Introduction
Ankle fractures represent 10% of all fractures with an incidence of about 137/10
5 population per year. It is the second most common lower limb fracture following hip fracture [
1]. In contrast, acute rupture of the Achilles tendon is also one of the common tendon injuries in adults, that occurs due to sudden dorsiflexion of a plantar flexed foot and is most commonly associated with sports activities like “weekend warrior’’ participating in basketball, soccer, and volleyball [
2,
3].
Although ankle fractures and Achilles tendon injuries are among the common traumatic presentations when they occur separately, concurrent Achilles tendon rupture and ipsilateral ankle fractures are extremely rare. Interestingly, one of the two injuries is often missed in the initial presentation in the majority of the previous reports. Even if the history and physical examination provide high sensitivity and specificity in the diagnosis of acute Achilles tendon rupture [
4], especially in cases with obvious traumatic wounds over the tendon substances, like in our patient, routine imaging studies are very important to prevent incomplete diagnosis [
5].
Our review of the literature revealed only fifteen single cases of ankle fractures associated with Achilles tendon rupture have been reported. Among these, 12 reported cases of Achilles tendon rupture were associated with medial malleolar fracture [
6,
7,
8,
9,
10,
11,
12,
13,
14,
15,
16,
17], 2 cases of Achilles tendon rupture were in combination with lateral malleolar fracture, [
2,
18] and only 1 case of acute Achilles tendon rupture with ipsilateral open bimalleolar ankle fracture was reported [
19].
The present case is the first report of a closed bimalleolar ankle fracture that was initially missed and only discovered intraoperatively while repairing of an open Achilles tendon rupture.
Case Presentation
A 34-year-old male patient presented after sustaining a road traffic accident of one-day duration. He was a pedestrian blown by a moving car while he was trying to cross a road. He is a marchant and has no previous complaints over the injury site. His past medical history is unremarkable.
On physical examination, he was unable to actively plantarflex his right ankle and a transverse 8 x 2cm wound over the posterior aspect of the right distal leg (
Figure 1). The Thompson test (Calf-squeeze) was positive, confirming complete Achilles tendon rupture. Otherwise, distal neurovascular structures were intact and no other site injuries were identified.
He was started IV-antibiotic, and dressed with sterile gauze. The short-leg posterior gutter was applied and the patient was taken to the operation theater for emergency irrigation and debridement with possible tendon repair.
Surgical Procedure
After getting written informed consent, the patient was taken to the operation theater the following day. Under spinal anesthesia, the patient was put into a prone position, and with a possible aseptic technique, the right lower limb was draped. Next, a longitudinal incision was made over the medial side of the Achilles tendon, integrating the traumatic laceration. A complete laceration of the Achilles tendon was identified about 8 cm proximal to its insertion. The wound was thoroughly irrigated with normal saline and the tendon ends were mobilized and debrided. However, in the middle of the procedure, one of the operating team members identified the fracture end of the lateral malleolus while retracting the lateral edge of the surgical incision. There was no fluoroscopy in the operating room and we decided to have a control X-ray after the tendon repair. The tendon was repaired with Vicryl #2 round in a Krackow fashion and paratenon was repaired with absorbable suture (vicryl 4-0 round). Skin and subcutaneous tissue were closed in layers.
