288 |
11,356 |
256x256 (128) |
| Basement Membrane |
Segmentation |
59 |
864 |
288 |
11,356 |
256x256 (128) |
Table 4.
Distribution of features by deep learning task.
Table 4.
Distribution of features by deep learning task.
| Task |
Feature of Interest |
Distribution |
| FOV Detection |
Tissue Contact |
In FOV: ~60%
Out of FOV: ~40% |
| Artifact Detection |
Presence of Artifact |
Present: 7%
Absent: 93% |
| Epithelial Surface |
N/A |
N/A |
| Basement Membrane |
Epithelial Stromal Transition |
Complete: ~70%
Broken: ~15%
Absent: ~15% |
Table 5.
Training hyperparameters for model development.
Table 5.
Training hyperparameters for model development.
| Task |
No. of Epochs
(Early Stopping Epoch) |
Early Stopping Scheme |
Batch Size |
LR Scheduler |
| FOV Detection |
10
(2) |
patience = 5,
Δmin = 0.01
mode = min. loss |
64 |
patience = 3,
factor = 0.1,
min. LR = 1x10-8
|
| Epithelial Surface |
30
(19) |
patience = 5,
Δmin = 0.01
mode = min. loss |
8 |
patience = 5,
factor = 0.1,
min. LR = 1x10-8
|
| Basement Membrane |
20
(9, 8)*
|
patience = 5,
Δmin = 0.01
mode = min. loss |
8 |
patience = 5,
factor = 0.1,
min. LR = 1x10-8
|
| Artifact Detection |
30
(18) |
patience = 5,
Δmin = 0.01
mode = min. loss |
64 |
patience = 3,
factor = 0.1,
min. LR = 1x10-7
|
Table 6.
Test Set Metrics for FOV and Artifact Detection CNNs.
Table 6.
Test Set Metrics for FOV and Artifact Detection CNNs.
| Task |
No. Tiles |
Bal. Accuracy (%) |
Sensitivity (%) |
Specificity (%) |
AUC |
mAP |
| FOV |
17,404 |
100.0* |
100.0* |
100.0* |
1.00 |
1.00 |
| Artifact Detection |
2,345 |
75.5 |
99.1 |
52.3 |
0.94 |
0.68 |
Table 7.
Test set metrics for epithelial surface training protocols. Best results marked in bold.
Table 7.
Test set metrics for epithelial surface training protocols. Best results marked in bold.
| Training Protocol |
DSC |
ME (mm) (M ± SD) |
| ± 24 pixels |
0.99 |
0.4 ± 9.9 |
| ± 12 pixels* |
0.98 |
0.4 ± 9.1 |
| ± 4 pixels |
0.94 |
-0.9 ± 10.4 |
Table 8.
Test set metrics for basement membrane training protocols. The best results are bolded.
Table 8.
Test set metrics for basement membrane training protocols. The best results are bolded.
| Training Protocol |
DSC |
PA (%) |
NA (%) |
ME (mm) (M ± SD) |
| ± 12 pixels |
0.91 |
95.8 |
80.9 |
2.9 ± 21.5 |
| ± 4 pixels |
0.76 |
93.1 |
75.1 |
0.1 ± 16.2 |
| ± 12 à ± 4 pixels* |
0.83 |
95.8 |
81.7 |
-0.5 ± 19.3 |
| ± 24 à ± 4 pixels |
0.76 |
95.1 |
80.1 |
1.5 ± 20.3 |
| ± 24 à ± 12 à ± 4 pixels |
0.79 |
95.3 |
81.2 |
-0.1± 19.8
|
Table 9.
Rater-Reference metrics for segmentation networks.
Table 9.
Rater-Reference metrics for segmentation networks.
| Task |
Metric |
Model |
Rater 1 |
Rater 2 |
Rater 3 |
Rater 4 |
Rater 5 |
| Epithelium |
DSC |
0.98 |
0.96 |
0.96 |
0.97 |
0.97 |
0.95 |
| ME (µm) |
0.4 ± 9.1 |
5.4 ± 11.4 |
2.1 ± 11.2 |
2.4 ± 11.1 |
3.6 ± 10.7 |
7.2 ± 13.5 |
| Basement Membrane |
DSC |
0.83 |
0.78 |
0.64 |
0.75 |
0.75 |
0.73 |
| PA (%) |
95.8 |
97.2 |
89.2 |
95.1 |
95.4 |
87.9 |
| NA (%) |
81.7 |
85.3 |
69.1 |
67.9 |
74.0 |
56.8 |
| ME (µm) |
-0.5 ± 19.3 |
0.6 ± 24.2 |
2.9 ± 32.8 |
-3.8 ± 24.8 |
-1.7 ± 18.5 |
-0.5 ± 14.7 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).