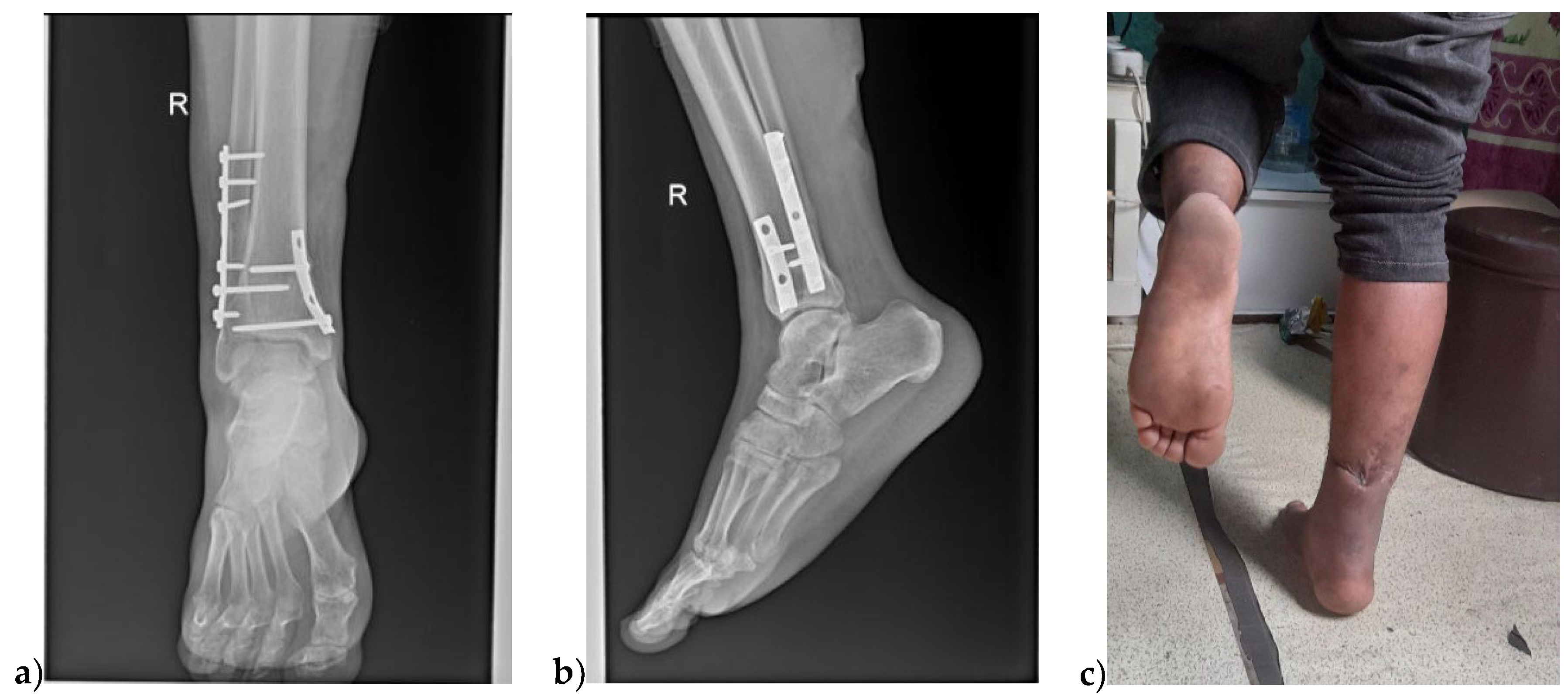
X-ray images were taken on the following day and showed a bimalleolar ankle fracture; vertically oriented non-displaced medial malleolar fracture and supra-syndesmotic lateral malleolus fracture (
Figure 2).
On the 3rd post-op, day the patient was re-draped in a supine position to proceed with the bimalleolar fracture fixation. First, through an anteromedial approach, about 8 cm of skin incision is made over the anterior third of the medial malleolus. A long saphenous vein was identified and protected. The ankle joint capsule was incised to visualize the articular surface reduction and the medial malleolus was stabilized with a pointed reduction clamp and buttressed with a 4-holed 1/3rd tubular plate (
Figure 3).
The lateral malleolus was approached with a direct lateral skin incision centered over the fracture site. A superficial peroneal nerve was identified while crossing anterior, the periosteum was elevated to expose the fracture site. The fracture was reduced and stabilized with a seven-holed 1/3rd tubular plate(
Figure 4). Wounds were dressed with a sterile gauze and a long leg gutter was applied in a 20
0 plantarflexed ankle position.
Follow-up and Outcomes
We discharged him on his 7th post-op day with 20
0 plantarflexed foot. At 2 weeks postoperatively, the wound sites were healed and suture materials were removed. At 6 weeks control X-ray was taken and showed the bimalleolar fracture was healing and active range of motion exercise started with a hinged ankle-foot orthosis. At 12 weeks the fracture consolidated and the patient was allowed full weight-bearing with some jogging. During his 6-month postoperative time, he was completely asymptomatic and able to perform single-legged heel raise exercises(
Figure 5).
Discussion
The combination of acute Achilles tendon rupture with ipsilateral ankle fracture is extremely infrequent, while both injuries are very common in isolation. The diagnosis of this concurrent injury has usually been reported to be delayed [
8,
12,
15,
20]. Thus, knowledge of these injury patterns will help clinicians to have a high index of suspicion and perform careful history with a thorough physical examination of musculoskeletal structures in the treatment of patients with concomitant Achilles tendon rupture and ankle fracture [
5].
Our review of the literature showed that medial malleolar fracture is the most frequent ankle fracture associated with Achilles tendon rupture followed by lateral malleolus [
2,
8,
10,
11,
12,
14,
15,
18,
20]. There is only one bimalleolar ankle fracture with concurrent Achilles tendon rupture reported, in which the tendon injury was missed on the initial evaluation and diagnosed intra-operatively [
19]; however, in our patient, the fact that there was an obvious wound over the Achilles rupture site deceived us from suspecting the presence of ankle fracture. An obvious clinical diagnosis of Achilles tendon rupture is also reported as one of the reasons for the misdiagnosed ankle fracture in this group of patients [
15].
Though the exact mechanism of this rare orthopedic injury is not known, sudden force applied to the forefoot and ankle, with subsequent hyperextension of the ankle and/or hindfoot inversion, remains implicated. Assal et al. suggested that patients with supination adduction ankle fracture pattern have a high likelihood of associated Achilles tendon rupture [
9]; however, in our patient, although medial malleolar fracture resembles the supination adduction fracture pattern, the level of fibular fracture is above the syndesmosis which doesn’t fit with supination adduction classification. The fact that there was an open wound at the tendon laceration site and the fibular fracture was near this wound; we believe that both Achilles tendon laceration and fibular fracture were caused by the same force and then medial malleolus fractured with inverted hindfoot.
Imaging studies play a crucial role in patients with acute Achilles tendon injury both to confirm the diagnosis and to rule out any possible accompanying injuries. The bimalleolar fracture was missed initially in the current patient and was only diagnosed intraoperatively by finding the fracture end of the fibula while exploring the wound for thorough debridement. During the initial procedure, thorough debridement of the wound and Achilles repair was done at the emergency time. Subsequently, an anteroposterior and lateral radiograph of the ipsilateral ankle joint was taken confirming a bimalleolar ankle fracture. Three days later the bimalleolar fracture was fixed on an elective basis and put in a 200 equinus splint. Therefore, the present report shows the importance of routine X-rays in patients with acute traumatic Achilles tendon rupture even if clinical examination confirms complete rupture.
Regarding the management of acute Achilles tendon rupture the ideal treatment option remains a topic of debate. According to recent research, conservative treatment with particular rehabilitation protocols produces comparable results in terms of healing, functional outcomes, and re-rupture rates as compared to surgical repair, which is typically recommended in younger, more active patients [
21,
22]. However, the management of acute Achilles tendon rupture associated with ipsilateral ankle fracture leads to increased disability and decreased quality of life, which requires a more comprehensive approach and close coordination between the patient and the health care team. We utilized open-surgical intervention as both the tendon injury and bimalleolar fracture have an absolute indication.
Conclusion
In conclusion the current case report should serve as a reminder to consider ligamentous or osseous ankle injuries in situations of acute Achilles tendon rupture. A thorough history and physical examination should be supplemented with routine anteroposterior and lateral X-rays to detect any associated fracture with acute Achilles tendon rupture. This report not only serves as a valuable learning resource but also provides insight that contributes to evidence-based medical practice.
Ethics and Consent
The patient provided informed consent for the publishing of this case report and accompanying photographs, and the hospital approved the cases.
Disclosure
There is no conflict of interest among the authors of this paper.
References
- Tornetta, P. Rockwood and Green’s fractures in adults 9th edition. 2020. 4528–4530 p.
- Pyle, L.H.; Al-Gharib, R.W.; Kissel, E.C. Lateral Malleolar Fracture with Concurrent Achilles Tendon Rupture: A Case Report and Literature Review. Case Rep. Emerg. Med. 2020, 2020, 6479140–4. [Google Scholar] [CrossRef] [PubMed]
- Erickson, B.J.; Cvetanovich, G.L.; Nwachukwu, B.U.; Villarroel, L.D.; Lin, J.L.; Bach, J.B.R.; McCormick, F.M. Trends in the Management of Achilles Tendon Ruptures in the United States Medicare Population, 2005-2011. Orthop. J. Sports Med. 2014, 2. [Google Scholar] [CrossRef]
- Kauwe, M. Acute Achilles Tendon Rupture. Clin Podiatr Med Surg. 2017 Apr;34(2):229–43.
- Elmajee, M.; Rafee, A.; Williams, T. Ankle Fracture Associated With Rupture of the Achilles Tendon: Case Report and Review of the Literature. J. Foot Ankle Surg. 2017, 56, 1320–1322. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.W.; Thompson, G.H. Achilles tendon rupture. Occurrence with a closed ankle fracture.. 1986, 216–8. [Google Scholar] [CrossRef]
- Barron, J.L.; Yocum, L.A. Unrecognized Achilles tendon rupture associated with ipsilateral medial malleolar fracture. Am. J. Sports Med. 1993, 21, 629–631. [Google Scholar] [CrossRef] [PubMed]
- Pieper HG, Radas CB, Quack G, Krahl H. Mediomalleolar fracture combined with Achilles tendon rupture - A rare simultaneous injury of the ankle. Int J Sports Med. 1998;19(1):68–70.
- Assal MSRPR. Fracture of the Ankle Associated With Rupture of the Achilles Tendon: Case Report and Review of the Literature. J Orthop Trauma. 2002 ;358–61. 16 May.
- Lubin JW1, Miller RA, Robinson BJ BF. Achilles tendon rupture associated with ankle fracture.
- Garneti, N.; Muralikuttan, K.; Shenolikar, A. Ankle fracture associated with an Achilles tendon rupture: a rare injury. Foot Ankle Surg. 2005, 11, 219–222. [Google Scholar] [CrossRef]
- Masamitsu Tanaka, HS. Concurrent occurrence of Achilles tendon rupture and medial malleolar fracture of the ankle joint: a case report. The Internet Journal of Orthopedic Surgery. 2009;15(1).
- Maffulli, N.; Richards, P.J. Subcutaneous rupture of the Achilles tendon and ipsilateral fracture of the medial malleolus. BMC Musculoskelet. Disord. 2006, 7, 59–59. [Google Scholar] [CrossRef] [PubMed]
- Türkmensoy, F.; Türkmen, I.; Turhan, Y.; Özkan, K.; Akçal, M.A. Achilles Tendon Rupture with Isolated Medial Malleolar Fracture in Ipsilateral Ankle: A Case Report. Open J. Orthop. 2013, 03, 224–226. [Google Scholar] [CrossRef]
- Nakajima, K.; Taketomi, S.; Inui, H.; Nakamura, K.; Sanada, T.; Tanaka, S. Missed Medial Malleolar Fracture Associated With Achilles Tendon Rupture: A Case Report and Literature Review. J. Foot Ankle Surg. 2016, 55, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Elmajee, M.; Rafee, A.; Williams, T. Ankle Fracture Associated With Rupture of the Achilles Tendon: Case Report and Review of the Literature. J. Foot Ankle Surg. 2017, 56, 1320–1322. [Google Scholar] [CrossRef] [PubMed]
- Bowers, M.; Hunt, K.J.; Metzl, J. High-Energy Achilles Tendon Rupture With Associated Medial Malleolus Fracture and Traumatic Peroneal Dislocation: A Case Report. Foot Ankle Spéc. 2021, 14, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Mattos e Dinato MC, de Farias Freitas M, D’Elia CO, Bitar AC, Rodrigues Gonçalves FM. Acute calcaneus tendon rupture associated with ipsilateral malleolar fracture: Case report and literature review. Journal of Foot and Ankle Surgery. 2010;49(6):565.e1-565.e4.
- Sarrel, K.; Girard, P. Gustilo IIIA Open Bimalleolar Fracture Dislocation of Ankle with Ipsilateral Achilles Tendon Rupture. J. Bone Jt. Surg. 2021, 11. [Google Scholar] [CrossRef]
- Lu, J.; Holledge, M.M. Medial malleolus fracture of the ankle combined with rupture of the Achilles tendon. J. Surg. Case Rep. 2016, 2016, rjw062. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-C.; Chen, P.-Y.; Yang, K.-C.; Wang, C.-L.; Chen, I.-H. Current treatment concepts for Achilles tendon rupture. Tzu Chi Med J. 2024, 36, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Maffulli, N. In Adults with Acute Achilles Tendon Rupture, Nonoperative Treatment, Open Repair, and Minimally Invasive Surgery Did Not Differ for Health Status at 12 Months. J. Bone Jt. Surg. 2022, 104, 2035–2035. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).